Abstract
To facilitate the applications of home blood pressure (HBP) monitoring in clinical settings, the Taiwan Hypertension Society and the Taiwan Society of Cardiology jointly put forward the Consensus Statement on HBP monitoring according to up-to-date scientific evidence by convening a series of expert meetings and compiling opinions from the members of these two societies. In this Consensus Statement as well as recent international guidelines for management of arterial hypertension, HBP monitoring has been implemented in diagnostic confirmation of hypertension, identification of hypertension phenotypes, guidance of anti-hypertensive treatment, and detection of hypotensive events. HBP should be obtained by repetitive measurements based on the " 722" principle, which is referred to duplicate blood pressure readings taken per occasion, twice daily, over seven consecutive days. The " 722" principle of HBP monitoring should be applied in clinical settings, including confirmation of hypertension diagnosis, 2 weeks after adjustment of antihypertensive medications, and at least every 3 months in well-controlled hypertensive patients. A good reproducibility of HBP monitoring could be achieved by individuals carefully following the instructions before and during HBP measurement, by using validated BP devices with an upper arm cuff. Corresponding to office BP thresholds of 140/90 and 130/80 mmHg, the thresholds (or targets) of HBP are 135/85 and 130/80 mmHg, respectively. HBP-based hypertension management strategies including bedtime dosing (for uncontrolled morning hypertension), shifting to drugs with longer-acting antihypertensive effect (for uncontrolled evening hypertension), and adding another antihypertensive drug (for uncontrolled morning and evening hypertension) should be considered. Only with the support from medical caregivers, paramedical team, or tele- monitoring, HBP monitoring could reliably improve the control of hypertension.
Keywords: Antihypertensive, Blood pressure, Home, Hypertension
1. INTRODUCTION
1.1 Home blood pressure monitoring
With the understanding that different hypertension phenotypes have distinct prognosis, out-of-office blood pressure (BP) monitoring receives growing attention in contemporary hypertension guidelines because it helps discern hypertension phenotypes along with office BP (OBP).1-4 Home BP (HBP) monitoring and ambulatory BP (ABP) monitoring are two recognized approaches to obtaining out-of-office BP. Thanks to technological advances and readable accessibility of automatic oscillometric sphygmomanometers, HBP monitoring is a promising, easy-to-use, and well-accepted modality to facilitate the diagnosis and control of hypertension.5
HBP monitoring is referred to measurements of BP at home usually by oneself, or on occasion, by caregivers or research assistants. Compared to OBP, HBP is more likely to be free of environmental and/or emotional stress (such as white-coat effect). Yet it is a feasible approach to documenting long-term BP variations.1 A good reproducibility and reliability of HBP could be achieved by careful measurements according to standardized instructions before and during HBP monitoring.4
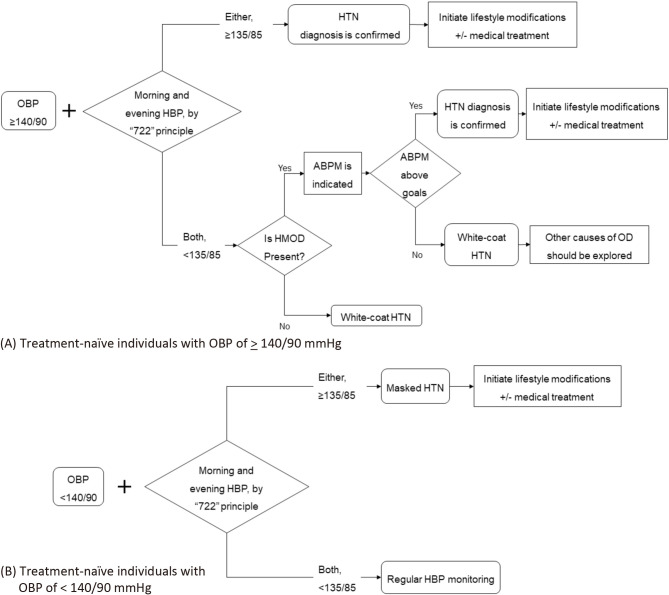
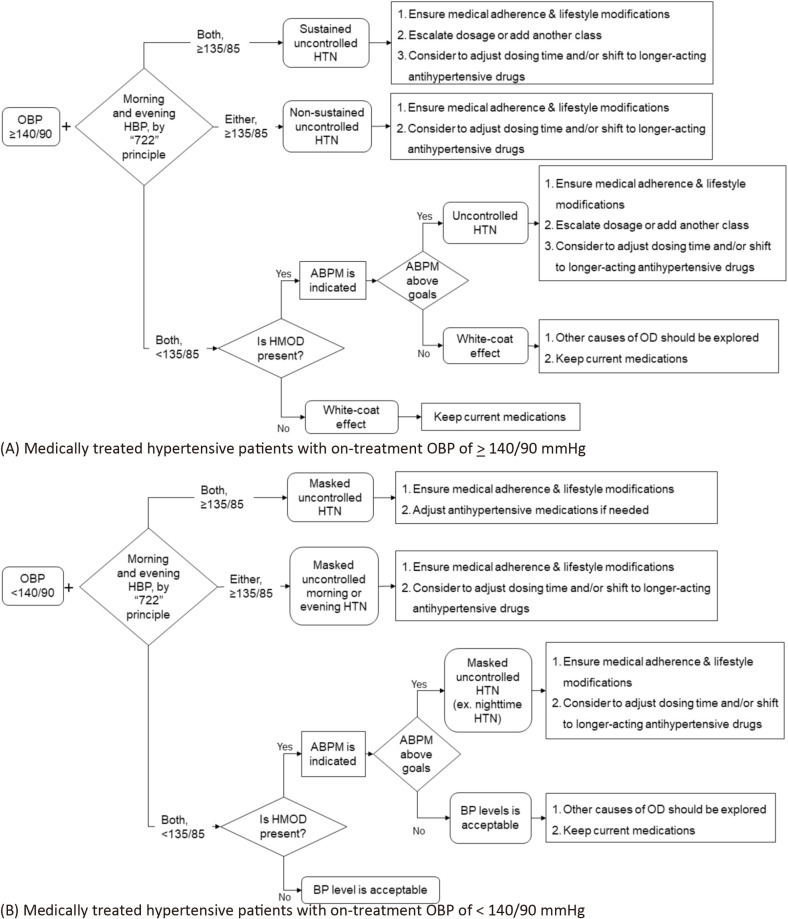
While evidence on the relationship between HBP and cardiovascular outcomes has been accumulating,6-10 the consensus on HBP monitoring to facilitate the applications of HBP monitoring in clinical settings is required. The Taiwan Hypertension Society (THS) and the Taiwan Society of Cardiology (TSOC) jointly put forward the Consensus Statement on HBP monitoring according to up-to-date scientific evidence (Table 1). We recommend the "722" principle to obtain reliable HBP measurement to confirm the diagnosis of hypertension and guide the adjustment of antihypertensive medications (Table 2). Schematic approaches which integrate OBP, HBP, and ABP for treatment-naïve individuals and individuals treated with antihypertensive medications are also provided (Figures 1 and 2).
Table 1. Consensus recommendations on HBP monitoring in diagnosis and management of arterial hypertension.
| Recommendations | COR | LOE |
| The role of HBP monitoring in the diagnosis and management of hypertension | ||
| 1. HBP is one form of out-of-office BP; and is, if measured appropriately, able to be used for diagnostic confirmation of OBP, identification of hypertension phenotypes, guidance of anti-hypertensive treatment, and improvement of hypertension control. | I | B |
| Methods to perform HBP monitoring correctly | ||
| 2. HBP is obtained at home, preferably using automated oscillometric upper-arm sphygmomanometer, which should be validatedand regularly calibrated (at least every 12 months). The device is better equipped with capabilities of automatic data recording and/or auto-transmission. | I | C |
| 3. Cuff selection: following manufacturer’s instructions (cuff bladder width and length are at least 40% and 80% of arm circumference, respectively). | I | B |
| Before measurement: | ||
| 30 min: avoid vigorous exercise and caffeine-containing drink; empty bladder | ||
| 5 min: sitting rest at a chair with back support and feet flat on the ground (not leg dangling or crossing) | ||
| On measurement: upper arm, the one with higher averaged SBP reading, supported at the level of heart. | ||
| Methods to obtain reliable HBP estimates | ||
| 4. As for hypertension diagnosis or HBP-guided antihypertensive management, HBP should be measured according to the “722” principle. That is, HBP should be measured for “7” (at least 4) consecutive days, in the morning (taken within 1 hour after awakening, but before taking food and medication) and the evening (within 1 hour before bedtime) (“2” occasions), and with ≥ “2” (≥ 3, if atrial fibrillation is present) BP readings, 1-min apart, on each occasion. Morning and evening HBP estimates are the averages of all morning and evening BP readings, respectively, except those obtained on the first day. | I | B |
| 5. The 722 principle should be applied in the confirmation of hypertension diagnosis and 2 weeks after adjustment of antihypertensive medications. In uncontrolled hypertensive patients, HBP monitoring should be performed following the 722 principle at least monthly. In well-controlled hypertensive patients, HBP monitoring could be performed following the 722 principle at least every 3 months. At least one measurement (duplicate readings, at least one minute apart, on one occasion) per week is a suitable alternative follow-up strategy for stable hypertensive patients. | IIa | C |
| Methods to diagnose and identify hypertension phenotypes | ||
| 6. Hypertension could be diagnosed if HBP estimate is ≥ 135/85 mmHg, whose corresponding OBP is ≥ 140/90 mmHg. | I | B |
| 7. HBP monitoring is adequate to identify sustained hypertension, white-coat hypertension, and masked hypertension, which could be confirmed by ABP monitoring if necessary. | I | C |
| Methods to implement HBP-guided initiation and titration of antihypertensive treatment | ||
| 8. Hypertension is regarded as well-controlled if both morning and evening HBP are < 135/85 mmHg (obtained based on the “722” principle). | IIa | C |
| 9. Patients with HMOD or at high risk for cardiovascular disease should be controlled at the level of HBP estimate of < 130/80 mmHg, whose corresponding OBP is < 130/80 mmHg. | IIa | B |
| 10. HBP-based hypertension management strategies including bedtime dosing (for uncontrolled morning hypertension), shifting to drugs with longer-acting antihypertensive effect (for uncontrolled evening hypertension), and adding another antihypertensive drug (for uncontrolled morning and evening hypertension) should be considered. | IIa | B |
| 11. Given that high home BP variability is associated with increased cardiovascular risk, adjustment of antihypertensive medications (with longer duration of actions or balanced 24-hour coverage) to lower home BP variability might be considered. | IIb | B |
| 12. HBP monitoring is recommended to identify orthostatic hypotension, postprandial hypotension, and hypotension events during antihypertensive treatment. | IIa | C |
| Methods to improve hypertension control with HBP monitoring | ||
| 13. HBP monitoring could improve hypertension control, especially when combined with active interventions (such as team-based interventions or telemonitoring). | IIa | B |
| 14. Implementation of HBP monitoring in clinical practice could be facilitated by increasing awareness of physicians and patients in “SERVE” ways, and insurance reimbursement. | IIa | C |
ABP, ambulatory blood pressure; BP, blood pressure; COR, class of recommendation; HBP, home blood pressure; HMOD, hypertension-mediated organ damage; LOE, level of evidence; OBP, office blood pressure.
Table 2. The “722” principle for home blood pressure monitoring.
| “722” principle | Timing of HBP monitoring |
| “7” | 7 (at least 4) consecutive days |
| “2” | 2 times per day: in the morning (taken within 1 hour after awakening, after voiding, and before taking food and medications) and in the evening (within 1 hour before bedtime) |
| “2” | 2 or more BP readings, 1 minute apart, taken per occasion (≥ 3 BP readings if atrial fibrillation) |
| Settings in the clinic | Frequency of HBP monitoring with the “722” principle |
| Normal blood pressure (< 120/80 mmHg) | Every 1 year |
| High normal blood pressure (120-129/< 80 mmHg) | Every 6 months |
| Elevated blood pressure (130-139/80-89 mmHg) | Every 3 months |
| Hypertension (≥ 140/90 mmHg) | |
| Treatment-naïve | One “722” cycle, for confirmation of diagnosis and phenotype identification |
| Initiation of drug therapy | 2 weeks later, then every 1 month if uncontrolled, or every 3 months if under control |
| Adjustment of drug therapy | 2 weeks later, then every 1 month if uncontrolled, or every 3 months if under control |
| Treated but uncontrolled | Every 1 month |
| Treated and controlled | Every 3 months |
BP, blood pressure; HBP, home blood pressure.
Figure 1.
Schematic representations of integrating home blood pressure monitoring with office and ambulatory blood pressure monitoring in management of hypertension for antihypertensive treatment-naïve individuals. ABPM, ambulatory blood pressure monitoring; BP, blood pressure; HBP, home blood pressure; HMOD, hypertension-mediated organ damage; HTN, hypertension; OBP, office blood pressure; OD, organ damage. The recommended flowchart of diagnosis and management of hypertension for treatment-naïve patients with office BP of ≥ 140/90 mmHg (A) or with office BP of < 140/90 mmHg (B). Averaged HBP is derived according the “722” principle.
Figure 2.
Schematic representations of integrating home blood pressure monitoring with office and ambulatory blood pressure monitoring in management of hypertension for hypertensive patients treated with antihypertensive medications. ABPM, ambulatory blood pressure monitoring; BP, blood pressure; CCB, calcium channel blocker; HBP, home blood pressure; HMOD, hypertension-mediated organ damage; HTN, hypertension; OBP, office blood pressure; OD, organ damage. The recommended flowchart of management of hypertension for medically treated hypertensive patients with on-treatment office BP of ≥ 140/90 mmHg (A) or with on-treatment office BP of < 140/90 mmHg (B). HBP includes morning and evening BP, of which both should be below HBP targets (< 135/80 mmHg, in general; < 130/80 mmHg, if at high risk).
