Abstract
Objectives:
Major depressive disorder (MDD) is one of the most disabling mental illnesses and it has a significant impact on society. This review aims to provide updated scientific evidence about the epidemiology of MDD.
Methods:
A systematic literature review of the PubMed and MEDLINE databases was performed to identify articles on the prevalence of MDD and its correlates. The search was restricted to manuscripts published between January 2001 and December 2018.
Results:
Sixty-three articles were included in the review. The lifetime prevalence of MDD ranged from 2 to 21%, with the highest rates found in some European countries and the lowest in some Asian countries. The main sociodemographic correlates were separated/divorced marital status and female gender. Child abuse, intimate partner violence, and comorbidity with other physical and mental disorders also were consistently associated with MDD across the reviewed studies.
Conclusions:
MDD is a highly prevalent condition worldwide. There are remarkable interregional differences in the disorder’s prevalence, as well as in certain sociodemographic correlates. MDD is also highly comorbid with physical and mental health problems.
Keywords: Major depressive disorder, prevalence, comorbidity, epidemiology, chronic physical conditions
Introduction
Major depressive disorder (MDD) is one of the most prevalent mental disorders worldwide, as well as one of the most disabling. According to the Global Burden of Disease study, depression is the fourth leading cause of disability (measured in disability adjusted life years), and it is expected to be the second by 2020.1 MDD has a greater impact on public health than physical conditions such as coronary heart disease, rheumatoid arthritis, or diabetes mellitus.2 Its economic impact is also considerable.3-5 Information on the prevalence and correlates of MDD is key to its prevention and management.
Since the 1980s, a number of population surveys have explored the prevalence of mental disorders. Some of the first large-scale studies were the Epidemiologic Catchment Area (1980-1985)6 and the National Comorbidity Survey (1990-1992),7 both conducted in the United States. It took several years before such studies were conducted in developing countries. Although a number of surveys have been carried out in recent years, their methodological differences make it difficult to obtain comparable results, even within the same country. This issue has been addressed by the World Health Organization through the World Mental Health project, a series of population surveys of identical methodology conducted as a coordinated effort in several countries.8 Nevertheless, some authors are questioning whether it is valid to apply the same methodology to Western and non-Western settings.9
It is assumed that the etiopathogenesis of MDD is the result of a complex interaction between biological and psychosocial factors and, although many studies have explored them over the years, they are far from being entirely elucidated. This systematic review offers a synthesis of current evidence about the epidemiology of MDD, exploring its prevalence, sociodemographic correlates, and potential risk factors in countries worldwide.
Methods
This review is divided into two parts, each with different inclusion/exclusion criteria and search strategies. The first part involves articles about MDD prevalence and sociodemographic factors, while the second involves articles about potential risk factors in the areas of traumatic experiences, physical health, and mental health. Applicable Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines were complied with.10 This protocol has not been registered.
Inclusion/exclusion criteria
Cross-sectional articles on MDD prevalence in the adult community-based population were included in the first part of the review. MDD was diagnosed according to ICD-10,11 DSM-IV,12 or DSM-513 criteria using valid scales and face-to-face interviews. The minimum sample size was set at 1,000 participants to increase the quality of the studies. We excluded all studies conducted among special populations (specific professions or groups of patients), those that used telephone interviews, those based on depressive symptoms rather than a complete diagnosis, and those that made no distinction between MDD and other affective disorders.
The second part included articles on the relationship between MDD and relevant risk factors, which were selected according to previous evidence14-16: child abuse, stressful life events, gender violence, chronic illness, mental illness, personality traits, and toxic substance exposure. Both cross-sectional and longitudinal studies were accepted. In addition to the above-mentioned diagnostic criteria, DSM-III criteria were also accepted for this part of the review to allow inclusion of prospective studies begun prior to the creation of the DSM-IV. All studies that included self-reported cases of MDD, those based on symptoms rather than a diagnosis, and those that did not distinguish between MDD and other affective disorders were excluded. Given that this type of study has smaller samples than observational studies, the sample size was reduced to a minimum of 100 participants.
Search strategy
For both parts, a search was performed in the PubMed and MEDLINE databases. Additional articles were retrieved from ResearchGate by inspecting the reference list of reviewed articles and consulting experts in the field. The search terms for articles about prevalence and sociodemographic factors were: (MDD[Title/Abstract]) AND prevalence[Title/Abstract]). The search was restricted to articles published in English or Spanish. Manuscripts in press were included if access was granted. For both parts, the publication date was limited to the 21st century (2001-2018) for more current results.
The MEDLINE search terms for the articles about risk factors were: MDD[Title/Abstract] AND (risk factors[Title/Abstract] OR personality[Title/Abstract] OR obesity[Title/Abstract] OR correlates[Title/Abstract] OR comorbidity[Title/Abstract] OR alcohol[Title/Abstract] OR smoking[Title/Abstract] OR abuse[Title/Abstract] OR violence[Title/Abstract] OR chronic conditions[Title/Abstract]). A similar search format was used in the PubMed database. The articles were selected according to their relevance and quality. We used critical appraisal checklists to assess quality.17
Two researchers (AP-S and HD) independently assessed the articles for inclusion. Agreement between reviewers, measured by intraclass correlation coefficient (ICC), was 0.81 (95% confidence interval [95%CI] 0.76-0.86). Differences between reviewers were resolved by discussion. Data extraction was performed by the same two researchers, using a purpose-built form. Data was collected on MDD prevalence and its association with independent variables, including effect sizes, which were expressed as odds ratio (OR) or hazard ratio (HR).
Results
Study selection
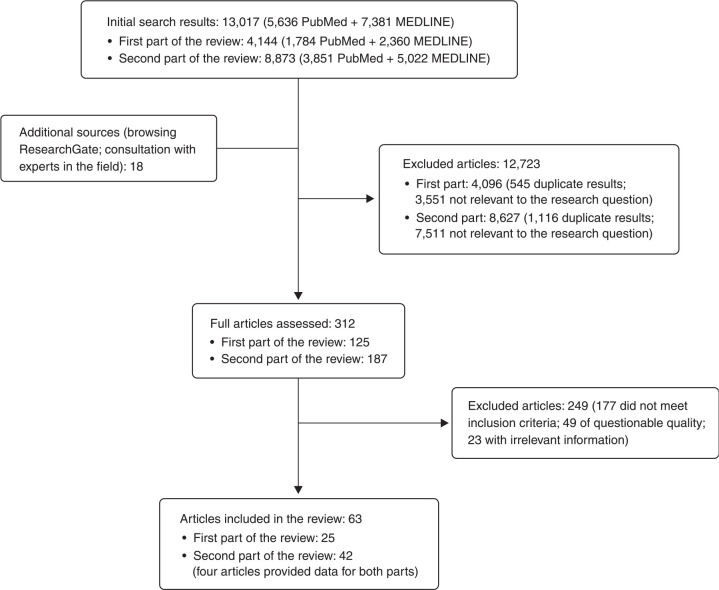
The initial search yielded 4,144 results for the first part of the review and 8,873 results for the second part, totaling 13,017 results. Following the initial screening, full-text revision and selection process, 63 articles were included in the final review. Twenty-five provided information about the prevalence and sociodemographic correlates of MDD (first part), while 42 assessed correlates of MDD related to physical health, mental health, and traumatic experiences (second part of the review). Since four of the 63 articles provided information for both parts of the review, they were counted twice (Figure 1).
Figure 1. Flow diagram of the bibliographic search.
Study characteristics
The 25 articles focusing on the prevalence and sociodemographic factors of MDD included data from 38 population-based surveys conducted in 29 countries. These studies were based on similar methodologies and had a cross-sectional design, allowing effective comparison between results. The majority included data about both the prevalence of MDD and the principal sociodemographic factors linked with the disorder. A total of 42 articles explored MDD risk factors. These articles were more heterogeneous, due to the variety of study designs (cross-sectional, retrospective and prospective). Recall bias, the limitations of the diagnostic tools, and study design were the most frequently reported limitations in the selected studies. We divided the results into five topics: MDD prevalence (25 articles), sociodemographic factors (17 articles), associations with traumatic experiences (14 articles), risk factors related to physical health (18 articles), and associations with mental health (19 articles).
Prevalence of MDD
Lifetime prevalence of MDD ranged from 2% in China,18 6.7% in South Korea,19 20.5% in Chile,20 to 21% in France.21 The 12-month prevalence ranged between 1.1% in China18 and 10.4% in Brazil.21 By continent, the highest prevalence was in Europe21,22 and the lowest in Asia.18,19,21-23 In European countries, average lifetime prevalence was 11.32% and average 12-month prevalence 5.2%.21,24-28 The full results are shown in Table 1.
