Abstract
Adult patients with severe chronic small intestinal dysmotility are not uncommon and can be difficult to manage. This guideline gives an outline of how to make the diagnosis. It discusses factors which contribute to or cause a picture of severe chronic intestinal dysmotility (eg, obstruction, functional gastrointestinal disorders, drugs, psychosocial issues and malnutrition). It gives management guidelines for patients with an enteric myopathy or neuropathy including the use of enteral and parenteral nutrition.
Keywords: small intestinal motility, nutrition support
1.0 Formulation of guidelines
1.1 Aim
This guideline aims to help clinicians manage patients who have or are thought to have severe small intestinal dysmotility that is causing malnutrition. It gives a logical guidance to determining the underlying diagnosis and shows how, knowing this, treatments may be tailored for each individual patient. It also aims to present some of the other factors contributing to the presentation and progress of the illness.
1.2 Development
The preliminary guidelines were compiled from the literature and a first document was drafted by Dr Nightingale and modified by members of the Neuro-gastroenterology and Motility Committee of the British Society of Gastroenterology (BSG) and by the Small Bowel and Nutrition Committee of the BSG. The article was reviewed by the patient organisation PINNT (Support and Advocacy group for people on home artificial nutrition) and modifications made to result in the current document.
The guidelines have applied the GRADE system.1 Strength of recommendation can be strong, moderate or weak. The evidence was graded according to the Oxford Centre for Evidence-based Medicine.2 Level 1 includes systematic reviews with homogeneity, individual randomised controlled trials (RCTs); level 2 includes systematic reviews of cohort studies, low quality RCTs and outcomes research; level 3 includes systematic reviews with heterogeneity and individual case–control studies; level 4 includes poor quality cohort or case series; and level 5 includes expert opinion without critical appraisal.
1.3 Scheduled review
The content and evidence base for these guidelines should be reviewed within 5 years of publication. We recommend that these guidelines are audited and request feedback from all users.
1.4 Service delivery
Patients with severe chronic small intestinal dysmotility are not common but should be managed by a multidisciplinary team headed by a clinician with expertise in managing these patients. If managed appropriately, particularly if receiving parenteral nutrition (PN), there may be an improved quality of safe care and also considerable cost savings. (Grade of evidence level 4, Strength of recommendation strong)
Any surgical procedure should be performed after extensive local/regional multidisciplinary team (MDT) discussions at hospitals with surgeons and histopathologists experienced in managing these patients. (Grade of evidence level 5, Strength of recommendation strong)
Patients being considered for PN or a surgical bypass/resection should be seen at a dedicated PN centre or by an integrated intestinal failure (IF) unit respectively. (Grade of evidence level 5, Strength of recommendation strong)
Regional networks may be established to ensure expertise is available to all and a national research forum may be established. (Grade of evidence level 5, Strength of recommendation strong)
1.5 Patients' experience
Patients with a severe chronic small intestinal dysmotility causing malnutrition should be managed as individuals; other factors including opioid use and psychosocial circumstances must be taken into account. (Grade of evidence level 5, Strength of recommendation strong)
Patients will become experts in coping with their condition and management. All decisions should be made in conjunction with them. They are often more knowledgeable about their condition and treatments than the clinicians, nurses and dietitians and this should be respected. (Grade of evidence level 5, Strength of recommendation strong)
Facilities for looking after these patients should be able to deal with physical, emotional, psychological, social and quality of life issues. (Grade of evidence level 5, Strength of recommendation strong)
Patients should be referred rapidly to places of more advanced expertise if management is difficult or unsuccessful. There should be a clinician, specialist nurse and/or a dietitian available and a psychologist/psychiatrist to discuss the patients. The healthcare professionals should be familiar to the patient and know their history, thus eliminating the need for lengthy, time-consuming explanations. (Grade of evidence level 5, Strength of recommendation strong)
The patients should be managed on wards or IF/home parenteral nutrition (HPN) units where the healthcare professionals are familiar with their specialist needs, especially if receiving PN. (Grade of evidence level 5, Strength of recommendation strong)
Patients, especially if receiving HPN, should have access to a helpline (ideally 24 hours) so that emergencies are dealt with appropriately and quickly. (Grade of evidence level 5, Strength of recommendation strong)
Written and audiovisual materials that explain and support the training techniques in enteral and PN should be available. (Grade of evidence level 5, Strength of recommendation strong)
Meeting other patients with similar problems may improve the way in which a patient copes with their condition. (Grade of evidence level 5, Strength of recommendation strong)
Where appropriate, patients should be offered contact numbers for the relevant support group that represents their specific disease. (Grade of evidence level 5, Strength of recommendation strong)
Follow-up appointments should be as deemed appropriate to the MDT and patient, and ideally the patient should not have to travel long distances for appointments. The appointment should be with experienced and familiar staff, thus enabling continuity of care. (Grade of evidence level 5, Strength of recommendation strong)
Staff should be aware of the latest research and developments and should make patients aware of any which may apply to them. (Grade of evidence level 5, Strength of recommendation strong)
For patients needing home parenteral nutrition (HPN)
The techniques needed for HPN should be taught by competent and enthusiastic staff who can convey the confidence required to undertake the therapy successfully and safely. The procedures taught should follow the British Intestinal Failure Alliance (BIFA) standardised parenteral support catheter guidelines.3 (Grade of evidence level 5, Strength of recommendation strong)
Patients need to know that an aseptic technique, in which the key parts are not touched, must be used whenever their feeding line is accessed. This is vital for safety and peace of mind. (Grade of evidence level 4, Strength of recommendation strong)
All patients who require HPN whether short or long term should receive information about the patient support group ‘PINNT’ (Support and Advocacy group for people on home artificial nutrition) and should be registered with the British Artificial Nutrition Survey (BANS). (Grade of evidence level 5, Strength of recommendation strong)
2.0 Summary of recommendations
2.1. Enteric myopathies are often a primary condition and have multi-visceral involvement (especially of urinary tract) and these other manifestations should be sought. Enteric myopathies may be secondary to a muscular disease (eg, muscular dystrophy) and an awareness of this is needed when managing the primary illness. (Grade of evidence level 5, Strength of recommendation strong)
2.2. Patients with an enteric neuropathy often have a serious underlying condition (often neurological or metabolic) which should be sought. (Grade of evidence level 5, Strength of recommendation strong)
2.3. A definite diagnosis should only be given when a detailed history, symptoms and investigations (including histology in a unit that has expertise in this area of pathology) confirm the diagnosis. If, as is commonly the case, a definitive diagnosis is not possible, an empirical working diagnosis of probable severe dysmotility may be necessary. (Grade of evidence level 5, Strength of recommendation strong)
2.4. Mechanical obstruction must be excluded and occasionally (if radiology is inconclusive) this involves a trial of a low fibre (residue) diet or even a liquid diet. (Grade of evidence level 5, Strength of recommendation strong)
2.5. The contributing effects of drugs on gut motility (especially opioids and anticholinergics) must be taken into account. (Grade of evidence level 4, Strength of recommendation strong)
2.6. Psychosocial/behavioural issues often play a part in how the symptoms manifest and specialist psychosocial support must be available expediently. (Grade of evidence level 5, Strength of recommendation strong)
2.7. The effects of abrupt weight loss on the gut function must be taken into account. (Grade of evidence level 5, Strength of recommendation strong)
2.8. Investigations which include radiology, radioisotope studies, manometry, autoimmune screens and histology should be performed judiciously and in keeping with current guidelines, but may not give a definitive diagnosis. Care must be taken in interpreting them in the presence of some drugs (eg, opioids, cyclizine or anticholinergic drugs), severe malnutrition or an eating disorder. (Grade of evidence level 5, Strength of recommendation strong)
2.9. These patients are complex with multiple issues contributing to their presentation and so they need MDT management. The team is likely to include a gastroenterologist, gastrointestinal physiologist, gastrointestinal surgeon, pain team, psychiatrist/psychologist, rheumatologist (including fatigue management), urologist, gynaecologist, radiologist, dietitian, specialist nurses, clinical biochemist, histopathologist and pharmacist. Regional networking (can be via a virtual MDT) is encouraged both for support/guidance and to collect data. (Grade of evidence level 5, Strength of recommendation strong)
2.10. The aims of treatment for patients with severe chronic small intestinal dysmotility are where possible to:
Reduce symptoms (eg, pain, vomiting, distension, constipation/diarrhoea, bloating/distension)
Reduce morbidity and mortality
Achieve a body mass index (BMI) within the normal range
Achieve an improved/good quality of life. (Grade of evidence level 5, Strength of recommendation strong)
2.11. Treatment should be directed at the main symptom, using as few drugs as possible, avoiding high doses of opioids and cyclizine and avoiding unnecessary surgery. Try to avoid medicalisation (eg, enteral access, suprapubic catheters, etc) early in the course of the illness. (Grade of evidence level 5, Strength of recommendation strong)
2.12. If the patient has taken long-term opioids, the narcotic bowel syndrome may have occurred and a gradual supervised opioid withdrawal should be considered. A pain specialist, if available, should be involved. (Grade of evidence level 4, Strength of recommendation strong)
2.13. If a patient is malnourished or at risk of becoming so, oral supplements/dietary adjustments should be tried. (Grade of evidence level 5, Strength of recommendation strong)
2.14. If feeding by the oral route is unsuccessful and if the patient is not vomiting, gastric feeding may be tried. (Grade of evidence level 5, Strength of recommendation strong)
2.15. If gastric feeding is unsuccessful, jejunal feeding initially via a nasojejunal tube may be tried and, if successful, a tube can be inserted endoscopically (through a gastrostomy (PEGJ) or as a direct jejunostomy) or surgically. A jejunostomy also can be useful for drug administration. (Grade of evidence level 5, Strength of recommendation strong)
2.16. If jejunal feeding fails (often due to abdominal distension or pain as the feed is infused) and if the patient is malnourished, then parenteral support may be needed. (Grade of evidence level 5, Strength of recommendation strong)
2.17. A venting gastrostomy may reduce vomiting but can have problems (leakage, not draining, or poor body image). (Grade of evidence level 5, Strength of recommendation strong)
2.18. Nutritional status, when possible, should be optimised before any surgical procedure. A percutaneous endoscopic gastrostomy (PEG) or stoma is generally delayed in severely malnourished or physiologically unfit patients. (Grade of evidence level 5, Strength of recommendation strong)
3.0 Key terms and definitions used in the guideline
Many terms are used in the literature. Only chronic intestinal pseudo-obstruction (CIPO) has been consistently used in the past to imply a dilated gut that does not function. Other terms such as 'enteric dysmotility' have been used to define the 'grey area' sitting between the functional gastrointestinal disorders and more severe CIPO. Enteric dysmotility has been primarily defined by manometric abnormalities, although histological abnormalities can also be found. It lacks the small bowel dilatation seen in CIPO and its current classification status remains uncertain.
In the past, different diagnostic labels have been given to patients based on the diagnostic test used. Unfortunately they are given to patients according to which diagnostic test is used. Currently they have not been merged to point to a specific diagnosis, which can be best given by histology. The histology may show abnormalities, but the extent they are due to malnutrition, previous surgery (including defunctioning bowel) or drug therapy is not completely clear.
Phrases that may be found on investigations
Radiology
slow transit
dilated bowel
no transitional zone
Scintigraphy
slow transit (gastric emptying, small bowel or colon) of liquid/solid
Manometry
propulsive failure
giant contractions
no migrating motor complexes (MMCs)
Pathological
neuropathy
plexitis, leiomyositis
myopathy
In this document the term 'intestinal dysmotility' is used to cover all conditions in which there is a failure to propel the luminal contents without there being an organic obstructing lesion. The intestinal dysmotility is considered severe when nutritional or fluid support is needed due to objective evidence of malnutrition, dehydration or electrolyte disturbance.
This guideline relates to adults and does not cover acute pseudo-obstruction (eg, ileus).
4.0 Introduction
Chronic small intestinal dysmotility occurs when there is a failure of coordinated intestinal propulsion, giving rise to the symptoms and signs of intestinal obstruction (colicky abdominal pain, nausea, vomiting usually with abdominal distension, and often a dilated bowel) in the absence of a mechanical cause.4 5 A frank obstructive picture with distended bowel is not always the case, especially if there is a neurological aetiology. For the purpose of this article, chronic will be taken as more than 6 months of symptoms. Chronic intestinal dysmotility may be defined as severe when there is associated malnutrition (BMI of less than 18.5 kg/m2 or more than 10% unintentional weight loss in last 3 months) and thus specific treatments which may include clinically assisted nutrition and hydration (CANH, formerly referred to as artificial nutritional support) may be needed.
Normal gastrointestinal motility is determined by intestinal smooth muscle function which in turn is influenced by neural and humoral factors. A disorder of one or more of these systems can result in intestinal pseudo-obstruction.4 There are many causes of acute or reversible/temporary intestinal dysmotility which include abdominal surgery, trauma, sepsis, metabolic (eg, hypokalaemia) or endocrine problems (eg, hypothyroidism), but they will not be discussed in this document as they do not usually result in long-term malnutrition. Dysmotility may occur in the small bowel and also in other areas of the gastrointestinal tract (eg, oesophagus, stomach and colon) and their involvement may complicate diagnostic tests and treatments. The primary problems with isolated oesophageal, gastric or colonic motility are not specifically discussed. Other medical causes of abdominal pain (eg, familial Mediterranean fever, angio-oedema, abdominal migraine and lead poisoning) are not specifically discussed but the clinician must be aware of them.
The diagnosis of these patients can be very difficult and may be empirical, especially when, as is most common, there is no definite histological confirmation of a disease process. The clinical features, results of investigations (eg, manometry) and histology may not all combine to indicate one specific diagnosis. Other factors that can give rise to the clinical picture or aggravate the condition are: unrecognised organic small bowel obstruction/the effects of previous abdominal surgery (including adhesions and neuropathic pain), drug usage (particularly opioids and drugs with anticholinergic effects), psychosocial problems including abnormal illness behaviour and malnutrition. In practice, all of these often play a part and contribute to the patient’s presentation. Untangling which of these factors gives rise to the dominant symptom can be challenging and needs the help of a MDT consisting of a gastroenterologist, gastrointestinal physiologist, gastrointestinal surgeon, pain team, psychiatrist/psychologist, rheumatologist (including a specialist in fatigue management), urologist, gynaecologist, neurologist, clinical biochemist, histopathologist, radiologist and nutritional support team.
If there is uncertainty about the diagnosis, this should be clearly documented and the diagnosis only described as working (probably or possible) and the contributing factors to this should be stated on the patient’s problem list (eg, previous surgery, opioid or cyclizine use, psychosocial problems or undernutrition). A definitive diagnosis should only be given if there is a clear cause identified. It is very difficult to remove a diagnostic label once it has been given, and a premature or erroneous organic diagnosis in those with predominantly psychosocial issues or abnormal illness behaviour may make the management of contributing issues very difficult. A definite diagnosis, although satisfying to have, rarely affects the patient’s clinical management from a medical perspective.
This document discusses the differential diagnoses, the medical and nutritional treatment of chronic small intestinal dysmotility (myopathy and neuropathy) which result in malnutrition. In its most severe form, patients with small bowel dysmotility may need long-term PN or even a small intestinal transplant, while in a milder form dietary adjustments may suffice.
5.0 Conditions that mimic or can contribute to the presentation
A patient with suspected small bowel dysmotility will have had basal investigations to exclude other causes; these include inflammatory markers (CRP, albumin, platelets and faecal calprotectin) which, if normal, make active inflammatory bowel disease unlikely. These may be followed, as appropriate, with the use of endoscopies and cross-sectional imaging including with intravenous contrast to diagnose structural/mucosal diseases. Several other conditions may appear as severe chronic intestinal dysmotility but with no primary bowel pathology (figure 1). In one series the most frequent misdiagnoses for dysmotility were volvulus, megacolon and chronic constipation.6
Figure 1.
