Abstract
Aims
Elective surgery has been severely curtailed as a result of the COVID-19 pandemic. There is little evidence to guide surgeons in assessing what processes should be put in place to restart elective surgery safely in a time of endemic COVID-19 in the community.
Methods
We used data from a stand-alone hospital admitting and operating on 91 trauma patients. All patients were screened on admission and 100% of patients have been followed-up after discharge to assess outcome.
Results
Overall, 87 (96%) patients remained symptom-free and recovered well following surgery. Four (4%) patients developed symptoms of COVID-19, with polymerase chain reaction ribonucleiuc acid (PCR-RNA) testing confirming infection.
Conclusion
Based on our findings, we propose that if careful cohorting and screening is carried out in a stand-alone cold operating site, it is reasonable to resume elective operating, in a time of endemic but low community prevalence of SAR-Cov2.
Cite this article: Bone Joint Open 2020;1-6:229–235.
Keywords: COVID-19, Elective surgery
Introduction
In just a few months, the COVID-19 pandemic has had an unprecedented global impact on the way healthcare is delivered. There has been a radical shift of emphasis away from providing routine planned care. Healthcare systems around the world have concentrated their focus and resources on planning and provision for a predicted surge of emergency respiratory admissions requiring high dependency multisystem support. The resultant strain on the available infrastructure to accommodate such a shift of focus in healthcare prioritisation has led to a range of measures to help flatten the incidence curve and enable a managed response to the crisis. These include social distancing measures, limiting all but essential services, and the cessation of all but the most urgent elective operations.1,2
Limited evidence suggests that operating on patients in the midst of a COVID-19 pandemic may carry a high risk of mortality.3 This has resulted in uncertainty around the organisation of surgical services and designing protocols guiding when to operate and whom to operate on. Recently instigated multicentre studies are attempting to gather more robust evidence with respect to surgical risk.4,5 However, at time of writing these are in their early stages of data gathering and their findings will take a while to manifest.
As the first peak of the pandemic is passed, healthcare organisations recognize the need for a planned return to routine care. This must be done safely within an environment where COVID-19 remains endemic. While guidelines exist, there is no direct evidence to support them.
Aims
We set out to examine whether a stand-alone orthopaedic hospital using a cohorting strategy can offer a safe environment for trauma orthopaedic operating. Our healthcare area has had a relatively low prevalence of confirmed COVID-19 infection at 0.03% and an incidence of 29 per 100,000. We hope that our experience will provide a guide for safe resumption of elective services when prevalence in a region is at the level we have experienced during our low peak. We set out to extrapolate this to an elective surgical environment and so provide initial benchmarking evidence based guidance on when elective operating may be safely restarted.
Background
Cornwall is a county in the UK with a permanent resident population of 568,210.6 Its population is mainly served by one hospital trust with several hospital sites. Prior to the COVID-19 pandemic, trauma orthopaedic operating was undertaken at the main hospital. Our trauma unit within this site ran three orthopaedic trauma theatres daily performing 3,842 operations annually. NHS orthopaedic elective surgery was undertaken at a stand-alone elective orthopaedic hospital. This unit performed 2,820 operations per annum.
