Supplemental digital content is available in the text.
Key Words: patient safety culture, maternal and child health, multilevel analysis
Objectives
The aim of this study was to assess patient safety culture (PSC) in maternal and child health (MCH) institutions in China and its individual, organizational, and regional variations.
Methods
Using the PSC survey for MCH institutions (PSCS-MCHI), 2021 valid respondents from 25 participating institutions were investigated in three regions (Beijing, Zhejiang, and Jiangxi) of China. Patient safety culture and its subscale scores (1–5) and factors associated with PSC as revealed by multilevel modeling.
Results
The respondents had an average PSC score of 3.55 (SD = 0.35), with subscale scores ranging between 2.46 (“staffing and workload”) and 4.02 (“work commitment”). There were limited regional differences in PSC: a three-level regression model was only confirmed for the subscale “staff empowerment” (P = 0.006). However, significant organizational variations in PSC were evident: a two-level regression model was assumed for the PSC scale and nine subscales (P < 0.001). The fixed-effect models showed that male respondents, frontline workers, those who were in their mid-career (11–20 y), overloaded (≥9 hours), and had a masters or higher degree reported worse PSC. Frontline workers were less positive than managers in ratings on “managerial response to risks” (−0.11 [−0.20 to −0.02]), “management support” (−0.18 [−0.28 to −0.07]), and “staff empowerment” (−0.23[−0.35 to −0.11]).
Conclusions
Patient safety culture in MCH institutions is shaped by organizational and individual characteristics. We observed a gap in perceived PSC between frontline worker, who are less positive, and managers. Actions for improving PSC should consider interventions on organizational management (such as appropriate staffing and workload management) and engagement of frontline workers in the development of management and training activities.
Patient safety is a global issue of concern. It is regarded as the first priority of health care.1,2 There are many structural and procedural strategies (e.g., facilities, technological innovations, clinical pathways, and guidelines) to ensure patient safety. However, patient safety culture (PSC) is fundamental to the successful implementation of these strategies.3–5
Patient safety culture is usually defined as “shared values, beliefs, norms and procedures related to patient safety among members of the organization.”4 It is part of the organizational culture, a very complex construct grounded in the context of an organization, which can distinguish between groups of people.6 Several PSC survey instruments have been developed, measuring a range of cultural issues in relation to leadership and management, teamwork and collaboration, openness and communication, reporting and learning from errors, and work environment.7,8 The most widely used ones include the hospital survey on PSC (HSOPSC),9 the safety attitudes questionnaire,10 and the patient safety climate in healthcare organizations survey.11 Although these instruments are administered to individual respondents, many studies revealed that great variations in PSC exist across different groups of people within and across institutions.9,12–14 What this amounts to is that PSC is likely to be a measure of hierarchically or clustered structured data.
This study aimed to explore the multilevel (regional, organizational, and individual) determinants of PSC in maternal and child health (MCH) institutions in China. Although there have been extensive studies documenting PSC in hospitals, there are negligible peer-reviewed studies to measure PSC in MCH institutions. Maternal and child health forms a vital part of the sustainable development goals.15 In China, a large MCH network has been developed comprising 3063 MCH institutions, with the majority (99.6%) run by the government.16 These MCH institutions cover all geographic catchments in a hierarchical structure (from central, provincial, and municipal to county levels), delivering maternal and obstetrical care, pediatric care, women’s health, and family planning services.17 In 2016, these MCH institutions used 460 thousand health workers, had 310.15 million outpatient encounters and 10.87 million episodes of hospital care, and delivered 4.24 million babies.18 The MCH network is also obligated to supervise MCH services delegated to other hospitals, community health services and clinics.17 The comprehensive network is commended by the World Health Organization as an exemplar for developing nations19,20 for its extraordinary achievement in MCH.21 In 2016, China had an under-five mortality rate of 10.2‰ an infant mortality rate of 7.5‰, and a maternal mortality ratio of 19.9 per 100,000,22 a proud outcome in comparison with some of the developed nations such as the United States.
The population health orientation of MCH institutions may set themselves apart from general hospitals in PSC.23 Indeed, we revealed some special features of PSC (e.g., a long-term view of child health outcomes and preventive nature of services) in MCH institutions in several studies.8,23,24 As a result, an adapted version of the PSC scale based on the HSOPSC established by the Agency for Healthcare Research and Quality was developed. In this study, we tested this scale and used this scale for determining regional, organizational, and individual determinants of PSC MCH institutions.
METHODS
Study Design and Setting
A cross-sectional survey was conducted in the following three regions of China: Beijing, Zhejiang, and Jiangxi. These regions were purposively selected. Beijing is a highly urbanized metropolitan region with a very high density of health resources. Health facilities in Beijing received patients across all regions of China.25 Zhejiang represents one of the most developed provinces in China but has great disparities in socioeconomic development within the region.26 Jiangxi is one of the least developed provinces in China, with gross domestic product per capita well below the average among all provinces in China.16
Sampling and Data Collection
All of the MCH institutions (n = 220) in the selected regions were invited and 25 (11.4%) agreed to participate in this study: 3 in Beijing, 14 in Zhejiang, and 8 in Jiangxi, accounting for 15.0%, 16.1%, and 7.1% of all MCH institutions in each region, respectively. These included one provincial MCH hospital, five municipal MCH hospitals, ten county MCH hospitals, and nine county MCH centers (The characteristics of the participating MCH institutions can be found in Appendix A, http://links.lww.com/JPS/A206). An MCH hospital delivers both individual-based specialist care and population-based preventive care. By contrast, MCH centers are much smaller, focusing on primary care (mostly population-based preventive care).
