Dear Editor,
We are sending this letter to “Travel medicine and Infectious Diseases” to share the results of our study which retrospectively looked at hospital admissions, ICU admissions and deaths due to Coronavirus disease 2019 (COVID-19) and what effects other factors had on these outcomes. Conducting these assessments on COVID-19 patients, especially the elderly, may establish risk stratification of patients before and upon hospital admission. This helps to fine-tune admission protocols and epidemiological surveillance processes to the reality of the pandemic. Such knowledge will empower health care practitioners to better manage the epidemic by paying due attention to higher risk groups.
The majority (81%) of cases of COVID-19 result in mild to moderate disease, some progress to severe (14%) and critical (5%) disease [1]. In Oman, a country of 4.49 million, the COVID-19 epidemic began with a travel-related case on February 24, 2020 and has spread all over the country with increasing numbers and death [2].
To better equip our health centers and improve our surveillance processes, we conducted a retrospective analysis of COVID-19 patients diagnosed by PCR in Oman from February 24, 2020 to July 19, 2020. The data were obtained from the national COVID-19 surveillance data. As the protocol for the management of COVID-19 in Oman only advises the moderate to severe cases of COVID-19 be admitted, it was justifiable to use the hospital admissions as a proxy of adverse outcome of disease. Deaths and ICU admissions were also used as a primary outcome. We studied the following factors in relation to outcomes: sex, age groups (0–15, 15–60, >60 years old), nationality (Omani/non-Omani), location, in addition to fever, cough, and sore throat as presenting symptoms. Comorbidities included were asthma, body mass index (BMI) > 40, neurological disease, chronic lung disease, immunocompromised, diabetes mellitus (DM), hypertension, chronic kidney disease (CKD), chronic hematological disorders, and chronic liver disease. Pregnancy was also studied as a factor.
A total of 68,967 PCR-confirmed cases of COVID-19 were diagnosed during the study period. Most of the patients were male (74.9%) between 15 and 60 years old and 54.2% of the cases were diagnosed in Muscat governorate, Oman's capital city. Regarding symptoms, 40.6% of these cases reported having a fever, 38.0% reported cough, and 37.8% complained of sore throat. Nevertheless, 34.8% of the cases were not documented to have a fever, cough, or sore throat whereas 12.3% reported having the three symptoms concurrently. Most of the cases (95.2%) had no comorbidities. The most common documented comorbid conditions were DM (2.9%), and hypertension (0.7%). During the study period, 2788 (4.0%) of the cases were admitted to the general ward, 243 (0.4%) were admitted to the ICU, and 377 (0.5%) died.
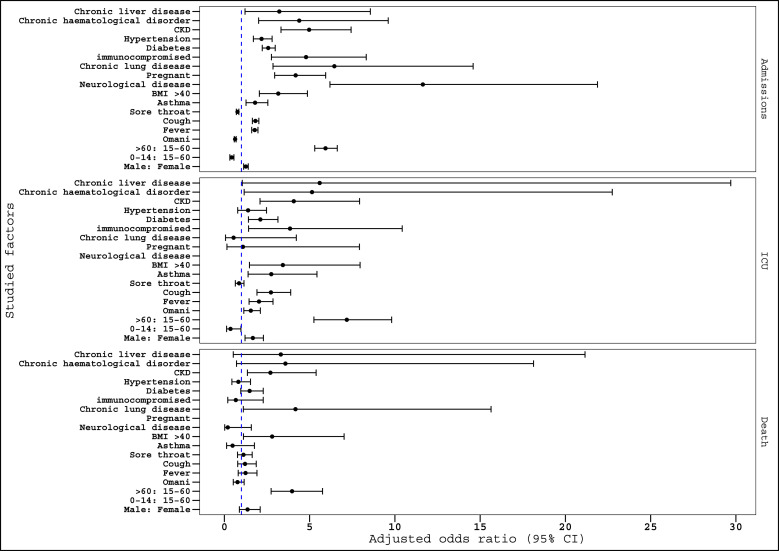
The multivariable logistic regression analysis shows that patients over 60 have a higher risk of admissions (AOR = 8.56, 95%, CI, 7.76–9.45), ICU admissions (AOR = 11.43, 95%, CI, 8.69–15.02), and deaths (AOR = 4.24, 95%, CI, 2.97–6.07) compared to those between 15 and 60 years old, Fig. 1 . Presenting with fever and cough is the most attributed factor to hospitalization, ICU admission, and death, Fig. 1. All the risk factors are shown to associate with a higher risk of admissions and ICU admissions as per Fig. 1. In addition, results showed that there was an increased risk of death among certain comorbid condition groups including BMI >40 (AOR = 2.8, 95%, CI, 1.12–7.02), chronic lung disease (AOR = 4.17, 95%, CI, 1.11–15.64) and CKD (AOR = 2.7, 95%, CI, 1.35–5.38).