With the advent of COVID-19 planning, and in line with NHS England recommendations, all elective surgery on these sites was stopped on 16 March 2020.1 As of 26 March 2020 all orthopaedic trauma operating was moved to the elective hospital site, which became a stand-alone cohorted trauma unit (CTU). This was supported with a core of ring fenced trauma anaesthetists. Further physician support was provided by an on-site care of the elderly consultant led team.An injury unit to assess all musculoskeletal injuries was also set up at the CTU site. The fracture clinic also moved to the CTU site. Where possible orthopaedic trauma patients are followed up virtually and all minor injury units have the ability to speak directly to a consultant level surgeon as a first point of contact for advice. Paediatric surgery continues to be carried out at the main site, where an on-call consultant and junior surgeon are based. Major trauma continues to be referred to the regional major trauma centre. Orthopaedic trauma operating and injury management was rationalised according to guidance issued from the British Orthopaedic Association7 and the Royal College of Surgeons.8
COVID-19 treatment protocol for patients requiring surgery
Initial assessment is undertaken in the injury unit, with patients either self-presenting or arriving by ambulance. This is staffed by an orthopaedic consultant, registrar, senior house officer, trauma practitioner, physiotherapist, plaster technician, one emergency department (ED) trained nurse and one ED healthcare assistant. Government personal protective equipment (PPE) guidelines are followed when assessing a patient.9 Initial triage consists of a COVID-19 screening questionnaire (Table I) and thermal camera temperature measurement, before the patient enters the hospital. If this raises suspicion of active COVID-19 infection then the patient is assessed in an isolated bay with full PPE precautions. All patients are provided with a surgical mask prior to entering the hospital.
Table I.
Patient screening questions.
| COVID-19 questions | |
|---|---|
| Cough? | Yes / No |
| Fever? | Yes / No |
| Feeling short of breath? | Yes / No |
| Members of household with symptoms? | Yes / No |
| Have they been advised to self-isolate? | Yes / No |
| Have they been advised to be ‘shielded’? | Yes / No |
Ward admission for non COVID-19 suspected patients is into four bedded bays on the first floor. Elderly/at risk patients are kept separate to younger/low risk patients. If COVID-19 is suspected or proven then patients are admitted to the second floor ward and PCR-RNA testing undertaken. If the subsequent test proves negative, patients are moved down to the non-COVID-19 ward. If a patient on the non-COVID-19 ward is subsequently found to be positive, all patients within the same bay are isolated and transferred to the COVID-19 ward and full PPE precautions undertaken. The vacated bay then undergoes a deep clean.
Surgery for non-COVID-19 patients is undertaken in one of two laminar flow, positive pressure theatres. Whenever possible general anaesthesia is avoided. Full PPE is worn by the theatre team when aerosolising procedures are performed.10,11 The use of power tools and pulse lavage is avoided if possible. Personnel are kept to a minimum in theatre (anaesthetist, operating department practitioner, surgeon, assistant, scrub nurse, in-theatre runner, and a runner based outside of theatre). No one exits theatre for 20 minutes after the last aerosolization procedure (including extubaton) has been undertaken. Recovery takes place in the recovery room in the normal manner. Theatres are cleaned with the chlorine disinfectant product, Actichlor.
Surgery for suspected or confirmed COVID-19 patients is undertaken in a dedicated theatre. This is isolated from the rest of the theatre complex. Staff wear full PPE and scrub with instruments being opened prior to the patient entering theatre. Anaesthesia is performed within the operating room. Recovery is performed within theatre and no one exits until the patient has left. Full clothing change and showering is then performed by all staff via a “dirty corridor”.
Post-surgery patients are discharged from hospital as soon as possible to minimise the hospital reservoir effect.12
Methods
Study design and data collection
Following relevant approval, we undertook a retrospective review of our databases (Bluespier, Droitwich, UK; RADAR, Leeds, UK; MAXIMS, Milton-Keynes, UK) to capture all episodes of operations undertaken since the inception of the CTU model until 17 April 2020. Data collected were those of relevance in previous studies examining surgical morbidity and mortality in the context of COVID-19 infection3,13,14 (Table II). At a minimum of 11.5 days since surgery, all patients were contacted by phone to ascertain whether they may have developed COVID-19 symptoms (Table III). 11⋅5 days was chosen based on evidence that this should capture 97.5% of cases.15 We also recorded data on staff self-isolation.
Table II.