Data were collected from January 2016 to April 2017. Facility data such as resources and volume of services were provided by the facility managers. Individual experiences in patient safety and PSC were captured through a self-completed questionnaire. The questionnaire was distributed to all staff members who were approachable at the time of the survey, including managers, doctors, nurses, midwives, public health workers, technicians, pharmacists, and allied health workers. An informed consent statement was attached to the questionnaire. Return of the questionnaire was deemed consent, which was completely voluntary and anonymous. The questionnaire took approximately 10 to 15 minutes to complete. Participants were asked to return the completed questionnaire to a deposit box placed in the workplace within 2 weeks.
A total of 2452 questionnaires were distributed (representing 29.4% of all staff members) and 2145 (87.5%) were returned. This resulted in a final sample size of 2021 (82.4% of distributed questionnaires) for data analyses (Fig. 1), after excluding the questionnaires containing more than 20% of missing items (≥8 items).
FIGURE 1.
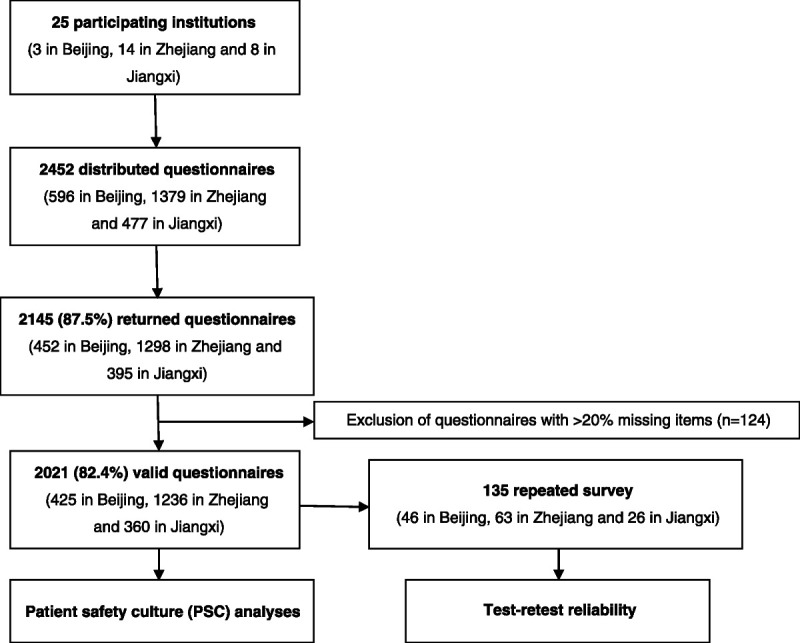
Flowchart of sampling of respondents.
A repeated survey was undertaken to examine the test-retest reliability of the questionnaire in 135 respondents who volunteered to complete the second survey 10 to 14 days after the initial survey (Fig. 1).
Measures
Patient safety culture was measured using the PSCS-MCHI, an adapted version of HSOPSC tailored to the special context of MCHI. It has been validated through a vigorous process involving in-depth interviews, Delphi consultations, and psychometric tests.8,23,24 The PSCS-MCHI contains 37 items, measuring the following ten subscales of PSC: patient engagement (6 items), managerial response to risks (4 items), management support (5 items), staff empowerment (4 items), staffing and workload (4 items), reporting of adverse events (3 items), defensive medical practice (3 items), work commitment (3 items), training (2 items), and transfer and handoff (3 items) (Appendix B, http://links.lww.com/JPS/A207). Respondents were asked to rate each item on a five-point Likert scale (1 = strongly disagree, 2 = disagree, 3 = neither, 4 = agree, 5 = strongly agree; negative wording was scored reversely). An average score of all responded items in each PSC subscale as well as an average score of subscales were calculated, with a higher score indicating better PSC.
The questionnaire also collected data related to the demographic characteristics and work experience of the respondents, including age, sex, education, years of working in health industry, years of working with current employer, average daily workload, contact with patients, and job position.
Statistical Analysis
The reliability and validity of the PSCS-MCHI were further confirmed in this study (Appendix C, http://links.lww.com/JPS/A208), as indicated by the Cronbach’s α coefficients, intraclass correlations (test-retest reliability), and fitness of data into the confirmatory factor model (standardized root mean-square residual = 0.050, root mean square error of approximation = 0.039, comparative fit index = 0.914, Tucker-Lewis Index = 0.901).27,28
We performed multilevel linear regression modeling (iterative generalized least squares, IGLS) to identify individual, organizational, and regional factors associated with PSC. Measurements at the individual level (n = 2021) were nested in 25 organizations from three regions.
We started with an empty model to determine appropriate levels of modeling for the ten PSC subscales, which were treated as continuous variables. The variance components were considered as random effects and partitioned into the following three levels: with level-1 variance () indicating individual variance within an organization; level-2 variance () indicating organizational variance within a region; and level-3 variance () indicating regional variance. The significance of the impact of regional and organizational variations on PSC was assessed using intraclass correlation coefficient (ICC): ICC(r) = /(++) for the regional level; ICC(o) = (+)/(++) for the organizational level.29–31 A significant change in deviance [−2*(log-likelihood)] when eliminating a higher level from the empty model (e.g., from three- to two-level or from two- to one-level) indicates that the higher-level model has a better goodness of fit to the data.32,33 We then established two- or three-level fixed-effect models including all explanatory variables. The explanatory variables at the individual level were all entered as categorical variables, including age (≤34 y, 35–54 y, ≥55 y), sex (male, female), education (no university degree, bachelor degree, master or higher degree), years of working in health industry (≤10 y, 11–20 y, ≥21 y), years of working with current employer (≤10 y, 11–20 y, ≥21 y), average daily workload in the past week (≤8 hours, 9–10 hours, ≥11 hours), patient contact (indirect, direct), and job position (manager, frontline worker).
