Abstract
Purpose
To assess the quality of life, functional status, and their predictors in tongue cancer patients up to three months after anterolateral thigh free flap (ALTFF) reconstruction.
Patients and Methods
Tongue cancer patients were examined before and one and three months after ALTFF reconstruction using three validated questionnaires: the MD Anderson Dysphagia Inventory (MDADI), Eating Assessment Tool (EAT-10), and Functional Assessment of Cancer Therapy-Head and Neck (FACT-H&N). Mean scores were compared using the Friedman test. Forward selection and backward elimination methods of multiple linear regression analysis were used to identify the predictors of quality of life and functional status using SPSS at a 95% significance level.
Results
The present study included 265 participants (88.68% males, mean age 46.7 ± 11.05 years). The mean MDADI and EAT-10 scores were highest at one month after the surgery and lowest at three months after the surgery (p < 0.05). The mean FACT-H&N score was lowest at one month after the surgery (p < 0.05); however, post hoc analysis revealed that the difference in the scores before and three months after the surgery was non significant (p > 0.05). Denture use, occupation, age, tumor site, illness duration, drinking habit, and diet predicted the patients’ quality of life, while denture use, betel nut consumption, age, marital status, and diet predicted their functional status.
Conclusion
Although tongue cancer patients have a poor quality of life and functional status in the first month after ALTFF reconstruction, their quality of life and functional status improve thereafter. We recommend the implementation of swallowing training programs and case-oriented psychological interventions to assist patients in coping with temporary deterioration during the first month after the surgery.
Keywords: tongue cancer, anterolateral thigh free flap reconstruction, MDADI, EAT-10
Introduction
The prevalence of tongue cancer ranges from about 3% to 90% depending on the geographical region or country.1,2 In contrast to older reports,3 the mortality and incidence of tongue cancer are now increasing, particularly in the younger population and in women.4,5 Lifestyle factors, such as smoking and drinking habits, are strongly linked to the pathogenesis of tongue cancer. Moreover, Human Papilloma infection and genetic factors play a vital role in neoplastic initiation and progression. Tongue cancer is considered the worst type of oral cancer, with a mortality rate higher than 40% within the first 5 years after diagnosis.4
Chemotherapy and radiotherapy are commonly utilized as adjuvant therapies for the management of tongue cancer, while surgical resection is the first line of treatment.6 The older approaches mainly aimed at survival and avoided extensive tongue resections, while the modern approaches aim at survival, preserve function, and improve the quality of life.7 This has been possible by replacing the resected tissue with tissue harvested from other parts of the body, which lays the foundation for oral reconstruction and rehabilitation.8 Soft tissue harvested for reconstruction, also known as a flap, could contain a muscle, fascia, skin, or bone depending on the extent of resection at the tissue recipient site.9
The flaps used for the reconstruction of tongue cancer defects are classified into different types according to their site of harvest.10 Of these, anterolateral thigh free flaps (ALTFFs) have been commonly used in the past three decades. The other types include radial/upper forearm, pectoralis major, and contralateral nasal free flaps.11,12 These flaps have shown different outcomes in improving patient survival, reducing morbidity and mortality, and improving the functional status and quality of life.13 Compared to other tissue flaps, ALTFF is superior in terms of being an adequately sized flap, sparing major vasculature, and having better cosmesis at both donor and recipient sites.14
The apparent success and popularity of ALTFF reconstruction are due to the surgical technique. However, there is limited knowledge regarding its success in improving the functional status and overall quality of life of patients. Therefore, the present study aimed to assess whether ALTFF reconstruction impacts the functional status and overall quality of life of tongue cancer patients.
Patients and Methods
Study Design
This was a prospective comparative study.
Study Setting
The present study was conducted at the Hunan Cancer Hospital of Central South University in Changsha City, Hunan Province, People’s Republic of China. The study complied with the Declaration of Helsinki and was approved by the Institutional Review Board of Central South University, Hunan Province, China (approval number: 2019014). Data were collected using Chinese versions of three questionnaires: the MD Anderson Dysphagia Inventory (MDADI), Eating Assessment Tool (EAT-10), and Functional Assessment of Cancer Therapy-Head and Neck (FACT-H&N). These questionnaires aimed to assess the quality of life and functional status of tongue cancer patients before and after undergoing ALTFF reconstruction. The initial assessments were conducted on the day of the surgery. The second and third assessments were conducted at one and three months after the surgery, respectively, during the follow-up. Data were collected for three months from July 1, 2019, to February 1, 2020, upon the receipt of eligible participants.
Study Participants
The inclusion criteria were as follows: (1) being newly diagnosed by the American Joint Committee on Cancer (AJCC)15 as having stage I–IV oral cancer, (2) seeking to undergo ALTFF reconstruction, (3) having undergone neck dissection, (4) being able to speak Chinese, (5) being above 18 years old, and (6) being diagnosed with tongue cancer at Hunan Cancer Hospital.
The exclusion criteria were as follows: (1) having a history of head and neck cancer, (2) having undergone previous resections extending outside the tongue base in the oropharynx, (3) having a history of tongue dysfunction before the diagnosis of tongue cancer (ie, being unable to speak, read/write, eat, or drink), (4) having a history of cervical spine surgery or other neurosurgical procedures that might affect swallowing, (5) having undergone radiotherapy or chemotherapy before the current surgery, (6) having different types of free flaps, (7) being lost to follow-up, and (8) experiencing flap failure.
The eligible participants were scheduled for a follow-up visit at one and three months after the surgery for the second and third assessments, respectively. Every eligible participant served as their own matched control before and after the surgery.