1.2 Guidelines/Focused Update/Consensus development
Taiwan Hypertension Guidelines and related works (Focused Update/Consensus) evaluate and integrate available evidence with the purpose of assisting healthcare professionals in constructing the best management strategies for each individual patient. Members of this Task Force were jointly selected by the Taiwan Hypertension Society (THS) and the Hypertension Committee of Taiwan Society of Cardiology (TSOC) to represent professionals from a broad array of backgrounds. The class of recommendation (COR) and level of evidence (LOE) were graded according to predefined scales as modified from the latest American and European guidelines for the management of arterial hypertension (Table 1A and 1B). The THS/TSOC Guidelines/Focused Update/Consensus undergo extensive review by the Task Force and external experts and are approved by all Task Force members. The guidelines and related works were developed independently without any involvement from the industry. The Task Force members’ comprehensive disclosure information is shown at the end of this Consensus. The THS/TSOC Hypertension Guidelines/Focused Update/Consensus represent the official position of the THS and TSOC.
Table 1A. THS/TSOC classes of recommendations (updated March 2019).
| Classes of recommendations | Definition | Suggested phrases |
| Class I (Benefit >>> Risk) | Evidence and/or general agreement that a given treatment of procedure is beneficial, useful, and effective | • Is recommended |
| • Is indicated | ||
| • Should be performed | ||
| Class II | Conflicting evidence and/or a divergence of opinion about the usefulness/efficacy of the given treatment or procedure | |
| Class IIa (Benefit >/>> Risk) | Weight of evidence/opinion is in favor of usefulness/efficacy | • Is probably recommended |
| • Should be considered | ||
| • Can be performed | ||
| Class IIb (Benefit ≥ Risk) | Usefulness/efficacy is less well established by evidence/opinion | • May/might be considered |
| • May/might be reasonable | ||
| • May/might be performed | ||
| Class III (Benefit ≤ Risk) | Evidence or general agreement that the given treatment or procedure is not useful/effective, and in some cases may be harmful | • Is not recommended |
| • Is not indicated | ||
| • Should not be performed |
THS, Taiwan Hypertension Society; TSOC, Taiwan Society of Cardiology.
Table 1B. THS/TSOC levels of evidence (updated Mar 2019).
| Level A | Data derived from multiple (≥ 2) RCTs, or meta-analyses of high-quality RCTs |
| Level B | Data derived from a single RCT, large non-randomized studies, meta-analyses of moderate-quality RCTs or non-randomized studies |
| Level C | Subgroup analyses, post-hoc analyses, retrospective studies, cohort studies, registries, small studies, or consensus of expert opinion |
RCT, randomized controlled trial; THS, Taiwan Hypertension Society; TSOC, Taiwan Society of Cardiology.
Adherence to guidelines and related works can be improved by shared decision making between healthcare professionals and patients, with patient engagement in choosing strategies based on individual preferences, values, and associated conditions. Guidelines and related works should not override clinical judgement, which is the right and responsibility of healthcare professionals. It is also the responsibility of healthcare professionals to verify the rules and regulations applicable to drugs and devices at the time of prescription.
2. DEFINITION AND CLINICAL SIGNIFICANCE OF HBP MONITORING
Consensus recommendation
#1. HBP is one form of out-of-office BP; and is, if measured appropriately, able to be used for diagnostic confirmation of OBP, identification of hypertension phenotypes, guidance of anti-hypertensive treatment, and improvement of hypertension control.
2.1 Definition of HBP monitoring
Highlights
• The term "HBP monitoring" indicates measurement of own blood pressures, not exclusively by oneself, at home.
HBP monitoring is referred to measurement of BP at home, usually by himself/herself,11 or on occasion, by caregivers or research assistants.12 While self-measured BP (SMBP) is referred to BP taken in non-medical out-of-office environments, such as at home, at a work place, at a pharmacy, or at a convenience store.13 HBP and SMBP are not entirely the same, though they are often deemed interchangeable.
2.2 Prognostic significance of HBP monitoring
Highlights
• HBP monitoring can predict hypertension-mediated organ damage and is a useful tool to predict cardiovascular prognosis.
• Nocturnal HBP, mostly measured at midnight, can be assessed by certain pre-programmed automatic devices. Nocturnal HBP fairly correlated with nighttime ABP.
HBP has the advantage over OBP as it improves cardiovascular risk assessment. As BP varies in response to physiological and environmental changes and over time, averaging multiple HBP readings predicts risks of cardiovascular morbidities and morality more accurately than OBP readings.6,7,14
2.2.1 HBP and hypertension-mediated organ damage (HMOD)
The presence of HMOD hallmarks the poor control of hypertension (Table 3). Relative to those without HMOD, patients with HMOD are even less likely to attain their BP targets.15 Studies have suggested that elevated HBP is more strongly associated with increased left ventricular mass and/or left ventricular hypertrophy when compared with OBP in patients with hypertension.16-18 Besides, albuminuria and carotid intimal thickness are more closely correlated with HBP than with OBP.19-22
Table 3. Hypertension-mediated organ damage (HMOD).
| Organ | HMOD |
| Brain | |
| Stroke (ischemia/hemorrhage) | |
| Transient ischemic attack | |
| Cognitive impairment | |
| Eyes | |
| Hypertensive retinopathy | |
| Heart | |
| Left ventricular hypertrophy by electrocardiography or echocardiography | |
| Nonvalvular atrial fibrillation | |
| Heart failure | |
| Kidney | |
| Chronic kidney disease | |
| Proteinuria/albuminuria | |
| Arteries | |
| Carotid atherosclerosis | |
| Aortic stiffness (baPWV ≥ 18 m/sec, cfPWV > 10 m/sec) | |
| Aortic aneurysm | |
| Peripheral artery disease (low ABI [< 0.9]) |
ABI, ankle-brachial index; baPWV, brachial-ankle pulse wave velocity; cfPWV, carotid-femoral pulse wave velocity.
2.2.2 HBP and cardiovascular risk
Prospective studies have shown that HBP predicts cardiovascular outcomes more accurately than OBP.7,12,23,24 The first evidence showing the superior prognostic value of HBP to OBP came from the Ohasama study of 1789 participants in Japan. Based on the initial BP measurements, HBP had a stronger predictive power for mortality than BP at screening did.7 It was later shown in 2051 Italian subjects of the Pressioni Arteriose Monitorate E Loro Associazioni (PAMELA) study, in which HBP improved predictive model for mortality when compared to OBP.6 Finally, in the Finn-Home study that enrolling 2081 subjects in Finland, HBP was prognostically superior to OBP for risk prediction of fatal and nonfatal cardiovascular events.24
2.2.3 HBP is complementary to OBP
BP measures in different settings provide complementary information. The discrepancies in BP levels between office measures and out-of-office measures define another two categories of patients who have discrepant office and out-of-office BP measures — namely white-coat hypertension and masked hypertension. Neither of the conditions is considered to be completely benign when compared to true normotension.25 When compared with normotension (defined as OBP < 140/90 mmHg and HBP < 135/85 mmHg), masked hypertension (defined as OBP < 140/90 mmHg and HBP ≥ 135/85 mmHg) clearly had a higher risk of cardiovascular events.14 Even though it remains an ongoing debate on whether those with white-coat hypertension (defined as OBP ≥ 140/90 mmHg and HBP < 135/85 mmHg) have unfavorable outcomes,14,26,27 the long-term mortality was still increased among those with persistently elevated OBP.28
2.2.4 Prognostic value of HBP versus ABP
HBP could be as reproducible as ABP.29 When information derived from ABP monitoring limits to a fixed day with unrestricted routine activities, HBP monitoring provides information at fixed timing and conditions over a longer period of time. HBP monitoring allows BP measured in standardized conditions and theoretically assesses BP variability (BPV), which has been further associated with HMOD and long-term events.30,31 Clinical studies and meta-analyses have suggested that HBP is as good as ABP in regard to their association with preclinical organ damage.21,32,33 Nevertheless, ABP is more prognostically informative than HBP or OBP.6,34
2.2.5 Nocturnal HBP
With the advance of technology, nocturnal HBP, mostly measured at midnight, can be assessed by automatic devices with pre-determined programming.35 Nocturnal HBP fairly correlated with nighttime ABP.36 With a limited number of patients, nocturnal HBP appeared to have modest correlations with HMOD, such as left ventricular mass index, albuminuria, and carotid intima-media thickness.36 In the Japan Morning Surge-Home Blood Pressure (J-HOP) study, nocturnal HBP was a predictor of coronary events and stroke, independent of morning HBP and OBP.37
2.3 Differences in the mean values of HBP, OBP, automated OBP (AOBP), and ABP
Highlights
• Differences exist between mean values of OBP and HBP. Whereas the differences between mean values of AOBP, HBP, and daytime ABP are negligible (Tables 4 and 5).
Table 4. Diagnostic criteria of hypertension according to office, home, and ambulatory blood pressure.
| Blood pressure | OBP, mmHg | HBP, mmHg | ABP, mmHg | ||
| 24-hr average | Daytime average | Nighttime average | |||
| Systolic | ≥ 140 | ≥ 135 | ≥ 130 | ≥ 135 | ≥ 120 |
| Diastolic | ≥ 90 | ≥ 85 | ≥ 80 | ≥ 85 | ≥ 70 |
ABP, ambulatory blood pressure; HBP, home blood pressure; OBP, office blood pressure.
Table 5. Corresponding values of systolic and diastolic readings between office blood pressure (OBP) and home blood pressure (HBP).
| Classification | OBP, mmHg | HBP, mmHg |
| Normal blood pressure | ||
| Systolic | 120 | 120 |
| Diastolic | 80 | 80 |
| High normal blood pressure | ||
| Systolic | 130 | 130 |
| Diastolic | 80 | 80 |
| Stage I hypertension | ||
| Systolic | 140 | 135 |
| Diastolic | 90 | 85 |
| Stage II hypertension | ||
| Systolic | 160 | 145 |
| Diastolic | 100 | 90 |
| Stage III hypertension | ||
| Systolic | 180 | 160 |
| Diastolic | 110 | 100 |
Data from the International Database of HOme blood pressure in relation to Cardiovascular Outcome (IDHOCO) study showed that HBP was generally lower than OBP in 5689 untreated subjects. The differences between HBP and OBP varied according to age. In this study, for systolic BP (SBP) readings, the difference between HBP and OBP was around 7 mmHg for individuals aged > 30 years, but was smaller in younger subjects (p = 0.001). For diastolic BP (DBP) readings, OBP was consistently higher than HBP and the in-between difference decreased with aging (p < 0.001).38
When considering about AOBP measurement and out-of-office measurement techniques, one recent meta-analysis of twenty-six studies showed that there were no significant differences in the mean values of AOBP with HBP (SBP, -2.65; 95% CI, -8.42 to 3.12; DBP, -1.67; 95% CI, -4.20 to 0.87), or with daytime ABP (SBP, -1.85; 95% CI, -4.50 to 0.79; DBP, 0.12; 95% CI, -1.42 to 1.66).39 In another study comparing daytime ABP and HBP, it was found that the mean difference between daytime ABP and HBP was 0.5 mmHg (95% CI, -1.9 to 2.9) for SBP, and 0.6 mmHg (95% CI, -1.1 to 2.3) for DBP, indicating differences in the averaged values between daytime ABP and HBP were negligible.40
2.4 Hypertension phenotypes identified by HBP and OBP
Highlights
• HBP monitoring is used to identify sustained hypertension, white-coat hypertension (effect), and masked (uncontrolled) hypertension.
• Other hypertension phenotypes, such as morning, evening, and nighttime hypertension, also predict cardiovascular risks.
Along with OBP, HBP could be used to determine several hypertension phenotypes, which are associated with increased risks for cardiovascular events. Besides white-coat and masked hypertension, concerns are growing regarding other hypertension phenotypes, such as morning, evening, and nighttime hypertension. Although historically being the gold standard for white-coat hypertension and masked hypertension, 24-hr ABP monitoring is not widely used because of its cost and inconvenience. In a study surveying the preference of BP monitoring in patients with untreated hypertension, it showed that 7-day HBP monitoring was preferred and more acceptable than 24-hr ABP monitoring, though the latter was conceived as more reliable than the former.41 HBP monitoring can provide multiple measurements over longer periods and identify day-to-day BP variability.
Morning and evening BP have been shown to predict future cardiovascular events.8,9,42 Differences in hypertension and related cardiovascular risks have been reported between Western and Asian populations. Asian patients have a higher rate of stroke and metabolic syndrome, which is often associated with higher morning and nighttime BP readings.43 Till recently, an innovative automated HBP monitoring device has been developed for measuring nighttime BP,37 and its clinical applications await further studies.
3. MEASUREMENT OF HBP
Consensus recommendations
#2. HBP is obtained at home, preferably using automated oscillometric upper-arm sphygmomanometer, which should be validated and regularly calibrated (at least every 12 months). The device is better equipped with capabilities of automatic data recording and/or auto-transmission.
#3. Cuff selection: following manufacturer’s instructions (cuff bladder width and length are at least 40% and 80% of arm circumference, respectively).
Before measurement:
30 min: avoid vigorous exercise and caffeine-containing drinks; empty bladder
5 min: sitting rest at a chair with back support and feet flat on the ground (not leg dangling or crossing)
On measurement: upper arm, the one with higher averaged SBP reading, supported at the level of heart.
#4. As for hypertension diagnosis or HBP-guided antihypertensive management, HBP should be measured according to the "722" principle. That is, HBP should be measured for "7" (at least 4) consecutive days, in the morning (taken within 1 hour after awakening, but before taking food and medication) and the evening (within 1 hour before bedtime) ("2" occasions), and with ≥ "2" (≥ 3, if atrial fibrillation is present) BP readings, 1-min apart, on each occasion. Morning and evening HBP estimates are the averages of all morning and evening BP readings, respectively, except those obtained on the first day.
