Abstract
Background:
High psychological readiness is an important element for returning to sports after anterior cruciate ligament (ACL) reconstruction. Identifying factors that contribute to psychological readiness is essential for planning interventions to return to play. No studies have used multivariate analysis to clarify factors associated with psychological readiness to return to specific sports.
Hypothesis:
To identify factors that contribute to an athlete’s psychological readiness to return after ACL reconstruction to sports that require cutting, pivoting, and jump-landings.
Study Design:
Cross-sectional study; Level of evidence, 3.
Methods:
Study participants were athletes who before injury had participated in sports with limited contact that required cutting, pivoting, and jump-landings (basketball, soccer, futsal, volleyball, badminton, tennis, and frisbee) and hoped to return to the same sport after reconstruction. Psychological readiness was measured using the Anterior Cruciate Ligament–Return to Sport After Injury Scale (ACL-RSI) in athletes more than 6 months after primary ACL reconstruction. To clarify factors associated with the ACL-RSI, univariate regression analysis and multivariate regression analysis were performed using the following independent variables: age, sex, body mass index, time from injury to reconstruction, time from reconstruction to testing, meniscal surgery, modified Tegner activity scale before injury, kinesiophobia, limb symmetry index of knee strength, limb symmetry indices of single-leg hop (SLH) distances, and subjective running ability.
Results:
Higher subjective running ability, a lower kinesiophobia score, and greater limb symmetry in the lateral SLH were positively associated with psychological readiness.
Conclusion:
The psychological readiness of athletes aiming to return after ACL reconstruction to limited-contact sports that require cutting, pivoting, and jump-landings was affected by subjective running ability, kinesiophobia, and asymmetry of lateral SLH distance. This information may be useful in planning appropriate interventions and thereby increasing the likelihood of an athlete’s returning to such sports.
Keywords: ACL-RSI, sport type, return to play
Primary and secondary anterior cruciate ligament (ACL) injuries tend to occur in athletes who participate in sports that require cutting, pivoting, and jump-landings, such as basketball, soccer, volleyball, and badminton.1,19,23,24 Many athletes who have damaged their ACLs have undergone reconstruction and long-term postoperative rehabilitation to improve knee function and performance and to return to the sport they were involved in before the injury.13 However, only 44% to 63% of athletes are able to return to their sport.3
Emotions, confidence, and risk appraisal, that is, psychological readiness, contribute to the ability to return to sport after ACL reconstruction.26 Webster and colleagues26 developed an Anterior Cruciate Ligament–Return to Sport After Injury Scale (ACL-RSI) to quantify the state of psychological readiness during recovery after ACL reconstruction. The ACL-RSI has a high internal consistency and good structural validity as examined using the Tampa Scale for Kinesiophobia (TSK), International Knee Documentary Committee (IKDC) Subjective Knee Form, and Knee injury and Osteoarthritis Outcome Score (KOOS).2,26
The ACL-RSI score in athletes postreconstruction is related to whether they can return to the sport they participated in before injury.2,14,26,27 Athletes who were able to return to their preinjury sport have displayed higher scores compared with those who were unable to return,2 and lower ACL-RSI scores have been associated with the occurrence of secondary injury after ACL reconstruction.17,18 These reports show that increasing the psychological readiness for return is an important element for returning to a sport after injury.
Information about specific factors that contribute to psychological readiness is needed to plan appropriate interventions and increase the likelihood of an athlete’s returning to play. In a study of 635 patients after primary ACL reconstruction, Webster et al28 evaluated the association between the ACL-RSI score and the following independent variables: patient characteristics, sports participation, anterior single-leg hop (SLH), subjective physical function, and postoperative elapsed time. However, that study did not include data on sport type, knee strength, lateral SLH, or running ability.
The purpose of this study was to identify factors that influence psychological readiness to return to sports specifically requiring cutting, pivoting, and jump-landings after primary ACL reconstruction. Patient characteristics, sports activity level, sports participation time, surgical timing, time from reconstruction, knee strength, objective and subjective functional measures, and kinesiophobia were evaluated and analyzed as independent variables. We hypothesized that SLH, knee strength, and running ability, which are important in such sports, as well as a high frequency of participation in sports before reconstruction and a short waiting period between injury and surgery, would influence an athlete's psychological readiness to return.
