Abstract
Vibrators are an evidence-based treatment for a variety of sexual dysfunctions and sexual enhancement; however, the use of a genital vibrator lacks best practice recommendations. This aim of this article is to provide current, best practice recommendations regarding the use of vibratory stimulation for the treatment of sexual dysfunction and/or sexual or relationship enhancement. A multidisciplinary team of sexual health specialists collaborated to develop best practice recommendations based on a narrative literature review. Recommendations for the use of vibratory stimulation for the treatment of sexual dysfunction are provided, with special attention to counseling patients on choosing and safely using a vibrator. Further study is needed to determine the most effective methods to counsel patients on vibrator use and to provide evidence-based cleaning recommendations.
Keywords: Female sexual arousal disorder, orgasmic disorder, sexual physiology, medical therapy, retrograde ejaculation
Introduction
Vibratory stimulation of the genitals is an evidence-based treatment for erectile dysfunction (Stein, Lin, & Wang, 2014), ejaculatory difficulties (Previnaire, Lecourt, Soler, & Denys, 2014; Sobrero, Stearns, & Blair, 1965; Sonksen & Ohl, 2002) and anorgasmia, (Graham, 2014) and has shown benefit for pelvic floor dysfunction and vulvar pain (Bakker et al., 2015; Dhar & Nunns, 2009; Zolnoun, Lamvu, & Steege, 2008). There is also a positive correlation between vibrator use and sexual arousal as well as overall sexual function (Herbenick et al., 2009; Reece et al., 2009). Thus, clinicians are increasingly recommending the use of vibrators as a therapy for sexual dysfunction (Herbenick, Barnhart, Beavers, & Benge, 2015). Further, vibrators are used by many for sexual enhancement, with over half (53%) of adult women and nearly half (44%) of adult men having used a vibrator in their lifetime (Herbenick et al., 2009; Reece et al., 2009).
Vibrators are classified by the US Food and Drug Administration (FDA) as an obstetrical and gynecological therapeutic device for the treatment of sexual dysfunction (Stabile, 2013). Vibrators are arguably a high-risk therapeutic device because they are inserted into body cavities and often shared between partners (Herbenick et al., 2009; Reece et al., 2009; Reece et al., 2010). In fact, the majority of sexual device-related emergency department visits are due to a vibrator beyond reach in the anal cavity of men (i.e. an anal foreign body) (Griffin & McGwin, 2009), and there has been at least one fatality due to rectal perforation from a vibrator (Waraich, Hudson, & Iftikhar, 2007). Additionally, sharing sexual devices has been shown to increase the risk of sexually transmitted infections, including human papillomavirus (HPV) and human immunodeficiency virus (HIV) (Anderson, Schick, Herbenick, Dodge, & Fortenberry, 2014; Kwakwa & Ghobrial, 2003).
The responsibility is on health care providers to educate patients about the safe use of sexual devices for sexual health. However, the vast majority of health care providers did not receive sexual health training in their graduate programs (Malhotra, Khurshid, Hendricks, & Mann, 2008). To our knowledge, no evidence-based recommendations exist on advising patients on the safe use of genital vibration. The present article proposes to fill that gap by outlining best practice recommendations, developed by a multidisciplinary team of health care providers, for advising patients on choosing and safely using a vibrator. These recommendations are appropriate for use by clinicians and nonclinicians, sexual medicine providers and sex educators, therapists, and counselors.
Methods
A multidisciplinary team of sexual health specialists, comprised of two clinical psychologists (a sex therapist and sex researcher), a health behavior research scientist and sex educator, a sexual medicine physician, a urologist and a pelvic floor physical therapist, collaborated to develop best practice recommendations. First, a narrative literature review (not a systematic review) was conducted. The literature review involved a comprehensive English-language search of several databases from 1946 to 23 August 2016, which included MEDLINE In-Process & Other Non-Indexed Citations and Ovid MEDLINE. Keywords included sexual dysfunction and vibrator. Papers were selected for inclusion based on the authors’ collective expertize and clinical experience. Authors then individually reviewed evidence and provided clinical recommendations based on their clinical specialty (e.g. urology, women’s health, physical therapy, sex therapy). The first author (J. E. Rullo) subsequently organized and consolidated these reviews and recommendations into best practice recommendations. All authors reviewed and revised this document for consensus.