ALTFF Reconstruction
Following a biopsy-proven cancer diagnosis, the stage of the disease was determined according to the American Joint Committee on Cancer/Union for International Cancer Control-TNM (AJCC/UICC-TNM) classification.15 The patients’ demographics, history of smoking, comorbidities (eg, diabetes), and adjuvant therapy were recorded. This was followed by recipient site evaluation concerning cosmesis and function, including the assessment of the size and location of the recipient site, exposure of vital structures, and susceptibility to infection. The recipient site was prepared by debriding granulation tissue (if any), trimming wound margins, and irrigating with 3 to 5 L of the antiseptic solution to reduce bacterial contamination.
Blood supply at the donor site was assessed using a hand-held Doppler probe, identifying the descending/oblique branch of the lateral circumflex femoral artery and its angiosome. This was followed by site mapping, exploratory incision, and, ultimately, dissection to identify the most suitable perforator artery. The flaps were harvested as septocutaneous or musculocutaneous, depending on their anatomical relationship with the underlying muscle. Thorough hemostasis and primary closure preceded general wound care.
During the first 72 hours after flap transfer, the recipient sites were observed hourly for signs of vascular compromise. The evaluation was performed by Doppler ultrasound, tissue oximetry, and clinical observation to detect the color change and reduced capillary refill. Three days after the surgery, the monitoring was performed at four-hour intervals.
Variables and Data Collection
The present study had two outcome variables: the patients’ quality of life and patients’ functional status.
The patients’ quality of life was evaluated by assessing the impact of dysphagia on their lives using the MDADI questionnaire16 and by assessing dysphagia symptom severity using the EAT-10 questionnaire.17 The FACT-H&N questionnaire was used to assess the patients’ functional status.18 From the existing literature, Cronbach’s alpha coefficients for the questionnaires were found to be as follows: MDADI, 0.85–0.93;16 EAT-10, 0.96;17 and FACT-H&N, 0.91.18
In addition, the patients’ demographics, medical history, disease burden, and lifestyle parameters were recorded.
After obtaining informed consent, every eligible participant was given the questionnaires. A brief period ranging from five to ten minutes was provided for filling each questionnaire, with a break between completing each questionnaire. The participants self-filled all the questionnaires.
Bias
Several measures were taken to mitigate non-response bias. Validated constructed questionnaires (ie, MDADI, EAT-10, and FACT-H&N) were used. The participants were asked to self-fill and submitted the duly filled questionnaires at the hospital within a structured time during their follow-up visits; the responses were strictly anonymous. Data collection was scheduled on the same day of the clinical follow-up visits at one and three months after the surgery. Moreover, the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) tool, customized for cohort studies to mitigate reporting and publication biases, was used during the write up of this report.19
Study Size
The sample size was calculated using the following formula:20 N = 4µα2 σ2/δ 2. The value of μα was found to be 1.96, and the standard deviation (σ) was found to be 18.8. The tolerance (δ) was 4.7, calculated by N = 246, considering a sample loss rate of 10% from a total of 271 cases. Therefore, a minimum of 271 participants was included in the present study.
Statistical Analyses
To compare the patients’ quality of life and functional status before and one and three months after ALTFF reconstruction based on the mean overall scores recorded from their respective validated questionnaires, the Friedman test was used if the raw scores demonstrated non-normal distributions. Post hoc analysis with Wilcoxon signed-rank tests was performed to determine significance in differences between each pair in the three comparison groups.
The overall recorded scores from each of the three questionnaires were used as continuous dependent variables against preset categorical independent predictors (ie, age, gender, education status, marital status, occupation, income status, illness duration, betel nut consumption, drinking habit, smoking habit, denture use, oral ulcer, diet, tumor site, and tumor size). Forward selection and backward elimination methods of multiple linear regression analysis were used to identify the predictors of quality of life and functional status at three different time points, namely before the surgery, one month after the surgery, and three months after the surgery, from each of three questionnaires. The MDADI and EAT-10 scores were used to identify the predictors of quality of life in terms of swallowing symptoms. Moreover, the FACT-H&N scores were used as dependent variables to identify the predictors of functional status.
The forward selection method systematically identifies only variables that have less than a 0.05 level of significance. In comparison, the backward elimination method systematically eliminates all variables with more than 0.10 level of significance. Statistical analyses were performed using the computer software SPSS (IBM Corp. Released 2012. IBM SPSS Statistics for Windows, Version 21.0, Armonk, NY: IBM Corp.) at a 95% significance level.
Results
In total, 271 tongue cancer patients were examined in the present study. Of these, six patients were excluded (four due to loss to follow-up, one for having a history of chemoradiotherapy, and unable to read and write). Ultimately, 265 tongue cancer patients (88.68% males) fulfilled the eligibility criteria for the present study. Table 1 summarizes the patients’ demographics, medical history, disease burden, and lifestyle parameters. The mean age of the participants was 46.7 ± 11.05 years, and most participants were aged between 40 and 59 years. More than half of the participants had not received a college education, and about one-third (35.47%) were farmers. Most participants (83.77%) were married. Two-thirds of the participants had a monthly income between 1000 and 7999 Chinese Yuan. Regarding lifestyle parameters, more than half of the participants reported having used betel nuts. One-third (31.7%) and two-thirds (63%) of the participants reported that they did not smoke and drink alcohol, respectively.
Table 1.