Methods
Participants
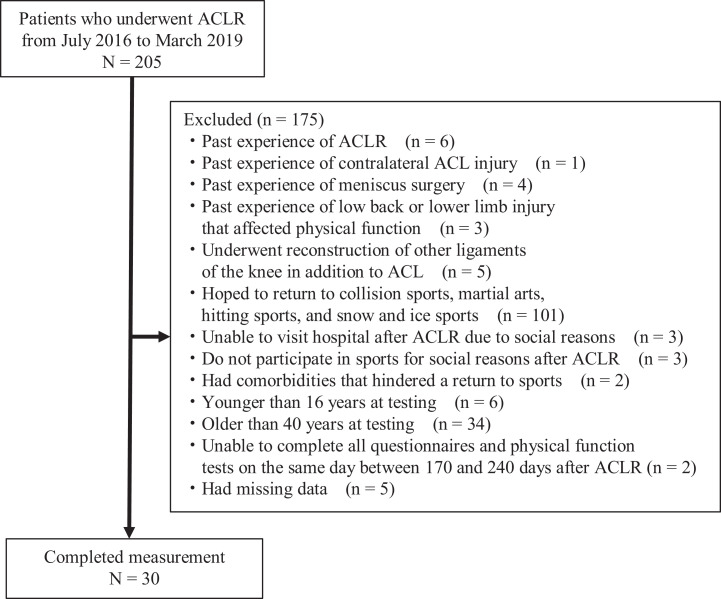
The institutional review board at our institution approved the study design, and all participants provided written informed consent. A total of 30 patients were selected from among 205 patients who underwent ACL reconstruction at a single hospital from July 2016 through March 2019 (Figure 1). Inclusion criteria were as follows: primary/unilateral anatomic double-bundle reconstruction using a hamstring tendon autograft; age ≥16 years and ≤40 years at testing; postoperative rehabilitation with the same protocol used in the sports physical therapy department of our institution; preinjury participation in cutting, pivoting, and jump-landing sports (basketball, soccer, futsal, volleyball, badminton, tennis, or frisbee); and partial participation in exercises related to their sport at approximately 6 months after reconstruction.
Figure 1.
Study flowchart. ACL, anterior cruciate ligament; ACLR, anterior cruciate ligament reconstruction.
Patients were excluded if they had past experience with ACL or meniscal injury or surgery, including on the contralateral side; had experienced injury that affected physical function in the low back or lower limb; had undergone reconstruction of other knee ligaments in addition to the ACL; hoped to return to collision sports with tackling (eg, American football and rugby), martial arts sports that require pairing and throwing (eg, judo and wrestling), hitting sports (eg, boxing), and snow and ice sports (eg, skiing and ice hockey); did not go to the hospital or participate in sports for social reasons, such as relocating or becoming pregnant after reconstruction; had comorbidities that hindered a return to sports; were <16 years or >40 years at testing; were unable to complete all questionnaires and physical function tests, including the ACL-RSI, on the same day between 170 and 240 days after reconstruction; or had missing data.
Postoperative Rehabilitation
The postoperative rehabilitation protocol was the same for all patients. Patients were permitted to begin isometric quadriceps exercises as tolerated on the day after ACL reconstruction. Using a knee brace (Straighten Position Knee-Joint Immobilizer; ALCARE) and crutches, 20 kg of partial weightbearing was permitted on the first day after reconstruction, which was gradually increased to the maximum body weight of each patient. Use of the knee brace and crutches was discontinued at 4 weeks after reconstruction. Range-of-motion exercises from full extension to 120° of flexion were started on the second day after reconstruction. Closed kinetic chain exercises such as weight shifting and squatting were started between 1 and 2 weeks after reconstruction. Open kinetic chain exercises such as seated knee extension using a machine load, and a perturbation training program were started 3 months after reconstruction.
Running exercises were started in athletes who had cleared the criterion of limb symmetry index (LSI) of 65% of the knee extension strength, measured by the Biodex Multi-Joint Testing and Rehabilitation System (BDX-4 Biodex Medical Systems Inc) at 3 months after reconstruction. Speed and distance of running were gradually increased for joint effusion and symptoms of each patient. Once 80% of subjective full-speed running ability was achieved, athletic exercises related to the desired sporting activities were initiated, with detailed instructions. The athletic exercises were specific to each patient, depending on the type of sport and position played. Participation in sports exercises with limited contact was allowed at 6 months after reconstruction, as long as the patient showed no problematic symptoms in the joint and had sufficient knee isokinetic flexion-extension strength at 60 deg/s (LSI, >80%) and had SLH ability (LSI, >80%) after the specified athletic training without contact had been completed.12,20 The criteria for determining when to participate in the actual game were 8 months after reconstruction and 90% LSI of knee strength and SLH.