#5. The 722 principle should be applied in the confirmation of hypertension diagnosis and 2 weeks after adjustment of antihypertensive medications. In uncontrolled hypertensive patients, HBP monitoring should be performed following the 722 principle at least monthly. In well-controlled hypertensive patients, HBP monitoring could be performed following the 722 principle at least every 3 months. At least one measurement (duplicate readings, at least one minute apart, on one occasion) per week is a suitable alternative follow-up strategy for stable hypertensive patients.
3.1 Validation and calibration of blood pressure devices
Highlights
• Periodic calibration of automated oscillometric sphygmomanometer should be done at an interval of not greater than 12 months.
• HBP monitors which measure BP with the upper arm cuff instead of signals from wrists or fingers should be used.
The mercury sphygmomanometer is once regarded as gold standard for BP measurement, but it is not practical to be used in community settings because of environmental concerns. The accuracy of non-mercury sphygmomanometer is considered acceptable if its estimated probability of a tolerable error (≤ 10 mmHg) is at least 85%.44 There are two common types of non-mercury sphygmomanometer: oscillometer and aneroid devices. The oscillometer devices are operated automatically, and the inflation and deflation of the cuff are controlled electronically. Periodic calibration of automated oscillometric sphygmomanometer should be done at an interval of not greater than 12 months.45
Aneroid sphygmomanometer is an alternative device in clinical setting as mercury sphygmomanometer is not available. The aneroid devices are operated manually and require a normal BP cuff and a stethoscope. They are liquid-free and use mechanical parts to relay BP to the gauge. There are wall-mounted type and portable type aneroid sphygmomanometer. Wall-mounted aneroid sphygmomanometer may require less frequent calibration than portable type device. In order to ensure the accuracy of aneroid sphygmomanometer, it is needed to calibrate, every 6 months for wall-mounted and every 2 to 4 weeks for portable type devices.13
Few wearable watch-type (with cuff) and cuffless BP monitoring devices may be accurate if used exactly as directed.46,47 More studies are needed to investigate the role of wearable BP monitoring device in clinical practice. Recently, the first study comparing a watch-type wearable BP monitor with a conventional ABP monitor showed the difference between the wearable and ambulatory devices was acceptable both in and out of the office.48 However, most experts recommend using a HBP monitor that uses the upper-arm cuff instead of wrist or finger BP monitors.13
3.2 Pre-measurement instructions
Highlights
• Standardization of measurement procedures should be implemented to improve the reliability of HBP monitoring in clinical practice.
• A validated automated oscillometric upper-arm cuff sphygmomanometer is recommended for HBP measurement.
• Selections of proper cuff size, and methods of measurements and recordings should be instructed to patients whom HBP monitoring is advised for.
Before BP measurement, choosing a validated automated oscillometric upper-arm cuff sphygmomanometer is advised. Wrist and finger BP devices are not recommended because their measurement reliability remains questionable. Select the proper cuff size according to the individual’s arm circumference. The length of inflatable cuff bladder must cover 80%-100% of the individual’s arm circumference. It is better to measure BP in a quiet room with comfortable temperature. Don’t smoke, drink alcohol, caffeinated beverages, have meals or exercise within 30 minutes before BP measurement. It is also suggested to have measurement before drug intake. Given that BP is lower in standing position, sitting position is the standard. Empty bladder, remain seated and relaxed at least 5 minutes before measurements. Have the arm resting on table, supported on a flat surface with mid-arm at heart level; back straight and supported on chair; legs uncrossed and feet flat on floor. Make sure the bottom of the cuff is placed directly above the bend of the elbow. Avoid talking or moving before, during and between measurements. Don’t take the measurement over clothes.
If BP is measured for the first time, it is suggested to check BP of right and left upper arms. Provided that the difference of < 15 mmHg between right and left upper-arm SBPs, the arm with higher SBP should be used. Measure BP at the same time every day if possible. It is best to take the readings daily in the morning and in the evening for 7 consecutive days (the so-called 722 principle, which is detailed in section 3.3) for people with unknown BP status or two weeks after antihypertensive medications are implemented or adjusted. The Task Force recommends to repeat the 7-day measurement course every 1-3 month for all hypertensive patients.50,51 Daily monitoring before your next clinic appointment for 4 to 7 consecutive days is suggested. Each time you measure, take ≥ 2 readings one minute apart and record all BP readings or the averages on each measurement occasion. Take the record to the clinics at every visit (Table 2). At least one measurement (duplicate readings, at least one minute apart, on one occasion) per week is a suitable alternative follow-up strategy for stable hypertensive patients.49
For those whose upper-arm BP cannot be measured, measuring leg BP is acceptable. Usually the SBP in the legs is 10% to 20% higher than the brachial SBP. BP measurement in the legs should be applied at the mid-thigh by listening over the popliteal artery in prone or supine position. The bladder of the cuff should be about 40% of the circumference of the thigh, and the length should be about 75% to 80% of this circumference. The pre-measurement preparation and other instruction is the same as measurement in sitting position. Make the annotation on your BP record if the measurement is done on legs.
3.3 Measurement frequency, timing, and number per occasion of HBP monitoring
Highlights
• Implementation of the "722" principle regarding how to obtain reliable HBP readings could facilitate the adoption of HBP monitoring in the community.
• Measurement frequency, timing, and number per occasion could be individualized to improve adherence and to drive the formation of habits.
Most clinical studies derived HBP estimates from the averages of morning and evening HBP readings separately over varying periods of time. The Ohasama study obtained 4-week single morning HBP in 1789 participants ≥ 40 years of age.7 After 6.6 years of follow-up, individuals with elevated averages of ≥ 3 HBP readings had a greater cardiovascular mortality risk than those with elevated OBP.7 In a community-based study, 1186 elderly aged ≥ 65 years were followed for 4 years to identify the association between HBP and death.52 Duplicate morning and evening HBP readings were measured for 5 consecutive days, and were averaged to obtain HBP estimates. The results indicated a U-shaped association of systolic HBP with all-cause mortality, of which increased cardiovascular death was associated with high systolic HBP, whereas increased non-cardiovascular death was with low systolic HBP. To compare with OBP with regard to predicting CV events, a study enrolling 4939 treated hypertensive patients followed for a mean of 3.2 years showed that, rather than elevated OBP, cardiovascular prognosis was poorer in those with elevated HBP, which was estimated as the average of 4-day triplicate morning and evening HBP readings.14 In the Didima study, 1997 adults aged 54.1 years undertook duplicate morning and evening HBP measurements for 3 days.53 HBP was defined as the average of all morning and evening HBP readings, and was as good as OBP in assessing the CV risk over a mean follow-up period of 8.2 years.53 To compare HBP and ABP in predicting the development of HMOD, 502 participants were enrolled to measure their BP twice every morning and every evening over the consecutive 7 days.54 By averaging all morning and evening readings, HBP marginally improved the predictability of OBP-based model, while ABP clearly improved the predictability of both HBP and OBP-based model.54
For evaluating the timing and number per occasion for blood pressure measurement, several clinical trials could be taken into consideration. The more measurements taken, the more precise BP estimates are, at expense of time consumed. An average of HBP of up to 14 days showed a dose-dependent increase in prognostic power than averages of fewer days in Ohasama study.55 In the Treatment of Hypertension Based on Home or Office Blood Pressure (THOP) trial, patients performed HBP measurement twice daily (in the morning between 6 and 10 AM and in the evening between 6 and 10 PM) on 3 consecutive days.56 In the Finn-Home Study, two SBP readings in the morning on a minimum of 3 days appear to be sufficient for measuring home BP variability in the general population, with an interval of 2 minutes between the 2 measures. More measurement would bring improvement in prognostic accuracy.57 The Improving the Detection of Hypertension (IDH) study took the value of the mean of 2 morning and 2 evening HBP readings for a minimum of 2 days, and a single morning and single evening or 2 morning BP readings for a minimum of 3 days. The measurements were separated for 1 minute.58 The Hypertension Intervention Nurse Telemedicine Study (HINTS) found the mean SBP could be accurately categorized with 80% probability based on the mean of 5 HBP measurements in most patients.59 IDHOCO study showed that hypertension would be reliably diagnosed by a mean of at least 6 readings during 6 days.60
We therefore recommend to measure HBP for 7 consecutive days (according to the Ohasama study, which reported the optimal prognostic power of averaging 14 measurements), in 2 occasions (in the morning and in the evening) per day, and 2 readings, 1 minute apart, in one occasion (the "722" principle) (Table 2). The minimal consecutive days could be shortened to 4 days (first day data discarded) since at least 6 measurements are required to reach adequate diagnosis in the IDHOCO study. Morning and evening HBP estimates are the averages of all morning and evening BP readings, respectively, except those obtained on the first day. The 722 principle should be applied in the confirmation of hypertension diagnosis and 2 weeks after adjustment of antihypertensive medications. In uncontrolled hypertensive patients, HBP monitoring should be performed following the 722 principle at least monthly. In well-controlled hypertensive patients, HBP monitoring could be performed at least once weekly,49 or following the 722 principle at least every 3 months (according to the HOMED-BP study, section 4.2.1).50,51,61
3.4 Use of oscillometric BP device in patients with atrial fibrillation
Highlights
• The optimal method for measuring BP in patients with atrial fibrillation remains under investigation, but consecutive (at least ≥ 3) readings should be obtained in patients with atrial fibrillation.
Atrial fibrillation (AF) is one of the most prevalent cardiac arrhythmias.62 Hypertension is the most common comorbidity in AF patients. In various registries and studies, about 60% to 80% of AF patients had hypertension. Uncontrolled hypertension predisposes AF patients into increased risk of hemorrhagic stroke. As a result, detection and management of hypertension is of utmost importance in AF patients.
Given oscillometric BP monitors use oscillometric pressure wave amplitude during cuff deflation or inflation to estimate SBP and DBP,63,64 irregular R-R interval in AF imposes challenges to estimate BP using oscillometric methods. The optimal method to measure BP in AF patients remains under investigation. There is evidence that increasing the number of consecutive measurements (to ≥ 3) may increase the correlation of noninvasive method and invasive BP measurement.65 In a meta-analysis,66 the authors revealed that automated monitors seemed to be more accurate in measuring SBP, but not DBP for AF. Nonetheless, another meta-analysis found difficulties in generalizing across different devices, because there is marked heterogeneity of accuracy between devices.67
Because proprietary algorithms vary to estimate BP in oscillometric BP devices, clinician should choose machines which have been validated specifically in AF patients.68 Various societies and organizations have proposed different validation protocols for BP monitors.13 There are resources on the web that list validated BP monitors like https://bihsoc.org/bp-monitors/provided by British and Irish Hypertension Society and https://stridebp.org/ by Stride BP. Since the validation results done in general population might not be applied to AF patients, ANSI/AAMI/ISO currently considered AF as a special population for which the additional validation is required.
4. HBP CUT-OFFS, TARGETS, AND HBP-BASED MANAGEMENT OF HYPERTENSION
Consensus recommendations
#6. Hypertension could be diagnosed if HBP estimate is ≥ 135/85 mmHg, whose corresponding OBP is ≥ 140/90 mmHg.
#7. HBP monitoring is adequate to identify sustained hypertension, white-coat hypertension, and masked hypertension, which could be confirmed by ABP monitoring if necessary.
#8. Hypertension is regarded as well-controlled if both morning and evening HBP are < 135/85 mmHg (obtained based on the "722" principle).
#9. Patients with HMOD or at high risk for cardiovascular disease should be controlled at the level of HBP estimate of < 130/80 mmHg, whose corresponding OBP is < 130/80 mmHg.
#10. HBP-based hypertension management strategies including bedtime dosing (for uncontrolled morning hypertension), shifting to drugs with longer-acting antihypertensive effect (for uncontrolled evening hypertension), and adding another antihypertensive drug (for uncontrolled morning and evening hypertension) should be considered.
#11. Given that high home BP variability is associated with increased cardiovascular risk, adjustment of antihypertensive medications (with longer duration of actions or balanced 24-hour coverage) to lower home BP variability might be considered.
#12. HBP monitoring is recommended to identify orthostatic hypotension, postprandial hypotension, and hypotension events during antihypertensive treatment.
4.1 HBP cut-offs corresponding to OBP
Highlights
• Corresponding to clinic BP of 140/90 mmHg, the HBP threshold for hypertension should be 135/85 mmHg.
• Corresponding to clinic BP of 130/80 mmHg, the HBP threshold for hypertension should be 130/80 mmHg.
• Corresponding to clinic BP of 130/80 mmHg, the HBP threshold for hypertension should be 130/80 mmHg.
4.1.1 Reverse causality
To determine the optimal BP levels for hypertension management, findings obtained from the survival data of observational cohort studies can cause critical misconception. Reverse causation is one of the bias that frequently misleads the study conclusions of the observational studies, which has been clearly demonstrated in a previous large observation study reporting a terminal decline of SBP in the final 2 years of life. The study findings that outcome (the mortality) can inversely influence the exposure (subjects’ BP) suggest that nonrandomized epidemiological associations of low SBP with higher mortality may be caused by reverse causality,69 which may help explain the discrepancy between clinical trial results and nonrandomized studies, and it is not appropriate to base BP treatment recommendations on nonrandomized data for effectiveness outcomes.70
4.1.2 Recent evolution of hypertension guideline and the role of HBP monitoring
It should be stressed that OBP (unattended or not), HBP, and ABP are all different BP modalities and should provide complimentary clinical values for the management of hypertension. Lately, the importance of out-of-office BP measurements to confirm the diagnosis of hypertension and assess hypertension control has been emphasized in several latest hypertension guidelines.1,4,71-74 In addition to the superior prognostic values, self-measurement of BP at home renders several advantages over conventional clinic office BP. HBP monitoring can help identify patients with different hypertension phenotypes including white-coat, masked, and sustained hypertension with readings taken according to standardized instructions. It is easy, well-tolerated, reliable, and accessible for patients,75 and associated with little measurement variability, and good reproducibility.76 However, the diagnosis and treatment of hypertension are still mainly based on the OBP in spite of the many advantages of HBP measurement. One reason for the limited use of HBP measurement is that physicians are unfamiliar with the operational thresholds of HBP for initiating and adjusting treatment. Besides, in the diagnosis of the hypertension phenotypes (normotension, sustained hypertension, white-coat hypertension, or masked hypertension), it is also imperative to take into account the cut-off thresholds of HBP used to define these phenotypes.
