ABSTRACT
Background: Healthcare workers (HCWs) are considered at elevated risk of experiencing mental health disorders in working with patients with COVID-19.
Objective: To estimate the prevalence of common mental health disorders in HCWs based in hospitals where pandemic-affected patients were treated.
Method: Databases were searched for studies published before 30 March 2020. Quantitative synthesis was used to obtain estimates of the prevalence of mental health disorders in four time windows, determined a priori (the acute phase, i.e. during and up to 1.5 months post-pandemic; 1.5–5.9 months; 6–11.9 months; 12 months and later).
Results: Nineteen studies met the review criteria. They predominantly addressed the acute phase of the SARS outbreak in Asia. The most studied outcomes were clinically significant post-traumatic stress symptoms (PTSS) and general psychiatric caseness. For clinically significant PTSS in the acute phase, the prevalence estimate was 23.4% (95% CI 16.3, 31.2; N = 4147; I2 = 96.2%); in the 12 months plus window, the estimate was 11.9% (8.4, 15.8; N = 1136; I2 = 74.3%). For general psychiatric caseness, prevalence estimates were acute phase, 34.1% (18.7, 51.4; N = 3971; I2 = 99.1%); 6–12 months, 17.9% (13.1, 23.2; N = 223; I2 = 0.0%); 12 months plus, 29.3% (6.0, 61.0; N = 710; I2 = 97.8%). No differences between doctors and nurses with respective to PTSS and general psychiatric caseness were apparent in the acute phase.
Conclusions: Mental health disorders are particularly common in HCWs working with pandemic-afflicted patients immediately following a pandemic, but the course of disorders following this period is poorly understood. There was considerable heterogeneity between studies, likely linked to methodological differences. More extended follow up of HCWs is needed.
KEYWORDS: PTSD, depression, anxiety, healthcare workers, pandemic, COVID-19
HIGHLIGHTS:
• Mental health difficulties, in particular post-traumatic stress, are common in healthcare workers working with patients infected during a pandemic. The long-term impact of working in such environments is poorly understood, however.
Antecedentes: Se considera que los trabajadores de la salud (TS) tienen un riesgo elevado de experimentar trastornos de salud mental al trabajar con pacientes con COVID-19.
Objetivo: Estimar la prevalencia de trastornos de salud mental comunes en los TS de los hospitales donde se trataron a pacientes afectados por una pandemia.
Método: Se realizaron búsquedas en las bases de datos para estudios publicados antes del 30 de marzo de 2020. Se utilizó una síntesis cuantitativa para obtener estimaciones de la prevalencia de trastornos de salud mental en cuatro ventanas de tiempo, determinadas a priori (la fase aguda, es decir, durante y hasta 1,5 meses después de la pandemia; 1.5-5.9 meses; 6-11.9 meses; y después de 12 meses).
Resultados: Diecinueve estudios cumplieron los criterios de esta revisión. Principalmente abordaron la fase aguda del brote de SARS en Asia. Los resultados más estudiados fueron los síntomas de estrés postraumático clínicamente significativos (SEPT) y casuística psiquiátrica general. Para los SEPT clínicamente significativo en la fase aguda, la estimación de prevalencia fue del 23,4% (IC del 95%: 16,3, 31,2; N = 4147; I2 = 96,2%); en los 12 meses adicionales, la estimación fue del 11,9% (8,4, 15,8; N = 1136; I2 = 74,3%). Para los casos de psiquiatría general, las estimaciones de prevalencia fueron: fase aguda, 34.1% (18.7, 51.4; N = 3971; I2 = 99.1%); 6-12 meses, 17.9% (13.1, 23.2; N = 223; I2 = 0.0%); después de 12 meses, 29.3% (6.0, 61.0; N = 710; I2 = 97.8%). No se observaron diferencias entre los médicos y las enfermeras con SEPT y casuística psiquiátrica general en la fase aguda.
Conclusiones: Los trastornos de salud mental son particularmente comunes en los TS que trabajan con pacientes afectados inmediatamente después de la pandemia, pero el curso de los trastornos después de este período es poco conocido. Hubo una considerable heterogeneidad entre los estudios, probablemente vinculada a diferencias metodológicas. Se necesita un seguimiento más extenso de los TS.
PALABRAS CLAVE: TEPT, depresión, ansiedad, Trabajadores de la salud, Pandemia, COVID-19
背景: 与COVID-19患者一起工作时, 医护人员 (HCW) 被认为具有较高的心理健康障碍患病风险。
目的: 评估治疗疫情感染患者的医院中医护人员常见心理健康障碍的患病率。
方法: 在数据库中检索2020年3月30日之前发表的研究。使用定量综合法获得先验确定的四个时间窗内的心理健康障碍患病率的估计值 (急性期, 即疫情中到疫情后 1.5 个月; 1.5-5.9 个月; 6-11.9 个月; 12 个月及以后) 。
结果: 19项研究符合综述标准。他们主要关注于亚洲SARS爆发的急性期。研究最多的结果是临床上显著的创伤后应激症状 (PTSS) 和一般精神病病例。对于急性期临床显著的PTSS, 患病率估计值为23.4%(95% CI 16.3, 31.2; N=4147; I2=96.2%);在12个月以上的窗口中, 估计值为11.9% (8.4, 15.8; N=1136; I2=74.3%) 。一般精神病病例的患病率估计值为:急性期为34.1% (18.7, 51.4; N=3971; I2=99.1%); 6-12个月为17.9% (13.1, 23.2; N=223; I2=0.0%); 12个月以上为29.3% (6.0, 61.0; N=710; I2=97.8%) 。急性期PTSS和一般精神病的患病率在医生和护士之间没有明显差异。
结论: 在疫情爆发的初期, 为受疫情影响的患者服务的 HCW 中常见心理健康障碍。但对这些障碍在后期的病程发展还知之甚少。研究之间存在相当大的异质性, 可能与方法学上的差异有关。需要对 HCW 进行进一步随访。
关键词: PTSD; 抑郁; 焦虑; 医护人员; 疫情大流行; COVID-19
1. Introduction
Healthcare workers (HCWs) including nurses, doctors, allied health professionals and all support staff based in hospitals where patients with COVID-19 are treated face considerable challenges and stress. In addition to the clinical challenges associated with treating a large volume of severely unwell patients, HCWs working with this group of infectious patients face threats to their own physical health (Adams & Walls, 2020), with a number of highly publicised HCW deaths already reported due to COVID-19. There is increasing recognition of the significant psychological impact of caring for those with COVID-19 given the immense pressure facing HCWs. For example, HCWs may face situations where they are at risk of sustaining moral injury (Greenberg, Docherty, & Gnanapragasam et al., 2020), while there are also difficulties in obtaining sufficient personal protective equipment. (Livingston, Desai, & Berkwits, 2020) Health systems are subsequently implementing mental health provision systems and additional psychological support (BBC News Online, 2020).