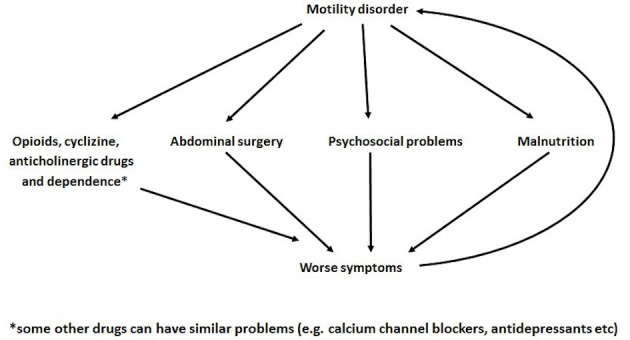
Progression of chronic small intestinal dysmotility.
5.1 Organic obstruction
A major problem, that is often not diagnosed, is a localised bowel obstruction as a result of adhesion formation. This may be suspected clinically when a patient has had a number of abdominal operations (with or without extensive adhesion division).7 A history of intermittent colicky abdominal pain with abdominal distension, loud bowel sounds, no bowel or stoma action and vomiting suggest this. A distal obstruction is suggested if the vomit is faeculent, while a more proximal one by green/yellow vomit. During an obstructive episode the bowel secretes more fluid, and when the obstruction resolves, diarrhoea follows (or a high stomal output). If a patient sticks to a low residue diet or even a liquid diet, the obstructive episodes may reduce or even be abolished. This approach, if successful, can be a useful supportive diagnostic test.
Radiologically, the clue to an organic obstruction is the demonstration of a distinct transition point between dilated and normal sized bowel, but this may not be apparent either because the obstruction has resolved or the bowel is fixed by adhesions and thus cannot dilate. It can be helpful to obtain an abdominal CT scan when the patient has an episode of severe pain. Contrast follow through studies or MRI scans, although useful when positive, may not be tolerated in the acute setting and do not always demonstrate the obstruction. Unsuspected diagnoses may be revealed (eg, small bowel volvulus from a band adhesion or an intussusception). Further clues to an organic obstruction are visible small bowel peristalsis, worse pain after prokinetic drugs or giant jejunal contractions on manometry.8 9
Multiple laparotomies themselves may result in secondary dysmotility, especially if the bowel becomes encased in fibrous tissue as can occur with sclerosing peritonitis. In addition, upper gut surgery (eg, a vagotomy, Whipple’s resection, gastro-enterostomy, bariatric procedures or any bowel anastomosis) can result in secondary small bowel dysmotility.10
Radiation damage can cause strictures and a localised obstruction and/or a generalised secondary dysmotility. Problems caused by radiation damage tend to be progressive over many years.
5.2 Opioid and other drug effects on the bowel
Opioid-induced bowel dysfunction can result from both opioid withdrawal and chronic opioid usage and manifests with features of dysmotility (especially constipation) when pain is not the dominant issue. The narcotic bowel syndrome may result from chronic usage and is defined as chronic, worsening or frequently occurring abdominal pain despite continued or escalating doses of narcotics in addition to dysmotility.11 The opioid usage induces a hyperalgesic effect. It may be becoming more prevalent but it is often not recognised by clinicians.12 13 In addition to being acknowledged to occur in patients with gastrointestinal disease (functional or organic), it also occurs in patients with no pre-existing gastrointestinal problems who take high doses of the opioids for other painful conditions (eg, joint problems or following surgery).
The components of therapy for narcotic bowel syndrome are recognition of the disorder, a trusting therapeutic relationship with the patient, replacement using neuropathic type pain drugs and controlled reduction in the opioid dose.14 Specific drug treatments have been tried for opioid-induced bowel dysfunction and narcotic bowel syndrome and include clonidine (to reduce withdrawal symptoms) and peripheral mu opioid antagonists (naloxone, methylnaltrexone, alvimopan).15–17
Opioids inhibit intestinal motility and so invalidate the tests of small bowel motility. They may also increase the risk of line infections in patients on long-term PN.
Survivors of cancer treatment may have bowel dysmotility which may be due to chemotherapy or opioid medication. Their management may require a wider MDT input.
Cyclizine is both an antihistamine and anticholinergic drug which acts as a centrally acting anti-emetic. There are many reports of it being taken for its euphoric effect, which is most marked when taken intravenously. In addition to causing addictive behaviour, it is of a low pH and so damages veins. It is not recommended for long-term use, especially in patients receiving PN.18
Other drugs such as anticholinergics, antidepressants, calcium channel blockers, chronic laxative abuse or some chemotherapeutic drugs (eg, vincristine) may also cause reduced gut propulsion.
5.3 Functional gastrointestinal disorders
Many of the symptoms of small intestinal dysmotility are the same as for patients with other functional abdominal gastrointestinal disorders (eg, irritable bowel syndrome, functional dyspepsia, cyclical vomiting, functional bloating/distension, functional constipation/diarrhoea and centrally mediated disorders of gastrointestinal pain).19
The differentiation and overlap with these functional gastrointestinal disorders is difficult. They all may have genetic and psychosocial influences (early life trauma, life stresses, coping mechanisms, lack of social support, etc). In addition, bacterial flora, inflammation, visceral sensation and motility may all contribute to the symptoms. In irritable bowel syndrome there may be an overlap with enteric neuropathy as increased lymphocytes have been observed in the jejunal myenteric plexus.20 However, significant malnutrition is rarely a consequence of these disorders.
The treatment—as for all dysmotility problems—is to identify and treat the main symptom. If weight loss has occurred, then the same therapies as for intestinal dysmotility may be tried at the same time as nutritional support is given. Significant caution should be exercised, however, to avoid escalating to more invasive forms of nutrition support in patients with functional symptoms, especially in pain predominant presentations, in the absence of objective features of biochemical disturbance or those who have a high or normal BMI. Such escalation of invasive intervention in these patients is subject to risks of iatrogenesis, and in clinical practice experience does not appear to improve global function, quality of life or symptoms.
5.4 Psychological/psychiatric problems
5.4.1 Anorexia nervosa
The American Psychiatric Association (APA) Diagnostic and Statistical Manual of Mental Disorders (DSM- 5) stated in 2013 that to diagnose a person with anorexia nervosa they must display: (1) persistent restriction of energy intake leading to significantly low body weight (in context of what is minimally expected for age, sex, developmental trajectory and physical health); (2) either an intense fear of gaining weight or of becoming fat, or persistent behaviour that interferes with weight gain (even though significantly low weight); (3) disturbance in the way one's body weight or shape is experienced, undue influence of body shape and weight on self-evaluation, or persistent lack of recognition of the seriousness of the current low body weight.21
However, the patients that present to gastroenterologists often do not have this typical presentation. Delayed gastric emptying, especially of solid, and delayed small and large bowel transit have been described in patients with anorexia nervosa.22–25 There is a report of a patient having a mega-duodenum and no propagating MMCs which both improved with an increased nutritional intake.26
5.4.2 Avoidant/restrictive eating
Some patients who have had psychosocial problems in the past may have disordered gut motility partly due to a disordered eating pattern, undernutrition and the drug treatments which they received.27
5.4.3 Psychiatric disorders and psychological distress
Other major psychiatric disorders can be encountered, sometimes masquerading as or confounding a dysmotility diagnosis.28 It is not uncommon for some of these patients to be referred to an IF unit. Psychological distress is common (box 1) and so an MDT approach including both clinical psychology and liaison psychiatry expertise is ideal (see also section 9.6).
Box 1. Contributing psychological factors.
Delay in diagnosis
Poor knowledge within the medical community
No cure
Pain and problems of analgesic drugs (including addiction)
Anxiety, depression, somatisation, poor coping, sickness role
Interaction with family, carers and job leading to low self-esteem/confidence/mood
5.5 Effect of undernutrition on gut function
Malnutrition itself can impair gut function and cause malabsorption with mucosal atrophy, reduced gastric acid and pancreatic enzyme secretion and more bacterial colonisation of the upper gut.29 30 The effects of undernutrition on gut motility and histological appearance are uncertain.
There is literature on the superior mesenteric artery syndrome (Wilkie's syndrome) in which the third part of the duodenum is compressed between the superior mesenteric artery and the aorta (when the left renal vein is compressed it is referred to as ‘nutcracker syndrome’). It is reported to be prevalent in patients who have suddenly lost weight and reported to improve when either the patient becomes better nourished or a duodeno-jejunostomy (bypass) is formed to avoid the obstruction. The symptoms attributed to this are postprandial epigastric pain, nausea/vomiting and loss of weight.31–35 Whether this is a cause or consequence of malnutrition and whether it is a radiological rather than true clinical entity remains contentious and some clinicians dispute its existence and think it is over diagnosed. Thus the risks of any surgery should be very carefully considered, especially as the benefits of surgery are not always predictable or clear.
5.6 Hypermobile Ehlers–Danlos syndrome (EDS) (joint hypermobility syndrome or Ehlers–Danlos syndrome hypermobility type)
Hypermobile Ehlers–Danlos syndrome (EDS) with its gastrointestinal associations is difficult to classify as most patients with EDS do not have a dysmotility of the small bowel, merely visceral hypersensitivity. Its symptoms may mimic dysmotility (neuropathy) and the presence of EDS can contribute to dysmotility, usually if postural tachycardia syndrome (PoTS) or other associated factors such as opiates are present. According to the 2017 classification, patients previously diagnosed with joint hypermobility syndrome and Ehlers–Danlos syndrome hypermobility type were reclassified as hypermobile Ehlers–Danlos syndrome (hEDS) if they met the strict criteria or Hypermobile Spectrum Disorders (HSD) if they had many but not all of the characteristics of hEDS.36 Patients with hEDS and HSD represent a third of patients referred to a tertiary neurogastroenterology clinic and these patients tend to be young, female with a poorer quality of life.37 hEDS/HSD is associated with a range of gut disorders (acid reflux, abdominal pain (especially typical is pain after eating or when any food arrives in the gut even from an enteral feed) and constipation).38 There is often autonomic dysregulation, particularly PoTs,37 chronic urinary retention due to a failure of the urethral sphincter to relax (Fowler’s syndrome) and hypoglycaemia.37 Mast cell activation disorder39 is being increasingly reported (most commonly in those having PoTs). An increasing number of patients with joint hypermobility and gut dysmotility are being seen by nutrition support teams because of weight loss and malnutrition. This group seems especially sensitive to opioids and cyclizine, both of which can exacerbate all of their symptoms.18 It is currently unclear the degree to which the association of hEDS with gut symptoms encompasses specifically any greater degree of chronic small intestinal dysmotility, or whether there are any different treatment approaches to patients without hEDS who have the same functional symptoms. The same cautions therefore should apply when considering escalating invasiveness of nutrition support in this group as to that of functional gastrointestinal disorders in general, especially if there is a pain predominant presentation.
6.0 Classification of chronic small intestinal dysmotility
Three major histopathological entities are recognised: myopathies, neuropathies and mesenchymopathies, depending respectively on the predominant involvement of smooth muscle cells, enteric neurons or the interstitial cells of Cajal (ICC). Mesenchymopathies, which involve ICC, which are the gut pacemakers, are being recognised. The abnormalities described include a decreased ICC density, loss of processes and damaged intracellular cytoskeleton and organelles as revealed by immunohistochemical analysis and electron microscopy. It may be that abnormalities with the ICC are the primary event or may result from a neuropathy. In babies, immaturity may result in a delay in maturation of ICCs that can lead to the appearance of a reduction in these cells, so care needs to be taken with the histological diagnosis. As conditions specifically falling into this category are few, this document will only discuss conditions traditionally classified as a myopathy or neuropathy (figure 2, box 2).
Figure 2.
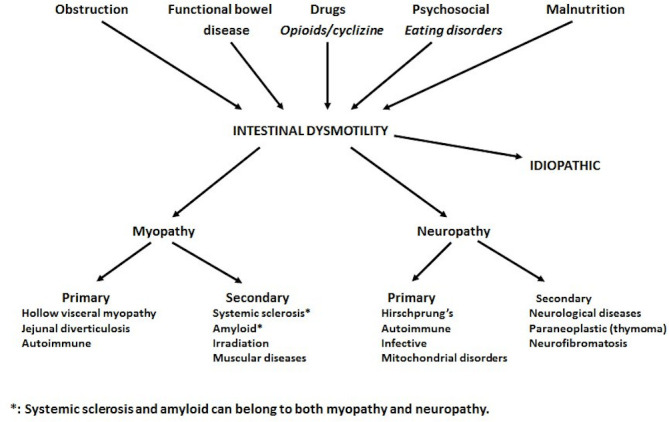
Main factors contributing to severe chronic intestinal dysmotility and its traditional classification.
Box 2. Classification of intestinal dysmotility.
Myopathies
Primary
-
Familial
Hereditary myopathy (eg, hollow visceral myopathy)
-
Acquired
Autoimmune
Jejunal diverticulosis
Secondary
Systemic sclerosis (and other connective tissue disorders (eg, SLE))
Amyloidosis
Chronic irradiation damage
-
Muscular diseases
Muscular dystrophies
Myofibrillar myopathies (eg, desmin myopathy)
Hereditary inclusion body myopathies
Metabolic storage disorder
Neuropathies*
Primary (intrinsic)
-
Familial/congenital/developmental
Hirschprung’s disease
Neurofibromatosis
Mitochondrial disorders (MNGIE, DNA depletion, Alpes or Pearson’s syndromes)
Neuronal dysplasia
Infant colic (developmental)
-
Autoimmune
Antineuronal antibodies
Ganglionosis
-
Infective
Chagas' disease,
Herpes viruses (eg, EBV, CMV, VZV) or
Polyoma viruses (JC virus)
Secondary (extrinsic)
-
Generalised neurological disorders
Brainstem lesions
Spinal cord injury
Multiple sclerosis
Parkinson’s disease
Neurological effects of diabetes mellitus
Autonomic system degeneration
-
Paraneoplastic syndromes (often with antineuronal antibodies (especially anti Hu))
Small cell lung cancer
Carcinoid
Neuroblastoma
Thymoma
-
Drugs/toxins
Vincristine, adriamycin
Antidepressants, Ca channel blockers, anticholergic drugs
Opioids
Clonidine
Isoniazid
-
Other
MEN IIb
Porphyria (acute intermittent)
Fabry’s disease
In most cases an empirical working diagnosis of idiopathic dysmotility will be applied.
*Histology is generally inflammatory or degenerative.
It can be hard to determine if a condition is primarily a myopathy or neuropathy as some secondary conditions (eg, systemic sclerosis, vasculitis or amyloid) may appear as both. The end result of a neuropathy is often dysfunctional enteric muscle which occasionally can dilate, as in a myopathy. Overall, a neuropathy is more common than a myopathy in causing small bowel dysmotility but the reverse may be true in CIPO. The diagnosis can be difficult to define partly because the radiological, isotopic, manometric and histological diagnoses may be different.
6.1 Myopathies
Primary myopathies most commonly occur in children and young adults and are often familial (genetic). Myopathies often have multivisceral involvement and thus a relatively high mortality. They are characteristically associated with massive gut dilatation. Many predominantly affect the circular muscle (except hollow visceral myopathy). Primary myopathies are more common in children whereas secondary myopathies are more common in adults. Some causes will remain idiopathic.
6.1.1 Primary myopathies
Primary myopathies are due to abnormalities in enteric muscle (eg, hollow visceral myopathy or autoimmune myopathy). There has been interest in reduced immunostaining of alpha-isoactin in jejunal circular muscle, observed in one40 then 28 more patients (overall 24% of patients having full thickness jejunal biopsies).41 However, it is not clear if this is the primary pathology or secondary to other factors (eg, drugs, undernutrition or previous surgery) or a normal anatomical variant, and therefore not a specific finding.42 Precise information as to the location of the biopsy (jejunum or ileum) is essential for interpretation in this context.