Results
Choosing a vibrator
Choosing a vibrator may feel overwhelming given the countless varieties of commercially available vibrators. Vibrators differ based on physical characteristics (size, shape, material) and functional characteristics (speed, type and intensity of vibration). These, in conjunction with treatment needs and patient preferences, should be reviewed when counseling a patient on choosing a vibrator (Table 1) (Herbenick et al., 2015).
Table 1.
How to choose a vibrator.
| Questions for choosing a vibrator | If answer is affirmative |
|---|---|
| (1) Would you prefer to use a vibrator for penetration? | Size and shape of vibrator matter. Continue to next question. |
| (2) Is penetration anal? | Vibrator must have a wide base or string. Continue to next question. |
| (3) Do you have pain with penetration? | Choose a vibrator average or below average in length and circumference and, if possible, seamless along the shaft. Alternatively, an external vibrator may be preferable. If no, then choice is based on preference. |
| (4) Do you want/need an intense vibration? | Choose an electric vibrator or vibrator with multiple speed/intensity options. |
| (5) Are you using this with a partner? | Involve partner in the selection process. |
| (6) Is privacy a concern? | Choose a cordless, waterproof vibrator for shower/bath, play music while using a vibrator, choose a quieter vibrator, find ways to create privacy. |
Physical characteristics of vibrators
Vibrators differ in size, shape and material. Most commonly, vibrators are shaped similar to a phallus, but also come in many other shapes. Of vibrators sold on popular websites, the average length is less than 6 inches, with a range of 2–15 inches. The average circumference is less than 4.5 inches, with a range of 1.57–7.85 inches (Herbenick et al., 2015). Some vibrators are hands-free and fit snugly between the labia; are strapped to the vulva with a harness; are shaped like a C with one end inserted in the vagina and the other stimulating the clitoris; or can be attached to a stable surface (with suction or non-slip base). Many vibrators have an appendage that provides clitoral stimulation in conjunction with vaginal stimulation. Some are shaped like eggs or animals and curve for purported Grafenberg-spot (G-spot) stimulation.
For patients desiring a vibrator that provides internal stimulation, shape and size are important factors to consider. For example, some vibrators that are designed specifically for external stimulation (e.g. vibrators known as bullets) are connected by wire to a remote control and thus are not recommended for internal use. Other external vibrators may not be safe for internal use due to an exposed or loose-fitting battery compartment and the need to avoid batteries being left in the vaginal canal.
Patients with genital, anal or pelvic pain, genitourinary syndrome of menopause or reporting pain with sexual activity, but who also desire internal vibration should be counseled to use a vibrator that is average or below average in length and circumference and that has a smooth, if not seamless, shaft. For safety (i.e. avoidance of the product drifting beyond reach), any sexual device inserted into the anus must have a string or a wide base. Insertional discomfort may be reduced, and pleasure increased, with the use of a lubricant (described further in what follows) (Herbenick et al., 2015; Sutton, Boyer, Goldfinger, Ezer, & Pukall, 2012).
Vibrators are made from many different materials including silicone, hard plastic, glass, stainless steel, wood, rubber, vinyl/cyberskin, jelly rubber and other varied thermoplastic elastomers not listed. Many companies that sell vibrators describe them as for “novelty use only”, presumably to bypass FDA regulation. Some unregulated vibrators made of jelly rubber have been found to contain phthalates, a potential human carcinogen. Several types of phthalates, including those used in vibrators, have been banned from use in children’s toys by the United States Congress (Stabile, 2013). However, after extensive study of phthalates in sex devices, the Danish Environmental Protection Agency concluded that they are safe to use for up to 1 hour per day. Even so, they warned that for women who are breastfeeding or pregnant, use should be limited to 15 minutes per week due to the potential for minor developmental effects on the fetus (Nilsson, Malmgren-Hansen, Bernth, Pedersen, & Pommer, 2006). Given the concerns mentioned above, it is reasonable to counsel patients to use vibrators made of nontoxic material, such as silicone, hard plastic, glass and stainless steel (Herbenick, 2010). As some vibrators described as “silicone” are likely mixed with other materials, consumers who prefer a vibrator made of silicone might choose one described as using “medical grade silicone” or might choose to purchase from a well-established manufacturer that is forthcoming about the materials used.