In order to better plan and develop these support systems, and to assist with education around reactions to working with COVID-19 patients, a rapid systematic review was undertaken to determine the prevalence of mental health disorders in HCWs working with patients infected through a pandemic. The review was focused on common mental health difficulties, such as post-traumatic stress, anxiety and depression, to allow an accurate prevalence of future demand on mental health services and to inform the provision of evidence-based interventions. We broadened our search to include studies relevant to the current COVID-19 crisis, e.g. pertaining to other coronavirus outbreaks (Severe Acute Respiratory Syndrome [SARS], Middle East Respiratory Syndrome [MERS]) and other epidemics that represent significant risks to HCWs (e.g. Ebola). In particular, we sought to establish the prevalence of different conditions at different phases, i.e. during and immediately after a pandemic, then over the following months.
In summary, the aim of this rapid systematic review was to estimate the prevalence of common mental health disorders (in particular post-traumatic stress, depression, anxiety or general psychopathology) in HCWs working in hospitals with patients infected through a pandemic in the period during or following the pandemic.
2. Method
2.1. Protocol and registration
The present review was not pre-registered given the perceived need to disseminate a rapid review pertaining to the mental health consequences for HCWs given the exponential rise in hospital admissions and deaths for COVID-19. The review was produced in accordance with Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) recommendations (Moher, Liberati, & Tetzlaff et al., 2009).
2.2. Eligibility criteria
Studies were included in the present review if they measured the prevalence of mental health disorders (in particular clinically significant post-traumatic stress, depression, anxiety or general psychopathology) in healthcare workers that worked in a hospital where care was provided to patients who had acquired an infection because of a pandemic, e.g. SARS, MERS, Ebola, COVID-19. No restrictions were placed on healthcare worker type (e.g. medical and non-medical staff were included) or department worked in.
Studies, or partial study data, were excluded if they i) focused exclusively on healthcare workers who had also developed the index illness at the centre of the pandemic; ii) the sample included in-patients with the index infection; iii) the study was not published in English; iv) the study reported on stress or occupational wellbeing measures, such as burnout, rather than a diagnosable or clinical significant mental health disorder; v) participants included staff at other non-affected hospitals; vi) only comprised qualitative data or vii) addressed work with pandemics with different routes of transmission to COVID-19, e.g. sexually transmitted or blood-borne pathogens including human immunodeficiency virus (HIV).
2.3. Information source
Databases searched included Medline, PsycINFO, CINAHL, PubMed, OVID and ScienceDirect. Manual searches of relevant review papers and empirical articles were also carried out to identify any studies that had not yet been included in the literature databases.
2.4. Search
Search terms were 1) terms related to identified pandemics (including SARS, MERS, Coronavirus, Ebola and ‘pandemic’) AND 2) ‘acute hospital (including all search engine variants) AND 3) ‘mental health’ (including post-traumatic stress, depression, anxiety and low mood variants) AND 4) ‘health* professional’ (including variants such as doctor and nurse). Searches were conducted on 30 March 2020 with databases searched from inception. See Supplementary Material 1 for full search terms.
2.5. Data collection process
Duplicates were removed from search results. Titles and abstracts were screened for eligibility. The full texts of eligible studies were then accessed and checked against the inclusion and exclusion criteria. Six researchers were split into pairs (SA and RB, JB and SP, and TC and GS), both of whom independently completed initial screening and data extraction. Disagreements were resolved by discussion with the wider team and a decision reached by consensus.
2.6. Data items
Descriptive data was extracted pertaining to key study characteristics (country and year of publication, pandemic, sex and role of participants, method of data collection). Data from comparison control groups (e.g. HCWs at another hospital that did not work with pandemic patients) were not extracted. Following our initial searches, the main outcomes we opted to consider were prevalence of clinically significant PTSS, depression, anxiety and general psychiatric caseness (i.e. scoring above cut-off on a general psychiatric screening questionnaire, such as the General Health Questionnaire). Prevalence data were therefore extracted for post-traumatic stress symptoms (PTSS), depression, anxiety and general psychiatric screening using the number of participants who scored above a defined cut-off on the given outcome measure or met threshold for a diagnosis based on a structured interview. Data were categorised according to four time periods, which were defined a priori: during the pandemic up to 1.49 months later (termed the ‘acute phase’); 1.5–5.9 months; 6–11.9 months; and 12 months or later. The end point for each pandemic was defined by the individual studies themselves; studies usually cited the World Health Organisation having declared their region as being removed from the infected areas.
2.7. Risk of bias
The quality of the included papers was assessed using an adapted version of the National Heart, Lung and Blood Institute Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies (https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools; see Supplementary Material 2 for full rating scheme). The assessment criteria included: study population defined; participation rate of over 50%; if follow-up, was the attrition rate described, and validity and reliability of measures for post-traumatic stress, anxiety, depression and general psychiatric screen. Individual studies were scored for quality (0 = not present/poor description, 1 = some description but some missing information, 2 = all desired information included) for each area of quality. Studies were given a percentage according to the degree of criteria being met. The percentage was used to indicate the study quality (>70% high, 50–69% medium, <50% low).
Quality assessment and extraction were double rated; there were no disagreements on quality rating.
Given how few studies were included in each meta-analysis (less than the 10 suggested for funnel plot asymmetry) (Sterne, Sutton, & Ioannidis et al., 2011), formal tests of publication bias are not reported.
2.8. Summary measures
The summary measure of interest was prevalence of a mental health difficulty, based on number scoring above cut-off on a self-report questionnaire measure (i.e. clinically significant levels of symptoms) or the number meeting diagnostic threshold based on a structured interview. Absolute prevalence was selected to be our outcome as we sought to determine the mental health burden for HCWs of working with patients infected through a pandemic, to inform the planning of support services. Comparison between pandemic-affected and non-pandemic-affected hospitals was not possible as we did not find any studies that reported prevalence rates in any control hospitals.
2.9. Synthesis of results
Prevalence outcomes were synthesised using a random-effects meta-analysis. Arcsine transformations were used to account for issues with study weightings when estimating prevalence (Barendregt, Doi, & Lee et al., 2013), with back-transformed values presented in all results. The metafor package (Viechtbauer, 2010) in R 3.4.2 (R: A language and environment for statistical computing, 2014) was used to conduct the meta-analysis.
