Abstract
Background.
Neuroticism is associated with the onset and maintenance of a number of mental health conditions, as well as a number of deleterious outcomes (e.g. physical health problems, higher divorce rates, lost productivity, and increased treatment seeking); thus, the consideration of whether this trait can be addressed in treatment is warranted. To date, outcome research has yielded mixed results regarding neuroticism’s responsiveness to treatment, perhaps due to the fact that study interventions are typically designed to target disorder symptoms rather than neuroticism itself. The purpose of the current study was to explore whether a course of treatment with the unified protocol (UP), a transdiagnostic intervention that was explicitly developed to target neuroticism, results in greater reductions in neuroticism compared to gold-standard, symptom focused cognitive behavioral therapy (CBT) protocols and a waitlist (WL) control condition.
Method.
Patients with principal anxiety disorders (N = 223) were included in this study. They completed a validated self-report measure of neuroticism, as well as clinician-rated measures of psychological symptoms.
Results.
At week 16, participants in the UP condition exhibited significantly lower levels of neuroticism than participants in the symptom-focused CBT (t(218) = − 2.17, p = 0.03, d = −0.32) and WL conditions(t(207) = −2.33, p = 0.02, d = −0.43), and these group differences remained after controlling for simultaneous fluctuations in depression and anxiety symptoms.
Conclusions.
Treatment effects on neuroticism may be most robust when this trait is explicitly targeted.
Keywords: Cognitive-behavioral therapy, neuroticism, transdiagnostic, unified protocol
Neuroticism is defined as the tendency to respond to various sources of stress with intense negative emotions (Barlow, 2002; Barlow, Ellard, Sauer-Zavala, Bullis, & Carl, 2014a, Barlow, Sauer-Zavala, Carl, Bullis, & Ellard, 2014b; Eysenck, 1947; Goldberg, 1993). The emotional experiences included within the neurotic spectrum include a range of negative effects (e.g. fear, irritability, anger, and sadness), with the greatest attention paid to anxious and depressive mood states. There is ample evidence to suggest that neuroticism is strongly associated with the onset of a number of mental and physical health conditions. Moreover, neuroticism is associated with other problematic outcomes (e.g. higher divorce rates, lost productivity, increased treatment seeking; Brickman, Yount, Blaney, Rothberg, & De-Nour, 1996; Clark, Watson, & Mineka, 1994; Khan, Jacobson, Gardner, Prescott, & Kendler, 2005; Krueger & Markon, 2006; Lahey, 2009; Sher & Trull, 1994; Smith & MacKenzie, 2006; Suls & Bunde, 2005; Weinstock & Whisman, 2006) over and above what can be explained by specific symptoms or formal psychiatric diagnoses. Given the public health significance of neuroticism, it is critical that we understand how best to alter it.
Malleability of neuroticism
Discrete conditions, such as the range of anxiety and depressive disorders, have long been the focus of intervention, rather than neuroticism, which has traditionally been considered more stable and inflexible (American Psychiatric Association, 2013). There is, however, increasing evidence that neuroticism may also change over time and in response to treatment. Several naturalistic, population-based studies suggest that neuroticism gradually decreases across the lifespan (Eaton, Krueger, & Oltmanns, 2011; Roberts & Mroczek, 2008; Roberts, Walton, & Viechtbauer, 2006) and may be influenced by life events (e.g. Roberts & Mroczek, 2008; Shiner, Allen, & Masten, 2017; Specht, Egloff, & Schmukle, 2011; Sutin, Costa, Wethington, & Eaton, 2010), though there appears to be great variability across individuals (Helson, Jones, & Kwan, 2002; Mroczek & Spiro, 2003; Small, Hertzog, Hultsch, & Dixon, 2003).
In addition to naturalistic fluctuations, neuroticism may also change as a direct result of psychiatric treatments. A recent meta-analysis observed moderate between group effects comparing various forms of active treatment, including cognitive behavioral therapy (CBT), to a no treatment control (Roberts et al., 2017). The authors of that study contend that greater change in neuroticism in the treatment group suggests the presence of intervention specific effects not attributable to changes in generalized distress or specific symptoms that are apt to fluctuate naturalistically in the control group (Clark, Vittengl, Kraft, & Jarrett, 2003; Jylhä & Isometsä, 2006; Widiger, Verheul, & van den Brink, 1999a, 1999b). But, the extent to which that is true depends on the degree of similarity between active and control treatments in altering symptomatic distress, and meta-analytic methods generally preclude the use of statistical techniques (e.g. Curran and Bauer, 2011; Fournier et al., 2019) to directly control for the role of symptoms when measuring change in neuroticism over time.
Additionally, whereas a meta-analysis can provide information about the average effect of a certain type of treatment (e.g. CBT), these methods ignore potentially important differences across studies. For example, when change in neuroticism has also been examined in the context of cognitive-behavioral interventions, results have been quite mixed. For example, some authors have found significant decreases in neuroticism following a course of CBT (e.g. Kring, Persons, and Thomas, 2007), whereas others have not observed such improvements (Davenport, Bore, & Campbell, 2010). In a large randomized-controlled trial (Tang et al., 2009), compared the effects of cognitive therapy (CT), selective serotonin reuptake inhibitors (SSRIs), and placebo on neuroticism in adults with major depressive disorder. Both CT and SSRIs resulted in significantly larger improvements in neuroticism than placebo, an effect that remained after controlling for changes in depressive symptoms for individuals in the SSRI condition, but not for those receiving CT. In contrast, the advantage of SSRIs over placebo on improvement for depressive symptoms was not maintained after controlling for neuroticism. These results suggest that SSRIs produce a specific effect on neuroticism and indicate that temperament and psychopathology can change independently. Additionally, they suggest that whereas depressive symptoms are responsive to placebo, neuroticism is not. Thus, one potential reason for the mixed literature with regard to whether cognitive-behavioral interventions reduce neuroticism is that all of the studies reviewed above featured treatments that were originally designed to target disorder-specific symptoms, rather than neuroticism itself. This raises the possibility that effective treatments for neuroticism may need to be tailored to more directly target this dimension.
Treatment of neuroticism
The Unified Protocol (UP) for Transdiagnostic Treatment of Emotional Disorders (Barlow et al. 2018a, 2018b) is a recently developed intervention with particular relevance for addressing neuroticism. The UP consists of several core treatment modules, described elsewhere (Payne, Ellard, Farchione, Fairholme, & Barlow, 2014) and summarized in Table 1, broadly aimed at extinguishing distress in response to the experience of strong emotions. By targeting aversive reactions to a wide variety of negative emotions when they occur, the UP may reduce reliance on the avoidant emotion regulation strategies that, paradoxically, have been shown to lead to more frequent and intense emotional experiences (Rassin, Muris, Schmidt, & Merckelbach, 2000; Wegner, Schneider, Carter, & White, 1987). Indeed, when negative emotions become less frequent over time, and when these changes are sustained, this may constitute decreases in neuroticism (for a description of what constitutes trait change, see Magidson, Roberts, Collado-Rodriguez, and Lejuez, 2014). The UP approach has shown efficacy in reducing symptoms for a range of anxiety and unipolar depressive disorders (Barlow et al., 2017; Boswell, Anderson, & Barlow, 2014; Ellard, Fairholme, Boisseau, Farchione, & Barlow, 2010; Farchione et al., 2012), and there is data to suggest that it exerts small to moderate effects on measures of neuroticism compared with a waitlist (WL) condition (Carl, Gallagher, Sauer-Zavala, Bentley, & Barlow, 2014).