Table 1. Prevalence of MDD, sample size, age of participants, data collection period, and type of measure by country.
| Study | Country | Age range (years) | Median age (years) | Data collection | n | Scales/criteria of MDD | Life prevalence (%) | 12-month prevalence (%) | Cross-sectional prevalence (%) |
|---|---|---|---|---|---|---|---|---|---|
| Assari29 | United States | ≥ 18 | 41.73 | 2001-2003 | 1,271 | CIDI/DSM-IV | - | 4.71±0.6 | - |
| Bromet21 | Belgium | ≥ 18 | 29.4 | 2001-2002 | 2,419 | CIDI/DSM-IV | 14.1±1.0 | 5.0±0.5 | - |
| France | ≥ 18 | 24.3 | 2001-2002 | 2,894 | CIDI/DSM-IV | 21.0±1.1 | 5.9±0.6 | - | |
| Germany | ≥ 18 | 18.8 | 2002-2003 | 3,555 | CIDI/DSM-IV | 9.9±0.6 | 3.0±0.3 | - | |
| Israel | ≥ 21 | 23.5 | 2002-2004 | 4,859 | CIDI/DSM-IV | 10.2±0.5 | 6.1±0.4 | - | |
| Italy | ≥ 18 | 28.4 | 2001-2003 | 4,712 | CIDI/DSM-IV | 9.9±0.5 | 3.0±0.2 | - | |
| Japan | ≥ 20 | 27.6 | 2002-2006 | 3,416 | CIDI/DSM-IV | 6.6±0.5 | 2.2±0.4 | - | |
| Netherlands | ≥ 18 | 31.9 | 2002-2003 | 2,372 | CIDI/DSM-IV | 17.9±1.0 | 4.9±0.5 | - | |
| Spain | ≥ 18 | 25.5 | 2001-2002 | 5,473 | CIDI/DSM-IV | 10.6±0.6 | 4.0±0.3 | - | |
| New Zealand | ≥ 18 | 27.7 | 2004-2005 | 12,790 | CIDI/DSM-IV | 17.8±0.4 | 6.6±0.3 | - | |
| Brazil | ≥ 18 | 30.1 | 2004-2007 | 5,037 | CIDI/DSM-IV | 18.4±0.8 | 10.4±0.6 | - | |
| Colombia | 18-65 | 23.8 | 2003 | 4,426 | CIDI/DSM-IV | 13.3±0.6 | 6.2±0.4 | - | |
| India | ≥ 18 | 23.5 | 2003-2005 | 2,992 | CIDI/DSM-IV | 9.0±0.5 | 4.5±0.4 | - | |
| Lebanon | ≥ 18 | 27.2 | 2002-2003 | 2,857 | CIDI/DSM-IV | 10.9±0.9 | 5.5±0.7 | - | |
| Mexico | 18-65 | 24.2 | 2001-2002 | 5,782 | CIDI/DSM-IV | 8.0±0.5 | 4.0±0.3 | - | |
| South Africa | ≥ 18 | 22.3 | 2003-2004 | 4,315 | CIDI/DSM-IV | 9.8±0.7 | 4.9±0.4 | - | |
| Ukraine | ≥ 18 | 30 | 2002 | 4,724 | CIDI/DSM-IV | 14.6±0.7 | 8.4±0.6 | - | |
| China | ≥ 18 | 27.8 | 2006-2007 | 7,132 | CIDI/DSM-IV | 6.5±0.4 | 3.8±0.3 | - | |
| Bunting24 | United Kingdom | ≥ 18 | - | 2004-2008 | 4,340 | CIDI/DSM-IV | - | 7.9±1.6 | - |
| Chen30 | China | 30-79 | - | 2004-2008 | 512,891 | CIDI/DSM-IV | - | 0.7 | - |
| Cho19 | South Korea | 18-74 | 29.2 | 2011 | 6,022 | CIDI/DSM-IV | 6.7±1.2 | 3.1±0.8 | - |
| Goldney22 | Australia | ≥ 15 | 30.4 | 2008 | 3,014 | PRIME-MD/DSM-IV | 10.3±1.1 | - | - |
| de Graaf25 | Netherlands | 18-64 | 22.7 | 2007-2009 | 6,646 | CIDI/DSM-IV | 18.7±1.2 | 5.2±0.6 | - |
| Gureje31 | Nigeria | ≥ 18 | - | 2002-2003 | 6,752 | CIDI/DSM-IV | 3.1±0.6 | 1.1±0.2 | - |
| Hasin32 | United States | ≥ 18 | - | 2000-2001 | 43,093 | AUDADIS-IV/DSM-IV | 13.2±0.6 | 5.3±0.3 | - |
| Jacobi26 | Germany | 18-79 | - | 2009-2012 | 5,318 | CIDI/DSM-IV | - | 6.0±0.8 | - |
| Kessler33 | United States | ≥ 18 | - | 2001-2002 | 9,090 | CIDI/DSM-IV | 16.2±1.1 | 6.6±0.7 | - |
| Kiejna27 | Poland | 18-64 | - | 2010-2011 | 10,081 | CIDI/DSM-IV | 3.0±0.3 | - | - |
| Kleinberg34 | Estonia | 18-84 | - | 2006-2008 | 6,105 | MINI/DSM-IV | - | - | 5.6±0.6 |
| Klijs35 | Netherlands | ≥ 18 | 43.7 | 2006-2012 | 71,058 | MINI /DSM-IV | - | - | 2.5 |
| Liu23 | China | ≥ 18 | - | 2010 | 16,032 | SCID/DSM-IV | 3.6±0.3 | - | 1.1±0.2 |
| Lu18 | China | ≥ 15 | - | 2005-2006 | 5,033 | CIDI/DSM-IV | 2.0±0.5 | 1.09±0.3 | 0.9±0.3 |
| Markkula28 | Finland | ≥ 30 | - | 2011 | 6,005 | CIDI/DSM-IV | - | 7.4±1.7 | - |
| Markkula20 | Chile | ≥ 17 | - | 20032010 | 5,4697,212 | CIDI-SF/DSM-IV | 20.5 ±2.218.4± 1.8 | - | - |
| Mohammadi36 | Iran | ≥ 18 | - | 2001 | 25,180 | SPI/DSM-IV | 3.0 | - | - |
| Munhoz37 | Brazil | ≥ 20 | - | 2006-2010 | 2,925 | PHQ-9/DSM-IV | 20.4 | - | - |
| Piazza & Fiestas38 | Peru | 18-65 | - | 2004-2005 | 3,930 | CIDI/DSM-IV | - | 2.7±0.4 | - |
| Porras-Segovia39 | Spain | 18-80 | 42.8 | 2011-2012 | 810 | MINI /DSM-IV | - | - | 5.6±0.7 |
| Slone40 | Mexico | ≥ 18 | - | 1999-2001 | 2,509 | CIDI/DSM-IV | 12.8±1.4 | 6.1±1.0 | - |
| Smith41 | United Kingdom | - | 54.5 | 2006-2010 | 172,751 | CIDI/DSM-IV | 6.4 | - | - |
| Topuzoglu42 | Turkey | 15-64 | - | 2007-2008 | 4,011 | CIDI/DSM-IV | - | 8.2±0.9 | - |
- = no data provided; AUDADIS-IV = Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV; CIDI = Composite International Diagnostic Interview; CIDI-SF = Composite International Diagnostic Interview-Short Form; MDD = major depressive disorder; MINI = Mini International Neuropsychiatric Interview; PHQ-9 = Patient Health Questionnaire-9; PRIME-MD = Primary Care Evaluation of Mental Disorders; SCID = Structured Clinical Interview for DSM Disorders; SPI = Standard Psychiatric Interview.
Sociodemographic factors
Among the sociodemographic factors linked to MDD, two stand out: female sex and being separated/divorced. Female sex was significantly associated with MDD in 26 of the 30 studies exploring this factor. A non-significant result was found in surveys undertaken in Belgium and Nigeria, as well as in two of the three surveys from China. Even when the results were not significant, depression rates were higher in women than men. OR values ranged from 1.4 in Australia22 to 2.8 in Iran.36 When controlling for other factors, the association between MDD and female sex prevailed in most studies21 and disappeared in a minority of them.39 The association between separation/divorce and MDD was statistically significant in 26 of the 29 population surveys that included this data. Compared to married people, the OR reached 8.2 in India21 and 19.3 in Lebanon, although the study’s wide CI (5.0-74.4) makes the real effect size uncertain.21
Employment status was also consistently linked with MDD: unemployment was positively associated with depression in the eight studies in which this data was collected. Other sociodemographic factors, such as socioeconomic status (SES) or education level, were only associated with MDD in some of the articles. A study conducted in the Netherlands with 71,058 community-dwelling adults showed that increased income, both on a neighborhood and an individual level, were significantly associated with a lower prevalence of MDD. However, high SES was associated with a higher prevalence of MDD among African-American men in another study.29
SES is also a potential confounding factor, since it has been associated with other potential correlates of MDD, including poorer physical health and greater drug use. Some studies that adjusted for this potential confounder found that variables such as obesity or a chronic physical condition retained their significance after adjustment.35,43 However, Chen et al.44 found that smoking was a risk factor for MDD only in African-American participants, who presented a significantly lower mean income than their Caucasian counterparts. Some of these factors showed contradictory results depending on the study: although a low education level was associated with MDD in India, Mexico, and Australia, in China and the United States it appeared to be a protective factor. The full results can be seen in Table 2.
Table 2. Correlates of major depressive disorder: gender, marital status, unemployment, SES, and education.