Functional characteristics of vibrators
Vibrators vary based on speed, type (e.g. pulsating, surging, escalating) and intensity (acceleration) of vibration. Of commonly sold vibrators, speeds vary from single to multispeed (low-medium-high) to variable speed. Variable speed allows the patient more options and a greater opportunity to explore a speed that works best for their needs. Vibrators also vary in the intensity of vibration, and for some women, specifically those whose sexual function may have been impacted by aging or health conditions, a more intense vibration may be necessary for arousal and orgasm (Connell et al., 2005; Guess et al., 2006; Vardi, Gruenwald, Sprecher, Gertman, & Yartnitsky, 2000). The Hitachi Magic Wand was identified in one study as having a high vibratory acceleration (Prause, Roberts, Legarretta, & Rigney Cox, 2012). However, this same study assessed the vibratory acceleration of a sampling of commercially available vibrators and demonstrated that every vibrator tested had adequate intensity to reach the minimum genital vibratory detection threshold in women averaging 40 years of age (Prause et al., 2012). Thus, although vibrators vary in intensity, it is likely that most commercially available vibrators will be intense enough to meet the needs of premenopausal users.
Vibrators also vary by the type of vibration. Vibrators commonly provide a steady, nonvariable vibration. However, some vibrators provide different types of vibration, including pulsating, surging and escalating. Some women may seek a vibrator with variable vibration in order to avoid genital numbness or desensitization. Genital desensitization has been reported by 16.5% of women who have ever used a vibrator, though it has largely been described as mild and transitory (Herbenick et al., 2009). While it is certainly possible that the genital nerves may adapt to high intensity vibratory stimulation and thus be temporarily less responsive to other forms of stimulation or lower intensity stimulation, this state improves quickly with the introduction of new types of stimulation. In other words, while psychologic dependence on the ease and intensity of stimulation with a vibrator is possible, physiologic dependence is unlikely. Similarly, it is unlikely that, given the continuous restructuring of female genital nerve beds, vibrator use could result in long-term genital desensitization (Prause et al., 2012).
Patient preference
Privacy and partnered use are two patient preferences to keep in mind when counseling patients on choosing a vibrator. Privacy is impacted by the volume level of the motor and by portability. Some vibrators are much quieter than others, and testing the noise level is recommended before purchasing if this is a potential concern. Vibrators also vary in terms of portability, with some operated by batteries (no electric cord) and others requiring an AC outlet (with electric cord). Electric vibrators have the power to provide greater vibratory intensity but have limited portability (Prause et al., 2012). The cord may be cumbersome, especially for partnered sex. Privacy is also impacted by whether the vibrator is waterproof, as a waterproof vibrator affords the patient privacy of use in the shower or bath.
Finally, if the patient plans to use the vibrator with a partner, it is important to encourage a conversation with the partner about his/her preferences. Many women are worried that vibrator use will negatively impact their sexual relationship (Marcus, 2011). Approximately 40% of women and men have used a vibrator with a partner (Herbenick et al., 2009; Reece et al., 2009). A partner’s knowledge and positivity toward vibrator use are associated with a woman’s sexual satisfaction (Herbenick et al., 2010). In the United States, most men and women feel positively about women’s use of vibrators (Herbenick etal., 2011).
Ultimately, for a first-time vibrator user, consider recommending a unit that allows maximum flexibility to explore and determine personal preferences (Figure 1).
Figure 1.
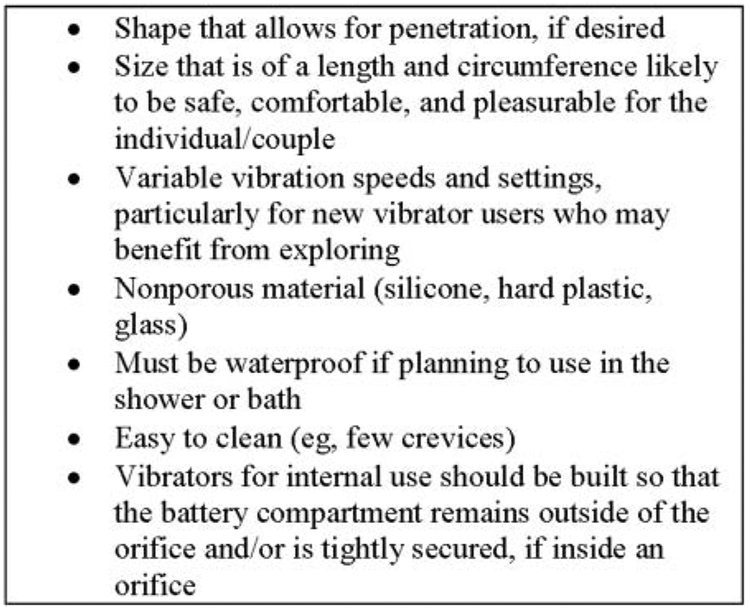
Recommendations for vibrator purchase.
