Abstract
Background:
Hair dyes are commonly used for the concealment of grey hair in India. The pigmentary alterations produced by hair dyes on the face and neck have not received sufficient attention.
Aims:
To study the pigmentary alterations on the face and neck in hair dye users, and identify possible risk factors associated with the face and neck hyperpigmentation.
Methods:
A hospital-based descriptive cross-sectional study was done on consecutive hair dye users. A detailed history was taken, and a clinical examination was done to record the pigmentary alterations. The patterns, areas affected, the intensity of hyperpigmentation, percentage of the area involved and risk factors were noted.
Results:
One hundred and twenty patients were included in the study. Around 118 (98.3%) patients had hyperpigmentation over face and/or neck: 16 (13.3%) barely perceivable, 40 (33.3%) mild, 44 (36.7%) moderate, and 18 (15%) severe pigmentation. The lateral forehead (106, 88.3%), the helix of the ear (106, 88.3%), central forehead (97, 80.8%), and zygomatic area (92, 76.7%) were the most frequently affected areas in our study. Fourteen patients (11.7%) had depigmented macules on the scalp and/or lips.
Conclusion:
Pigmentary alterations, particularly hyperpigmentation over the upper face and ears are common with the use of hair dyes. The skin type may play a role in the intensity of hyperpigmentation.
Keywords: Contact dermatitis, hair dye, melanosis
Introduction
The face and neck are commonly affected in several diverse acquired pigmentary disorders such as melasma, photoallergic and phototoxic drug reactions, lichen planus pigmentosus, pigmented contact dermatitis, post-inflammatory hyperpigmentation, ashy dermatosis, erthromelanosis follicularis faciei et colli, erythrose peribuccale of Brocq, ephelides, maturational dyschromia, acanthosis nigricans, and exogenous ochronosis.[1,2] Hair dyes have been implicated in some reports of facial pigmented contact dermatitis, lichen planus pigmentosus, acquired dermal macular hyperpigmentation, and depigmentation.[3,4,5,6,7] However, there is a paucity of studies on the pigmentary alterations on the face and neck in hair dye users. Hence our objective was to study the pigmentary alterations on the face and neck in hair dye users and identify possible risk factors associated with the face and neck hyperpigmentation.
Methods
Setting
A hospital-based descriptive cross-sectional study was done in the department of dermatology of a tertiary care institute located in south India. The study was done for a period of 1 year from November 2017 to October 2018.
Study participants
Consecutive consenting semi-permanent/permanent hair dye users of both genders, and above 18 years of age, attending the dermatology outpatient department were included in the study. Patients with other congenital or acquired causes of face and neck pigmentary alterations, including the use of cosmetics, fairness creams, leave on shampoos, hair oils other than coconut oil, herbal agents such as turmeric and topical or systemic drugs, or systemic conditions known to be associated with pigmentary alterations were excluded from the study. Patients with depigmentation were included only if the depigmentation started after the use of hair dyes, without any history of preexisting dermatoses, and if the onset of depigmentation was at or near the site where hair dyes were used. Pregnant and lactating women and irregular hair dye users (frequency of use less than once in 6 months) were also excluded from the study.
Study procedure
Institutional ethics committee permission was obtained and patients who met the selection criteria were included. A detailed history was taken and clinical examination is done. Data collected included age, gender, Fitzpatrick skin type, and characteristics of hair dye use (frequency of use, duration, color preference, method of application, duration of application, type of hair dye, hair dye brand used, listed hair dye ingredients, total number of dyes used, and associated symptoms).[8] Pigmentary alterations, including hyperpigmentation and depigmentation, were noted. The pattern, areas affected, the intensity of hyperpigmentation (graded subjectively as 0-absence of pigmentation, 1-barely perceivable pigmentation, 2-mild, 3-moderate, 4-severe) and the percentage of the area involved was noted. The distribution of hyperpigmentation was subdivided based on the cosmetic units and subunits of the face.[9] Pigmentation over the transverse nasal crease, nasolabial fold, mental crease, retro-auricular crease, hairline, and neck was also noted. Patients with hyperpigmentation who consented for patch testing were patch tested with paraphenylene diamine and the Indian Cosmetic and Fragrance series. The results were read at 48 and 96 h, according to the International Contact Dermatitis Research Group guidelines.[10]
Statistical analysis
Data were entered in Microsoft Office Excel and SPSS statistical package version 24.0 (IBM Corp, Armonk, NY, USA) was used for data analysis. The proportion of patients with hyperpigmentation following hair dye use and its severity was calculated and reported with its 95% confidence interval (CI). Unadjusted prevalence ratios (PRs) and their 95% CI were calculated to establish the strength of their association with the risk factor. Those variables with a P value of < 0.10 in the bivariate analysis were included in the multivariate binary regression analysis to calculate adjusted prevalence ratios. The level of significance was set at 5%.
