Supplemental Digital Content is available in the text.
Keywords: cerebral hemorrhage; disease outbreaks; incidence; ischemic attack, transient; Italy
Background and Purpose:
We aimed to investigate the rate of hospital admissions for cerebrovascular events and of revascularization treatments for acute ischemic stroke in Italy during the coronavirus disease 2019 (COVID-19) outbreak.
Methods:
The Italian Stroke Organization performed a multicenter study involving 93 Italian Stroke Units. We collected information on hospital admissions for cerebrovascular events from March 1 to March 31, 2020 (study period), and from March 1 to March 31, 2019 (control period).
Results:
Ischemic strokes decreased from 2399 in 2019 to 1810 in 2020, with a corresponding hospitalization rate ratio (RR) of 0.75 ([95% CI, 0.71–0.80] P<0.001); intracerebral hemorrhages decreased from 400 to 322 (hospitalization RR, 0.81 [95% CI, 0.69–0.93]; P=0.004), and transient ischemic attacks decreased from 322 to 196 (hospitalization RR, 0.61 [95% CI, 0.51–0.73]; P<0.001). Hospitalizations decreased in Northern, Central, and Southern Italy. Intravenous thrombolyses decreased from 531 (22.1%) in 2019 to 345 in 2020 (19.1%; RR, 0.86 [95% CI, 0.75–0.99]; P=0.032), while primary endovascular procedures increased in Northern Italy (RR, 1.61 [95% CI, 1.13–2.32]; P=0.008). We found no correlation (P=0.517) between the hospitalization RRs for all strokes or transient ischemic attack and COVID-19 incidence in the different areas.
Conclusions:
Hospitalizations for stroke or transient ischemic attacks across Italy were reduced during the worst period of the COVID-19 outbreak. Intravenous thrombolytic treatments also decreased, while endovascular treatments remained unchanged and even increased in the area of maximum expression of the outbreak. Limited hospitalization of the less severe patients and delays in hospital admission, due to overcharge of the emergency system by COVID-19 patients, may explain these data.
The coronavirus disease 2019 (COVID-19) outbreak in Italy required the reorganization of the health care system and the application of strict rules of social containment. In the period February 20 to March 31, 2020, a 30% reduction of hospital admission for acute coronary syndrome was reported.1 Recent studies reported also a clear reduction in stroke admissions during this early phase of the COVID-19 outbreak.2,3
Aim of this study is to investigate possible changes in the rates of hospital admissions for cerebrovascular events and of revascularization treatments for acute ischemic stroke during the COVID-19 outbreak and to detect the possible relationship between changes in hospitalization and incidence of COVID-19.
Methods
We performed a multicenter study involving 93 (43 in Northern, 34 in Central, and 16 in Southern Italy) of the 190 Stroke Units covering the entire National territory in Italy. All the participating centers were members of the Italian Stroke Organization and included in the Italian Stroke Organization Monitor study for the assessment of acute stroke care standards across Italy. Participation was on a voluntary basis, and all Stroke Units were asked to join the project; participating centers included primary and secondary stroke centers located across the whole Italian territory. We collected information on hospitalizations for acute stroke or transient ischemic attack (TIA) and revascularization procedures over 2 study periods, from March 1 to March 31, 2020 (study period), and from March 1 to March 31, 2019 (control period). The system of care for stroke in some of the regions located in Northern Italy (Lombardia, Veneto, Emilia Romagna) changed during the worst period of COVID-19 outbreak because of creation of hospitals dedicated exclusively to COVID-19 patients. However, there was not any shortage of hospital beds dedicated to stroke, as patients were transported to different hospitals with stroke unit within the same region.