Data were entered and managed using Epidata 3.1. The confirmatory factor analysis was performed using Mplus 5.1. The multilevel linear regression models were established using MLwiN 2.1. The SPSS 20.0 software was used for group comparisons with analysis of variance tests.
RESULTS
Most respondents (52.7%) were younger than 35 years. The majority (82.9%) were women, frontline workers (91.5%), and had direct contact (85.8%) with patients. Approximately one-third did not have a university degree. Less than half had more than 10 years of work experience in the health industry (Table 1).
TABLE 1.
Characteristics of Respondents (N = 2021)
| Characteristics | n (%) |
|---|---|
| Region | |
| Beijing | 425 (21.0) |
| Zhejiang | 1236 (61.2) |
| Jiangxi | 360 (17.8) |
| Organization | |
| Provincial hospital | 293 (14.5) |
| Municipal hospital | 661 (32.7) |
| County hospital | 740 (36.6) |
| County center | 327 (16.2) |
| Individual characteristics | |
| Age, y | |
| ≤34 | 1066 (52.7) |
| 35–54 | 866 (42.9) |
| ≥55 | 76 (3.8) |
| Missing | 13 (0.6) |
| Sex | |
| Male | 284 (14.1) |
| Female | 1675 (82.9) |
| Missing | 62 (3.1) |
| Education | |
| No university degree | 675 (33.4) |
| Bachelor degree | 1146 (56.7) |
| Master degree or higher | 194 (9.6) |
| Missing | 6 (0.3) |
| Years of working in health industry | |
| 0–10 | 1081 (53.5) |
| 11–20 | 513 (25.4) |
| ≥21 | 419 (20.7) |
| Missing | 8 (0.4) |
| Years of working with current employer | |
| 0–10 | 1271 (62.9) |
| 11–20 | 431 (21.3) |
| ≥21 | 311 (15.4) |
| Missing | 8 (0.4) |
| Average daily workload, h | |
| ≤8 | 1278 (63.2) |
| 9–10 | 572 (28.3) |
| ≥11 | 161 (8.0) |
| Missing | 10 (0.5) |
| Contact with patients | |
| Indirect | 162 (8.0) |
| Direct | 1735 (85.8) |
| Missing | 124 (6.1) |
| Job position | |
| Manager | 158 (7.8) |
| Frontline staff | 1850 (91.5) |
| Missing | 13 (0.6) |
Percentages may not add to 100 because rounding.
The respondents had an average PSC score of 3.55 (SD = 0.35), with subscale scores ranging between 2.46 (“staffing and workload”) and 4.02 (“work commitment”). Significant PSC scale and subscale variations across regions (except for “management support” and “work commitment”) and organizations (except for “reporting of adverse events” and “work commitment”) were found (Fig. 2, Appendix D, http://links.lww.com/JPS/A209, and Appendix E, http://links.lww.com/JPS/A210).
FIGURE 2.
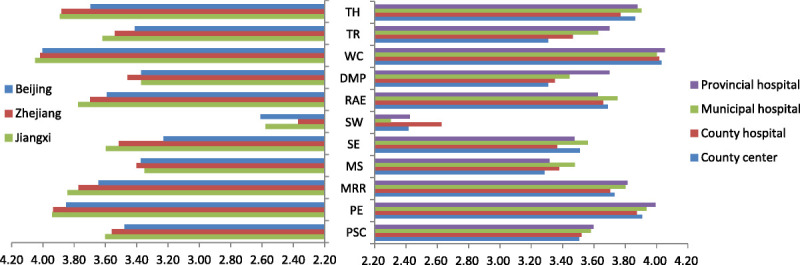
Average PSC scores across organizations and regions. DMP, defensive medical practice; PE, patient engagement; MRR, managerial response to risks; MS, management support; RAE, reporting of adverse events; SE, staff empowerment; SW, staffing and workload; TH, transfer and handoff; TR, training; WC, work commitment.
In the empty models, the ICCs for PSC scores ranged from 0.0% to 5.3% at the regional level and from 0.5% to 9.1% at the organizational level. A three-level model was confirmed for the subscale “staff empowerment” (P = 0.006). Two-level models were selected for the rest of the PSC subscales and the overall PSC score (P < 0.001), except for “work commitment” (P = 0.113), for which a one-level model was assumed (Table 2).
TABLE 2.