Baseline data.
| Age |
| Sex |
| NICE surgical complexity score (1 to 3) |
| Comorbidities (hypertension, heart disease, COPD, malignancy, kidney disease, diabetes, dementia, cerebrovascular disease, smoker) |
| ASA |
| Anaesthesia type |
| Length of surgery |
| Transfusion |
| Length of stay |
| Date of death |
| Readmission |
| Cause of death |
| Complications |
| COVID-19 test result (if taken) |
| Discharge destination |
COPD, chronic obstructive pulmonary disease; ASA, American Society of Anaesthesiologists classification of Physical Health.
Table III.
Telephone questions.
| Since discharge have you had... |
|---|
| Persistent cough |
| Fever (measured) |
| Shortness of breath |
| Anosmia |
| Symptomatic household members |
| Letter advising to self isolate from Public Health England |
| Advice to self-isolate since discharge |
Surgical difficulty
We used NICE criteria to categorize the level of surgical complexity, risk, and difficulty:16 Level 1 minor surgery such as excision of a lesion; Level 2 intermediate surgery such as arthroscopic meniscectomy; and Level 3 major/complex surgery such as arthroplasty or fracture fixation.
Definitions
A patient was considered to be positive if they had a positive sample analysed by PCR-RNA technique. In addition, any patient who was unable to be tested but had clinical symptoms17 without an alternative likely diagnosis was considered positive.
Role of funding source
The authors have not received any funding for this study. All authors had access to all the data and the corresponding author had final responsibility for the decision to submit.
Results
Baseline characteristics
We identified a total of 91 patients. No patient was lost to follow-up. The median age was 68 years (18 to 95). Male to female ratio was 45:46. Just under half the patients (40) were American Society of Anaestheisiologists Physical Health score (ASA) 3 or 4. The comorbidity profile of this patient cohort was representative for orthopaedic trauma. (Table IV).
Table IV.
Baseline characteristics of operative patients.
| Variable | Total (n = 91) |
|---|---|
| Age, median (IQR) | 68 (48 to 84) |
| Sex, n (%) | |
| Female | 46 (50.5) |
| Male | 45 (49.5) |
| Comorbidity n (%) | |
| HTN | 18 (19.8) |
| Diabetes | 10 (11) |
| Heart disease (IHD, CCF, valve abnormality, arrhythmia) |
19 (20.9) |
| COPD | 6 (6.6) |
| Active carcinoma | 7 (7.7) |
| CKD | 6 (6.6) |
| Cerebrovascular disease | 4 (4.4) |
| Dementia | 11 (12.1) |
| Other | 48 (52.8) |
| Current or previous smoking | 50 (55) |
| Surgical complexity, n (%) | |
| Level-1 | 6 (6.6) |
| Level-2 | 17 (18.9) |
| Level-3 | 68 (74.7) |
| ASA, n (%) | |
| I | 32 (35.2) |
| II | 20 (22) |
| III | 36 (39.6) |
| IV | 3 (3.3) |
| V | 0 (0) |
| Surgical time in minutes, median (IQR) | 64 (50 to 99) |
IQR, interquartile range; COPD, chronic obstructive pulmonary disease; HTN, hypertension.
Surgical difficulty
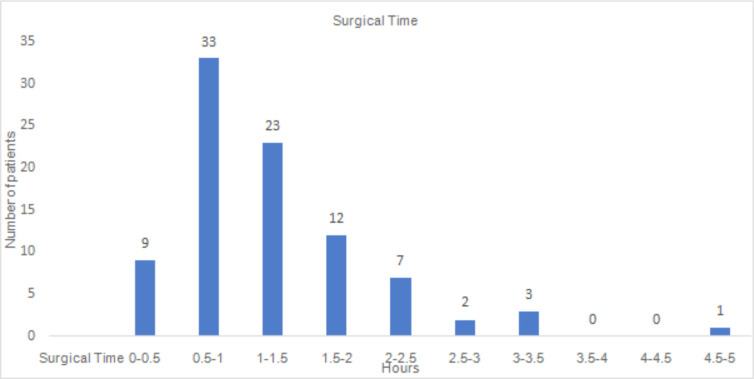
The majority of patients (75%) had Level 3 operations (Table V). Median surgical time was 64 minutes (IQR 60 to 90) (Figure 1).