Dependent Variable: Psychological Readiness to Return to Sport
Patients completed the ACL-RSI, which is a 12-item scale designed to measure psychological readiness to return to sport after ACL injury or reconstruction.14,26 The ACL-RSI includes 3 domains: emotions, confidence, and risk appraisal. The scores for each domain are summed and averaged for a total score between 0 and 100; higher scores indicate greater psychological readiness. The scale was validated and its predictive value demonstrated in previous studies.2,14,25 The Japanese version of the ACL-RSI was created and has been confirmed to be a highly practical questionnaire with good surface validity and internal consistency.11 Scores on the ACL-RSI were the primary outcome (dependent) variable for this study.
Independent Variables
Patient characteristics, preinjury Tegner activity level, preinjury sports participation time, days from injury to reconstruction, days after reconstruction, and meniscal surgery procedure were determined using medical records. On the day the ACL-RSI was completed, knee strength, leg anterior reach distance, and SLH distances were measured, and subjective running ability and kinesiophobia were determined using interviews and questionnaires. All physical function tests and interviews were conducted by 4 physical therapists (J.A., K.H., S.O., T.O.) with more than 10 years of clinical experience in the rehabilitation of athletes after ACL reconstruction.
Patient Data
Sex was determined based on medical records. On the day the ACL-RSI was completed, height and weight were measured and body mass index was calculated.
Preinjury Sports Activity Level and Participation Time
The sports activity level before injury was graded using the modified Tegner activity scale.7 The grades of lower-division futsal and recreation-level futsal were 8 and 6, respectively. Participants were interviewed regarding the average time (hours) of participating in sports the week before injury.
Time From Injury to Reconstruction and Reconstruction to Testing
The date of injury and the date of reconstruction were confirmed by the patient and medical record, and the number of days from the date of injury to the date of reconstruction was calculated. The number of days from surgery to testing (days after reconstruction) was also calculated.
Meniscal Surgery
Meniscal injuries and treatments were confirmed from detailed records of arthroscopic findings during reconstruction. Injured segment (anterior, middle, or posterior), injury type (longitudinal, radial, or horizontal), and treatment method (suture, centralization, or partial meniscectomy) were confirmed. Participants were defined as being treated regardless of method used.
Knee Strength
The Biodex Multi-Joint Testing and Rehabilitation System was used to evaluate the isokinetic strength of the knee extension-flexion. To minimize compensatory movements during testing, participants were seated and secured with padded straps around the thigh, pelvis, and torso. The femoral condyle of the tested limb was aligned with the rotation axis of the torque meter. Participants performed 3 to 5 repetitions of submaximal knee extension-flexion to familiarize themselves with the testing motion. To determine the strength of knee extension-flexion, participants performed 5 consecutive concentric contractions of extension-flexion at 60 and 180 deg/s. The peak torque within the 5 trials was extracted and normalized by body weight. The nonsurgical limb was tested first. The intraclass correlation coefficient of the concentric peak torque of the knee using the Biodex System was close to 0.90, indicating a high to very high reproducibility.6 The LSI of the knee strength was calculated by dividing the surgical limb value by the nonsurgical limb value and multiplying by 100.
Leg Anterior Reach Distance
The leg anterior reach distance with maximal effort was measured using the Y Balance Test Kit (Perform Better).8,10 Participants were instructed to perform the leg anterior reach using a combination of verbal cues and demonstration. Participants did not wear shoes during testing and began on their nonsurgical limb. Participants were asked to perform a single-limb stance on the extremity while reaching outside their base of support to push a reach indicator box along the measurement pipe of the kit. Loss of balance resulting in a stepping strategy was recorded as a trial error indicating the trial should then be repeated. Participants were allowed at least 6 practice trials before recording. The LSI of the anterior reach distance was calculated by dividing the surgical limb value by the nonsurgical limb value and multiplying by 100.
SLH Distance
SLH distances toward 3 directions (anterior, lateral, and medial) were measured in random order.9,22 Participants stood on 1 leg and were instructed to hop as far as possible and land on the same leg; the longest distance of 3 trials was recorded for each leg and each direction. The test was considered successful if the landing was stable. If the patient landed with an early touchdown of the contralateral limb, which represented loss of balance, or took additional hops after landing, the hop was repeated. Patients were initially given a verbal description of the test, and they were allowed to perform as many practice trials as they wanted, until they felt confident about the procedure. Three trials were performed for each leg, always starting with the nonsurgical limb. For anterior SLH, the distance between the front end of the toe at the starting position and the trailing edge of the heel at the landing position was measured. For lateral SLH, the distance between the lateral side of the foot at the starting position and the medial side of the foot at the landing position was measured. For medial SLH, the distance between the medial side of the foot at the starting position and the lateral side of the foot at the landing position was measured. Results were represented by LSI, calculated by dividing the distance on the surgical limb by the distance on the nonsurgical limb and multiplying by 100.
