Abstract
Aims
This study aims to define the epidemiology of trauma presenting to a single centre providing all orthopaedic trauma care for a population of ∼ 900,000 over the first 40 days of the COVID-19 pandemic compared to that presenting over the same period one year earlier. The secondary aim was to compare this with population mobility data obtained from Google.
Methods
A cross-sectional study of consecutive adult (> 13 years) patients with musculoskeletal trauma referred as either in-patients or out-patients over a 40-day period beginning on 5 March 2020, the date of the first reported UK COVID-19 death, was performed. This time period encompassed social distancing measures. This group was compared to a group of patients referred over the same calendar period in 2019 and to publicly available mobility data from Google.
Results
Orthopaedic trauma referrals reduced by 42% (1,056 compared to 1,820) during the study period, and by 58% (405 compared to 967) following national lockdown. Outpatient referrals reduced by 44%, and inpatient referrals by 36%, and the number of surgeries performed by 36%. The regional incidence of traumatic injury fell from 5.07 (95% confidence interval (CI) 4.79 to 5.35) to 2.94 (95% CI 2.52 to 3.32) per 100,000 population per day. Significant reductions were seen in injuries related to sports and alcohol consumption. No admissions occurred relating to major trauma (Injury Severity Score > 16) or violence against the person. Changes in population mobility and trauma volume from baseline correlated significantly (Pearson’s correlation 0.749, 95% CI 0.58 to 0.85, p < 0.001). However, admissions related to fragility fractures remained unchanged compared to the 2019 baseline.
Conclusion
The profound changes in social behaviour and mobility during the early stages of the COVID-19 pandemic have directly correlated with a significant decrease in orthopaedic trauma referrals, but fragility fractures remained unaffected and provision for these patients should be maintained.
Cite this article: Bone Joint Open 2020;1-6:182–189.
Keywords: COVID-19, Adult trauma, Social distancing
Introduction
Epidemiology is an important aspect of anticipating healthcare resource requirements. Any change in epidemiology during a pandemic merits investigation because resources are scarce and workforce planning often requires redeployment to key areas. On 11 March 2020, the COVID-19 outbreak was defined as a pandemic by the World Health Organization (WHO). Musculoskeletal trauma can be expected to continue to occur throughout a pandemic and often involves emergency or urgent management of time-sensitive injuries. The nature and volume of musculoskeletal injuries, however, would likely change from baseline, especially as social distancing and quarantine measures are introduced on a population scale.
The compliance of a population with social distancing measures is inferred by the reduction in population mobility compared to baseline levels. This data is currently being made publicly available by Google as Community Mobility Report datasets that highlight the percentage change in visits to places like food shops and parks within a geographical area from 15 February 2020 compared to the five-week period of 3 January to 6 February 2020.1 Google Location History (GLH) data is passively collected by Android mobile phone users and those using Google Maps on other mobile phones who have ‘opted in’ on location settings. It has been validated as spatially equivalent to GPS tracker data within 100 metres and avoids the bias of self-reporting in survey data.2 A reduction in trauma volumes through social distancing would be desirable because it may help reduce the burden on an overstretched healthcare system and conserve personal protective equipment (PPE). If such a change in trauma volume correlated with mobility data, this could be used to estimate trauma service requirements.
The aim of this study is to identify the impact of the social distancing measures implemented in the UK as part of the COVID-19 pandemic response on musculoskeletal trauma volume and epidemiology. The secondary aim was to correlate adult musculoskeletal trauma epidemiology with mobility data obtained by Google from mobile phone carriage during the pandemic.
Methods
The study was reviewed and registered with the institutional musculoskeletal audit and quality improvement group. Data from 1,056 consecutive patients with musculoskeletal injuries referred to the orthopaedic trauma service in Edinburgh during a 40-day period of the COVID pandemic were compared with data from 1,820 consecutive patients referred with musculoskeletal injuries to the same service over the same period in 2019. This 40-day period from 5 March (the date of the first UK COVID-19 death) to 13 April 2020 (the expected peak) spanned the various social distancing measures introduced by the UK government (Table I). All patients referred to the orthopaedic trauma service at the study centre, including both in-patients requiring admission and those referred as out-patients from our regional emergency departments and minor injury units were included. At our institution, all such out-patient referrals are made via a trauma triage clinic (TTC) whereby medical records and radiographs are reviewed remotely and triaged to discharge, an out-patient review, further investigations or surgery.3 The study institution is the only provider of orthopaedic care (both major trauma and community level trauma, via two emergency departments, a minor injuries unit and primary care) for the region, currently estimated as a population of 897,770.4
Table I.