Familial
Hollow visceral myopathy is the best known example of a familial visceral myopathy. It is a rare congenital disorder that usually presents in the first or second decade of life and, in addition to gross dilatation of the gastrointestinal tract (that often starts with a megaduodenum), there may also be associated dilatation of the urinary tract and associated frequent urinary tract infections.43–45 The disease has been reported to follow an autosomal dominant mode of inheritance.46 47 In infants other features may include malrotation, pyloric stenosis and bladder atony. There is a loss of enteric smooth muscle with vacuolar degeneration and fibrosis.48 The longitudinal muscle is predominantly affected. This may be due to the transformation of smooth muscle cells to collagen synthesising myofibroblasts.49 In one study of adult patients, four of six patients had urinary tract involvement with dilatation of the ureters and/or incomplete bladder emptying.43
Acquired: autoimmune myopathy
A few cases only of a lymphocytic enteric leiomyositis involving the smooth muscle cells have been reported.50–52 Eosinophilic leiomyositis has also been reported, and in this context must prompt investigation for parasites, including dog hookworm.
Jejunal diverticulosis
Diverticula in the jejunum usually result from congenital abnormalities or dysmotility (eg, disordered high pressure bowel contractions) and may be associated with subclinical systemic sclerosis. Careful examination of any resected specimen should be carried out to examine the muscle and nerve layers of the bowel wall, both in the region of the diverticula and adjacent bowel.
6.1.2 Secondary myopathies
Secondary myopathies occur as part of a multi-system disease (eg, systemic sclerosis, amyloid, chronic irradiation damage or muscular diseases).53 The problems of pseudo-obstruction are often only clinically apparent towards the end of the illness when nutritional support may be needed.
Systemic sclerosis (scleroderma) and other connective tissue disorders
Most patients with systemic sclerosis do get gastrointestinal involvement particularly of the oesophagus.54 While the end result and main pathology is smooth muscle atrophy and gut wall fibrosis,55 it may start with microvasculature damage due to collagen deposits and inflammation which cause neural damage that progresses to muscle dysfunction and fibrosis. While systemic sclerosis patients with gross gastrointestinal involvement present in the terminal phase of the illness, this is not always the case and some present with gastrointestinal involvement early in the disease without cutaneous involvement and the disease may not progress for many years. The clinical outcome in elderly scleroderma patients is the poorest of all adult onset dysmotility patients.56 However, where indicated, long-term PN can offer a safe and effective means of nutritional support in patients with severe small bowel involvement.57 Other connective tissue and rheumatological disorders have been associated with dysmotility including systemic lupus erythematosus, rheumatoid arthritis and Still's disease.58 59
Amyloidosis
The primary type distribution may be associated with gut involvement. The most common underlying diagnosis is myeloma (often producing lambda chains). While classified as a myopathy, it can also cause neurological damage and, like systemic sclerosis, may cause both a myopathy and a neuropathy. The rectum can be spared so duodenal sampling should also be considered. Any full thickness biopsy for motility investigation should also be examined for amyloidosis. Genetic testing is now readily available for the hereditary type of amyloidosis, which may present more commonly in men and with peripheral neuropathy and cardiac as well as gut involvement.
Chronic irradiation damage
This usually occurs after pelvic irradiation for gynaecological cancers or genitourinary cancers. The sigmoid and terminal ileal areas are often most involved. However, the whole small bowel can be involved giving rise to a pseudo-obstruction picture or as discrete areas of strictures. Surgery is very difficult and has a high risk of an enterocutaneous fistula(s) being created. Gut permeability, secretion, motility and blood supply can all be affected, giving rise to any or all of the following: malabsorption, protein losing enteropathy, diarrhoea, perforation/fistulas, bleeding and obstruction. These problems can all occur months or years after more than 45 Gy irradiation has been given. The irradiation is more likely to give problems if a patient is already malnourished, has diabetes mellitus, hypertension or a vasculitis.60
Muscular diseases
Myopathies may occur associated with congenital muscular disorders (muscular dystrophies, myofibrillar myopathies (eg, desmin myopathy), hereditary inclusion body myopathies), but the muscle weakness (and often cardiac problems) dominates the clinical picture although gastrointestinal problems if sought are common. Metabolic storage disorders can have a myopathic process and occasionally can be treated with specific enzyme replacement therapy.61
6.2 Neuropathies
An enteric neuropathy may occur as a primary pathology (congenital, autoimmune or infective), secondary to a generalised neurological disorder, paraneoplastic process, metabolic disorder (eg, diabetes) or drugs/toxins or as a developmental abnormality. Visceral neuropathy is less well reported in the literature than visceral myopathy. Visceral neuropathy is commonly acquired in adulthood or in old age and is associated with a high morbidity usually due to factors other than the neuropathy. Luminal dilatation is rarely seen except at the end stage of the disease.
Two forms of pathology are found—either enteric neural degeneration (in the absence of inflammation) or inflammatory.62 Degenerative neuropathies can result from mitochondrial dysfunction and the pathological findings include neuronal swelling, intranuclear inclusions, axonal degeneration and hypoganglionosis. The aetiology of many degenerative enteric neuropathies will remain idiopathic. Inflammatory neuropathies may include both plexitis and neuritis and can be lymphocytic or less commonly eosinophilic, the former promoting autoimmune screening, the latter investigation for parasites.
6.2.1 Primary neuropathy
The enteric neuropathies can affect both the submucosal and myenteric plexuses but the myenteric plexus is predominantly affected. The term 'visceral neuropathy' is used for primary intrinsic enteric nervous damage.
Congenital/familial/developmental
Familial visceral neuropathies include Hirschprung’s disease, mitochondrial cytopathies and Von Recklinghausen’s disease. Hirschprung’s disease can affect any part of the gut.
Mitochondrial disorders are relatively common if specifically sought. One study showed 19% of 80 adult patients labelled as CIPO to have this.63 Mitochondrial cytopathies such as mitochondrial neurogastrointestinal encephalomyopathy (MNGIE) (the most common) (also referred to as thymidine phosphorylase deficiency) is an autosomal recessive disorder characterised by severe gastrointestinal dysmotility (including bacterial overgrowth and lactic acidosis), cachexia and neurological problems including leukoencephalopathy (96%), polyneuropathy (96%), ophthalmoplegia (91%) (with ptosis) and hearing loss (55%).64 65 The disease is caused by mutations in the thymidine phosphorylase (TP) gene. Gastrointestinal dysmotility is the most prominent manifestation, with recurrent diarrhoea and symptoms of obstruction. Patients with MNGIE present between the first and third decade (mean age 18 years)66 and usually have a very reduced life expectancy and tend to die in early adulthood (mean 37.6 years; range 26–58 years). It, like all mitochondrial defects, can be tested for by plasma and urine thymidine deoxyuridine, white cell thymine phosphorylase, the Tymp gene, MR brain scanning and muscle biopsy.
Autoimmune
Auto-antibodies directed at enteric neurons, usually neuronal ion channels (eg, voltage-gated potassium channels) can occur as a paraneoplastic phenomenon, when the anti-neuronal nuclear antibody (ANNA-1 or anti-Hu) is most commonly found, and antineuronal antibodies can occur in non-paraneoplastic motility disorders.67–69 Other auto-antibodies associated with dysmotility include acetyl cholinesterase receptor antibody (AchR) (ganglionic, nicotinic and M3 type), antibodies against the voltage-gated potassium channel-complex (VGKC-complex), voltage-gated calcium channel antibodies (VGCC), smooth muscle and gonadotropin-releasing hormone (GnRH).59 The pathogenetic role of auto-antibodies is, however, currently unclear. Coeliac disease has also been implicated in some cases of dysmotility.
Infective
Both herpes (Epstein–Barr virus and cytomegalovirus)70 and polyoma viruses (John Cunningham (JC) virus)71 72 have had their DNA isolated in the myenteric plexuses of some patients with visceral neuropathy. They may be causative agents rather than innocent bystanders but this has yet to be proven. Chagas’ disease (South American trypanosomiasis) typically causes a megaesophagus and megacolon. Chagas’ enteropathy is common and gives rise to dyspepsia, intestinal pseudo-obstruction with bacterial overgrowth.73 Lyme disease and botulism have also been reported as reversible causes of dysmotility.
6.2.2 Secondary neuropathy
The neuropathic process may affect the nerves external (extrinsic neuropathy) to the gut and so indirectly affect gut motility or may be part of a generalised illness. Indeed, most cases of visceral neuropathy are part of a generalised neurological disorder rather than a primary neuronal disorder of the gastrointestinal tract
Generalised neurological disorders
Disorders of the parasympathetic or sympathetic nerves that innervate the gut (including autonomic system degeneration and the neurological effects of diabetes mellitus (most common) and other endocrine or metabolic disorders) can indirectly cause gut dysmotility. Brainstem lesions, spinal cord injury, multiple sclerosis, Parkinson’s disease (basal ganglia calcification) and leukoencephalopathy can all affect gut motility.74 75 A lymphocytic leiomyositis and myenteric ganglionitis have been described in the ileum of children with cystic fibrosis and distal ileal obstruction.76 Myotonic dystrophy, multiple sclerosis, Parkinson’s disease and porphyria may all be associated with an enteric neuropathy.
Paraneoplastic
Small cell lung cancer, carcinoid tumours, neuroblastoma and thymoma with anti-neuronal nuclear antibodies have all been described to cause an enteral neuropathy. There is often a dense inflammatory infiltrate of lymphocytes and plasma cells affecting both plexuses but mainly the myenteric (myenteric ganglionitis). Anti-Hu neuronal antibody is characteristic.77 Removal of a thymoma may result in resolution of the dysmotility and the patient gaining weight. CRMP 5 (CV2) and AchR auto-antibodies have also been associated with paraneoplastic dysmotility and should prompt a careful search for occult malignancy.59
Drugs/toxins
Vincristine is directly neurotoxic and causes a visceral neuropathy. Anticholinergics (eg, phenothiazines and tricyclic antidepressants) have been associated with severe dysmotility. A case series of 102 life-threatening episodes of clozapine-induced gastrointestinal dysmotility episodes were collated with some evidence for dose dependence. A number of other drugs have been associated with severe dysmotility which, in most cases, improves with stopping the drug or reducing the dose; these include baclofen, buserelin, clonidine, fludaribine, phenytoin and verapamil. Lead poisoning can be a rare reversible cause.59
6.3 Idiopathic
In the majority of patients and in most centres, the precise aetiology of chronic severe dysmotility is not characterised histopathologically and remains based on the clinical presentation, physiological testing and exclusion of obstructive and mucosal disease. This in part reflects a low uptake of full thickness biopsies outside of the context of stoma formation or other surgical intervention. In selected populations of PN dependent patients with dysmotility, high rates of full thickness biopsies were associated with high rates of neuromuscular abnormalities of which two-thirds were primary and one-third were secondary causes, although not all biopsies yielded a diagnosis. The threshold and acceptability of full thickness biopsy testing, especially as most will not lead to a change in management, has not currently achieved consensus. There also remain some unresolved issues for gastrointestinal neuromuscular pathology standardisation and interpretation.59 For the near future, therefore, it is likely that the aetiology in the majority of dysmotility patients will remain idiopathic.
7.0 Physiological consequences of severe small intestinal dysmotility
7.1 Impairment of coordinated gut contractions and the migrating myoelectric complex (MMC)
If the MMC is impaired, then the small bowel will not be cleared of debris predisposing to gut stasis and bacterial overgrowth. With enteric neuropathies, gut coordination is disrupted and the presence of chyme in the small bowel can cause severe painful non-propulsive large contractions. This is one of the causes of abdominal pain shortly after eating.
7.2 Gut stasis
The failure of forward propulsion may also cause constipation and this is often the first symptom. Gut stasis results in abdominal distension and, if much fluid accumulates (oral intake and normal gut secretions), it may produce a large volume vomit. The vomit may be faeculent and contain food debris from several days previously.
7.3 Bacterial overgrowth and malabsorption
The combination of a dilated gut with reduced propulsion and ineffective MMC allows anaerobic bacteria to proliferate in stagnant loops of bowel. This bacterial overgrowth results in bile salts being deconjugated, less effective secondary bile acids (eg, lithocolic acid) being made and pancreatic enzyme degradation occurs so that steatorrhoea and malnutrition may occur. Associated with steatorrhoea is malabsorption of the fat soluble vitamins A and E (less so D and rarely K) with deficiency symptoms (night blindness, poor colour vision, dry flaky skin and ataxia). Vitamin B12 may be malabsorbed but both folic acid and vitamin K can be manufactured by the bacteria and so may give rise to high serum levels.
Occasionally the bacteria can manufacture D-lactic acid (normally L-isomer) giving rise to D-lactic acidosis (high anion gap acidosis) and other bacteria can manufacture ammonia which may appear in high levels in the blood.
Small intestinal bacterial overgrowth (SIBO) is when excess micro-organisms are present in the small intestine and lead to a malabsorption syndrome with occasionally a protein losing enteropathy. Subtotal villous atrophy may be found on histology. There are several endogenous mechanisms for preventing bacterial overgrowth: gastric acid secretion, intestinal motility, intact ileo-caecal valve, intestinal immunoglobulin secretion and bacteriostatic properties of pancreatic and biliary secretions. The aetiology of SIBO is usually complex, associated with disorders of these mechanisms. In some patients more than one factor may be involved.
There is currently no gold standard for the diagnosis of SIBO and the commonly available methodologies (the culture of jejunal aspirates and a variety of breath tests) are limited by large variations in their performance and interpretation.78
7.4 Problems of undernutrition
Patients who rapidly lose more than 10% of their body weight frequently have demonstrable physiological changes which include skeletal and cardiac muscle weakness, poor concentration and mental function including memory, prolonged sleeping, reduced sexual function, a low body temperature and a propensity to develop infections which are potentially severe.79 In the gut, malabsorption with mucosal atrophy, reduced gastric acid and pancreatic enzyme secretion and more bacterial colonisation of the upper gut can occur although the experimental backing for this is inferred from studies in patients with anorexia nervosa.22–26
8.0 Clinical features of chronic small intestinal dysmotility and management plan
8.1 History, examination and blood tests
The features of patients with a myopathy are summarised in table 1. The clinical history and examination should determine if there are associated systemic neuromuscular, connective tissue or endocrine diseases (muscular diseases, neurological disease, storage diseases, systemic sclerosis, diabetes mellitus, irradiation, etc) and thus if the myopathy or neuropathy is a primary or secondary disorder. Exploring the family history will detect some congenital diseases, as will asking about foreign travel (Chagas' disease). Examination especially includes the neuromuscular system and testing for joint hypermobility. Autonomic neuropathy should be considered if orthostatic, pupillary or sudomotor (sweating) dysfunction accompanies dysmotility. Simple clinical bedside assessment of orthostatic pulse rate change (lying to standing) may identify PoTs (box 3).52
Table 1.
Symptoms, medical history and medication of 28 patients with an enteric myopathy41
| Symptoms | |
| Duration, median (range) | 14 (4–33) |
| Abdominal pain | 28 (100%) |
| Distension | 23 (82%) |
| Nausea/vomiting | 22 (79%) |
| Constipation | 17 (61%) |
| Diarrhoea | 6 (21%) |
| Weight loss | 10 (36%) (5 given PN) |
| Medical history | |
| Radiological obstructive episodes | 9 (32%) |
| Previous laparotomies | 8 (29%) (median 2 (range 1–3)) |
| Psychiatric history | 6 (21%) (4 depression) |
| Medication | |
| Opiates | 7 (25%) |
| Antispasmodics | 13 (46%) |
| Prokinetics | 13 (46%) |
| Laxatives | 8 (29%) |
Box 3. Management plan for small intestinal dysmotility.
Determine and order the primary symptoms
Exclude mechanical obstruction (CT abdomen with oral contrast)
Evaluate other contributing factors: drug therapy (eg, opioids, cyclizine and anticholinergics), psychosocial (may need formal psychological/psychiatric assessment) and quality of life issues
Nutritional assessment (BMI, percentage weight loss and other anthropometric tests)
Start nutritional treatment (consider/treat refeeding risks)
Perform tests to help establish aetiology (box 4) and consider tests of autonomic function
Therapeutic plan/objectives of care to address patient's symptoms, nutritional status, psychosocial issues and quality of life
Try to establish a clinical diagnosis (or probable one). Perform physiologic assessment of the parts of the gastrointestinal (GI) tract that may be involved. These are done when nutritional status is near normal and the patient is off drugs likely to affect GI motility. Consider full thickness jejunal biopsy
Consider surgical options
Regular review and reconsider diagnosis as the clinical situation changes. Treat the predominant symptom/problem
Symptoms need to be listed in order of importance to the patient, and a record made of all the drugs currently taken or that have been taken for long periods (especially opioids and cyclizine).