Subjective Running Ability
Participants were asked about subjective running ability, with maximal effort representing 100% of ability before injury, using the following question: “What do you think your current straight running ability is now if your straight running ability at full power before the injury was 100%?” This question was included because knee kinematic abnormalities during walking were reported to be associated with low ACL-RSI scores in patients after ACL reconstruction.31 We considered that this kind of relationship would also apply to running, so we included subjective running ability as an independent variable in this study.
Kinesiophobia
Kinesiophobia levels were objectively quantified with the Japanese version of the TSK. The TSK includes 17 items, with scores ranging from 17 to 48 points; higher scores indicate higher levels of kinesiophobia.16,29
Statistical Analysis
The normality of each variable was confirmed by the Shapiro-Wilk test. Normally distributed data for continuous variables were summarized with means and standard deviations. Nonnormally distributed data were summarized with medians and interquartile ranges. Simple regression analysis was performed to see the relationship between the ACL-RSI score as a dependent variable and each independent variable (age, sex, body mass index, days from injury to reconstruction, days after reconstruction, meniscal surgery, preinjury modified Tegner score, TSK, knee strength LSI, SLH LSI, and subjective running ability). Multiple regression analysis was performed by the stepwise method, with factors with a risk rate <0.1 in the single regression analysis as the independent variable and the ACL-RSI score as the dependent variable. All data were analyzed with the Statistical Package for the Social Sciences (Version 21.0; IBM Corp) for Windows. P < .05 was used to indicate statistical significance. Post hoc power analysis was performed with G*Power Version 3.1.9.2 (University of Dusseldorf). A post hoc power analysis of the main result (multiple regression) showed an effect size of 0.66, which corresponds to a power (1 – beta) of 94.8%.
Results
Table 1 shows the characteristics of the study participants. The average age of the 30 participants was 20 years, and 73% were women. The median preinjury Tegner score was 7.5, the mean time from reconstruction to testing was 187.5 days, and the average ACL-RSI score was 65.1. Outcome scores are shown in Table 2. The median subjective assessment of running ability was 80% of preinjury ability, and the mean TSK score was 34.5. The mean LSI of the lateral SLH was 84.1%.
Table 1.
Participant Characteristics (N = 30)a
| Age, y | 20.0 (7.3) |
| Women:men | 22:8 |
| Height, cm | 164.4 ± 0.1 |
| Weight, kg | 58.7 ± 8.2 |
| Body mass index, kg/m2 | 21.7 ± 2.0 |
| ACL-RSI score (0-100) | 65.1 ± 18.3 |
| Preinjury Tegner score | 7.5 (2.0) |
| Sports participation time before injury, h/wk | 4.0 (5.0) |
| Time from injury to reconstruction, d | 66.5 (97.3) |
| Meniscus, treated:nontreated, n | 17:13 |
| Time from reconstruction to testing, d | 187.5 ± 15.9 |
| Participating sports (basketball, soccer, futsal, volleyball, badminton, tennis, frisbee), n | 7, 8, 2, 6, 5, 1, 1 |
aData are reported as mean ± SD or median (interquartile range) unless otherwise indicated. ACL-RSI, Anterior Cruciate Ligament–Return to Sport after Injury Scale.
Table 2.
Outcome Scores (N = 30)a
| Knee extension strength (60 deg/s) LSI, % | 84.6 ± 10.0 |
| Knee flexion strength (60 deg/s) LSI, % | 86.9 ± 16.6 |
| Knee extension strength (180 deg/s) LSI, % | 81.0 ± 6.7 |
| Knee flexion strength (180 deg/s) LSI, % | 87.4 ± 16.2 |
| Leg anterior reach distance LSI, % | 98.3 ± 4.1 |
| Anterior SLH distance LSI, % | 87.9 ± 8.9 |
| Lateral SLH distance LSI, % | 84.1 ± 12.5 |
| Medial SLH distance LSI, % | 89.1 ± 10.4 |
| Subjective running ability, % | 80.0 (25.8) |
| Tampa Scale for Kinesiophobia | 34.5 ± 6.0 |
aData are reported as mean ± SD or median (interquartile range). LSI, limb symmetry index; SLH, single-leg hop.