Patients’ Demographics, Medical History, Disease Burden, and Lifestyle Parameters
| Patient-Related Parameters | Sub-Categories | Proportions (%) |
|---|---|---|
| Age | 20–39 years | 45 (16.98) |
| 40–59 years | 157 (59.24) | |
| 60–79 years | 63 (23.77) | |
| Gender | Male | 235 (88.68) |
| Female | 30 (11.32) | |
| Education status | Below junior high school | 76 (28.68) |
| Junior high school | 106 (40) | |
| Technical secondary school or college | 53 (20) | |
| Bachelor’s degree or above | 30 (11.32) | |
| Marital status | Married | 222 (83.77) |
| Unmarried | 12 (4.5) | |
| Widowed or divorced | 31 (11.70) | |
| Occupation | Unemployed or retired | 58 (21.89) |
| Institutional or company employee | 62 (23.40) | |
| Farmer | 94 (35.47) | |
| Business or freelance | 51 (19.25) | |
| Income status | ≤1000 Chinese Yuan | 39 (14.72) |
| 1000–2999 Chinese Yuan | 101 (38.11) | |
| 3000–7999 Chinese Yuan | 79 (29.8) | |
| ≥8000 Chinese Yuan | 46 (17.4) | |
| Illness duration | <3 months | 95 (35.8) |
| 3–12 months | 119 (44.9) | |
| 13–36 months | 45 (17) | |
| >36 months | 5 (1.9) | |
| Betel nut consumption | No | 121 (45.7) |
| Yes (one to nine pieces/day) | 30 (11.3) | |
| Yes (10–19 pieces/day) | 70 (26.4) | |
| Yes (>20 pieces/day) | 44 (16.6) | |
| Drinking habit | No | 167 (63.0) |
| Yes (white wine, one to four times) | 64 (24.2) | |
| Yes (white wine, ≥five times) | 20 (7.5) | |
| Yes (rice beer and red wine) | 14 (5.3) | |
| Smoking habit | No | 84 (31.7) |
| Yes (≤19 pieces) | 75 (28.3) | |
| Yes (≥20 pieces) | 106 (40) | |
| Denture use | Yes | 164 (61.9) |
| No | 101 (38.1) | |
| Oral ulcer | Yes | 110 (41.5) |
| No | 155 (58.5) | |
| Diet | Liquid | 258 (97.4) |
| Semisolid | 3 (1.1) | |
| Solid | 4 (1.5) | |
| Tumor stage | I | 77 (29.1) |
| II | 128 (48.3) | |
| III | 59 (22.3) | |
| IV A | 1 (0.4) | |
| IV B | 0 (0.0) | |
| Tumor site | First part of the tongue | 214 (80.8) |
| Second part of the tongue | 51 (19.2) | |
| Tumor size | <2 cm | 50 (18.9) |
| 2–4 cm | 190 (71.7) | |
| >4 cm | 25 (9.4) | |
| Removal size | <2 cm | 62 (23.4) |
| 2–5 cm | 101 (38.1) | |
| >5 cm | 96 (36.2) | |
| Type of surgery | Partial hemiglossectomy | 205 (77.4) |
| Hemiglossectomy | 60 (22.6) | |
| Total glossectomy | 0 (0) | |
| Adjuvant therapy | No adjuvant therapy | 116 (43.8) |
| Radiotherapy | 122 (46.0) | |
| Chemoradiotherapy | 27 (10.2) | |
| Postoperative therapy | Chemotherapy | 75 (28.3) |
| Radiotherapy | 190 (71.7) | |
| Gastrostomy tube | Placed | 61 (23.0) |
| Not placed | 204 (77.0) | |
| Tracheostomy | Performed | 108 (40.8) |
| Not performed | 157 (59.2) | |
| Neck dissection | None | 123 (46.4) |
| Unilateral | 142 (53.6) | |
| Bilateral | 0 (0) | |
| Neck dissection type | Radical | 1 (0.4) |
| Modified radical | 190 (71.7) | |
| Selective | 74 (27.9) | |
| Flap shape | Mushroom | 202 (76.2) |
| Bilobed | 63 (23.8) | |
| Flap dimensions (mean ± standard deviation) | Length: 7.5 ± 1.6 cm | |
| Width: 4.3 ± 0.7 cm | ||
| Surface area: 35.7 ± 11.8 cm2 | ||
| Swallowing initiation (mean ± standard deviation) | 13.4 ± 3.1 days |
Regarding medical history, most participants (44.9%) reported having been ill for 3–12 months, with about half (48.3%) having stage II disease. Moreover, 58.5% of the participants reported having an oral ulcer, and 71.7% had tumors measuring 2–5-cm. 80.8% had the tumor located in the first part of the tongue, as a result of which swallowing was hindered, and 97.4% of the participants only relied on a liquid diet.
Quality of Life and Functional Status Before and After Surgery
Table 2 summarizes the comparison of the patients’ quality of life and functional status before and one and three months after ALTFF reconstruction. There was a significant difference in the mean MDADI scores before and one and three months after the surgery (F = 438.815, p = 0.00). The mean score at three months after the surgery (7.05 ± 2.11) was lower than those before the surgery (27.36 ± 14.67, p = 0.00) and one month after the surgery (47.77 ± 19.08, p = 0.00). However, the mean MDADI score at one month after the surgery (47.77 ± 19.08) was higher than before the surgery (27.36 ± 14.67, p = 0.00). These findings suggest the worsening of swallowing symptoms during the first month after the surgery, followed by a significant improvement during the third month after the surgery.
Table 2.