Table V.
Type of surgery and grading of surgical complexity.
| Surgical procedure | Complexity | Number of cases |
|---|---|---|
| Ankle spanning external fixator | 2 | 2 |
| Application of circular frame | 3 | 1 |
| Arthroscopic meniscal repair | 3 | 1 |
| Arthroscopic debridement shoulder | 2 | 1 |
| Arthroscopic removal loose body knee | 2 | 1 |
| Arthroscopic rotator cuff repair | 3 | 2 |
| Aspiration of total hip arthroplasty | 1 | 1 |
| Cephalomedullary femoral nail | 3 | 6 |
| Distal biceps repair | 3 | 1 |
| Dynamic hip screw | 3 | 10 |
| Extensor tendon repair finger | 2 | 1 |
| First-stage revision total hip arthroplasty | 3 | 2 |
| Hand/wrist tenosynovectomy | 2 | 1 |
| Hip hemiarthroplasty | 3 | 21 |
| Intramedullary tibial nail | 3 | 1 |
| Knee spanning external fixator | 2 | 2 |
| MUA Ddslocated total hip arthroplasty | 1 | 3 |
| MUA dislocated native hip | 1 | 1 |
| NCB plate femoral periprosthetic fracture | 3 | 5 |
| Open reduction and scapho-lunate repair for perilunate dislocation | 3 | 1 |
| Open washout of infected total knee arthroplasty | 3 | 1 |
| Open reduction dislocated total hip arthroplasty | 2 | 1 |
| ORIF ankle | 3 | 5 |
| ORIF calcaneum | 3 | 1 |
| ORIF distal radii | 3 | 4 |
| ORIF proximal ulna and radial head excision | 3 | 1 |
| ORIF tibial plateau | 3 | 1 |
| Proximal femoral arthroplasty | 3 | 1 |
| Reconstruction of coracoclavicular ligament | 3 | 1 |
| Removal of foreign body foot | 1 | 1 |
| Repair ruptured patella tendon | 2 | 2 |
| Repair ruptured quadriceps tendon | 2 | 1 |
| Shoulder hemiarthroplasty | 3 | 1 |
| Tension band wire olecranon | 3 | 2 |
| Washout of flexor tendon sheath finger | 2 | 1 |
| WLE middle finger (papillary adenocarcinoma) | 2 | 1 |
| WLE toe melanoma | 2 | 1 |
| Wound debridement and split skin graft | 2 | 1 |
ORIF, open reduction and internal fixation.
Fig. 1.
Length of surgery in 30-minute intervals.
COVID-19 patients
During the study, undertaking PCR testing was limited and reserved for patients and staff where symptoms suggested potential COVID-19 infection. Overall, 24 patients were tested. Four patients tested positive for COVID-19. Three of these patients had arrived via the main hospital ED and two were nursing home residents. Two of these patients died within the study period. The other two have recovered and been discharged back to their original residence. All four patients tested positive following surgery; two while CTU inpatients and two while community hospital inpatients (Table VI).
Table VI.
Characteristics of COVID-19-positive patients.