Table 1.
UP core modules
| Topic name | Session | Main topics covered | Relevance for neuroticism |
|---|---|---|---|
| Mindful Emotion Awareness | 4–6 | Nonjudgmental awareness of thoughts, feelings, behaviors; Increasing present-focused attention toward emotional experiences; practice applying these skills in response to emotional experiences as they occur by anchoring in the present | Observing emotions nonjudgmentally allows patients to learn they are temporary, perhaps decreasing automatic emotional avoidance that exacerbates negative emotionality in the long term |
| Cognitive Flexibility | 5–8 | Reciprocal relationship between thoughts and emotions; strategies for questioning negative first impressions; generating alternative appraisals of emotion-eliciting situations | Directly challenging cognitions about emotions (i.e. ‘I’m weak to feel this way) may also decrease emotional avoidance, preventing rebound effects |
| Countering Emotional Behaviors | 6–10 | Emotions are associated with urges to engage in behaviors which may/may not be helpful in the short/long term; examples of unhelpful emotional behaviors for different emotions; engaging in alternative actions can lead to different emotional consequences | Deliberately engaging in behaviors that approach emotions, rather than avoid them, demonstrates to patients that emotions are not dangerous - again, reducing habitual avoidant coping |
| Tolerating Physical Sensations | 7–11 | Psychoeducation on the role that physical sensations play in emotional experiences is provided, patients engage in interoceptive exposures (e.g. breathing through a thin straw, hyperventilating) designed to deliberate bring on the physical sensations that are similar to what they experience in the context of strong emotions | Physical sensations contribute to the overall intensity of a subjective emotional experience and our appraisals of these sensations (i.e. ‘a racing heart is dangerous’) may increase the urgency to avoid emotional experiences |
| Emotion Exposures | 8–15 | Deliberately creating opportunities to face strong emotions in order facilitate new learning about emotions themselves (e.g. that they don’t last forever, that they can be tolerated); practicing previous skills in the context of an emotional experience | The goal of emotion exposures is to extinguish distress in response to emotional experiences, themselves, decreased aversive reactivity may reduce reliance on avoidant coping that ultimately exacerbates the frequency/intensity of emotional experiences |
Note: The label ‘core modules’ refers to skills included in the UP that are purported to decrease aversive/avoidant reactions to emotional experience. In addition to the five core modules listed here, the UP also includes an introductory session on the nature of emotional disorders/overview of treatment (session 1), a motivational enhancement/goal setting module (session 2), and a psychoeducation module on the adaptive nature of emotions (sessions 3–4), and a relapse prevention module (session 12 for patients with panic disorder and session 16 for patients with all other principal diagnoses). Given that the UP is delivered flexibly at the discretion of patients and clinicians, the core modules were delivered across 1–2 sessions, with the exception of emotion emotions exposures that occurred for at least 4 sessions. Thus, we are unable to definitively link modules to sessions, though we can generally determine when patients were likely to receive specific content.
It is important to note that the UP is a cognitive behavioral intervention and, as described above, the literature is mixed with regard to whether CBT exerts an effect on neuroticism. In contrast to more traditional CBT approaches that focus on coping with discrete symptom constellations, the UP may be more adept at targeting neuroticism by addressing aversive/avoidant reactions to a broader range of strong emotions. For example, gold-standard cognitive-behavioral approaches for panic disorder are aimed at extinguishing anxiety associated with physiological sensations during a panic episode, over time leading to a reduction of the physiological sensations themselves. The UP is also designed to lead to these improvements, but in addition, may help the patient to tolerate a wider range of negative emotions that arise across a variety of life circumstances. This broad potential to change patients’ relationship with their emotional experiences may allow for significant reductions in neuroticism. By contrast, standard disorder-focused CBT protocols, while efficacious for disorder symptoms, may not target a wide enough range of emotions to lead to robust changes in neuroticism.
Present study
The purpose of the present study is to add to the growing literature exploring the responsiveness of neuroticism to cognitive behavioral treatment generally, as well as to a transdiagnostic CBT protocol designed to target the broad array of negative emotional responses that characterize neuroticism. The present study utilized data from a large randomized-controlled trial comparing the UP to empirically supported single-diagnosis CBT protocols (SDPs), along with a WL control group, for diverse principal anxiety disorders and comorbid conditions (Barlow et al., 2017). First, with our large sample, we sought to replicate preliminary findings (see Carl et al., 2014) suggesting that the UP leads to significantly greater reductions in neuroticism compared to a WL control group. Additionally, we sought to explore the notion that changes in temperament, specifically neuroticism, are more robust when they are directly targeted in treatment. As a strict test of this hypothesis, we compared change in neuroticism as a function of active treatment condition and hypothesized that the UP would lead to greater changes in this dimension compared to disorder-specific, symptom-focused CBT protocols (SDP condition), all of which have established efficacy in treating symptoms. Given the evidence that some degree of change on measures of neuroticism reflects fluctuations in mood state, we examined change in neuroticism controlling for simultaneous changes in depression and anxiety symptoms.
Method
Participants
Participants in the present study were drawn from a large, intent-to-treat sample (N = 223) of treatment-seeking individuals who participated in a trial comparing two active treatment conditions and a WL control condition. The study was approved by a university institutional review board and written informed consent was obtained prior to any research activity. Individuals were eligible for the study if they were (1)18 years or older; (2) fluent in English; and (3) assigned a principal (most interfering and severe) diagnosis of panic disorder, with or without agoraphobia (PD/A), generalized anxiety disorder (GAD), obsessive-compulsive disorder (OCD), or social anxiety disorder (SOC; see Table 2). Most patients met the criteria for at least one comorbid diagnosis [188 (84.3%)] and the mean (s.d.) number of comorbid diagnoses was 2.3 (1.8); there were no differences in clinical severity or prevalence of comorbid disorders as a function of study condition (Barlow et al., 2017; Sauer-Zavala et al., 2020; Steele et al., 2018). Individuals taking psychotropic medications were required to have been stable on the same dose for at least 6 weeks prior to enrollment, and to maintain these medications and dosages throughout the treatment. Exclusion criteria consisted primarily of conditions that required immediate or simultaneous treatments that might interact with the study treatment in unknown ways (see Barlow et al., 2017).
Table 2.