| Marital status | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Study | Country | Female | Separated | Divorced | Widowed | Single | Unemployed | SES | Education |
| Assari29 | United States | - | Married vs. other: 0.33 (0.12-0.91) | 1.61 (0.64-4.06) | 1.10 (1.00-1.20) | 12 years or more: 0.59 (0.28-1.23) | |||
| Bromet21 | Belgium | NS | 7.3 (1.8-29.7) | NS | NS | NS | - | NS | - |
| Brazil | 2.6 (1.9-3.5) | 1.6 (1.1-2.3) | 3.0 (1.9-4.9) | NS | NS | - | NS | - | |
| China | NS | 6.2* | NS | NS | - | Low vs. high: NSMedium-low vs. high: NS Medium-high vs. high: 0.5 (0.3-0.8) | - | ||
| Colombia | 1.9 (1.4-2.7) | NS | NS | NS | NS | - | NS | - | |
| France | 1.7 (1.2-2.5) | 6.2 (1.8-21.3) | NS | NS | 2.0 (1.2-3.5) | - | Low vs. high: 2.4 (1.2-4.6) | - | |
| Germany | 1.7 (1.0-3.0) | 3.1 (1.4-7.1)* | 2.3 (1.2-4.5) | 2.6 (1.6-4.2) | - | Low vs. high: 2.7 (1.3-5.6) | - | ||
| India | 1.9 (1.3-2.7) | 8.2 (2.2-30.6)* | 2.2 (1.5-3.2) | 0.3 (0.1-0.6) | - | Low vs. high: NSMedium-low vs. high: 2.1 (1.2-3.8)Medium-high vs. high: 2.0 (1.2-3.5) | - | ||
| Israel | 1.6 (1.2-2.1) | NS | 2.2 (1.5-3.4) | 2.1 (1.4-3.3) | NS | - | NS | - | |
| Italy | 2.5 (1.6-3.8) | 2.8 | NS | NS | NS | - | NS | - | |
| Japan | 2.3 (1.4-4.0) | 10.8 (2.1-55.6) | 5.1 (2.1-12.6) | NS | 3.1 (1.6-5.7) | - | NS | - | |
| Lebanon | 2.1 (1.3-3.4) | 19.3 (5.0-74.4) | NS | NS | NS | - | NS | - | |
| Mexico | 2.1 (1.5-2.9) | 1.9 (1.0-3.6) | NS | 2.7 (1.5-5.0) | NS | - | Low vs. high 2.1 (1.4-3.2) | - | |
| Netherlands | 2.3 (1.5-3.5) | 2.7* | NS | NS | - | NS | - | ||
| New Zealand | 1.7 (1.4-2.1) | 3.4 (2.4-4.8) | 2.8 (2.0-3.8) | NS | 2.3 (1.8-3.0) | - | Low vs. high: 2.2 (1.6-3.0)Medium-low vs. high: 1.5 (1.2-2.0) | - | |
| South Africa | 2.2 (1.5-3.2) | NS | 2.1 (1.3-3.5) | 2.3 (1.3-4.0) | 0.7 (0.5-1.0) | - | NS | - | |
| Spain | 2.7 (1.9-3.8) | 3.2 (1.3-7.7) | 3.3 (1.2-8.9) | NS | NS | - | NS | - | |
| Ukraine | 2.5 (2.0-3.0) | 6.6 (1.1-38.0) | 4.2 (2.9-6.2) | 8.0 (5.3-12.0) | NS | - | NS | - | |
| Chen44 | Taiwan | - | 2.87 (1.84-4.48)† | 3.34 (1.71-6.52) | - | Low vs. high: 2.18 (1.49-3.18) | Lowest education: 2.70 (1.51-4.83) | ||
| Chen30 | China | 1.6 (1.5-1.7) | - | - | - | - | - | - | - |
| Goldney22 | Australia | 1.4 (1.2-1.7) | 1.7 (1.4-2.0)‡ | 1.9 (1.5-2.2) | - | - | |||
| Gureje31 | Nigeria | NS | NS | - | - | - | - | NS | - |
| Hasin32 | United States | 2.0 (1.8-2.4) | 2.2 (1.9-2.6)‡ | - | Lowest vs. highest: OR: 1.7 | - | |||
| Kessler33 | United States | 1.7 (1.5-2.0) | 1.5 (1.2-1.8)† | 1.2 (1.0-1.4) | 1.5 (1.1-2.0) | NS | - | ||
| Kleinberg34 | Estonia | 1.8 (1.4-2.3) | 1.6 (1.1-2.2)* | 1.8 (1.3-2.4) | 1.5 (1.0-2.3) | 5.2 (2.8-9.4) | Lowest vs. highest: OR: 4.5 | - | |
| Klijs35 | Netherlands | 1.62 (1.46-1.79) | 1.9 (1.7-2.1)‡ | - | Individual income: 0.6 (0.6-0.7)Neighborhood income: 0.6 (0.6-0.7) | Lowest education: 6.0 (4.8-7.5) | |||
| Liu23 | China | 2.1 (1.5-2.8) | 2.3 (1.6- 3.4)† | 0.5 (0.2-0.9) | 3.7 (2.4-5.8) | Average vs. lowest: 0.3Highest vs. lowest: NS | - | ||
| Lu18 | China | NS | 1.6 (1.1- 4.2)† | NS | 2.4 (1.4-4.0) | - | - | ||
| Markkula28 | Finland | 2.3 (1.6-3.4) | 1.5 (1.2- 2.0)‡ | - | - | ||||
| Munhoz37 | Brazil | 2.4 (2.0-2.9) | 1.5 (1.1-1.9)† | 1.5 (1.2-2.0) | 1.2 (1.0-1.4) | - | - | ||
| Porras-Segovia39 | Spain | 1.9 (1.4-2.6) | - | - | - | - | |||
| Slone40 | Mexico | 1.8 (1.4-2.4) | 1.5 (1.0-2.1)‡ | - | - | - | |||
| Topuzoglu42 | Turkey | 2.7 (2.1-3.5) | NS | - | - | - | 2.7 (1.6-4.3) | NS | - |
Data presented as OR (95% confidence interval).
NS = non-significant; OR = odds ratio; SES = socioeconomic status.
Separated and divorced are included in the same group.
Separated, divorced, and widowed are included in the same group.
Separated, divorced, widowed, and single are included in the same group.
Mental health-related correlates of major depressive disorder
Importantly, MDD is also related to other mental illnesses. Its association with anxiety disorders, especially general anxiety disorder, is particularly strong. In two prospective studies, general anxiety disorder was also shown to be a consistent risk factor, doubling the probability of developing MDD,45,46 while an OR >8 was found between general anxiety disorder and MDD in a cross-sectional study.32 However, other studies found no significant association between the two conditions,47 while others found a strong association with different classes of phobia.48
The association between personality disorders and MDD was inconsistent and depended on the type of disorder. Although borderline and paranoid personality disorders were significantly associated with MDD in all of the studies that assessed them, other disorders, such as histrionic or evasive personality disorders, were associated with MDD in some but not all studies.32,49,50 Although one prospective study found no significant association between personality traits and MDD,8 in three other studies neuroticism was found to be a risk factor, while extroversion was a protective factor.51-53
Five studies found that tobacco use appeared to be related to MDD.44,52-55 Although some studies found an association between alcohol consumption and MDD,56 a large proportion of the studies did not.44,46,47,57 At low or moderate doses, alcohol consumption was even shown to be a protective factor.54,57
The most commonly studied risk factor was child abuse in its different forms (physical, psychological, and sexual), and nine studies found a significant association between it and MDD, although only certain subtypes of abuse were significant in some studies. In a Chinese retrospective study with 12,000 participants, those who claimed to have suffered childhood sexual abuse had a considerably higher prevalence of MDD, with an OR of 4.1.58 A prospective study followed U.S. children, beginning at the age of 11, for 28 years, finding that those who had suffered physical abuse had an OR of 1.6 for MDD compared to those who had not.59 This association may be mediated by genetic factors.60
No relevant association between traumatic experiences and MDD was found in the few studies that explored the relationship.61 Nevertheless, in one study, a significant synergistic effect was found with child abuse: the strength of the association increased from an OR of 5.1, when only child abuse was present, to an OR of 12.4 when both child abuse and traumatic life experiences during adulthood were present.62 Other studies found that intimate partner violence63,64 or traumatic experiences30 increased the risk of MDD. Gender-based violence was also consistently associated with MDD. A prospective study in the UK followed 1,000 women over 10 years, and those who claimed to have suffered gender-based violence had twice the risk of developing MDD.65 The full results can be found in Tables 3 and 4.
Table 3. Correlates of major depressive disorder: child abuse, intimate partner violence, and traumatic experiences.
| Study | Country | Design | n | Child abuse | IPV | TE |
|---|---|---|---|---|---|---|
| Bonomi63 | United States | Cross-sectional | 1,928 | - | 3.7 (2.6-4.1) | - |
| Chen58 | China | Retrospective | 12,000 | Sexual: 4.1 (3.2-5.2) | - | - |
| Chen30 | China | Cross-sectional | 512,891 | - | - | 14.7 (13.7-15.7) |
| Deyessa64 | Ethiopia | Cross-sectional | 1,994 | Sexual: 2.0 (1.1-3.6) | Physical: 2.6 (1.6-4.1); Emotional: 3.9 (2.2-6.9) | - |
| Gutiérrez60 | Spain | Prospective | 2,679 | Physical: 2.5 (1.9-3.3); Emotional: 2.1 (1.7-2.7); Sexual: 1.8 (1.1-3.0) | - | - |
| Kessler45 | United States | Prospective | 5,001 | Physical: 2.2 (1.8-2.7); Sexual: 1.8 (1.3-2.5) | - | - |
| Klijs35 | Netherlands | Cross-sectional | 71,058 | - | - | 1.18 (1.15-1.22) |
| Kounou49 | Togo | Retrospective | 181 | Physical: NS; Emotional: 3.7 (1.5-9.4); Sexual: 2.2 (1.0-4.8) | - | - |
| Ouellet-Morin65 | United Kingdom | Prospective | 978 | 1.9 (1.4-2.6) | 1.7 (1.1-2.8) | - |
| Power62 | United Kingdom | Retrospective | 455 | 5.1 (2.6-9.9); SLE: 12.4 (6.5-23.6) | - | NS |
| Schulz66 | Germany | Cross-sectional | 2,046 | Physical: 1.1 (1.1-1.2); Emotional: 1.1 (1.1-1.2); Sexual: 1.1 (1.1-1.2) | - | - |
| Spinhoven67 | Netherlands | Retrospective | 2,981 | Physical: 1.6; Emotional: 1.9;Sexual: 1.5 | - | - |
| Stegenga61 | United Kingdom | Prospective | 6,910 | - | - | 1: 2.4 (1.6-3.6); ≥ 2: 4.0 (2.8-5.9) |
| Widom59 | United States | Prospective | 1,196 | Physical: 1.6 (1.0-2.5); Sexual: NS;Multiple: 1.8 (1.0-3.0) | - | - |
Data presented as odds ratio/hazard ratio (95% confidence interval).
IPV = intimate partner violence; NS = non-significant; SLE = stressful life events; TE = traumatic experiences.