Table 3 shows the results of univariate regression to identify factors associated with the ACL-RSI score. Variables with a significant single regression coefficient with the ACL-RSI score were subjective running ability, TSK, and LSI of lateral SLH distance. A simple regression coefficient of the knee flexion strength (180 deg/s) trended toward significance. Table 4 shows the results of multiple regression analysis. Variables with significant partial correlations were subjective running ability (P < .001), TSK (P = .001), and LSI of lateral SLH distance (P = .023). The variance inflation factor did not exceed 10 for any variable, and there was no multicollinearity between variables.
Table 3.
Univariate Regression to Identify Factors Associated With Psychological Readiness (ACL-RSI Score)a
| Independent Variable | β Coefficient (95% CI) | P |
|---|---|---|
| Age, y | –0.403 (–1.645 to 0.838) | .511 |
| Sex | –0.485 (–16.243 to 15.272) | .950 |
| Body mass index, kg/m2 | 0.671 (–2.778 to 4.121) | .693 |
| Preinjury Tegner score | –0.091 (–7.040 to 6.859) | .979 |
| Preinjury sports participation time, h/wk | –0.769 (–2.190 to 0.652) | .277 |
| Time from injury to reconstruction, days | 0.003 (–0.057 to 0.063) | .911 |
| Meniscal repair | –12.971 (–29.653 to 3.712) | .122 |
| Time from reconstruction to testing, d | –0.158 (–0.599 to 0.283) | .470 |
| Knee extension strength (60 deg/s) LSI, % | –0.118 (–0.824 to 0.587) | .733 |
| Knee flexion strength (60 deg/s) LSI, % | 0.263 (–0.151 to 0.677) | .203 |
| Knee extension strength (180 deg/s) LSI, % | –0.044 (–1.101 to 1.014) | .933 |
| Knee flexion strength (180 deg/s) LSI, % | 0.347 (–0.070 to 0.763) | .099 |
| Leg anterior reach distance LSI, % | –0.256 (–1.970 to 1.458) | .762 |
| Anterior SLH distance LSI, % | 0.491 (–0.282 to 1.264) | .204 |
| Lateral SLH distance LSI, % | 0.579 (0.058 to 1.099) | .031 |
| Medial SLH distance LSI, % | 0.147 (–0.530 to 0.824) | .660 |
| Subjective running ability, % | 0.804 (0.450 to 1.158) | <.001 |
| Tampa Scale for Kinesiophobia | –1.388 (–2.429 to –0.347) | .011 |
aACL-RSI, Anterior Cruciate Ligament–Return to Sport after Injury Scale; LSI, limb symmetry index; SLH, single-leg hop.
Table 4.
Multivariate Regression to Identify Factors Associated With Psychological Readiness (ACL-RSI Score)a
| Independent Variable | β Coefficient (95% CI) | P |
|---|---|---|
| Subjective running ability, % | 0.657 (0.359 to 0.955) | <.001 |
| Tampa Scale for Kinesiophobia | –1.265 (–1.983 to –0.546) | .001 |
| Lateral SLH distance LSI, % | 0.421 (0.063 to 0.778) | .023 |
aACL-RSI, Anterior Cruciate Ligament–Return to Sport after Injury Scale; LSI, limb symmetry index; SLH, single-leg hop.
Discussion
In this study, the ACL-RSI was used to quantify the psychological readiness of athletes after ACL reconstruction to return to limited-contact sports requiring cutting, pivoting, and jump-landings. We found that the psychological readiness of these athletes was associated with high subjective running ability, low kinesiophobia, and more symmetrical lateral SLH distance.
Participants in this study were aiming to return to their sports at least 6 months after reconstruction. Their mean ACL-RSI score was 65. The ACL-RSI score in previous studies of athletes who had undergone reconstruction was reported to be 57 to 77 at about 6 months,14,15 and the score in this study was within this range.
There have been no previous reports showing the relationship between subjective running ability and ACL-RSI score. A study on kinematics during walking on flat ground reported that the knee flexion angle at initial contact and the stance phase were smaller on the surgical side than on the nonsurgical side in the group with a low ACL-RSI score.31 In the current study, subjective running ability was extracted as a significant factor related to psychological readiness. Kinematic data during running and walking were not analyzed, but lack of knee flexion angle during initial contact and the stance phase may be associated with a low level of subjective running ability, which may have reduced the level of psychological readiness. In athletes aiming to return to sports requiring a lot of cutting, pivoting, and jump-landings and with limited contact, improvement of kinematics and subjective ability during running may lead to psychological readiness at approximately 6 months after surgery.