Demographic and clinical characteristics
| Variable | UP (n = 88) | SDP (n = 91) | WL (n = 44) | F/χ 2 | p |
|---|---|---|---|---|---|
| Age, M (s.d.) | 30.95 (11.54) | 30.37 (10.03) | 32.68 (11.84) | 0.66 | 0.52 |
| White | 82.95% | 83.52% | 84.09% | 0.03 | 0.99 |
| Female | 54.55% | 56.04% | 56.82% | 0.07 | 0.96 |
| Married | 16.28% | 17.44% | 40.91% | 11.94 | 0.003 |
| Unemployed | 10.71% | 19.54% | 15.91% | 2.58 | 0.28 |
| Education (>12 years) | 81.18% | 92.05% | 95.45% | 7.65 | 0.02 |
| Principal diagnosis | 1.07 | 0.98 | |||
| Social phobia | 26.14% | 27.47% | 22.73% | ||
| Panic disorder | 28.41% | 24.18% | 27.27% | ||
| GAD | 25.00% | 29.67% | 29.55% | ||
| Obsessive compulsive disorder | 20.45% | 18.68% | 20.45% | ||
| Comorbid diagnoses | 0.69 | 0.71 | |||
| Any | 81.82% | 85.71% | 86.36% | ||
| Number | 2.22 | 2.32 | 2.36 | 0.12 | 0.89 |
| Taking medications | 55.29% | 58.89% | 48.84% | 1.19 | 0.55 |
UP, unified protocol; SDP, single-diagnosis protocols; WL, waitlist.
Measures
Diagnostic
The Anxiety Disorders Interview Schedule (ADIS; Brown & Barlow, 2014; Brown, Barlow, & DiNardo, 1994) is a semi-structured clinical interview that focuses on DSM diagnoses of anxiety, mood, somatic symptom, and substance use disorders, with screening questions for several additional disorders. Patients were assessed for current DSM diagnoses by individual evaluators who were blinded to condition allocation.
Neuroticism
The Eysenck Personality Questionnaire Revised-Short-Form (EPQR-S; Eysenck and Eysenck, 1975) is a commonly used 48-item inventory consisting of the following subscales: Extraversion, Neuroticism, Psychoticism, and a Lie Scale. This scale has been shown to have good reliability and excellent validity (Brown, 2007). The present study utilized the neuroticism subscale (12 items) and internal consistency at each assessment point was adequate (α ranged from 0.63 to 0.77). Example items include ‘are your feelings easily hurt’ and ‘would you call yourself a nervous person’ and respondents are prompted to select from either ‘yes’ or ‘no’.
Anxiety and depressive symptoms
The Hamilton Anxiety Ratings Scale (HARS; Hamilton, 1959) and Hamilton Depression Ratings Scale (HDRS; Hamilton, 1960) were used to provide clinician-rated assessment of anxiety and depressive symptoms, respectively. Both measures were administered in accordance with the Structured Interview Guide for the Hamilton Anxiety and Depression [SIGH-A (Shear et al., 2001), SIGH-D (Williams, 1988)]. These commonly used measures have demonstrated good levels of interrater and test–retest reliability, as well as convergent validity with similar clinician rated and self-report measures of psychiatric symptoms (Shear et al., 2001). Independent clinical evaluators received extensive training on the SIGH-A and SIGH-D and had to demonstrate acceptable levels of reliability prior to their participation in the trial.
Procedure
A detailed description of the procedures, including randomization and participant flow, can be found in Barlow et al. (2017). In short, patients were randomized by their principal diagnosis (PD/A, GAD, OCD, or SOC), following a 2:2:1 allocation ratio, to UP, SDP, and WL control study conditions, respectively. After a baseline diagnostic assessment and randomization, patients in the UP and SDP conditions received between 12 and 16, 50–90 min (see below) weekly individual treatment sessions. They completed assessment batteries that included clinician-rated and self-report measures at baseline, following sessions 4, 8, and 12, and 16.
Treatment
The Unified Protocol (UP; Barlow et al. 2018a, 2018b) is a transdiagnostic cognitive-behavioral intervention designed to address the range of anxiety, depressive, and related disorders. The UP consists of eight treatment modules that are described in more detail elsewhere (e.g. Payne et al., 2014). Treatment session length of the UP was matched to the SDPs for each principal diagnosis (in accordance with the guidelines described below). The SDPs adopted in the present study included: Mastery of Anxiety and Panic – 4th edition (MAP-IV; Craske and Barlow, 2006); Treating Your OCD with Exposure and Response (Ritual) Prevention Therapy – 2nd edition (Foa, Yadin, & Lichner, 2012); Mastery of Anxiety and Worry – 2nd edition (MAW-II; Zinbarg, Craske, and Barlow, 2006); and Managing Social Anxiety: A Cognitive-Behavioral Therapy Approach – 2nd edition (MSA-II; Hope, Heimberg, and Turk, 2010). As recommended by the treatment developers, the OCD, MSA, and MAW protocols were conducted over the course of 16 sessions, whereas the MAP-IV was conducted over 12 sessions. All treatments were administered independently, with treatment sessions lasting for approximately 50–60 min. An exception was the OCD treatment protocols, which lasted 80–90 min for both UP and SDP conditions.
Waitlist
Individuals in the WL control condition were asked to complete study assessments during a 16-week period, without receipt of study interventions. Following completion of their WL participation, patients in this condition were offered 16 sessions of treatment with the UP.
Therapists and treatment integrity
Therapists for the study consisted of doctoral students in clinical psychology, postdoctoral fellows, and licensed psychologists. Initial training and certification in the treatment protocols followed the procedures that had been employed in clinical trials at our center over the last 30 years (Barlow, Gorman, Shear, & Woods, 2000). The therapists were responsible for administering both UP and SDPs. Twenty percent of treatment sessions were randomly selected and sent to raters who were associated with the development of the specific treatments; these individuals rated study therapists for adherence and competence. Treatment fidelity scores were good to excellent (M, UP = 4.44 out of 5; SDPs = 4.09 out of 5).
Data analytic strategy
Our primary statistical analyses examined whether change in total neuroticism scores across the 16 weeks of active treatment differed among the treatment groups. Continuous data from the EPQ neuroticism scale were analyzed using multilevel models (MLMs, also known as hierarchical linear models or growth curve models) that adjusted for the repeated measures with nested random effects. Using this approach, each subject’s symptom trajectory and EPQ neuroticism score at week-16 was estimated from a collection of patient-specific parameters. To optimally model the pattern of change over time, we examined linear, log-transformed, square-root transformed, and quadratic change trajectories. The best fitting model, determined by sample size adjusted Akaike information criterion (AICc), was the quadratic representation of time (AICc = 3594.1, for all other models, AICc > 3605.7). As such, we focus our primary hypotheses on model-estimated neuroticism scores at the intercept, centered to represent scores at week-16 or the end of treatment. Intercepts and instantaneous slopes were included as random effects, and an unstructured covariance matrix estimated the correlation among them. Because the inclusion of a random quadratic term did not significantly improve model fit (χ2(3) = 6.90, p = 0.08), it was modeled as a fixed effect. All independent variables, including terms representing the effect of treatment and the covariates, were entered simultaneously at the appropriate model level (Raudenbush and Byrk). Full maximum likelihood estimation was used, and the degrees of freedom were estimated with the Kenward–Roger approximation. All analyses were performed using SAS Version 9.4 Proc Mixed (SAS Institute Inc., Cary, NC).