Safe use of a vibrator
In addition to assisting patients in choosing a vibrator that best fits their needs, it is also the responsibility of the provider to counsel patients on safe use. Safe use involves but is not limited to recommendations on how to avoid transfer of sexually transmitted infections (Figure 2) (Aaronson & Shindel, 2010; Committee on Adolescent Health Care, 2013).
Figure 2.
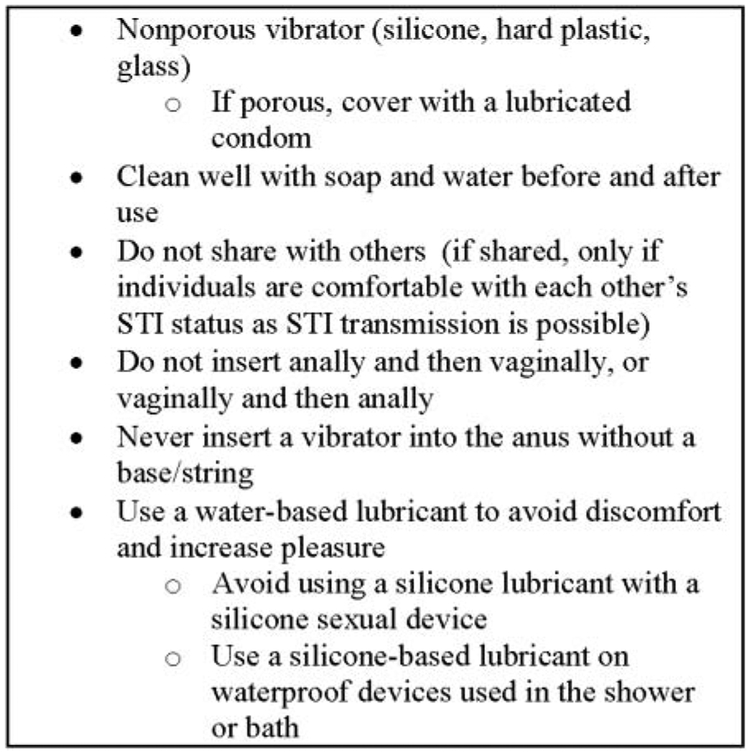
Recommendations for safe vibrator use.
To reduce the risk of sexually transmitted infections, patients should be counseled not to share sexual devices (Committee on Adolescent Health Care, 2013). Sharing of sexual devices has been shown to increase the risk of bacterial vaginosis in women who have sex with women (Marrazzo, Thomas, Agnew, & Ringwood, 2010), has the potential to transfer HPV (Anderson et al., 2014) and has been implicated in at least one case of HIV transmission (Kwakwa & Ghobrial, 2003). Additionally, patients should be advised that inserting a sexual device anally and then vaginally may introduce harmful bacteria into the vagina. For women with HPV, inserting a sexual device vaginally and then anally may introduce HPV into the anus. After anal or vaginal use, a sexual device must be cleaned properly before use in any other body orifice (Committee on Adolescent Health Care, 2013). About 20% of men and 14% of women report never having cleaned a vibrator before or after use (Herbenick et al., 2009; Reece et al., 2009).
Cleaning recommendations are determined by the material composition of the device. Both silicone and thermoplastic elastomer vibrators have been shown to have the potential to transmit HPV immediately after being cleaned by a commercially available sexual device cleaning product. This potential was even greater for thermoplastic elastomer, which maintained traces of HPV 24 hours after cleaning. Despite this risk, there are currently no evidence-based cleaning recommendations for sexual devices (Anderson et al.,2014). Additionally, at the time of this writing, no other organisms have been tested for potential transmission with vibrator use.