| Age | Sex | Comorbidities | Admitted from | Operation | ASA | Surgical Time (Hrs:Mins) | Anaesthetic | Discharged to | COVID-19-positive | Outcome |
|---|---|---|---|---|---|---|---|---|---|---|
| 89 | F | IDDM, retinopathy, PVD, chronic leg ulcers, dementia, chronic anaemia, CKD 4, HTN, heart failure, AF | Own home (Via ED) 26/3/20 |
Femoral nail 27/3/20 | 3 | 2:10 | Spinal | Community hospital 3/4/20 |
12/4/20 | Own home 29/4/20 Asymptomatic |
| 94 | F | AF, HTN, TIA, SAH, cerebrovascular disease, heart failure, osteoporosis, CKD 3 | Own home (Via ED) 25/3/20 |
DHS 27/3/20 | 3 | 0:45 | Spinal | Community hospital 31/3/20 |
8/4/20 | RIP 15/4/20 |
| 85 | M | Parkinsons, HTN, AV block & PPM, IHD, PE, BPH – Long-term catheter, CKD 3, heart failure, diverticulosis, Chronic anaemia | Nursing home 27/3/20 |
Hip hemiarthroplasty 29/3/20 | 3 | 1:11 | Spinal | Died as inpatient | 31/3/20 | RIP 14/4/20 |
| 85 | M | Dementia, previous EtOH dependence, BPH, sleep apnoea, CKD 2 | Nursing home (Via ED) 6/4/20 |
Hip Hemi 7/4/20 | 3 | 1:34 | GA | Community hospital 16/4/20 |
8/4/20 | Nursing home 1/5/20 Asymptomatic |
IDDM, insulin dependent diabetes mellitus; PVD, peripheral vascular disease; CKD, chronic kidney disease; HTN, hypertension; AF, atrial fibrillation; TIA, transient ischaemic attack; SAH, subarachnoid haemorrhage; PPM, permanent pace maker; IHD, ischaemic heart disease; PE, pulmonary embolism; BPH, benign prostatic hypertrophy; EtOH, ethyl alcohol; DHS, dynamic hip screw; ASA, American Society of Anaesthesiologists physical health score.
Phone call follow-up
At 11.5 days, one patient had experienced shortness of breath and one had a cough. One patient developed a fever, but this was secondary to a urinary tract infection. They were otherwise well. Subsequent follow-up of these at a further 14 days found their symptoms resolved. In all, 13 patients (including all four COVID-19-positive patients) had received a letter from Public Health England advising self-isolation.
Staff sickness
Overall, 35 (14%) of clinical staff with patient facing roles underwent self-isolation (Table VII).
Table VII.
Reasons for staff self-isolation.
| Reason | (n = 258) |
|---|---|
| COVID-19-positive | 2 |
| At risk | 13 |
| Pregnant | 4 |
| Suspected | 16 |
All four of the COVID-19 cases tested positive postoperatively. Their operations had not been undertaken in the COVID-19 theatre. One member of theatre staff had isolated with symptoms since the procedures, but they had not been exposed to any of the four identified cases.
In all, 74 members of ward based staff were present on the wards while the four patients who subsequently developed COVID-19 were inpatients. Subsequently, three out of the 74 isolated with symptoms, although none tested positive.
Discussion
While there are many guidelines,18-21 this is the first study to examine the risks associated with undertaking surgery within a protocolised, cohorted framework aware of the potential morbidity associated with the COVID-19 pandemic. While there have been reports related to the 2003 SARS outbreak,22 as yet there is only one related to the current outbreak.3 It reports on 34 patients undergoing elective surgery who subsequently went on to develop COVID-19. They report a 44⋅1% need for intensive treatment unit (ITU) postoperatively and an overall 20.5% mortality rate. Complexity of surgery, length of surgery, patient age, and comorbidity burden were all associated with an increased risk of ITU admission and death.
During our study time frame, four patients tested positive for COVID-19 (Table VI). Two of these subsequently died. Three of these patients initially presented to the ED at the main hospital and two were nursing home residents. All four of these patients were elderly (85 to 94 years), significantly comorbid, and underwent complex Level 3 Hip fracture surgery for an injury which is known to carry a high mortality burden. In Lei et al’s paper,3 it is worth noting that their two hip arthroplasty patients both died. In our study, the two COVID-19-positive patients who died were the only two deaths in the 48 hip-related fractures that were operated on over our study period (4%) emphasizing that, within the limitations of this study, we can only infer an association rather than a causal effect. This limited evidence does not counter Lei’s finding that major surgery in comorbid patients potentially carries a high risk of death. However, we await the results of multicentre studies such as COVERT4 and PREDICT5 to further elucidate this association.