A basic nutritional assessment will include measuring the patient’s height and weight and asking their usual weight in health and their weight change over the last 2 weeks, 3 and 6 months. From these their BMI and percentage weight loss can be calculated. In addition they are asked about recent changes in their food intake.
Tests to help make the diagnosis are summarised in box 4. Blood tests will include routine blood count, renal (including potassium and magnesium), liver, bone chemistry, thyroid function, glucose, myeloma screen, anti-tissue transglutaminase (for coeliac disease). Nutritional measures if undernourished or steatorrhoea include vitamin A, E, D, INR, iron, ferritin. B12, red blood cell folate, selenium, zinc and copper. Consideration is given to requesting auto-antibodies (especially antineuronal antibodies (see section 6.2 and box 4).
Box 4. Non-physiological tests to determine the aetiology of chronic small intestinal dysmotility.
Specific investigations are performed once organic obstruction, drug effects and eating disorders have been excluded. Physiological/histological tests are done after severe malnutrition has been treated.
Screen for hypothyroidism, coeliac disease and diabetes
Chest X-ray (or CT/PET CT) for thymoma or other neoplastic conditions (eg, small cell carcinoma of lung)
Antibodies for scleroderma (anti-centromere, anti Sc170, anti M3R) and other connective tissue disorders (ANA, ANCA, anti DNA, anti SMA)
Antibodies that may be associated with paraneoplastic diseases (mainly small cell carcinoma and thymoma). These may include type 1 anti-neuronal nuclear antibody (ANNA-1 'anti Hu'), anti-collapsin response mediator protein 5 (anti CRMP-5 also known as anti CV2), ganglionic acetyl cholinesterase receptor antibody (AChR antibody) especially if autonomic dysfunction,59 and anti-voltage gated potassium channel (VGKC)-complex antibodies.
Test for mitochondrial disorders with plasma and urine thymidine and deoxyuridine, WBC thymine phosphorylase. If there is a high suspicion then test for the TYMP gene and also screen for related diseases (eg, 'MELAS' (mitochondrial encephalopathy with lactic acidosis and stroke-like episodes) with the m.3243A>G mutation). Muscle biopsy and sequencing of mitochondrial genome may be considered.
If none of these are positive consider full thickness jejunal biopsy.
In MNGIE, direct evidence is provided by a plasma thymidine concentration greater than 3 µmol/L and a plasma deoxyuridine concentration greater than 5 µmol/L. Thymidine phosphorylase enzyme activity in leukocytes will be less than 10% of the control mean. Molecular genetic testing of TYMP, the gene encoding thymidine phosphorylase, detects mutations in affected individuals.
Rectal examination with an unprepared sigmoidoscopy will identify stool consistency and colour and permit biopsy for amyloid. Steatorrhoea will be detected and constipation/diarrhoea confirmed. Basic tests of autonomic function include lying and standing systolic blood pressure and heart rate with ECG confirmation.
8.1.1 Myopathy
Symptoms include chronic abdominal pain, abdominal distension and bloating, early satiety, recurrent nausea and vomiting and alternating diarrhoea and constipation. Without treatment, weight loss and protein-energy malnutrition may ensue.79 The frequency of symptoms for those with a probable myopathy is shown in table 1.41 The vomiting may be faeculent and often of high volume giving rise to a risk of pulmonary aspiration.
In hollow visceral myopathy (HVM), in addition to the features above, patients have a very dilated small bowel. They may have urological complaints including bladder-emptying dysfunction.43–45 Children with HVM may present at or before birth with hydronephrosis, megaureters and megacystis, or in the first year of life with constipation and episodes of intestinal pseudo-obstruction.43 44 The presence of digital arches on fingerprint, mitral valve prolapse, joint laxity and constipation before age 10 years all favour the diagnosis.74 HVM may present at any age, but early adulthood is most common.46 47
Signs of autoimmune disease (arthropathy, Raynaud's disease or proteinuria) may suggest a secondary myopathy, or the pseudo-obstructive syndrome associated with scleroderma may be declared by the cutaneous manifestations of this disease.
8.1.2 Neuropathy
Many of the features are the same as for a myopathy, particularly with severe abdominal pain after food; however, abdominal distension is often absent and the plain abdominal radiograph may appear normal.80
8.2 Radiological tests
The diagnosis is usually first suspected after plain abdominal radiographs have shown a dilated small and large bowel. Once suspected, investigations aim to confirm that there is impaired transit of luminal contents, to identify the region of the bowel affected, ideally to identify the propulsive abnormality and to show a specific pathology.6 Investigations help establish the presence of intestinal pseudo-obstruction and may delineate an underlying cause. In practice the diagnosis is often presumed after several laparotomies have excluded a physical obstruction, although CT/barium follow-through/MR enterography excluding a transition point in a diffusely distended small bowel suggests CIPO and may prevent unnecessary laparotomy. CT may also help distinguish severe dysmotility from functional bloating due to abdomino-phrenic dysinergia.81 Dynamic MRI of the small bowel is becoming increasingly helpful,82 83 though is less established. MRI brain can be helpful in the diagnosis of MNGIE.59
The measurement of whole gut time can be measured by serial X-rays of ingested radio-opaque markers (small lengths of barium-impregnated polyvinyl tubing).
Small bowel transit using a barium follow-through examination will usually give some indication of accelerated or delayed transit and a dilated duodenal loop (megaduodenum) may be one of the earliest signs of visceral myopathy.83 In addition, in HVM there may be oesophageal aperistalsis and variable dilatation of the small and large bowel.
8.3 Radioisotopic investigations
Gastric emptying can be measured using gamma scintigraphy to obtain serial images of labelled solid (scrambled eggs, liver or pancake), semi-solid (thick soup) or liquid (orange juice) meals in the stomach. Gastric emptying measurements may be helpful in determining whether the stomach is involved in a generalised disorder of propulsion or a localised one (eg, Chagas' disease). These isotopic meals can be extended to measuring the transit of the meal through the small bowel and, if the isotope has a long half-life, orocaecal and colonic transit may be determined. Liquid meals may not clearly demonstrate an abnormality.
8.4 Endoscopic tests
Jejunal aspirate for bacterial overgrowth is infrequently performed but usually by endoscopy (or fluoroscopy with jejunal intubation). A clinically significant overgrowth is when counts exceed 105/mL (usual is less than 104/mL). Common species include Bacteroides, Enterococcus and Lactobacillus. However, most of the bacteria likely to be relevant in causing symptoms cannot be cultured. Endoscopy also has a role in mucosal sampling and palliative venting. Capsule endoscopy examination can sometimes give transit information but is rarely used due to the risk of the capsule being retained and some regard it as contraindicated.
8.5 Non-invasive investigations of gut transit
Orocaecal transit can be measured using the rise in breath hydrogen due to the degradation of ingested polysaccharides (eg, lactulose). In health this is caused by caecal bacteria fermenting the ingested agent, but this is unhelpful if there is propulsive failure as small bowel bacterial overgrowth is common and is not a recommended test for this application.84 85 It is also unhelpful following a significant small bowel resection or if there is an enteric fistula.
Breath tests to diagnose bacterial overgrowth may be misleading and produce false negative results compared with culture of small bowel aspirate.78 86 This has in part been due to broad variations in how these tests are performed and interpreted. Recent work in the UK and USA has taken place to develop evidence-based consensus guidelines for breath testing in terms of dose of substrate (75 g glucose, 10 g lactulose) and cut-off values. In addition, while hydrogen only breath testing was previously used, modern testing protocols have incorporated the measurement of methane. Increased intestinal methane levels have been associated with delayed small bowel transit as measured by scintigraphy and therefore should be measured in patients with suspected small bowel dysmotility to improve the test's utility.86 Other tests that may indicate bacterial overgrowth include raised urinary indicans, blood D-lactate or alcohol levels.
8.6 Manometry
Intraluminal pressure sensors incorporated into a catheter can detect the patterns of contractile events. For the diagnosis of pseudo-obstruction, the logical investigation is small bowel manometry. Small bowel motor activity was initially studied using multi-lumen perfused tube systems, with a pump and strain gauge transducer external to the patient.87 This gave information on motor activity in the antrum and proximal duodenum, and detected abnormal motility88 and some types of pseudo-obstruction.89 90 This technique required the patient to remain in a laboratory attached to a machine for more than 6 hours and was not good at recording fasting, and postprandial activity.91
An alternative is the wireless motility capsule (WMC) which is an ambulatory, minimally invasive diagnostic modality that allows continuous assessment of intraluminal pH, temperature and pressure during its transit through the gastrointestinal tract. The technology allows for both measurement of transit times in multiple regions of the upper and lower gastrointestinal tract, as well as pressure profiles in the antro-duodenum. The standardised equipment and procedures in WMC allow the comparisons of data across multicentres. The role of the technology has been best established in the evaluation of a large number of healthy volunteers92 and in patients with suspected gastroparesis and suspected chronic constipation. The worry with this technique in these patients is that the capsule may remain in the bowel and not be passed. However, a study in patients with Crohn’s disease has shown that the same precautions used when considering patients for capsule endoscopy (ie, clinical and radiological assessment and use of a patency capsule) can mitigate much of the risk in potential WMC patients.93
Twenty-four hour ambulatory jejunal manometry94 uses a catheter with built-in miniature strain gauge transducers95 and records data to a solid-state digital recorder.96 The digital encoding of pressure data simplifies the analysis of continuous 24-hour recordings by computer software.97 98 This technique has proved useful in several conditions99 100 including pseudo-obstruction. During nocturnal sleep, normal stereotypic MMC activity is clearly evident101 and in some patients with pseudo-obstruction the abnormal contractile activity of the small bowel results in distortion of the fasting MMC pattern. Manometry of patients with pseudo-obstruction can be difficult in the later stages of disease because the peristaltic activity required to propel a manometry catheter into position in the proximal jejunum is lacking, and endoscopic assistance may be needed. A patient with a neuropathy may have a normal diameter gut but it may be hyperactive with many uncoordinated and often strong contractions (bursts).90
The effect of any drugs the patient may be taking must be taken into account in interpreting any results (eg, opioids, anticholinergics and cyclizine). Manometry does not always produce results that are clinically helpful.90
8.7 Pathology and histology
The biochemical examinations recommended are listed in box 4.
Adequate biopsy material is not often available and few laboratories have an experienced gastrointestinal neuropathologist. There also remain some additional pitfalls for collecting and analysing samples including sampling error, effects of bowel handling, sparsity of normal data and specificity. Good histological samples are needed to make a firm diagnosis. Close liaison between the surgeon and pathology laboratory is crucial so that a full thickness specimen of bowel is immediately processed. The samples should be divided. In an ideal situation some is snap-frozen in liquid nitrogen and the main portion fixed for routine histology and electron microscopy. In practice the latter two may be the best option. The immediate processing of samples is important if a detailed examination of the nerves, ganglia and muscle tissue is to be carried out. Diagnosis of a neuropathy may be difficult in conventionally orientated and stained sections of gut, and whole mount plexus assessment is a research tool. The most important element is to ensure that enough sections and material is examined in a centre with experience of dysmotility.
A full thickness jejunal biopsy is usually taken laparoscopically and is often helpful diagnostically, but the procedure in centres without much experience can be unhelpful and have a significant risk. Published data from centres with expertise suggest a median operating time of 50 min, conversion rate to open operation 2% and length of stay 1 day with an 8% readmission rate for obstructive symptoms.102 In myopathies the diagnosis may be established. A neuropathy in general shows either degenerative changes or inflammation.
All full thickness biopsies should be stained with Congo red stains to look for the presence of amyloid. As full thickness jejunal biopsies may not change the clinical management and are associated with risks, they are often performed when a laparotomy does not find an organic cause of obstruction or when the patient happens to be undergoing surgery for another reason (eg, a jejunal tube placement).103
MNGIE can be diagnosed with a skeletal muscle biopsy in addition to the blood and genetic testing.
9.0 Treatments
The drug treatments for intestinal dysmotility are shown in box 5. Most of the drugs are commonly used to treat milder forms of the symptoms. Treatment is occasionally directed at the underlying condition but more often is targeted at a specific symptom.
Box 5. Drug therapies for intestinal dysmotility.
Laxatives (after adequate fluid in diet)
Osmotic
macrogols (PEG), lactulose, magnesium salts
Stimulant
anthraquinone group (senna and dantron)
bisacodyl, sodium picosulfate, docusate sodium
phosphate enema, glycerol suppository
parasympathomimetics: bethanechol, neostigmine, pyridostigmine
5HT4 receptor agonists: prucalopride
Bulk forming
unprocessed wheat bran, methylcellulose, ispaghula and sterculia
Faecal softeners/lubricants
liquid paraffin, arachis oil (ground nut oil, peanut oil) enemas
Peripheral opioid-receptor antagonists
methylnaltrexone
Secretagoges
Linaclotide, Tenapanor*
Antispasmodics
Antimuscarinics
tertiary amine: dicycloverine hydrochloride
quaternary ammonium compounds: propantheline bromide, hyoscine butylbromide
Direct smooth muscle relaxant
alverine, mebeverine and peppermint oil
Prokinetics
Dopamine receptor 2 antagonists
metoclopramide, domperidone
Macrolides
erythromycin
Antidiarrhoeal drugs
Opioid agonists
loperamide, codeine phosphate, diphenoxylate
5-HT3 antagonist
Ondansetron
Anti-emetics
D2 receptor antagonists (see above)
cyclizine
ondansetron
ramosetron*
Analgesics
tricyclic antidepressant (low dose) amitriptyline
selective serotonin reuptake inhibitor
serotonin and norepinephrine reuptake inhibitor (duloxetine)
gabapentin
pregabalin
antispasmodic drugs
opioids (low dose)
Antibiotics for bacterial overgrowth
amoxycillin-claevulinic acid
ciprofloxacin
metronidazole, tinidazole
cephalosporin
tetracycline, doxycycline
non-absorbable antibiotics: rifaxamin, neomycin
*Not licensed in the UK.
9.1 Underlying condition
An underlying disease may need to be treated (eg, connective tissue disorder, enteric myositis, neoplastic disease or myotonic dystrophy). Diabetic control should be very good and may necessitate an insulin pump. Electrolyte, mineral or endocrine abnormalities should be prevented and treated when detected.
Immunosuppressive treatment has a small evidence base restricted to case series or reports. Prednisolone and ciclosporin have been reported to be of particular benefit in autoimmune myopathy.104 There is a case report of an improvement with initially prednisolone 1 mg/kg and azathioprine 2 mg/kg/day, then subsequently the prednisolone was replaced with budesonide 9 mg/day.52
There must always be awareness that organic obstruction can be missed as a diagnosis and, if a prokinetic drug105 makes pain worse, then an organic obstruction must be considered. Similarly, a successful trial of a low fibre or liquid diet suggests an organic obstruction.
Some metabolic storage disorders can be treated with specific enzyme replacement therapy.61
9.2 Specific drug treatments of symptoms
No treatment is ideal, and even though some help to correct physiological abnormalities, they may not affect the patient’s symptoms (boxes 3 and 5).
Drug therapy106 can be difficult and often drugs with conflicting actions are used (prokinetic for constipation and anticholinergic for colicky pain). Essentially, the drug therapy is targeted at the symptom perceived as most important by the patient.
