Abstract
Objective
There is limited information on the severity of COVID-19 infection in children with comorbidities. We investigated the effects of pediatric comorbidities on COVID-19 severity by means of a systematic review and meta-analysis of published literature.
Methods
PubMed, Embase, and Medline databases were searched for publications on pediatric COVID-19 infections published January 1st to October 5th, 2020. Articles describing at least one child with and without comorbidities, COVID-19 infection, and reported outcomes were included.
Results
42 studies containing 275,661 children without comorbidities and 9,353 children with comorbidities were included. Severe COVID-19 was present in 5.1% of children with comorbidities, and in 0.2% without comorbidities. Random-effects analysis revealed a higher risk of severe COVID-19 among children with comorbidities than for healthy children; relative risk ratio 1.79 (95% CI 1.27 – 2.51; I2 = 94%). Children with underlying conditions also had a higher risk of COVID-19-associated mortality; relative risk ratio 2.81 (95% CI 1.31 – 6.02; I2 = 82%). Children with obesity had a relative risk ratio of 2.87 (95% CI 1.16 – 7.07; I2 = 36%).
Conclusions
Children with comorbidities have a higher risk of severe COVID-19 and associated mortality than children without underlying disease. Additional studies are required to further evaluate this relationship.
Keywords: Coronavirus, COVID-19, Pediatrics, Comorbidity, Meta-Analysis
Introduction
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is the causative agent of the human coronavirus disease 2019 (COVID-19) pandemic that officially began on March 11, 2020 (Cucinotta and Vanelli, 2020). At the time of writing of this report —November 9th, 2020 — there had been 50,539,082 confirmed cases with an associated 1,258,321 deaths worldwide resulting from COVID-19 infection (COVID-19 Map, 2020). The virus primarily affects the lower respiratory tract, and infected individuals primarily present with fever, cough, and dyspnea, however gastrointestinal (GI) manifestations can also occur (Huang et al., 2020, Shi et al., 2020). Although the infection course is usually non-fatal, severe COVID-19 infection with life-threatening presentations of acute respiratory distress syndrome (ARDS) and multiple organ failure can occur (Huang et al., 2020, Zhou et al., 2020). Risk factors for severe manifestations of SARS-CoV-2 illness and associated mortality include age greater than 65 years (Du et al., 2020; Wu and McGoogan, 2020), and underlying comorbidities such as diabetes, hypertension, and obesity (Caussy et al., 2020; Du et al., 2020; Guan et al., 2020; Wu and McGoogan, 2020).
Multiple studies on COVID-19 infection in children have noted differences in infection rates, symptoms, and mortality as compared to adults (Dong et al., 2020; Wu and McGoogan, 2020). One of the most comprehensive early studies of pediatric patients with SARS-CoV-2 infection reported that children develop a relatively mild disease course with 83% of confirmed cases presenting with mild to moderate infection, with an additional 13% being asymptomatic, and only 3% presenting with severe and critical illness (Dong et al., 2020). However, such early case series potentially suffer from decreased testing of mildly infected individuals thereby leading to a potentially low rate of documented asymptomatic infections. A recent outbreak in a children’s overnight camp in the United States reported an asymptomatic infection rate of 26% among COVID-19 infected children (Szablewski, 2020). Nonetheless, the disease course in children can be heterogenous in nature, with the most common clinical signs and symptoms including fever, headaches, and sore throat (Szablewski, 2020). Critical illness in children and adults alike typically manifests with severe pneumonia characterized by specific oxygen concentrations less than 92%, autoinflammatory shock, and respiratory distress (Sankar et al., 2020). Such cases frequently require mechanical ventilation and treatment with antiviral and immunomodulating regimens (Sankar et al., 2020, Zimmermann and Curtis, 2020).