Two of the patients returned a positive test within two days of their operation, suggesting that they were likely infected at time of surgery. One of them survived. Neither of these two were cohorted in the same bay and no other patients they came into contact with developed symptoms. The other two returned a positive test following discharge to a community hospital at 12 and 16 days postoperatively. One of them survived. They were both inpatients at the same time. It is unclear whether these two developed the infection while inpatients at the CTU or in the community. Given they were both comorbid and undergoing Level 3 operations, we might expect that the physiological stress of surgery would accelerate the onset of COVID-19 symptoms3 and yet they had been discharged asymptomatic at four days and seven days respectively. What is clear, however, is that all four had a high risk presentation in terms of either coming from a nursing home environment or via the main hospital ED or both. We now consider such presentations as high risk and isolate patients until a PCR-RNA test result is known.
We did not operate on anyone who was known to be COVID-19 positive. If COVID-19 infection is suspected, our protocol means surgery is delayed until a COVID-19 test result is obtained. The one exception was a patient systemically septic with an infected knee arthroplasty, where delaying surgery until PCR-RNA results became available would have carried an unacceptably high risk. The COVID-19 theatre was also used a further four times for patients in order that staff could familiarise themselves with surgery under a full COVID-19 protocol. We acknowledge we have yet to have a situation where a known COVID-19 positive patient has presented with a significant injury that under normal circumstances would require surgery. When this occurs, an MDT approach involving the patient, family, anaesthetics, physician, intensive care, and surgeon would be undertaken with the high risk nature of the surgery and conservative management options fully explored.
As of the end of the study period, our healthcare area had a detected incidence of 29 cases per 100,000 and a detected prevalence of 0⋅03% in the population as a whole. Compared to the rest of the UK where prevalence as of 28 April was 0.21% and incidence of 208 cases per 100,000, our geographical area has remained relatively well shielded.23 These figures are, however, likely to represent a large underestimation as they only account for the known cases. Despite this, we emphasize that with a higher incidence per 100,000 population our results may not be reproducible.
In line with the rest of the UK,23 our healthcare area has started to see a drop-off in numbers of patients requiring hospitalization due to COVID-19. However, the majority of models predict a COVID-19 incidence that undergoes at least one, if not more troughs and peaks over the coming months.24,25
Our study indicates that protocolised operating in the manner described, using a stand-alone orthopaedic hospital at a time of endemic, but relatively low COVID-19 prevalence offers a low risk solution to both staff and patients for complex level 3 orthopaedic trauma surgery. This also appears to apply to higher risk comorbid and elderly patients. Surgical risk and patient groups vary between specialities, however these results have the potential to be extrapolated to other surgical disciplines. In the absence of any other such studies, these results can act as a baseline with which other investigators may compare their outcomes.
Implications for restarting elective surgery
There is recognition that COVID-19 will pose an ongoing risk for some time. However, recent figures indicate that the UK, as has happened in other parts of the world, has just passed its first peak of hospitalizations.23 Within the UK, this has prompted the NHS England Chief Executive to “start to make judgements on whether there is capacity for at least some routine non-urgent elective care”.26 A similar recognition of the need for an exit strategy that allows for a safe restart of planned routine care, within an ongoing endemic COVID-19 situation has also been acknowledged in the USA,27 Europe,28 and internationally.29
The Royal College of Surgeons of England, as well as some trusts and private units around the UK, are developing protocols to guide safe restarting of elective surgery.30 These guidelines are based on a pragmatic approach, aiming to minimise the risk of COVID-19 infection to patients and staff. Our trauma operating protocol was built on the reported evidence and guidelines available and though it does not specifically deal with elective surgery, extrapolation is possible.
As a trauma unit, we did not deny access to any patients. In addition, at the time of our study, testing for COVID-19 infection was restricted. Despite this, the cohorting strategy was effective. Within an elective scenario one has the ability to build in more control with respect to patient selection.