Comparison of Patients’ Quality of Life and Functional Status Before and One and Three Months After ALTFF Reconstruction
| Tool Utilized | Subitems | Before the Surgery (Mean ± Standard Deviation) | One Month After the Surgery (Mean ± Standard Deviation) | Three Months After the Surgery (Mean ± Standard Deviation) | p-value (from the Friedman Test) |
|---|---|---|---|---|---|
| MDADI | – | 27.36 ± 14.67 | 47.77 ± 19.08 | 7.05 ± 2.11 | 0.00 |
| EAT-10 | – | 6.91 ± 6.00 | 21.79 ± 5.98 | 5.01 ± 1.79 | 0.00 |
| FACT-H&N | Psychological | 6.24 ± 3.04 | 11.07 ± 4.11 | 4.75 ± 1.69 | 0.00 |
| Family Social Status | 19.50 ± 6.05 | 18.61 ± 5.87 | 16.93 ± 3.19 | 0.00 | |
| Emotional | 5.55 ± 3.03 | 6.46 ± 3.24 | 4.27 ± 1.63 | 0.00 | |
| Functional | 11.41 ± 4.79 | 9.57 ± 4.93 | 11.03 ± 5.34 | 0.00 | |
| Head and Neck Cancer (Special) | 18.18 ± 4.33 | 7.85 ± 4.09 | 5.43 ± 2.23 | 0.00 | |
| Overall | 60.88 ± 10.07 | 53.54 ± 10.87 | 40.88 ± 9.61 | 0.00 |
Note: Values in bold are statistically significant.
There was a significant difference in the mean EAT-10 scores before and one and three months after the surgery (F = 330.382, p = 0.00). The mean score at three months after the surgery (5.01 ± 1.79) was lower than those before the surgery (6.91 ± 6.00, p = 0.004) and one month after the surgery (21.79 ± 5.98, p = 0.00). The mean EAT-10 score at one month after the surgery (21.79 ± 5.98) was higher than before the surgery (6.91 ± 6.00, p = 0.00). These findings suggest a poorer quality of life due to the worsening of swallowing symptoms during the first month after the surgery, followed by a significant improvement during the third month after the surgery.
The mean FACT-H&N score was analyzed by combining all the five subitem scores mentioned above (in Table 2); the FACT-H&N score at three months after the surgery (40.88 ± 9.61) was lower than those before the surgery (60.88 ± 10.07, p = 0.00) and one month after the surgery (53.54 ± 10.87, p = 0.00). The mean score at one month after the surgery (53.54 ± 10.87) was lower than before the surgery (60.88 ± 10.07, p = 0.00). These findings indicate progressive improvement in the patients’ quality of life from the first to the third month after the surgery.
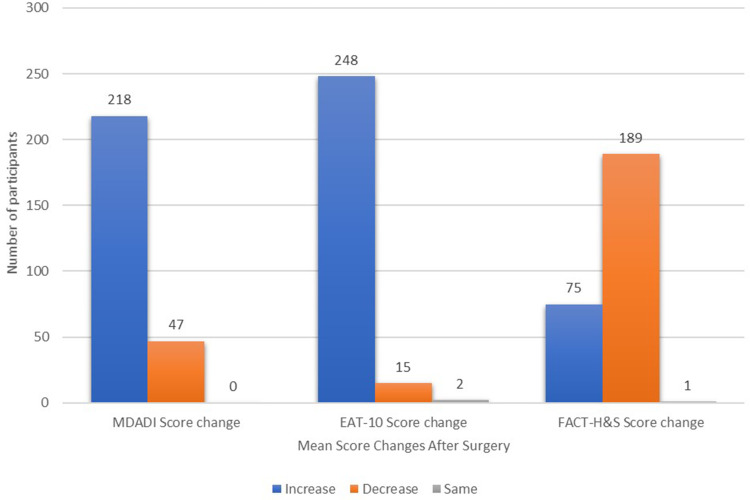
Figure 1 summarizes the comparison of mean scores indicative of the patients’ quality of life and functional status before the surgery until three months after the surgery.
Figure 1.
Comparing mean scores indicative of the patients’ quality of life and functional status before the surgery until three months after the surgery.
Factors Associated with Quality of Life and Functional Status
Tables 3 and 4 summarize the coefficients from the forward selection and backward elimination methods, respectively, of multiple linear regression analysis models for factors predicting the quality of life and functional status at three different time points: before the surgery, one month after the surgery, and three months after the surgery. The use of MDADI scores as dependent variables did not reveal any factor was predicting the quality of life before the surgery. Age (p = 0.017) and denture use (p = 0.000) predicted the quality of life at one month after the surgery, while drinking habit (p = 0.023) and diet (p = 0.035) predicted the quality of life at three months after the surgery.
Table 3.
Coefficients from the Forward Selection Method of Multiple Linear Regression Analysis Models for Factors Predicting the Quality of Life and Functional Status at Three Different Time Points: Before the Surgery, One Month After the Surgery, and Three Months After the Surgery
| Questionnaire | Predicting Factor | Before Surgery | One Month After the Surgery | Three Months After the Surgery | |||
|---|---|---|---|---|---|---|---|
| Unstandardized Beta Coefficients (95.0% Confidence Interval) | p-value | Unstandardized Beta Coefficients (95.0% Confidence Interval) | p-value | Unstandardized Beta Coefficients (95.0% Confidence Interval) | p-value | ||
| MDADI | Denture use | NS | NS | −14.001 (−18.594, −9.409) | 0.000 | NS | NS |
| Age | NS | NS | 4.306 (0.792, 7.820) | 0.017 | NS | NS | |
| Drinking habit | NS | NS | NS | NS | 0.346 (0.049, 0.644) | 0.023 | |
| Diet | NS | NS | NS | NS | 1.026 (0.075, 1.977) | 0.035 | |
| EAT-10 | Occupation | −1.149 (−1.846, −0.452) | 0.001 | NS | NS | NS | NS |
| Denture use | 2.063 (0.577, 3.549) | 0.007 | −3.642 (−5.068, −2.216) | 0.000 | NS | NS | |
| Illness duration | NS | NS | NS | NS | 0.300 (0.092, 0.509) | 0.005 | |
| FACT-H&N | Denture use | −5.129 (−6.180, −4.078) | 0.000 | −4.924 (−7.611, −2.237) | 0.000 | NS | NS |
| Betel nut consumption | 0.740 (0.313, 1.167) | 0.001 | NS | NS | NS | NS | |
| Age | 1.016 (0.208, 1.823) | 0.014 | NS | NS | NS | NS | |
| Diet | NS | NS | 6.812, (1.879, 11.745) | 0.007 | NS | NS | |
Note: Values in bold are statistically significant.