4.1.3 Corresponding HBP values to OBP values
Different BP thresholds for home and office BP have been proposed in recent hypertension guidelines.1,4,71-74 The new American College of Cardiology (ACC)/American Heart Association (AHA) guideline has also proposed new BP thresholds for initiation or titration of antihypertensive drug treatment.71 The OBP cutoff of 140/90 and 160/100 mmHg is proposed to be equivalent to lower HBP threshold of 135/85 and 145/90 mmHg, respectively. The HBP cutoff level for stage 1 hypertension is proposed to be the same as the OBP threshold of 130/80 mmHg.
HBP cutoffs can be identified by the regression approach and/or outcome-based approach, which estimate the HBP values with which subjects have comparable risk of cardiovascular events in agreement with the corresponding OBP thresholds.77 Unanimously, the OBP thresholds recommended in evidence-based hypertension guidelines are based on the findings of randomized controlled trials.
Based on the findings of outcome-based international cohort studies,78 we have corresponded the HBP levels to the commonly used OBP thresholds as shown in Table 5. In summary, corresponding to OBP of 140/90 mmHg, HBP threshold for hypertension should be 135/ 85 mmHg; and corresponding to OBP of 130/80 mmHg, HBP threshold for hypertension should be 130/80 mmHg. Although a few reports present HBP thresholds in specific patient populations, unless disease could modify the agreement between OBP and HBP, the above recommendation should be consistent between populations with different diseases.
4.2 Strategies for HBP-based management of hypertension
Highlights
• It is mandatory that morning HBP, evening HBP, and the average of both should be below targets in HBP-based management of hypertension.
• Adjustment of anti-hypertensive regimens, dosages, and dosing time should work in concert to control both morning and evening HBP.
4.2.1 Morning vs. evening HBP
Defined as morning HBP ≥ 135/85 mmHg,79 morning hypertension becomes an emerging target for the control of hypertension.80 Activation of the sympathetic nervous system around waking time in the morning, increased dietary salt intake, and inadequate antihypertensive medications are attributable to morning hypertension.79 Given the evidence from cohort studies and clinical trials of telemonitoring-assisted BP control,8,9,42,81 morning BP could be sufficient for management of hypertension, if evening BP is not feasible.5
The Hypertension Objective Treatment Based on Measurement by Electrical Devices of Blood Pressure (HOMED-BP) study randomized 3518 untreated hypertensive patients (HBP of 135-179/85-119 mmHg at baseline) into usual-control group (target HBP of 125-134/80-84 mmHg) and tight-control group (target HBP of < 125/80 mmHg), in which antihypertensive medications were adjusted according to morning HBP estimates.82 The adjustment of antihypertensive dosages and regimens were guided by the pre-specified algorithm. Patients were asked to measure HBP twice every morning, which ought to be taken within 1 hour after waking and 2-minute sitting rest, and before drug and food intake. Morning HBP estimates were the averages of the 5-day morning HBP readings, just preceding each clinic visit at an interval of 2 to 8 weeks. Although the primary endpoint of difference in developing cardiovascular events was neutral between two treatment groups, the authors indicated that, on-treatment morning SBP of < 131.6 mmHg could confer a minimum 5-year cardiovascular risk of ≤ 1%, probably indicating the feasibility of HBP-guided management of hypertension.82
To explore the association between on-treatment morning HBP and incidence of cardiovascular events, the Home Blood Pressure Measurement With Olmesartan Naive Patients to Establish Standard Target Blood Pressure (HONEST) study prospectively followed 21591 hypertensive patients, of whom the mean age was 64.9 years and 50.6% women.8 The participants were asked to measure their HBP at 1 week, 4 weeks, 16 weeks, 6 months, 12 months, 18 months, and 24 months. At each measurement time point, twice morning and twice evening HBP were obtained for 2 days, and the average of morning or evening HBP during follow-up period were used for analysis. The primary endpoint was 2-year incidence of cerebral infarction, intracerebral hemorrhage, subarachnoid hemorrhage, unclassified stroke, myocardial infarction, coronary revascularization procedures for angina pectoris, or sudden death. HONEST study demonstrated that the risk of cardiovascular events was raised with the increasing morning and evening HBP, and would be at a minimum if morning or evening HBP was lower than 124 mmHg.8 The authors also found that, even in patients with systolic OBP of < 130 mmHg, those with morning SBP of ≥ 145 mmHg were at a higher cardiovascular risk with the hazard ratio of 2.47, relative to those with morning SBP of < 125 mmHg. Subsequent analysis also showed that, as compared to OBP, morning HBP appeared to be a stronger predictor for coronary events, but similar for predicting stroke incidence.42
On the other hand, the J-HOP study was aimed at comparing the predictability of morning and evening HBP regarding the stroke or coronary risk.9 A total of 4310 patients with a history of cardiovascular diseases or risk factors, or both were followed for a mean of 4 years. Three morning and three evening HBP were measured for 14 days. Morning HBP was taken within 1 hour of waking and before taking antihypertensive medication, while evening ones were before going to bed. The averages of morning or evening HBP were used for analysis. The results showed that, morning SBP improved traditional risk models for stroke prediction, rather than evening ones; but neither one did for cardiovascular risk prediction.9
All these findings support our recommendations that HBP obtained by the "722" principle could be used to assess cardiovascular risks and guide the initiation and adjustment of antihypertensive medications. According to the HOMED-BP study, it is reasonable to recommend, in well-controlled hypertensive patients, HBP monitoring could be performed, following the 722 principle, at least every 3 months.
4.2.2 HBP-based antihypertensive dosing time
It has been reported that taking morning or evening HBP before drug ingestion could be used to guide the adjustment of antihypertensive medications.83 A study investigated the effect of add-on bedtime-dosing doxazosin in hypertensive patients with morning SBP of > 135 mmHg, who had been on 3-month amlodipine monotherapy.84 The results showed that bedtime doxazosin treatment effectively reduced morning SBP from 145.6 mmHg to 132.4 mmHg (p < 0.01), without significant change of evening BP; but also reduced left ventricular mass index and relative wall thickness.84 The effect of bedtime dosing of doxazosin on morning HBP were also demonstrated in the Japan Monitoring Surge-1 (JMS-1) study.85 In the Hygia Chronotherapy Trial designed to determine whether bedtime dosing, as compared to usual therapy, would reduce cardiovascular risk, 19084 hypertensive patients were enrolled in primary care setting. Patients were assigned to the bedtime-dosing group in which at least one antihypertensive medication was given at bedtime, or to the control group in which all antihypertensive medications were given during daytime. As compared with the control group, bedtime dosing lowered asleep BP, but also the composite risk of cardiovascular death, myocardial infarction, coronary revascularization, heart failure, and stroke by 45% (adjusted hazard ratio, 0.55, 95% CI, 0.50-0.60, p < 0.001) over a median follow-up of 6.3 years.86 Concerns regarding results of the Hygia study have been raised because of the doubtful study design of a randomized control trial, the questionable study protocol, and suspicious 48-hour consecutive ABP monitoring.87
HBP-based hypertension management strategies including bedtime dosing (for uncontrolled morning hypertension), shifting to drugs with longer-acting antihypertensive effect (for uncontrolled evening hypertension), and adding another antihypertensive drug (for uncontrolled morning and evening hypertension) are recommended by the Task Force.
4.3 HBP-derived BP variability (BPV)
Highlights
• Although there are inconsistencies in current definitions and parameters of BPV, the coefficient of variation (CoV) might be used as the home BPV measurement in clinical practice.
• Given that increased home BPV is associated with an increased cardiovascular risk, the reduction in BPV achieved by adjusting drug classes and dosing regimens might be prognostically beneficial.
A physiological BP phenomenon is characterized by continuous dynamic and oscillations occurring over lifetime and is described as the so-called BPV. BPV is considered the result of complex interactions between intrinsic cardiovascular physiologic regulation and extrinsic environmental and behavior factors.43 BPV is classified according to the time span of variations, including very short-term (seconds or minutes, also known as beat-to beat), short-term (within a day, also known as 24-hr), mid-term (between days, also known as day-to-day) and long-term (between clinic visits over months and years, also known as visit-to visit) BPV.88 By this definition, the home BPV was categorized as mid-term BPV. Currently, home BPV can usually be assessed with 4 different indexes: standard deviation (SD), CoV, average real variability (ARV), and variation independent of the mean (VIM).89 CoV (standard deviation/mean × 100%) is commonly recommended as the home BPV measurement because it requires only 3 to 7-day morning BP readings to calculate.90
In the IDHOCO study, individuals with increased HBP-derived CoV of SBP were at increased cardiovascular risk (hazard ratio per 1-SD increase, 1.13; 95% CI, 1.05-1.21) independent of mean systolic HBP level.91 Incorporating home BPV into traditional risk prediction models did not always improve performance of cardiovascular risk prediction. However, in the J-HOP study, 4231 Japanese patients with history of or risk factors for cardiovascular diseases demonstrated that day-by-day home BPV measurements could be used to distinguish high- and low-risk outpatients.92 Based on findings from the J-HOP study, the CoV of SBP of > 6.1% was proposed as the threshold for increased cardiovascular risk especially in Asian people.
Many lines of evidence suggest that increased mid-term (such as day-to-day) BPV is associated with target organ damage and increased cardiovascular events, while evidence on visit-to-visit or seasonal home BPV is limited. Many cohort studies including the Ohasama,93 Finn-Home,90 International Database of Home Blood Pressure in Relation to Cardiovascular Outcome (IDHOCO),91 and meta-analysis94 have provided evidence that increased day-to-day variability in SBP assessed by HBP monitoring is associated with an increased risk of cardiovascular events. Recently, real world HBP variability in over 56,000 individuals with nearly 17 million measurements by wireless BP monitors also suggested the clinical significance of home BPV measurement.95 Although current guidelines do not include the use of BPV as a target in hypertension management, controlling BPV might be considered in addition to lowering mean BP values.43
Dihydropyridine calcium channel blockers (CCB), either used as monotherapy or in combination, have been associated with the most effective reduction in long-term BPV. In the Japan Combined Treatment With Olmesartan and a Calcium-Channel Blocker Versus Olmesartan and Diuretics Randomized Efficacy Study (J-CORE), 207 hypertensive subjects were randomly allocated to an add-on treatment with hydrochlorothiazide or azelnidipine after 12 weeks of olmesartan monotherapy.96 Despite similar reduction in SBP between the two groups, a higher decrease in day-to-day BPV was associated with CCB/olmesartan combination treatment compared with diuretic/olmesartan group. Aside from the use of specific drugs, it seems that short-acting antihypertensive drugs, should be avoided.97 Thus, the choice of long-acting drugs, in particular, dihydropyridine calcium antagonists, and the combination of long-lasting compounds, might be considered in individuals with elevated BPV, although the possible clinical benefits of such strategies have not yet been fully proved.
4.4 Using HBP monitoring to detect hypotensive events during antihypertensive treatment
Highlights
• HBP monitoring is recommended for identifying orthostatic hypotension, postprandial hypotension, and hypotension events during treatment.
Hypertension can be controlled with antihypertensive treatment, but excessive BP reduction may cause harms. The Systolic Blood Pressure Intervention Trial (SPRINT) demonstrated a survival benefit from more aggressive hypertension treatment in patients with high cardiovascular disease risk, but also increased risk of severe hypotension and syncope.98 In a cohort from the Spanish registry of ABP monitoring including 70997 patients with hypertension receiving antihypertensive treatment showed that one in eight treated hypertensive patients are at risk of hypotension according to daytime BP, of whom 68% were not identified to have hypotension by OBP.99 Out of office BP monitoring could better screen the hypotensive events than OBP.
Orthostatic hypotension (OH) is defined as a decrease in SBP of ≥ 20 mmHg or a decrease in diastolic BP of ≥ 10 mmHg within 3 minutes of standing compared with BP from the sitting or supine position.100 OH has been confirmed to be associated with falls, syncope, cardiovascular events and all-cause mortality.101-103 Some patients are unaware of symptoms of OH despite significant falls in BP.104 It has been reported that HBP monitoring was better than OBP in screening OH.105
Postprandial hypotension (PPH) is defined as a fall in SBP of ≥ 20 mmHg within 2 hours after a meal. PPH is associated with increased risk of falls, syncope, stroke, cerebrovascular damage, coronary events and mortality, particularly in the elderly.106,107 Asymptomatic PPH is often under-recognized and neglected. Some studies have demonstrated that HBP monitoring is a suitable screening tool to detect PPH.108,109
5. SOCIETAL AND TECHNOLOGICAL ASPECTS OF HBP MONITORING
Consensus recommendations
#13. HBP monitoring could improve hypertension control, especially when combined with active interventions (such as team-based interventions or telemonitoring).
#14. Implementation of HBP monitoring in clinical practice could be facilitated by increasing awareness of physicians and patients in "SERVE" ways, and insurance reimbursement.
5.1 Team-based approach with support of information technology for hypertension management
Highlights
• Structured, team-based care should be implemented with HBP monitoring, especially in uncontrolled hypertensive patients.
• HBP monitoring integrated to hospital information technology (IT) infrastructure using internet- and smartphone-based strategies, combined with team-based intervention, should be attempted to achieve better hypertension control.