Variances, ICCs, and Significance Testing in Empty Models of PSC
| Parameter | PSC | Sub-PSC | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1-PE | 2-MRR | 3-MS | 4-SE | 5-SW | 6-RAE | 7-DMP | 8-WC | 9-TR | 10-TH | ||
| Variance | |||||||||||
| 0.000 | 0.000 | 0.003 | 0.000 | 0.023 | 0.008 | 0.004 | 0.000 | 0.000 | 0.000 | 0.005 | |
| 0.007 | 0.003 | 0.006 | 0.036 | 0.007 | 0.022 | 0.002 | 0.038 | 0.001 | 0.041 | 0.010 | |
| 0.115 | 0.210 | 0.255 | 0.359 | 0.403 | 0.448 | 0.313 | 0.408 | 0.201 | 0.553 | 0.252 | |
| ICC(r) (%) | 0.0 | 0.0 | 1.1 | 0.0 | 5.3 | 1.7 | 1.3 | 0.0 | 0.0 | 0.0 | 1.9 |
| ICC(o) (%) | 5.7 | 1.4 | 3.4 | 9.1 | 6.9 | 6.3 | 1.9 | 8.5 | 0.5 | 6.9 | 5.6 |
| −2 * log-likelihood | |||||||||||
| (1) one-level | 1455.797 | 2609.907 | 3025.379 | 3792.333 | 4002.365 | 4230.816 | 3417.299 | 4075.498 | 2496.937 | 4656.083 | 3051.099 |
| (2) two-level | 1403.548 | 2599.606 | 2997.354 | 3713.416 | 3935.630 | 4152.261 | 3404.694 | 3969.235 | 2494.419 | 4578.660 | 2982.551 |
| (3) three-level | 1403.548 | 2599.606 | 2996.790 | 3713.416 | 3928.019 | 4149.873 | 3402.330 | 3969.235 | 2494.419 | 4578.660 | 2981.406 |
| P (3) versus (2), df = 1 | 1.000 | 1.000 | 0.453 | 1.000 | 0.006 | 0.122 | 0.124 | 1.000 | 1.000 | 1.000 | 0.285 |
| P (2) versus (1), df = 1 | <0.001 | 0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | 0.113 | <0.001 | <0.001 |
The fixed-effect modeling revealed that PSC was associated with age, sex, work experience, workload, job position, and patient contacts (Table 3). Overall, male respondents, frontline workers, those who were in their mid-career (11–20 y), reported higher daily average work hours (≥9 hours) and had a masters or higher degree reported worse PSC. Older respondents (≥55 y) gave a higher score to “staffing and workload,” but lower scores to “work commitment” and “transfer and handoff” compared with their younger counterparts. Male respondents reported worse PSC in all subscales except for “staffing and workload” and “training.” Those with a higher degree were mainly concerned about “staffing and workload,” “reporting of adverse events,” and “training.” A longer working experience was associated with a higher score in “work commitment” but lower scores in “staff empowerment,” “staffing and workload,” and “training.” Respondents who reported higher daily average work hours performed lower scores in “patient engagement,” “staffing and workload,” and “training.” Respondents who reported having direct contact with patients were associated with higher scores in “patient engagement,” “managerial response to risks,” “defensive medical practice,” “work commitment,” and “transfer and handoff” but a lower score in “staffing and workload.” Frontline workers reported lower scores in “managerial response to risks,” “management support,” and “staff empowerment” than their managers (Table 3).
TABLE 3.
Fixed-Effect Models of Variables Associated With PSC: Regression Coefficients and Confidence Intervals (β [95% CI])
| Explanatory Variables | PSC (2-Level) | Sub-PSC | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1-PE (2-Level) | 2-MRR (2-Level) | 3-MS (2-Level) | 4-SE (3-Level) | 5-SW (2-Level) | 6-RAE (2-Level) | 7-DMP (2-Level) | 8-WC (1-Level) | 9-TR (2-Level) | 10-TH (2-Level) | ||
| Constant | 3.56 (3.48 to 3.65) | 3.77 (3.66 to 3.88) | 3.73 (3.61 to 3.86) | 3.39 (3.23 to 3.54) | 3.69 (3.46 to 3.92) | 2.87 (2.70 to 3.03) | 3.62 (3.49 to 3.75) | 3.22 (3.06 to 3.39) | 3.85 (3.75 to 3.96) | 3.69 (3.49 to 3.88) | 3.73 (3.60 to 3.86) |
| Age (≤34 y as reference) | |||||||||||
| 35–54 | −0.01 (−0.06 to 0.05) | −0.03 (−0.10 to 0.05) | −0.04 (−0.13 to 0.04) | −0.02 (−0.12 to 0.08) | 0.04 (−0.06 to 0.15) | 0.10 (−0.01 to 0.20) | −0.07 (−0.16 to 0.02) | 0.02 (−0.08 to 0.13) | 0.01 (−0.06 to 0.08) | −0.05 (−0.17 to 0.07) | −0.03 (−0.11 to 0.05) |
| ≥55 | −0.02 (−0.12 to 0.09) | −0.06 (−0.20 to 0.09) | −0.05 (−0.21 to 0.11) | −0.01 (−0.19 to 0.18) | 0.08 (−0.12 to 0.28) | 0.25 (0.05 to 0.45) | −0.10 (−0.28 to 0.07) | 0.04 (−0.16 to 0.24) | −0.16 (−0.30 to −0.02) | 0.01 (−0.23 to 0.25) | −0.17 (−0.33 to −0.01) |