Timeline of key points in the COVID-19 pandemic in the UK and social distancing measures.
| Date | Event | Population status |
|---|---|---|
| 29/01/20 | First confirmed COVID-19 case in UK | |
| 05/03/20 | First COVID-19 death in UK | COVID-19 aware |
| 14/03/20 | First COVID-19 death in Scotland | |
| 16/03/20 | First Prime Minister briefing to UK public: Advice to avoid pubs/restaurants |
Socially distanced |
| 20/03/20 | First formal restrictions in UK: Schools close All pubs, restaurants, gyms, and social venues close |
|
| 23/03/20 | UK lockdown | Lockdown |
| 12/04/20 | Anticipated peak of COVID-19 deaths | |
| 13/04/20 | 40 days after first UK COVID-19 death |
Patients were identified from electronically stored admissions lists, theatre lists, and TTC referrals for the two defined time periods. Electronic patient records were examined and the following recorded: age, sex, deprivation quintile (Scottish Index of Multiple Deprivation, SIMD), residential status, diagnosis, fracture location, polytrauma, fragility fracture status, date of injury, date of presentation, mechanism of injury, and relationship to alcohol. Arthroplasty complications were defined as any complication of surgery which would require arthroplasty expertise to treat (for example, dislocated/infected arthroplasties). Fragility fractures were defined as low energy fractures occurring in falls from standing height or less5 (including but not limited to fractures of the distal radii, proximal humeri, pubic rami, proximal or distal femur and ankle) typically occurring in patients ≥ 65 years of age or in those with confirmed osteoporosis. For TTC patients, diagnosis and mechanism of injury were recorded, in addition to patient demographics.
SIMD quintiles were assigned according to the patient’s postcode.6 The SIMD ranks geographical areas based upon seven domains: income, employment, education, housing, health, crime, and geographical access. Data zones are defined by postcodes and once ranked nationally are divided into population-weighted quintiles with one representing the most deprived and five the least deprived.
Mobility data for Edinburgh City was obtained from Google1 for the period 5 March to 11 April 2020. At the time of writing, mobility data was not available beyond this date. This data is publicly available and obtained from Android mobile phone users and those using Google maps on other phones who have ‘opted-in’ to location history account. It demonstrates how visits and length of visits to five categories of location (retail & recreation; groceries & pharmacy; parks; transit stations; and workplace) differ from baseline activity (the median for that day of the week for the preceding six weeks). It has previously been validated as a reliable and accurate measure of human mobility against GPS data and survey data.2 In Scotland, Google community mobility data is reported by council region. Edinburgh orthopaedic trauma services has a catchment area including four council regions: Edinburgh City (2018 population 522,350); East Lothian (2018 population 101,940); Midlothian (2018 population 91,340); and West Lothian (2018 population 182,140).7 As each council area displayed similar trends in mobility reduction, data for Edinburgh City representing 58% of the catchment population was utilized.
Statistical analysis
Statistical analysis was performed using SPSS version 25.0 (IBM, Armonk, New York, USA). Data were tested for normality and univariate analysis was performed using parametric (t-test: unpaired) and non-parametric (Mann-Whitney U-test) tests as appropriate to assess differences in continuous variables between 2019 and 2020. Nominal categorical variables were assessed using Chi squared or Fisher’s exact test. Baseline trauma volumes were defined as the daily volume of trauma referred in 2019. Changes in trauma volume from baseline were calculated as the difference in trauma volume in 2020 compared to the same day in 2019 and were converted to percentage changes from baseline. Pearson’s correlation was used to assess the relationship between the percentage changes from baseline in trauma volume and Google mobility data.1 Where trauma volume was plotted graphically against mobility data a 3 day rolling mean was used for trauma volume. A p value of < 0.05 was considered statistically significant.
The data collection was carried out in accordance with the GMC guidelines for good clinical practice and the Declaration of Helsinki. Patient and Public Involvement was not possible in the context of current social distancing rules.
Source of funding
This study was completed without funding.
Results
Orthopaedic trauma referrals
During the 40-day period of the COVID-19 pandemic analyzed, 1,056 patients were referred with musculoskeletal injuries to the orthopaedic trauma service with a median age of 48 years (interquartile range (IQR) 31 to 73; 13 to 99) and 582/1056 (55%) were female. This represented a 42% reduction in volume compared to the same period in 2019 during which 1820 patients were referred to the same service (p < 0.001, Mann-Whitney U test) (Table II, Figure 1). Overall, the incidence of musculoskeletal injuries during this 40-day period of the COVID-19 pandemic decreased from 5.07 per 100,000 per day (95% CI 4.79 to 5.35) in 2019 to 2.94 per 100,000 (95% CI 2.52 to 3.32) for the same period in 2020.