Team-based care is a patient-centered approach, and can be designed as a strategy been implemented at the health system level to improve patient care by having two or more health care providers working collaboratively with each patient. These teams include physicians, nurses, pharmacists, primary care providers, social workers, community health workers and dietitians.2 Team-based approach, unlike uni-level approach, overcomes the barriers of hypertension control with system support and communication between different providers in the team and is more likely to improve BP control.
5.1.1 The combination of team-based approach and HBP monitoring for hypertension management
It has been reported that the combination of HBP monitoring with additional supports might result in even better BP control.110,111 The combination of team-based care and HBP monitoring has been tested in different clinical settings. In the e-BP trial, 778 participants with uncontrolled hypertension were randomly assigned to usual care, HBP monitoring, or HBP monitoring with pharmacist care management.112 At 12 months after intervention, the combination of HBP monitoring with pharmacist care management had significantly higher percentage of patients with controlled BP compared with usual care; while HBP monitoring had only a nonsignificant increase in the percentage of controlled BP as compared to usual care. This study suggests that the pharmacist management significantly improved the BP reduction effect of HBP monitoring. A recent follow-up analysis of e-BP trial also demonstrated a significantly lower BP in intervention group for up to 24 months.113 This result suggests an even longer lasting effect of pharmacist-assisted care model.
Nurses as the additional support to HBP monitoring have also been tested in several studies. A randomized trial has been conducted to evaluate the effect of nurse-led, HBP telemonitoring compared with usual care among urban African American.114 Nurses provided tele-counseling about individual BP goal, lifestyle modification and medication adherence in accordance with guidelines. The intervention group had significantly lower BP compared with usual care group over a 12-month period. In a subsequent randomized trial, 416 African American or Hispanic participants were randomly assigned into the combination of nurse management and HBP monitoring, HBP monitoring, or usual care group.115 At 9 months, the combination of nurse management and HBP monitoring group but not HBP monitoring group resulted in significantly lower SBP compared with usual care group.
Dietitian is also an important part in team-based hypertension management. Dietitian-delivered nutritional counseling improves the adherence and BP control by setting individual goals and creating individual action plans.116 Diet recommendations such as sodium and calories restriction have been shown to be effective in BP control. Studies with meals provided under supervision resulted in even greater reduction in BP.116
5.1.2 How to implement a team-based care for BP control
Guidance for implementing team-based care for hypertension has been proposed.117 Action steps for clinicians to start team-based care with HBP monitoring has also been suggested in the Million Heart project of Centers for Disease Control.118 Briefly, the implementation may involve the following actions: (1) prepare care teams to support HBP monitoring: create a patient-centered care team with multi-disciplinary team members, typically physicians, nurses, pharmacist, and dietitian; provide standardized training for team members to instruct HBP monitoring techniques to patients; (2) incorporate clinical support system for HBP monitoring: design workflows to reflect the new model of care; incorporate health IT into the model, to encourage communication among the team members and patients; establish a feedback loop; (3) empower patients to use HBP monitoring: improve the awareness, willingness and competency of patients to use HBP monitoring with the help of timely and frequent communication between team members and patients.
5.1.3 Integration with IT infrastructures
With the help of health IT, the communications between team members and patients can be immediate and be more effective. HBP records can be transmitted to web-based platform immediately after BP measurement. These records can be relayed to care providers automatically. Care providers can then assess the BP record and electronic health record, interact with patients, and tailor the antihypertensive medications without delay.119 Mobile health interventions such as smartphone applications may support hypertension self-management by improving medication adherence, providing patient-directed feedback, facilitating communication with health care providers, collecting BP data for further analysis, and enhancing self-BP monitor willingness.120 Commercially available smartphone applications were reported to be effective in improving hypertension management if coupled with feedback from clinicians.113,121-123
5.2 Self-monitoring and telemonitoring of HBP
Highlights
• Self-monitoring of BP (SMBP) could confer greater clinical benefit if accompanied by co-interventions, such as self-titration, automatic feedback, education, and counseling.
SMBP refers to the BP measurement by a patient at home or outside a clinical setting. The frequency of monitoring varied widely among studies, ranging from daily, 2 days per week, 3 days per week, weekly, and first week per month.122 A variety of guidelines have recommended SMBP as an adjunct method in the diagnosis of hypertension.4,124 However, despite of these recommendations, it has been controversial whether SMBP alone confers benefit in control of hypertension, and if so, whether the benefits come from additional support to facilitate BP control. Another potential disadvantage of SMBP is the inaccuracy of patient reports and the inability of physician to derive a meaningful conclusion on the basis of handwritten BP logbooks.5
Telemonitoring of BP (TMBP) is meant to be a process of automatic BP transmission from the patient’s home to a remote computer of the telemedicine provider.125 When data are received at the central telemedicine server, they are stored, automatically analyzed, and reports are generated. A medical report will then forward to the patient and the health care provider through a website, e-mail, or dedicated smartphone apps. Several systems are available on the market, which are characterized by different modalities of data collection, transmission, and reporting. TMBP represents an opportunity to improve the accuracy and reliability of HBP reports, to assess the real-time data, and to facilitate the delivery of co-interventions.126
The relevance of co-interventions was demonstrated by the randomized study, Targets and Self-Management for the Control of Blood Pressure in Stroke and at Risk Groups (TASMIN-SR) study, on hypertensive patients at risk of cardiovascular disease.127 In these patients, SMBP combined self-titration of anti-hypertensive medication resulted in lower SBP at 12 months, as compared with usual care (128.2/73.8 vs. 137.8/76.3 mmHg). Furthermore, lowering BP did not increase adverse events. This study also found that the average daily antihypertensive medications of the intervention group was higher than that of the usual care group (3.34 vs. 2.61 pills/day). Therefore, even without tele-monitoring, SMBP with self-titration of anti-hypertensive medication could be effective for better BP control. The more recent randomized trial, Telemonitoring And/or Self-Monitoring of blood pressure IN Hypertension (TASMINH4), assessed the efficacy of self-monitored BP, with or without telemonitoring, for antihypertensive titration in primary care, as compared to usual care.51 The study demonstrated that self-monitoring, either with or without telemonitoring, leads to significantly lower BP than titration guided by clinical settings at one year. Using telemonitoring leads to more rapid lowering of BP after 6 months. This study used the lower home BP target (135/85 mmHg) suggested by guidelines, as opposed to the higher home BP targets (140/90 mmHg) used in previous studies.
In a recent systematic review and individual patient data meta-analysis, Tucker et al. identified 25 trials that compared the effectiveness of SMBP to usual care.122 The intensity of co-interventions was graded and their effectiveness was compared. SMBP was more effective than usual care at lowering BP at 12 months, but this effect was strongly influenced by whether co-interventions were given. There was no difference in BP comparing SMBP alone versus usual care. In contrast, there was a reduction in BP when SMBP was combined with co-interventions (web/phone feedback, education, in-person counseling or telecounseling), with the reduction increasing with the intensity of co-intervention. This meta-analysis suggests that the implementation of SMBP should be accompanied by co-interventions.
5.3 Increase awareness of physicians
Highlights
• Awareness of physicians plays an important role in promoting HBP monitoring to their patients.
• To facilitate memorizing, the Task Force summarized the highlights about how to increase awareness of physicians on HBP monitoring into the acronym " SERVE ":
■ Scientific evidence of HBP monitoring to improve clinical outcomes
■ Educational and training programs for physicians
■ Recommendations of HBP monitoring by clinical guidelines
■ Validated devices in the office and affordable devices in the market
■ Educational and training programs for patients
According to previous studies, the majority of primary care physicians are aware of the importance of HBP monitoring,128-131 and they are willing to encourage and educate their patients to record their HBP. However, many physicians lack sufficient knowledge about the correct use of HBP monitoring recommended by international or local guidelines, such as the normal range of HBP, the use of upper-arm cuff device, or the number of measurements.130 Physicians with younger age,130 female gender,129 who practices in smaller communities,128,129 or who have more patients using HBP monitoring128,129 are more likely to embrace HBP monitoring into their standard care for hypertension. However, there are still some concerns from physicians, which may discourage them from promoting HBP monitoring to their patients. For example, some are concerned about the lack of standard protocol for HBP monitoring, and the lack of training for their patients is another important issue. Other concerns were patients’ excessive preoccupation with BP measurement, or the lack of accurate BP devices.129 Another critical concern is the lack of accessible information of validated devices.129
Steps are suggested to increase the awareness of physicians on the importance of HBP monitoring. First, it is necessary to promote HBP monitoring to physicians in a more aggressive manner. By educational seminars, physicians can be more familiar with the evidence of HBP monitoring. They can learn the recommendations for the applications of HBP monitoring in diagnosis and management of hypertension, such as how to get a reliable HBP reading, the treatment targets in specific groups, or the HBP-based management strategy. The international and local hypertension guidelines should also emphasize the role of HBP monitoring in hypertension management. In addition, it is essential to organize public education programs of HBP monitoring for general population or hypertensive patients by government agencies or academic societies. With a growing access to HBP monitoring in general populations and more experiences with current HBP monitoring devices, physicians will be more motivated to promote HBP monitoring to their patients. Physicians will have more confidence in response to the information obtained from HBP monitoring if there are reliable validated devices in the office to confirm the accuracy of patients’ HBP records. Furthermore, the penetration rate of HBP monitoring would be higher if there are more affordable BP devices in the market, which will also increase physicians’ acceptance to HBP monitoring and subsequently leading to a positive feedback. Finally, more scientific evidence is needed to demonstrate that HBP monitoring indeed improves BP control and outcomes in patients with hypertension. All of these steps can increase the awareness of physicians on the role of HBP monitoring for management of hypertension, thereby encouraging them to promote HBP monitoring to their patients.
5.4 Health policy and reimbursement
Highlights
• Health policy and reimbursement for HBP monitoring would be effective in saving costs and reducing the economic burden of hypertension.
Medical cost of cardiovascular disease is an important social and medical issue in Western as well as in Eastern countries.132,133 Without taking the effects of HBP monitoring on both diagnosis and treatment of hypertension into consideration, prior economic evaluation did not show salient evidence regarding the cost-effectiveness of HBP monitoring. Therefore, reimbursement of HBP monitoring is uncommon. Lack of reimbursement in turn discourages the use of HBP monitoring.
Funahashi et al. constructed a decision tree model using data from the Ohasama study and a Japanese national database. They found introduction of HBP measurement for the diagnosis and treatment of hypertension would be very effective to save costs.134 Most of this was attributable to avoiding the start of treatment for untreated individuals who were diagnosed as hypertensive by OBP but whose BP was in the normal range when based on HBP (i.e. white-coat hypertension).75,134
Lovibond et al. adopted a societal perspective in their comparative economic evaluation of ABP monitoring, HBP monitoring, and OBP measurement in the United Kingdom.135 They found that ABP monitoring is the most cost-effective method for hypertension diagnosis and that HBP monitoring is either indistinguishable from or, in certain scenarios among the youngest population, superior to OBP measurement. However, differences in the benefits in treatment of hypertension during patient follow-up were not investigated among these three BP measurement modalities. Another study from insurer perspective evaluated the cost-effectiveness of HBP monitoring in hypertension diagnosis and treatment in the United States. The results indicated that HBP monitoring was generally more cost beneficial when it was used to diagnose hypertension in younger individuals and to monitor hypertension treatment in older individuals.136
Numerous studies have shown the value of HBP monitoring in self-monitoring and hypertension control, as well as antihypertensive drug adherence especially when paired with communication strategies, such as telemonitoring.137,138 There was a systematic review evaluating the economic benefits of SMBP interventions to control hypertension.139 Three types of interventions were evaluated: SMBP used alone, SMBP with additional support, and SMBP within team-based care. The result showed SMBP with additional support or team-based care are cost effective, rather than SMBP alone. Similar findings were found in a meta-analysis showing that SMBP combined with additional support was preferred than usual care with regard to cost-effectiveness analysis.123
6. CONCLUSIONS: INTEGRATING HBP MONITORING IN THE DIAGNOSIS AND MANAGEMENT OF HYPERTENSION
In the recent international guidelines for management of arterial hypertension, HBP monitoring has been integrated into the assessment sets for the identification of hypertension phenotypes, including white-coat hypertension, masked hypertension, and morning or evening hypertension.1,4,140 A good reproducibility of HBP monitoring could be achieved if individuals carefully follow the instructions before and during HBP measurement, by using validated BP devices. It is feasible to use HBP to initiate and adjust antihypertensive medications to achieve both morning and evening HBP targets, as well as to avoid hypotensive events.
In two recent BP screening campaigns conducted in community pharmacies in Taiwan, about one third of hypertensive patients receiving antihypertensive medications were uncontrolled with screening BP of ≥ 140/90 mmHg.141-143 With the support from medical caregivers, paramedical team, or telemonitoring, HBP monitoring could improve the control of hypertension. In this Consensus Statement on HBP monitoring, we present evidence regarding the role of HBP monitoring, and propose the algorithms integrating HBP, OBP, and ABP in the diagnosis and management of hypertension (Figures 1 and 2). Moreover, the improvement in hypertension control could be expected by raising the awareness of physicians and patients on the clinical significance and benefit of HBP monitoring, and facilitating the establishment of health policy and insurance imbursement for widespread application of HBP monitoring in healthcare system.
Acknowledgments
None.
CONFLICT OF INTEREST
Hung-Ju Lin has been on the speakers bureau for AstraZeneca, China Chemical & Pharmaceutical Co., Ltd., Daiichi-Sankyo, Menarini, Novartis, Pfizer, and Takeda. Tzung-Dau Wang has been on the speakers bureau for AstraZeneca, Boehringer Ingelheim, Daiichi-Sankyo, Medtronic, Novartis, Pfizer, Sanofi, and Takeda and has received research grants from Omron. Hao-Min Cheng has been on the speakers bureau for Eli Lilly and AstraZeneca; Pfizer Inc.; Bayer AG; Boehringer Ingelheim Pharmaceuticals, Inc.; Daiichi Sankyo, Novartis Pharmaceuticals, Inc.; SERVIER; Co., Pharmaceuticals Corporation; Sanofi; TAKEDA Pharmaceuticals International and served as an advisor or consultant for ApoDx Technology, Inc. All other authors report no potential conflicts of interest in relation to this article.