2.10. Additional analyses
Given significant heterogeneity in the literature, the post-hoc decision was undertaken to conduct sensitivity analyses. These involved restricting our quantitative syntheses to SARS-only literature and particular measures, and where possible reporting results by HCW profession groups.
3. Results
3.1. Study selection
The numbers of studies screened, assessed for eligibility, and included in the review, with reasons for exclusions at each stage, are presented in a PRISMA flowchart (see Figure 1). Nineteen studies provided usable data. Two articles related to the same cohort but at different time intervals (Lu, Shu, & Chang et al., 2006; Lung, Lu, & Chang et al., 2009); these are therefore reported as a single study.
Figure 1.
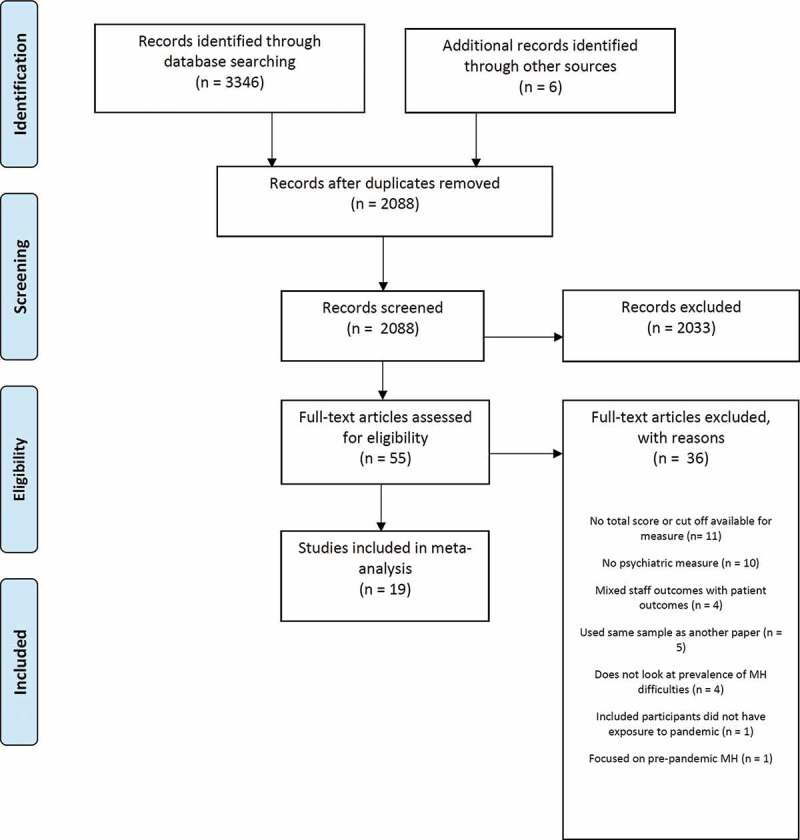
PRISMA flowchart.
One group reported two articles on the same hospital but the sampling frame for the follow-up study was so different to the first that these articles are reported separately (Maunder, 2004; Maunder, Lancee, & Balderson et al., 2006). The same Canadian study group also reported follow-up data on a smaller sub-set of participants but using structured interviews rather than self-report questionnaire screening (Lancee, Maunder, & Goldbloom, 2008); a separate note on this additional study is provided below. References for all articles included in the review are provided in Supplementary Material 3.
3.2. Study characteristics
Nineteen studies met inclusion criteria for this review, comprising 8550 HCWs. Study characteristics are reported in Table 1. The majority of included studies related to the SARS pandemic in Asian hospitals. SARS is a condition associated with coronavirus infection (SARS-CoV), characterised by a high transmission rate to HCWs and with similar presenting symptoms to COVID-19 (e.g. dry cough, shortness of breath). The main transmission route and the progression for patients with severe disease are similar in both COVID-19 infection and SARS. One study reported findings from the COVID-19 pandemic. One set of studies pertained to the SARS outbreak in Canada, and a further study pertained to the H1N1 pandemic in Greece. All but two studies involved mixed healthcare worker samples; the remaining two focused exclusively on nurses. Reported outcomes were classified as being related to PTSS, depression, anxiety or a general psychiatric screen. Three studies reported that mental health interventions were offered to HCWs in response to the pandemic.
Table 1.
Study characteristics.
| Study | Epidemic | N | % Female | Country | Staff type | Mental health intervention reported? | PTSD measure | General psychiatric screen | Depression measure | Anxiety measure | Study quality |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Chan et al. (2004) | SARS | 661 | NR | Singapore | Mixed | Existing Peer Support Programme | IES (≥30) | GHQ-28 (≥5) | - | - | Medium |
| Chen et al. (2005) | SARS | 86 | 100 | Taiwan | Nurses | No | IES (≥35) | - | - | - | High |
| Chong et al. (2004) | SARS | 1257 | 81.1 | Taiwan | Mixed | Group debriefing | - | CHQ-12 (≥3) | - | - | Medium |
| Goulia et al. (2010) | H1N1 | 469 | 68.4 | Greece | Mixed | No | - | GHQ-28 (≥11) | - | - | Low |
| Jung et al. (2020) | MERS | 147 | 100 | South Korea | Nurses | No | IES-R (Korean) (≥18) | - | - | - | Medium |
| Lai et al. (2020) | Covid-19 | 1257 | 76.7 | China | Mixed | Psychological assistance services | IES-R (≥26) | - | PHQ-9 (≥10) | GAD-7 (≥7) | High |
| Lee et al. (2018) | MERS | 77 | 90 | South Korea | Mixed | No | IES-R (≥25) | - | - | - | Low |
| Lin et al. (2007) | SARS | 92 | 91.3 | Taiwan | Mixed | No | DTS (≥40) | CHQ-12 (≥3) | - | - | High |
| Liu et al. (2012) | SARS | 549 | 75 | China | Mixed | No | IES-R (≥20) | - | CES-D (≥25) | - | High |
| Lu et al. (2006) & Lung et al. (2009) | SARS | 127a | 58 | Taiwan | Mixed | No | - | CHQ-12 (≥3) | - | - | High |
| Maunder et al. (2004) | SARS | 1557 | NR | Canada | Mixed | No | IES (≥20) | - | - | - | Medium |
| Maunder et al. (2006) | SARS | 587 | 86 | Canada | Mixed | No | IES (≥26) | K-10 (≥16) | - | - | Medium |
| Nickell et al. (2004) | SARS | 510 | 78.8 | Canada | Mixed | No | - | GHQ-12 (≥3) | - | - | Medium |
| Phua et al. (2005) | SARS | 96 | 69 | Singapore | Mixed | Yes (not described) | IES (≥26) | GHQ-28 (≥5) | - | - | High |
| Sim, Chong et al. (2004) | SARS | 277 | 85.2 | Singapore | Mixed | No | IES-R (diagnosis) | GHQ-28 (≥5) | - | - | High |
| Sin & Chan (2004) | SARS | 47 | NR | Singapore | Mixed | No | IES (≥30) | GHQ-28 (≥5) | - | - | Medium |
| Su et al. (2007) | SARS | 102 | NR | Taiwan | Nurses | No | DTS (≥23) | - | BDI (≥10) | - | High |
| Tam et al. (2004) | SARS | 652 | 79 | Hong Kong | Mixed | No | - | CHQ-12 (≥3) | - | - | Medium |
Notes. Cut-offs for each measure are reported in parentheses. a123 at follow-up. BDI = Beck Depression Inventory; CES-D = Centre for Epidemiological Studies Depression Scale; CHQ = Chinese Health Questionnaire; DTS = Davidson Trauma Scale; GAD-7 = Generalised Anxiety Disorder Assessment; GHQ = General Health Questionnaire; IES = Impact of Events Scale; IES-R = Impact of Events Scale-Revised; K10 = Kessler Psychological Distress Scale; NR = not reported.