Table II.
Mean number of orthopaedic referrals per day for the 40-day period 5 March to 13 April in 2019 and 2020.
| Setting | Variable | 2019 | 2020 | p-value | ||
|---|---|---|---|---|---|---|
| Mean | 95% CI | Mean | 95% CI | |||
| All trauma referrals | 45.5 | 43.2 to 48.1 | 26.4 | 22.9 to 30.0 | < 0.001* | |
| Outpatient | TTC | 35.4 | 33.2 to 37.7 | 19.9 | 16.7 to 22.9 | < 0.001* |
| Hospital admissions | All admissions | 10.1 | 8.90 to 11.4 | 6.53 | 5.68 to 7.44 | < 0.001* |
| Operative admissions | 7.0 | 6.08 to 7.97 | 4.0 | 4.00 to 4.00 | < 0.001* | |
| Non-operative admissions | 3.13 | 2.60 to 3.65 | 6.53 | 5.68 to 7.44 | < 0.001* | |
| Fragility factures | 5.03 | 4.28 to 5.87 | 4.23 | 3.68 to 4.83 | 0.173* | |
| Femoral fragility fractures | 2.98 | 2.49 to 3.49 | 2.67 | 2.18 to 3.14 | 0.503* | |
| Non-fragility fractures | 5.1 | 4.36 to 5.86 | 2.30 | 1.75 to 2.85 | < 0.001* | |
Mann Whitney U test.
TTC, trauma triage clinic (new outpatient trauma referrals)
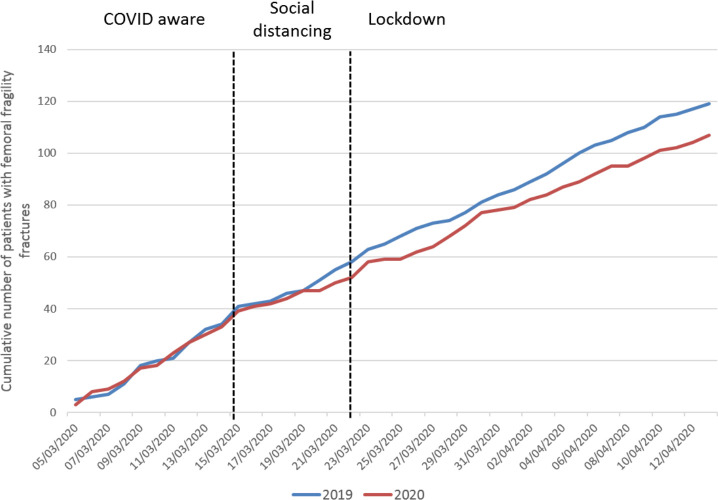
Fig. 1.
Distribution of inpatient and outpatient trauma volume for the 40-day period 5 March to 13 April 2020. The baseline trauma volume from 2019 is shown in red.
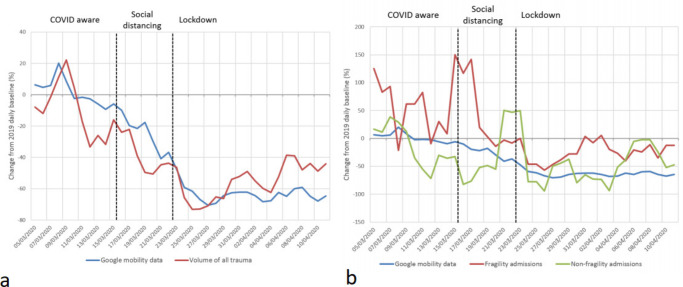
The greatest reduction in trauma volume was in new outpatient TTC referrals (Table II, Figure 1), which reduced by 44% (2019 n = 1,415; 2020 n = 795, p < 0.001, Mann-Whitney U test). Significant reductions also occurred in operative admissions (36% reduction, from 280 in 2019 to 179 in 2020, p < 0.001 Mann-Whitney U Test) and non-operative admissions (34% reduction from 125 in 2019 to 82 in 2020, p < 0.001 Mann-Whitney U Test). Though 42 fewer fragility fractures were admitted over the 40-day period of the COVID-19 pandemic compared to the previous year, the volume of fragility fractures admitted per day did not differ significantly (2019 mean per day (95% CI 5.0 (4.3 to 5.9); 2020 mean per day 4.2 (3.7 to 4.8), p = 0.173, Mann Whitney U-test). Femoral fragility fractures in particular did not change significantly from the 2019 baseline during the pandemic (2019 mean per day: 3.0 (2.5 to 3.5); 2020 mean per day 2.7 (2.2 to 3.1), p = 0.503, Mann Whitney U-test), (Table II, Figures 2 and 3). During the COVID-19 pandemic, fragility fractures represented a significantly greater relative proportion of admissions: 201/405 (50%) in 2019 vs 169/261 (65%) in 2020, p < 0.001 (Chi squared). Moreover, compared with 2019, there was no significant difference in the proportion of orthopaedic admissions managed operatively during the pandemic (2019: 280/405, 69%; 2020: 179/261,69%, p = 0.880 Chi squared).