Prokinetic treatments are used to try and improve the dysmotility itself and can return some of the measured abnormalities towards normal. They may especially help with vomiting and constipation. Prokinetic drugs are generally not used after a bowel anastomosis. Some of the previously used prokinetic drugs have been withdrawn or can only be used with extreme caution. They include domperidone and metoclopramide (D2 dopamine receptor antagonists) which stimulate gastric emptying and small intestinal transit, and enhance the strength of oesophageal sphincter contraction. Metoclopramide also increases the release of acetylcholine from some enteric nerves. Domperidone is a selective antagonist of peripheral D2 dopamine receptors, which does not have the acetylcholine-like effect of metoclopramide. National Patient Safety Agency (NPSA) alerts have been issued for domperidone highlighting problems with prolonged QTc, therefore long-term use should be subject to QTc monitoring. The extrapyramidal side effects of metoclopramide (especially in children) and the potentially irreversible tardive dyskinesia in elderly subjects, together with no evidence of consistent benefit in gastroparesis, caused the European Medicines Agency’s Committee to recommend that metoclopramide is not used in the long term.107 Cisapride, a 5-HT4 agonist, enhances acetylcholine release in the myenteric plexus without having anti-dopaminergic effects and may have been of particular benefit if MMCs were present on small intestinal manometry. In a 6-week double-blind, placebo-controlled trial in 26 patients, cisapride helped abdominal pain, improved solid gastric emptying and the MMC.105 Unfortunately, due to an increased risk of fatal cardiac arrhythmias (probably relating to a prolonged QT interval) in patients taking other medications or suffering from underlying conditions known to increase the risk of cardiac arrhythmias, cisapride was withdrawn. Tegaserod, a 5-HT4 receptor partial agonist, increased stool frequency in irritable bowel syndrome108 109 and improved the symptoms in functional dyspepsia,110 but was withdrawn due to an increased risk of heart attacks or strokes.
Prucalopride, a high affinity selective 5HT4 receptor agonist, has been used for constipation and appears not to have the cardiac risks of cisapride or tegaserod as it does not affect the QT interval. This is by having no significant action on the 5-HT1B/D and on the cardiac human ether-a-go-go K+ channels.111
Erythromycin, a motilin agonist, is potentially useful112 if there are absent or impaired antroduodenal migrating complexes but is subject to tachyphylaxis. Doses of 900 mg/day have been recommended.113 Azithromycin may be more effective for small bowel dysmotility.114
A somatostatin analogue (octreotide), given by a relatively painful subcutaneous injection, may be dramatically beneficial, especially in systemic sclerosis when other treatments have failed.115–117 It can improve vomiting and pain, partly because octreotide (in normal subjects) reduces the perception of volume distension due to inhibition of sensory afferent pathways.115 Octreotide may cause low amplitude MMCs to return.117 Octreotide may have a beneficial effect when erythromycin has been unsuccessful; its effect (50–100 μg once or twice a day) is apparent within 48 hours and is maintained for more than 2 years. It may be more effective when combined with erythromycin.118
The parasympathomimetics bethanechol, distigmine, neostigmine and pyridostigmine enhance parasympathetic activity in the gut and increase intestinal motility. They are rarely used because of both their gastrointestinal and cardiovascular side effects (diarrhoea and severe bradycardia). Pyridostigmine has, however, been shown to help refractory constipation (including in diabetes) and was well tolerated using a stepped dosing regimen.119 120
Naloxone 1.6 mg given subcutaneously each day or methylnaltrexone given subcutaneously on alternate days may be beneficial in blocking dysmotility effects of opioids or in improving motility through blocking endogenous opioids.121
9.2.1 Constipation
Constipation may be a problem in early stages, but is rarely present when IF occurs. In the early stages of these diseases, constipation may be managed by diet ensuring that it includes an adequate intake of fibre and fluid. Bulk forming laxatives such as unprocessed wheat bran (or oat bran) taken with food or fruit juice are effective and methylcellulose (which is also a faecal softener), ispaghula, and sterculia are useful in patients who cannot tolerate bran.
Osmotic laxatives (macrogols (polyethylene glycol), lactulose or magnesium salts) increase the amount of water in the large bowel, either by drawing fluid from the body into the bowel or by retaining the fluid that was administered. Macrogols are inert polymers of ethylene glycol (PEG) which sequester fluid in the bowel. Lactulose is a semi-synthetic disaccharide which is not absorbed from the gastrointestinal tract. It produces osmotic diarrhoea of low pH and prevents the proliferation of ammonia-producing organisms. Magnesium salts are useful where rapid bowel evacuation is required. Sodium salts should be avoided as they may give rise to sodium and water retention.
If there is an inadequate response to an osmotic laxative, a stimulant laxative can be added. Stimulant laxatives increase intestinal motility and often cause abdominal cramp; they should be avoided in intestinal obstruction. Excessive use of stimulant laxatives can cause diarrhoea and hypokalaemia. The anthraquinone laxatives (senna, dantron, cascara) are converted in the intestine to active sennosides, which may function by stimulating the myenteric plexus in the colon and also by inhibiting colonic water absorption. Their principal effect is in the descending and sigmoid colon. Their effect is largely local and depends on sufficient intestinal motility to present them to the colon for bacterial degradation to their active form. Sennosides, with prolonged use, had been thought to damage the intestine muscle and/or myenteric neurons but there is no clinical or animal evidence to support this.122 123 Poorly absorbed diphenylmethane derivatives (bisacodyl, phenolphthalein, sodium picosulfate) stimulate sensory nerves in the proximal colon and increase sodium and water movement into the colonic lumen. Castor oil can have a place with its principal effect on small bowel fluid secretion. Docusate sodium probably acts both as a stimulant and also as a softening agent.
Dantron, cascara and castor oil are rarely used, dantron because of potential carcinogenicity.
5HT4 receptor agonists (prucalopride) are selective serotonin 5HT4 receptor agonists with prokinetic properties. Prucalopride is licensed for the treatment of chronic constipation in women when other laxatives have failed to provide an adequate response. Headache and gastrointestinal symptoms (including abdominal pain, nausea and diarrhoea) are the most frequent but rare side effects. The side effects generally occur at the start of treatment and are usually transient. It has the potential to be a useful prokinetic drug now that cicapride and tegaserod have largely been withdrawn. Linaclotide (a 14-amino acid peptide) which acts in the intestinal lumen on guanylate cyclase-C (GC-C) so generating cyclic guanosine monophosphate (cGMP), which stimulates chloride secretion, resulting in increased luminal fluid secretion and an acceleration of intestinal transit. It also may have some visceral analgesic activity.
Methylnaltrexone is a peripherally acting mu-opioid-receptor antagonist that is licensed for the treatment of opioid-induced constipation in patients receiving palliative care when response to other laxatives is inadequate; it should be used as an adjunct to existing laxative therapy. Methylnaltrexone does not alter the central analgesic effect of opioids. Naloxegol is an oral agent and has the same properties.
Faecal softeners (liquid paraffin), the traditional lubricant, have potential disadvantages of minimal efficacy (hence usually used in combination with other agents) and safety issues (aspiration of paraffin, perianal burning). Bulk laxatives and non-ionic surfactant ‘wetting’ agents (docusate sodium) also have softening properties. Enemas containing arachis oil (ground-nut oil, peanut oil) lubricate and soften impacted faeces and promote a bowel movement. Dioctyl sulfosuccinate, an anionic detergent, can be used to break down hard stools.
Stimulant suppositories (glycerol) or enemas (phosphate) may also be effective although they are often less acceptable to the patient. Glycerol suppositories act as a rectal stimulant by virtue of the mildly irritant action of glycerol. Constipation may need regular enemas initially using low volume phosphate preparations progressing to high volume saline washouts or transanal irrigation systems.
Treatment of faecal impaction may need a manual evacuation under anaesthetic if disimpaction does not occur after oral and rectal treatment, or if there is a megarectum. The outcome of colectomy±ileorectal anastomosis is poor for these patients and best avoided. Sometimes a defunctioning loop ileostomy, which is reversible, may be performed before considering a total colectomy.
9.2.2 Pain
Pain is often poorly correlated with motor events. A simple measure such as reducing fibre in the diet can reduce abdominal distension by reducing bacterial fermentation and the production of gases. Low FODMAP diets may also have a role, but are restrictive in nature and should not be used in an already malnourished individual. Peppermint oil may also help.
Antimuscarinics that are used for gastrointestinal smooth muscle spasm include the tertiary amine dicycloverine hydrochloride and the quaternary ammonium compounds propantheline bromide and hyoscine butylbromide. The quaternary ammonium compounds are less lipid soluble than atropine and are less likely to cross the blood–brain barrier; they are also less well absorbed from the gastrointestinal tract. Dicycloverine hydrochloride has a much less marked antimuscarinic action than atropine and may also have some direct action on smooth muscle. Hyoscine butylbromide is advocated as a gastrointestinal antispasmodic and is commonly tried, but it is poorly absorbed so intramuscular preparations may be more effective and can be used in the long term at home.124
Direct relaxants of intestinal smooth muscle (alverine citrate, mebeverine and peppermint oil) which may relieve pain in irritable bowel syndrome are commonly tried and have no serious adverse effects.
Persistent abdominal pain may be a major problem and its mechanism may include central nervous system sensitisation making it very difficult to treat. Features of neuropathic pain should be sought and managed with neuropathic agents. Opioid-induced hyperalgesia as part of the narcotic bowel syndrome can also develop and needs appropriate management (see section 5.2). If other analgesics prove ineffective, opioids and their derivatives may be tried though they themselves have pro-absorptive/antisecretory effects and cause slowing of intestinal transit. Some opioids, such as tapentadol, may have a better dysmotility side effect profile. Targinact (oxycodone and naloxone combined) is marketed as a way of giving analgesia without causing constipation. A small amount of naloxone crosses the blood–brain barrier to block the dependence action of oxycodone, although when first used it may precipitate some withdrawal symptoms from the previous opioid-like drug. Naloxegol is a PEGylated naloxone formulation not combined with opioid and therefore should not cross the blood–brain barrier, owing to the PEGylation, to minimise withdrawal side effects.
Oral liquid preparations may be used but sublingual or transdermal buprenorphine or fentanyl have the advantage of bypassing the abnormal gut function. It may be of value to give a patient a 'pain holiday' in hospital during which sedation and continuous subcutaneous opiates, or even epidural anaesthesia, may reduce the pain threshold so allowing a reduction in maintenance analgesic dosage. Escalation beyond a low dose of opioid is likely to be ineffective in managing chronic pain and is associated with unacceptable risks, including catheter-related bloodstream infections, and should be de-escalated or discontinued if the chronic pain persists, even if no other effective pain medication is available.125
There is a growing appreciation for the role in abdominal pain management of the gut-brain neuromodulators, frequently used in neuropathic pain management.126 These include a tricyclic agent that can be used at sub-antidepressant doses for abdominal pain or discomfort in patients who have not responded to laxatives, loperamide or antispasmodics. Low doses of a tricyclic antidepressant are used (eg, amitriptyline, initially 5–10 mg each night, increased if necessary in steps of 10 mg at intervals of at least 2 weeks to maximum 30–50 mg each night). A selective serotonin reuptake inhibitor (SSRI) may be considered in those who do not respond to a tricyclic antidepressant, but they are considered to be less effective analgesics than the serotonin-norepinephrine reuptake inhibitors (SNRIs), of which duloxetine is the first choice.126 127 The role of gabapentin and pregabalin is well established for chronic neuropathic pain, and there is emerging evidence that the use of combination gut-brain neuromodulators from more than one class is more effective than monotherapy.126 127 SNRI and SSRI classes, however, should not be combined due to risks of serotonin syndrome.
9.2.3 Vomiting
Now that domperidone and metoclopramide are no longer used in the long term and as cyclizine can cause psychological dependence and addictive behaviour,18 the 5-HT3 antagonists like ondansetron are most commonly used but can result in constipation.
If a nasogastric draining tube helps symptoms, then a venting gastrostomy (ideally over 20 French gauge (FG)) usually inserted endoscopically (though it may also be done radiologically or surgically) may reduce vomiting by decompressing the stomach. The difficulty is having a large enough gastrostomy tube to allow all debris from the stomach to drain. Sometimes a tube can be inserted into the small bowel if very dilated to decompress it. These venting ostomies are often successful but are associated with many complications such as leakage and infection (often with candida) and generally need to be changed more regularly than a feeding ostomy.
9.2.4 Diarrhoea: bacterial overgrowth and bile salt malabsorption
Antidiarrhoeal drugs such as loperamide, diphenoxylate or, rarely, codeine phosphate are very occasionally used for symptomatic benefit. Opioids with a central action, such as codeine, are not the first choice because of the risk of dependence and sedation.
Steatorrhea may be secondary to an overgrowth of anaerobic bacteria in the motionless dilated loops of bowel.
As the disease progresses, bacterial overgrowth can result in diarrhoea. This can be reduced with oral amoxycillin-claevulinic acid combination, metronidazole/tinidazole, cephalosporin, tetracycline (doxycycline), ciprofloxacin, cotrimoxazole or non-absorbable antibiotics such as rifaximin or neomycin. Rifaxamin is often the first choice if it is on the local drug formulary. These may be used as necessary or in repeated courses every 2–6 weeks, often rotating (sometimes with a 1–2-week period of no antibiotic) to another antibiotic for a similar period of time before repeating. If metronidazole is used in the long term, the patient must be warned to stop if they develop numbness or tingling in their feet as an early sign of reversible peripheral neuropathy and be used at the lowest dose possible. Ciprofloxacin use longer term can cause tendonitis and rupture and again low dose and vigilance are required. The risk of resistant organisms, including Clostridioides difficile, should also be considered. There are no data currently about the use of probiotics.
Bacterial overgrowth is virtually inevitable and can cause cachexia without necessarily causing diarrhoea, so antibiotics (as suggested above) may be needed.
Bile salt malabsorption may occur and respond, if tolerated, to bile salt sequestrants (cholestyramine and colesevelam). It is most likely if terminal ileum has been resected or if there are large areas of fluid-filled dilated bowel.
Octreotide, occasionally used for its effects in reducing secretions and slowing gastrointestinal motility, has also been used in refractory SIBO.
9.2.5 Bloating/distension
Bloating and distension are common symptoms and not easy to treat. Reducing gas-forming microbes (eg, those producing CO2, methane and hydrogen sulphide) with a low fibre diet or an antibiotic (rifaxamin), giving simethicone or peppermint oil or reducing visceral hypersensitivity (antidepressants) or constipation may help along with increasing physical exercise.128
9.3 Neuromodulation (pacemakers)
There is some limited evidence for gastric electrical stimulation (gastric pacing) to improve vomiting symptoms where gastroparesis is prominent and small bowel function relatively intact.129–131 Patients with diabetic gastroparesis respond best and, in general, responders tend to have more severe vomiting. Patients with idiopathic gastroparesis have a potentially higher rate of poor response to gastric electrical stimulation.132 Non-invasive vagal nerve stimulation has shown some promise both for improving gastroduodenal motility and reducing pain sensitivity.133
The dorsal column pathways are involved in the transmission of visceral pelvic pain. Spinal cord stimulation suppresses the visceral response to colon distension in an animal model and therefore may be an effective therapy for chronic pelvic pain of visceral origin. There has been success reported in one study of 35 patients in whom the catheter tip was situated at the T5 position for a median of 9 days (range 4–14).134 The Cochrane database concludes that more studies are needed.135
Sacral nerve stimulation uses electrical stimulation applied to the sacral nerves, eliciting a physiological effect on the lower bowel, anal sphincter and pelvic floor, and has shown some success in treating faecal incontinence and constipation.136–138 A Cochrane review concluded that from three studies there was “very limited evidence that sacral nerve stimulation can improve continence in selected people with faecal incontinence, and reduce symptoms in selected people with constipation” and larger “good quality randomised crossover trials are needed”.139 There is no evidence that sacral nerve stimulation helps any of the symptoms in patients with CIPO.
Small intestinal electrical stimulation is at an experimental stage.
9.4 Nutritional support
Nutritional assessment and support is an important aspect of management. With appropriate therapy, many patients with CIPO manage to maintain their nutritional status through the oral/enteral route without the need for PS.
9.4.1 Dietary adjustments/fluid management
Gastric motility may be far less deranged for liquids than for solids with the result that many patients tolerate liquid feeds better than solid meals. Sometimes frequent small meals with low-fat, low-fibre and liquid nutritional supplements may be helpful.
If the patient has a stoma and a short bowel, fluid restriction, a sipped glucose saline solution, use of loperamide sometimes in high dose (occasionally with the addition of codeine phosphate) will reduce the risks of dehydration, sodium and magnesium depletion. If a high net secretory output occurs, a proton pump inhibitor (or occasionally octreotide) may be needed.140
Post-feeding orthostatic symptoms in partial autonomic failure may respond to dietary adjustments and drugs such as fludrocortisone, midodrine and octreotide.