3.3. Risk of bias within studies
Overall, eight studies were rated as high quality, eight as medium quality and two as low quality (Table 1; see Supplementary Material 4 for full quality ratings). The majority of studies (15 of 18) were judged to have clearly specified their study population. Ten of the studies had a participation rate greater than 50%. All assessment tools were self-report questionnaire measures; one study used a structured interview with a sub-set of HCWs, which will be reported separately. In only two studies was it explicitly stated that a PTSS measure was completed in relation to the relevant pandemic.
3.4. Prevalence of psychiatric disorders
3.4.1. Prevalence of clinically significant post-traumatic stress symptoms (PTSS)
Nine studies were used to derive prevalence estimates for PTSS in the acute phase and two in the 12 months onwards window; single studies addressed the 1.5–5.9 and 6–11.9 m windows. Forest plots for each time window are displayed in Figure 2. The pooled estimate for clinically significant PTSS in the acute phase (i.e. during the pandemic itself and up to 1.5 months after the end of the pandemic) was 23.4% (95% CI, 16.3, 31.2; k = 9; N = 4147; Chan et al. 2004, Chen et al. 2005, Lai et al. 2020, Lee et al. 2018, Lin et al. 2007, Maunder et al. 2004, Sim, Chong et al. 2004, Sim & Chan 2004, Su et al. 2007). The pooled studies had a large degree of heterogeneity (Q[8] = 190.00, p <.0001; I2 = 96.2%). A single study addressed the 1.5–5.9 m window (57.1%; 95% CI 49.1, 65.0; N = 147; Jung et al. 2020), and a single study also addressed the 6–11.9 m window (17.7%; 95% CI 10.8, 25.9; N = 96; Phua et al. 2005).
Figure 2.
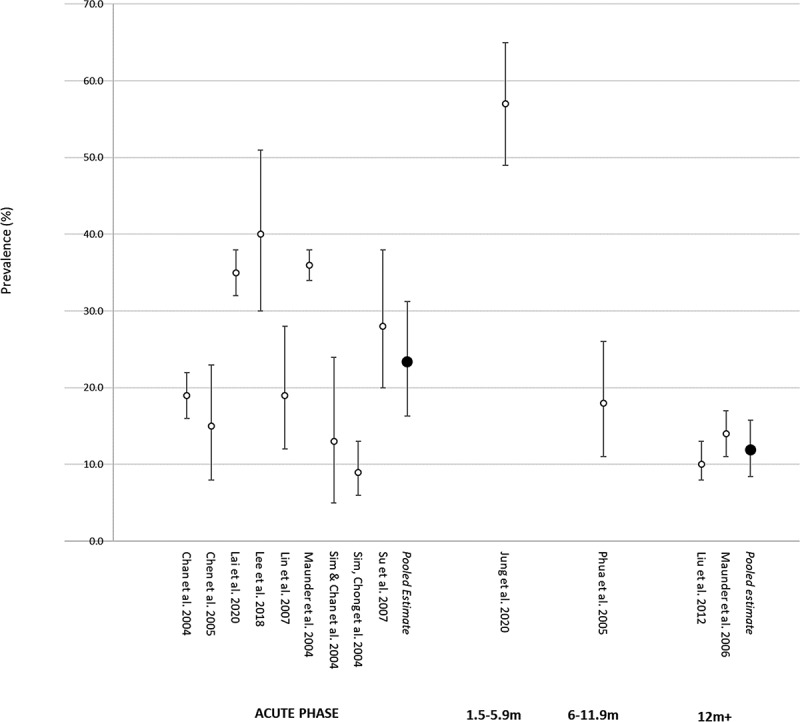
Forest plot showing prevalence of PTSS by time window.
The pooled estimate for the period 12 months onwards was 11.9% (95% CI 8.4, 15.8; k = 2; N = 1136; Liu et al. 2012, Maunder et al. 2006). The pooled studies had a large degree of heterogeneity (Q[1] = 3.89, p < .05; I2 = 74.3%). One of these studies (Lancee et al., 2008) also conducted structured clinical interviews for PTSD with a sub-set of HCWs in Toronto (139 of 587; 24%). Two HCWs met criteria for current PTSD, with one identifying the SARS experience as the most severe traumatic event.
3.4.2. Prevalence of anxiety
One study reported the prevalence of clinically significant anxiety in the acute phase, as measured by the GAD-7 (Spitzer, Kroenke, & Williams et al., 2006) (12.3%; 95% CI 10.5, 14.1; N = 1257; Lai et al. 2020).
3.4.3. Prevalence of depression
Two studies were used to derive the prevalence estimate for depression in the acute phase; one study addressed the 12 months onwards window. Forest plots for each time window are displayed in Supplementary Material 5. The pooled estimate for depression in the acute phase was 20.2% (95% CI 9.5, 33.7; k = 2; N = 1359). The pooled studies had a large degree of heterogeneity (Q[1] = 9.26, p < 0.003; I2 = 89.2%). A further study considered the prevalence of depression in the 12 month onwards window (8.7%; 95% CI 6.5, 11.3; N = 549; Liu et al. 2012). In their study that utilised structured interviews for psychiatric disorders, Lancee and colleagues (Lancee et al., 2008) found that there was one new case with a major depressive episode, among 93 HCWs who reported no pre-SARS mental health disorders.