From our limited experience, and that of Lei et al,3 it appears that undergoing surgery when asymptomatic with a COVID-19 infection may carry a high risk of mortality and morbidity. As such, our study supports recommendations that patients undergo a period of self-isolation for fourteen days prior to surgery and a COVID-19 PCR-RNA test ± lung CT ± further screening tests and screening questionnaire in the immediate day or two before surgery.
Our four COVID-19 positive patients had significant pre-operative exposure risk. They were all either a nursing home resident and/or had a recent attendance at a “hot” hospital. Within an elective service, such patients would need to undergo a period of strict self-isolation as detailed above.
Our limited experience supports the available literature,3,13,14 which suggests that elderly comorbid patients are at more risk than their younger fitter counterparts. Our study supports guidance that in the initial phases surgery should be limited to lower risk patients until elective hospital cohort systems have been stress tested.
Finally, given the risk, the authors of this paper recommend including in the consent process a discussion with the patient about the morbidity and mortality risks of developing a COVID-19 infection following surgery.
We acknowledge the weakness of this single centre, retrospective review with a small sample size. At the time of the study, PCR-RNA testing was limited and thus asymptomatic infection may have been missed. With a lack of any form of benchmark in the literature, it is our hope that the results from this study will help guide a safe return to elective surgery.
Conclusion
In a time of endemic but low COVID-19 prevalence, our data indicate that surgery may be carried out safely if a cohorting ward strategy is adopted in a stand-alone surgical unit. These findings support the previously untested guidance from surgical governing bodies on how and when to restart elective surgery. Our data provides a baseline for future comparison by investigators.
Footnotes
Author contributions: M. Lazizi and C. J. Marusza: Collected and analyzed the data analysis, Wrote the paper.
S. A. Sexton: Analyzed the data, Wrote the paper.
R. G. Middleton: Analyzed the data, Wrote the paper.
M. Lazizi and CJ. Marusza are joint first authors.
Funding statement: No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Ethical review statement: The authors have not received any funding for this study.
References
- 1.Important and urgent – next steps on NHS response to COVID-19. https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/urgent-next-steps-on-nhs-response-to-covid-19-letter-simon-stevens.pdf (date last accessed May 4, 2020).
- 2.Koçak Tufan Z, Kayaaslan B. Crushing the curve, the role of national and international institutions and policy makers in COVID-19 pandemic. Turk J Med Sci. 2020;50(SI-1):495–508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lei S, Jiang F, Su W, et al. . Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection. EClinicalMedicine. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.CovidSurg – Globalsurg. https://globalsurg.org/covidsurg/ (date last accessed May 5, 2020).
- 5.PanSurg PREDICT. https://www.pansurg.org/predict/ (date last accessed May 5, 2020).
- 6.Estimates of the population for the UK, England and Wales, Scotland and Northern Ireland - Office for National Statistics. https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/datasets/populationestimatesforukenglandandwalesscotlandandnorthernireland (date last accessed May 5, 2020).
- 7.BOAST - Management of patients with urgent orthopaedic conditions and trauma during the coronavirus pandemic. https://www.boa.ac.uk/resources/covid-19-boasts-combined.html (date last accessed May 5, 2020).
- 8.Guidance for surgeons working during the COVID-19 pandemic — the surgical Royal Colleges of the United Kingdom and ireland. https://www.rcseng.ac.uk/coronavirus/joint-guidance-for-surgeons-v1/ (date last accessed May 5, 2020).
- 9.New personal protective equipment (PPE) guidance for NHS teams - GOV.UK. https://www.gov.uk/government/news/new-personal-protective-equipment-ppe-guidance-for-nhs-teams (date last accessed May 5, 2020).
- 10.Putting on (donning) personal protective equipment (PPE) for aerosol generating procedures (AGPs) – gown version. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/879098/PHE_COVID-19_Donning_gown_version.pdf (date last accessed May 5, 2020).