Even so, previous reports have indicated clusters of an inflammatory syndrome, called “Multisystem Inflammatory Syndrome associated with COVID-19 (MIS-C)” or “Paediatric inflammatory multisystem syndrome (PIMS)” Kawasaki-like disease, a potentially fatal vasculitis, occurring in children following COVID-19 infection (Riollano‐Cruz et al., 2020; Verdoni et al., 2020). Such reports indicate the potential (albeit uncommon) for severe and potentially fatal COVID-19 in pediatric patients. Although previous studies have established pre-existing comorbidities as significant risk factors for severe SARS-CoV-2 infection in adults (Du et al., 2020, Guan et al., 2020), questions remain regarding childhood comorbidities and associated COVID-19 outcomes. While systematic reviews and meta-analyses examining COVID-19 in pediatric patients have been published (Ding et al., 2020, Hoang et al., 2020), these reports did not evaluate the risk of severe SARS-CoV-2 infection specifically in children with pre-existing conditions. Consequently, the objective of this systematic review and meta-analysis is to examine the relative risk of severe COVID-19 infection and associated mortality in children with comorbidities.
Methods
Search Strategy and Selection Criteria
For this systematic review and meta-analysis PubMed, Medline, and Embase databases were queried for articles published from January 1st, 2020 until October 5th, 2020. The Medline and Embase searches were conducted via the Ovid interface. The search terms “COVID-19”, “SARS-nCoV-2”, “SARS-CoV-2”, “2019-nCoV”, “novel coronavirus”, and “coronavirus” were used to obtain articles relating to the novel coronavirus pandemic occurring in 2020. To obtain literature pertaining specifically to SARS-CoV-2 infection in pediatric patients, the terms “child*”, “pediatr*”, “paediatr*”, “teenage”, “adolescent”, “infant”, and “newborn” were queried in conjunction with the coronavirus search. For the full search queries, see Supplement S1. To capture articles potentially missed by our systematic search, Google Scholar was queried for articles pertaining to COVID-19 infection in pediatric patients. Further articles were obtained by examining the references of highly relevant systematically retrieved articles. Only articles in English were considered for inclusion. References were managed with Endnote (version X9.0) software which was also used for duplicate removal. The systematic literature search was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta Analyses (PRISMA) recommendations (Moher et al., 2009).
Following deduplication, the reference titles were reviewed by BKT. Titles that did not imply a subject matter relevant to COVID-19 in pediatric patients were excluded. Following title review, the full-text content of the remaining literature was thoroughly analyzed by the author BKT. The following exclusion criteria were applied to the full-text articles: articles not mentioning pediatric comorbidities; adult only studies; articles where the pediatric comorbidity data was indistinguishable from adult comorbidity data; pre-existing reviews, systematic-reviews, and meta-analyses; articles with patients without confirmed COVID-19 infections; basic science studies; clinical discussions, recommendations, and guidelines; articles without reported patient outcomes; and studies of other coronaviruses. Articles containing at least one paediatric patient with comorbidities, and one paediatric patient without comorbidities were included. Furthermore, we included articles for which the severity and outcomes of SARS-CoV-2 infection in the paediatric patients was clearly defined. Following full-text review, BKT and KJ graded the remaining studies using the National Institutes of Health (NIH) Quality Assessment Tool for Case Series and Studies (Study Quality Assessment Tools, 2020). Any disagreements in rating were handled via discussion by the two reviewers until a consensus was reached. For the literature grading see Supplement S2.
Data Extraction and Case Definitions
The study authors; design; country of origin; aims; pediatric sample size; COVID-19 infection counts; disease severity; comorbidity counts; pediatric intensive care unit (PICU) admittance counts; and mortality counts were extracted from the included literature. The extracted comorbidities were either defined by the studies or classified into representative broader categories by BKT and KJ. Comorbidities such as trisomy 21, prematurity, and undefined genetic abnormalities were deemed as “other” pre-existing conditions. Obesity was defined by the studies where available, or by the authors as a body mass index (BMI) at or greater than the 95th percentile for children of the same age and sex according to CDC definitions (Defining Childhood Obesity, 2019). To operationalize severe COVID-19 infection across the different studies, severe infection was deemed as any SARS-CoV-2 infection requiring supplemental help to normal breathing and/or admission to a PICU unless otherwise explicitly stated in the literature. Finally, paediatric patients were defined as participants suffering from COVID-19 who were below 21 years of age.