In a study of patients who returned to sports a mean of 7 months after reconstruction, there was a negative association between the KOOS pain score and ACL-RSI score, which showed that psychological readiness was high when pain was low.15 In the current study, TSK was identified as a significant factor related to psychological readiness. One study showed that viewing a contemporary art video that provides positive “insight,” combined with adequate rehabilitation, could improve short-term clinical outcomes, including TSK score, in patients who underwent ACL reconstruction.30 TSK quantifies psychological anxiety about pain and not just the degree of pain.5 If kinesiophobia can be reduced by such psychology-based interventions then these interventions may help improve psychological readiness in athletes. The current study showed that it is important to quantify psychological anxiety with the degree of pain and to improve psychological readiness while taking these factors into account.
In a study of 635 patients after primary ACL reconstruction, Webster et al28 reported that an athlete’s ACL-RSI score was associated with younger age, male sex, higher frequency of preoperative sports participation, shorter preoperative waiting time, and higher anterior SLH LSI. In the current study, these variables were included in the regression analysis as independent variables but were not shown to be related to the ACL-RSI score. In addition, we found that lateral SLH, instead of anterior SLH, was shown to be related to ACL-RSI score. Although the power obtained by post hoc analysis of multiple regression was 94.8% in our study, it cannot be denied that our comparatively small cohort size (N = 30) affected the results. The difference in findings between Webster et al and the current study may also be attributed to the difference in the postoperative period (12 months vs 6 months in the current study) and the specificity of the sport the athletes wished to return to. According to the results of this study, it is important to enhance lateral SLH ability in the surgical limb and increase the LSI of lateral SLH to enhance the psychological readiness in athletes aiming to return to limited-contact sports requiring cutting, pivoting, and jump-landings at approximately 6 months after reconstruction.
In terms of the ACL-RSI score, a previous study evaluated groups divided into >90% and ≤90% of multiple lower- limb muscle function test LSIs, including anterior SLH, with results showing that there was no significant between-group difference at 8 months after primary ACL reconstruction, but the difference tended toward significance at 12 months.4 The ACL-RSI score at the time of return was high when the range of increase in knee extension strength from before reconstruction to return to play was large.15 A study of patients who returned to sports after a mean of 7 months after ACL reconstruction showed that those with a higher knee extension strength LSI at the time of return had higher ACL-RSI scores.15 In the current study, knee flexion strength LSI at an angular velocity of 180 deg/s was not significantly related to ACL-RSI score in the multiple regression analysis. The relationship between the LSI of knee strength and SLH and psychological readiness may vary depending on the postoperative period.
Only the study by Webster et al28 revealed factors related to ACL-RSI score by multivariate analysis in patients after reconstruction. However, that study did not examine athletes by sport type. There are no studies comparing ACL-RSI scores by sport type. Subjective outcomes after surgery, such as the IKDC score, have been reported to vary by sport.21 ACL injury rates vary depending on the type of sport in which athletes participate and the presence or absence of contact.19 Thus, in terms of psychological readiness after reconstruction, it is important to clarify the characteristics of each type of sport in which athletes participate. We believe that this study provides important information on the factors related to psychological readiness in athletes who wish to return to sports with limited contact that involve cutting, pivoting, and jump-landings. Improving the symmetry of the lateral SLH distance, kinesiophobia, and subjective running ability may help athletes return to these types of sports.
This study has some limitations. First, the sample size of this study was small, which may have affected the difference between the results of this study and the results of previous studies. Second, there are limits to generalizing the results of this study to patients with significantly different characteristics, such as age and sex, surgical procedures, different sports, and postoperative days before return to a sport.14,15 Participants in this study were young (average, 20 years), and 73% were women. This cohort is not representative of patients after ACL reconstruction in our practice as a whole. Third, this study excluded athletes aiming to participate in high-contact sports that require cutting, pivoting, and jump-landings, such as rugby and American football. Research on factors associated with psychological readiness for these high-contact sports is currently being performed separately. Finally, because this study was cross-sectional, a longitudinal study is needed to clarify causality between events.
Conclusion
The psychological readiness of athletes aiming to return after ACL reconstruction to limited-contact sports that require cutting, pivoting, and jump-landings is affected by subjective running ability, kinesiophobia, and asymmetry of lateral SLH distance. This information may be useful in planning appropriate interventions and thereby increasing the likelihood of an athlete’s returning to such sports.