For the study period, deidentified data were prospectively retrieved from administrative codes following the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM), while data for the control period were retrospectively retrieved from the same administrative codes. Extracted data were checked with medical records to verify the accuracy of the diagnostic code. We considered the following diagnoses: ischemic strokes (ICD-9-CM codes 433–434), intracerebral hemorrhages (ICD-9-CM code 431), and TIAs (ICD-9-CM code 435). We also recorded revascularization procedures for ischemic stroke including intravenous thrombolysis alone (ICD-9-CM code 99.10), endovascular treatment alone (ICD-9-CM code 39.76), and combined treatment.
The patients’ sex, age, and diagnosis (ischemic stroke, intracerebral hemorrhage, and TIA) and type of revascularization procedure for acute ischemic stroke patients were reported in a computerized database for the two study periods. Data were classified according to Italian regions or autonomous provinces and areas (North, Center, and South). We also collected information on the prevalence of COVID-19 in mid-March 2020 by public documents of the Italian Institute of Health.4
The study was conducted in accordance with the Declaration of Helsinki. All included patients gave their informed consent on admission for data collection and publication of deidentified data.
Statistical Analysis
Categorical variables were reported as numbers and proportions, while continuous variables were reported as means and SDs. The primary outcome was the change in hospitalization rate for stroke or TIA in the study period as compared with the control period. The secondary outcomes were the change in hospitalization rate for stroke subtypes (ischemic stroke, TIA, and intracerebral hemorrhage) and changes in revascularization procedures for acute ischemic stroke. Hospitalization rate ratios (HRRs) comparing the study period to the control period were calculated using Poisson regression to model the number of hospitalizations per 31-day period. We also calculated the proportions of patients who were treated with the revascularization procedure over all admitted patients with acute ischemic stroke. Rate ratios (RRs) for sex distribution and for revascularization procedures were also calculated according to Poisson distributions. Patients’ age was compared using Student t test. Subgroup analyses were performed according to Italian regions or autonomous provinces and areas. To evaluate whether there could be a potential competitive influence of COVID-19 on stroke hospitalization, we assessed the association between all strokes/TIA HRRs and the cumulative incidence of COVID-19 in mid-March 2020 by means of inverse-variance weighted linear regression. Statistical significance was set at <0.05. Analyses were conducted using R for Windows, version 4.0.0.
Results
In March 2020, 2379 subjects (53.0% men; mean age, 73.5±12.9 years) were hospitalized, as compared with 3145 subjects (53.4% men; mean age, 73.6±13.3 years) in March 2019. Patients’ age and sex distribution did not differ between the two periods (Table I in the Data Supplement).
Ischemic strokes decreased from 2399 in 2019 to 1810 in 2020 (HRR, 0.75 [95% CI, 0.71–0.80]; P<0.001), intracerebral hemorrhages decreased from 400 to 322 (HRR, 0.81 [95% CI, 0.69–0.93]; P=0.004), and TIAs decreased from 322 to 196 (HRR, 0.61 [95% CI, 0.51–0.73]; P<0.001). Hospitalizations decreased in Northern, Central, and Southern Italy for total events and for ischemic strokes (Figure 1). In 2020, 672 (37.1%) ischemic stroke patients underwent acute interventions as compared with 914 (38.1%) in 2019 (RR, 0.97 [95% CI, 0.88–1.08]; P=0.630). Intravenous thrombolyses decreased from 531 (22.1%) in 2019 to 345 in 2020 (19.1%; RR, 0.86 [95% CI, 0.75–0.99]; P=0.032), while no changes were observed for primary endovascular procedures and combined treatments overall (Figure 2). Analyses by area showed that primary endovascular procedures increased in Northern Italy (RR, 1.61 [95% CI, 1.13–2.32]; P=0.008) driven by Lombardia (RR, 1.74 [95% CI, 1.00–3.12]; P=0.045). Pearson analysis showed no correlation (P=0.517) between the HRRs for all strokes or TIA and COVID-19 incidence in the Italian regions or autonomous provinces (Figure 3). Secondary analyses according to regions or autonomous provinces are reported in Tables II and III in the Data Supplement.
Figure 1.