9.4.2 Vitamin/mineral deficiencies
Care is needed to ensure that micronutrient deficiencies particularly of iron, vitamin B12 and the fat-soluble vitamins, especially vitamin A, D and E, do not occur. Magnesium deficiency is common especially if a high output stoma. Magnesium oxide may cause fewer osmotic effects than other preparations but is expensive.
Bone mineral density is important to address and should be assessed with dual energy x-ray absorptiometry (DEXA) scanning in those with malnutrition. For patients who cannot take oral measures to improve bone density, parenteral bisphosphonates such as zoledronate should be considered.
9.4.3 Enteral nutrition
Enteral nutrition is preferred if the gut is accessible and absorbing. In carefully selected patients, feeding jejunostomy with or without decompression (venting) gastrostomy may be tried. A percutaneous endoscopic or radiological gastro-jejunostomy is preferred to a direct jejunostomy where possible as direct jejunostomy tubes are more subject to leakage, retention, pain and skin problems, and gastro-jejunostomies can achieve both post-pyloric feeding and venting with generally easier endoscopic placement whereas direct jejunal tubes will often need to be placed surgically. Invasive enteral tube insertion should be preceded where possible by a trial of naso-enteral tube feeding to ensure absorption and tolerance prior to running the risks of mortality and morbidity associated with invasive tube placement.
If liquid enteral feeds are given, any excess can be aspirated by enteric tube or gastrostomy before the start of the next meal to ensure that excess volumes do not accumulate in the stomach. Gastrostomies can be used, therefore, to aspirate liquid gastric contents (decompression of venting gastrostomy) as well as a conduit for feeding, particularly when there is a need to bypass a malfunctioning oesophagus and/or stomach. Pulmonary aspiration of large volume vomits is a very serious complication that may be difficult to prevent. A low antral site for gastro-jejunal tube placement is preferred to optimise drainage/venting and also stability of the jejunal extension.
9.4.4 Parenteral nutrition (PN)
Long-term PN should be reserved for patients with significant malnutrition or electrolyte disturbance who cannot tolerate enteral nutrition. Complications associated with total PN include infections, sepsis and cholestatic hepatic dysfunction.
If safe nutritional status cannot be maintained through the oral and enteral route, then HPN may be required. One problem of HPN in these patients is that they have more problems than do patients with a short bowel.103 They particularly have a higher incidence of catheter-related bloodstream infection, septicaemia and venous thrombosis. The reasons for this are not entirely clear. Procoagulation states sometimes exist, and it is possible that there is increased bacterial translocation from the gut. Opioid medication (which at high doses suppresses some aspects of immune function) and/or cyclizine increase the risk of catheter-related bloodstream infection, partly as the care taken by the patient in the management of their infusions at home,141 due to cognitive effects, is reduced. The use of feeding lines to administer any drug is to be strongly discouraged because of the risk of catheter infection. Such patients test the capabilities of the best organised nutrition teams to the full and should be managed in centres with a large experience.142 Vigilance for psychopathology and ongoing involvement of psychology and liaison psychiatry should be offered. There may be a benefit from the mutual support patients can give to each other in these situations, although patients with significant psychopathology can have a detrimental effect on others.
Howard et al 143 have emphasised that the clinical outcome on HPN, like the mortality risk, is to a large extent a reflection of the underlying condition. While about 70% of patients with Crohn’s disease or ischaemic bowel conditions are fully rehabilitated after the first year on HPN, only a third of those with chronic intestinal dysmotility are similarly rehabilitated and it is most likely if the gut is not dilated.99 Impairment of strength and of well-being as a result of undernutrition and fluid and electrolyte imbalance will be corrected by HPN, but if the patient continues to experience vomiting, diarrhoea or abdominal pain from the underlying condition, quality of life will remain suboptimal. The annual risk of catheter-related sepsis among HPN patients is consistently around 0.5 per 1000 catheter days but tends to be higher among those with chronic pseudo-obstruction, especially if they remain on opioid analgesia103 144; by contrast, patients with systemic sclerosis who may tend to have lower opioid requirements have lower catheter infection rates.145
Over half of those with pseudo-obstruction receiving HPN will be alive at 10 years.146
9.5 Surgical options
Surgery is to be avoided in this group of patients who are at high risk of iatrogenic injury; however, judicious palliative surgical intervention (resection, bypass or stoma formation) can improve symptoms and quality of life.147 148 If constipation is difficult to manage and high volume saline washouts are needed, then colectomy with ileorectal anastomosis or ileostomy may be necessary but diarrhoea or continuing episodes of obstruction may remain a problem. Adhesiolysis in the absence of a clear focal obstruction carries a high risk of severe complications and morbidity with ultimately more adhesion recurrence and worsening pain. Urology is often needed to help with neuromuscular disorders of the urinary tract (dilated ureters and bladder) and stents and/or a suprapubic catheter may need to be inserted. Especially in women, there may be fertility problems due to dilated non-functioning fallopian tubes. Often the pains experienced result in gynaecological referrals.
9.5.1 Bypass surgery and enteric resections
There are several reports of surgery in adults to help these patients with pseudo-obstruction, although the clear separation into those with a myopathy and those with a neuropathy is not always made.90 147 After diagnostic laparotomy, bypass operations (gastro-enterostomy, duodeno-jejunostomy and jejuno-enterostomy) can be performed in adults to reduce vomiting if there is dilated gut. If gastric surgery is being performed, a vagotomy must be avoided as this will further retard gastrointestinal transit. Many have an ileostomy56 90 often to treat constipation and some develop a short bowel from multiple resections. The reports of success are variable and any undertaking of surgery needs to be a multidisciplinary decision and based on each individual patient. Outcome is poorer in patients with evidence of small bowel dysmotility who undergo colectomy.
9.5.2 Small intestinal transplantation
Dysmotility is a rare indication for intestinal transplantation in adults with dysmotility needing HPN, but since the outcomes of HPN are currently better, transplantation should be reserved for those who develop complications related to PN including IF-associated liver disease, central vein thrombosis with reduced venous access, and recurrent catheter-related bloodstream infections.140 149 150 If other organs are damaged, a multivisceral transplantation may be considered. The role of small bowel transplantation solely to improve quality of life by ceasing PN is somewhat contentious, but as worldwide experience of transplantation increases with corresponding improvements in survival rates, the indications for transplantation may broaden in the future. It is vital that all patients considered for transplantation are reviewed by an experienced MDT with expertise in IF and a transplant centre.151 Pain is not a good indication for a transplant.
9.6 Psychosocial treatments
Psychological support from nurses, physicians and psychologists is important. Vigilance needs to be maintained for the presence of psychopathology even in patients with a strong suspicion of gastrointestinal neuromuscular disorder. In one case series, six patients diagnosed initially with IF had significant psychopathology requiring specialised psychiatric unit treatment.25 In addition to psychological distress including anxiety and depression, other psychological problems encountered can include somatisation disorder, personality disorders, substance misuse and disordered eating (see also section 5.4). Dysmotility disorders can also be associated with a risk of self-harm including suicide. Clinical psychology and liaison psychiatry provide overlapping but complementary approaches and ideally a MDT involving both specialties should be available.
10.0 Outcomes
Outcome can vary from minor symptoms consistent with irritable bowel syndrome to problems resulting in home parenteral feeding, major analgesics and frequent hospital admissions. Causes of death in these patients include pulmonary aspiration, pulmonary embolism, cardiac failure and suicide. Cardiac failure may be the terminal event in hollow visceral myopathy. The relationship between 'megaduodenum' and upper gastrointestinal tract cancer seems tenuous if it exists. Death will often be related to the underlying condition—obviously so in the case of pseudo-obstruction occurring as a paraneoplastic phenomenon, and also particularly in the degenerative neuropathies, collagen vascular disorders and infiltrative conditions such as amyloid. Amiot et al reported 51 patients with CIPO who required HPN, representing 26 years of experience, and found that surgery was required in 84% of patients and survival probability was 94%, 78%, 75% and 68% at 1, 5, 10 and 15 years, respectively.56 Higher mortality was associated with systemic sclerosis. The 20-year experience of HPN from the Mayo Clinic found that the survival for patients with dysmotility disorders was second worse only to cancer due to the progression of the underlying disease, which was similar to data from St Mark’s Hospital in the UK. Recently published data from the Salford IF Unit have demonstrated worse outcomes for patients with a CIPO than a non-CIPO dysmotility phenotype.141 However, it would appear that there is room for improved outcomes in this challenging patient population by cost-effective investment in tertiary multidisciplinary provision.
11.0 Summary
Most cases of intestinal dysmotility will be without a clear diagnosis and thus labelled as idiopathic. Addressing the patient’s primary symptoms and treating malnutrition are the keys to management.
Footnotes
Twitter: @JoMartin_path
Contributors: JMDN wrote the manuscript. PP, JM, AE and SL contributed additional material and adjusted the text. JEM provided pathology input.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: There are no original data in this work.
References
- 1. Guyatt G, Oxman AD, Akl EA, et al. GRADE guidelines: 1. Introduction—GRADE evidence profiles and summary of findings tables. J Clin Epidemiol 2011;64:383–94. 10.1016/j.jclinepi.2010.04.026 [DOI] [PubMed] [Google Scholar]
- 2. Oxford University Centre for Evidence-Based Medicine Levels of evidence, 2009. Available: https://www.cebm.net/2009/06/oxford-centre-evidence-based-medicine-levels-evidence-march-2009/
- 3. Cawley C, Lal S, Nightingale J, et al. British Intestinal Failure Alliance (BIFA) guidance. Standardised parenteral support catheter guidelines. Available: www.bapen.org.uk/pdfs/bifa/standardised-parenteral-support-catheter-guidelines.pdf
- 4. Powell-Tuck J, Martin J, Domizio P, et al. Intestinal pseudo-obstruction : Nightingale JMD, Intestinal failure. Greenwich Medical Media Ltd, 2001: 123–39. [Google Scholar]
- 5. Kamm MA. Intestinal pseudo-obstruction. Gut 2000;47(Suppl 4):iv84. 10.1136/gut.47.suppl_4.iv84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Mann SD, Debinski HS, Kamm MA. Clinical characteristics of chronic idiopathic intestinal pseudo-obstruction in adults. Gut 1997;41:675–81. 10.1136/gut.41.5.675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Parker MC, Wilson MS, van Goor H, et al. Adhesions and colorectal surgery? Call for action. Colorect Dis 2007;9:66–72. 10.1111/j.1463-1318.2007.01342.x [DOI] [PubMed] [Google Scholar]
- 8. Bassotti G, Sietchiping-Nzepa F, de Roberto G, et al. Pseudo-pseudo-obstruction. Eur J Gastroenterol Hepatol 2004;16:1039–41. 10.1097/00042737-200410000-00014 [DOI] [PubMed] [Google Scholar]
- 9. Silk DBA. Pseudo-pseudo-obstruction: lessons in diagnosis and management. Eur J Gastroenterol Hepatol 2004;16:959–60. 10.1097/00042737-200410000-00002 [DOI] [PubMed] [Google Scholar]
- 10. Holdstock DJ, Misiewicz JJ. Factors controlling colonic motility: colonic pressures and transit after meals in patients with total gastrectomy, pernicious anaemia or duodenal ulcer. Gut 1970;11:100–10. 10.1136/gut.11.2.100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Rogers M, Cerda JJ. The narcotic bowel syndrome. J Clin Gastroenterol 1989;11:132–5. [PubMed] [Google Scholar]
- 12. Tuteja AK, Biskupiak J, Stoddard GJ, et al. Opioid-induced bowel disorders and narcotic bowel syndrome in patients with chronic non-cancer pain. Neurogastroenterol Motil 2010;22:e96:424–30. 10.1111/j.1365-2982.2009.01458.x [DOI] [PubMed] [Google Scholar]
- 13. Choung RS, Locke GR, Zinsmeister AR, et al. Opioid bowel dysfunction and narcotic bowel syndrome: a population-based study. Am J Gastroenterol 2009;104:1199–204. 10.1038/ajg.2009.71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Drossman DA, Morris CB, Edwards H, et al. Diagnosis, characterization, and 3-month outcome after detoxification of 39 patients with narcotic bowel syndrome. Am J Gastroenterol 2012;107:1426–40. 10.1038/ajg.2012.142 [DOI] [PubMed] [Google Scholar]
- 15. McNicol ED, Boyce D, Schumann R, et al. Mu-opioid antagonists for opioid-induced bowel dysfunction. Cochrane Database Syst Rev 2008:CD006332. 10.1002/14651858.CD006332.pub2 [DOI] [PubMed] [Google Scholar]
- 16. Sandgren JE, McPhee MS, Greenberger NJ. Narcotic bowel syndrome treated with clonidine. Resolution of abdominal pain and intestinal pseudo-obstruction. Ann Intern Med 1984;101:331–4. 10.7326/0003-4819-101-3-331 [DOI] [PubMed] [Google Scholar]
- 17. Akhondzadeh S, Ahmadi-Abhari SA, Assadi SM, et al. Double-blind randomized controlled trial of baclofen vs. clonidine in the treatment of opiates withdrawal. J Clin Pharm Ther 2000;25:347–53. 10.1046/j.1365-2710.2000.00295.x [DOI] [PubMed] [Google Scholar]
- 18. Nightingale J, Meade U, Leahy G, the BIFA Committee . The use of cyclizine in patients receiving parenteral nutrition, 2018. Available: www.bapen.org.uk/pdfs/bifa/position-statements/position-statement-on-use-of-cyclizine-in-patients-receiving-pn.pdf
- 19. Drossman DA, Chang L, Chey W, et al., Rome IV: the functional gastrointestinal disorders. Raleigh, NC: Rome foundation, 2016. [Google Scholar]