To identify potential confounds to our primary hypotheses, we examined whether the treatment groups differed on clinical and demographic characteristics using a liberal p value (p< 0.10) to identify potentially important covariates. Likewise, we examined each clinical and demographic characteristic in separate MLMs (one model for each) to determine whether it was associated with the week-16 neuroticism scores, instantaneous slopes, or quadratic change trajectories at p < 0.10. Any variable on which the groups differed or any variable associated with any of these model parameters was included as a covariate in all of the models described below.
The test of our primary hypothesis was conducted in two steps. First, across all three groups, we examined differences in model-estimated neuroticism scores at week-16, controlling for the covariates identified using the procedures above. We included the WL control group in this analysis to provide an estimate of neuroticism change over time in the absence of treatment. Next, in order to examine whether any observed differences in neuroticism scores at week-16 remained after controlling for changes over time in anxiety and depression, we repeated the models above, adding measures of anxiety and depression as time varying covariates. In these models, we controlled for both mean levels of depression and anxiety over the acute phase of treatment, as well as assessment-to-assessment fluctuations in depression and anxiety levels over the treatment period (Curran & Bauer, 2011). Given the complexity of these latter models and given the smaller sample size in the WL condition, only the two active treatments, UP and SDP, were compared in this second step.
Results
Demographic and clinical measures
Table 2 displays demographic and clinical measures at baseline for the UP, SDP, and WL groups. The three groups differed with respect to the proportion of patients who were married, with the WL group containing the highest percentage, and in the proportion of participants who had received at least some college education, with the UP group containing the lowest percentage. The groups did not differ regarding any of the remaining variables at baseline.
Separate MLMs were used to screen the relationship between the baseline demographic and clinical variables and parameters representing change in neuroticism scores across treatment. Participant age was associated with instantaneous slopes at week-16 (F(1,665) = 4.38, p = 0.04) and with the quadratic term representing the curvature of the trajectory (F(1,538) = 4.62, p = 0.03); unemployment was associated with the quadratic term at the level of a non-significant trend (F(1,507) = 2.99, p = 0.08, see full model results in online Supplementary Table S1). As such, these four variables (marital status, education level, age, and unemployment) were included as covariates in models testing our primary hypotheses.
Change in neuroticism in the three treatment groups
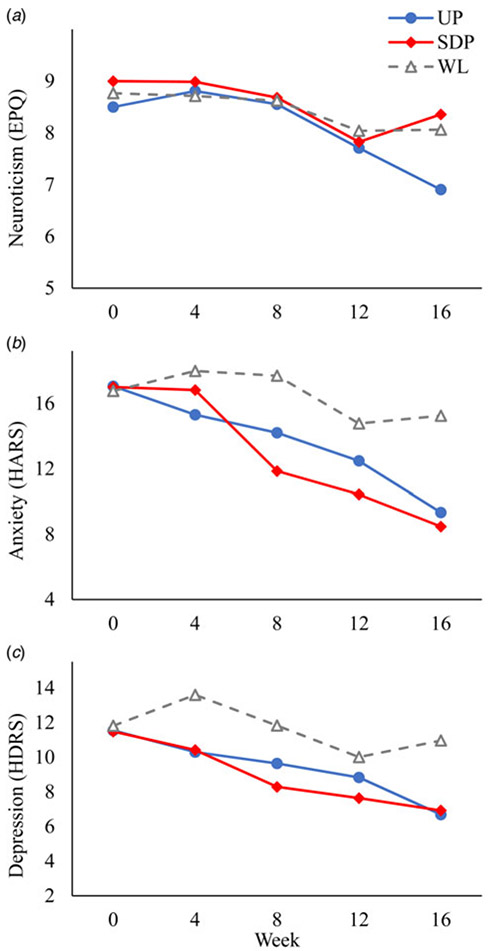
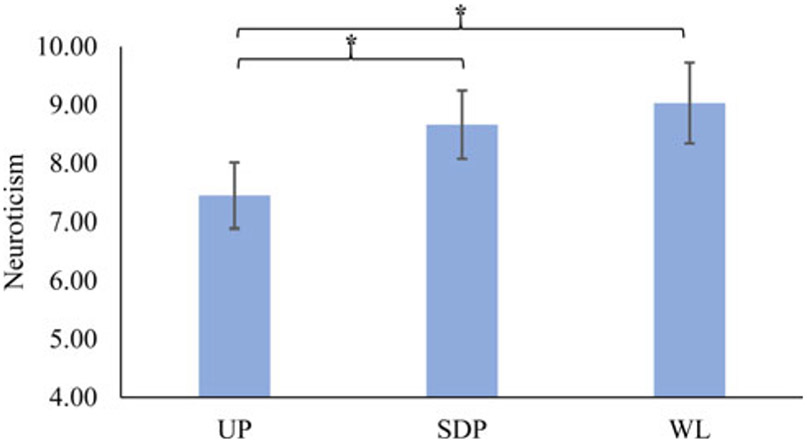
Table 3 presents the parameters from the MLM of change in EPQ neuroticism scores over time and Fig. 1 displays the raw means at each assessment point for EPQ neuroticism, HARS, and HDRS, separately for each treatment. We observed no differences among the treatments at baseline on neuroticism (F(2,216) = 0.81, p = 0.45), HARS (F(2,220) = 0.02, p = 0.98), or HDRS (F(2,220) = 0.04, all p = 0.96). The primary statistic of interest in the MLM was the effect of treatment on estimated neuroticism scores at the week-16, controlling for the above covariates. We observed a significant main effect of treatment (F(2,213) = 3.57, p = 0.03, Table 3, Fig. 2) such that the UP group evidenced lower week-16 neuroticism scores than either the SDP [t(218) = −2.17, p = 0.03, d = −0.32, 95% confidence interval (CI) −0.62 to −0.03] or the WL (t(207) = −2.33, p = 0.02, d = −0.43, 95% CI −0.80 to −0.07) groups. We observed no difference in week-16 neuroticism scores between the SDP and WL groups (t(212) = −0.55, p = 0.58, d = −0.10, 95% CI −0.46 to 0.26).
Table 3.