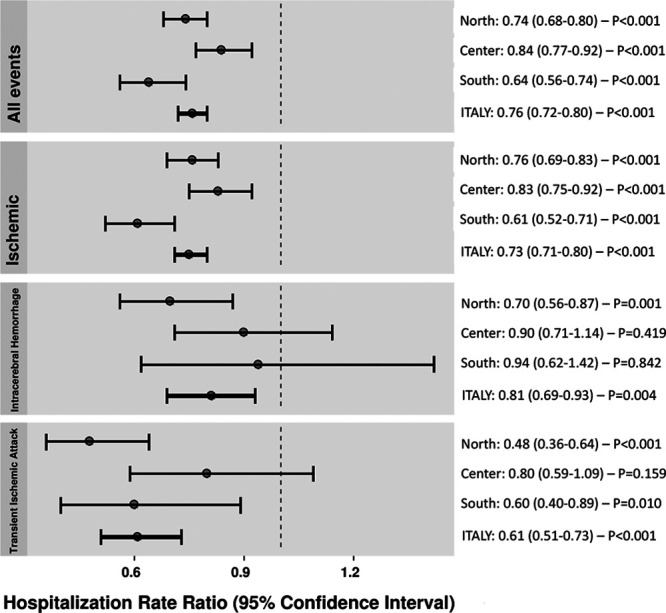
Hospitalization rate ratios of cerebrovascular events and subtypes in Italy, March 2020 vs March 2019.
Figure 2.

Rate ratios of procedures for acute ischemic stroke in Italy, March 2020 vs March 2019.
Figure 3.

Correlation between the hospitalization rate ratio for all strokes or transient ischemic attack (March 2020 vs March 2019) and coronavirus disease 2019 (COVID-19) incidence in mid-March 2020. Each dot represents an Italian Region or Autonomous Province.
Discussion
Our study shows a significant decrease in hospitalization of stroke and TIA across Italy during the worst period of the COVID-19 outbreak. The relevant decline in the hospitalization of ischemic strokes is in line with other reports from different countries.2,3 We also found a decline in hospitalizations for intracerebral hemorrhage and TIA not clearly reported in previous articles. The decline was found in the whole country, even in regions with low COVID-19 incidence, suggesting that competing COVID-19 fatality was not the cause of the decline in hospitalizations for stroke or TIA. Isolation due to forced social distancing or a general disruption of the system of care due to the pandemic emergency might have caused the decline in stroke detection.5 Limited hospitalization of the less severe patients may also explain the reduction in hospitalization.6 Intravenous thrombolytic treatments decreased possibly due to a delay in hospital arrivals, as a consequence of patient reluctance to come to hospitals with COVID-19 patients. Moreover, in March 2020, all patients were considered as possibly affected by COVID-19, and procedures required to be admitted, as swabs and placement of protection devices, may have caused further delay. On the other hand, endovascular treatments remained unchanged and even increased in the area of maximum expression of the outbreak. Notably, the rate of endovascular or combined procedures did not decrease, and primary endovascular treatments actually increased in Northern Italy indicating that the most severe strokes continued to seek for medical care. Primary centralization of patients for endovascular procedures was adopted in those areas and might be an effective strategy to limit the impact on stroke management of possible future events challenging the health system, such as the COVID-19 outbreak.
Our study has limitations. Data were retrieved from administrative codes, so that we did not collect information on stroke severity, outcomes, and mechanisms of the events. Moreover, COVID-19 infection in included patients was not reported. Despite this, we think that our data may add relevant information to the general knowledge, particularly because they refer to an entire country with differences in COVID-19 incidence across regions, they provide information not only on ischemic stroke but also on TIA and intracerebral hemorrhage, and lastly because we showed no correlation between COVID-19 incidence and changes in hospitalization rates.
COVID-19 outbreak impacted indirectly on stroke care and lead to a reduction of stroke admissions and treatments. Strategies to improve maintenance of stroke care during possible future outbreak of COVID-19 or of other infective diseases are needed.