3.4.4. Prevalence of general psychiatric screening cases
Eight studies were used to derive the prevalence estimate for general psychiatric caseness within the acute phase, two in the 6–12 m window and two in the 12 months onwards window. Forest plots for each time window are displayed in Figure 3. The pooled estimate for the prevalence of positive cases on general psychiatric screening instruments in the acute phase was 34.1% (95% CI 18.7, 51.4; k = 8, N = 3971; Chan et al 2004, Chong et al 2004, Goulia et al 2010, Lin et al 2007, Nickell et al 2004, Sim, Chong et al 2004, Sim & Chan 2004, Tam et al 2004). The pooled studies had a large degree of heterogeneity (Q[7] = 1199.28, p < 0.0001; I2 = 99.1%).
Figure 3.
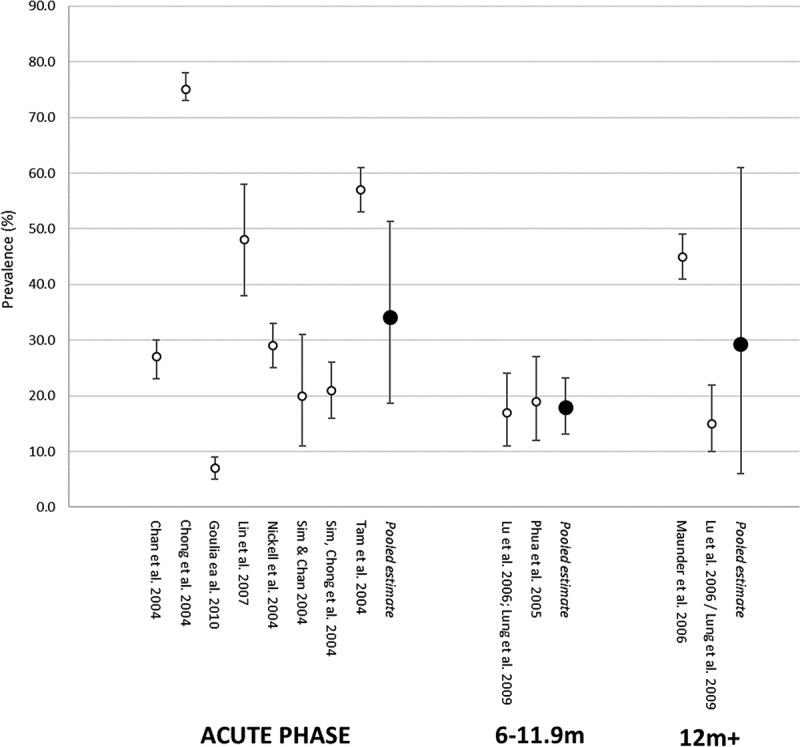
Forest plot showing prevalence of general psychiatric screening by time window.
For the 6- to 12- month window the pooled estimate was 17.9% (95% CI 13.1, 23.2; k = 2; N = 223; Lu et al 2009/Lung et al 2009, Phua et al 2005), with no significant heterogeneity (Q[1] = 0.08, p = 0.78; I2 = 0.0%). For the 12 months onwards window, the pooled estimate was 29.3% (95% CI 6.0, 61.0; k = 2; N = 710; Maunder et al 2006, Lu et al 2006/Lung et al 2009). These studies were associated with a large degree of heterogeneity (Q[1] = 44.60, p < .0001; I2 = 97.8%). Maunder and colleagues (2006) used a relatively low threshold for indicating caseness, possibly inflating the numbers that screened positive (44.9%); when applying the same criteria to a hospital not affected by the SARS epidemic, the authors found a large proportion (30.2%) scored above this threshold.
3.4.5. Prevalence by profession
Further meta-analyses were conducted to consider whether prevalence differed by profession. These were restricted to the acute phase given how little data was available at follow up. The main professions considered were doctors and nurses. Regarding clinically significant PTSS the prevalence estimate for doctors was 18.7% (95% CI = 6.0, 36.4; k = 3; N = 698; Chan et al. 2004, Lai et al. 2020, Sim, Chong et al. 2004), while for nurses it was 21.4% (95% CI 13.0, 31.3; k = 5; N = 1686; Chan et al. 2004, Chen et al. 2005, Lai et al. 2020, Sim, Chong et al. 2004, Su et al. 2007); for the 3 studies that included both doctors and nurses, there was no difference in prevalence (odds ratio = .87 [95% CI .71, 1.08]; Chan et al. 2004, Lai et al. 2020, Sim, Chong et al. 2004). Regarding general psychiatric screening cases the estimate for doctors was 31.6% (95% CI 13.8, 52.7; k = 5; N = 508; Chan et al. 2004, Chong et al. 2004, Goulia et al. 2010, Nickell et al. 2004, Sim, Chong et al. 2004), while for nurses it was 38.2% (95% CI 19.0, 59.4; k = 5; 1683; Chan et al. 2004, Chong et al. 2004, Goulia ea al. 2010, Nickell et al. 2004, Sim, Chong et al. 2004); there was no significant in prevalence between nurses and doctors (the same five studies; odds ratio = 1.29 [95% CI = 0.45, 1.32]).
3.5. Exploratory sub-group analyses in the acute phase
Given the significant heterogeneity present for most of the meta-analyses conducted, exploratory sub-group analyses were undertaken to see if more consistent findings might be discernible. Such analyses were only possible in relation to the acute phase. Moderator analyses were not undertaken, given how few studies were available.
First, meta-analyses were undertaken that included only those studies which addressed the SARS pandemic (the bulk of the retrieved literature). The SARS-only prevalence meta-analysis for acute PTSS yielded a pooled prevalence estimate of 19.7% (95% CI 13.1, 27.4; k = 7; N = 2813; Chan et al. 2004, Chen et al. 2005, Lin et al. 2007, Maunder et al. 2004, Sim, Chong et al. 2004, Sim & Chan 2004, Su et al. 2007), only slightly less than the estimate for all studies. There remained a large degree of heterogeneity (Q[6] = 159.51, p < .0001; I2 = 93.8%). The SARS-only prevalence meta-analysis for acute general psychiatric screening cases yielded a pooled prevalence estimate of 39.1% (95% CI 23.9, 55.6; k = 7; N = 3502; Chan et al. 2004, Chong et al. 2004, Lin et al. 2007, Nickell et al. 2004, Sim, Chong et al. 2004, Sim & Chan 2004, Tam et al. 2004), a slightly higher than figure than that obtained for all studies. Again, this did not improve heterogeneity, which remained large (Q[6]) = 749.37, p.0001; I2 = 99.8%).