MLM of changes in neuroticism over 16 weeks
| Effect | Beta (s.e.) | df | t/F value | p |
|---|---|---|---|---|
| Week-16 neuroticism scores (primary outcome of interest) | ||||
| Intercept | 9.03 (0.69) | 217 | 13.06 | <0.0001 |
| Age | −0.03 (0.03) | 229 | −0.97 | 0.33 |
| Married | 0.82 (0.67) | 213 | 1.22 | 0.22 |
| Unemployed | 0.15 (0.69) | 218 | 0.22 | 0.83 |
| Education (>12 years) | −1.05 (0.81) | 212 | −1.30 | 0.20 |
| Treatment | 2,213 | 3.57 | 0.03 | |
| UP v. WL | −1.58 (0.68) | 207 | −2.33 | 0.02 |
| SDP v. WL | −0.37 (0.67) | 212 | −0.55 | 0.58 |
| Instantaneous slope at week-16 | ||||
| Instantaneous slope | 0.11 (0.09) | 619 | 1.24 | 0.22 |
| Age | 0.01 (0.003) | 626 | 1.79 | 0.07 |
| Married | −0.01 (0.08) | 619 | −0.08 | 0.93 |
| Unemployed | 0.06 (0.08) | 621 | 0.75 | 0.45 |
| Education (>12 years) | −0.16 (0.09) | 618 | −1.75 | 0.08 |
| Treatment | 2,619 | 12.40 | <0.0001 | |
| UP v. WL | −0.36 (0.08) | 614 | −4.35 | <0.0001 |
| SDP v. WL | −0.10 (0.08) | 619 | −1.16 | 0.25 |
| Quadratic trajectory | ||||
| Quadratic trajectory | 0.007 (0.005) | 491 | 1.47 | 0.14 |
| Age | 0.0004 (0.0002) | 513 | 2.09 | 0.04 |
| Married | −0.003 (0.004) | 489 | −0.61 | 0.54 |
| Unemployed | 0.005 (0.005) | 498 | 1.06 | 0.29 |
| Education (>12 years) | −0.007 (0.005) | 473 | −1.39 | 0.17 |
| Treatment | 2,494 | 10.02 | <0.0001 | |
| UP v. WL | −0.017 (0.005) | 488 | −3.71 | 0.0002 |
| SDP v. WL | −0.003 (0.005) | 495 | −0.74 | 0.46 |
UP, unified protocol; SDP, single-disorder protocols; WL, waitlist.
Fig. 1.
Raw mean (a) neuroticism, (b) anxiety, and (c) depression scores in each treatment at each assessment week.
Fig. 2.
Estimated neuroticism scores at week-16. Error bars represent ±1 s.e. UP, unified protocol; SDP, single-disorder protocols; WL, waitlist. *p <0.05.
Change in neuroticism in the two active treatment arms, controlling for symptoms
In a separate model, we examined differences in week-16 neuroticism scores between the UP and SDP conditions controlling for mean level and fluctuations in depression and anxiety over the trial. First, we observed a significant between-subjects effect of average depression on estimated neuroticism levels at week-16 such that individuals with higher mean levels of depression had higher post-treatment neuroticism scores (F(1,191) = 9.35, p = 0.003). We observed no effect of fluctuations in depression scores over the trial on neuroticism scores (F(1,487) = 0.78, p = 0.38). By contrast, we observed a significant association between fluctuations in anxiety levels and neuroticism scores whereby increased levels of anxiety, relative to an individual’s mean, were associated with increases in neuroticism scores (F(1,516) = 50.47, p < 0.001). The effect of between-participant differences in mean anxiety on week-16 neuroticism scores was not significant (F(1,197) = 0.69, p = 0.41). Critically, the main effect of treatment on week-16 neuroticism remained significant when controlling for all of these effects and for the covariates identified above,†,1 such that week-16 neuroticism scores were lower in the UP than the SDP groups (F(1,176) = 7.72, p = 0.006, d = −0.42, 95% CI −0.71 to −0.12; full model results are presented in online Supplementary Table S2).2
Discussion
The current study is the first of its kind to compare different, active behavioral treatments with respect to their effect on neuroticism. Results suggest that the UP, a transdiagnostic intervention designed to target the broad array of negative emotional reactions, was associated with significant reductions in this dimension in a treatment-seeking sample of individuals with heterogeneous anxiety disorders and comorbid conditions. Notably, patients in the UP condition evidenced lower levels of neuroticism at week-16 (post-treatment) than did those in the SDP and WL conditions. Further, no differences were seen between the SDP and WL conditions on neuroticism scores at week-16, indicating that gold-standard, symptom-focused approaches may not provide an advantage over no treatment (i.e. WL) in targeting this dimension, despite the advantage of these approaches over WL in targeting symptoms (Barlow et al., 2017). Of note, the greatest divergence among UP and SDP treatments in the trajectories of change in neuroticism occurred during the final four sessions. At this point in the study, all patients were engaging in exposures, but the focus of these exercises differed across conditions. The goal of exposure in the SDPs is to extinguish distress in response to specific fear-eliciting situations (e.g. public speaking and contamination), whereas in the UP condition, the focus is on facilitating new learning about emotions themselves (e.g. emotions are temporary and tolerable) regardless of situation. The UP may reduce neuroticism to a greater extent due to its focus on exposure to a broad array of negative emotions across situations, as opposed to the situation specific focus of SDPs. But, future research would be necessary to clarify the mechanisms underlying the unique effect of specific UP treatment components on neuroticism.
Additionally, despite significant symptom improvement observed across both active treatment conditions, fluctuations in depression and anxiety do not appear to account for changes in neuroticism in this sample. Specifically, we simultaneously controlled for average levels of depression and anxiety across treatment, as well fluctuations in these symptoms, and the UP condition continued to show significantly lower neuroticism scores at week-16 compared to the SDP condition. Together, these findings provide evidence that neuroticism may be most apt to change in treatment when it is directly targeted. Given that symptoms improved in both active treatment conditions, yet reductions in neuroticism were only observed for the UP condition, it is worth considering the clinical significance of a treatment that can address both acute disorder symptoms and temperamental vulnerabilities. Future research should explore whether change in neuroticism leads to functional improvements related a wide range emotional experience (i.e. tolerating anger in a romantic relationship), beyond the circumscribed emotional/situational impairments that abate in disorder-specific CBT in the short term. Additional work can examine whether reductions in neuroticism prevent the emergence of future emotional disorders that are also characterized by aversive, avoidant responses to strong emotions.