Results
One hundred and twenty patients were included in the study. There were 83 (69.2%) males and 37 (30.8%) females (male:female = 2.2:1). The mean age of the study population was 47 (±10 SD) years. Twenty-one (17.5%) patients had Fitzpatrick skin type IV and 99 patients have Fitzpatrick skin type V. The characteristics of hair dye use are listed in Table 1. The duration of hair dye use among the study participants ranged from 7 months to 20 years. The median duration of hair dye use among the participants was 5.5 years with an IQR of 2 to 7 years. Twenty-six (21.7%) patients used hair dye over both scalp and mustache, and one patient used hair dye over both scalp and beard (0.8%). Thirty (25%) patients reported symptoms such as pruritus, burning sensation, headache, and/or dizziness on hair dye applications. The brands used by the patients were Banjaras black henna, Godrej expert rich crème, Garnier color naturals, Loreal Inoa, VIP hair color shampoo, Black rose hair color shampoo, Supervasmol 33 kesh kala, Indica, and one unlabeled hair dye. Six patients gave a history of the use of V care herbal hair dye (only botanical agents listed as ingredients), in addition to the regular hair dyes. Labels that were incomplete or were potentially misleading to consumers (e.g., Black henna- Figure 1 and Ayurprash - Figure 2) were also noted.
Table 1.
Characteristics of hair dye use
| Characteristics of hair dye use | Number of patients, (%) n=120 | |
|---|---|---|
| Duration of hair dye use | <1 year | 18 (15) |
| 1–5 years | 42 (35) | |
| >5 years | 60 (50) | |
| Frequency of hair dye application | <=once in 30 days | 96 (80) |
| >once in 30 days | 24 (20) | |
| Number of hair dyes used | 1 | 88 (73.3) |
| 2 | 25 (20.8) | |
| 3 | 7 (5.83) | |
| Colour preference | Black | 119 (99.1) |
| Brown | 1 (0.83) | |
| Symptoms | Symptoms present | 30 (25) |
| Asymptomatic | 90 (75) |
Figure 1.
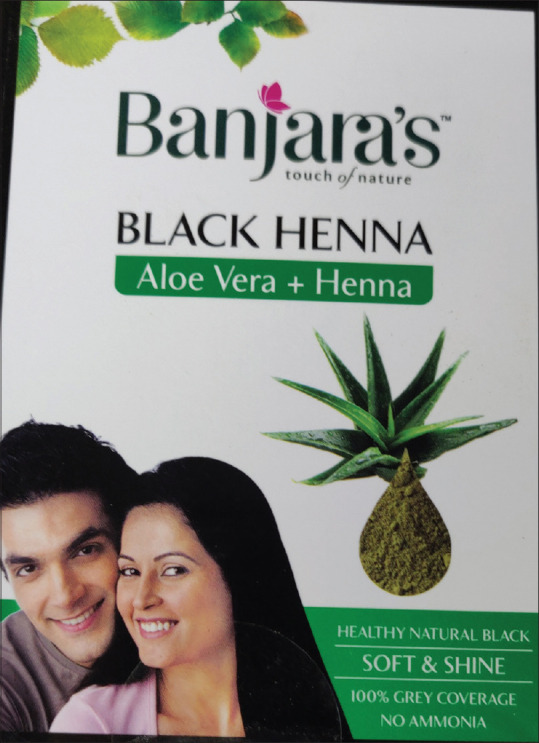
Misleading label (black henna) which contained paraphenylene diamine with henna
Figure 2.