Statistical Analyses
PICU admission and mortality outcomes were assessed using a random effects meta-analysis (Schwarzer et al., 2015). A random effects model was chosen due to the potential variation in sampled study populations leading to differences in outcomes by co-morbidities. Estimation of random-effects variance was conducted using the Sidik-Jonkman estimator with Hartung-Knapp adjustment (IntHout et al., 2014). For individual trials with no events in one or both groups, a continuity correction of the opposite treatment arm size was added to each cell for each effect measure (Sweeting et al., 2004). Binary estimators including risk ratios, and risk difference were estimated using the Mantel-Haenszel method (Mantel and Haenszel, 1959, Robins et al., 1986). All analyses and data visualization were conducted in R version 4.0.2 using the meta and tidyverse libraries (Balduzzi et al., 2019; Team, R Core, and others, 2020; Wickham et al., 2019).
Role of the Funding Source
This study did not receive any funding. The study design, data analysis, and writing of the manuscript was conceptualized only by the authors.
Results
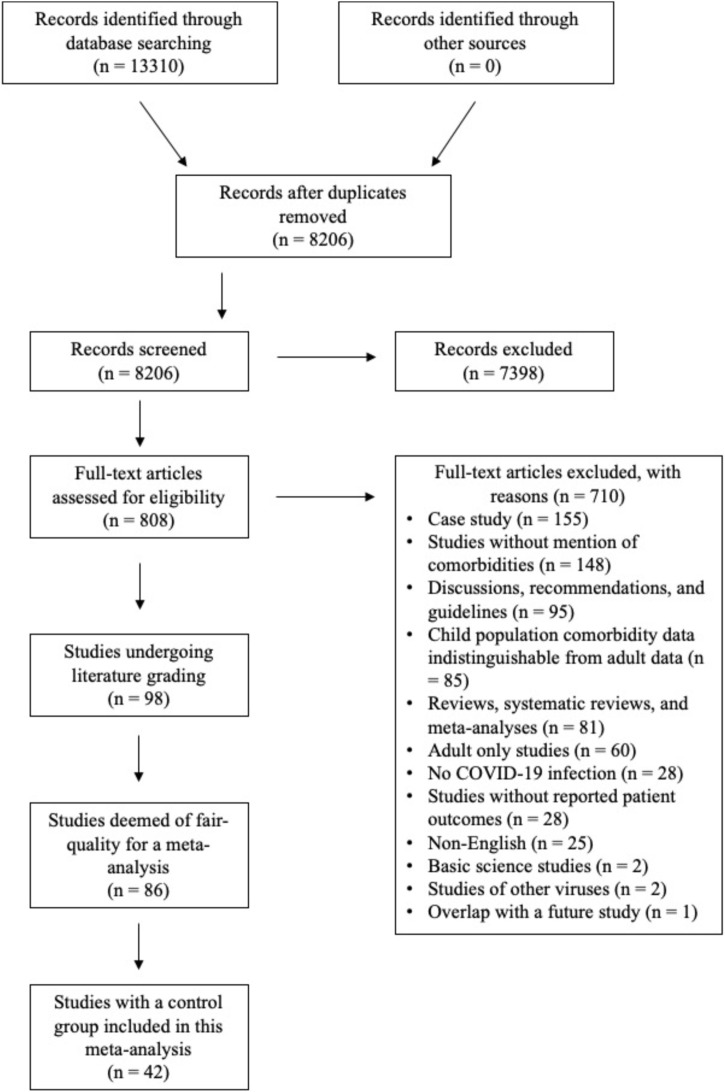
There were 13310 studies identified from our systematic search across the three databases (Fig. 1 ). Following de-duplication, 8206 records were reviewed based on a title screen, of which 7398 were deemed irrelevant to the subject matter of this study. The full-texts of the remaining 808 articles were reviewed for the presence of pediatric study participants who had: 1) pre-existing comorbidities; and 2) COVID-19 infection, for which clear outcomes were reported. 98 articles then underwent literature grading, with 86 studies deemed fair for further analysis. Among these 86 articles, only 42 had pediatric case-control participants without comorbidities with either severe COVID-19 and/or COVID-19-associated mortality. Five studies (Bellino et al., 2020; Bixler et al., 2020; Blumfield and Levin, 2020; Moraleda et al., 2020; Otto et al., 2020) only examined children who died from COVID-19 and were therefore only included in the mortality analysis. These 42 studies were therefore the basis for our analysis examining the effects of comorbidities on severe and potentially fatal manifestations of pediatric SARS-CoV-2 infection. Among the 42 articles, 18 studies were from the USA (43%), and 4 studies were from China (10%), Italy (10%), and Spain (10%) respectively. Of the remaining studies, 3 were from France (7%), 2 were from the United Kingdom (5%), and Iran (5%), and 1 was from Austria (2%), Brazil (2%), India (2%), Turkey (2%), and Uruguay (2%) (Table 1 ).
Fig. 1.
PRISMA flow diagram for the identification of studies pertaining to COVID-19 and children with comorbidities published between January 1 st, 2020 and October 5th, 2020.
Table 1.
Summary and characteristics of the 42 studies included in this systematic review and meta-analysis.
| STUDY | Study type | Country | Study Aim | COVID-19 Infection (N = 285,004) | With comorbidities and COVID-19 (n = 9353) |