The current findings add to the existing body of literature aimed at addressing whether temperamental variables, such as neuroticism, are responsive to treatment efforts. First, consistent with Tang et al.’s (2009) results, we found that neuroticism and psychopathology (i.e. depression and anxiety) are not isomorphic and can change independently. Additionally, though evidence of neuroticism’s sensitivity to change in the context of previous treatment outcome trials has been mixed (Eaton et al., 2011; Kring et al., 2007; Tang et al., 2009), by comparing emotion-focused (UP) and traditional CBT (SDP) approaches, the present study suggests that more robust effects are demonstrated when neuroticism is targeted more directly. Moreover, the present study extends the meta-analytic work of Roberts et al. (2017). Our between condition effects comparing the UP to WLC were similar to Roberts’ estimates exploring differences in the magnitude of neuroticism change between treatment in general (any orientation) and a no-treatment condition; however, the present study provides an even more stringent evaluation by explicitly controlling for fluctuations in depression and anxiety, along with directly comparing the UP to other effective CBT approaches. Regarding these comparisons, we observed an advantage of the UP over the other CBT approaches for the reduction of neuroticism that is similar to the effect-size differences reported between active medications and placebo in the treatment of depressive symptoms (Turner et al., 2008). Given that emerging dimensional models of psychopathology include additional broad domains, beyond neuroticism, that can account for the full range of mental disorders (e.g. Kotov et al., 2017), it is important for future research to explore whether additional personality dimensions are also amenable to change in response to targeted treatments.
Limitations of the current study warrant mention. First, the treatments evaluated in the current study were developed at our center (three of the four SDPs and the UP) and were delivered by providers with strong CBT training. This limitation may impact generalizability of study results to other locations and patient populations. Additionally, the majority of the work addressing neuroticism’s responsiveness to treatment has been conducted in the context of major depressive disorder (Tang et al., 2009); the present sample consisted of individuals with principal anxiety disorders and, although a subset were also diagnosed with a comorbid depressive disorder, it is unclear whether results will generalize to individuals with primary depression (n = 31, see Sauer-Zavala et al., 2020). Additionally, it would also be useful for future research to include more frequent assessment of neuroticism and symptom levels to elucidate the relative timing of changes in these features during treatment, along with larger samples and longer follow-up periods in which return to treatment was carefully controlled. These features would allow for the kinds of measurement models that can better disentangle state/trait effects over time (Fournier et al., 2019), and they would allow for the determination of the relative durability of neuroticism changes with treatment.
Conclusions
Given that neuroticism is associated with a wide range of public health problems, interventions that target this dimension in treatment may have far reaching effects. The current study demonstrates that the UP has a specific effect on change in neuroticism relative to other active CBT treatments. These findings shed light on the mixed literature with regard to neuroticism’s treatment responsiveness; by directly comparing neuroticism-focused CBT (i.e. UP) to more traditional approaches, results suggest that improvements in neuroticism are more robust when it is directly targeted in treatment.
Supplementary Material
Acknowledgments
Financial support. This study was funded by grant R01 MH090053 from the National Institute of Mental Health awarded to Dr David H. Barlow.
Footnotes
Supplementary material. The supplementary material for this article can be found at https://doi.org/10.1017/S0033291720000975.
Conflict of interest. Dr Barlow receives royalties from Oxford University Press (which includes royalties for all five treatment manuals included in this study), Guilford Publications Inc., Cengage Learning, and Pearson Publishing. Dr Fournier receives royalties from Guilford Publications Inc. There are no disclosures for the remaining authors.
Ethical standards. The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
In separate analyses, we utilized the procedure suggested by Curran and Bauer whereby linear trends in the time-varying covariates were removed first using ordinary least squares methods and the residuals from these modes were used to represent the within-person effects. The results of this approach were quite similar to those reported in the main text, and the effects of treatment on estimated post-treatment neuroticism scores remained significant (F(1,171) = 5.73, p = 0.02).
We conducted three additional tests to determine whether the observed treatment differences in neuroticism change were driven by symptomatic fluctuations. First, to the time-varying covariate model examining change in HARS (anxiety) and HDRS (depression) symptoms over the trial, we added two additional time-varying symptom covariates, one assessing anxiety symptoms [Overall Anxiety Severity and Interference Scale (OASIS); Norman, Hami Cissell, Means-Christensen, & Stein, 2006] and one assessing depression symptoms [Overall Depression Severity and Interference Scale (ODSIS); Bentley, Gallagher, Carl, & Barlow, 2014]. As with the HARS and HRDS, the mean levels of these variables were added to the model, as were the session-by-session fluctuations. As above, treatment with the UP was associated with lower neuroticism scores at week-16 than was SDP (F(1,186) = 5.57, p = 0.02, d = −0.35, 95% CI −0.65 to −0.06), controlling for the baseline covariates listed above and these four time-varying symptom scores. Next, we estimated change in each of the four symptom measures (HAS, HDS, OASIS, and ODSIS) separately by estimating separate MLMs for each symptom measure (as the DV), using the baseline covariates as above, the effect of time, and the effect of treatment, allowing for random intercepts and slopes. From these models, we estimated individualized Best Linear Unbiased Predictions of baseline and week-16 scores for each symptom, and calculated an individualized estimate of pre-post treatment change. These four estimated depression and anxiety change scores were added to the primary model examining change in neuroticism between UP and SDP, along with the baseline covariates. Again, UP was associated with reduced neuroticism scores compared to SDP at week-16, simultaneously controlling for estimated pre-post change in the four symptom scores (F(1,177) = 16.08, p < 0.001, d = −0.60, 95% CI −0.90 to −0.30). As a final and strict test of whether UP versus SDP treatment assignment could explain incremental variance in week-16 neuroticism scores once the influence of all covariates including changing symptoms and the passage of time had first been removed, we estimated residual 16 week neuroticism scores from an MLM of neuroticism scores over time that consisted of the baseline covariates, the four time-varying symptoms covariates, and the linear and quadratic effects of time, with random effects as above. We observed a significant effect of treatment (F(1,109) = 8.27, p = 0.005, d = −0.55, 95% CI −0.93 to −0.17) on these residualized week-16 neuroticism scores whereby UP was associated with lower scores than was SDP.
The notes appear after the main text.