Abbreviation: NS, not significant.
Table 4.
Coefficients from the Backward Elimination Method of Multiple Linear Regression Analysis Models for Factors Predicting Quality of Life and Function at Three Different Times; Before Surgery, One Month After Surgery and Three Months After Surgery
| Questionnaire | Predicting Factor | Before Surgery | One Month After Surgery | Three Months After Surgery | |||
|---|---|---|---|---|---|---|---|
| Unstandardized Beta Coefficients (95.0% Confidence Interval) | p-value | Unstandardized Beta Coefficients (95.0% Confidence Interval) | p-value | Unstandardized Beta Coefficients (95.0% Confidence Interval) | p-value | ||
| MDADI | Age | −0.846 (−4.104, 2.412) | 0.610 | 3.391 (−.203, 6.985) | 0.064 | 0.050 (−0.414,0.514) | 0.832 |
| Occupation | −1.786 (−3.682,0.110) | 0.065 | −1.897 (−4.082, 0.288) | 0.089 | 0.124 (−0.146,0.394) | 0.367 | |
| Denture | 3.370 (−0.942,7.681) | 0.125 | −14.393 (−19.288, −9.498) | 0.000 | 0.453 (−0.161,1.068) | 0.148 | |
| Drinking | 1.843 (−0.302,3.987) | 0.092 | 0.032 (−2.600,2.664) | 0.981 | 0.346 (0.049, 0.644) | 0.023 | |
| Diet | 0.521 (−6.741, 7.784) | 0.888 | 0.673 (−8.241,9.586) | 0.882 | 1.026 (0.075, 1.977) | 0.035 | |
| EAT-10 | Occupation | −1.114 (−1.808, −0.419) | 0.002 | −0.427 (−1.159,0.306) | 0.252 | −0.027 (−0.258,0.205) | 0.821 |
| Drinking | 0.791 (−0.045, 1.627) | 0.064 | −0.146 (−0.974,0.683) | 0.729 | −0.124 (−.385,0.138) | 0.354 | |
| Marriage | 0.812 (−.368,1.992) | 0.176 | 1.029 (−.018, 2.076) | 0.054 | −0.310 (−0.666,0.047) | 0.088 | |
| Denture | 2.135 (0.393,3.877) | 0.016 | −3.592 (−5.020, −2.165) | 0.000 | −.0200 (−0.726,0.326) | 0.455 | |
| Tumor size | 0.470 (−1.049,1.988) | 0.543 | 1.305 (−0.071, 2.680) | 0.063 | −0.013 (−0.472,0.446) | 0.956 | |
| Tumor site | −0.769 (−2.704,1.167) | 0.435 | −1.983 (−3.809, −.157) | 0.033 | −0.029 (−0.614,0.556) | 0.921 | |
| FACT-H&N | Age | 0.838 (−0.022, 1.698) | 0.056 | −0.456 (−2.788,1.876) | 0.701 | −1.144 (−3.318,1.029) | 0.301 |
| Marriage | −0.803 (−1.574, −0.032) | 0.041 | −1.085 (−3.175,1.005) | 0.308 | 0.651 (−1.297,2.599) | 0.511 | |
| Graduation | −0.489 (−1.046, 0.068) | 0.085 | −0.496 (−2.120,1.128) | 0.548 | −0.138 (−1.652,1.376) | 0.858 | |
| Betelnut | 0.837 (0.406, 1.268) | 0.000 | −0.528 (−1.665,0.610) | 0.362 | −0.176 (−1.236,0.884) | 0.744 | |
| Denture | −5.365 (−6.425, −4.305) | 0.000 | −4.334 (−7.086, −1.581) | 0.002 | −0.713 (−3.589,2.164) | 0.626 | |
| Income | 0.214 (−0.416,0.845) | 0.504 | 1.294 (−0.123, 2.711) | 0.073 | 0.425 (−1.083,1.932) | 0.580 | |
| Diet | 1.389 (−0.639,3.417) | 0.179 | 7.536 (2.561, 12.512) | 0.003 | −0.049 (−4.894,4.797) | 0.984 | |
Note: Values in bold are statistically significant.
The use of EAT-10 scores as dependent variables revealed denture use (p = 0.007) and occupation (p = 0.001) as factors predicting the quality of life before the surgery, denture use (p = 0.000) and tumor site (p = 0.033) as factors predicting the quality of life at one month after the surgery, and illness duration (p = 0.005) as the factor predicting the quality of life at three months after the surgery.
The use of FACT-H&N scores as dependent variables revealed denture use (p = 0.000), betel nut consumption (p = 0.001), age (p = 0.014), and marital status (p = 0.041) as factors predicting the functional status before the surgery and denture use (p = 0.000) and diet (p = 0.007) as factors predicting the functional status at one month after the surgery. We could not identify any factor that predicted the functional status at three months after the surgery.