REFERENCES
- 1.Umemura S, Arima H, Arima S, et al. The Japanese Society of Hypertension guidelines for the management of hypertension (JSH 2019). Hypertens Res. 2019;42:1235–1481. doi: 10.1038/s41440-019-0284-9. [DOI] [PubMed] [Google Scholar]
- 2.Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:1269–1324. doi: 10.1161/HYP.0000000000000066. [DOI] [PubMed] [Google Scholar]
- 3.Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J. 2018;39:3021–3104. doi: 10.1093/eurheartj/ehy339. [DOI] [PubMed] [Google Scholar]
- 4.Chiang CE, Wang TD, Ueng KC, et al. 2015 guidelines of the Taiwan Society of Cardiology and the Taiwan Hypertension Society for the management of hypertension. J Chin Med Assoc. 2015;78:1–47. doi: 10.1016/j.jcma.2014.11.005. [DOI] [PubMed] [Google Scholar]
- 5.Park S, Buranakitjaroen P, Chen CH, et al. Expert panel consensus recommendations for home blood pressure monitoring in Asia: the Hope Asia Network. J Hum Hypertens. 2018;32:249–258. doi: 10.1038/s41371-017-0025-y. [DOI] [PubMed] [Google Scholar]
- 6.Sega R, Facchetti R, Bombelli M, et al. Prognostic value of ambulatory and home blood pressures compared with office blood pressure in the general population: follow-up results from the Pressioni Arteriose Monitorate e Loro Associazioni (PAMELA) study. Circulation. 2005;111:1777–1783. doi: 10.1161/01.CIR.0000160923.04524.5B. [DOI] [PubMed] [Google Scholar]
- 7.Ohkubo T, Imai Y, Tsuji I, et al. Home blood pressure measurement has a stronger predictive power for mortality than does screening blood pressure measurement: a population-based observation in Ohasama, Japan. J Hypertens. 1998;16:971–975. doi: 10.1097/00004872-199816070-00010. [DOI] [PubMed] [Google Scholar]
- 8.Kario K, Saito I, Kushiro T, et al. Home blood pressure and cardiovascular outcomes in patients during antihypertensive therapy: primary results of HONEST, a large-scale prospective, real-world observational study. Hypertension. 2014;64:989–996. doi: 10.1161/HYPERTENSIONAHA.114.04262. [DOI] [PubMed] [Google Scholar]
- 9.Hoshide S, Yano Y, Haimoto H, et al. Morning and evening home blood pressure and risks of incident stroke and coronary artery disease in the Japanese general practice population: The Japan Morning Surge-Home Blood Pressure Study. Hypertension. 2016;68:54–61. doi: 10.1161/HYPERTENSIONAHA.116.07201. [DOI] [PubMed] [Google Scholar]
- 10.Ntineri A, Kalogeropoulos PG, Kyriakoulis KG, et al. Prognostic value of average home blood pressure and variability: 19-year follow-up of the Didima study. J Hypertens. 2018;36:69–76. doi: 10.1097/HJH.0000000000001497. [DOI] [PubMed] [Google Scholar]
- 11.Kario K, Shimbo D, Hoshide S, et al. Emergence of home blood pressure-guided management of hypertension based on global evidence. Hypertension. 2019;74:Hypertensionaha11912630. doi: 10.1161/HYPERTENSIONAHA.119.12630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fagard RH, Van Den Broeke C, De Cort P. Prognostic significance of blood pressure measured in the office, at home and during ambulatory monitoring in older patients in general practice. J Hum Hypertens. 2005;19:801–807. doi: 10.1038/sj.jhh.1001903. [DOI] [PubMed] [Google Scholar]
- 13.Muntner P, Shimbo D, Carey RM, et al. Measurement of blood pressure in humans: a scientific statement from the American Heart Association. Hypertension. 2019;73:e35–e66. doi: 10.1161/HYP.0000000000000087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bobrie G, Chatellier G, Genes N, et al. Cardiovascular prognosis of "masked hypertension" detected by blood pressure self-measurement in elderly treated hypertensive patients. JAMA. 2004;291:1342–1349. doi: 10.1001/jama.291.11.1342. [DOI] [PubMed] [Google Scholar]
- 15.Tanabe A, Asayama K, Hanazawa T, et al. Left ventricular hypertrophy by electrocardiogram as a predictor of success in home blood pressure control: HOMED-BP study. Hypertens Res. 2017;40:504–510. doi: 10.1038/hr.2016.176. [DOI] [PubMed] [Google Scholar]
- 16.Kleinert HD, Harshfield GA, Pickering TG, et al. What is the value of home blood pressure measurement in patients with mild hypertension? Hypertension. 1984;6:574–578. doi: 10.1161/01.hyp.6.4.574. [DOI] [PubMed] [Google Scholar]
- 17.Shibamiya T, Obara T, Ohkubo T, et al. Electrocardiographic abnormalities and home blood pressure in treated elderly hypertensive patients: Japan home versus office blood pressure measurement evaluation in the elderly (J-HOME-Elderly) study. Hypertens Res. 2010;33:670–677. doi: 10.1038/hr.2010.55. [DOI] [PubMed] [Google Scholar]
- 18.Shimbo D, Pickering TG, Spruill TM, et al. Relative utility of home, ambulatory, and office blood pressures in the prediction of end-organ damage. Am J Hypertens. 2007;20:476–482. doi: 10.1016/j.amjhyper.2006.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mulè G, Caimi G, Cottone S, et al. Value of home blood pressures as predictor of target organ damage in mild arterial hypertension. J Cardiovasc Risk. 2002;9:123–129. doi: 10.1177/174182670200900208. [DOI] [PubMed] [Google Scholar]
- 20.Niiranen T, Jula A, Kantola I, et al. Home-measured blood pressure is more strongly associated with atherosclerosis than clinic blood pressure: the Finn-HOME Study. J Hypertens. 2007;25:1225–1231. doi: 10.1097/HJH.0b013e3280d94336. [DOI] [PubMed] [Google Scholar]
- 21.Stergiou GS, Argyraki KK, Moyssakis I, et al. Home blood pressure is as reliable as ambulatory blood pressure in predicting target-organ damage in hypertension. Am J Hypertens. 2007;20:616–621. doi: 10.1016/j.amjhyper.2006.12.013. [DOI] [PubMed] [Google Scholar]
- 22.Tseng CC, Wolff LF. Inhibitory effect of stannous fluoride and other commonly used antimicrobial agents on oral bacteria. J Formos Med Assoc. 1991;90:565–571. [PubMed] [Google Scholar]
- 23.Asayama K, Ohkubo T, Kikuya M, et al. Prediction of stroke by self-measurement of blood pressure at home versus casual screening blood pressure measurement in relation to the Joint National Committee 7 classification: the Ohasama study. Stroke. 2004;35:2356–2361. doi: 10.1161/01.STR.0000141679.42349.9f. [DOI] [PubMed] [Google Scholar]
- 24.Niiranen TJ, Hanninen MR, Johansson J, et al. Home-measured blood pressure is a stronger predictor of cardiovascular risk than office blood pressure: the Finn-Home study. Hypertension. 2010;55:1346–1351. doi: 10.1161/HYPERTENSIONAHA.109.149336. [DOI] [PubMed] [Google Scholar]
- 25.Kario K, Thijs L, Staessen JA. Blood pressure measurement and treatment decisions. Circ Res. 2019;124:990–1008. doi: 10.1161/CIRCRESAHA.118.313219. [DOI] [PubMed] [Google Scholar]
- 26.Stergiou GS, Asayama K, Thijs L, et al. Prognosis of white-coat and masked hypertension: international database of HOme blood pressure in relation to cardiovascular outcome. Hypertension. 2014;63:675–682. doi: 10.1161/HYPERTENSIONAHA.113.02741. [DOI] [PubMed] [Google Scholar]
- 27.Tientcheu D, Ayers C, Das SR, et al. Target organ complications and cardiovascular events associated with masked hypertension and white-coat hypertension: analysis from the Dallas Heart Study. J Am Coll Cardiol. 2015;66:2159–2169. doi: 10.1016/j.jacc.2015.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mancia G, Facchetti R, Grassi G, Bombelli M. Adverse prognostic value of persistent office blood pressure elevation in white coat hypertension. Hypertension. 2015;66:437–444. doi: 10.1161/HYPERTENSIONAHA.115.05367. [DOI] [PubMed] [Google Scholar]
- 29.Stergiou GS, Baibas NM, Gantzarou AP, et al. Reproducibility of home, ambulatory, and clinic blood pressure: implications for the design of trials for the assessment of antihypertensive drug efficacy. Am J Hypertens. 2002;15:101–104. doi: 10.1016/s0895-7061(01)02324-x. [DOI] [PubMed] [Google Scholar]
- 30.Eguchi K, Hoshide S, Schwartz JE, et al. Visit-to-visit and ambulatory blood pressure variability as predictors of incident cardiovascular events in patients with hypertension. Am J Hypertens. 2012;25:962–968. doi: 10.1038/ajh.2012.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kawai T, Ohishi M, Kamide K, et al. The impact of visit-to-visit variability in blood pressure on renal function. Hypertens Res. 2012;35:239–243. doi: 10.1038/hr.2011.170. [DOI] [PubMed] [Google Scholar]
- 32.Bliziotis IA, Destounis A, Stergiou GS. Home versus ambulatory and office blood pressure in predicting target organ damage in hypertension: a systematic review and meta-analysis. J Hypertens. 2012;30:1289–1299. doi: 10.1097/HJH.0b013e3283531eaf. [DOI] [PubMed] [Google Scholar]
- 33.Gaborieau V, Delarche N, Gosse P. Ambulatory blood pressure monitoring versus self-measurement of blood pressure at home: correlation with target organ damage. J Hypertens. 2008;26:1919–1927. doi: 10.1097/HJH.0b013e32830c4368. [DOI] [PubMed] [Google Scholar]
- 34.Niiranen TJ, Mäki J, Puukka P, et al. Office, home, and ambulatory blood pressures as predictors of cardiovascular risk. Hypertension. 2014;64:281–286. doi: 10.1161/HYPERTENSIONAHA.114.03292. [DOI] [PubMed] [Google Scholar]
- 35.Asayama K, Fujiwara T, Hoshide S, et al. Nocturnal blood pressure measured by home devices: evidence and perspective for clinical application. J Hypertens. 2019;37:905–916. doi: 10.1097/HJH.0000000000001987. [DOI] [PubMed] [Google Scholar]
- 36.Kollias A, Ntineri A, Stergiou GS. Association of night-time home blood pressure with night-time ambulatory blood pressure and target-organ damage: a systematic review and meta-analysis. J Hypertens. 2017;35:442–452. doi: 10.1097/HJH.0000000000001189. [DOI] [PubMed] [Google Scholar]
- 37.Kario K, Kanegae H, Tomitani N, et al. Nighttime blood pressure measured by home blood pressure monitoring as an independent predictor of cardiovascular events in general practice. Hypertension. 2019;73:1240–1248. doi: 10.1161/HYPERTENSIONAHA.118.12740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ntineri A, Stergiou GS, Thijs L, et al. Relationship between office and home blood pressure with increasing age: The International Database of HOme blood pressure in relation to Cardiovascular Outcome (IDHOCO). Hypertens Res. 2016;39:612–617. doi: 10.1038/hr.2016.32. [DOI] [PubMed] [Google Scholar]
- 39.Pappaccogli M, Di Monaco S, Perlo E, et al. Comparison of automated office blood pressure with office and out-off-office measurement techniques. Hypertension. 2019;73:481–490. doi: 10.1161/HYPERTENSIONAHA.118.12079. [DOI] [PubMed] [Google Scholar]
- 40.Stergiou GS, Tzamouranis D, Nasothimiou EG, et al. Are there really differences between home and daytime ambulatory blood pressure? Comparison using a novel dual-mode ambulatory and home monitor. Journal of Human Hypertension. 2010;24:207–212. doi: 10.1038/jhh.2009.60. [DOI] [PubMed] [Google Scholar]
- 41.Nasothimiou EG, Karpettas N, Dafni MG, Stergiou GS. Patients’ preference for ambulatory versus home blood pressure monitoring. Journal of Human Hypertension. 2014;28:224–229. doi: 10.1038/jhh.2013.104. [DOI] [PubMed] [Google Scholar]
- 42.Kario K, Saito I, Kushiro T, et al. Morning home blood pressure is a strong predictor of coronary artery disease: The HONEST Study. J Am Coll Cardiol. 2016;67:1519–1527. doi: 10.1016/j.jacc.2016.01.037. [DOI] [PubMed] [Google Scholar]
- 43.Sogunuru GP, Kario K, Shin J, et al. Morning surge in blood pressure and blood pressure variability in Asia: evidence and statement from the HOPE Asia Network. J Clin Hypertens (Greenwich) 2019;21:324–334. doi: 10.1111/jch.13451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Stergiou GS, Alpert B, Mieke S, et al. A universal standard for the validation of blood pressure measuring devices: association for the Advancement of Medical Instrumentation/European Society of Hypertension/International Organization for Standardization (AAMI/ESH/ISO) collaboration statement. Hypertension. 2018;71:368–374. doi: 10.1161/HYPERTENSIONAHA.117.10237. [DOI] [PubMed] [Google Scholar]
- 45.Turner MJ, Speechly C, Bignell N. Sphygmomanometer calibration--why, how and how often? Aust Fam Physician. 2007;36:834–838. [PubMed] [Google Scholar]