COmorbidities and Severe COVID-19A (n = 481) |
Comorbidities and mortality (N = 135) |
|---|---|---|---|---|---|---|---|
| (Abdel-Mannan et al., 2020) | Retrospective | U.K | Report neurological manifestations of children with COVID-19 | 4 | 1 | 1 | 0 |
| (Anand et al., 2020) | Retrospective | India | Describe the clinical profile of neonates born to mothers with COVID-19 | 7 | 3 | 0 | 0 |
| (Bellino et al., 2020) | Retrospective | Italy | Describe characteristics of COVID-19 in pediatric patients | 3836 | 206 | 4 | |
| (Belhadjer et al., 2020) | Retrospective | France | Report cases of acute heart failure associated with COVID-19 in children | 31 | 4 | 4 | 0 |
| (Bhumbra et al., 2020) | Retrospective | USA | Describe the infection course of children hospitalized with COVID-19 | 24 | 8 | 3 | |
| (Biko et al., 2020) | Retrospective | USA | Describe imaging features, comorbidities, and outcomes of children with COVID-19 | 313 | 41 | 17 | 0 |
| (Bixler et al., 2020) | Retrospective | USA | Report the SARS-CoV-2-associated deaths in children residing in the USA | 121 | 91 | 91 | |
| (Blumfield and Levin, 2020) | Retrospective | USA | Report the outcomes of critically-ill children with COVID-19 | 18 | 12 | 2 | |
| (Cai et al., 2020) | Case-series | China | Report the outcomes and clinical characteristics of pediatric patients with COVID-19 that did not have respiratory symptoms as the first manifestation of infection | 5 | 3 | 2 | 0 |
| (Chao et al., 2020) | Retrospective | USA | Report the risk factors associated with severe COVID-19 in pediatric patients | 46 | 31 | 12 | 1 |
| (de Farias et al., 2020) | Prospective | Brazil | Describe the characteristics of COVID-19-associated PIMS in 11 children | 11 | 5 | 5 | 2 |
| (DeBiasi et al., 2020) | Retrospective | USA | Examine the epidemiology of pediatric COVID-19 infection in Washington, DC | 165 | 69 | 5 | 0 |
| (Derespina et al., 2020) | Retrospective | USA | Describe outcomes of COVID-19 in children in New York City | 70 | 52 | 52 | 2 |
| (Diorio et al., 2020) | Prospective | USA | Report the hematological differences between MIS-C and COVID-19 in children | 14 | 13 | 9 | 2 |
| (Du et al., 2020) | Retrospective | China | Report the outcomes of and laboratory characteristics of COVID-19 among hospitalized pediatric patients with a focus on allergic patients | 182 | 59 | 2 | 0 |
| (Eghbali et al., 2020) | Case-series | Iran | Describe 4 cases of pediatric COVID-19 in Iran | 4 | 2 | 2 | 1 |
| (Garazzino et al., 2020) | Retrospective | Italy | Report outcomes and disease characteristics of COVID-19 among multiple pediatric care centres in Italy | 168 | 33 | 2 | 0 |
| (García-Salido et al., 2020) | Prospective | Spain | Describe series of children admitted to a Spanish PICU due to COVID-19 | 7 | 1 | 1 | 0 |
| (Giacomet et al., 2020) | Retrospective | Italy | Describe the characteristics of severe vs non-severe COVID-19 in children | 127 | 20 | 6 | 0 |
| (González-Dambrauskas et al., 2020) | Retrospective | Uruguay | Examine the characteristics and outcomes of pediatric patients in PICUs due to COVID-19 infection |