The “ayurprash” label (the dye contains chemicals such as paraphenylene diamine) may potentially mislead the consumers
One hundred and eighteen (98.3%) patients had hyperpigmentation over face and/or neck [Figure 3a-e]: 16 (13.3%) barely perceivable 40 (33.3%) mild, 44 (36.7%) moderate, and 18 (15%) severe pigmentation. The distribution of hyperpigmentation is given in Table 2. Among the 118 patients, 78 (66.1%) had blotchy, 39 (33.1%) diffuse, and one (0.8%) patient had both diffuse and reticular pigmentation. Fifty-four (45.8%) of these patients had pigmentation affecting more than 30% of the face and neck.
Figure 3.

(a-e) Face and ear hyperpigmentation in hair dye users
Table 2.
Distribution of hyperpigmentation on face and neck of the study participants
| Area of involvement | Frequency, (%) n=120 | |
|---|---|---|
| Forehead | 1a: central | 97 (80.8) |
| 1b: lateral | 106 (88.3) | |
| 1c: brow | 8 (6.7) | |
| Nose | 2a: dorsum | 26 (21.7) |
| 2b: lateral wall | 30 (25) | |
| 2c: ala | 26 (21.7) | |
| 2d: tip | 2 (1.7) | |
| 2e: columella | 6 (5) | |
| Eyelid | 3a: superior | 82 (68.3) |
| 3b: inferior | 80 (66.7) | |
| 3c: lateral canthus | 29 (24.2) | |
| 3d: medial canthus | 43 (35.8) | |
| Cheek | 4a: infraorbital | 41 (34.2) |
| 4b: zygomatic | 92 (76.7) | |
| 4c: buccal | 36 (30) | |
| 4d: parotid-massetric | 49 (40.8) | |
| Upper lip | 5a: philtrum | 23 (19.2) |
| 5b: lateral | 23 (19.2) | |
| 5c: vermillion | 38 (31.7) | |
| Lower lip | 6a: central | 23 (19.2) |
| 6b: vermillion | 39 (32.5) | |
| Chin | 7 | 79 (65.8) |
| Ear | 8a: helix | 106 (88.3) |
| 8b: antihelix | 62 (51.7) | |
| 8c: concha | 11 (9.2) | |
| 8d: earlobe | 52 (43.3) | |
| 8e: retroauricular | 58 (48.3) | |
| Nasal crease | 46 (38.3) | |
| Nasolabial fold | 25 (20.8) | |
| Mental crease | 21 (17.5) | |
| Hair line | 58 (48.3) | |
| Retroauricular crease | 19 (15.8) |
The association between the intensity of pigmentation and possible risk factors is given in Table 3. Bivariate analysis revealed male gender (P = 0.03) and Fitzpatrick skin type V (P = 0.009) as risk factors for moderate/severe pigmentation. After adjustment of 95% CI, multivariate analysis revealed Fitzpatrick skin type V (0.01) as a risk factor for moderate/severe pigmentation. Among the hair dye brands, eight of the eleven (72.7%) patients who used Supervasmol 33 kesh kala had hyperpigmentation over more than 30% of face and neck (P = 0.05). We encountered negative patch test reactions in a limited number of sixteen patients that we patch tested with paraphenylene diamine and the Indian Cosmetic and Fragrance Series.
Table 3.