Fig. 2.
Cumulative number of patients with femoral fragility fractures for the 40-day period 5 March to 13 April for the years 2019 (baseline) and 2020 (COVID-19 pandemic).
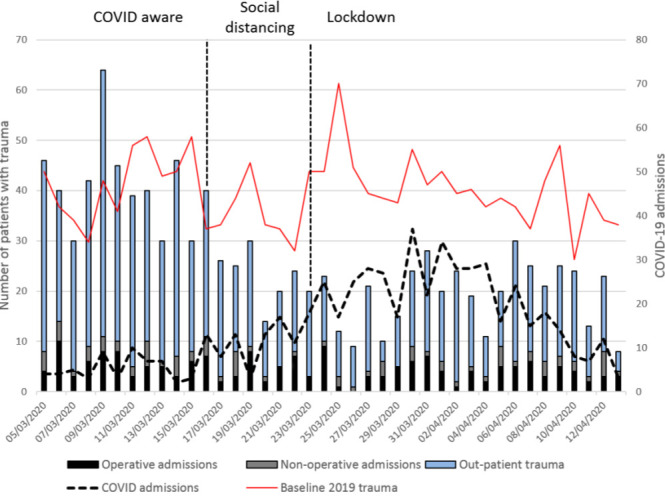
Fig. 3.
Change from baseline in trauma volume and population mobility in the Edinburgh population for a) all trauma and b) patients admitted with fragility and non-fragility trauma.
Impact of social distancing measures
As social distancing measures were introduced and the population progressed from being COVID-19 aware, to formally socially distanced and finally to being in lockdown (Table I), the daily volume of all trauma reduced significantly from a mean of 41 referrals per day (95% CI 36.0 to 46.6) to 19.3 referrals per day (95% CI 16.4 to 22.2, p < 0.001, Kruskall Wallis) (Table III). This was predominantly driven by significant reductions in outpatient trauma referrals and admissions for non-operative fracture management as social distancing progressed (Table III).
Table III.
Mean number of orthopaedic referrals per day for three periods encompassing different social distancing measures: COVID aware (5 to 16 March); formal social distancing (17 to 23 March); and lockdown (24 March to 13 April).
| Setting | COVID-19 aware (5/03 to 16/03) |
Social distancing (17/03 to 23/03) |
Lockdown (24/03 to 13/04) |
p-value | |||
|---|---|---|---|---|---|---|---|
| Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | ||
| All trauma referrals | 41.0 | 36.0 to 46.6 | 22.7 | 18.6 to 26.25 | 19.29 | 16.44 to 22-19 | < 0.001* |
| Outpatient TTC | 32.4 | 28.1 to 37.7 | 17.1 | 14.0 to 20.0 | 13.6 | 11.1 to 15.9 | < 0.001* |
| Hospital admissions | |||||||
| All admissions | 8.58 | 6.94 to 10.1 | 5.57 | 3.67 to 7.50 | 5.67 | 4.61 to 6.71 | 0.020* |
| Operative admissions | 5.67 | 4.43 to 6.87 | 4.29 | 2.60 to 6.17 | 3.86 | 3.00 to 4.76 | 0.109* |
| Non-operative admissions | 2.92 | 2.15 to 3.67 | 1.29 | 0.33 to 2.83 | 1.81 | 1.33 to 2.32 | 0.013* |
| Fragility factures | 5.42 | 4.18 to 6.67 | 3.57 | 2.75 to 4.43 | 3.76 | 3.1 to 4.45 | 0.065* |
| Femoral fragility fractures | 3.42 | 2.5 to 4.29 | 2.43 | 1.0 to 4.0 | 2.33 | 1.77 to 2.9 | 0.169* |
| Non-fragility fractures | 3.17 | 2.0 to 4.3 | 2.0 | 0.75 to 3.25 | 1.9 | 1.20 to 2.56 | 0.194* |
TTC, trauma triage clinic (new outpatient trauma referrals).