Footnotes
Final revision submitted May 11, 2020; accepted June 11, 2020.
One or more of the authors has declared the following potential conflict of interest or source of funding: This work was supported by the JSPS KAKENHI (grant No. JP26350606). AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Tokyo Medical and Dental University (ID No. M2019-019).
References
- 1. Anderson T, Wasserman EB, Shultz SJ. Anterior cruciate ligament injury risk by season period and competition segment: an analysis of National Collegiate Athletic Association injury surveillance data. J Athl Train. 2019;54(7):787–795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ardern CL, Österberg A, Tagesson S, et al. The impact of psychological readiness to return to sport and recreational activities after anterior cruciate ligament reconstruction. Br J Sports Med. 2014;48(22):1613–1619. [DOI] [PubMed] [Google Scholar]
- 3. Ardern CL, Webster KE, Taylor NF, Feller JA. Return to sport following anterior cruciate ligament reconstruction surgery: a systematic review and meta-analysis of the state of play. Br J Sports Med. 2011;45(7):596–606. [DOI] [PubMed] [Google Scholar]
- 4. Beischer S, Hamrin Senorski E, Thomeé C, Samuelsson K, Thomeé R. How is psychological outcome related to knee function and return to sport among adolescent athletes after anterior cruciate ligament reconstruction? Am J Sports Med. 2019;47(7):1567–1575. [DOI] [PubMed] [Google Scholar]
- 5. Chmielewski TL, Jones D, Day T, et al. The association of pain and fear of movement/reinjury with function during anterior cruciate ligament reconstruction rehabilitation. J Orthop Sports Phys Ther. 2008;38(12):746–753. [DOI] [PubMed] [Google Scholar]
- 6. de Araujo Ribeiro Alvares JB, Rodrigues R, de Azevedo Franke R, et al. Inter-machine reliability of the Biodex and Cybex isokinetic dynamometers for knee flexor/extensor isometric, concentric and eccentric tests. Phys Ther Sport. 2015;16(1):59–65. [DOI] [PubMed] [Google Scholar]
- 7. Fältström A, Hägglund M, Kvist J. Patient-reported knee function, quality of life, and activity level after bilateral anterior cruciate ligament injuries. Am J Sports Med. 2013;41(12):2805–2813. [DOI] [PubMed] [Google Scholar]
- 8. Garrison JC, Bothwell JM, Wolf G, Aryal S, Thigpen CA. Y Balance Test™ anterior reach symmetry at three months is related to single leg functional performance at time of return to sports following anterior cruciate ligament reconstruction. Int J Sports Phys Ther. 2015;10(5):602–611. [PMC free article] [PubMed] [Google Scholar]
- 9. Gustavsson A, Neeter C, Thomeé P, et al. A test battery for evaluating hop performance in patients with an ACL injury and patients who have undergone ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2006;14(8):778–788. [DOI] [PubMed] [Google Scholar]
- 10. Hallagin C, Garrison JC, Creed K, et al. The relationship between pre-operative and twelve-week post-operative Y-balance and quadriceps strength in athletes with an anterior cruciate ligament tear. Int J Sports Phys Ther. 2017;12(6):986–993. [PMC free article] [PubMed] [Google Scholar]
- 11. Hirohata K, Aizawa J, Furuya H, et al. The Japanese version of the Anterior Cruciate Ligament—Return to Sport After Injury (ACL-RSI) Scale has acceptable validity and reliability. Knee Surg Sports Traumatol Arthrosc. 2020;28(8):2519–2525. [DOI] [PubMed] [Google Scholar]
- 12. Koga H, Muneta T, Yagishita K, et al. Mid- to long-term results of single-bundle versus double-bundle anterior cruciate ligament reconstruction: randomized controlled trial. Arthroscopy. 2015;31(1):69–76. [DOI] [PubMed] [Google Scholar]
- 13. Lai CCH, Ardern CL, Feller JA, Webster KE. Eighty-three per cent of elite athletes return to preinjury sport after anterior cruciate ligament reconstruction: a systematic review with meta-analysis of return to sport rates, graft rupture rates and performance outcomes. Br J Sports Med. 2018;52(2):128–138. [DOI] [PubMed] [Google Scholar]
- 14. Langford JL, Webster KE, Feller JA. A prospective longitudinal study to assess psychological changes following anterior cruciate ligament reconstruction surgery. Br J Sports Med. 2009;43(5):377–381. [DOI] [PubMed] [Google Scholar]