- 46.Kuwabara M, Harada K, Hishiki Y, Kario K. Validation of two watch-type wearable blood pressure monitors according to the ANSI/AAMI/ISO81060-2: 2013 guidelines: Omron HEM-6410T-ZM and HEM-6410T-ZL. J Clin Hypertens (Greenwich) 2019;21:853–858. doi: 10.1111/jch.13499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Islam SMS, Cartledge S, Karmakar C, et al. Validation and acceptability of a cuffless wrist-worn wearable blood pressure monitoring device among users and health care professionals: mixed methods study. JMIR Mhealth Uhealth. 2019;7:e14706. doi: 10.2196/14706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kario K, Shimbo D, Tomitani N, et al. The first study comparing a wearable watch-type blood pressure monitor with a conventional ambulatory blood pressure monitor on in-office and out-of-office settings. J Clin Hypertens (Greenwich) 2020;22:135–141. doi: 10.1111/jch.13799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Unger T, Borghi C, Charchar F, et al. 2020 International Society of Hypertension Global Hypertension Practice Guidelines. Hypertension. 2020;75:1334–1357. doi: 10.1161/HYPERTENSIONAHA.120.15026. [DOI] [PubMed] [Google Scholar]
- 50.Pickering TG, Miller NH, Ogedegbe G, et al. Call to action on use and reimbursement for home blood pressure monitoring: executive summary. Hypertension. 2008;52:1–9. doi: 10.1161/HYPERTENSIONAHA.107.189011. [DOI] [PubMed] [Google Scholar]
- 51.McManus RJ, Mant J, Franssen M, et al. Efficacy of self-monitored blood pressure, with or without telemonitoring, for titration of antihypertensive medication (TASMINH4): an unmasked randomised controlled trial. Lancet. 2018;391:949–959. doi: 10.1016/S0140-6736(18)30309-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Okumiya K, Matsubayashi K, Wada T, et al. A U-shaped association between home systolic blood pressure and four-year mortality in community-dwelling older men. J Am Geriatr Soc. 1999;47:1415–1421. doi: 10.1111/j.1532-5415.1999.tb01559.x. [DOI] [PubMed] [Google Scholar]
- 53.Stergiou GS, Baibas NM, Kalogeropoulos PG. Cardiovascular risk prediction based on home blood pressure measurement: the Didima study. J Hypertens. 2007;25:1590–1596. doi: 10.1097/HJH.0b013e3281ab6c69. [DOI] [PubMed] [Google Scholar]
- 54.Niiranen TJ, Maki J, Puukka P, et al. Office, home, and ambulatory blood pressures as predictors of cardiovascular risk. Hypertension. 2014;64:281–286. doi: 10.1161/HYPERTENSIONAHA.114.03292. [DOI] [PubMed] [Google Scholar]
- 55.Ohkubo T, Asayama K, Kikuya M, et al. How many times should blood pressure be measured at home for better prediction of stroke risk? Ten-year follow-up results from the Ohasama study. J Hypertens. 2004;22:1099–1104. doi: 10.1097/00004872-200406000-00009. [DOI] [PubMed] [Google Scholar]
- 56.Staessen JA, Den Hond E, Celis H, et al. Antihypertensive treatment based on blood pressure measurement at home or in the physician’s office: a randomized controlled trial. JAMA. 2004;291:955–964. doi: 10.1001/jama.291.8.955. [DOI] [PubMed] [Google Scholar]
- 57.Juhanoja EP, Johansson JK, Puukka PJ, et al. Optimal schedule for assessing home BP variability: The Finn-Home Study. Am J Hypertens. 2018;31:715–725. doi: 10.1093/ajh/hpy030. [DOI] [PubMed] [Google Scholar]
- 58.Bello NA, Schwartz JE, Kronish IM, et al. Number of measurements needed to obtain a reliable estimate of home blood pressure: results from the improving the detection of hypertension study. J Am Heart Assoc. 2018;7:e008658. doi: 10.1161/JAHA.118.008658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Powers BJ, Olsen MK, Smith VA, et al. Measuring blood pressure for decision making and quality reporting: where and how many measures? Ann Intern Med. 2011;154:781–788, w-289-790. doi: 10.7326/0003-4819-154-12-201106210-00005. [DOI] [PubMed] [Google Scholar]
- 60.Niiranen TJ, Asayama K, Thijs L, et al. Optimal number of days for home blood pressure measurement. Am J Hypertens. 2015;28:595–603. doi: 10.1093/ajh/hpu216. [DOI] [PubMed] [Google Scholar]
- 61.Asayama K, Ohkubo T, Metoki H, et al. Cardiovascular outcomes in the first trial of antihypertensive therapy guided by self-measured home blood pressure. Hypertens Res. 2012;35:1102–1110. doi: 10.1038/hr.2012.125. [DOI] [PubMed] [Google Scholar]
- 62.Chiang CE, Wu TJ, Ueng KC, et al. 2016 guidelines of the Taiwan Heart Rhythm Society and the Taiwan Society of Cardiology for the management of atrial fibrillation. J Formos Med Assoc. 2016;115:893–952. doi: 10.1016/j.jfma.2016.10.005. [DOI] [PubMed] [Google Scholar]
- 63.Alpert BS, Quinn D, Gallick D. Oscillometric blood pressure: a review for clinicians. J Am Soc Hypertens. 2014;8:930–938. doi: 10.1016/j.jash.2014.08.014. [DOI] [PubMed] [Google Scholar]
- 64.Kollias A, Stergiou GS. Automated measurement of office, home and ambulatory blood pressure in atrial fibrillation. Clin Exp Pharmacol Physiol. 2014;41:9–15. doi: 10.1111/1440-1681.12103. [DOI] [PubMed] [Google Scholar]
- 65.Halfon M, Wuerzner G, Marques-Vidal P, et al. Use of oscillometric devices in atrial fibrillation: a comparison of three devices and invasive blood pressure measurement. Blood Press. 2018;27:48–55. doi: 10.1080/08037051.2017.1383852. [DOI] [PubMed] [Google Scholar]
- 66.Stergiou GS, Kollias A, Destounis A, Tzamouranis D. Automated blood pressure measurement in atrial fibrillation: a systematic review and meta-analysis. J Hypertens. 2012;30:2074–2082. doi: 10.1097/HJH.0b013e32835850d7. [DOI] [PubMed] [Google Scholar]
- 67.Clark CE, McDonagh STJ, McManus RJ. Accuracy of automated blood pressure measurements in the presence of atrial fibrillation: systematic review and meta-analysis. J Hum Hypertens. 2019;33:352–364. doi: 10.1038/s41371-018-0153-z. [DOI] [PubMed] [Google Scholar]
- 68.Clark CE, McDonagh STJ, McManus RJ Blood Pressure Measurement Working Party of the B; Irish Hypertension S. Measurement of blood pressure in people with atrial fibrillation. J Hum Hypertens. 2019;33:763–765. doi: 10.1038/s41371-019-0261-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ravindrarajah R, Hazra NC, Hamada S, et al. Systolic blood pressure trajectory, frailty, and all-cause mortality > 80 years of age: cohort study using electronic health records. Circulation. 2017;135:2357–2368. doi: 10.1161/CIRCULATIONAHA.116.026687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Huang CJ, Chiang CE, Williams B, et al. Effect modification by age on the benefit or harm of antihypertensive treatment for elderly hypertensives: a systematic review and meta-analysis. Am J Hypertens. 2019;32:163–174. doi: 10.1093/ajh/hpy169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. J Am Coll Cardiol. 2018;71:2199–2269. [Google Scholar]
- 72.Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J. 2018;39:3021–3104. doi: 10.1093/eurheartj/ehy339. [DOI] [PubMed] [Google Scholar]
- 73.Chiang CE, Wang TD, Lin TH, et al. The 2017 focused update of the guidelines of the Taiwan Society of Cardiology (TSOC) and the Taiwan Hypertension Society (THS) for the management of hypertension. Acta Cardiol Sin. 2017;33:213–225. doi: 10.6515/ACS20170421A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Lee HY, Shin J, Kim GH, et al. 2018 Korean Society of Hypertension guidelines for the management of hypertension: part II-diagnosis and treatment of hypertension. Clin Hypertens. 2019;25:20. doi: 10.1186/s40885-019-0124-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Fukunaga H, Ohkubo T, Kobayashi M, et al. Cost-effectiveness of the introduction of home blood pressure measurement in patients with office hypertension. J Hypertens. 2008;26:685–690. doi: 10.1097/HJH.0b013e3282f42285. [DOI] [PubMed] [Google Scholar]
- 76.Ragot S, Genès N, Vaur L, Herpin D. Comparison of three blood pressure measurement methods for the evaluation of two antihypertensive drugs: feasibility, agreement, and reproducibility of blood pressure response. Am J Hypertens. 2000;13:632–639. doi: 10.1016/s0895-7061(99)00258-7. [DOI] [PubMed] [Google Scholar]
- 77.Cheng HM, Chuang SY, Sung SH, et al. Derivation and validation of diagnostic thresholds for central blood pressure measurements based on long-term cardiovascular risks. J Am Coll Cardiol. 2013;62:1780–1787. doi: 10.1016/j.jacc.2013.06.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Niiranen TJ, Asayama K, Thijs L, et al. Outcome-driven thresholds for home blood pressure measurement: international database of home blood pressure in relation to cardiovascular outcome. Hypertension. 2013;61:27–34. doi: 10.1161/HYPERTENSIONAHA.111.00100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Wang JG, Kario K, Chen CH, et al. Management of morning hypertension: a consensus statement of an Asian expert panel. The Journal of Clinical Hypertension. 2018;20:39–44. doi: 10.1111/jch.13140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Kario K, Shimbo D, Hoshide S, et al. Emergence of home blood pressure-guided management of hypertension based on global evidence. Hypertension. 2019;74:229–236. doi: 10.1161/HYPERTENSIONAHA.119.12630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.McManus RJ, Mant J, Bray EP, et al. Telemonitoring and self-management in the control of hypertension (TASMINH2): a randomised controlled trial. Lancet. 2010;376:163–172. doi: 10.1016/S0140-6736(10)60964-6. [DOI] [PubMed] [Google Scholar]
- 82.Asayama K, Ohkubo T, Metoki H, et al. Cardiovascular outcomes in the first trial of antihypertensive therapy guided by self-measured home blood pressure. Hypertens Res. 2012;35:1102–1110. doi: 10.1038/hr.2012.125. [DOI] [PubMed] [Google Scholar]
- 83.Ménard J, Chatellier G, Day M, Vaur L. Self-measurement of blood pressure at home to evaluate drug effects by the trough: peak ratio. J Hypertens Suppl. 1994;12:S21–S25. [PubMed] [Google Scholar]
- 84.Ikeda T, Gomi T, Shibuya Y, et al. Add-on effect of bedtime dosing of the alpha(1)-adrenergic receptor antagonist doxazosin on morning hypertension and left ventricular hypertrophy in patients undergoing long-term amlodipine monotherapy. Hypertens Res. 2007;30:1097–1105. doi: 10.1291/hypres.30.1097. [DOI] [PubMed] [Google Scholar]
- 85.Kario K, Matsui Y, Shibasaki S, et al. An alpha-adrenergic blocker titrated by self-measured blood pressure recordings lowered blood pressure and microalbuminuria in patients with morning hypertension: the Japan Morning Surge-1 Study. J Hypertens. 2008;26:1257–1265. doi: 10.1097/HJH.0b013e3282fd173c. [DOI] [PubMed] [Google Scholar]
- 86.Hermida RC, Crespo JJ, Domínguez-Sardiña M, et al. Bedtime hypertension treatment improves cardiovascular risk reduction: the Hygia Chronotherapy Trial. Eur Heart J. 2019:ehz754. doi: 10.1093/eurheartj/ehz754. [DOI] [PubMed] [Google Scholar]
- 87.Kreutz R, Kjeldsen SE, Burnier M, et al. Blood pressure medication should not be routinely dosed at bedtime. We must disregard the data from the HYGIA project. Blood Press. 2020;29:135–136. doi: 10.1080/08037051.2020.1747696. [DOI] [PubMed] [Google Scholar]
- 88.Parati G, Ochoa JE, Lombardi C, Bilo G. Assessment and management of blood-pressure variability. Nat Rev Cardiol. 2013;10:143–155. doi: 10.1038/nrcardio.2013.1. [DOI] [PubMed] [Google Scholar]
- 89.Kario K, Park S, Chia YC, et al. 2020 consensus summary on the management of hypertension in Asia from the HOPE Asia Network. J Clin Hypertens (Greenwich) 2020;22:351–362. doi: 10.1111/jch.13751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Johansson JK, Niiranen TJ, Puukka PJ, Jula AM. Prognostic value of the variability in home-measured blood pressure and heart rate: the Finn-Home Study. Hypertension. 2012;59:212–218. doi: 10.1161/HYPERTENSIONAHA.111.178657. [DOI] [PubMed] [Google Scholar]
- 91.Juhanoja EP, Niiranen TJ, Johansson JK, et al. Outcome-driven thresholds for increased home blood pressure variability. Hypertension. 2017;69:599–607. doi: 10.1161/HYPERTENSIONAHA.116.08603. [DOI] [PubMed] [Google Scholar]
- 92.Hoshide S, Yano Y, Mizuno H, et al. Day-by-day variability of home blood pressure and incident cardiovascular disease in clinical practice: The J-HOP Study (Japan Morning Surge-Home Blood Pressure). Hypertension. 2018;71:177–184. doi: 10.1161/HYPERTENSIONAHA.117.10385. [DOI] [PubMed] [Google Scholar]
- 93.Kikuya M, Ohkubo T, Metoki H, et al. Day-by-day variability of blood pressure and heart rate at home as a novel predictor of prognosis: the Ohasama study. Hypertension. 2008;52:1045–1050. doi: 10.1161/HYPERTENSIONAHA.107.104620. [DOI] [PubMed] [Google Scholar]