Table 4. Correlates of major depressive disorder: mental comorbidities and drug use.
| Study | Country | Design | n | Results |
|---|---|---|---|---|
| Assari51 | United States | Prospective | 1,219 | Neuroticism: 2.23 (1.14-4.34); smoking: NS; drinking: NS |
| Barkow47 | Multiple | Prospective | 729 | Dysthymia: 1.7 (1.0-2.9); GAD: NS; panic disorder: NS; agoraphobia: 2.7 (1.5-4.7); alcohol dependence: 2.0 (1.1-3.7) |
| Bellos57 | Multiple | Prospective | 5,438 | Occasional alcohol use: NS; light: 0.7 (0.5-0.9); moderate: 0.5 (0.4-0.8); high: NS; very high: 1.7 (1.05-2.67) |
| Chen44 | United States | Cross-sectional | 2,590 | Second-hand smoking: 2.97 (1.2-7.7)Heavy alcohol drinking: 0.91 (0.52-1.57) |
| Choy48 | United States | Cross-sectional | 5,877 | Any phobia: 1.9 (1.6-2.4); claustrophobia: 1.6; hydrophobia: 1.4; aerophobia: 1.3;blood phobia: 1.4; acrophobia: 1.7; zoophobia: 1.8; astraphobia: NS |
| Fergusson56 | New Zealand | Prospective | 1,265 | Alcohol abuse: 1.9 (1.5-2.4) |
| Hasin32 | United States | Cross-sectional | 43,093 | GAD: 8.6 (7.1-10.5); panic disorder: 5.4 (4.2-7.0); social phobia: 4.1 (3.4-5.1); specific phobia: 2.5 (2.1-3.0); any personality disorder: 3.6 (3.2-4.1); avoidant: 4.2 (3.4-5.2); dependent: 4.0 (2.6-6.1); antisocial: 2.5 (2.0-3.1); histrionic: 2.8 (2.1-3.7); paranoid: 3.7 (3.1-4.4); schizoid: 3.7 (3.0-4.5); obsessive: 2.6 (3.0-3.2); alcohol misuse: 1.3 (1.1-1.7); drug abuse: 2.2 (1.7-2.9); tobacco consumption: 2.2 (2.0-2.5) |
| Jylhä52 | Finland | Cross-sectional | 581 | Neuroticism: 1.1 (1.1-1.2); extroversion: 0.9 (0.9-1.0) |
| Kendler53 | Sweden | Prospective | 20,692 | Neuroticism: 1.3 (1.3-1.4); extroversion: 1.0 (0.9-1.0) |
| Kessler33 | United States | Cross-sectional | 9,090 | GAD: 3.2 (2.3-4.3); neuroticism: NS; extroversion: NS |
| Klijs35 | Netherlands | Cross-sectional | 71,058 | Tobacco consumption: 1.8 (1.6-2.00); heavy alcohol drinking: 1.17 (1.00-1.36) |
| Kounou49 | Togo | Retrospective | 181 | Antisocial personality disorder: NS; avoidant: NS; borderline: 5.6 (1.8-18.0); histrionic: NS; narcissistic: NS; obsessive: NS; paranoid: 3.3 (1.1-9.6); schizoid: 3.7 (1.3-10.8) |
| Mathew46 | United States | Prospective | 816 | Anxiety disorder: 2.3 (1.7-3.2); tobacco consumption: NS; alcohol: NS; others drugs: NS |
| Munhoz37 | Brazil | Cross-sectional | 2,925 | Alcohol misuse: 0.82 (0.70-0.97) |
| Meng & D’Arcy54 | Canada | Prospective | 12,227 | Tobacco consumption: 1.7 (1.2-1.6); alcohol, regular use: 0.8 (0.7-0.9) |
| Ohayon & Schatzberg55 | Multiple | Cross-sectional | 18,980 | Tobacco consumption: < 20 c/d: 1.3 (1.0-1.5); ≥ 20 c/d: NS |
| Ouellet-Morin65 | United Kingdom | Prospective | 978 | Antisocial personality disorder: 2.4 (1.4-4.1); substance abuse: NS |
| Pasco68 | Australia | Retrospective | 974 | Tobacco consumption: 1.9 (1.0-3.7) |
| Reichborn-Kjennerud50 | Norway | Cross-sectional | 2,801 | Histrionic personality disorder: NS; borderline: 1.8 (1.6-2.0); paranoid: 1.1 (1.0-1.3); schizoid: NS; schizotypal: NS; avoidant: 1.1 (1.0-1.2); antisocial: NS; narcissistic: NS; dependent: NS; obsessive: NS |
Data presented as odds ratio/hazard ratio (95% confidence interval).
c/d = cigarettes/day; GAD = general anxiety disorder; NS = non-significant.
Physical health-related correlates
The majority of the reviewed studies showed a statistically significant association between physical conditions and MDD.31,54,55,69-73 Size effects typically increased with the number of chronic physical conditions suffered.54 A 16-year prospective study found that the presence of chronic illnesses increased the risk of MDD by 50%.54 In the Spanish population, a 2012 cross-sectional study of 2,121 community-dwelling adults found that MDD was significantly associated with chronic physical conditions and disability.72
With respect to specific conditions, larger effect sizes were found for back pain,55 cephalea,55,74 coronary disease,75 arthritis,71 asthma,76 diabetes,77 and stroke.75 The World Health Surveys, whose combined sample was 245,404 participants from 60 countries, showed a significant association between depression and four chronic diseases: angina, arthritis, asthma, and diabetes.78 In a 2008 study, several medical disorders, including gastric ulcer, allergic rhinitis, arthritis, thyroid disease, hypertension, and asthma, were found to be more prevalent in people with recurrent depressive disorders.79 Conversely, better health has been inversely associated with MDD, with an OR of 0.68 (0.61-0.75) in a recent study.43
Several studies also found an association between MDD and obesity.43,80-82 In a recent study of Spanish community-dwelling adults, body mass index (BMI) was directly associated with MDD prevalence after adjusting for age and sex (OR = 1.06; 95%CI 1.04-1.09; p < 0.001). In the same study, the BMI categories underweight (BMI < 18.5 kg/m2) and obese (BMI ≥ 30 kg/m2) were also associated with a higher prevalence of MDD, independently of age or gender.43
However, stratification by gender often shows a stronger association between obesity and MDD among women, and in some cases the association disappears in men.80,81 In a 20-year U.S. prospective study, the relative risk of MDD in obese women was 3.9, while no significant association was found in men.80 A 2018 study investigated whether depression was associated with higher BMI, as well as with a genetic risk score involving 73 obesity-related polymorphisms. The authors found a significant association between depression and both variables, which was stronger in women than in men.81 The association between MDD and physical health factors is presented in Table 5.
Table 5. Correlates of major depressive disorder: physical conditions and obesity.
| Study | Country | Design | n | Results |
|---|---|---|---|---|
| Anderson80 | United States | Prospective | 776 | HR for obesity in females: 3.9 (1.3-11.8); in males: NS |
| Barkow47 | Multiple | Prospective | 729 | HR for chronic pain: NS |
| Baune75 | Australia | Cross-sectional | 4,181 | OR for coronary disease: 1.6 (1.1-2.3); stroke: 2.3 (1.3-4.0) |
| Chen76 | China | Retrospective | 7,265 | HR for asthma: 1.8 (1.1-2.9) |
| Chien77 | Taiwan | Cross-sectional | 766,427 | OR for diabetes: 1.5 (1.4-1.7) |
| Currie & Wang69 | Canada | Cross-sectional | 118,533 | OR for one or more CPC: 1.3 (1.3-1.3); back pain: 6.2 (5.16-7.58) |
| Egede70 | United States | Cross-sectional | 30,801 | OR for one or more CPCs: 2.6 (2.3-2.9); one CPC: 2.2 (2.0-2.5); two CPCs: 3.9 (3.2-4.8); three or more CPCs: 6.5 (5.2-8.2) |
| Gabilondo72 | Spain | Cross-sectional | 5,473 | OR for one CPC: NS; two CPCs: NS; three or more CPCs: 4.0 (2.7-5.9); disability: (2.1-6.3); cancer: NS; chronic pain: 2.1 (1.5-3.0); respiratory diseases 2.5 (1.7-3.7); ulcer: NS; CV disease: 1.8 (1.2-2.8); diabetes: NS |
| Gureje31 | Nigeria | Cross-sectional | 6,752 | OR for ulcer: 5.2 (2.0-13.3); musculoskeletal disease: 2.6 (1.4-4.8); chronic pain: 2.5 (1.4-4.7) |
| Klijs35 | Netherlands | Cross-sectional | 71,058 | OR for one CPC: 1.9 (1.6-2.2); two or more CPCs: 2.2 (2.0-2.5); underweight: 2.0 (1.3-3.0); overweight: NS; obesity: 1.5 (1.3-1.8) |
| Kounou49 | Togo | Retrospective | 181 | HR for one or more CPCs: 2.6 (1.1-6.2) |
| Mather83 | Canada | Cross-sectional | 36,984 | OR for one or more CPCs: 1.4 (1.2-1.6) |
| Meng & D’Arcy54 | Canada | Prospective | 12,227 | HR for one or more CPCs: 1.5 (1.3-1.6) |
| Modgill74 | Canada | Retrospective | 15,254 | OR for migraine: 1.6 (1.3-1.9) |
| Ohayon & Schatzberg55 | Multiple | Cross-sectional | 18,980 | OR for one or more CPCs: 2.2 (1.8-2.8); chronic pain: 3.6 (2.9-4.4); one or more CPC + pain: 5.2 (4.0-6.8); overweight (BMI 25-27): 0.7 (0.6-0.9); obesity: NS |
| Porras-Segovia43 | Spain | Cross-sectional | 4,507 | OR for increases in BMI: 1.1 (1.1-1.1); underweight: 2.1 (1.1-4.1); overweight: NS; obesity: 2.4 (1.8-3.3) |
| Stegmann71 | Multiple | Cross-sectional | 8,796 | OR for one CPC: 1.5 (1.2-1.9); two: 2.0 (1.5-2.8); three: 3.5 (2.2-5.5); four or more CPCs: 5.6 (2.9-11.0); arthritis: 2.3 (1.8-2.8); allergic: 1.3 (1.0-1.7); CV disease: 2.2 (1.5-3.2); hypertension: NS; asthma: NS; diabetes: NS; ulcer: 2.0 (1.4-2.8) |
| Tyrrell81 | United States | Retrospective | 340,786 | OR for increases in genetically determined BMI: 1.2 (1.1-1.3) |
Data presented as OR/HR (95% confidence interval).