Fig. 1.
Multivariable logistic regression investigating the factors associated with hospitalization, ICU admission, and death from COVID-19, Oman, 24th February 2020–19th July 2020. The reference level is the absence of the covariate (dummy variables) unless stated in the figure by ‘:’.
The pattern of association found in our study was like many other studies [3,4]. Our study also found that the presentation of fever and cough was statistically associated with higher admission and ICU admission rate, whereas, sore throat was found to be protective for admission and ICU admission. This is because, and as suggested by our field epidemiological investigators that sore throat is subjective and can sometimes be falsely claimed by patients, a trend also found by Lovato A et al. [5].
Though our study had its limitations such as the availability of admission beds, accessibility to the health institutions, and admissions for observation and the study's retrospective nature, it is important to monitor susceptible populations for development of severe infection. Overall, as this population-based study highlighted, it is important to identify and thus closely monitor the susceptible populations for the development of severe COVID-19 infection. Now that we know what factors generally lead to which specific outcomes, we can plan accordingly. With the use of artificial intelligence, which was introduced recently to the national surveillance system in Oman for case follow-up, we can now fine-tune the risk stratification of the COVID-19 susceptible/confirmed cases utilizing the findings of this study, thus better follow-up and manage of the cases. Furthermore, this study is a call for more detailed prospective studies, and we implore others to explore symptoms and comorbidities to these ends in a detailed manner.
Funding
No funding was needed for this study.
Authors’ contribution
Adil Al Wahaibi conducted the statistical analysis and wrote the draft manuscript and discussion, Badar Al Rawahi wrote the introduction, Prakash Kurubarahalli Patel participated in the discussion, Sulien Al Khalili reviewed and edited the manuscript, Amal Al Maani reviewed and edited the manuscript, Seif Al-Abri supervised the study and participated in all stages of manuscript preparation.
Declaration of competing interest
The authors declare that they have no conflict of interest.
Acknowledgment
The authors would like to thank Lesley Carson for her editorial assistance in finalizing the manuscript.
References
- 1.WHO Coronavirus disease (COVID-19) dashboard n.d. https://covid19.who.int
- 2.Wahaibi A.A., Manji A.A., Maani A.A., Rawahi B.A., Harthy K.A., Alyaquobi F. COVID-19 epidemic monitoring after non-pharmaceutical interventions: the use of time-varying reproduction number in a country with a large migrant population. Int J Infect Dis. 2020;S1201–9712(20):30668. doi: 10.1016/j.ijid.2020.08.039. 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tian W., Jiang W., Yao J., Nicholson C.J., Li R.H., Sigurslid H.H. Predictors of mortality in hospitalized COVID-19 patients: a systematic review and meta-analysis. J Med Virol. 2020 doi: 10.1002/jmv.26050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cai Q., Chen F., Wang T., Luo F., Liu X., Wu Q. Obesity and COVID-19 severity in a designated hospital in Shenzhen, China. Diabetes Care. 2020;43(7):1392–1398. doi: 10.2337/dc20-0576. [DOI] [PubMed] [Google Scholar]
- 5.Lovato A., Rossettini G., de Filippis C. Sore throat in COVID-19: comment on “Clinical characteristics of hospitalized patients with SARS-CoV-2 infection: a single arm meta-analysis. J Med Virol. 2020;92(7):716–718. doi: 10.1002/jmv.25818. [DOI] [PMC free article] [PubMed] [Google Scholar]