17 | 12 | 12 | 1 |
| (Götzinger et al., 2020) | Cross-sectional | Austria | Examine the characteristics and outcomes of children with COVID-19 across Europe | 582 | 145 | 25 | 2 |
| (Kainth et al., 2020) | Retrospective | USA | Describe the presentation, course, and severity of pediatric COVID-19 | 65 | 30 | 10 | 1 |
| (Kaushik et al., 2020) | Retrospective | USA | Assess the outcomes of COVID-19-associated MIS-C | 33 | 16 | 16 | |
| (Leeb, 2020) | Retrospective | USA | Examine the epidemiology of COVID-19 among US children | 277,285 | 7738 | 109 | 14 |
| (Lovinsky-Desir et al., 2020) | Retrospective | USA | Examine the impact of asthma on COVID-19 severity | 55 | 24 | 24 | |
| (Mannheim et al., 2020) | Case-series | USA | Report the clinical characteristics of pediatric COVID-19 in Chicago | 64 | 13 | 4 | |
| (Meslin et al., 2020) | Case-series | France | Present outcomes of 6 children with COVID-19 in France | 6 | 2 | 0 | 0 |
| (Moraleda et al., 2020) | Case-series | Spain | Describe clinical features of MIS-C in Spain | 31 | 10 | 2 | |
| (Moreno-Galarraga et al., 2020) | Retrospective | Spain | Describe the presentations of COVID-19 in Spain | 11 | 4 | 0 | 0 |
| (Otto et al., 2020) | Retrospective | USA | Describe the outcomes and features of COVID-19 in children | 424 | 242 | 2 | |
| (Oualha et al., 2020) | Retrospective | France | Describe severe presentations of COVID-19 in children | 27 | 19 | 19 | 2 |
| (Parri et al., 2020) | Retrospective | Italy | Examine the diagnostic, clinical presentation, interventions and outcomes of pediatric patients with confirmed COVID-19 in Italy. | 170 | 38 | 6 | 0 |
| (Riollano‐Cruz et al., 2020) | Retrospective | USA | Describe the first COVID-19 MIS-C associated cases in New York City | 15 | 5 | 4 | 0 |
| (Schwartz et al., 2020) | Case-series | Iran | Describe the characteristics and outcomes of COVID-19 in neonates in Iran | 19 | 15 | 10 | 0 |
| (Shekerdemian et al., 2020) | Cross-sectional | USA | Characterize COVID-19 infection in North American PICUs | 48 | 40 | 40 | |
| (Sun et al., 2020) | Retrospective | China | Examine the clinical characteristics of pediatric COVID-19 | 8 | 1 | 1 | 0 |
| (Swann et al., 2020) | Prospective | UK | Explore the clinical characteristics of pediatric COVID-19 and MIS-C in the UK | 651 | 276 | 63 | 6 |
| (Tagarro et al., 2020) | Retrospective | Spain | Describe the epidemiology and treatment of COVID-19 in Madrid | 41 | 11 | 1 | 0 |
| (Waltuch et al., 2020) | Case series | USA | Describe the characteristics and outcomes of 4 pediatric cases of COVID-19 | 4 | 2 | 2 | 0 |
| (Yayla, 2020) | Retrospective | Turkey | Examine characteristics of COVID-19 in children in Turkey | 220 | 21 | 2 | 0 |
| (Zachariah et al., 2020) | Retrospective | USA | Compare the features of pediatric COVID-19 disease between severe and mild infection | 50 | 33 | 8 | |
| (Zheng et al., 2020) | Retrospective | China | Describe the clinical characteristics of pediatric COVID-19 | 25 | 2 | 2 | 0 |
Abbreviations: COVID-19 - coronavirus disease 2019; PICU - pediatric intensive care unit.