- 20. Törnblom H, Lindberg G, Nyberg B, et al. Full-thickness biopsy of the jejunum reveals inflammation and enteric neuropathy in irritable bowel syndrome. Gastroenterology 2002;123:1972–9. 10.1053/gast.2002.37059 [DOI] [PubMed] [Google Scholar]
- 21. American Psychiatric Association Diagnostic and statistical manual of mental disorders. 5th edn Arlington: American Psychiatric Association, 2013. [Google Scholar]
- 22. Robinson PH, Clarke M, Barrett J. Determinants of delayed gastric emptying in anorexia nervosa and bulimia nervosa. Gut 1988;29:458–64. 10.1136/gut.29.4.458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Hutson WR, Wald A. Gastric emptying in patients with bulimia nervosa and anorexia nervosa. Am J Gastroenterol 1990;85:41–6. [PubMed] [Google Scholar]
- 24. Hirakawa M, Okada T, Iida M, et al. Small bowel transit time measured by hydrogen breath test in patients with anorexia nervosa. Dig Dis Sci 1990;35:733–6. 10.1007/BF01540176 [DOI] [PubMed] [Google Scholar]
- 25. Kamal N, Chami T, Andersen A, et al. Delayed gastrointestinal transit times in anorexia nervosa and bulimia nervosa. Gastroenterology 1991;101:1320–4. 10.1016/0016-5085(91)90083-W [DOI] [PubMed] [Google Scholar]
- 26. Buchman AL, Ament ME, Weiner M, et al. Reversal of megaduodenum and duodenal dysmotility associated with improvement in nutritional status in primary anorexia nervosa. Dig Dis Sci 1994;39:433–40. 10.1007/BF02090220 [DOI] [PubMed] [Google Scholar]
- 27. Paine P, McMahon M, Farrer K, et al. Jejunal feeding: when is it the right thing to do? Frontline Gastroenterol:flgastro-2019-101181 10.1136/flgastro-2019-101181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Bourke J, Soldan J, Silk DBA, et al. 'Idiopathic' intestinal failure--the importance of identifying and treating primary psychopathology. Neurogastroenterol Motil 2012;24:242–51. 10.1111/j.1365-2982.2011.01847.x [DOI] [PubMed] [Google Scholar]
- 29. Winter TA, Lemmer ER, O'Keefe SJ, et al. The effect of severe undernutrition, and subsequent refeeding on digestive function in human patients. Eur J Gastroenterol Hepatol 2000;12:191–6. 10.1097/00042737-200012020-00010 [DOI] [PubMed] [Google Scholar]
- 30. Reynolds JV, O'Farrelly C, Feighery C, et al. Impaired gut barrier function in malnourished patients. Br J Surg 1996;83:1288–91. 10.1002/bjs.1800830934 [DOI] [PubMed] [Google Scholar]
- 31. Thieme ET, Postmus R. Superior mesenteric artery syndrome. Ann Surg 1961;154(6)Suppl:139–43. 10.1097/00000658-196112000-00017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Welsch T, Büchler MW, Kienle P. Recalling superior mesenteric artery syndrome. Dig Surg 2007;24:149–56. 10.1159/000102097 [DOI] [PubMed] [Google Scholar]
- 33. Merrett ND, Wilson RB, Cosman P, et al. Superior mesenteric artery syndrome: diagnosis and treatment strategies. J Gastrointest Surg 2009;13:287–92. 10.1007/s11605-008-0695-4 [DOI] [PubMed] [Google Scholar]
- 34. Smith BG, Hakim-Zargar M, Thomson JD. Low body mass index: a risk factor for superior mesenteric artery syndrome in adolescents undergoing spinal fusion for scoliosis. J Spinal Disord Tech 2009;22:144–8. 10.1097/BSD.0b013e31816b6b9a [DOI] [PubMed] [Google Scholar]
- 35. Wyten R, Kelty CJ, Falk GL. Laparoscopic duodenojejunostomy for the treatment of superior mesenteric artery (SMA) syndrome: case series. J Laparoendosc Adv Surg Tech A 2010;20:173–6. 10.1089/lap.2009.0237 [DOI] [PubMed] [Google Scholar]
- 36. Malfait F, Francomano C, Byers P, et al. The 2017 International Classification of the Ehlers-Danlos syndromes. Am J Med Genet C Semin Med Genet 2017;175:8–26. 10.1002/ajmg.c.31552 [DOI] [PubMed] [Google Scholar]
- 37. Fikree A, Grahame R, Aktar R, et al. A prospective evaluation of undiagnosed joint hypermobility syndrome in patients with gastrointestinal symptoms. Clin Gastroenterol Hepatol 2014;12:1680–7. 10.1016/j.cgh.2014.01.014 [DOI] [PubMed] [Google Scholar]
- 38. Beckers AB, Keszthelyi D, Fikree A, et al. Gastrointestinal disorders in joint hypermobility syndrome/Ehlers-Danlos syndrome hypermobility type: a review for the gastroenterologist. Neurogastroenterol Motil 2017;29:e13013. 10.1111/nmo.13013 [DOI] [PubMed] [Google Scholar]
- 39. Valent P, Akin C, Doctor AC. Doctor, I think I am suffering from MCAS: differential diagnosis and separating facts from fiction. J Allergy Clin Immunol Pract 2019;7:1109–14. 10.1016/j.jaip.2018.11.045 [DOI] [PubMed] [Google Scholar]
- 40. Smith VV, Lake BD, Kamm MA, et al. Intestinal pseudo-obstruction with deficient smooth muscle alpha-actin. Histopathology 1992;21:535–42. 10.1111/j.1365-2559.1992.tb00441.x [DOI] [PubMed] [Google Scholar]
- 41. Knowles CH, Silk DBA, Darzi A, et al. Deranged smooth muscle alpha-actin as a biomarker of intestinal pseudo-obstruction: a controlled multinational case series. Gut 2004;53:1583–9. 10.1136/gut.2003.037275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Gamba E, Carr NJ, Bateman AC. Deficient alpha smooth muscle actin expression as a cause of intestinal pseudo-obstruction: fact or fiction? J Clin Pathol 2004;57:1168–71. 10.1136/jcp.2003.015297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Schuffler MD, Lowe MC, Bill AH. Studies of idiopathic intestinal pseudoobstruction. I. Hereditary hollow visceral myopathy: clinical and pathological studies. Gastroenterology 1977;73:327–38. [PubMed] [Google Scholar]
- 44. Schuffler MD, Pagon RA, Schwartz R, et al. Visceral myopathy of the gastrointestinal and genitourinary tracts in infants. Gastroenterology 1988;94:892–8. 10.1016/0016-5085(88)90544-6 [DOI] [PubMed] [Google Scholar]
- 45. Higman D, Peters P, Stewart M. Familial hollow visceral myopathy with varying urological manifestations. Br J Urol 1992;70:435–8. 10.1111/j.1464-410X.1992.tb15804.x [DOI] [PubMed] [Google Scholar]
- 46. Schuffler MD, Pope CE. Studies of idiopathic intestinal pseudoobstruction. II. Hereditary hollow visceral myopathy: family studies. Gastroenterology 1977;73:339–44. [PubMed] [Google Scholar]
- 47. Rodrigues CA, Shepherd NA, Lennard-Jones JE, et al. Familial visceral myopathy: a family with at least six involved members. Gut 1989;30:1285–92. 10.1136/gut.30.9.1285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Fitzgibbons PL, Chandrasoma PT. Familial visceral myopathy. Evidence of diffuse involvement of intestinal smooth muscle. Am J Surg Pathol 1987;11:846–54. [PubMed] [Google Scholar]
- 49. Martin JE, Benson M, Swash M, et al. Myofibroblasts in hollow visceral myopathy: the origin of gastrointestinal fibrosis? Gut 1993;34:999–1001. 10.1136/gut.34.7.999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Smith VV, Milla PJ. Histological phenotypes of enteric smooth muscle disease causing functional intestinal obstruction in childhood. Histopathology 1997;31:112–22. 10.1046/j.1365-2559.1997.2250839.x [DOI] [PubMed] [Google Scholar]
- 51. Ruuska TH, Karikoski R, Smith VV, et al. Acquired myopathic intestinal pseudo-obstruction may be due to autoimmune enteric leiomyositis. Gastroenterology 2002;122:1133–9. 10.1053/gast.2002.92396 [DOI] [PubMed] [Google Scholar]
- 52. Oton E, Moreira V, Redondo C, et al. Chronic intestinal pseudo-obstruction due to lymphocytic leiomyositis: is there a place for immunomodulatory therapy? Gut 2005;54:1343–4. 10.1136/gut.2005.071811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Schuffler MD, Rohrmann CA, Chaffee RG, et al. Chronic intestinal pseudo-obstruction. A report of 27 cases and review of the literature. Medicine 1981;60:173–96. [PubMed] [Google Scholar]
- 54. Domsic R, Fasanella K, Bielefeldt K. Gastrointestinal manifestations of systemic sclerosis. Dig Dis Sci 2008;53:1163–74. 10.1007/s10620-007-0018-8 [DOI] [PubMed] [Google Scholar]
- 55. Schuffler MD, Beegle RG. Progressive systemic sclerosis of the gastrointestinal tract and hereditary hollow visceral myopathy: two distinguishable disorders of intestinal smooth muscle. Gastroenterology 1979;77:664–71. 10.1016/0016-5085(79)90218-X [DOI] [PubMed] [Google Scholar]
- 56. Amiot A, Joly F, Alves A, et al. Long-term outcome of chronic intestinal pseudo-obstruction adult patients requiring home parenteral nutrition. Am J Gastroenterol 2009;104:1262–70. 10.1038/ajg.2009.58 [DOI] [PubMed] [Google Scholar]
- 57. Harrison E, Herrick AL, Dibb M, et al. Long-term outcome of patients with systemic sclerosis requiring home parenteral nutrition. Clin Nutr 2015;34:991–6. 10.1016/j.clnu.2014.11.002 [DOI] [PubMed] [Google Scholar]
- 58. Perlemuter G, Chaussade S, Wechsler B, et al. Chronic intestinal pseudo-obstruction in systemic lupus erythematosus. Gut 1998;43:117–22. 10.1136/gut.43.1.117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Paine P, McLaughlin J, Lal S. Review article: the assessment and management of chronic severe gastrointestinal dysmotility in adults. Aliment Pharmacol Ther 2013;38:1209–29. 10.1111/apt.12496 [DOI] [PubMed] [Google Scholar]
- 60. Forbes A. Radiation enteritis : Nightingale JMD, Intestinal failure. Greenwich Medical Media Ltd, 2001: 141–52. [Google Scholar]
- 61. Cousins AJ. Home enzyme replacement therapy for lysosomal storage disorders. Br J Home Healthcare 2008;4:7–9. [Google Scholar]
- 62. Veress B, Nyberg B, Törnblom H, et al. Intestinal lymphocytic epithelioganglionitis: a unique combination of inflammation in bowel dysmotility: a histopathological and immunohistochemical analysis of 28 cases. Histopathology 2009;54:539–49. 10.1111/j.1365-2559.2009.03265.x [DOI] [PubMed] [Google Scholar]
- 63. Amiot A, Tchikviladzé M, Joly F, et al. Frequency of mitochondrial defects in patients with chronic intestinal pseudo-obstruction. Gastroenterology 2009;137:101–9. [DOI] [PubMed] [Google Scholar]
- 64. Nishino I, Spinazzola A, Papadimitriou A, et al. Mitochondrial neurogastrointestinal encephalomyopathy: an autosomal recessive disorder due to thymidine phosphorylase mutations. Ann Neurol 2000;47:792–800. [DOI] [PubMed] [Google Scholar]
- 65. Blondon H, Polivka M, Joly F, et al. Digestive smooth muscle mitochondrial myopathy in patients with mitochondrial-neuro-gastro-intestinal encephalomyopathy (MNGIE). Gastroentérologie Clinique et Biologique 2005;29:773–8. 10.1016/S0399-8320(05)86346-8 [DOI] [PubMed] [Google Scholar]
- 66. Rahman S. Gastrointestinal and hepatic manifestations of mitochondrial disorders. J Inherit Metab Dis 2013;36:659–73. 10.1007/s10545-013-9614-2 [DOI] [PubMed] [Google Scholar]
- 67. Knowles CH, Lang B, Clover L, et al. A role for autoantibodies in some cases of acquired non-paraneoplastic gut dysmotility. Scand J Gastroenterol 2002;37:166–70. 10.1080/003655202753416821 [DOI] [PubMed] [Google Scholar]
- 68. Törnblom H, Lang B, Clover L, et al. Autoantibodies in patients with gut motility disorders and enteric neuropathy. Scand J Gastroenterol 2007;42:1289–93. 10.1080/00365520701396216 [DOI] [PubMed] [Google Scholar]
- 69. Kashyap P, Farrugia G. Enteric autoantibodies and gut motility disorders. Gastroenterol Clin North Am 2008;37:397–410. vi-vii. 10.1016/j.gtc.2008.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Debinski HS, Kamm MA, Talbot IC, et al. DNA viruses in the pathogenesis of sporadic chronic idiopathic intestinal pseudo-obstruction. Gut 1997;41:100–6. 10.1136/gut.41.1.100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Selgrad M, De Giorgio R, Fini L, et al. JC virus infects the enteric glia of patients with chronic idiopathic intestinal pseudo-obstruction. Gut 2009;58:25–32. 10.1136/gut.2008.152512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Lindberg G. Chronic intestinal pseudo-obstruction: how important is JC virus infection? Gut 2009;58:2–3. 10.1136/gut.2008.160101 [DOI] [PubMed] [Google Scholar]
- 73. Meneghelli UG. Chagasic enteropathy. Rev Soc Bras Med Trop 2004;37:252–60. 10.1590/S0037-86822004000300012 [DOI] [PubMed] [Google Scholar]
- 74. Pulliam TJ, Schuster MM. Congenital markers for chronic intestinal pseudoobstruction. Am J Gastroenterol 1995;90:922–6. [PubMed] [Google Scholar]
- 75. Matulis SR, McJunkin B, Chang HH. Familial visceral neuropathy as part of a diffuse neuronal syndrome: four fatal cases in one sibship. Am J Gastroenterol 1994;89:792–6. [PubMed] [Google Scholar]
- 76. Smith VV, Schäppi MG, Bisset WM, et al. Lymphocytic leiomyositis and myenteric ganglionitis are intrinsic features of cystic fibrosis: studies in distal intestinal obstruction syndrome and meconium ileus. J Pediatr Gastroenterol Nutr 2009;49:42–51. 10.1097/MPG.0b013e318186d35a [DOI] [PubMed] [Google Scholar]
- 77. Vianello M, Vitaliani R, Pezzani R, et al. The spectrum of antineuronal autoantibodies in a series of neurological patients. J Neurol Sci 2004;220:29–36. 10.1016/j.jns.2004.01.008 [DOI] [PubMed] [Google Scholar]
- 78. Arasaradnam RP, Brown S, Forbes A, et al. Guidelines for the investigation of chronic diarrhoea in adults: British Society of Gastroenterology, 3rd edition. Gut 2018;67:1380–99. 10.1136/gutjnl-2017-315909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. National Collaborating Centre for Acute Care Group NICE guidelines. Nutritional support in adults: oral supplements, enteral and parenteral feeding, 2006. [PubMed] [Google Scholar]
- 80. Di Nardo G, Blandizzi C, Volta U, et al. Review article: molecular, pathological and therapeutic features of human enteric neuropathies. Aliment Pharmacol Ther 2008;28:25–42. 10.1111/j.1365-2036.2008.03707.x [DOI] [PubMed] [Google Scholar]
- 81. Accarino A, Perez F, Azpiroz F, et al. Abdominal distention results from caudo-ventral redistribution of contents. Gastroenterology 2009;136:1544–51. 10.1053/j.gastro.2009.01.067 [DOI] [PubMed] [Google Scholar]
- 82. Menys A, Butt S, Emmanuel A, et al. Comparative quantitative assessment of global small bowel motility using magnetic resonance imaging in chronic intestinal pseudo-obstruction and healthy controls. Neurogastroenterol Motil 2016;28:376–83. 10.1111/nmo.12735 [DOI] [PubMed] [Google Scholar]
- 83. de Jonge CS, Smout AJPM, Nederveen AJ, et al. Evaluation of gastrointestinal motility with MRI: advances, challenges and opportunities. Neurogastroenterol Motil 2018;30:e13257. 10.1111/nmo.13257 [DOI] [PubMed] [Google Scholar]
- 84. Rezaie A, Buresi M, Lembo A, et al. Hydrogen and methane-based breath testing in gastrointestinal disorders: the North American consensus. Am J Gastroenterol 2017;112:775–84. 10.1038/ajg.2017.46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Valdovinos MA, Camilleri M, Thomforde GM, et al. Reduced accuracy of 14C-D-xylose breath test for detecting bacterial overgrowth in gastrointestinal motility disorders. Scand J Gastroenterol 1993;28:963–8. 10.3109/00365529309098292 [DOI] [PubMed] [Google Scholar]
- 86. Suri J, Kataria R, Malik Z, et al. Elevated methane levels in small intestinal bacterial overgrowth suggests delayed small bowel and colonic transit. Medicine 2018;97:e10554. 10.1097/MD.0000000000010554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Vantrappen G, Janssens J, Hellemans J, et al. The interdigestive motor complex of normal subjects and patients with bacterial overgrowth of the small intestine. J Clin Invest 1977;59:1158–66. 10.1172/JCI108740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Oliveira RB, Meneghelli UG, de Godoy RA, et al. Abnormalities of interdigestive motility of the small intestine in patients with Chagas' disease. Dig Dis Sci 1983;28:294–9. 10.1007/BF01324944 [DOI] [PubMed] [Google Scholar]