Association between intensity of pigmentation and age, gender, skin type, patterns of use, and the presence of symptoms
| Characteristics | Number of patients (%) n=120 | Moderate/severe pigmentation (%) n=62 | Unadjusted PR (95%CI) | P (bivariate analysis) | Adjusted PR (95% CI) | P (multivariate analysis) | |
|---|---|---|---|---|---|---|---|
| Age in years | <40 | 25 (20.8) | 12 (48) | 1 (Reference) | NA | NA | |
| ≥40 | 95 (79.2) | 50 (52.6) | 1.1 (0.7–1.7) | 0.69 | |||
| Gender | Male | 83 (69.2) | 49 (59) | 1.7 (1.0–2.7) | 0.03* | 1.5 (0.96–2.3) | 0.07 |
| Female | 37 (30.8) | 13 (35.1) | 1 (Reference) | 1 (Reference) | |||
| Skin type | Type IV | 21 (17.5) | 3 (14.3) | 1 (Reference) | 1 (Reference) | ||
| Type V | 99 (82.5) | 59 (59.6) | 4.2 (1.4–12.0) | 0.009* | 3.8 (1.3–11.0) | 0.01* | |
| Duration of hair dye use | <1 year | 18 (15) | 10 (55.6) | 1 (Reference) | |||
| 1–5 years | 42 (35) | 17 (40.5) | 0.7 (0.4–1.3) | 0.26 | NA | NA | |
| <5 years | 60 (50) | 35 (58.3) | 1.0 (0.6–1.7) | 0.83 | |||
| Frequency of use | <=once in 30 days | 96 (80) | 53 (55.2) | 1.5 (0.8–2.5) | 0.10 | 1.4 (0.9–2.3) | 0.15 |
| >once in 30 days | 24 (20) | 9 (37.2) | 1 (Reference) | 1 (Reference) | |||
| Duration of each | <10 minutes | 18 (15) | 7 (38.9) | 1 (Reference) | |||
| application | 11–60 minutes | 97 (80.8) | 52 (53.6) | 1.4 (0.7–2.5) | 0.30 | NA | NA |
| >60 minutes | 5 (4.2) | 3 (60) | 1.5 (0.6–3.8) | 0.35 | |||
| Symptoms | Symptoms present | 30 (25) | 14 (46.7) | 1 (Reference) | NA | NA | |
| Asymptomatic | 90 (75) | 48 (53.3) | 1.1 (0.7–1.7) | 0.54 |
PR=Prevalence Ratio, CI=Confidence Interval, NA=Not applicable, *Statistically significant (P≤0.05)
Fourteen patients (11.7%) reported depigmentation after the use of hair dyes. Ten male patients who dyed both their hair and mustache had depigmentation of the lower lips. Two female patients had depigmented macules on the scalp, upper, and lower lips [Figure 4a and b], and one female patient had depigmented macules along the retro-auricular crease. Depigmented macules restricted to the scalp were seen in one male patient.
Figure 4.

(a) A patient with depigmented macules on the scalp; (b) Depigmented macules on the lips in the same patient
Discussion
Indian dermatologists observe hair dye-induced pigmentation on a day-to-day basis, the diagnosis is primarily based on a temporal onset and exclusion of other causes. The mechanisms are unclear, and there are several factors that hamper the identification of the etiological agents [Table 4]. Hyperpigmentation of varying intensities, patterns, and distribution was seen among the hair dye users in our study. In a Korean study, Han et al. reported hyperpigmentation in 3.8% of 105 patients with hair dye allergies.[11] In an Indian study, Patel et al. reported pigmentation in 10% of 263 hair dye users in India.[12] However, further details of the pigmentation were not described. Woo et al. reported pigmented contact dermatitis with diffuse pigmentation over face and neck in 11 patients following the use of henna hair dyes. The lateral face including the forehead, temple, and neck near hairline were the most frequently affected areas in their study.[4] The lateral forehead (106, 88.3%), the helix of the ear (106, 88.3%), central forehead (97, 80.8%) and zygomatic area (92,7 6.7%) were the most frequently affected areas in our study. The varying anatomy of the cosmetic units and distance from the scalp may play a role in the susceptibility to pigmentation.
Table 4.
Challenges in identifying the incriminating agent of hair dye induced pigmentation
| 1. Availability of unlabeled hair dyes/incompletely labelled hair dyes/hair dyes with misleading labels in the Indian market. |
| 2. Concentration of individual ingredients are not mentioned. |
| 3. The ingredients listed may differ from the actual ingredients due to poor regulation. |
| 4. The composition of commercially marketed hair dyes change at frequent intervals. |
| 5. Limited toxicological data on pigmentary changes produced by hair dye ingredients. |
Skin color was a risk factor for the intensity of pigmentation on multivariate analysis. Post-inflammatory hyperpigmentation, including the distinct morphological types such as pigmented contact dermatitis and lichen planus pigmentosus, is more common in darker skin types.[13] This may also play a role in the underreporting of pigmentation despite the global use of hair dyes. Paraphenylenediamine is more common and is present in higher concentrations in non-European dyes compared to European dyes. Paraphenylene diamine, after mixing in oxidative conditions, should not exceed 2% and toluene-2,5- diamine should not exceed 4%.[14] Higher concentrations of paraphenylene diamine in the poorly regulated dyes may also play a role in the higher proportion of pigmentary alterations. Some of our patients used unlabelled and incomplete labeled hair dyes. In addition, brands that contained paraphenylene diamine had labels such as “black henna” and “ayurprash” that can potentially mislead or confuse consumers about the safety of the product. Most patients (72.7%) who used Supervasmol 33 kesh kala had pigmentation affecting more than 30% of the face and neck (P = 0.05). The actual content of the hair dyes in the Indian market and the potential of individual chemicals in pigmentation needs to be explored.