Discussion
Due to the limited available knowledge regarding the success of ALTFF reconstruction in tongue cancer patients, the present study aimed to assess the short-term quality of life, functional status, and their predictors in tongue cancer patients before and one and three months after ALTFF reconstruction. Our results revealed that the mean MDADI scores increased at one month after the surgery and then decreased three months after the surgery (F = 438.815, p = 0.00). This finding indicates that ALTFF reconstruction in tongue cancer patients is associated with a poorer quality of life due to the worsening of swallowing symptoms during the first month after the surgery, followed by an improvement after that. We think that a more prolonged period enhances the healing and recovery of a surgical site, in addition to allowing adequate time for psychological adaption. The finding of worsened swallowing symptoms during the first month after oral reconstruction is in accordance with the finding of Dwivedi et al20 Romer et al21 reported a similar result.
Moreover, they recommended only surgical excision without reconstruction for oral cancer patients, as it reconstruction is associated with a poorer quality of life due to the worsening of swallowing symptoms. Similarly, Dzioba et al22 reported that swallowing symptoms and other quality of life parameters improved with time. However, Zhen et al23 suggested an additional swallowing training program for patients during the recovery period will be help enhance the swallowing function and improve the quality of life.
We also found that the mean EAT-10 scores increased during the month after the surgery but decreased by the third month after the surgery (F = 330.382, p = 0.00). This finding indicates that the patients’ quality of life becomes poorer due to the worsening of swallowing symptoms during the first month after the ALTFF reconstruction of the tongue, followed by an improvement during the third month after the surgery. The finding of worsened swallowing symptoms is in accordance with the finding of Albergotti et al,24 who reported a poorer quality of life during the first month after the surgery, followed by an improvement thereafter. Similarly, Likhterov et al25 reported a poorer quality of life in terms of increased EAT-10 scores and worsened saliva weight. We recommend a prior explanation to patients of the expected deterioration in swallowing symptoms during the first month after the surgery, necessitating temporary feeding tube placement. We also recommend the enrollment of oral diet-eligible candidates in swallowing training programs.
The mean FACT-H&N scores also decreased during the first month after the surgery but increased by the third month after the surgery (F = 28.886, p = 0.00). This finding indicates the worsening of the patients’ functional status during the first month after the surgery, followed by an improvement thereafter. However, post hoc analysis with the Kruskal–Wallis test showed a nonsignificant improvement between the mean scores before and after the surgery (p = 0.53). Thus, despite a significant improvement in the patients’ functional status by the third month after the surgery, the ultimate result was more or less the same as before the surgery. Family social status and head and neck cancer (special) subitem scores at one month after the surgery were better than those before the surgery (p < 0.05). However, psychological, functional, and emotional subitem scores were poorer at one month after the surgery (p < 0.05). These results are consistent with Mochizuki et al,26 who demonstrated an improvement in all subitem scores, except for the psychological one. Bussu et al9 also reported similar results; however, they used a pedicle instead of a free flap.
Moreover, Koizumi et al27 reported an improvement in all five subitem scores after the surgery. We recommend postoperative psychological consultations for all tongue cancer patients undergoing ALTFF reconstruction. This recommendation is based on the finding of poor psychological subitem scores. However, as all the FACT-H&N subitem scores improved by the third month after the surgery, we recommend scheduling the aforementioned psychological intervention before the surgery and within one month after the surgery.
In the present study, denture use (p = 0.007) and occupation (p = 0.001) were found to be factors predicting the quality of life in terms of swallowing symptoms before the surgery. These results are in accordance with those of Hahn et al28 and Goswami et al,29 respectively. Age (p = 0.017), tumor site (p = 0.033), and denture use (p = 0.000) were found to significantly predict the quality of life at one month after the surgery. Fujimoto et al30 reported similar findings regarding age; however, their study had a follow-up period of six months. Meier et al31 reported similar findings regarding the tumor site, while Hahn et al reported similar findings regarding denture use. We identified illness duration (p = 0.005), drinking habit (p = 0.023), and diet (p = 0.035) as factors predicting the patients’ quality of life at three months after the surgery. Our findings are in accordance with those of Khandelwal et al;32 however, their study had a longer follow-up period (ie, one to five years).
We also found that denture use (p = 0.000), betel nut consumption (p = 0.001), age (p = 0.014),30 and marital status (p = 0.041) were predictors of the patients’ functional status before the surgery. Marital status is an independent predictor of a better quality of life and functional status of patients with many types of cancers. Concerning tongue cancer, Sun et al33 demonstrated married patients as having better five-year functional improvement than unmarried patients. This finding has been linked to the social and psychological support provided by the spouse to the patient.34 Moreover, we found that diet (p = 0.007) and denture use (p = 0.000) were predictors of the patients’ functional status three months after the surgery. Oral surgery could result in xerostomia, impaired chewing, or impaired swallowing, which could influence the patients’ diet and thereby impact the patients’ nutritional status and ability to recover.35
Despite being promising, the findings of the present study should be interpreted with caution due to the several limitations of the study. The study involved a survey and was susceptible to nonresponse bias. Several measures were taken to mitigate the same. The STROBE tool was used to reduce reporting and publication biases. Therefore, more robust research mitigating the biases encountered in the present study needs to be conducted. Moreover, the present study lacked objective functional measures, such as videofluoroscopic evaluation, fiberoptic endoscopic evaluation of swallowing, and oropharyngoesophageal scintigraphic evaluation; therefore, robust studies utilizing these tools for evaluation are required. The strength of the present study is that our findings contribute further to the existing literature regarding the functional status and quality of life of patients undergoing ALTFF reconstruction.
Conclusion
Tongue cancer patients have a poorer quality of life due to the worsening of swallowing symptoms and function during the first month after ALTFF reconstruction, followed by a significant improvement thereafter. We recommend postoperative swallowing training programs for all patients undergoing ALTFF reconstruction. Moreover, we recommend case-oriented psychological interventions, according to the risk mentioned above factors, to help patients cope with the expected deterioration in the quality of life and functional status during the first month after the surgery.