| Sex (male as reference) | |||||||||||
| Female | 0.10 (0.05 to 0.14) | 0.08 (0.02 to 0.14) | 0.07 (0.00 to 0.13) | 0.15 (0.07 to 0.22) | 0.09 (0.00 to 0.17) | 0.03 (−0.05 to 0.12) | 0.14 (0.07 to 0.21) | 0.23 (0.15 to 0.32) | 0.06 (0.00 to 0.12) | 0.01 (−0.08 to 0.11) | 0.11 (0.04 to 0.18) |
| Education (no university degree as reference) | |||||||||||
| Bachelor degree | −0.02 (−0.05 to 0.02) | 0.03 (−0.02 to 0.08) | 0.02 (−0.03 to 0.08) | 0.08 (0.02 to 0.14) | −0.02 (−0.09 to 0.05) | −0.17 (−0.24 to −0.10) | −0.01 (−0.07 to 0.05) | 0.01 (−0.06 to 0.08) | 0.02 (−0.03 to 0.07) | −0.12 (−0.20 to −0.04) | −0.00 (−0.06 to 0.05) |
| Masters or higher degree | −0.07 (−0.13 to −0.01) | 0.01 (−0.07 to 0.10) | −0.06 (−0.16 to 0.03) | 0.08 (−0.03 to 0.19) | −0.07 (−0.18 to 0.05) | −0.13 (−0.25 to −0.01) | −0.17 (−0.27 to −0.07) | −0.02 (−0.14 to 0.10) | 0.05 (−0.03 to 0.12) | −0.37 (−0.51 to −0.23) | −0.02 (−0.11 to 0.08) |
| Years of working in health industry (≤10 y as reference) | |||||||||||
| 11–20 | −0.10 (−0.16 to −0.03) | −0.03 (−0.11 to 0.06) | −0.02 (−0.12 to 0.08) | −0.10 (−0.21 to 0.02) | −0.20 (−0.32 to −0.08) | −0.27 (−0.39 to −0.14) | −0.05 (−0.15 to 0.06) | −0.09 (−0.21 to 0.03) | −0.00 (−0.08 to 0.09) | −0.20 (−0.34 to −0.06) | −0.05 (−0.15 to 0.04) |
| ≥21 | −0.02 (−0.10 to 0.06) | 0.07 (−0.04 to 0.18) | 0.06 (−0.06 to 0.19) | −0.01 (−0.15 to 0.14) | −0.07 (−0.22 to 0.08) | −0.30 (−0.46 to −0.15) | 0.05 (−0.08 to 0.19) | −0.05 (−0.20 to 0.10) | 0.13 (0.03 to 0.24) | −0.14 (−0.32 to 0.04) | 0.01 (−0.12 to 0.13) |
| Years of working with current employer (≤10 y as reference) | |||||||||||
| 11–20 | −0.00 (−0.06 to 0.06) | 0.00 (−0.08 to 0.09) | −0.01 (−0.10 to 0.08) | −0.09 (−0.20 to 0.01) | 0.01 (−0.11 to 0.12) | 0.02 (−0.09 to 0.14) | −0.02 (−0.12 to 0.08) | −0.03 (−0.14 to 0.08) | 0.00 (−0.08 to 0.08) | 0.13 (−0.01 to 0.26) | 0.01 (−0.08 to 0.10) |
| ≥21 | −0.07 (−0.15 to 0.01) | −0.08 (−0.19 to 0.02) | −0.07 (−0.18 to 0.05) | −0.10 (−0.23 to 0.04) | −0.15 (−0.30 to −0.01) | 0.01 (−0.14 to 0.15) | −0.05 (−0.17 to 0.08) | −0.02 (−0.17 to 0.12) | −0.07 (−0.17 to 0.03) | −0.10 (−0.27 to 0.07) | −0.06 (−0.17 to 0.06) |
| Average daily workload (≤8 h as reference) | |||||||||||
| 9–10 | −0.07 (−0.10 to −0.03) | −0.06 (−0.11 to −0.01) | −0.01 (−0.06 to 0.05) | −0.04 (−0.11 to 0.02) | −0.04 (−0.11 to 0.03) | −0.30 (−0.37 to −0.23) | 0.00 (−0.06 to 0.06) | −0.06 (−0.12 to 0.01) | −0.03 (−0.08 to 0.02) | −0.11 (−0.19 to −0.03) | −0.03 (−0.09 to 0.02) |
| ≥11 | −0.10 (−0.16 to −0.04) | −0.03 (−0.11 to 0.05) | −0.05 (−0.14 to 0.05) | 0.06 (−0.05 to 0.16) | −0.10 (−0.21 to 0.01) | −0.51 (−0.62 to −0.39) | −0.09 (−0.19 to 0.01) | −0.07 (−0.18 to 0.04) | −0.04 (−0.11 to 0.04) | −0.13 (−0.27 to 0.00) | −0.04 (−0.13 to 0.05) |
| Patient contacts (indirect as reference) | |||||||||||
| Direct | 0.05 (−0.01 to 0.11) | 0.10 (0.02 to 0.18) | 0.10 (0.01 to 0.20) | 0.05 (−0.06 to 0.15) | −0.02 (−0.14 to 0.09) | −0.15 (−0.26 to −0.03) | 0.00 (−0.10 to 0.10) | 0.12 (0.01 to 0.23) | 0.11 (0.03 to 0.19) | 0.05 (−0.09 to 0.18) | 0.11 (0.01 to 0.20) |
| Job position (manager as reference) | |||||||||||
| Frontline worker | −0.07 (−0.13 to −0.00) | 0.01 (−0.07 to 0.10) | −0.11 (−0.20 to −0.02) | −0.18 (−0.28 to −0.07) | −0.23 (−0.35 to −0.11) | −0.01 (−0.13 to 0.11) | 0.03 (−0.08 to 0.13) | −0.11 (−0.23 to 0.01) | 0.00 (−0.08 to 0.09) | −0.07 (−0.20 to 0.07) | −0.01 (−0.10 to 0.09) |
Bold numbers indicate that the regression coefficients are significant (P < 0.05).
DISCUSSION
Challenges and Implications of PSC in MCH Institutions
The PSCS-MCHI is an adapted version of HSOPSC tailored to the special context of MCH institutions in China. Its compositions draw a profile of PSC in MCH institutions, including the following ten subscales: “patient engagement,” “managerial response to risks,” “management support,” “staff empowerment,” “staffing and workload,” “reporting of adverse events,” “defensive medical practice,” “work commitment,” “training,” and “transfer and handoff”.