BMI = body mass index; CPC = chronic physical condition; CV = cardiovascular; HR = hazard ratio; NS = non-significant; OR = odds ratio.
Discussion
Most studies on the epidemiology of MDD have been conducted in Western countries, while data from developing countries is comparatively scarce. Cross-sectional studies are also more numerous than longitudinal ones, which is probably a result of the higher costs associated with the latter.84
Prevalence of major depressive disorder
The results show that MDD is a highly prevalent condition worldwide, and there is no evidence of a substantial change in the prevalence of MDD over the past few decades.6,7 Interregional differences in the prevalence of MDD are notable. The low prevalence found in Asian countries is remarkable, especially compared to the figures found in Western countries. However, it does not necessarily follow that the inhabitants of countries with a low prevalence of depression suffer less or are happier, given that Asian countries have some of the highest suicides rates in the world.85
Pérez-Sales’86 work on anthropological psychology indicated that the pathoplasticity of mental disorders was the main cause for this disparity: the same condition may have different forms of clinical expression depending on the cultural context. For instance, it is believed that somatization is more frequent in non-Western populations, since the separation between body and mind is not as culturally established. In China, where the prevalence of depression is strikingly low, neurasthenia is, in contrast, very prevalent. Neurasthenia, which is scarcely known in the West, consists of extreme fatigue, muscle aches, and unspecified somatic discomfort. It has been suggested that this condition could be analogous to depression in some Eastern countries.86
While the DSM-IV was in development, a workgroup was tasked with resolving the problems of applying Western diagnostic categories to non-Western populations. Despite the workgroup’s efforts, many authors question the intercultural validity of this and similar diagnostic classifications.86,87 We must also consider the limitations of the diagnostic tools commonly employed in research, which were originally designed for Western populations and may not be ideal in other settings, even after translation and validation.88,89 Finally, the possibility of genetic susceptibility to depression in certain populations cannot be ruled out.90 These interregional differences may result in both underestimation and/or overestimation of MDD, depending on the country.
Sociodemographic factors
Our results confirm the association between MDD and some sociodemographic factors classically associated with this and other depressive disorders. Female sex was the sociodemographic factor most consistently associated with MDD. In his review on the subject, Kessler91 states that although women have a higher risk of developing depression, there are no significant differences in the clinical course of the condition, with similar persistence and recurrence rates. A synergic effect between biological and environmental factors underlies this association.91 Some of these factors are hormonal profiles and social inequality. Additionally, the open expression of sadness in males is sometimes frowned upon, which can affect the validity of the scales.92-94 Some authors have also found gender differences in the expression of the serotonin transporter polymorphisms associated with depression,95 as well as in the cellular immunity response to stress and depression.96 It has even been suggested that there could be gender-related subtypes of depression.97
SES is another factor associated with MDD. Since 1980, a number of studies have found an inverse association between SES and psychiatric disorders, including depressive disorders.98 However, in our review, SES was not consistently associated with MDD, revealing contradictory results depending on the country. The effects of educational level were similar. For a proper assessment of these large interregional differences, we should consider that having a low salary or education level may not have the same effect on subjective well-being across cultures.99 For instance, high SES increased the risk of MDD in African-American males. Perceived discrimination has been proposed as a potential mediator for increased MDD risk in African-American men with high-SES. However, a study examining the role of this variable failed to confirm this effect.29 Finally, some factors significantly associated with MDD, such as marital status and unemployment, might have a two-way relationship with MDD.
Physical and mental comorbidities of MDD
MDD is associated with poorer physical health, including high comorbidity with chronic physical conditions and higher rates of disability. There are multiple mechanisms by which physical conditions can predispose individuals to MDD. The traumatic experience of illness and the dysfunction that comes with it can trigger a depressive episode.100 Biological factors can also be involved: modified inflammatory pathways and immune system changes have been implicated in the pathogenesis of depression,101 and depression has a pro-inflammatory effect. This could result in a two-way relationship between depression and physical condition.102
In obesity, a key element appears to be distorted body image and resultant loss of self-esteem. The association between MDD and obesity may also be explained by increased circulation of pro-inflammatory cytokines and C-reactive protein, a finding of some review articles.103,104 The association between MDD and obesity was gender-dependent, with greater effect sizes in women and, in some cases, non-significant results in men. This could be the result of different body weight standards for men and women, i.e., due to cultural influences, women tend to be more susceptible to weight stigma than men.105
Comorbidity with mental disorders is another important factor. There is a strong, often two-way, relationship between MDD and other mental conditions. Patients with MDD may develop other mental comorbidities over the course of the disorder, while MDD may also appear during the course of other conditions, such as anxiety disorders.106 Furthermore, as with physical conditions, mental illness is a traumatic experience that could trigger a depressive episode. Finally, different mental disorders can share certain pathogenic mechanisms.107,108
Personality traits can increase the risk of a depressive episode, and social interaction may also mediate this association. Positive social interaction enables the creation of strong bonds and the development of a solid support network. Furthermore, personality can influence coping strategies and the ability to overcome adversity.109
Tobacco use may also be a risk marker since people with symptoms of depression and anxiety tend to smoke more. In addition, oxidative stress induced by tobacco may contribute to the development of depression.110 On the other hand, the effectiveness of bupropion for treating both depression and nicotine addiction suggests that both pathologies could share some neurochemical characteristics.68
The relationship between alcohol and MDD is ambiguous. The causes and consequences of low to moderate alcohol consumption are radically different than those of alcohol abuse, which is not the case with other drugs. The fact that limited alcohol consumption may protect against depression can be explained by social factors. In Western countries, where alcohol is widely distributed and socially accepted, average use may imply good social adjustment to some extent.111,112
The traumatic experience most strongly associated with MDD was child abuse, which can predispose to the development of depression during adulthood in various ways. One of the best-known theories is that of learned helplessness: people who repeatedly suffer negative stimuli beyond their control may lose the ability to cope with future hardships.113 This could explain why, in our review, stressful life events were not significantly associated with depression when considered alone, but were associated with it when combined with child abuse. Thus, they may have a synergic effect, increasing the risk of depression in those who suffered abuse during childhood.
Finally, some limitations should be addressed. Since most of the included studies were cross-sectional, causal relationships could not be established. The risk factor studies had heterogeneous methodologies, which impedes comparison of the results. Additionally, in retrospective studies there may be a recall bias regarding traumatic experiences.
Conclusion
In conclusion, the present review has grouped the most important recent findings worldwide about the prevalence and correlates of MDD, offering a broad overview of the current situation. Despite the heterogeneity of the studies, we were able to reach some strong conclusions. First, MDD is a prevalent condition worldwide. Second, the fact that several correlates were consistently associated with MDD has implications for health-care planning. Third, we found relevant cross-cultural differences, which makes us question whether standard diagnostic classifications and measurement tools are appropriate for non-Western cultures.
Three main issues should be considered in future research: 1) the methodological heterogeneity of epidemiological studies; 2) the lack of studies from developing countries, especially in Africa; and 3) the cultural idiosyncrasies of each country, which affect the validity of our measurements and even the concept of depression.
Disclosure
The authors report no conflict of interest.
Acknowledgements
This study received grant support from Instituto de Salud Carlos III (ISCIII CM19/00026).
The authors wish to thank Ella Martin for translating the article into English.