Although scientific evidence is lacking, soap and water may be sufficient to clean non-porous (silicone, hard plastic, glass, stainless steel) materials. Care should be taken to thoroughly clean any crevices in the device and when cleaning devices with mechanical components (battery compartment, motor). Air drying is recommended to avoid towel lint. For jelly rubber sexual devices that contain phthalates or for risk-avoidant individuals, a condom can be used on the vibrator (Committee on Adolescent Health Care, 2013; Herbenick, 2009).
The incorrect use of a vibrator is the most common sexual device-related emergency in both men and women (Griffin & McGwin, 2009). This is especially relevant for men who have sex with men, 87% of whom report anal insertion of a vibrator during self-stimulation (Reece et al., 2010). Sexual devices used in the anus should have a wide base or an attached string to avoid loss in the anal cavity. Patients should seek medical treatment immediately if an injury occurs with the use of a sexual device, including lodging of a vibrator in any body orifice (Donaldson et al., 2014; Griffin & McGwin, 2009).
Finally, some vibrators are now operated with smart phone applications, and the privacy of the data being collected by these applications has recently come under question (Reisinger, 2016). With increasing technologically advanced sexual devices, it is important to share this privacy concern with patients.
Counseling patients on vibrator use
After taking a sexual health history and determining that a patient may benefit from the use a vibrator, recommendation of a vibrator will require discussion and education. Women who feel positive about vibrator use may in turn experience greater benefit from vibrator use. Conversely, those who feel negatively about vibrator use may not be good candidates for vibrator treatment (Herbenick et al., 2011).
When introducing vibrator use to a patient, consideration of the discomfort and embarrassment that many patients experience with what they perceive to be a “sex toy” must be taken into account. Terminology should be considered when introducing a vibrator (e.g. vibrator, sex toy, personal massager, sexual stimulation device, sexual enhancement product, bedroom toy, sexual health device, marital device and medical device), as different terms may be more or less acceptable to different patients. For example, clinical experience suggests that patients with a higher level of conservative beliefs related to sexual health may be more receptive to a marital device versus a vibrator.
Patients have reported feeling more at ease when a sexual device was introduced with a combination of a playful and factual attitude. This was described in one study as a “light and straightforward” approach (Cullen et al., 2012). Factual information may be of benefit to the patient including normalizing the use of a vibrator (i.e. over half of women, and nearly half of men, have used a vibrator) (Herbenick et al., 2009; Reece et al., 2009), explaining the specific uses and empirically supporting the benefits of a vibrator for their treatment needs.
Many patients may feel uncertain about how to use a vibrator. With the exception of the safe use guidelines listed in Figure 2, there is no wrong way to use a vibrator. Patients should be encouraged to explore vibrator use all over the body, not just the genitals, and be reminded that vibrator use is for both men and women; involving a partner (Herbenick et al., 2009; Reece et al., 2009) in vibrator use may increase sexual satisfaction (Herbenick et al., 2010). Women may be concerned about introducing a vibrator to their partner, and providers may need to discuss how to approach this conversation and can even facilitate the conversation if both partners are available at the time of visit (Marcus, 2011).
A lubricant may be useful to decrease or avoid insertional pain or to enhance pleasure (Herbenick et al., 2011; Herbenick et al., 2015). Lubricants are categorized by their base (water, silicone, petroleum and natural oil) (Andelloux, 2011; Kingsberg, Kellogg, & Krychman, 2009). Petroleum- and natural oil-based lubricants can be problematic with sexual devices made of certain materials and latex condoms (Andelloux, 2011); therefore, water- and silicone-based lubricants that do not contain glycerin are generally favored for use with sexual devices, with the exception of silicone-based devices with which only water-based lubricant is generally recommended. In one study, participants using water-based lubricants reported significantly less genital discomfort (e.g. entry pain, penetration pain, burning, bleeding) compared to those using silicone-based lubricants (Herbenick etal., 2011).