A three-level regression model was only confirmed for the subscale “staff empowerment,” indicating limited regional differences in PSC of MCH institutions. This may be attributable to the strong top-down governance and administration of MCH services. For the last few decades, the central government of China has set MCH as a priority in the health care system development, serving as a foundation for sustainable human development. A series of legislations, regulations, and policies have been put into place, giving clearly defined instructions to the funding, workforce, and services arrangements for MCH institutions. Empirical evidence shows that these measures have significantly improved regional equality of MCH care and MCH outcomes in China.21,34,35 Furthermore, the significant variation of “staff empowerment” in both regional and organizational level also reveals that the top-down MCH system is a double-edged sword for PSC. It should be necessary to make a priority of optimizing frontline workers’ engagement in decision-making, through creating a work environment with an informal power structure, developing the decision-making capabilities of frontline workers by training or educational programs, and ensuring their participation in decision-making processes by policies and regulations, etc.36–40
There are significant organizational variations in PSC. The PSC scale and its nine subscales presented significant heterogeneity across MCH institutions in this study, suggesting a two-level regression model. This result is consistent with the findings of other studies. Indeed, PSC is rooted in the context of organizational arrangements.9,14,41,42 In the Chinese context, it seems that the size of MHC institutions matters. Those in the medium to large range (e.g., 500–999 health workers or 500–999 beds) seemed to have better PSC, but a further increase in the size may not necessarily bring benefits in PSC (Appendix E, http://links.lww.com/JPS/A210). Further studies are warranted to explore the underlined reasons and mechanisms. For those huge institutions in the size, it may be reasonable to compose into various target groups of the interventions with different purposes, because an inherently hierarchical structure exits in an organization where culture is often deeply embedded within different levels and subgroups.5
Management can make a difference to organizational PSC. However, they have to realize that individual variations in PSC always exist in an organization. This study revealed that MCH institutions in China share similar individual determinants of PSC in comparison with other health institutions,12,39,43 which indicate that management actions for improving PSC need to consider age, sex, educational background, work experience, and workloads of their staff members. This study presents the worse perceived PSC among respondents who are male, in their mid-career, or having a master or higher degree, which is consistent with the findings of previous studies, possibly because of neglect, arrogancy, or burnout of patient safety.39,44 It is worth noting that a gap in perceived PSC exists between managers and frontline workers. This is a common finding across several studies44–46 that has some implications on the development of PSC training and management programs. Frontline workers usually hold a less positive perception on PSC than their managers. Therefore, staff participation and engagement in training and management decision-making are extremely important in driving effective cultural changes.2,38,47,48
Managers themselves should be made accountable for PSC. Of the ten PSC subscales, “staffing and workload” was rated as a particular concern by the study participants in comparison to those of studies undertaken in other countries.49–51 Previous studies of hospitals in China conveyed similar concerns.39,42,43,52 Interestingly, China has already had a MCH workforce of 2.8 per 10,000 population,16 higher than the recommended standard (1:10,000) from the national health authority.53 However, 36.3% of respondents in this study still reported overloading (>8 h/d). This is not uncommon in MCH institutions in China.34,54,55 In October 2015, China abandoned its one-child family policy, allowing each family to have two children. The baby boom has not happened as expected, but with a cut of 630 thousand births from 17.86 million in 2016 to 17.23 million in 2017. However, an increasing of pregnant women with advanced age has emerged undoubtedly,56,57 with higher risks of pregnant complications and adverse birth outcomes,58,59 imposing greater pressure on MCH services. Therefore, it should be the urgent matter to improve the efficiency, capacity, and quality of MCH services.
Limitations and Further Studies
The study sample is not representative of the entire country of China. Because of limitations in sample size and availability of data, we were not able to further analyze PSC scores across units and wards as was done in some previous studies.9,13,33,60 Further studies are needed to establish representative benchmarking for MCH institutions. There is also a need to explore the underlining mechanisms of organizational variations in PSC.
CONCLUSIONS
The PSCS-MCHI is a reliable instrument for measuring PSC in MCH institutions. In China, regional differences in PSC in MCH institutions are limited. However, great organizational variations in PSC exist. Actions for improving PSC should consider interventions at the organizational level (such as appropriate staffing and workload management) as well as at the individual level (such as training). Furthermore, it is important to engage frontline workers in the development of management and training activities.
ACKNOWLEDGMENTS
The authors thank the 25 participating institutions, including the individuals who offered help and participated in the survey.
Footnotes
W.L. and C.L. contributed equally to this study.
The authors disclose no conflict of interest.
This study was supported by the China-US Center for Medical Professionalism, Peking University Health Science Center (PUHSC-MPC1302).
Supplemental digital contents are available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site (www.journalpatientsafety.com).
Contributor Information
Yuanyuan Wang, Email: yyuanwang@163.com.
Yanjun Fan, Email: fyj@chinawch.org.cn.
Xiaoli Wang, Email: xlwang@bjmu.edu.cn.
Yuanying Ma, Email: mayuanying88@zju.edu.cn.
Chunmei Wu, Email: wuchunmei08@gmail.com.
Huifeng Shi, Email: nsxm@pku.edu.cn.
Hui Han, Email: hanhui0201@163.com.
Chaojie Liu, Email: c.liu@latrobe.edu.au.