Hair dyes have been implicated in pigmented contact dermatitis and lichen planus pigmentosus[5,15] Bishnoi et al. reported contact sensitization to hair dyes as an etiological factor in one-third of the patients with acquired dermal macular hyperpigmentation. Oral or cutaneous lichen planus was significantly higher in the patients without positive patch test results.[6] However, associated classical papular cutaneous or oral lichen planus was not seen in any patient in our study. We could patch test only a limited number of patients in our study. However, facial pigmentation may occur even in the absence of positive patch test reactions.[5] This suggests that mechanisms other than contact sensitization may be involved. Histopathological characteristics of hair dye induced pigmentation are still not clear. The histopathological features of lichen planus pigmentosus and pigmented contact dermatitis overlap and a skin biopsy is not of definite diagnostic value in differentiating the two conditions.[5] Maturational hyperpigmentation, which also predominantly affects the cheeks, is a close differential for hair dye-induced pigmentation. The exact etiology of maturational hyperpigmentation is not clear. Factors such as obesity and allergies have been implicated in its etiology.[16] Although obese patients, patients with acanthosis nigricans or a history of atopy were excluded from our study; a contributory role of hair dyes in maturational hyperpigmentation of nonobese patients' needs to be explored.
Some patients (11.7%) in our study developed depigmentation over the scalp and/or lips. Permanent hair dyes contain potent contact allergens and toxic phenols that are similar to chemical inducers of vitiligo. Wu et al., in a large cohort of women, demonstrated an association of vitiligo with the use of permanent hair dyes.[17] Ghosh et al. attributed 27.4% of 864 cases of chemical leukoderma to hair dyes.[18] However, depigmentation produced by chemicals cannot be clinically or histopathologically differentiated from vitiligo and hence the term “chemical-induced vitiligo” has been used to describe depigmentation secondary to chemical exposure.[7]
Patients continued to use hair dyes despite the development of pigmentation. Black (99.1%) was the preferred hair color. Lack of awareness about the pigmentary alterations or the social pressures to conceal grey hair may have led to the continued use of hair dyes.
Limitations
Patch testing of all patients, photo-patch testing, dermatoscopy, and histopathological examination were not done in our study. We used subjective scores for grading the degree of pigmentation instead of colorimeters or spectrophotometers. The role of other contributory factors for pigmentation, such as sunlight, sweat and pollution, could not be explored.
Conclusion
Pigmentary alterations, particularly hyperpigmentation over the upper face and ears, are common in hair dye users. The lateral forehead, the helix of the ear, central forehead and ear helix are the most commonly affected areas. The skin type may play a role in the intensity of hyperpigmentation. The contents of the hair dyes available in the Indian market are often unclear due to inadequate labeling. The etiological ingredients and the possible mechanisms of hyperpigmentation and depigmentation need to be explored in further studies. Strict regulation of the contents and labeling of hair dyes is needed.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
This study was partially funded by the reseach funds of Sri Manakula Vinayagar Medical College and Hospital.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Ricciardo B, Kumarasinghe P. A clinical classification of pigmentary disorders. In: Kumarasinghe P, editor. Pigmentary Skin Disorders. Cham: Springer; 2018. pp. 1–26. [Google Scholar]