Funding Statement
No funds were given.
Abbreviations
ALTFF, anterolateral free flap; MDADI, MD Anderson Dysphagia Inventory; EAT-10, Eating Assessment Tool; FACT-H&N, Functional Assessment of Cancer Therapy-Head and Neck; IRB, Institutional Review Board; STROBE, STrengthening the Reporting of Observational Studies in Epidemiology.
Data Sharing Statement
The datasets used and analyzed in the present study are available from the corresponding author on reasonable request.
Ethical Approval and Informed Consent
Approval to conduct this study was obtained from the Institutional Review Board (IRB) of Central South University, Hunan Province, People’s Republic of China (approval number: 2019014). Written informed consent was obtained from all participants.
Author Contributions
All authors made substantial contributions to the conception and design, acquisition of data, and analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed on the journal to which the article will be submitted; gave the final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare no competing interests.
References
- 1.Ghantous Y, Yaffi V, Abu-Elnaaj I. [Oral cavity cancer: epidemiology and early diagnosis]. Refu’at Ha-Peh Veha-Shinayim. 2015;32(3):55–63, 71. Hebrew. [PubMed] [Google Scholar]
- 2.Kingsley K, O’Malley S, Ditmyer M, Chino M. Analysis of oral cancer epidemiology in the US reveals state-specific trends: implications for oral cancer prevention. BMC Public Health. 2008;8(1):87. doi: 10.1186/1471-2458-8-87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sarkaria JN, Harari PM. Oral tongue cancer in young adults less than 40 years of age: rationale for aggressive therapy. Head Neck. 1994;16(2):107–111. doi: 10.1002/hed.2880160202 [DOI] [PubMed] [Google Scholar]
- 4.Paderno A, Morello R, Piazza C. Tongue carcinoma in young adults: a review of the literature. Acta Otorhinolaryngol Italica. 2018;38(3):175–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ng JH, Iyer NG, Tan MH, Edgren G. Changing epidemiology of oral squamous cell carcinoma of the tongue: a global study. Head Neck. 2017;39(2):297–304. doi: 10.1002/hed.24589 [DOI] [PubMed] [Google Scholar]
- 6.Sgaramella N, Gu X, Boldrup L, et al. Searching for new targets and treatments in the battle against squamous cell carcinoma of the head and neck, with specific focus on tumours of the tongue. Curr Top Med Chem. 2018;18(3):214–218. doi: 10.2174/1568026618666180116121624 [DOI] [PubMed] [Google Scholar]
- 7.Patel UA, Hartig GK, Hanasono MM, Lin DT, Richmon JD. Locoregional flaps for oral cavity reconstruction: a review of modern options. Otolaryngol Head Neck Surg. 2017;157(2):201–209. doi: 10.1177/0194599817700582 [DOI] [PubMed] [Google Scholar]
- 8.Dziegielewski PT, Ho ML, Rieger J, et al. Total glossectomy with laryngeal preservation and free flap reconstruction: objective functional outcomes and systematic review of the literature. Laryngoscope. 2013;123(1):140–145. doi: 10.1002/lary.23505 [DOI] [PubMed] [Google Scholar]
- 9.Bussu F, Salgarello M, Adesi LB, et al. Oral cavity defect reconstruction using anterolateral thigh free flaps. B-ENT. 2011;7(1):19–25. [PubMed] [Google Scholar]
- 10.Deshmukh A, Kannan S, Thakkar P, Chaukar D, Yadav P, D’Cruz A. Tongue flap revisited. J Cancer Res Ther. 2013;9(2):215–218. doi: 10.4103/0973-1482.113354 [DOI] [PubMed] [Google Scholar]
- 11.Minkara A, Simmons MR, Goodale A, Patil YJ. Subjective morbidity following radial free flap reconstruction in head and neck tumour patients. J Laryngol Otol. 2019;133(3):230–235. doi: 10.1017/S0022215119000197 [DOI] [PubMed] [Google Scholar]
- 12.Tong X-J, Tang Z-G, Shan Z-F, Guo X-C. The anterolateral thigh flap for soft tissue reconstruction in patients with tongue squamous cell carcinoma. World J Surg Oncol. 2016;14(1):213. doi: 10.1186/s12957-016-0972-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhang J, Wang Y, Han X, Chen H. Comparison of clinical results and quality of life in tongue cancer patients undergoing submental island flap and radial forearm free flap reconstruction. J Oral Maxillofac Surg. 2020;78(9):1639–1644. doi: 10.1016/j.joms.2020.04.045 [DOI] [PubMed] [Google Scholar]
- 14.Cai YC, Li C, Zeng DF, et al. Comparative analysis of radial forearm free flap and anterolateral thigh flap in tongue reconstruction after radical resection of tongue cancer. ORL. 2019;81(5–6):252–264. doi: 10.1159/000502151 [DOI] [PubMed] [Google Scholar]
- 15.Kano S, Sakashita T, Tsushima N, et al. Validation of the 8th edition of the AJCC/UICC TNM staging system for tongue squamous cell carcinoma. Int J Clin Oncol. 2018;23(5):844–850. doi: 10.1007/s10147-018-1276-5 [DOI] [PubMed] [Google Scholar]
- 16.Chen AY, Frankowski R, Bishop-Leone J, et al. The development and validation of a dysphagia-specific quality-of-life questionnaire for patients with head and neck cancer: the M. D. Anderson dysphagia inventory. Arch Otolaryngol Head Neck Surg. 2001;127(7):870–876. [PubMed] [Google Scholar]