References
- 1.Murray CJ, Lopez AD. Evidence-based health policy--lessons from the global burden of disease study. Science. 1996;274:740–3. doi: 10.1126/science.274.5288.740. [DOI] [PubMed] [Google Scholar]
- 2.Egede LE. Depression: greater effect on overall health than angina, arthritis, asthma or diabetes. Evid Based Ment Health. 2008;11:57. doi: 10.1136/ebmh.11.2.57. [DOI] [PubMed] [Google Scholar]
- 3.Jönsson B, Bebbington PE. What price depression? The cost of depression and the cost- effectiveness of pharmacological treatment. Br J Psychiatry. 1994;164:665–73. doi: 10.1192/bjp.164.5.665. [DOI] [PubMed] [Google Scholar]
- 4.Kessler RC. The costs of depression. Psychiatr Clin North Am. 2012;35:1–14. doi: 10.1016/j.psc.2011.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Reddy MS. Depression: the disorder and the burden. Indian J Psychol Med. 2010;32:1–2. doi: 10.4103/0253-7176.70510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bourdon KH, Rae DS, Locke BZ, Narrow WE, Regier DA. Estimating the prevalence of mental disorders in US adults from the epidemiologic catchment area survey. Public Health Rep. 1992;107:663–8. [PMC free article] [PubMed] [Google Scholar]
- 7.Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the national comorbidity survey. Arch Gen Psychiatry. 1994;51:8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- 8.Kessler RC, Üstün TB. The WHO world mental health surveys: global perspectives on the epidemiology of mental disorders. New York:: Cambridge University;; 2008. [Google Scholar]
- 9.Weich S, Araya R. International and regional variation in the prevalence of common mental disorders: do we need more surveys? Br J Psychiatry. 2004;184:289–90. doi: 10.1192/bjp.184.4.289. [DOI] [PubMed] [Google Scholar]
- 10.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8:336–41. doi: 10.1016/j.ijsu.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 11.World Health Organization (WHO) The ICD-10 classification of mental and behavioural disorders. Geneva:: WHO;; 2009. [Google Scholar]
- 12.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR) Arlington:: American Psychiatric Publishing;; 2000. [Google Scholar]
- 13.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) Arlington:: American Psychiatric Publishing;; 2013. [Google Scholar]
- 14.Cervilla J. Trastornos afectivos. In: Cervilla J, editor. Compendio de psiquiatría. Granada:: Avicam;; 2017. pp. 245–67. editor. p. [Google Scholar]
- 15.Vallejo J. Trastornos depresivos. In: Vallejo J, editor. Introducción a la psicopatología y la psiquiatría. Barcelona:: Masson;; 2006. pp. 485–512. editor. p. [Google Scholar]
- 16.Sadock BJ, Sadock VA. Mood disorders. In: Sadock BJ, Sadock VA, editors. Kaplan & Sadock's synopsis of psychiatry. Philadelphia:: Lippincott Williams & Wilkins;; 2009. pp. 527–78. p. [Google Scholar]
- 17.Cardiff University, Specialist Unit for Review Evidence . Critical appraisal checklists [Internet] 2018. [cited 2020 Mar 2] https://www. cardiff. ac. uk/specialist-unit-for-review-evidence/resources/critical-appraisal-checklists. [Google Scholar]
- 18.Lu J, Ruan Y, Huang Y, Yao J, Dang W, Gao C. Major depressive disorder in Kunming: prevalence, correlates and co-morbidity in a south-western city of China. J Affect Disord. 2008;111:221–6. doi: 10.1016/j.jad.2008.02.018. [DOI] [PubMed] [Google Scholar]
- 19.Cho MJ, Seong SJ, Park JE, Chung IW, Lee YM, Bae A, et al. Prevalence and correlates of DSM-IV mental disorders in South Korean adults: the Korean epidemiologic catchment area study 2011. Psychiatry Investig. 2015;12:164–70. doi: 10.4306/pi.2015.12.2.164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Markkula N, Zitko P, Peña S, Margozzini P, Retamal CP. Prevalence, trends, correlates and treatment of depression in Chile in 2003 to 2010. Soc Psychiatry Psychiatr Epidemiol. 2017;52:399–409. doi: 10.1007/s00127-017-1346-4. [DOI] [PubMed] [Google Scholar]
- 21.Bromet E, Andrade LH, Hwang I, Sampson NA, Alonso J, de Girolamo G, et al. Cross-national epidemiology of DSM-IV major depressive episode. BMC Med. 2011;9:90. doi: 10.1186/1741-7015-9-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Goldney RD, Eckert KA, Hawthorne G, Taylor AW. Changes in the prevalence of major depressive disorder in an Australian community sample between 1998 and 2008. Aust N Z J Psychiatry. 2010;44:901–10. doi: 10.3109/00048674.2010.490520. [DOI] [PubMed] [Google Scholar]
- 23.Liu J, Yan F, Ma X, Guo HL, Tang YL, Rakofsky JJ, et al. Prevalence of major depressive disorder and socio-demographic correlates: results of a representative household epidemiological survey in Beijing, China. J Affect Disord. 2015;129:74–81. doi: 10.1016/j.jad.2015.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bunting B, Murphy S, O’Neill S, Ferry F. Prevalence and treatment of 12-month DSM-IV disorders in the Northern Ireland study of health and stress. Soc Psychiatry Psychiatr Epidemiol. 2013;48:81–93. doi: 10.1007/s00127-012-0518-5. [DOI] [PubMed] [Google Scholar]
- 25.de Graaf R, ten Have M, van Gool C, van Dorsselaer S. Prevalence of mental disorders and trends from 1996 to 2009. Results from the Netherlands mental health survey and incidence study-2. Soc Psychiatry Psychiatr Epidemiol. 2012;47:203–13. doi: 10.1007/s00127-010-0334-8. [DOI] [PubMed] [Google Scholar]
- 26.Jacobi F, Höfler M, Siegert J, Mack S, Gerschler A, Scholl L, et al. Twelve-month prevalence, comorbidity and correlates of mental disorders in Germany: the mental health module of the German health interview and examination survey for adults (DEGS1-MH) Int J Methods Psychiatr Res. 2014;23:304–19. doi: 10.1002/mpr.1439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kiejna A, Piotrowski P, Adamowski T, Moskalewicz J, Wciórka J, Stokwiszewski J, et al. The prevalence of common mental disorders in the population of adult Poles by sex and age structure – an EZOP Poland study. Psychiatr Pol. 2015;49:15–27. doi: 10.12740/PP/30811. [DOI] [PubMed] [Google Scholar]
- 28.Markkula N, Suvisaari J, Saarni SI, Pirkola S, Peña S, Saarni S, et al. Prevalence and correlates of major depressive disorder and dysthymia in an eleven-year follow-up – results from the Finnish health 2011 survey. J Affect Disord. 2015;173:73–80. doi: 10.1016/j.jad.2014.10.015. [DOI] [PubMed] [Google Scholar]
- 29.Assari S, Lankarani MM, Caldwell CH. Does discrimination explain high risk of depression among high-income African American men? Behav Sci (Basel) 2018;8:40. doi: 10.3390/bs8040040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chen Y, Bennett D, Clarke R, Guo Y, Yu C, Bian Z, et al. Patterns and correlates of major depression in Chinese adults: a cross-sectional study of 0. 5 million men and women. Psychol Med. 2017;47:958–70. doi: 10.1017/S0033291716002889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gureje O, Uwakwe R, Oladeji B, Makanjuola VO, Esan O. Depression in adult Nigerians: results from the Nigerian survey of mental health and well-being. J Affect Disord. 2010;120:158–64. doi: 10.1016/j.jad.2009.04.030. [DOI] [PubMed] [Google Scholar]
- 32.Hasin DS, Goodwin RD, Stinson FS, Grant BF. Epidemiology of major depressive disorder. Results from the national epidemiologic survey on alcoholism and related conditions. Arch Gen Psychiatry. 2005;62:1097–106. doi: 10.1001/archpsyc.62.10.1097. [DOI] [PubMed] [Google Scholar]
- 33.Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, et al. The epidemiology of major depressive disorder: results from the national comorbidity survey replication (NCS-R) JAMA. 2003;289:3095–105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- 34.Kleinberg A, Aluoja A, Vasar V. Point prevalence of major depression in Estonia. Results from the 2006 Estonian Health Survey. Eur Psychiatry. 2010;25:485–90. doi: 10.1016/j.eurpsy.2010.06.005. [DOI] [PubMed] [Google Scholar]
- 35.Klijs B, Kibele EU, Ellwardt L, Zuidersma M, Stolk RP, Wittek RP, et al. Neighbourhood income and major depressive disorder in a large Dutch population: results from the lifelines cohort study. BMC Public Health. 2016;16:773. doi: 10.1186/s12889-016-3332-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mohammadi MR, Davidian H, Noorbala AA, Malekafzali H, Naghavi HR, Pouretemad HR, et al. An epidemiological survey of psychiatric disorders in Iran. Clin Pract Epidemiol Ment Health. 2005;1:16. doi: 10.1186/1745-0179-1-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Munhoz TN, Santos IS, Matijasevich A. Major depressive episode among Brazilian adults: a cross-sectional population-based study. J Affect Disord. 2013;150:401–7. doi: 10.1016/j.jad.2013.04.031. [DOI] [PubMed] [Google Scholar]
- 38.Piazza M, Fiestas F. [Annual prevalence of mental disorders and use of mental health services in Peru: results of the World Mental Health Survey, 2005] Rev Peru Med Exp Salud Publica. 2014;31:30–8. [PubMed] [Google Scholar]
- 39.Porras-Segovia A, Valmisa E, Gutiérrez B, Ruiz I, Rodríguez-Barranco M, Cervilla J. Prevalence and correlates of major depression in Granada, Spain: results from the GranadΣp study. Int J Soc Psychiatry. 2018;64:450–8. doi: 10.1177/0020764018771405. [DOI] [PubMed] [Google Scholar]
- 40.Slone LB, Norris FH, Murphy AD, Baker CK, Perilla JL, Diaz D, et al. Epidemiology of major depression in four cities in Mexico. Depress Anxiety. 2006;23:158–67. doi: 10.1002/da.20137. [DOI] [PubMed] [Google Scholar]