- 2.Vashi NA, Kundu RV. Facial hyperpigmentation: Causes and treatment. Br J Dermatol. 2013;169:41–56. doi: 10.1111/bjd.12536. [DOI] [PubMed] [Google Scholar]
- 3.On HR, Hong WJ, Roh MR. Low-pulse energy Q-switched Nd: YAG laser treatment for hair-dye-induced Riehl's melanosis. J Cosmet Laser Ther. 2015;17:135–8. doi: 10.3109/14764172.2015.1007058. [DOI] [PubMed] [Google Scholar]
- 4.Woo YR, Kim JS, Lim JH, Choi JY, Kim M, Yu DS, et al. Acquired diffuse slate-grey facial dyspigmentation due to henna: An unrecognized cause of pigment contact dermatitis in Korean patients. Eur J Dermat. 2018;28:644–8. doi: 10.1684/ejd.2018.3404. [DOI] [PubMed] [Google Scholar]
- 5.Sharma VK, Gupta V, Pahadiya P, Vedi KK, Arava S, Ramam M. Dermoscopy and patch testing in patients with lichen planus pigmentosus on face: A cross-sectional observational study in fifty Indian patients. Ind J Dermatol Venereol Leprol. 2017;83:656–62. doi: 10.4103/ijdvl.IJDVL_469_16. [DOI] [PubMed] [Google Scholar]
- 6.Bishnoi A, Vinay K, Parsad D, Handa S, Saikia UN, Muthu SK. Contact sensitization to hair colors in acquired dermal macular hyperpigmentation: Results from a patch and photo patch-test study of 108 patients. J Eur Acad Dermatol Venereol. 2019;33:1349–57. doi: 10.1111/jdv.15576. [DOI] [PubMed] [Google Scholar]
- 7.Harris JE. Chemical-induced vitiligo. Dermatol Clin. 2017;35:151–61. doi: 10.1016/j.det.2016.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wilkinson DS, Fregert S, Magnusson B, Bandmann HJ, Calnan CD, Cronin E. Terminology of contact dermatitis. Acta Derm Venereol. 1970;50:287–92. [PubMed] [Google Scholar]
- 9.Roberts WE. Skin type classification systems old and new. Dermatol Clin. 2009;27:529–33. doi: 10.1016/j.det.2009.08.006. [DOI] [PubMed] [Google Scholar]
- 10.Russo F, Linares M, Iglesias ME, Martínez-Amo JL, Cabo F, Tercedor J, et al. Reconstruction techniques of choice for the facial cosmetic units. Actas Dermosifiliograf. 2017;108:729–37. doi: 10.1016/j.ad.2017.02.017. [DOI] [PubMed] [Google Scholar]
- 11.Han JH, Lee HJ, Bang CH, Lee JH, Park YM, Lee JY. P-phenylenediamine hair dye allergy and its clinical characteristics. Ann Dermatol. 2018;30:316–21. doi: 10.5021/ad.2018.30.3.316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Patel D, Narayana S, Krishnaswamy B. Trends in use of hair dye: A cross-sectional study. Int J Trichol. 2013;5:140. doi: 10.4103/0974-7753.125610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rodrigues M, Ayala-Cortés AS. Post-inflammatory hyperpigmentation. In: Kumarasinghe P, editor. Pigmentary Skin Disorders. Cham: Springer; 2018. pp. 197–208. [Google Scholar]
- 14.Antelmi A, Bruze M, Zimerson E, Engfeldt M, Young E, Persson L, et al. Evaluation of concordance between labelling and content of 52 hair dye products: Overview of the market of oxidative hair dye. Eur J Dermatol. 2017;27:123–31. doi: 10.1684/ejd.2016.2934. [DOI] [PubMed] [Google Scholar]
- 15.Shenoi SD, Rao R. Pigmented contact dermatitis. Ind J Dermatol Venereol Leprol. 2007;73:285–7. doi: 10.4103/0378-6323.35728. [DOI] [PubMed] [Google Scholar]
- 16.Alexander AM. Maturational hyperpigmentation. In: Kelly AP, Taylor SC, editors. Dermatology for Skin of Color. New York: McGraw-Hill; 2009. p. 344. [Google Scholar]
- 17.Wu S, Li WQ, Cho E, Harris JE, Speizer F, Qureshi AA. Use of permanent hair dyes and risk of vitiligo in women. Pigment Cell Melanoma Res. 2015;28:744–6. doi: 10.1111/pcmr.12402. [DOI] [PubMed] [Google Scholar]
- 18.Ghosh S, Mukhopadhyay S. Chemical leucoderma: A clinic-aetiological study of 864 cases in the perspective of a developing country. Br J Dermatol. 2009;160:40–7. doi: 10.1111/j.1365-2133.2008.08815.x. [DOI] [PubMed] [Google Scholar]