- 17.Belafsky PC, Mouadeb DA, Rees CJ, et al. Validity and reliability of the Eating Assessment Tool (EAT-10). Ann Otol Rhinol Laryngol. 2008;117(12):919–924. doi: 10.1177/000348940811701210 [DOI] [PubMed] [Google Scholar]
- 18.Chang JT, Chang CH, Juang YY, et al. Internal consistency of the traditional Chinese character version of the Functional Assessment of Cancer Therapy-Head and Neck (FACT-H&N). Chang Gung Med J. 2008;31(4):384–39419. [PubMed] [Google Scholar]
- 19.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344–349. PMID: 18313558. doi: 10.1016/j.jclinepi.2007.11.008 [DOI] [PubMed] [Google Scholar]
- 20.Dwivedi RC, Chisholm EJ, Khan AS, et al. An exploratory study of the influence of clinico-demographic variables on swallowing and swallowing-related quality of life in a cohort of oral and oropharyngeal cancer patients treated with primary surgery. Eur Arch Otorhinolaryngol. 2012;269(4):1233–1239. doi: 10.1007/s00405-011-1756-y [DOI] [PubMed] [Google Scholar]
- 21.Romer CAE, Broglie Daeppen MA, Mueller M, Huber GF, Guesewell S, Stoeckli SJ. Long-term speech and swallowing function after primary resection and sentinel node biopsy for early oral squamous cell carcinoma. Oral Oncol. 2019;89:127–132. doi: 10.1016/j.oraloncology.2018.12.027 [DOI] [PubMed] [Google Scholar]
- 22.Dzioba A, Aalto D, Papadopoulos-Nydam G, et al. Functional and quality of life outcomes after partial glossectomy: a multi-institutional longitudinal study of the head and neck research network. J Otolaryngol Head Neck Surg. 2017;46(1):56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhen Y, Wang JG, Tao D, Wang HJ, Chen WL. Efficacy survey of swallowing function and quality of life in response to therapeutic intervention following rehabilitation treatment in dysphagic tongue cancer patients. Eur J Oncol Nurs. 2012;16(1):54–58. doi: 10.1016/j.ejon.2011.03.002 [DOI] [PubMed] [Google Scholar]
- 24.Albergotti WG, Jordan J, Anthony K, et al. A prospective evaluation of short-term dysphagia after transoral robotic surgery for squamous cell carcinoma of the oropharynx. Cancer. 2017;123(16):3132–3140. doi: 10.1002/cncr.30712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Likhterov I, Ru M, Ganz C, et al. Objective and subjective hyposalivation after treatment for head and neck cancer: long-term outcomes. Laryngoscope. 2018;128(12):2732–2739. doi: 10.1002/lary.27224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mochizuki Y, Matsushima E, Omura K. Perioperative assessment of psychological state and quality of life of head and neck cancer patients undergoing surgery. Int J Oral Maxillofac Surg. 2009;38(2):151–159. doi: 10.1016/j.ijom.2008.11.007 [DOI] [PubMed] [Google Scholar]
- 27.Koizumi A, Matsushima E, Mochizuki Y, Omura K, Amagasa T. Changes in the psychological characteristics of oral cancer patients in the perioperative period: a quantitative evaluation. J Med Dent Sci. 2013;60(1):41–53. [PubMed] [Google Scholar]
- 28.Hahn TR, Kruskemper G, Enkling N, Kubler NR. [On quality of life after surgical therapy of oral cancer - a retrospective multi-center study: the connection between dedentition, denture, quality of life, and dysphagia, and the resulting rehabilitation schemes]. Mund Kiefer Gesichtschir. 2007;11(1):27–32. Germany. doi: 10.1007/s10006-006-0038-0 [DOI] [PubMed] [Google Scholar]
- 29.Goswami S, Gupta SS. How Patients of oral cancer cope up with impact of the disease? A Qualitative Study in Central India. Indian J Palliat Care. 2019;25(1):103–109. doi: 10.4103/IJPC.IJPC_9_19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fujimoto Y, Hasegawa Y, Yamada H, Ando A, Nakashima T. Swallowing function following extensive resection of oral or oropharyngeal cancer with laryngeal suspension and cricopharyngeal myotomy. Laryngoscope. 2007;117(8):1343–1348. doi: 10.1097/MLG.0b013e3180686590 [DOI] [PubMed] [Google Scholar]
- 31.Meier JK, Schuderer JG, Zeman F, et al. Health-related quality of life: a retrospective study on local vs. microvascular reconstruction in patients with oral cancer. BMC Oral Health. 2019;19(1):62. doi: 10.1186/s12903-019-0760-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Khandelwal A, Neeli A, Gadiyar A, Khandelwal A. Assessment of quality of life of patients 1–5 years after treatment for oral cancer. Indian J Dent Res. 2017;28(5):538–544. doi: 10.4103/ijdr.IJDR_97_17 [DOI] [PubMed] [Google Scholar]
- 33.Sun W, Qiu Z, Tan W, et al. The influence of marital status on survival in patients with oral tongue squamous cell carcinoma. Oncotarget. 2017;8(47):82092–82102. doi: 10.18632/oncotarget.18538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shi X, Zhang -T-T, Hu W-P, Ji Q-H. Marital status and survival of patients with oral cavity squamous cell carcinoma: a population-based study. Oncotarget. 2017;8(17):28526–28543. doi: 10.18632/oncotarget.16095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gellrich N-C, Handschel J, Holtmann H, Krüskemper G. Oral cancer malnutrition impacts weight and quality of life. Nutrients. 2015;7(4):2145–2160. doi: 10.3390/nu7042145 [DOI] [PMC free article] [PubMed] [Google Scholar]