Water-based lubricants are safe to use with latex and silicone sexual devices and are easy to clean (do not stain), but they tend to dry out quickly and wash away particularly quickly in the shower or bath. Silicone-based lubricants last longer, are waterproof and are more slippery than water-based lubricants (Andelloux, 2011). However, they are not recommended for use with silicone sexual devices. Although scientific evidence is lacking, silicone lubricants are thought to degrade silicone sexual devices. Silicone lubricants are also not recommended for men struggling with erectile dysfunction, as clinical experience suggests that the slipperiness of the lubricant may inhibit the friction needed for maintenance of an erection.
Finally, vibrators can be purchased from a variety of online and offline retail stores, some specific to sex and others not. Compared to offline retail stores, online purchases substantially increase the likelihood of receiving adult-content email spam (Zolnoun et al., 2008). To avoid email spam and embarrassment, most women prefer to purchase a vibrator directly from their provider (Cullen et al., 2012; Jannini, Limoncin, Ciocca, Buehler, & Krychman, 2012; Zolnoun et al., 2008); however, selling these products directly to patients could create ethical dilemmas for providers (Jannini et al., 2012). Retailers carry a wide variety of products in terms of quality and selection. Clinical experience suggests that patients appreciate the recommendation of a specific vibrator model that will fit their treatment needs and recommendations on where it can be purchased.
Conclusion
Counseling patients on vibrator use requires assistance in choosing the appropriate vibrator based on treatment needs and personal preference, as well as education regarding the safe use of a vibrator and incorporating vibrator use into a partnered sexual relationship. Additional study is needed to determine the most effective methods to counsel patients on vibrator use and evidence-based cleaning recommendations.
Footnotes
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Aaronson DS, & Shindel AW (2010). Advocating for safer use of sexual enhancement products. Journal of Sexual Medicine, 7, 2285–2287. doi: 10.1111/j.1743-6109.2010.01770.x [DOI] [PubMed] [Google Scholar]
- Andelloux M (2011). Products for sexual lubrication: Understanding and addressing options with your patients. Nursing Women’s Health, 15, 253–257. doi: 10.1111/j.1751-486X.2011.01642.x [DOI] [PubMed] [Google Scholar]
- Anderson TA, Schick V, Herbenick D, Dodge B, & Fortenberry JD (2014). A study of human papillomavirus on vaginally inserted sex toys, before and after cleaning, among women who have sex with women and men. Sexually Transmitted Infections, 90, 529–531. doi: 10.1136/sextrans-2014-051558 [DOI] [PubMed] [Google Scholar]
- Bakker RM, Vermeer WM, Creutzberg CL, Mens JW, Nout RA, & Ter Kuile MM (2015). Qualitative accounts of patients’ determinants of vaginal dilator use after pelvic radiotherapy. Journal of Sexual Medicne, 12, 764–773. doi: 10.1111/jsm.12776 [DOI] [PubMed] [Google Scholar]
- Committee on Adolescent Health Care. Committee on Gynecologic Practice. (2013). Addressing health risks of noncoital sexual activity: Committee opinion no. 582. Obstetrics & Gynecology, 122, 1378–1383. [DOI] [PubMed] [Google Scholar]
- Connell K, Guess MK, Bleustein CB, Powers K, Lazarou G, Mikhail M, & Melman A (2005). Effects of age, menopause, and comorbidities on neurological function of the female genitalia. International Journal of Impotence Research, 17, 63–70. doi: 10.1038/sj.ijir.3901230 [DOI] [PubMed] [Google Scholar]
- Cullen K, Fergus K, Dasgupta T, Fitch M, Doyle C, & Adams L (2012). From “sex toy” to intrusive imposition: A qualitative examination of women’s experiences with vaginal dilator use following treatment for gynecological cancer. Journal of Sexual Medicine, 9, 1162–1173. doi: 10.1111/j.1743-6109.2011.02639.x [DOI] [PubMed] [Google Scholar]