References
- American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders (DSM-5) (5th ed). Arlington, VA: APA. [Google Scholar]
- Barlow DH (2002). Anxiety and its disorders: The nature and treatment of anxiety and panic. New York, NY: Guilford Press. [Google Scholar]
- Barlow DH, Ellard KK, Sauer-Zavala S, Bullis JR, & Carl JR (2014a). The origins of neuroticism. Perspectives on Psychological Science, 9, 481–496. [DOI] [PubMed] [Google Scholar]
- Barlow DH, Farchione TJ, Bullis JR, Gallagher MW, Murray-Latin H, Sauer-Zavala S, … Cassiello-Robbins C (2017). The unified protocol for transdiagnostic treatment of emotional disorders compared with diagnosis-specific protocols for anxiety disorders: A randomized clinical trial. JAMA Psychiatry, 74, 875–884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barlow DH, Farchione TJ, Sauer-Zavala S, Murray Latin H, Ellard KK, Bullis JR, … Cassiello-Robbins C (2018a). Unified protocol for the transdiagnostic treatment of emotional disorders: Therapist guide (2nd edn). New York, NY: Oxford University Press. [Google Scholar]
- Barlow DH, Gorman JM, Shear MK& Woods SW (2000). Cognitive-behavioral therapy, imipramine, or their combination for panic disorder: A randomized controlled trial. JAMA, 283, 2529–2536. [DOI] [PubMed] [Google Scholar]
- Barlow DH, Sauer-Zavala S, Carl JR, Bullis JR, & Ellard KK, (2014b). The nature, diagnosis, and treatment of neuroticism: Back to the future. Clinical Psychological Science, 2, 344–365. [Google Scholar]
- Barlow DH, Sauer-Zavala S, Farchione TJ, Murray Latin H, Ellard KK, Bullis JR, … Cassiello-Robbins C (2018b). Unified protocol for the transdiagnostic treatment of emotional disorders: Patient workbook (2nd edn). New York, NY: Oxford University Press. [Google Scholar]
- Bentley KH, Gallagher MW, Carl JR, & Barlow DH (2014). Development and validation of the overall depression severity and impairment scale. Psychological Assessment, 26, 815–830. [DOI] [PubMed] [Google Scholar]
- Boswell JF, Anderson LM, & Barlow DH (2014). An idiographic analysis of change processes in the unified transdiagnostic treatment of depression. Journal of Consulting and Clinical Psychology, 82, 1060. [DOI] [PubMed] [Google Scholar]
- Brickman AL, Yount SE, Blaney NT, Rothberg ST, & De-Nour AK (1996). Personality traits and long-term health: Status the influence of neuroticism and conscientiousness on renal deterioration in type-1 diabetes. Psychosomatics, 37, 459–468. [DOI] [PubMed] [Google Scholar]
- Brown TA (2007). Temporal course and structural relationships among dimensions of temperament and DSM-IV anxiety and mood disorder constructs. Journal of Abnormal Psychology, 116, 313. [DOI] [PubMed] [Google Scholar]
- Brown TA, & Barlow DH (2014). Anxiety and related disorders interview schedule for DSM-5 (ADIS-5L): Lifetime version. Client interview schedule. New York, NY: Oxford University Press. [Google Scholar]
- Brown TA, Barlow DH, & DiNardo PA (1994). Anxiety disorders interview schedule for DSM-IV (ADIS-IV): Client interview schedule. Albany, NY: Graywind Publications Incorporated. [Google Scholar]
- Carl JR, Gallagher MW, Sauer-Zavala SE, Bentley KH, & Barlow DH (2014). A preliminary investigation of the effects of the unified protocol on temperament. Comprehensive Psychiatry, 55, 1426–1434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark LA, Vittengl J, Kraft D, & Jarrett RB (2003). Separate personality traits from states to predict depression. Journal of Personality Disorders, 17, 152–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark LA, Watson D, & Mineka S (1994). Temperament, personality, and the mood and anxiety disorders. Journal of Abnormal Psychology, 103, 103. [PubMed] [Google Scholar]
- Craske MG, & Barlow DH (2006). Mastery of your anxiety and panic: Therapist guide. New York, NY: Oxford University Press. [Google Scholar]
- Curran PJ, & Bauer DJ (2011). The disaggregation of within-person and between-person effects in longitudinal models of change. Annual Review of Psychology, 62, 583–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davenport J, Bore M, & Campbell J (2010). Changes in personality in pre- and post-dialectical behaviour therapy borderline personality disorder groups: A question of self-control. Australian Psychologist, 45, 59–66. [Google Scholar]
- Eaton NR, Krueger RF, & Oltmanns TF (2011). Aging and the structure and long-term stability of the internalizing spectrum of personality and psychopathology. Psychology and Aging, 26, 987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellard KK, Deckersbach T, Sylvia LG, Nierenberg AA, & Barlow DH (2012). Transdiagnostic treatment of bipolar disorder and comorbid anxiety with the unified protocol: A clinical replication series. Behavior Modification, 36, 482–508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellard KK, Fairholme CP, Boisseau CL, Farchione TJ, & Barlow DH (2010). Unified protocol for the transdiagnostic treatment of emotional disorders: Protocol development and initial outcome data. Cognitive and Behavioral Practice, 17, 88–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eysenck HJ (1947). Dimensions of personality. London, UK: Routledge & Paul. [Google Scholar]
- Eysenck HJ, & Eysenck SBG (1975). Manual of the Eysenck personality questionnaire (junior and adult). London, UK: Hodder and Stoughton. [Google Scholar]
- Farchione TJ, Fairholme CP, Ellard KK, Boisseau CL, Thompson-Hollands J, Carl JR, … Barlow DH (2012). Unified protocol for transdiagnostic treatment of emotional disorders: A randomized controlled trial. Behavior Therapy, 43, 666–678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foa EB, Yadin E, & Lichner TK (2012). Treating your OCD with exposure and response (ritual) prevention workbook. New York, NY: Oxford University Press. [Google Scholar]
- Fournier JC, Wright A, Tackett JL, Uliaszek A, Pilkonis PA, Manuck SB, & Bagby RM (2019). Decoupling personality and acute psychiatric symptoms in a depressed and a community sample. Clinical Psychological Science, 7, 566–581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg LR (1993). The structure of phenotypic personality traits. American Psychologist, 48(1), 26–34. 10.1037/0003-066X.48.1.26 [DOI] [PubMed] [Google Scholar]
- Hamilton M (1959). The assessment of anxiety states by rating. British Journal of Medical Psychology, 32, 50–55. [DOI] [PubMed] [Google Scholar]
- Hamilton M (1960). A rating scale for depression. Journal of Neurology, Neurosurgery, and Psychiatry, 23, 56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helson R, Jones C, & Kwan VS (2002). Personality change over 40 years of adulthood: Hierarchical linear modeling analyses of two longitudinal samples. Journal of Personality and Social Psychology, 83, 752. [PubMed] [Google Scholar]
- Hope DA, Heimberg RG, & Turk CL (2010). Managing social anxiety: A cognitive-behavioral therapy approach. New York, NY: Oxford University Press. [Google Scholar]
- Jylhä P, & Isometsä E (2006). The relationship of neuroticism and extraversion to symptoms of anxiety and depression in the general population. Depression and Anxiety, 23, 281–289. [DOI] [PubMed] [Google Scholar]
- Khan AA, Jacobson KC, Gardner CO, Prescott CA, & Kendler KS (2005). Personality and comorbidity of common psychiatric disorders. The British Journal of Psychiatry, 186, 190–196. [DOI] [PubMed] [Google Scholar]