Second, meta-analyses that used only the same measure were undertaken. For the IES (PTSS) (Horowitz, Wilner, & Alvarez, 1979), a point estimate of 21.0% was obtained (95% CI 11.7, 32.0; k = 4; N = 2351; Q[3] = 87.25, p < .0001; I2 = 95.7%; Chan et al. 2004, Chen et al. 2005, Maunder et al. 2004, Sim & Chan 2004). For the IES-R (Weiss & Marmar, 1997) a point estimate of 26.6% was obtained (95% CI 9.4, 48.7; k = 3; N = 1611; Q[2] = 97.67, p < .0001; I2 = 97.9%; Lai et al. 2020, Lee et al. 2018, Sim, Chong et al. 2004). For the GHQ-28 (Goldberg & Hillier, 1979) a point estimate of 17.7 (95% CI 9.3, 28.1; k = 4; N = 1462; Q[3] = 87.60, p < .0001; I2 = 94.9%; Chan et al. 2004, Goulia et al. 2010, Sim, Chong et al. 2004, Sim & Chan 2004). For each analysis there remained a large degree of heterogeneity.
It is noteworthy that even when restricting analyses to a single measure (e.g. IES, IES-R, GHQ-28), different cut-off scores were used to denote caseness. For example, if the point estimate GHQ-28 in the acute phase was restricted to studies that used a cut-off score of 5, a point estimate of 23.4% was obtained (95% CI 18.6, 28.5; k = 3; N = 993; Chan et al. 2004, Sim, Chong et al. 2004, Sim & Chan 2004) that did not have significant heterogeneity (Q[2] = 4.88, p = 0.087; I2 = 58.7%).
4. Discussion
The studies identified in this rapid systematic review and meta-analysis predominantly addressed clinically significant PTSS and general psychiatric caseness in HCW in the acute phase, i.e. during and immediately after a pandemic. Fewer studies addressed longer-term follow up. The majority of the studies considered the SARS pandemic. Our findings suggest that a significant minority of HCWs met threshold for clinically significant PTSS and general psychiatric caseness in the acute phase, with no apparent differences between doctors and nurses with respect to either outcome. However, a precise estimate of either PTSS and general psychiatric caseness cannot be derived from the reviewed literature given the large heterogeneity in study findings.
The limited data from follow-up studies suggested that there was a lower rate of PTSS several months after a pandemic (in particular SARS). Only two studies addressed PTSS rates more than 12 months post-pandemic and the results demonstrated significant heterogeneity. Both studies were large (>500 participants) and yielded a reasonably precise estimate of PTSS prevalence (95% CI 8.4–15.8%) that was markedly lower than the (albeit more imprecise) estimate for the acute phase. Whilst this could indicate a reduction in PTSS over time, it is important to stress that the lower number of follow-up studies and the high heterogeneity within the included studies make comparison between time points very difficult; as such an apparent reduction in PTSS should be considered with caution.
For general psychiatric screening, the picture was not clear. While two studies suggested an improvement by the time of the 6–12 month post-pandemic window, there was considerable heterogeneity at the time on the 12 months onwards timeframe. We would highlight the potential contribution to between-study heterogeneity of using different cut-offs in screening instruments. The one study to use structured interview assessments at follow-up found very low rates of psychiatric disorder that might be directly attributable to HCW experiences during a pandemic.
We found that PTSS were elevated during the acute phase and at 12 months, similar to existing populations of at-risk health workers such as rescue workers (10%) (Berger, Coutinho, & Figueira et al., 2012), paramedics (11%) (Petrie, Milligan-Saville, & Gayed et al., 2018), and HCWs in general (14.8%) (Jacob Sendler, Rutkowska, & Makara-Studzinska, 2016) who report higher levels of PTSS than the general population (e.g. 3.5%) (Kessler, Chiu, & Demler et al., 2005). Whilst there were very limited data pertaining to the course of clinically significant PTSS, our findings may be considered broadly consistent with the existing literature that suggests that natural recovery is common in trauma-exposed individuals. (Hiller, Meiser-Stedman, & Fearon et al., 2016; Morina, Wicherts, & Lobbrecht et al., 2014)
However, it is likely that the COVID may have a longer, ongoing acute phase than in those studies reviewed such staff may have longer exposure to stress whilst experiencing PTSS. Furthermore, it is possible that COVID-19 represents a degree of threat more serious than that from previous pandemics due to factors including lack of personal protective equipment, impaired systemic resilience factors related to social distancing and uncertainties around the duration of the pandemic. As such, our findings may provide an under-estimate. Comparison with a recent review of HCWs exposed to COVID-19 (Pappa, Ntella, & Giannakas et al., 2020) is appropriate. This systematic review and meta-analysis found that 23.3% and 22.8% HCWs working during the first few months of the COVID-19 pandemic experienced symptoms of anxiety and depression, respectively, as well as 38.9% experiencing insomnia. Sex and occupational differences were also reported within the sample, with female HCWs reporting increased symptoms compared to male medical staff. These findings suggest a slight increase in the prevalence of depression compared with the findings of the present review.
A recent position paper called for high-quality research on the mental health effects of COVID-19 within vulnerable groups, including HCW (Holmes, O’Connor, & Perry et al., 2020). With respect to clinical care for HCWs, these findings underline the need to consider closely the mental health needs of this workforce, particularly given how frequent acute mental health disturbance may be. In themselves, such acute reactions to pandemics may be not be classed as ‘disorders’ given the very real threat that close clinical contact with infected patients may present. Whilst these reactions are considered normal, it is imperative to consider how best to support staff during the ongoing crisis, including how to detect persistent PTSD early. An ‘active monitoring’ approach as proposed by the UK NICE guidelines for PTSD (National Institute for Health and Care Excellence, 2018) or a screen and treatment approach as used in response to other major incidents (Gobin, Rubin, & Albert et al., 2018) may be advisable for HCWs experiencing an acute PTSS reaction. Indeed, the persistence of PTSS, and the emergence of what may be properly classed as disorders, is not well understood in this population and service planning for HCWs may need to draw on estimates drawn from other trauma-exposed populations. Moreover, our findings demonstrate the variety of screening tools and cut-off scores that have been used to determine ‘caseness’. Clinically, services that use such tools need to be careabout the use of screening instruments to identify at-risk staff, and the potential impact of even small differences in cut-offs.
This review highlights the need for urgent research to include more extensive follow-up, in particular using prospective longitudinal cohorts of HCWs, and consider disorders other than PTSS; depression in particular has received very limited attention. While screening instruments for outcomes like PTSS and depression have obvious benefits in terms of cost-effectiveness, they may also miss key aspects of HCW experience and may fail to consider the impact of other factors, e.g. prior or non-healthcare traumatic experiences. Other aspects of health and well-being (e.g. substance abuse, functioning) were not considered in detail. Though some longer versions of the GHQ/CHQ do include items relating to social functioning, these were not normally presented separately. More detailed assessment (e.g. using structured interviews), similar to that undertaken by Lancee and colleagues (Lancee et al., 2008) may be warranted. It was beyond the scope of the present rapid review to identify risk factors for mental health disorders. Although we were able to consider differences in prevalence for two professions (doctors and nurses), the needs of other HCWs, and allied professions and hospital staff also need to be addressed in detail.