- Dhar R, & Nunns D (2009). Vulvodynia management. Obstetrics, Gynaecology and Reproductive Medicine, 19, 175–177. [Google Scholar]
- Donaldson JF, Tait C, Rad M, Walker S, Lam TB, Abdel-Fattah M, & Swami SK (2014). Obstructive uropathy and vesicovaginal fistula secondary to a retained sex toy in the vagina. Journal of Sexual Medicine, 11(10), 2595–2600. doi: 10.1111/jsm.12575 [DOI] [PubMed] [Google Scholar]
- Graham CA (2014). Orgasm disorders in women In Binik YM & Hall KSK (Eds.), Princples and practice of sex therapy (5th ed., pp. 89–111). New York, NY: The Guilford Press. [Google Scholar]
- Griffin R, & McGwin GJ (2009). Sexual stimulation device-related injuries. Journal of Sex and Marital Therapy, 35, 253–261. doi: 10.1080/00926230902851249 [DOI] [PubMed] [Google Scholar]
- Guess MK, Connell K, Schrader S, Reutman S, Wang A, LaCombe J, … Mikhail M (2006). Genital sensation and sexual function in women bicyclists and runners: Are your feet safer than your seat ? Journal of Sexual Medicine, 3, 1018–1027. doi: 10.1111/j.1743-6109.2006.00317.x [DOI] [PubMed] [Google Scholar]
- Herbenick D (2009). How to clean sex toys. How to have sex. May 15, 2009; Retrieved from http://mysexprofessor.com/how-to-have-sex/how-to-clean-sex-toys/ [Google Scholar]
- Herbenick D (2010). Female masturbation. Female Patient, 12, 46–49. [Google Scholar]
- Herbenick D, Barnhart KJ, Beavers K, & Benge S (2015). Vibrators and other sex toys are commonly recommended to patients, but does size matter? Dimensions of commonly sold products. Journal of Sexual Medicine, 12, 641–645. doi: 10.1111/jsm.12798 [DOI] [PubMed] [Google Scholar]
- Herbenick D, Reece M, Hensel D, Sanders S, Jozkowski K, & Fortenberry JD (2011). Association of lubricant use with women’s sexual pleasure, sexual satisfaction, and genital symptoms: A prospective daily diary study. Journal of Sexual Medicine, 8, 202–212. doi: 10.1111/j.1743-6109.2010.02067.x [DOI] [PubMed] [Google Scholar]
- Herbenick D, Reece M, Sanders S, Dodge B, Ghassemi A, & Fortenberry JD (2009). Prevalence and characteristics of vibrator use by women in the United States: Results from a nationally representative study. Journal of Sexual Medicine, 6, 1857–1866. doi: 10.1111/j.1743-6109.2009.01318.x [DOI] [PubMed] [Google Scholar]
- Herbenick D, Reece M, Sanders SA, Dodge B, Ghassemi A, & Fortenberry JD (2010). Women’s vibrator use in sexual partnerships: Results from a nationally representative survey in the United States. Journal of Sex and Marital Therapy, 36, 49–65. doi: 10.1080/00926230903375677 [DOI] [PubMed] [Google Scholar]
- Herbenick D, Reece M, Schick V, Jozkowski KN, Middelstadt SE, Sanders SA, … Fortenberry JD (2011). Beliefs about women’s vibrator use: Results from a nationally representative probability survey in the United States. Journal of Sex and Marital Therapy, 37(5), 329–345. doi: 10.1080/0092623X.2011.606745 [DOI] [PubMed] [Google Scholar]
- Jannini EA, Limoncin E, Ciocca G, Buehler S, & Krychman M (2012). Ethical aspects of sexual medicine. Internet, vibrators, and other sex aids: Toys or therapeutic instruments ? Journal of Sexual Medicine, 9, 2994–3001. doi: 10.1111/jsm.12018 [DOI] [PubMed] [Google Scholar]
- Kingsberg SA, Kellogg S, & Krychman M (2009). Treating dyspareunia caused by vaginal atrophy: A review of treatment options using vaginal estrogen therapy. International Journal of Women’s Health, 1, 105–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwakwa HA, & Ghobrial MW (2003). Female-to-female transmission of human immunodeficiency virus. Clinical Infectious Diseases, 36, e40–e41. doi: 10.1086/345462 [DOI] [PubMed] [Google Scholar]