REFERENCES
- 1.Institute of Medicine. To Err Is Human: Building a Safer Health System. Washington, DC: National Academics Press; 1999. [Google Scholar]
- 2.World Health Organization, WHO Patient Safety. Patient Safety Curriculum Guide: Multi-Professional Edition. Geneva: World Health Organization; 2011. [Google Scholar]
- 3.DiCuccio MH. The relationship between patient safety culture and patient outcomes: a systematic review. J Patient Saf. 2015;11:135–142. [DOI] [PubMed] [Google Scholar]
- 4.Weaver SJ Lubomksi LH Wilson RF, et al. Promoting a culture of safety as a patient safety strategy: a systematic review. Ann Intern Med. 2013;158(5 Pt 2):69–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Morello RT Lowthian JA Barker AL, et al. Strategies for improving patient safety culture in hospitals: a systematic review. BMJ Qual Saf. 2013;22:11–18. [DOI] [PubMed] [Google Scholar]
- 6.Hofstede GH, Hofstede GJ, Minkov M. Cultures and Organizations: Software of the Mind: Intercultural Cooperation and Its Importance for Survival. 3rd ed New York: McGraw-Hill; 2010. [Google Scholar]
- 7.Xuanyue M Yanli N Hao C, et al. Literature review regarding patient safety culture. J Evid Based Med. 2013;6:43–49. [DOI] [PubMed] [Google Scholar]
- 8.Wang Y Wang Y Shi H, et al. Systematic review of patient safety culture measuring tools for medical institutions at home and abroad. Chin Hosp Manag. 2018;38:36–39, 61. [Google Scholar]
- 9.Sorra JS, Dyer N. Multilevel psychometric properties of the AHRQ hospital survey on patient safety culture. BMC Health Serv Res. 2010;10:199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sexton JB Helmreich RL Neilands TB, et al. The Safety Attitudes Questionnaire: psychometric properties, benchmarking data, and emerging research. BMC Health Serv Res. 2006;6:44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Singer S Meterko M Baker L, et al. Workforce perceptions of hospital safety culture: development and validation of the patient safety climate in healthcare organizations survey. Health Serv Res. 2007;42:1999–2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gallego B Westbrook MT Dunn AG, et al. Investigating patient safety culture across a health system: multilevel modelling of differences associated with service types and staff demographics. Int J Qual Health Care. 2012;24:311–320. [DOI] [PubMed] [Google Scholar]
- 13.Zhu J Li L Zhao H, et al. Development of a patient safety climate survey for Chinese hospitals: cross-national adaptation and psychometric evaluation. BMJ Qual Saf. 2014;23:847–856. [DOI] [PubMed] [Google Scholar]
- 14.Burlison JD Quillivan RR Kath LM, et al. A multilevel analysis of U.S. hospital patient safety culture relationships with perceptions of voluntary event reporting. J Patient Saf. 2016. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Health - United Nations Sustainable Development 2017. Available at: http://www.un.org/sustainabledevelopment/health/. Accessed April 11, 2017.
- 16.National Health and Family Planning Commission. National Health Statistics Yearbook 2017. Beijing: Peking Union Medical College Press; 2017. [Google Scholar]
- 17.Guidance on standardized organizational construction and management of maternal and child health service institutions - National Health and Family Planning Commission of the People’s Republic of China. 2016. Available at: http://www.nhfpc.gov.cn/fys/s3581/201512/a0dcaf1f20624769a9a3b2dafa0280ab.shtml. Accessed April 11, 2017.
- 18.National Center for Women and Children’s Health, China CDC. Annual report of health resources and performances in maternal and child health institutions. 2016 annual report of resources and operations of maternal and child health institutions in China. 2017. Available at: http://www.chinawch.cn/jgjc/xzzx/cyzlxz/201711/P020171108465376564917.pdf. Accessed December 19, 2017.
- 19.National Health and Family Planning Commission. Partnership for Maternal Newborn & Child Health, World Health Organization, World Bank, Alliance for Health Policy and Systems Research. Success factors for women’s and children’s health: China. Geneva: World Health Organization; 2015. [Google Scholar]
- 20.Ahmed SM Rawal LB Chowdhury SA, et al. Cross-country analysis of strategies for achieving progress towards global goals for women’s and children’s health. Bull World Health Organ. 2016;94:351–361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Guo Y, Bai J, Na H. The history of China’s maternal and child health care development. Semin Fetal Neonatal Med. 2015;20:309–314. [DOI] [PubMed] [Google Scholar]
- 22.National Health and Family Planning Commission of the People’s Republic of China. 2016 bulletin of health statistics in China. 2017. Available at: http://www.nhfpc.gov.cn/guihuaxxs/s10748/201708/d82fa7141696407abb4ef764f3edf095.shtml. Accessed August 8, 2017.
- 23.Wang Y Liu W Shi H, et al. Measuring patient safety culture in maternal and child health institutions in China: a qualitative study. BMJ Open. 2017;7:e015458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang Y Han H Fan Y, et al. A patient safety culture scale for maternal and child health institutions based on classical test theory and item response theory. Mod Prev Med. 2018;45:431–436. [Google Scholar]
- 25.Song L Mao A Dong P, et al. Analysis of cross-regional medical treatment management: a case study of cancer patients in Beijing. Chin Health Serv Manag. 2018;35:81–85, 116. [Google Scholar]
- 26.Ding P. Study on the evolvement of county economic discrepancy and coordinated development of Zhejiang Province. Zhejiang University; 2013. [Google Scholar]
- 27.Byrne BM. Structural Equation Modeling With Amos: Basic Concepts, Applications, and Programming. Third ed New York: Routledge: Taylor & Francis Group; 2016. [Google Scholar]
- 28.Chen IC, Li HH. Measuring patient safety culture in Taiwan using the Hospital Survey on Patient Safety Culture (HSOPSC). BMC Health Serv Res. 2010;10:152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wang J, Xie H, Fischer JH. Multilevel Models: Applications Using SAS. Berlin; Boston; Beijing: De Gruyter; Higher Education Press; 2012. [Google Scholar]