This study is strengthened by its inclusion of studies addressing clinically similar situations, its detailed coverage of methodological issues and its a priori definition of time windows. The study is limited by the limited available data and its heterogeneity, and the relative narrowness of outcomes the literature has addressed (e.g. sex differences could not be considered).
5. Conclusion
There is evidence that HCWs working in pandemics are at increased risk of a range of adverse mental health outcomes, at least in the acute phase; two studies suggesting elevated rates of clinically significant PTSS at follow up. Research is needed to understand the long-term effects of psychological stress and trauma on HCWs during COVID and how best to support HCWs during and after the pandemic.
Supplementary Material
Disclosure statement
Sophie M. Allan, Rebecca Bealey, Jennifer Birch,Toby Cushing, Sheryl Parke, Georgina Sergi and Richard Meiser-Stedman report no conflicts of interest. Michael Bloomfield is aconsultant psychiatrist at the Traumatic Stress Clinic in Londonwhich is part of the UK National Health Service. Dr Bloomfield has previously undertaken consultancy work for SpectrumTherapeutics.
Supplemental Material
Supplemental data for this article can be accessed here.
References
- Adams, J. G., & Walls, R. M. (2020). Supporting the health care workforce during the COVID-19 global epidemic. JAMA, 323(15), 1439. [DOI] [PubMed] [Google Scholar]
- Barendregt, J. J., Doi, S. A., Lee, Y. Y., Norman, R. E., Vos, T. (2013). Meta-analysis of prevalence. Journal of Epidemiology and Community Health, 67(11), 974–12. [DOI] [PubMed] [Google Scholar]
- BBC News Online . (2020). Coronavirus: Mental health hotline for NHS staff. Secondary Coronavirus: Mental health hotline for NHS staff. Retrieved from https://www.bbc.co.uk/news/health-52202570.
- Berger, W., Coutinho, E. S. F., Figueira, I., Marques-Portella, C., Luz, M. P., Neylan, T. C., Marmar, C. R., & Mendlowicz, M. V. (2012). Rescuers at risk: A systematic review and meta-regression analysis of the worldwide current prevalence and correlates of PTSD in rescue workers. Social Psychiatry and Psychiatric Epidemiology, 47(6), 1001–1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen, C. S., Wu, H. Y., Yang, P., Yen, C. F. (2005). Psychological distress of nurses in Taiwan who worked during the outbreak of SARS. Psychiatric Services, 56(1), 76–79. [DOI] [PubMed] [Google Scholar]
- Chong, M. Y., Wang, W. C., Hsieh, W. C., Lee, C. Y., Chiu, N. M., Yeh, W. C., Huang, O. L.,Wen, J. K., Chen, C. L. (2004). Psychological impact of severe acute respiratory syndrome on health workers in a tertiary hospital. British Journal of Psychiatry, 185(2), 127–33. [DOI] [PubMed] [Google Scholar]
- Gobin, M., Rubin, G. J., Albert, I., Beck, A., Danese, A., Greenberg, N., Grey, N., Smith, P., & Oliver, I. (2018). Outcomes of mental health screening for UK nationals affected by the 2015-2016 terrorist attacks in Tunisia, Paris, and Brussels. Journal of Traumatic Stress, 31(4), 471–479. [DOI] [PubMed] [Google Scholar]
- Goldberg, D. P., & Hillier, V. F. (1979). A scaled version of the General Health Questionnaire. Psychological Medicine, 9(1), 139–145. [DOI] [PubMed] [Google Scholar]
- Goulia, P., Mantas, C., Dimitroula, D., Mantis, D., Hyphantis, T. (2010). General hospital staff worries, perceived sufficiency of information and associated psychological distress during the A/H1N1 influenza pandemic. BMC Infectious Diseases, 10(1), 322–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenberg, N., Docherty, M., Gnanapragasam, S., & Wessely S. (2020). Managing mental health challenges faced by healthcare workers during COVID-19 pandemic. BMJ, 368. doi: 10.1136/bmj.l6968 [DOI] [PubMed] [Google Scholar]
- Hiller, R. M., Meiser-Stedman, R., Fearon, P., Lobo, S., McKinnon, A., Fraser, A., & Halligan, S. L. (2016). Research review: Changes in the prevalence and symptom severity of child posttraumatic stress disorder in the year following trauma - a meta-analytic study. Journal of Child Psychology and Psychiatry, and Allied Disciplines. doi: 10.1111/jcpp.12566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes, E. A., O’Connor, R. C., Perry, V. H., V. H., Tracey, I., Wessely, S., Arseneault, L., Ballard, C., Christensen, H., Cohen Silver, R., Everall, I., Ford, T., John, A., Kabir, T., King, K., Madan, I., Michie S., Przybylski, A. K., Shafran, R., Sweeney, A., Worthman, C. M., Yardley, L., Cowan, K., Cope, C., Hotopf, M., & Bullmore, E. (2020). Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. The Lancet Psychiatry, 7(6), 547–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horowitz, M., Wilner, N., & Alvarez, W. (1979). The impact of event scale: A measure of subjective stress. Psychosomatic Medicine, 41, 209–218. [DOI] [PubMed] [Google Scholar]
- Jacob Sendler, D., Rutkowska, A., & Makara-Studzinska, M. (2016). How the exposure to trauma has hindered physicians’ capacity to heal: Prevalence of PTSD among healthcare workers. The European Journal of Psychiatry, 30(4), 321–334. [Google Scholar]
- Jung, H., Jung, S. Y., Lee, M. H., & Kim, M. S. (2020). Assessing the Presence of Post-Traumatic Stress and Turnover Intention Among Nurses Post-Middle East Respiratory Syndrome Outbreak: The Importance of Supervisor Support. Workplace Health & Safety, 2165079919897693–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler, R. C., Chiu, W. T., Demler, O., Merikangas, K. R., & Walters, E. E. (2005). Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the national comorbidity survey replication. Archives of General Psychiatry, 62(6), 617–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai, J., Ma, S., Wang, Y., Cai, Z., Hu, J., Wei, N., Wu, J., Du, H., Chen, T., Li, R., Tan, H., Kang, L., Yao, L., Huang, M., Wang, H., Wang, G., Liu, Z., Hu, S. (2020). Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Network Open, 2020, e203976-e76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lancee, W. J., Maunder, R. G., & Goldbloom, D. S. (2008). Prevalence of psychiatric disorders among Toronto hospital workers one to two years after the SARS outbreak. Psychiatric Services (Washington, DC), 59(1), 91–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin, C. Y., Peng, Y. C.., Wu, Y. H., Chang, J., Chan, C. H., Yang, D. Y. (2007). The psychological effect of severe acute respiratory syndrome on emergency department staff. Emergency Medicine Journal, 24(1), 12–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, X., Kakade, M., Fuller, C. J., Fan, B., Fang, Y., Kong, J., Guan, Z., & Wu, P. (2012). Depression after exposure to stressful events: lessons learned from the severe acute respiratory syndrome epidemic. Comprehensive Psychiatry, 53(1), 15–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Livingston, E., Desai, A., & Berkwits, M. (2020). Sourcing personal protective equipment during the COVID-19 pandemic. JAMA, 323(19), 1912. [DOI] [PubMed] [Google Scholar]