- Malhotra S, Khurshid A, Hendricks KA, & Mann JR (2008). Medical school sexual health curriculum and training in the United States. Journal of the National Medical Association, 100, 1097–1106. [DOI] [PubMed] [Google Scholar]
- Marcus BS (2011). Changes in a woman’s sexual experience and expectations following the introduction of electric vibrator assistance. Journal of Sexual Medicine, 8, 3398–3406. doi: 10.1111/j.1743-6109.2010.02132.x [DOI] [PubMed] [Google Scholar]
- Marrazzo JM, Thomas KK, Agnew K, & Ringwood K (2010). Prevalence and risks for bacterial vaginosis in women who have sex with women. Sexually Transmitted Diseases, 37, 335–339. [PMC free article] [PubMed] [Google Scholar]
- Nilsson NH, Malmgren-Hansen B, Bernth N, Pedersen E, & Pommer K (2006). Survey and health assesment of chemicals substances in sex toys. Copenhagen: The Danish Environmental Protection Agency; Retrieved from http://www2.mst.dk/udgiv/publications/2006/87-7052-227-8/pdf/87-7052-228-6.pdf [Google Scholar]
- Prause N, Roberts V, Legarretta M, & Rigney Cox LM (2012). Clinical and research concerns with vibratory stimulation: A review and pilot study of common stimulation devices. Sexual and Relationship Therapy, 27, 17–34. doi: 10.1080/14681994.2012.660141 [DOI] [Google Scholar]
- Previnaire JG, Lecourt G, Soler JM, & Denys P (2014). Sexual disorders in men with multiple sclerosis: Evaluation and management. Annals of Physical and Rehabilitation Medicine, 57, 329–336. doi: 10.1016/j.rehab.2014.05.002 [DOI] [PubMed] [Google Scholar]
- Reece M, Herbenick D, Sanders SA, Dodge B, Ghassemi A, & Fortenberry JD (2009). Prevalence and characteristics of vibrator use by men in the United States. Journal of Sexual Medicine, 6, 1867–1874. doi: 10.1111/j.1743-6109.2009.01290.x [DOI] [PubMed] [Google Scholar]
- Reece M, Rosenberger JG, Schick V, Herbenick D, Dodge B, & Novak DS (2010). Characteristics of vibrator use by gay and bisexually identified men in the United States. Journal of Sexual Medicine, 7(10), 3467–3476. doi: 10.1111/j.1743-6109.2010.01873.x [DOI] [PubMed] [Google Scholar]
- Reisinger S (2016). “Smart” vibrator leads to cutting-edge privacy class action. Corporate Counsel. September 14, 2016; Retrieved from http://www.corpcounsel.com/id=1202767414940/Smart-Vibrator-Leads-to-CuttingEdge-Privacy-Class-Action?slreturn=20160905143251 [Google Scholar]
- Sobrero AJ, Stearns HE, & Blair JH (1965). Technic for the induction of ejaculation in humans. Fertility and Sterility, 16, 765–767. [DOI] [PubMed] [Google Scholar]
- Sonksen J, & Ohl DA (2002). Penile vibratory stimulation and electroejaculation in the treatment of ejaculatory dysfunction. International Journal of Andrology, 25, 324–332. [DOI] [PubMed] [Google Scholar]
- Stabile E (2013). Commentary: Getting the government in bed: How to regulate the sex-toy industry. Berkeley Journal of Gender, Law and Justice, 28(2), 161–184. [Google Scholar]
- Stein MJ, Lin H, & Wang R (2014). New advances in erectile technology. Therapeutic Advances in Urology, 6, 15–24. doi: 10.1177/1756287213505670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutton KS, Boyer SC, Goldfinger C, Ezer P, & Pukall CF (2012). To lube or not to lube: Experiences and perceptions of lubricant use in women with and without dyspareunia. Journal of Sexual Medicine, 9, 240–250. doi: 10.1111/j.1743-6109.2011.02543.x [DOI] [PubMed] [Google Scholar]
- Vardi Y, Gruenwald I, Sprecher E, Gertman I, & Yartnitsky D (2000). Normative values for female genital sensation. Urology, 56, 1035–1040. [DOI] [PubMed] [Google Scholar]
- Waraich NG, Hudson JS, & Iftikhar SY (2007). Vibrator-induced fatal rectal perforation. New Zealand Medical Journal, 120(1260), U2685. [PubMed] [Google Scholar]
- Zolnoun D, Lamvu G, & Steege J (2008). Patient perceptions of vulvar vibration therapy for refractory vulvar pain. Sexual and Relationship Therapy, 23, 345–353. doi: 10.1080/14681990802411685 [DOI] [PMC free article] [PubMed] [Google Scholar]