- 30.Homwong N Diaz A Rossow S, et al. Three-level mixed-effects logistic regression analysis reveals complex epidemiology of swine rotaviruses in diagnostic samples from North America. PLoS One. 2016;11:e0154734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Li X, Hedeker D. A three-level mixed-effects location scale model with an application to ecological momentary assessment data. Stat Med. 2012;31:3192–3210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jones K, Subramanian S. Developing Multilevel Models Using MLwiN 2.1-A Training Manual: Centre for Multilevel Modelling. University of Bristol; 2010:1–341. [Google Scholar]
- 33.Deilkås E, Hofoss D. Patient safety culture lives in departments and wards: multilevel partitioning of variance in patient safety culture. BMC Health Serv Res. 2010;10:85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ren Z Song P Theodoratou E, et al. China’s human resources for maternal and child health: a national sampling survey. BMC Health Serv Res. 2015;15:561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fang P Dong S Xiao J, et al. Regional inequality in health and its determinants: evidence from China. Health Policy. 2010;94:14–25. [DOI] [PubMed] [Google Scholar]
- 36.Amiri M, Khademian Z, Nikandish R. The effect of nurse empowerment educational program on patient safety culture: a randomized controlled trial. BMC Med Educ. 2018;18:158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Farokhzadian J, Dehghan Nayeri N, Borhani F. The long way ahead to achieve an effective patient safety culture: challenges perceived by nurses. BMC Health Serv Res. 2018;18:654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Armellino D, Quinn Griffin MT, Fitzpatrick JJ. Structural empowerment and patient safety culture among registered nurses working in adult critical care units. J Nurs Manag. 2010;18:796–803. [DOI] [PubMed] [Google Scholar]
- 39.Liu C Liu W Wang Y, et al. Patient safety culture in China: a case study in an outpatient setting in Beijing. BMJ Qual Saf. 2014;23:556–564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dirik HF, Intepeler SS. The work environment and empowerment as predictors of patient safety culture in Turkey. J Nurs Manag. 2017;25:256–265. [DOI] [PubMed] [Google Scholar]
- 41.Chen IC, Ng HF, Li HH. A multilevel model of patient safety culture: cross-level relationship between organizational culture and patient safety behavior in Taiwan’s hospitals. Int J Health Plann Manage. 2012;27:e65–e82. [DOI] [PubMed] [Google Scholar]
- 42.Jia PL Zhang LH Zhang MM, et al. Safety culture in a pharmacy setting using a pharmacy survey on patient safety culture: a cross-sectional study in China. BMJ Open. 2014;4:e004904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nie Y Mao X Cui H, et al. Hospital survey on patient safety culture in China. BMC Health Serv Res. 2013;13:228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zhou P Bundorf MK Gu J, et al. Survey on patient safety climate in public hospitals in China. BMC Health Serv Res. 2015;15:53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hickner J Smith SA Yount N, et al. Differing perceptions of safety culture across job roles in the ambulatory setting: analysis of the AHRQ Medical Office Survey on Patient Safety Culture. BMJ Qual Saf. 2016;25:588–594. [DOI] [PubMed] [Google Scholar]
- 46.Banaszak-Holl J Reichert H Todd Greene M, et al. Do safety culture scores in nursing homes depend on job role and ownership? Results from a national survey. J Am Geriatr Soc. 2017;65:2244–2250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Reason J. Human error: models and management. BMJ. 2000;320:768–770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Horwitz SK, Horwitz IB. The effects of organizational commitment and structural empowerment on patient safety culture. J Health Organ Manag. 2017;31:10–27. [DOI] [PubMed] [Google Scholar]
- 49.Wagner C Smits M Sorra J, et al. Assessing patient safety culture in hospitals across countries. Int J Qual Health Care. 2013;25:213–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Vlayen A Hellings J Claes N, et al. A nationwide hospital survey on patient safety culture in Belgian hospitals: setting priorities at the launch of a 5-year patient safety plan. BMJ Qual Saf. 2012;21:760–767. [DOI] [PubMed] [Google Scholar]
- 51.Danielsson M Nilsen P Rutberg H, et al. A National Study of Patient Safety Culture in Hospitals in Sweden. J Pat Saf. 2017. doi: 10.1097/PTS.0000000000000369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wang M, Tao H. How does patient safety culture in the surgical departments compare to the rest of the county hospitals in Xiaogan City of China? Int J Environ Res Public Health. 2017;14:E1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.National Health Department of the People’s Republic of China. Management regulation for MCH institutions. 2006. Available at: http://www.chinacdc.cn/n272442/n272530/n273736/n273872/n321585/36150.html. Accessed July 26, 2018.
- 54.Wang JP Luo R Jin X, et al. Analysis on human status and demand in MCH institution in China. Chin J Women Child Health. 2014;5:1–5. [Google Scholar]
- 55.Wang K Luo R Wang JP, et al. Influence of human resources allocation on service development of maternal and children health care institutions. Chin J Woman Child Health Res. 2016;27:650–654. [Google Scholar]
- 56.Li P Liao Z Wang C, et al. Maternal characteristics and birth outcomes under different family planning policy. Chin J Reprod Health. 2018;501–505. [Google Scholar]
- 57.Ye F, Huang J. Antenatal care for women in their second pregnancies in China. Lancet Glob Health. 2016;4:E303. [DOI] [PubMed] [Google Scholar]
- 58.Wennberg AL Opdahl S Bergh C, et al. Effect of maternal age on maternal and neonatal outcomes after assisted reproductive technology. Fertil Steril. 2016;106:1142–49.e14. [DOI] [PubMed] [Google Scholar]
- 59.Rosato E Perrone G Capri O, et al. Hypertension and early menopause after the use of assisted reproductive technologies in women aged 43 years or older: long-term follow-up study. J Obstet Gynaecol Res. 2016;42:1782–1788. [DOI] [PubMed] [Google Scholar]
- 60.Fujita S Seto K Kitazawa T, et al. Characteristics of unit-level patient safety culture in hospitals in Japan: a cross-sectional study. BMC Health Serv Res. 2014;14:508. [DOI] [PMC free article] [PubMed] [Google Scholar]