- Kotov R, Krueger RF, Watson D, Achenbach TM, Althoff RR, Bagby MR, … Zimmerman M (2017). The hierarchical taxonomy of psychopathology (HiTOP): A dimensional alternative to traditional nosologies. Journal of Abnormal Psychology, 126, 454–477. [DOI] [PubMed] [Google Scholar]
- Kring AM, Persons JB, & Thomas C (2007). Changes in affect during treatment for depression and anxiety. Behaviour Research and Therapy, 45, 1753–1764. [DOI] [PubMed] [Google Scholar]
- Krueger RF, & Markon KE (2006). Reinterpreting comorbidity: A model-based approach to understanding and classifying psychopathology. Annual Review of Clinical Psychology, 2, 111–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey BB (2009). Public health significance of neuroticism. The American Psychologist, 64, 241–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magidson JF, Roberts B, Collado-Rodriguez A, & Lejuez CW (2014). Theory-driven intervention for changing personality: Expectancy value theory, behavioral activation, and conscientiousness. Developmental Psychology, 50, 1442–1450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mroczek DK, & Spiro A III. (2003). Modeling intraindividual change in personality traits: Findings from the normative aging study. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 58, P153–P165. [DOI] [PubMed] [Google Scholar]
- Norman SB, Hami Cissell S, Means-Christensen AJ, & Stein MB (2006). Development and validation of an overall anxiety severity and impairment scale (OASIS). Depression and Anxiety, 23, 245–249. [DOI] [PubMed] [Google Scholar]
- Payne LA, Ellard KK, Farchione TJ, Fairholme CP, & Barlow DH (2014). Emotional disorders: A unified transdiagnostic protocol. In Barlow DH (ed.), Clinical handbook of psychological disorders: A step-by-step treatment manual (5th ed). New York, NY: Guilford Press. [Google Scholar]
- Rassin E, Muris P, Schmidt H, & Merckelbach H (2000). Relationships between thought–action fusion, thought suppression and obsessive–compulsive symptoms: A structural equation modeling approach. Behaviour Research and Therapy, 38, 889–897. [DOI] [PubMed] [Google Scholar]
- Roberts BW, Luo J, Briley DA, Chow PI, Su R, & Hill PL (2017). A systematic review of personality trait change through intervention. Psychological Bulletin, 143, 117–141. [DOI] [PubMed] [Google Scholar]
- Roberts BW, & Mroczek D (2008). Personality trait change in adulthood. Current Directions in Psychological Science, 17, 31–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts BW, Walton KE, & Viechtbauer W (2006). Patterns of mean-level change in personality traits across the life course: A meta-analysis of longitudinal studies. Psychological Bulletin, 132, 1. [DOI] [PubMed] [Google Scholar]
- Sauer-Zavala S, Bentley KH, Steele SJ, Tirpak JW, Ametaj AA, Nauphal M, & Barlow DH (2020). A preliminary randomized evaluation. Journal of Affective Disorders, 264, 438–445. 10.1016/j.jad.2019.11.072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sauer-Zavala S, Boswell JF, Gallagher MW, Bentley KH, Ametaj A, & Barlow DH (2012). The role of negative affectivity and negative reactivity to emotions in predicting outcomes in the unified protocol for the transdiagnostic treatment of emotional disorders. Behaviour Research and Therapy, 50, 551–557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sauer-Zavala S, Gutner CA, Farchione TJ, Boettcher HT, Bullis JR, & Barlow DH (2017). Current definitions of ‘transdiagnostic’ in treatment development: A search for consensus. Behavior Therapy, 48, 128–138. [DOI] [PubMed] [Google Scholar]
- Shear MK, Vander Bilt J, Rucci P, Endicott J, Lydiard B, Otto MW, … others (2001). Reliability and validity of a structured interview guide for the Hamilton Anxiety Rating Scale (SIGH-A). Depression and Anxiety, 13,166–178. [PubMed] [Google Scholar]
- Sher KJ, & Trull TJ (1994). Personality and disinhibitory psychopathology: Alcoholism and antisocial personality disorder. Journal of Abnormal Psychology, 103, 92. [DOI] [PubMed] [Google Scholar]
- Shiner RL, Allen TA, & Masten AS (2017). Adversity in adolescence predicts personality trait change from childhood to adulthood. Journal of Research in Personality, 67, 171–182. [Google Scholar]
- Small BJ, Hertzog C, Hultsch DF, & Dixon RA (2003). Stability and change in adult personality over 6 years: Findings from the Victoria Longitudinal Study. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 58, P166–P176. [DOI] [PubMed] [Google Scholar]
- Smith TW, & MacKenzie J (2006). Personality and risk of physical illness. Annual Review of Clinical Psychology, 2, 435–467. [DOI] [PubMed] [Google Scholar]
- Specht J, Egloff B, & Schmukle SC (2011). Stability and change of personality across the life course: The impact of age and major life events on mean-level and rank-order stability of the big five. Journal of Personality and Social Psychology, 101, 862–882. [DOI] [PubMed] [Google Scholar]
- Steele SJ, Farchione TJ, Cassiello-Robbins C, Ametaj A, Sbi S, Sauer-Zavala S, & Barlow DH (2018). Efficacy of the Unified Protocol for transdiagnostic treatment of comorbid psychopathology accompanying emotional disorders compared to treatments targeting single disorders. Journal of psychiatric research, 104, 211–216. 10.1016/j.jpsychires.2018.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suls J, & Bunde J (2005). Anger, anxiety, and depression as risk factors for cardiovascular disease: The problems and implications of overlapping affective dispositions. Psychological Bulletin, 131, 260. [DOI] [PubMed] [Google Scholar]
- Sutin AR, Costa PT, Wethington E, & Eaton W (2010). Turning points and lessons learned: Stressful life events and personality trait development across middle adulthood. Psychology and Aging, 25, 524–533. [DOI] [PubMed] [Google Scholar]
- Tang TZ, DeRubeis RJ, Hollon SD, Amsterdam J, Shelton R, & Schalet B (2009). A placebo-controlled test of the effects of paroxetine and cognitive therapy on personality risk factors in depression. Archives of General Psychiatry, 66, 1322–1330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wegner DM, Schneider DJ, Carter SR, & White TL (1987). Paradoxical effects of thought suppression. Journal of Personality and Social Psychology, 53, 5. [DOI] [PubMed] [Google Scholar]
- Weinstock LM, & Whisman MA (2006). Neuroticism as a common feature of the depressive and anxiety disorders: A test of the revised integrative hierarchical model in a national sample. Journal of Abnormal Psychology, 115,68. [DOI] [PubMed] [Google Scholar]
- Widiger TA, Verheul R, & van den Brink W (1999a). Handbook of personality: Theory and research. New York, NY: Guilford Press. [Google Scholar]
- Widiger TA, Verheul R, & van den Brink W (1999b). Personality and psychopathology. In Pervin LA, & John OP (Eds.), Handbook of personality: Theory and research (2nd ed, pp. 347–366). New York, NY: Guilford Press. [Google Scholar]
- Williams JB (1988). A structured interview guide for the Hamilton Depression Rating Scale. Archives of General Psychiatry, 45, 742–747. [DOI] [PubMed] [Google Scholar]
- Zinbarg RE, Craske MG, & Barlow DH (2006). Mastery of your anxiety and worry (MAW): Therapist guide. New York, NY: Oxford University Press. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.