- 94.Stevens SL, Wood S, Koshiaris C, et al. Blood pressure variability and cardiovascular disease: systematic review and meta-analysis. BMJ. 2016;354:i4098. doi: 10.1136/bmj.i4098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Kim KI, Nikzad N, Quer G, et al. Real world home blood pressure variability in over 56,000 individuals with nearly 17 million measurements. Am J Hypertens. 2018;31:566–573. doi: 10.1093/ajh/hpx221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Matsui Y, O'Rourke MF, Hoshide S, et al. Combined effect of angiotensin II receptor blocker and either a calcium channel blocker or diuretic on day-by-day variability of home blood pressure: the Japan Combined Treatment With Olmesartan and a Calcium-Channel Blocker Versus Olmesartan and Diuretics Randomized Efficacy Study. Hypertension. 2012;59:1132–1138. doi: 10.1161/HYPERTENSIONAHA.111.189217. [DOI] [PubMed] [Google Scholar]
- 97.Parati G, Schumacher H, Bilo G, Mancia G. Evaluating 24-h antihypertensive efficacy by the smoothness index: a meta-analysis of an ambulatory blood pressure monitoring database. J Hypertens. 2010;28:2177–2183. doi: 10.1097/HJH.0b013e32833e1150. [DOI] [PubMed] [Google Scholar]
- 98.Group SR, Wright JT, Jr., Williamson JD, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373:2103–2116. doi: 10.1056/NEJMoa1511939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Divison-Garrote JA, Banegas JR, De la Cruz JJ, et al. Hypotension based on office and ambulatory monitoring blood pressure. Prevalence and clinical profile among a cohort of 70,997 treated hypertensives. J Am Soc Hypertens. 2016;10:714–723. doi: 10.1016/j.jash.2016.06.035. [DOI] [PubMed] [Google Scholar]
- 100.Freeman R, Wieling W, Axelrod FB, et al. Consensus statement on the definition of orthostatic hypotension, neurally mediated syncope and the postural tachycardia syndrome. Auton Neurosci. 2011;161:46–48. doi: 10.1016/j.autneu.2011.02.004. [DOI] [PubMed] [Google Scholar]
- 101.Juraschek SP, Daya N, Rawlings AM, et al. Association of history of dizziness and long-term adverse outcomes with early vs later orthostatic hypotension assessment times in middle-aged adults. JAMA Intern Med. 2017;177:1316–1323. doi: 10.1001/jamainternmed.2017.2937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Juraschek SP, Daya N, Appel LJ, et al. Orthostatic hypotension and risk of clinical and subclinical cardiovascular disease in middle-aged adults. J Am Heart Assoc. 2018;7:e008884. doi: 10.1161/JAHA.118.008884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Ricci F, Fedorowski A, Radico F, et al. Cardiovascular morbidity and mortality related to orthostatic hypotension: a meta-analysis of prospective observational studies. Eur Heart J. 2015;36:1609–1617. doi: 10.1093/eurheartj/ehv093. [DOI] [PubMed] [Google Scholar]
- 104.Freeman R, Illigens BMW, Lapusca R, et al. Symptom recognition is impaired in patients with orthostatic hypotension. Hypertension. 2020;75:1325–1332. doi: 10.1161/HYPERTENSIONAHA.119.13619. [DOI] [PubMed] [Google Scholar]
- 105.Cremer A, Rousseau AL, Boulestreau R, et al. Screening for orthostatic hypotension using home blood pressure measurements. J Hypertens. 2019;37:923–927. doi: 10.1097/HJH.0000000000001986. [DOI] [PubMed] [Google Scholar]
- 106.Aronow WS, Ahn C. Association of postprandial hypotension with incidence of falls, syncope, coronary events, stroke, and total mortality at 29-month follow-up in 499 older nursing home residents. J Am Geriatr Soc. 1997;45:1051–1053. doi: 10.1111/j.1532-5415.1997.tb05965.x. [DOI] [PubMed] [Google Scholar]
- 107.Kohara K, Jiang Y, Igase M, et al. Postprandial hypotension is associated with asymptomatic cerebrovascular damage in essential hypertensive patients. Hypertension. 1999;33:565–568. doi: 10.1161/01.hyp.33.1.565. [DOI] [PubMed] [Google Scholar]
- 108.Barochiner J, Alfie J, Aparicio LS, et al. Postprandial hypotension detected through home blood pressure monitoring: a frequent phenomenon in elderly hypertensive patients. Hypertens Res. 2014;37:438–443. doi: 10.1038/hr.2013.144. [DOI] [PubMed] [Google Scholar]
- 109.Alfie J. Utility of home blood pressure monitoring to evaluate postprandial blood pressure in treated hypertensive patients. Ther Adv Cardiovasc Dis. 2015;9:133–139. doi: 10.1177/1753944715593444. [DOI] [PubMed] [Google Scholar]
- 110.Agarwal R, Bills JE, Hecht TJ, Light RP. Role of home blood pressure monitoring in overcoming therapeutic inertia and improving hypertension control: a systematic review and meta-analysis. Hypertension. 2011;57:29–38. doi: 10.1161/HYPERTENSIONAHA.110.160911. [DOI] [PubMed] [Google Scholar]
- 111.Lauffenburger JC, Shrank WH, Bitton A, et al. Association between patient-centered medical homes and adherence to chronic disease medications: a Cohort Study. Ann Intern Med. 2017;166:81–88. doi: 10.7326/M15-2659. [DOI] [PubMed] [Google Scholar]
- 112.Green BB, Cook AJ, Ralston JD, et al. Effectiveness of home blood pressure monitoring, Web communication, and pharmacist care on hypertension control: a randomized controlled trial. JAMA. 2008;299:2857–2867. doi: 10.1001/jama.299.24.2857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Margolis KL, Asche SE, Dehmer SP, et al. Long-term outcomes of the effects of home blood pressure telemonitoring and pharmacist management on blood pressure among adults with uncontrolled hypertension: follow-up of a cluster randomized clinical trial. JAMA Netw Open. 2018;1:e181617. doi: 10.1001/jamanetworkopen.2018.1617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Artinian NT, Flack JM, Nordstrom CK, et al. Effects of nurse-managed telemonitoring on blood pressure at 12-month follow-up among urban African Americans. Nurs Res. 2007;56:312–322. doi: 10.1097/01.NNR.0000289501.45284.6e. [DOI] [PubMed] [Google Scholar]
- 115.Hebert PL, Sisk JE, Tuzzio L, et al. Nurse-led disease management for hypertension control in a diverse urban community: a randomized trial. J Gen Intern Med. 2012;27:630–639. doi: 10.1007/s11606-011-1924-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Riegel GR, Ribeiro PAB, Rodrigues MP, et al. Efficacy of nutritional recommendations given by registered dietitians compared to other healthcare providers in reducing arterial blood pressure: systematic review and meta-analysis. Clin Nutr. 2018;37:522–531. doi: 10.1016/j.clnu.2016.12.019. [DOI] [PubMed] [Google Scholar]
- 117.HEARTS Technical package for cardiovascular disease management in primary health care: implementation guide. Licence: CC BY-NC-SA 3.0 IGO. Geneva: World Health Organization; 2018 (WHO/NMH/NVI/18.14). [Google Scholar]
- 118.Centers for Disease Control and Prevention. Self-measured blood pressure monitoring: action steps for public health practitioners. Atlanta, GA: Centers for Disease Control and Prevention, US Dept of Health and Human Services; 2013. [Google Scholar]
- 119.Omboni S. Connected health in hypertension management. Front Cardiovasc Med. 2019;6:76. doi: 10.3389/fcvm.2019.00076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Thangada ND, Garg N, Pandey A, Kumar N. The emerging role of mobile-health applications in the management of hypertension. Curr Cardiol Rep. 2018;20:78. doi: 10.1007/s11886-018-1022-7. [DOI] [PubMed] [Google Scholar]
- 121.Fletcher BR, Hartmann-Boyce J, Hinton L, McManus RJ. The effect of self-monitoring of blood pressure on medication adherence and lifestyle factors: a systematic review and meta-analysis. Am J Hypertens. 2015;28:1209–1221. doi: 10.1093/ajh/hpv008. [DOI] [PubMed] [Google Scholar]
- 122.Tucker KL, Sheppard JP, Stevens R, et al. Self-monitoring of blood pressure in hypertension: a systematic review and individual patient data meta-analysis. PLoS Med. 2017;14:e1002389. doi: 10.1371/journal.pmed.1002389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Uhlig K, Patel K, Ip S, et al. Self-measured blood pressure monitoring in the management of hypertension: a systematic review and meta-analysis. Ann Intern Med. 2013;159:185–194. doi: 10.7326/0003-4819-159-3-201308060-00008. [DOI] [PubMed] [Google Scholar]
- 124.Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH). Eur Heart J. 2018;39:3021–3104. doi: 10.1093/eurheartj/ehy339. [DOI] [PubMed] [Google Scholar]
- 125.Lee CJ, Park S. The role of home blood pressure telemonitoring for blood pressure control. Pulse (Basel, Switzerland) 2016;4:78–84. doi: 10.1159/000448375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Parati G, Dolan E, McManus RJ, Omboni S. Home blood pressure telemonitoring in the 21st century. J Clin Hypertens (Greenwich) 2018;20:1128–1132. doi: 10.1111/jch.13305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.McManus RJ, Mant J, Haque MS, et al. Effect of self-monitoring and medication self-titration on systolic blood pressure in hypertensive patients at high risk of cardiovascular disease: the TASMIN-SR randomized clinical trial. JAMA. 2014;312:799–808. doi: 10.1001/jama.2014.10057. [DOI] [PubMed] [Google Scholar]
- 128.Cheng C, Studdiford JS, Diamond JJ, Chambers CV. Primary care physician beliefs regarding usefulness of self-monitoring of blood pressure. Blood Press Monit. 2003;8:249–254. doi: 10.1097/00126097-200312000-00005. [DOI] [PubMed] [Google Scholar]
- 129.Logan AG, Dunai A, McIsaac WJ, et al. Attitudes of primary care physicians and their patients about home blood pressure monitoring in Ontario. J Hypertens. 2008;26:446–452. doi: 10.1097/HJH.0b013e3282f2fdd4. [DOI] [PubMed] [Google Scholar]
- 130.Obara T, Ohkubo T, Fukunaga H, et al. Practice and awareness of physicians regarding home blood pressure measurement in Japan. Hypertens Res. 2010;33:428–434. doi: 10.1038/hr.2010.10. [DOI] [PubMed] [Google Scholar]
- 131.Tislér A, Dunai A, Keszei A, et al. Primary-care physicians’ views about the use of home/self blood pressure monitoring: nationwide survey in Hungary. J Hypertens. 2006;24:1729–1735. doi: 10.1097/01.hjh.0000242396.15097.f3. [DOI] [PubMed] [Google Scholar]
- 132.Tang CH, Chuang PY, Chen CA, Fang YC. Medical costs of cardiovascular diseases in Taiwan. Value Health. 2014;17:A759–A760. doi: 10.1016/j.jval.2014.08.251. [DOI] [PubMed] [Google Scholar]
- 133.Virani SS, Alonso A, Benjamin EJ, et al. Heart disease and stroke statistics-2020 update: a report from the American Heart Association. Circulation. 2020;141:e139–e596. doi: 10.1161/CIR.0000000000000757. [DOI] [PubMed] [Google Scholar]
- 134.Funahashi J, Ohkubo T, Fukunaga H, et al. The economic impact of the introduction of home blood pressure measurement for the diagnosis and treatment of hypertension. Blood Press Monit. 2006;11:257–267. doi: 10.1097/01.mbp.0000217996.19839.70. [DOI] [PubMed] [Google Scholar]
- 135.Lovibond K, Jowett S, Barton P, et al. Cost-effectiveness of options for the diagnosis of high blood pressure in primary care: a modelling study. Lancet. 2011;378:1219–1230. doi: 10.1016/S0140-6736(11)61184-7. [DOI] [PubMed] [Google Scholar]
- 136.Arrieta A, Woods JR, Qiao N, Jay SJ. Cost-benefit analysis of home blood pressure monitoring in hypertension diagnosis and treatment: an insurer perspective. Hypertension. 2014;64:891–896. doi: 10.1161/HYPERTENSIONAHA.114.03780. [DOI] [PubMed] [Google Scholar]
- 137.Fletcher BR, Hinton L, Hartmann-Boyce J, et al. Self-monitoring blood pressure in hypertension, patient and provider perspectives: a systematic review and thematic synthesis. Patient Educ Couns. 2016;99:210–219. doi: 10.1016/j.pec.2015.08.026. [DOI] [PubMed] [Google Scholar]
- 138.Parati G, Omboni S, Albini F, et al. Home blood pressure telemonitoring improves hypertension control in general practice. The TeleBPCare study. J Hypertens. 2009;27:198–203. doi: 10.1097/hjh.0b013e3283163caf. [DOI] [PubMed] [Google Scholar]
- 139.Jacob V, Chattopadhyay SK, Proia KK, et al. Economics of self-measured blood pressure monitoring: a community guide systematic review. Am J Prev Med. 2017;53:e105–e113. doi: 10.1016/j.amepre.2017.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. Hypertension. 2018;71:e13–e115. doi: 10.1161/HYP.0000000000000065. [DOI] [PubMed] [Google Scholar]
- 141.Lin HJ, Pan HY, Kobeissi E, et al. May measurement month 2017: results from Taiwan-East Asia. Eur Heart J Suppl. 2019;21(Suppl D):D115–D117. doi: 10.1093/eurheartj/suz073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Lin HJ, Pan HY, Beaney T, et al. May measurement month 2018: an analysis of blood pressure screening results from Taiwan. Eur Heart J Suppl. 2020;22(Suppl H):H125–H127. doi: 10.1093/eurheartj/suaa087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Cheng HM, Lin HJ, Wang TD, Chen CH. Asian management of hypertension: current status, home blood pressure, and specific concerns in Taiwan. J Clin Hypertens (Greenwich) 2020;22:511–514. doi: 10.1111/jch.13747. [DOI] [PMC free article] [PubMed] [Google Scholar]