- 41.Smith DJ, Nicholl BI, Cullen B, Martin D, Ul-Haq Z, Evans J, et al. Prevalence and characteristics of probable major depression and bipolar disorder within UK biobank: cross-sectional study of 172, 751 participants. PLoS One. 2013;8:e75362. doi: 10.1371/journal.pone.0075362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Topuzoğlu A, Binbay T, Ulas H, Elbi H, Tanik FA, Zağli N, et al. The epidemiology of major depressive disorder and subthreshold depression in Izmir, Turkey: prevalence, socioeconomic differences, impairment and help-seeking. J Affect Disord. 2015;181:78–86. doi: 10.1016/j.jad.2015.04.017. [DOI] [PubMed] [Google Scholar]
- 43.Porras-Segovia A, Rivera M, Molina E, López-Chaves D, Gutiérrez B, Cervilla J. Physical exercise and body max index as correlates of major depressive disorder in community-dwelling adults: results from the PISMA-ep study. J Affect Disord. 2019;251:263–9. doi: 10.1016/j.jad.2019.01.050. [DOI] [PubMed] [Google Scholar]
- 44.Chen CY, Chang CM, Lin HL, Chu CL. The association between exposure to second-hand smoke and major depressive disorder in perimenopausal women: results from apopulation-based study. Ann Med. 2018;50:596–604. doi: 10.1080/07853890.2018.1534264. [DOI] [PubMed] [Google Scholar]
- 45.Kessler RC, Gruber M, Hettema JM, Hwang I, Sampson N, Yonkers KA. Co-morbid major depressive disorder and generalized anxiety disorders in the national comorbidity survey follow-up. Psychol Med. 2008;38:365–74. doi: 10.1017/S0033291707002012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mathew AR, Pettit JW, Lewinsohn PM, Seeley JR, Roberts RE. Co-morbidity between major depressive disorder and anxiety disorders: shared etiology or direct causation? Psychol Med. 2011;41:2023–34. doi: 10.1017/S0033291711000407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Barkow K, Maier W, Ustün TB, Gänsicke M, Wittchen HU, Heun R. Risk factors for depression at 12-month follow-up in adult primary health care patients with major depression: an international prospective study. J Affect Disord. 2003;76:157–69. doi: 10.1016/s0165-0327(02)00081-2. [DOI] [PubMed] [Google Scholar]
- 48.Choy Y, Fyer AJ, Goodwin RD. Specific phobia and comorbid depression: a closer look at the national comorbidity survey data. Compr Psychiatry. 2007;48:132–6. doi: 10.1016/j.comppsych.2006.10.010. [DOI] [PubMed] [Google Scholar]
- 49.Kounou KB, Bui E, Dassa KS, Hinton D, Fischer L, Djassoa G, et al. Childhood trauma, personality disorders symptoms and current major depressive disorder in Togo. Soc Psychiatry Psychiatr Epidemiol. 2013;48:1095–103. doi: 10.1007/s00127-012-0634-2. [DOI] [PubMed] [Google Scholar]
- 50.Reichborn-Kjennerud T, Czajkowski N, Røysamb E, Ørstavik RE, Neale MC, Torgersen S, et al. Major depression and dimensional representations of DSM-IV personality disorders: a population-based twin study. Psychol Med. 2010;40:1475–84. doi: 10.1017/S0033291709991954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Assari S. Neuroticism predicts subsequent risk of major depression for whites but not blacks. Behav Sci (Basel) 2017;7:64. doi: 10.3390/bs7040064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Jylhä P, Melartin T, Rytsälä H, Isometsä E. Neuroticism, introversion, and major depressive disorder-traits, states, or scars? Depress Anxiety. 2009;26:325–34. doi: 10.1002/da.20385. [DOI] [PubMed] [Google Scholar]
- 53.Kendler KS, Gatz M, Gardner CO, Pedersen NL. Personality and major depression: a Swedish longitudinal, population-based twin study. Arch Gen Psychiatry. 2006;63:1113–20. doi: 10.1001/archpsyc.63.10.1113. [DOI] [PubMed] [Google Scholar]
- 54.Meng X, D’Arcy C. The projected effect of risk factor reduction on major depression incidence: a 16-year longitudinal Canadian cohort of the national population health survey. J Affect Disord. 2014;158:56–61. doi: 10.1016/j.jad.2014.02.007. [DOI] [PubMed] [Google Scholar]
- 55.Ohayon MM, Schatzberg AF. Using chronic pain to predict depressive morbidity in the general population. Arch Gen Psychiatry. 2003;60:39–47. doi: 10.1001/archpsyc.60.1.39. [DOI] [PubMed] [Google Scholar]
- 56.Fergusson DM, Boden JM, Horwood LJ. Tests of causal links between alcohol abuse or dependence and major depression. Arch Gen Psychiatry. 2009;66:260–6. doi: 10.1001/archgenpsychiatry.2008.543. [DOI] [PubMed] [Google Scholar]
- 57.Bellos S, Skapinakis P, Rai D, Zitko P, Araya R, Lewis G, et al. Cross-cultural patterns of the association between varying levels of alcohol consumption and the common mental disorders of depression and anxiety: secondary analysis of the WHO Collaborative Study on psychological problems in general health care. Drug Alcohol Depend. 2013;133:825–31. doi: 10.1016/j.drugalcdep.2013.08.030. [DOI] [PubMed] [Google Scholar]
- 58.Chen J, Cai Y, Cong E, Liu Y, Gao J, Li Y, et al. Childhood sexual abuse and the development of recurrent major depression in Chinese women. PLoS One. 2014;9:e87569. doi: 10.1371/journal.pone.0087569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Widom CS, DuMont K, Czaja SJ. A prospective investigation of major depressive disorder and comorbidity in abused and neglected children grown up. Arch Gen Psychiatry. 2007;64:49–56. doi: 10.1001/archpsyc.64.1.49. [DOI] [PubMed] [Google Scholar]
- 60.Gutiérrez B, Bellón JÁ, Rivera M, Molina E, King M, Marston L, et al. The risk for major depression conferred by childhood maltreatment is multiplied by BDNF and SERT genetic vulnerability: a replication study. J Psychiatry Neurosci. 2015;40:187–96. doi: 10.1503/jpn.140097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Stegenga BT, Nazareth I, Grobbee DE, Torres-González F, Švab I, Maaroos HI, et al. Recent life events pose greatest risk for onset of major depressive disorder during mid-life. J Affect Disord. 2012;136:505–13. doi: 10.1016/j.jad.2011.10.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Power RA, Lecky-Thompson L, Fisher HL, Cohen-Woods S, Hosang GM, Uher R, et al. The interaction between child maltreatment, adult stressful life events and the 5-HTTLPR in major depression. J Psychiatr Res. 2013;47:1032–5. doi: 10.1016/j.jpsychires.2013.03.017. [DOI] [PubMed] [Google Scholar]
- 63.Bonomi AE, Anderson ML, Reid RJ, Rivara FP, Carrell D, Thompson RS. Medical and psychosocial diagnoses in women with a history of intimate partner violence. Arch Intern Med. 2009;169:1692–7. doi: 10.1001/archinternmed.2009.292. [DOI] [PubMed] [Google Scholar]
- 64.Deyessa N, Berhane Y, Alem A, Ellsberg M, Emmelin M, Hogberg U, et al. Intimate partner violence and depression among women in rural Ethiopia: a cross-sectional study. Clin Pract Epidemiol Ment Health. 2009;5:8. doi: 10.1186/1745-0179-5-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ouellet-Morin I, Fisher HL, York-Smith M, Fincham-Campbell S, Moffitt TE, Arseneault L. Intimate partner violence and new-onset depression: a longitudinal study of women’s childhood and adult histories of abuse. Depress Anxiety. 2015;32:316–24. doi: 10.1002/da.22347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Schulz A, Becker M, Van der Auwera S, Barnow S, Appel K, Mahler J, et al. The impact of childhood trauma on depression: does resilience matter? Population-based results from the study of health in Pomerania. J Psychosom Res. 2014;77:97–103. doi: 10.1016/j.jpsychores.2014.06.008. [DOI] [PubMed] [Google Scholar]
- 67.Spinhoven P, Elzinga BM, Hovens JG, Roelofs K, Zitman FG, van Oppen P, et al. The specificity of childhood adversities and negative life events across the life span to anxiety and depressive disorders. J Affect Disord. 2010;126:103–12. doi: 10.1016/j.jad.2010.02.132. [DOI] [PubMed] [Google Scholar]
- 68.Pasco JA, Williams LJ, Jacka FN, Ng F, Henry MJ, Nicholson GC, et al. Tobacco smoking as a risk factor for major depressive disorder: population-based study. Br J Psychiatry. 2008;193:322–6. doi: 10.1192/bjp.bp.107.046706. [DOI] [PubMed] [Google Scholar]
- 69.Currie SR, Wang JL. Chronic back pain and major depression in the general Canadian population. Pain. 2004;107:54–60. doi: 10.1016/j.pain.2003.09.015. [DOI] [PubMed] [Google Scholar]
- 70.Egede LE. Major depression in individuals with chronic medical disorders: prevalence, correlates and association with health resource utilization, lost productivity and functional disability. Gen Hosp Psychiatry. 2007;29:409–16. doi: 10.1016/j.genhosppsych.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 71.Stegmann ME, Ormel J, de Graaf R, Haro JM, de Girolamo G, Demyttenaere K, et al. Functional disability as an explanation of the associations between chronic physical conditions and 12-month major depressive episode. J Affect Disord. 2010;124:38–44. doi: 10.1016/j.jad.2009.10.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Gabilondo A, Vilagut G, Pinto-Meza A, Haro JM, Alonso J. Comorbidity of major depressive episode and chronic physical conditions in Spain, a country with low prevalence of depression. Gen Hosp Psychiatry. 2012;34:510–7. doi: 10.1016/j.genhosppsych.2012.05.005. [DOI] [PubMed] [Google Scholar]
- 73.Louter MA, Pelzer N, de Boer I, Kuijvenhoven BE, van Oosterhout WP, van Zwet EW, et al. Prevalence of lifetime depression in a large hemiplegic migraine cohort. Neurology. 2016;87:2370–4. doi: 10.1212/WNL.0000000000003376. [DOI] [PubMed] [Google Scholar]
- 74.Modgill G, Jette N, Wang JL, Becker WJ, Patten SB. A population-based longitudinal community study of major depression and migraine. Headache. 2012;52:422–32. doi: 10.1111/j.1526-4610.2011.02036.x. [DOI] [PubMed] [Google Scholar]