Kruskal Wallis
Impact on major trauma
During the pandemic no major trauma/polytrauma (ISS > 16) patients were admitted compared to 23/405 (6%) of admissions in the same time period in 2019 (p < 0.001, Chi squared). Compared to baseline figures (Table IV), during the pandemic patients who were admitted to hospital were significantly older (median age 78 yrs (IQR 59 to 96) during the pandemic versus 70 yrs (49 to 83) 2019 baseline, p < 0.001, Mann-Whitney U Test) and were more likely to have fragility fractures (169/261 (65%) during the pandemic versus 201/405 (50%) 2019 baseline, p < 0.001, Chi squared) or lower limb injuries (166/261 (83%) during the pandemic versus 228/405 (73%) 2019 baseline, p = 0.017, Chi squared) (Table IV). The deprivation quintiles differed in outpatient trauma between 2019 and 2020, but no such relationship was identified for those admitted to hospital (Table IV).
Table IV.
Patient characteristics for orthopaedic admissions. Median (IQR), number (%).
| Variable | 2019 (n = 405) | 2020 (n = 261) | p-value |
|---|---|---|---|
| Age, median (IQR) | 70 (49 to 83) | 78 (59 to 86) | < 0.001* |
| Female sex, n (%) | 246 (61) | 159 (61) | 0.963† |
| Residency outside Edinburgh, n (%) | 29 (7) | 1 (1) | < 0.001† |
| SIMD, n (%) | |||
| (most deprived) Quintile 1 | 48 (12) | 28 (11) | 0.396† |
| 2 | 79 (20) | 53 (20) | |
| 3 | 78 (39) | 51 (20) | |
| 4 | 75 (19) | 38 (15) | |
| (least deprived) Quintile 5 | 106 (26) | 86 (33) | |
| Time to presentation days, median (IQR) | 0 (0 to 0) | 0 (0 to 0) | 0.073* |
| Injury type, n (%) | |||
| Polytrauma | 23 (6) | 0 (0) | < 0.001† |
| Fragility fracture | 201 (50) | 169 (65) | < 0.001† |
| Upper or lower limb, n (%) | |||
| Upper limb injury | 86 (27) | 33 (17) | 0.017† |
| Lower limb injury | 228 (73) | 166 (83) | |
| Mechanism of injury, n (%) | 0.023† | ||
| All Falls | 270 (67) | 196 (75) | 0.017† |
| From standing | 235 (58) | 171 (66) | |
| Downstairs | 9 (2) | 4 (2) | |
| From height < 2 metres | 6 (1) | 10 (4) | |
| From height > 2 metres | 20 (5) | 11 (4) | |
| Motor vehicle accidents, n (%) | 23 (6) | 12 (5) | 0.549† |
| Pedestrian hit by vehicle | 4 (1) | 2 (1) | |
| Cyclist fall or hit by vehicle | 8 (2) | 4 (2) | |
| Motor cyclist fall or hit by vehicle | 7 (2) | 3 (1) | |
| Occupant of vehicle | 4 (1) | 3 (1) | |
| Sports, n (%) | 28 (7) | 3 (1) | 0.001 |
| Assault | 4 (1) | 0 (0) | |
| Direct blow/crush | 4 (1) | 1 (1) | |
| Other | 6 (1) | 5 (2) | |
| Atraumatic | 70 (17) | 43 (16) | |
| Alcohol-related, n (%) | 44 (11) | 13 (5) | 0.011† |
IQR, interquartile range; SIMD, Scottish Index of Multiple Deprivation.
Mann-Whitney U test
Chi square
Mechanism of injury
The mechanism of injury among patients requiring admission to hospital differed significantly during the study periods (p = 0.023, Chi squared, Table IV). Sports (3/261 (1%) versus 28/405 (7%)) and alcohol-related injuries (13/261 (5%) versus 44/405 (11%)) were significantly less common during the pandemic (p < 0.001 and p = 0.011 respectively, Chi squared), whereas falls were more frequent (196/261 (75%) versus 270/405 (67%), p = 0.017, Chi squared). No admissions were required for injuries sustained following an assault. A similar pattern was evident for new outpatient trauma referrals (Table V) where a significant difference in mechanism of injury (p < 0.001, Chi squared) was driven by an increase in the proportion of falls and a reduction in sporting injuries during social distancing (Table V). Location of injury data was available for these outpatient referrals and demonstrated significant differences in injury location between 2019 and 2020 (p < 0.001, Chi squared, Table V) with the number of injuries sustained at home increasing from 35% (490/1,415) to 57% (455/795) during the early stages of the pandemic.
Table V.