Acknowledgments
We are grateful to Elisa Salvati, Stefania Fiorillo, and Lorenzo Bazzani from the Angels Group Italy, for their invaluable help in organizing the database of March 2020.
Sources of Funding
None.
Disclosures
Dr Ornello reports nonfinancial relationships with Novartis, Allergan, and Teva; Dr Sacco reports personal fees and nonfinancial support from Allergan, Abbott, Eli Lilly, Novartis, and Teva; personal fees from Medscape; and other from Bayer, Pfizer, Medtronic, Starmed, Bristol-Myers Squibb, and Daiichi Sankyo outside the submitted work; Dr Toni reports personal fees for advisory board and speakers’ honoraria from Abbott, Bayer, Boehringer Ingelheim, Daiichi Sankyo, Medtronic, and Pfizer; Dr Ricci reports nonfinancial support from Bayer. The other authors report no conflicts.
Supplemental Materials
List of Participating Centers and Investigators
Tables I–III
Supplementary Material
Nonstandard Abbreviations and Acronyms
- COVID-19
- coronavirus disease 2019
- HRR
- hospitalization rate ratio
- ICD-9-CM
- International Classification of Diseases, Ninth Revision, Clinical Modification
- RR
- rate ratio
- TIA
- transient ischemic attack
For Sources of Funding and Disclosures, see page 3749.
This manuscript was sent to Marc Fisher, Senior Consulting Editor, for review by expert referees, editorial decision, and final disposition.
A list of participating centers and investigators is provided in the Data Supplement.
The Data Supplement is available with this article at https://www.ahajournals.org/doi/suppl/10.1161/STROKEAHA.120.031293.
Contributor Information
Stefano Ricci, Email: stefano.ricci@uslumbria1.it.
Raffaele Ornello, Email: raffaele.ornello@gmail.com.
Paolo Eusebi, Email: paoloeusebi@gmail.com.
Luca Petraglia, Email: luca.petraglia@uniroma1.it.
Danilo Toni, Email: danilo.toni@uniroma1.it.
References
- 1.De Filippo O, D’Ascenzo F, Angelini F, Bocchino PP, Conrotto F, Saglietto A, Secco GG, Campo G, Gallone G, Verardi R, et al. Reduced rate of hospital admissions for ACS during COVID-19 outbreak in Northern Italy. N Engl J Med. 2020;383:88–89. doi: 10.1056/NEJMc2009166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhao J, Li H, Kung D, Fisher M, Shen Y, Liu R. Impact of the COVID-19 epidemic on stroke care and potential solutions. Stroke. 2020;51:1996–2001. doi: 10.1161/STROKEAHA.120.030225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rudilosso S, Laredo C, Vera V, Vargas M, Renú A, Llull L, Obach V, Amaro S, Urra X, Torres F, et al. Acute stroke care is at risk in the era of COVID-19: experience at a comprehensive stroke center in Barcelona. Stroke. 2020;51:1991–1995. doi: 10.1161/STROKEAHA.120.030329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Istituto Superiore di Sanità (ISS). Epidemia COVID-19. Aggiornamento nazionale 23 marzo 2020. Accessed May 29, 2020. https://www.epicentro.iss.it/coronavirus/bollettino/Bollettino-sorveglianza-integrata-COVID-19_23-aprile-2020.pdf
- 5.Aguiar de Sousa D, Sandset EC, Elkind MSV. The curious case of the missing strokes during the COVID-19 pandemic. Stroke. 2020;51:1921–1923. doi: 10.1161/STROKEAHA.120.030792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Teo KC, Leung WCY, Wong YK, Liu RKC, Chan AHY, Choi OMY, Kwok WM, Leung KK, Tse MY, Cheung RTF, et al. Delayed presentation of acute ischemic strokes during the COVID-19 crisis. J Neurointerv Surg. 2020;12:639–642. doi: 10.1161/STROKEAHA.120.030105 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