- 75.Baune BT, Adrian I, Arolt V, Berger K. Associations between major depression, bipolar disorders, dysthymia and cardiovascular diseases in the general adult population. Psychother Psychosom. 2006;75:319–26. doi: 10.1159/000093955. [DOI] [PubMed] [Google Scholar]
- 76.Chen MH, Su TP, Chen YS, Hsu JW, Huang KL, Chang WH, et al. Higher risk of developing major depression and bipolar disorder in later life among adolescents with asthma: a nationwide prospective study. J Psychiatr Res. 2014;49:25–30. doi: 10.1016/j.jpsychires.2013.10.015. [DOI] [PubMed] [Google Scholar]
- 77.Chien IC, Wu EL, Lin CH, Chou YJ, Chou P. Prevalence of diabetes in patients with major depressive disorder: a population-based study. Compr Psychiatry. 2012;53:569–75. doi: 10.1016/j.comppsych.2011.06.004. [DOI] [PubMed] [Google Scholar]
- 78.Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V, Ustun B. Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet. 2007;370:851–8. doi: 10.1016/S0140-6736(07)61415-9. [DOI] [PubMed] [Google Scholar]
- 79.Farmer A, Korszun A, Owen MJ, Craddock N, Jones L, Jones I, et al. Medical disorders in people with recurrent depression. Br J Psychiatry. 2008;192:351–5. doi: 10.1192/bjp.bp.107.038380. [DOI] [PubMed] [Google Scholar]
- 80.Anderson SE, Cohen P, Naumova EN, Jacques PF, Must A. Adolescent obesity and risk for subsequent major depressive disorder and anxiety disorder: prospective evidence. Psychosom Med. 2007;69:740–7. doi: 10.1097/PSY.0b013e31815580b4. [DOI] [PubMed] [Google Scholar]
- 81.Tyrrell J, Mulugeta A, Wood AR, Zhou A, Beaumont RN, Tuke MA, et al. Using genetics to understand the causal influence of higher BMI on depression. Int J Epidemiol. 2019;48:834–48. doi: 10.1093/ije/dyy223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Jung SJ, Woo HT, Cho S, Park K, Jeong S, Lee YJ, et al. Association between body size, weight change and depression: systematic review and meta-analysis. Br J Psychiatry. 2017;211:14–21. doi: 10.1192/bjp.bp.116.186726. [DOI] [PubMed] [Google Scholar]
- 83.Mather AA, Cox BJ, Enns MW, Sareen J. Associations of obesity with psychiatric disorders and suicidal behaviors in a nationally representative sample. J Psychosom Res. 2009;66:277–85. doi: 10.1016/j.jpsychores.2008.09.008. [DOI] [PubMed] [Google Scholar]
- 84.Saveanu RV, Nemeroff CB. Etiology of depression: genetic and environmental factors. Psychiatr Clin North Am. 2012;35:51–71. doi: 10.1016/j.psc.2011.12.001. [DOI] [PubMed] [Google Scholar]
- 85.Chen YY, Wu KC, Yousuf S, Yip PS. Suicide in Asia: opportunities and challenges. Epidemiol Rev. 2012;34:129–44. doi: 10.1093/epirev/mxr025. [DOI] [PubMed] [Google Scholar]
- 86.Pérez-Sales P. Psicologiía y psiquiatriía transcultural. Bilbao:: Desclée de Brouwer;; 2004. [Google Scholar]
- 87.Mezzich JE, Kirmayer LJ, Kleinman A, Fabrega H, Jr, Parron DL, Good BJ, et al. The place of culture in DSM-IV. J Nerv Ment Dis. 1999;187:457–64. doi: 10.1097/00005053-199908000-00001. [DOI] [PubMed] [Google Scholar]
- 88.Ali GC, Ryan G, De Silva MJ. Validated screening tools for common mental disorders in low and middle income countries: a systematic review. PLoS One. 2016;11:e0156939. doi: 10.1371/journal.pone.0156939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Jablensky A. Psychiatric classifications: validity and utility. World Psychiatry. 2016;15:26–31. doi: 10.1002/wps.20284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Simon GE, Goldberg DP, von Korff M, Üstün TB. Understanding cross-national differences in depression prevalence. Psychol Med. 2002;32:585–94. doi: 10.1017/s0033291702005457. [DOI] [PubMed] [Google Scholar]
- 91.Kessler RC. Epidemiology of women and depression. J Affect Disord. 2003;74:5–13. doi: 10.1016/s0165-0327(02)00426-3. [DOI] [PubMed] [Google Scholar]
- 92.Pudrovska T, Karraker A. Gender, job authority, and depression. J Health Soc Behav. 2014;55:424–41. doi: 10.1177/0022146514555223. [DOI] [PubMed] [Google Scholar]
- 93.Hausner H, Hajak G, Spiessl H. Gender differences in help-seeking behavior on two internet forums for individuals with self-reported depression. Gend Med. 2008;5:181–5. doi: 10.1016/j.genm.2008.05.008. [DOI] [PubMed] [Google Scholar]
- 94.Piccinelli M, Wilkinson G. Gender differences in depression. Critical review. Br J Psychiatry. 2000;177:486–92. doi: 10.1192/bjp.177.6.486. [DOI] [PubMed] [Google Scholar]
- 95.Chang CC, Chang HA, Fang WH, Chang TC, Huang SY. Gender-specific association between serotonin transporter polymorphisms (5-HTTLPR and rs25531) and neuroticism, anxiety and depression in well-defined healthy Han Chinese. J Affect Disord. 2017;207:422–8. doi: 10.1016/j.jad.2016.08.055. [DOI] [PubMed] [Google Scholar]
- 96.Fagniart M, Reynaert C, Jacques D, Lepièce B, Zdanowicz N. Depression, gender and cellular immunity: influence of gender and severity of depression on the cellular immunity. Psychiatr Danub. 2016;28((Suppl 1)):179–82. [PubMed] [Google Scholar]
- 97.Kuehner C. Why is depression more common among women than among men? Lancet Psychiatry. 2017;4:146–58. doi: 10.1016/S2215-0366(16)30263-2. [DOI] [PubMed] [Google Scholar]
- 98.Dohrenwend BP. Socioeconomic status (SES) and psychiatric disorders. Are the issues still compelling? Soc Psychiatry Psychiatr Epidemiol. 1990;25:41–7. doi: 10.1007/BF00789069. [DOI] [PubMed] [Google Scholar]
- 99.Cheng C, Cheung MW, Montasem A. 44 Members of the International Network of Well-Being Studies Explaining differences in subjective well-being across 33 nations using multilevel models: universal personality, cultural relativity, and national income. J Pers. 2016;84:46–58. doi: 10.1111/jopy.12136. [DOI] [PubMed] [Google Scholar]
- 100.Helgeson VS, Zajdel M. Adjusting to chronic health conditions. Annu Rev Psychol. 2017;68:545–71. doi: 10.1146/annurev-psych-010416-044014. [DOI] [PubMed] [Google Scholar]
- 101.Miller AH, Maletic V, Raison CL. Inflammation and its discontents: the role of cytokines in the pathophysiology of major depression. Biol Psychiatry. 2009;65:732–41. doi: 10.1016/j.biopsych.2008.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Carney RM, Freedland KE, Miller GE, Jaffe AS. Depression as a risk factor for cardiac mortality and morbidity: a review of potential mechanisms. J Psychosom Res. 2002;53:897–902. doi: 10.1016/s0022-3999(02)00311-2. [DOI] [PubMed] [Google Scholar]
- 103.Chan KL, Cathomas F, Russo SJ. Central and peripheral inflammation link metabolic syndrome and major depressive disorder. Physiology (Bethesda) 2019;34:123–33. doi: 10.1152/physiol.00047.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Ambrósio G, Kaufmann FN, Manosso L, Platt N, Ghisleni G, Rodrigues AL, et al. Depression and peripheral inflammatory profile of patients with obesity. Psychoneuroendocrinology. 2018;91:132–41. doi: 10.1016/j.psyneuen.2018.03.005. [DOI] [PubMed] [Google Scholar]
- 105.Tronieri JS, Wurst CM, Pearl RL, Allison KC. Sex differences in obesity and mental health. Curr Psychiatry Rep. 2017;19:29. doi: 10.1007/s11920-017-0784-8. [DOI] [PubMed] [Google Scholar]
- 106.Talkovsky AM, Green KL, Osegueda A, Norton PJ. Secondary depression in transdiagnostic group cognitive behavioral therapy among individuals diagnosed with anxiety disorders. J Anxiety Disord. 2017;46:56–64. doi: 10.1016/j.janxdis.2016.09.008. [DOI] [PubMed] [Google Scholar]
- 107.Podlogar MC, Rogers ML, Stanley IH, Hom MA, Chiurliza B, Joiner TE. Anxiety, depression, and the suicidal spectrum: a latent class analysis of overlapping and distinctive features. Cogn Emot. 2018;32:1464–77. doi: 10.1080/02699931.2017.1303452. [DOI] [PubMed] [Google Scholar]
- 108.McTeague LM, Huemer J, Carreon DM, Jiang Y, Eickhoff SB, Etkin A. Identification of common neural circuit disruptions in cognitive control across psychiatric disorders. Am J Psychiatry. 2017;174:676–85. doi: 10.1176/appi.ajp.2017.16040400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Roohafza H, Feizi A, Afshar H, Mazaheri M, Behnamfar O, Hassanzadeh-Keshteli A, et al. Path analysis of relationship among personality, perceived stress, coping, social support, and psychological outcomes. World J Psychiatry. 2016;6:248–56. doi: 10.5498/wjp.v6.i2.248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Bortolasci CC, Vargas HO, Souza-Nogueira A, Barbosa DS, Moreira EG, Nunes SO, et al. Lowered plasma paraoxonase (PON) 1 activity is a trait marker of major depression and PON1 Q192R gene polymorphism-smoking interactions differentially predict the odds of major depression and bipolar disorder. J Affect Disord. 2014;159:23–30. doi: 10.1016/j.jad.2014.02.018. [DOI] [PubMed] [Google Scholar]
- 111.Chan AM, von Mühlen D, Kritz-Silverstein D, Barrett-Connor E. Regular alcohol consumption is associated with increasing quality of life and mood in older men and women: the Rancho Bernardo Study. Maturitas. 2009;62:294–300. doi: 10.1016/j.maturitas.2009.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Valencia-Martín JL, Galán I, Guallar-Castillón P, Rodríguez-Artalejo F. Alcohol drinking patterns and health-related quality of life reported in the Spanish adult population. Prev Med. 2013;57:703–7. doi: 10.1016/j.ypmed.2013.09.007. [DOI] [PubMed] [Google Scholar]
- 113.Vollmayr B, Gass P. Learned helplessness: unique features and translational value of a cognitive depression model. Cell Tissue Res. 2013;354:171–8. doi: 10.1007/s00441-013-1654-2. [DOI] [PubMed] [Google Scholar]