Patient characteristics for trauma outpatient referrals. Median (IQR), number (%)
| Variable | 2019 (n = 1415) | 2020 (n = 795) | p-value |
|---|---|---|---|
| Age, median (IQR) | 42 (21 to 60) | 44 (27 to 64) | 0.001* |
| Female sex, n (%) | 702(50) | 423 (53) | 0.108† |
| SIMD, n (%) | 0.043† | ||
| (most deprived) Quintile 1 | 201 (14) | 136 (17) | |
| 2 | 312 (22) | 159 (20) | |
| 3 | 233 (16) | 103 (13) | |
| 4 | 257 (18) | 134 (17) | |
| (least deprived) Quintile 5 | 373 (26) | 232 (29) | |
| Place of injury, n (%) | < 0.001 | ||
| Home | 487 (34) | 338 (42) | |
| Care Institution or hospital | 3 (0) | 2 (1) | |
| Educational establishment | 47 (3) | 20 (3) | |
| Public place | 391 (28) | 245 (31) | |
| Sports or leisure facility | 210 (15) | 54 (7) | |
| Roads or transport | 11 (1) | 1 (1) | |
| Pub or club | 8 (1) | 2 (1) | |
| Other | 159 (11) | 72 (9) | |
| Upper or lower limb, n (%) | 0.513† | ||
| Upper limb injury | 958 (68) | 557 (70) | |
| Lower limb injury | 450 (32) | 234 (30) | |
| Mechanism of injury, n (%) | < 0.001† | ||
| Fall | |||
| From height < 2 metres | 387 (27) | 280 (35) | |
| From height > 2 metres | 14 (1) | 3 (1) | |
| Motor vehicle accident, n (%) | |||
| Pedestrian hit by vehicle | 2 (1) | 2 (1) | |
| Cyclist fall or hit by vehicle | 18 (1) | 11 (1) | |
| Motor cyclist fall or hit by vehicle | 10 (1) | 5 (1) | |
| Occupant of vehicle | 6 (1) | 1 (1) | |
| Sports, n (%) | 231 (16) | 88 (11) | |
| Atraumatic | 0 (0) | 1 (1) | |
| Assault | 21 (1) | 4 (1) | |
| Other | 611 (43) | 399 (50) |
IQR, interquartile range; SIMD, Scottish Index of Multiple Deprivation.
Mann-Whitney U test
Chi squared
Google mobility data
Population mobility changes from baseline in Edinburgh as reported by Google correlated significantly with changes in total trauma volume from baseline for all reported activities (Table VI, Figure 3). The change from baseline in the volume of all trauma correlated significantly with mean mobility change from baseline (Pearson’s correlation 0.749 (0.58 to 0.85 95%CI) p < 0.001). Mobility did not correlate significantly with admissions to hospital and correlated least with fragility fractures that did not alter from their baseline significantly. Considering femoral fragility fractures alone, volume did not correlate with population mobility (Pearson’s correlation 0.211 (95% CI -0.20 to 0.507), p = 0.204)). Femoral fragility fracture volume did not change significantly with social distancing over the study period (Figure 2 and 3).
Table VI.
Correlations between trauma volume differences from baseline and population mobility differences from baseline as reported by Google.
| Type of activity | All trauma | Operative admissions | Nonoperative admissions | TTC | ||||
|---|---|---|---|---|---|---|---|---|
| PC | p-value | PC | p-value | PC | p-value | PC | p-value | |
| Retail and recreation | 0.825 | < 0.001 | 0.256 | 0.157 | 0.346 | 0.066 | 0.797 | < 0.001 |
| Grocery and pharmacy | 0.653 | < 0.001 | 0.147 | 0.422 | 0.434 | 0.019 | 0.622 | < 0.001 |
| Parks | 0.767 | < 0.001 | 0.250 | 0.167 | 0.251 | 0.188 | 0.725 | < 0.001 |
| Transit stations | 0.817 | < 0.001 | 0.307 | 0.087 | 0.330 | 0.080 | 0.778 | < 0.001 |
| Work | 0.786 | < 0.001 | 0.301 | 0.094 | 0.378 | 0.043 | 0.737 | < 0.001 |
| All activities | 0.749 | < 0.001 | 0.271 | 0.133 | 0.360 | 0.055 | 0.775 | < 0.001 |
PC = Pearson’s correlation.; TTC, trauma triage clinic referrals
Discussion
This study has demonstrated that behavioural changes and legislative restrictions during the early phase of the 2020 COVID-19 pandemic had a marked effect on adult trauma volume, reducing it by 42% compared to the same 40 day period in 2019, and by 58% in the early stages following “lockdown”. The volume of both out-patient trauma and hospital admissions for non-fragility fractures reduced significantly during the pandemic and this correlated significantly with reductions in population mobility from baseline levels as reported by Google.1 Polytrauma reduced significantly, with no cases of musculoskeletal polytrauma admitted during the 40 days of the pandemic studied. During the pandemic, low energy falls from standing predominated, sporting and alcohol-related injuries reduced significantly, and the patients admitted were significantly older. Fragility fractures requiring hospital admission, and femoral fragility fractures specifically, remained unchanged throughout this period. This key finding can be used to inform service provision during a pandemic with social distancing. The capacity for managing adult trauma can be appropriately reduced releasing operating theatre and ward resources, to areas of need. In our own centre, this has included taking on additional responsibilities for minor injuries and providing a ‘proning-service’ in the critical care areas. However, the demand for multidisciplinary care for elderly fragility fractures remains unchanged and should be prioritised where possible.