- 11.Hirschmann MT, Hart A, Henckel J, et al. . COVID-19 coronavirus: recommended personal protective equipment for the orthopaedic and trauma surgeon. Knee Surg Sports Traumatol Arthrosc. 2020;28(6):1690–1698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yu J, Ouyang W, Chua MLK, Xie C. SARS-CoV-2 transmission in patients with cancer at a tertiary care hospital in Wuhan, China. JAMA Oncol. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen T, Wu D, Chen H, et al. . Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ. 2020;368:m1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhou F, Yu T, Du R, et al. . Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lauer SA, Grantz KH, Bi Q, et al. . The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann Intern Med. 2020;172(9):577–582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Recommendations | routine preoperative tests for elective surgery | guidance | NICE. https://www.nice.org.uk/guidance/ng45/chapter/recommendations (date last accessed May 5, 2020).
- 17.Coronavirus disease 2019 (COVID-19) - Symptoms, diagnosis and treatment. BMJ Best Practice. 2019. [Google Scholar]
- 18.Coccolini F, Perrone G, Chiarugi M, et al. . Surgery in COVID-19 patients: operational directives. World J Emerg Surg. 2020;15(1):25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zarzaur BL, Stahl CC, Greenberg JA, Savage SA, Minter RM. Blueprint for restructuring a department of surgery in concert with the health care system during a pandemic: the University of Wisconsin experience. JAMA Surg. 2020. [DOI] [PubMed] [Google Scholar]
- 20.Coimbra R, Edwards S, Kurihara H, et al. . European Society of trauma and emergency surgery (ESTES) recommendations for trauma and emergency surgery preparation during times of COVID-19 infection. Eur J Trauma Emerg Surg. 2020;1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Balibrea JM, Badia JM, Rubio Pérez I, et al. . Surgical management of patients with COVID-19 infection. recommendations of the Spanish association of surgeons. Cir Esp. 2020;98(5):251–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tien HC, Chughtai T, Jogeklar A, Cooper AB, Brenneman F. Elective and emergency surgery in patients with severe acute respiratory syndrome (SARS). Can J Surg. 2005;48(1):71–74. [PMC free article] [PubMed] [Google Scholar]
- 23.Coronavirus COVID-19) cases in the UK. https://coronavirus.data.gov.uk/ (date last accessed May 5, 2020).
- 24.Adam D. Special report: the simulations driving the world's response to COVID-19. Nature. 2020;580(7803):316–318. [DOI] [PubMed] [Google Scholar]
- 25.Verity R, Okell LC, Dorigatti I, et al. . Estimates of the severity of coronavirus disease 2019: a model-based analysis. Lancet Infect Dis. 2020;20(6):669–677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chief exec. https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/04/second-phase-of-nhs-response-to-covid-19-letter-to-chief-execs-29-april-2020.pdf (date last accessed May 5, 2020).
- 27.Joint Statement Roadmap for Resuming elective surgery after COVID-19 pandemic | American Society of Anesthesiologists (ASA). https://www.asahq.org/about-asa/newsroom/news-releases/2020/04/joint-statement-on-elective-surgery-after-covid-19-pandemic (date last accessed May 5, 2020).
- 28.ESSKA recommendations and guidelines for resuming elective surgery - European Society of Sports Traumatology, Knee Surgery and Arthroscopy. https://www.esska.org/news/504296/ESSKA-recommendations-and-guidelines-for-resuming-elective-surgery.htm (date last accessed May 5, 2020).
- 29.Parvizi J, Gehrke T, Krueger CA, et al. . Current concepts review Resuming elective orthopaedic surgery during the COVID-19 pandemic.
- 30.Recovery of surgical services during and after COVID-19 — Royal College of Surgeons. https://www.rcseng.ac.uk/coronavirus/recovery-of-surgical-services/ (date last accessed May 5, 2020).