- 15. Lepley AS, Pietrosimone B, Cormier ML. Quadriceps function, knee pain, and self-reported outcomes in patients with anterior cruciate ligament reconstruction. J Athl Train. 2018;53(4):337–346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Matsudaira H, Inutsuka K, Kikuchi N, et al. Development of a Japanese version of the Tampa Scale for Kinesiophobia (TSK-J): translation and linguistic validation. Rinsho Seikeigeka. 2013;48(1):13–19. [Google Scholar]
- 17. McPherson AL, Feller JA, Hewett TE, Webster KE. Psychological readiness to return to sport is associated with second anterior cruciate ligament injuries. Am J Sports Med. 2019;47(4):857–862. [DOI] [PubMed] [Google Scholar]
- 18. McPherson AL, Feller JA, Hewett TE, Webster KE. Smaller change in psychological readiness to return to sport is associated with second anterior cruciate ligament injury among younger patients. Am J Sports Med. 2019;47(5):1209–1215. [DOI] [PubMed] [Google Scholar]
- 19. Montalvo AM, Schneider DK, Webster KE, et al. Anterior cruciate ligament injury risk in sport: a systematic review and meta-analysis of injury incidence by sex and sport classification. J Athl Train. 2019;54(5):472–482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Muneta T, Koga H, Mochizuki T, et al. A prospective randomized study of 4-strand semitendinosus tendon anterior cruciate ligament reconstruction comparing single-bundle and double-bundle techniques. Arthroscopy. 2007;23(6):618–628. [DOI] [PubMed] [Google Scholar]
- 21. Nwachukwu BU, Voleti PB, Chang B, et al. Comparative influence of sport type on outcome after anterior cruciate ligament reconstruction at minimum 2-year follow-up. Arthroscopy. 2017;33(2):415–421. [DOI] [PubMed] [Google Scholar]
- 22. Reid A, Birmingham TB, Stratford PW, Alcock GK, Giffin JR. Hop testing provides a reliable and valid outcome measure during rehabilitation after anterior cruciate ligament reconstruction. Phys Ther. 2007;87(3):337–349. [DOI] [PubMed] [Google Scholar]
- 23. Schilaty ND, Nagelli C, Bates NA, et al. Incidence of second anterior cruciate ligament tears and identification of associated risk factors from 2001 to 2010 using a geographic database. Orthop J Sports Med. 2017;5(8):2325967117724196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Takahashi S, Nagano Y, Ito W, Kido Y, Okuwaki T. A retrospective study of mechanisms of anterior cruciate ligament injuries in high school basketball, handball, judo, soccer, and volleyball. Medicine (Baltimore). 2019;98(26):e16030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Webster KE, Feller JA. Exploring the high reinjury rate in younger patients undergoing anterior cruciate ligament reconstruction. Am J Sports Med. 2016;44(11):2827–2832. [DOI] [PubMed] [Google Scholar]
- 26. Webster KE, Feller JA, Lambros C. Development and preliminary validation of a scale to measure the psychological impact of returning to sport following anterior cruciate ligament reconstruction surgery. Phys Ther Sport. 2008;9(1):9–15. [DOI] [PubMed] [Google Scholar]
- 27. Webster KE, McPherson AL, Hewett TE, Feller JA. Factors associated with a return to preinjury level of sport performance after anterior cruciate ligament reconstruction surgery. Am J Sports Med. 2019;47(11):2557–2562. [DOI] [PubMed] [Google Scholar]
- 28. Webster KE, Nagelli CV, Hewett TE, Feller JA. Factors associated with psychological readiness to return to sport after anterior cruciate ligament reconstruction surgery. Am J Sports Med. 2018;46(7):1545–1550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Woby SR, Roach NK, Urmston M, Watson PJ. Psychometric properties of the TSK-11: a shortened version of the Tampa Scale for Kinesiophobia. Pain. 2005;117(1-2):137–144. [DOI] [PubMed] [Google Scholar]
- 30. Zaffagnini S, Russo RL, Marcheggiani Muccioli GM, Marcacci M. The Videoinsight® method: improving rehabilitation following anterior cruciate ligament reconstruction—a preliminary study. Knee Surg Sports Traumatol Arthrosc. 2013;21(4):851–858. [DOI] [PubMed] [Google Scholar]
- 31. Zarzycki R, Failla M, Capin JJ, Snyder-Mackler L. Psychological readiness to return to sport is associated with knee kinematic asymmetry during gait following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2018;48(12):968–973. [DOI] [PMC free article] [PubMed] [Google Scholar]