To the authors knowledge, these are the first quantified and detailed data of UK trauma service requirements during the COVID-19 pandemic to be correlated with Google mobility data. Human mobility is fundamental to understanding global issues in the health and social sciences such as infrastructure use and the spread of infectious disease.2 Google mobility data was developed for this purpose, but to date is an underutilized dataset that can be used to understand human population movement. It is being published presently to aid in the worldwide COVID pandemic response.1 The study centre is well placed for such an epidemiological study as orthopaedic care (including both major trauma and community level care) is provided to the population by a single orthopaedic centre. The correlation between trauma volume and population mobility is novel and demonstrates that compliance with social lockdown policies aids the health service by reducing the trauma burden. If this correlation between trauma volume and community mobility is consistent, mobility data could be used to estimate trauma service requirement during social distancing internationally. This study has limitations. Only a 40-day period during the early stages of the pandemic was covered. Location of injury data was not available for patients admitted to hospital. Google mobility data only reports mobility for individuals with Android operating system mobile phones (currently 47.5% of UK mobile phone market) and those using Google maps on other operating systems who have agreed for their location data to be collected. This may not be an accurate reflection of the true wider population mobility, and of the elderly population in particular. The mobility data used here pertained to the largest and most densely populated region of the study centre catchment area – Edinburgh City. Data for East Lothian, Midlothian, and West Lothian were not included, and this potentially introduces bias, though the trends in mobility reduction from baseline were the same for each of the four regions. The relationship between mobility data and trauma volume may differ in other parts of the UK. Social distancing measures differ internationally, and this relationship may not be present in other countries.
Based on the current modelling studies available, a recent Cochrane review has concluded that early implementation of quarantine in addition to other public health measures including school closures, travel restrictions and social distancing, are important in reducing incidence and mortality during the COVID-19 pandemic.8 Although nationwide lockdowns have already proven effective to contain the COVID-19 outbreak in some countries, there is concern regarding the negative unintended consequences of the prolonged quarantine in jeopardizing health,9 and mental health in particular.10 The numbers of patients who have sustained injury during this period but who have not yet presented, and who may yet require salvage orthopaedic trauma management, remains unknown. On the other hand, the current study demonstrates that a significant consequence of social distancing is a > 40% reduction in the volume of musculoskeletal trauma and a 58% reduction since national “lockdown”. The current study demonstrates that this reduction in trauma is directly proportional to reduced population activity and mobility. In turn this allows the release of valuable secondary care resources to care for the large numbers of patients requiring medical care for COVID-19 infection. Fragility fractures, however, occur largely in the domestic setting and continue to occur at the baseline rate. These patients, comprising the most vulnerable, comorbid and elderly section of the trauma population, are of course at increased risk of new complications such as contracting COVID-19 infection during a hospital admission and undergoing surgery.
Surgical decision making and admitting behaviours may be affected during a pandemic to minimize the exposure of patients to the hospital environment.11 Although our study has found that the relative proportions of upper and lower limb injuries were unchanged during the pandemic, admissions for upper limb injuries were reduced compared to baseline during the period of the pandemic studied. Though there was no significant difference from baseline in the proportion of orthopaedic admissions managed operatively during the pandemic, a reduction in upper limb admissions may represent altered decision making to more nonoperative management in some patients with upper limb injuries to avoid hospital exposure.
The social distancing measures introduced by the UK government during the early part of the COVID-19 pandemic had a significant effect in reducing musculoskeletal trauma volume by 40% to 58% at a large UK trauma centre. This potentially releases resource to be redeployed including theatre capacity, PPE, manpower, and hospital beds, in order to care for patients and support fellow healthcare professionals during the pandemic. Whether this change persists as social distancing continues remains to be seen. This reduction in musculoskeletal trauma correlated significantly with the reduction in population mobility within our region suggesting that compliance with social distancing can be used to predict trauma service requirements specific to a community. As lockdown is eased and population mobility increases, in can be expected that adult trauma will do so similarly. The incidence of fragility fractures in general, and femoral fragility fractures specifically, was unchanged during this period of the pandemic. These fractures typically occur in the patients most vulnerable to COVID-19 and in the case of femoral fragility fractures are normally associated with significant morbidity and mortality, as well as requiring operative intervention. Multidisciplinary services for fragility fracture patients should be maintained where possible as the volume of these patients has not reduced significantly during the COVID-19 pandemic.