- Lee, S. M., Kang, W. S., Cho, A. R., Kim, T., & Park, J. K. (2018). Psychological impact of the 2015 MERS outbreak on hospital workers and quarantined hemodialysis patients. Compr Psychiatry, 87, 123–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu, Y. C., Shu, B. C., Chang, Y. Y., & Lung, F. W. (2006). The mental health of hospital workers dealing with severe acute respiratory syndrome. Psychotherapy and Psychosomatics, 75(6), 370–375. [DOI] [PubMed] [Google Scholar]
- Lung, F. W., Lu, Y. C., Chang, Y. Y., & Shu, B. C. (2009). Mental symptoms in different health professionals during the SARS attack: A follow-up study. Psychiatric Quarterly, 80(2), 107–16. [DOI] [PubMed] [Google Scholar]
- Maunder, R. (2004). The experience of the 2003 SARS outbreak as a traumatic stress among frontline healthcare workers in Toronto: Lessons learned. Philosophical Transactions B: Biological Sciences, 359(1447), 1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maunder, R. G., Lancee, W. J., Balderson, K. E., Bennett, J. P., BorgundvaagX, B., Evans, S., Fernandes, C. M., Goldbloom, D. S., Gupta, M., Hunter, J. J., & Hall, L. M. (2006). Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerging Infectious Diseases, 12(12), 1924–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maunder, R. G., Lancee, W. J., Rourke, S., Hunte,r J. J., Goldbloom, D., Balderson, K., Petryshen, P., Steinberg, R., Wasylenki, D., Koh, D., & Fones, C. S. (2004). Factors associated with the psychological impact of severe acute respiratory syndrome on nurses and other hospital workers in Toronto. Psychosom Med, 66(6), 938–42. [DOI] [PubMed] [Google Scholar]
- Moher, D., Liberati, A., Tetzlaff, J., & Altman, D. G. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Annals of Internal Medicine, 151(4), 264–269. [DOI] [PubMed] [Google Scholar]
- Morina, N., Wicherts, J. M., Lobbrecht, J., & Priebe, S. (2014). Remission from post-traumatic stress disorder in adults: A systematic review and meta-analysis of long term outcome studies. Clinical Psychology Review, 34(3), 249–255. [DOI] [PubMed] [Google Scholar]
- National Institute for Health and Care Excellence . (2018). Guideline 116: Post-traumatic stress disorder. Secondary Guideline 116: Post-traumatic Stress Disorder. Retrieved from https://www.nice.org.uk/guidance/ng116
- Nickell, L. A., Crighton, E. J., Tracy, C. S., Al-Enazy, H., Bolaji, Y., Hanjrah, S., Hussain, A., Makhlouf, S., Upshur, R. E. (2004). Psychosocial effects of SARS on hospital staff: survey of a large tertiary care institution. Cmaj, 170(5), 793–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pappa, S., Ntella, V., Giannakas, T., Giannakoulis, V. G., Papoutsi, E., & Katsaounou, P. (2020). Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain, Behavior, and Immunity. doi: 10.1016/j.bbi.2020.05.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petrie, K., Milligan-Saville, J., Gayed, A., Deady, M., Phelps, A., Dell, L., Forbes, D., Bryant, R. A., Calvo, R. A., Glozier, N., & Harvey, S. B. (2018). Prevalence of PTSD and common mental disorders amongst ambulance personnel: A systematic review and meta-analysis. Social Psychiatry and Psychiatric Epidemiology, 53(9), 897–909. [DOI] [PubMed] [Google Scholar]
- Phua, D. H., Tang, H. K., & Tham, K. Y. (2005). Coping Responses of Emergency Physicians and Nurses to the 2003 Severe Acute Respiratory Syndrome Outbreak. Academic Emergency Medicine (AEM), 12(4), 322. [DOI] [PubMed] [Google Scholar]
- R: A language and environment for statistical computing . (2014). [program]. Vienna, Austria: R Foundation for Statistical Computing. [Google Scholar]
- Sim, S. S., & Chan, Y. H. (2004). Psychological impact of the SARS outbreak on a Singaporean rehabilitation department. International Journal of Therapy & Rehabilitation, 11(9), 417. [Google Scholar]
- Spitzer, R. L., Kroenke, K., Williams, J. B. W., & Lowe, B. (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166(10), 1092–1097. [DOI] [PubMed] [Google Scholar]
- Sterne, J. A., Sutton, A. J., Ioannidis, J. P., Terrin, N., Jones, D. R., Lau, J., Carpenter, J., Rücker, G., Harbord, R. M., Schmid, C. H., & Tetzlaff, J. (2011). Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. Bmj, 343, d4002. [DOI] [PubMed] [Google Scholar]
- Su, T. P., Lien, T. C., Yang, C. Y., Su, Y. L., Wang, J. H., Tsai, S. L., & Yin, J. C. (2007). Prevalence of psychiatric morbidity and psychological adaptation of the nurses in a structured SARS caring unit during outbreak: A prospective and periodic assessment study in Taiwan. Journal of Psychiatric Research, 41(1–2), 119–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tam, C. W., Pang, E. P., Lam, L. C., 7 Chiu, H. F. (2004). Severe acute respiratory syndrome (SARS) in Hong Kong in 2003: stress and psychological impact among frontline healthcare workers. Psychol Med, 34(7), 1197–204. [DOI] [PubMed] [Google Scholar]
- Viechtbauer, W. (2010). Conducting meta-analyses in R with the metafor package. Journal of Statistical Software, 36(3), 1–48. [Google Scholar]
- Weiss, D., & Marmar, C. (1997). The impact of event scale—Revised, assessing psychological trauma and PTSD (pp. 399–411). New York: Guilford. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