- 89. Stanghellini V, Camilleri M, Malagelada JR. Chronic idiopathic intestinal pseudo-obstruction: clinical and intestinal manometric findings. Gut 1987;28:5–12. 10.1136/gut.28.1.5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Stanghellini V, Cogliandro RF, De Giorgio R, et al. Natural history of chronic idiopathic intestinal pseudo-obstruction in adults: a single center study. Clin Gastroenterol Hepatol 2005;3:449–58. 10.1016/S1542-3565(04)00675-5 [DOI] [PubMed] [Google Scholar]
- 91. Quigley EM, Donovan JP, Lane MJ, et al. Usefulness and limitations as an outpatient study. Dig Dis Sci 1992;37:20–8. [DOI] [PubMed] [Google Scholar]
- 92. Wang YT, Mohammed SD, Farmer AD, et al. Regional gastrointestinal transit and pH studied in 215 healthy volunteers using the wireless motility capsule: influence of age, gender, study country and testing protocol. Aliment Pharmacol Ther 2015;42:761–72. 10.1111/apt.13329 [DOI] [PubMed] [Google Scholar]
- 93. Yung D, Douglas S, Hobson AR, et al. Morpho-functional evaluation of small bowel using wireless motility capsule and video capsule endoscopy in patients with known or suspected Crohn's disease: pilot study. Endosc Int Open 2016;4:E480–6. 10.1055/s-0042-100718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Quigley EMM, Deprez PH, Hellstrom P, et al. Ambulatory intestinal manometry: a consensus report on its clinical role. Dig Dis Sci 1997;42:2395–400. 10.1023/A:1018803819455 [DOI] [PubMed] [Google Scholar]
- 95. Gill RC, Kellow JE, Browning C, et al. The use of intraluminal strain gauges for recording ambulant small bowel motility. Am J Physiol 1990;258:G610–5. 10.1152/ajpgi.1990.258.4.G610 [DOI] [PubMed] [Google Scholar]
- 96. Lindberg G, Iwarzon M, Stål P, et al. Digital ambulatory monitoring of small-bowel motility. Scand J Gastroenterol 1990;25:216–24. 10.1080/00365521.1990.12067094 [DOI] [PubMed] [Google Scholar]
- 97. Waldron B, Storey BE, Smith D, et al. Computerised method for acquisition and display of gastrointestinal motility data. Med Biol Eng Comput 1991;29:304–8. 10.1007/BF02446713 [DOI] [PubMed] [Google Scholar]
- 98. Benson MJ, Castillo FD, Wingate DL, et al. The computer as referee in the analysis of human small bowel motility. Am J Physiol 1993;264:G645–54. 10.1152/ajpgi.1993.264.4.G645 [DOI] [PubMed] [Google Scholar]
- 99. Oliveira RB, Wingate DL, Castillo FD, et al. Prolonged small bowel manometry in Chagas' disease: a model for the diagnosis of enteric dysmotility. Gastroenterology 1997;112:A800. [Google Scholar]
- 100. Hackelsberger N, Schmidt T, Renner R, et al. Ambulatory long-term jejunal manometry in diabetic patients with cardiac autonomic neuropathy. Neurogastroenterol Motil 1997;9:77–83. 10.1046/j.1365-2982.1997.d01-23.x [DOI] [PubMed] [Google Scholar]
- 101. Kellow JE, Gill RC, Wingate DL. Prolonged ambulant recordings of small bowel motility demonstrate abnormalities in the irritable bowel syndrome. Gastroenterology 1990;98:1208–18. 10.1016/0016-5085(90)90335-X [DOI] [PubMed] [Google Scholar]
- 102. Knowles CH, Veress B, Tornblom H, et al. Safety and diagnostic yield of laparoscopically assisted full-thickness bowel biospy. Neurogastroenterol Motil 2008;20:774–9. 10.1111/j.1365-2982.2008.01099.x [DOI] [PubMed] [Google Scholar]
- 103. Vasant DH, Kalaiselvan R, Ablett J, et al. The chronic intestinal pseudo-obstruction subtype has prognostic significance in patients with severe gastrointestinal dysmotility related intestinal failure. Clin Nutr 2018;37:1967–75. 10.1016/j.clnu.2018.09.008 [DOI] [PubMed] [Google Scholar]
- 104. Giniès J-L, François H, Joseph M-G, et al. A curable cause of chronic idiopathic intestinal pseudo-obstruction in children: idiopathic myositis of the small intestine. J Pediatr Gastroenterol Nutr 1996;23:426–9. 10.1097/00005176-199611000-00012 [DOI] [PubMed] [Google Scholar]
- 105. Camilleri M, Malagelada JR, Abell TL, et al. Effect of six weeks of treatment with cisapride in gastroparesis and intestinal pseudoobstruction. Gastroenterology 1989;96:704–12. 10.1016/0016-5085(89)90893-7 [DOI] [PubMed] [Google Scholar]
- 106. British National Formulary , 2010. Available: https://www.bnf.org/
- 107. European Medicines Agency European Medicines Agency recommends changes to the use of metoclopramide. changes aim mainly to reduce the risk of neurological side effects, 2013. Available: https://www.ema.europa.eu/en/news/european-medicines-agency-recommends-changes-use-metoclopramide
- 108. Evans BW, Clark WK, Moore DJ, et al. Tegaserod for the treatment of irritable bowel syndrome and chronic constipation. Cochrane Database Syst Rev 2007:CD003960. 10.1002/14651858.CD003960.pub3 [DOI] [PubMed] [Google Scholar]
- 109. Bardhan KD, Forbes A, Marsden CL, et al. The effects of withdrawing tegaserod treatment in comparison with continuous treatment in irritable bowel syndrome patients with abdominal pain/discomfort, bloating and constipation: a clinical study. Aliment Pharmacol Ther 2004;20:213–22. 10.1111/j.1365-2036.2004.02032.x [DOI] [PubMed] [Google Scholar]
- 110. Chey WD, Howden CW, Tack J, et al. Long-term tegaserod treatment for dysmotility-like functional dyspepsia: results of two identical 1-year cohort studies. Dig Dis Sci 2010;55:684–97. 10.1007/s10620-009-1049-0 [DOI] [PubMed] [Google Scholar]
- 111. Emmanuel AV, Kamm MA, Roy AJ, et al. Randomised clinical trial: the efficacy of prucalopride in patients with chronic intestinal pseudo-obstruction--a double-blind, placebo-controlled, cross-over, multiple n = 1 study. Aliment Pharmacol Ther 2012;35:48–55. 10.1111/j.1365-2036.2011.04907.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Surrenti E, Camilleri M, Kammer PP, et al. Antral axial forces postprandially and after erythromycin in organic and functional dysmotilities. Dig Dis Sci 1996;41:697–704. 10.1007/BF02213125 [DOI] [PubMed] [Google Scholar]
- 113. Minami T, Nishibayashi H, Shinomura Y, et al. Effects of erythromycin in chronic idiopathic intestinal pseudo-obstruction. J Gastroenterol 1996;31:855–9. 10.1007/BF02358615 [DOI] [PubMed] [Google Scholar]
- 114. Chini P, Toskes PP, Waseem S, et al. Effect of azithromycin on small bowel motility in patients with gastrointestinal dysmotility. Scand J Gastroenterol 2012;47:422–7. 10.3109/00365521.2012.654402 [DOI] [PubMed] [Google Scholar]
- 115. Soudah HC, Hasler WL, Owyang C. Effect of octreotide on intestinal motility and bacterial overgrowth in scleroderma. N Engl J Med 1991;325:1461–7. 10.1056/NEJM199111213252102 [DOI] [PubMed] [Google Scholar]
- 116. Owyang C. Octreotide in gastrointestinal motility disorders. Gut 1994;35(3 suppl):S11–14. 10.1136/gut.35.3_Suppl.S11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Perlemuter G, Cacoub P, Chaussade S, et al. Octreotide treatment of chronic intestinal pseudoobstruction secondary to connective tissue diseases. Arthritis Rheum 1999;42:1545–9. [DOI] [PubMed] [Google Scholar]
- 118. Verne GN, Eaker EY, Hardy E, et al. Effect of octreotide and erythromycin on idiopathic and scleroderma-associated intestinal pseudoobstruction. Dig Dis Sci 1995;40:1892–901. 10.1007/BF02208652 [DOI] [PubMed] [Google Scholar]
- 119. Bharucha AE, Low PA, Camilleri M, et al. Pilot study of pyridostigmine in constipated patients with autonomic neuropathy. Clin Auton Res 2008;18:194–202. 10.1007/s10286-008-0476-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Bharucha AE, Low P, Camilleri M, et al. A randomised controlled study of the effect of cholinesterase inhibition on colon function in patients with diabetes mellitus and constipation. Gut 2013;62:708–15. 10.1136/gutjnl-2012-302483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Schang JC, Devroede G. Beneficial effects of naloxone in a patient with intestinal pseudoobstruction. Am J Gastroenterol 1985;80:407–11. [PubMed] [Google Scholar]
- 122. Dufour P, Gendre P. Long-term mucosal alterations by sennosides and related compounds. Pharmacology 1988;36(Suppl 1):194–202. 10.1159/000138440 [DOI] [PubMed] [Google Scholar]
- 123. Kiernan JA, Heinicke EA. Sennosides do not kill myenteric neurons in the colon of the rat or mouse. Neuroscience 1989;30:837–42. 10.1016/0306-4522(89)90175-9 [DOI] [PubMed] [Google Scholar]
- 124. Pearson JS, Pollard C, Whorwell PJ. Avoiding analgesic escalation and excessive healthcare utilization in severe irritable bowel syndrome: a role for intramuscular anticholinergics? Therap Adv Gastroenterol 2014;7:232–7. 10.1177/1756283X14540028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Faculty of Pain Medicine of the Royal College of Anaethetists. Opioids aware. Available: www.fpm.ac.uk/opioids-aware
- 126. Sobin WH, Heinrich TW, Drossman DA. Central neuromodulators for treating functional GI disorders: a primer. Am J Gastroenterol 2017;112:693–702. 10.1038/ajg.2017.57 [DOI] [PubMed] [Google Scholar]
- 127. Kilgallon E, Vasant DH, Green D, et al. Chronic continuous abdominal pain: evaluation of diagnostic features, iatrogenesis and drug treatments in a cohort of 103 patients. Aliment Pharmacol Ther 2019;49:1282–92. 10.1111/apt.15241 [DOI] [PubMed] [Google Scholar]
- 128. Mari A, Abu Backer F, Mahamid M, et al. Bloating and abdominal distension: clinical approach and management. Adv Ther 2019;36:1075–84. 10.1007/s12325-019-00924-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129. Abell T, McCallum R, Hocking M, et al. Gastric electrical stimulation for medically refractory gastroparesis. Gastroenterology 2003;125:421–8. 10.1016/S0016-5085(03)00878-3 [DOI] [PubMed] [Google Scholar]
- 130. Andersson S, Lönroth H, Simrén M, et al. Gastric electrical stimulation for intractable vomiting in patients with chronic intestinal pseudoobstruction. Neurogastroenterol Motil 2006;18:823–30. 10.1111/j.1365-2982.2006.00801.x [DOI] [PubMed] [Google Scholar]
- 131. Soffer E, Abell T, Lin Z, et al. Review article: gastric electrical stimulation for gastroparesis--physiological foundations, technical aspects and clinical implications. Aliment Pharmacol Ther 2009;30:681–94. 10.1111/j.1365-2036.2009.04082.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. Musunuru S, Beverstein G, Gould J. Preoperative predictors of significant symptomatic response after 1 year of gastric electrical stimulation for gastroparesis. World J Surg 2010;34:1853–8. 10.1007/s00268-010-0586-1 [DOI] [PubMed] [Google Scholar]
- 133. Frøkjaer JB, Bergmann S, Brock C, et al. Modulation of vagal tone enhances gastroduodenal motility and reduces somatic pain sensitivity. Neurogastroenterol Motil 2016;28:592–8. 10.1111/nmo.12760 [DOI] [PubMed] [Google Scholar]
- 134. Kapural L, Nagem H, Tlucek H, et al. Spinal cord stimulation for chronic visceral abdominal pain. Pain Med 2010;11:347–55. 10.1111/j.1526-4637.2009.00785.x [DOI] [PubMed] [Google Scholar]
- 135. Mailis-Gagnon A, Furlan AD, Sandoval JA, et al. Spinal cord stimulation for chronic pain. Cochrane Database Syst Rev 2004:CD003783. 10.1002/14651858.CD003783.pub2 [DOI] [PubMed] [Google Scholar]
- 136. Jarrett MED, Varma JS, Duthie GS, et al. Sacral nerve stimulation for faecal incontinence in the UK. Br J Surg 2004;91:755–61. 10.1002/bjs.4545 [DOI] [PubMed] [Google Scholar]
- 137. Kenefick NJ. Sacral nerve neuromodulation for the treatment of lower bowel motility disorders. Ann R Coll Surg Engl 2006;88:617–23. 10.1308/003588406X149174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138. Kamm MA, Dudding TC, Melenhorst J, et al. Sacral nerve stimulation for intractable constipation. Gut 2010;59:333–40. 10.1136/gut.2009.187989 [DOI] [PubMed] [Google Scholar]
- 139. Mowatt G, Glazener C, Jarrett M. Sacral nerve stimulation for faecal incontinence and constipation in adults. Cochrane Database Syst Rev 2007:CD004464. 10.1002/14651858.CD004464.pub2 [DOI] [PubMed] [Google Scholar]
- 140. Nightingale J, Woodward JM, Small Bowel and Nutrition Committee of the British Society of Gastroenterology . Guidelines for management of patients with a short bowel. Gut 2006;55(Suppl 4):iv1–12. 10.1136/gut.2006.091108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141. Dibb M, Soop M, Teubner A, et al. Survival and nutritional dependence on home parenteral nutrition: three decades of experience from a single referral centre. Clin Nutr 2017;36:570–6. 10.1016/j.clnu.2016.01.028 [DOI] [PubMed] [Google Scholar]
- 142. Pironi L, Steiger E, Joly F, et al. Intravenous supplementation type and volume are associated with 1-year outcome and major complications in patients with chronic intestinal failure. Gut 2020;69:1787–1795. 10.1136/gutjnl-2018-318172 [DOI] [PubMed] [Google Scholar]
- 143. Howard L, Heaphey L, Fleming CR, et al. Four years of North American Registry home parenteral nutrition outcome data and their implications for patient management. JPEN J Parenter Enteral Nutr 1991;15:384–93. 10.1177/0148607191015004384 [DOI] [PubMed] [Google Scholar]
- 144. Richards DM, Scott NA, Shaffer JL, et al. Opiate and sedative dependence predicts a poor outcome for patients receiving home parenteral nutrition. JPEN J Parenter Enteral Nutr 1997;21:336–8. 10.1177/0148607197021006336 [DOI] [PubMed] [Google Scholar]
- 145. Harrison E, Herrick AL, McLaughlin J, et al. 22 years experience managing patients with systemic sclerosis on home parenteral nutrition. Clin Nutr ESPEN 2015;10:e178. 10.1016/j.clnesp.2015.03.005 [DOI] [PubMed] [Google Scholar]
- 146. Lloyd DAJ, Vega R, Bassett P, et al. Survival and dependence on home parenteral nutrition: experience over a 25-year period in a UK referral centre. Aliment Pharmacol Ther 2006;24:1231–40. 10.1111/j.1365-2036.2006.03106.x [DOI] [PubMed] [Google Scholar]
- 147. Mughal MM, Irving MH. Treatment of end stage chronic intestinal pseudo-obstruction by subtotal enterectomy and home parenteral nutrition. Gut 1988;29:1613–7. 10.1136/gut.29.11.1613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148. Murr MM, Sarr MG, Camilleri M. The surgeon's role in the treatment of chronic intestinal pseudoobstruction. Am J Gastroenterol 1995;90:2147–51. [PubMed] [Google Scholar]
- 149. Kaufman SS, Avitzur Y, Beath SV, et al. New insights into the indications for intestinal transplantation: consensus in the year 2019. Transplantation 2020;104:937–46. 10.1097/TP.0000000000003065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150. Lauro A, Pinna AD, Tossani E, et al. Multimodal surgical approach for adult patients with chronic intestinal pseudo-obstruction: clinical and psychosocial long-term outcomes. Transplant Proc 2018;50:226–33. 10.1016/j.transproceed.2017.11.012 [DOI] [PubMed] [Google Scholar]
- 151. Nightingale J. Nutrition support teams: how they work, are set up and maintained. Frontline Gastroenterol 2010;1:171–7. 10.1136/fg.2009.000224 [DOI] [PMC free article] [PubMed] [Google Scholar]