Acknowledgements
The authors thank all of the orthopaedic surgeons whose patients were included in this study. The authors acknowledge the financial support of NHS Research Scotland (NRS), through Anish Amin and Chloe Scott of NHS Lothian.
Footnotes
Author contributions: C. Scott: Concept, Carried out data analysis and interpretation, Prepared and reviewed the manuscript.
G. Holland: Collected the data, Prepared and reviewed the manuscript.
M. F R Powell-Bowns: Collected the data, Prepared and reviewed the manuscript.
C. Brennan: Collected the data, Prepared and reviewed the manuscript.
M. Gillespie: Collected the data, Prepared and reviewed the manuscript.
S. Mackenzie: Collected the data, Prepared and reviewed the manuscript.
N. Clement: Carried out data analysis and interpretation, Prepared and reviewed the manuscript.
A. Amin: Carried out data analysis and interpretation, Prepared and reviewed the manuscript.
T. White: Carried out data analysis and interpretation, Prepared and reviewed the manuscript.
A. Duckworth: Carried out data analysis and interpretation, Prepared and reviewed the manuscript.
Funding statement: No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article
Twitter: Follow C. E. H. Scott @EdinburghKnee
Follow A. D. Duckworth @DuckworthOrthEd
ICMJE COI statement: C. Scott reports editorial board membership of The Bone & Joint Journal and Bone & Joint Research, and consultancy and grants/grants pending from Stryker Orthopaedics, all of which are unrelated to this article. T. White reports consultancy from Acumed, and grants/grants pening from Acumed and Smith & Nephew, which are unrelated to this article. A. Duckworth reports grants from Scottish Government Quality Improvement Grant, Smith & Nephew, and Acumed, and book royalties from Elsevier and Taylor & Francis, all of which are unrelated to this article.
References
- 1.Google Google COVID-19 Community Mobility Reports. Available from. https://www.google.com/covid19/mobility/ (date last accessed 23/04/2020).
- 2.Ruktanonchai NW, Ruktanonchai CW, Floyd JR, Tatem AJ. Using Google location history data to quantify fine-scale human mobility. Int J Health Geogr. 2018;17(1):28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.White TO, Mackenzie SP, Carter TH, et al. The evolution of fracture clinic design : the activity and safety of the Edinburgh Trauma Triage Clinic, with one-year follow-up. Bone Joint J. 2017;99-B(4):503–507. [DOI] [PubMed] [Google Scholar]
- 4.Government, S Population Estimates (Current Geographic Boundaries). 2020.
- 5.NICE Osteoporosis - prevention of fragility fractures. Available from. 2016. https://cks.nice.org.uk/osteoporosis-prevention-of-fragility-fractures#!management (date last accessed 24/04/2020).
- 6.Scottish_Government. The Scottish Government Scottish Index of Multiple Deprivation. 2016 350 [cited 2016 02/11/2016]
- 7.City Population United Kingdom - Urban Areas in Scotland. Available from. https://www.citypopulation.de/en/uk/cities/scotlandua/?cityid=7156 (date last accessed 19/05/2020).
- 8.Nussbaumer-Streit B, Mayr V, Dobrescu AI, et al. Quarantine alone or in combination with other public health measures to control COVID-19: a rapid review. Cochrane Database Syst Rev. 2020;4:CD013574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lippi G, Henry BM, Bovo C, Sanchis-Gomar F. Health risks and potential remedies during prolonged lockdowns for coronavirus disease 2019 (COVID-19). Diagnosis. 2020;7(2):85–90. [DOI] [PubMed] [Google Scholar]
- 10.Venkatesh A, Edirappuli S. Social distancing in covid-19: what are the mental health implications? BMJ. 2020;369:m1379. [DOI] [PubMed] [Google Scholar]
- 11.BOA Management of patients with urgent orthopaedic conditions and trauma during the coronavirus pandemic. Available from. 2020. https://www.boa.ac.uk/uploads/assets/ee39d8a8-9457-4533-9774e973c835246d/4e3170c2-d85f-4162-a32500f54b1e3b1f/COVID-19-BOASTs-Combined-FINAL.pdf (date last accessed 23/04/20).