A Defined by the studies, or PICU admission, or need for supplemental breathing aid during the course of infection.
Study Patient Characteristics
From the 42 articles, a total of 285,004 pediatric patients with laboratory-confirmed SARS-CoV-2 infection were identified. Among this cohort, 9,353 (3.3%) had at least one underlying comorbidity (Table 1). Gender demographic data was available for 280,999 COVID-19 infected children, of which 142,411 (50.7%) were female and 138,588 (49.3%) were male. We were able to extrapolate age-category data in 362 children. Of these, 138 (38%) were under 1 year of age, 82 (21%) 1 to 5 years of age, 31 (8%) 6 to 10, 22 (6%) 10 – 14, and 89 (23%) were older than 14 years of age. To the best of our ability, we have excluded any study participants that were over 21 years, such as those present in the study by DeBiasi and colleagues.
Relative Risk of Pediatric Comorbidities on Severe COVID-19 Infection
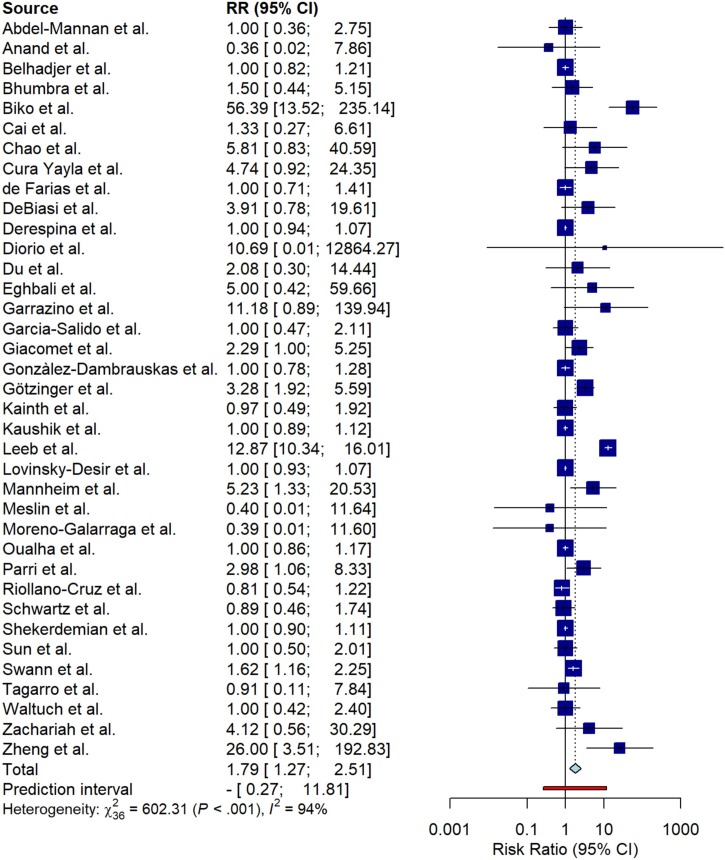
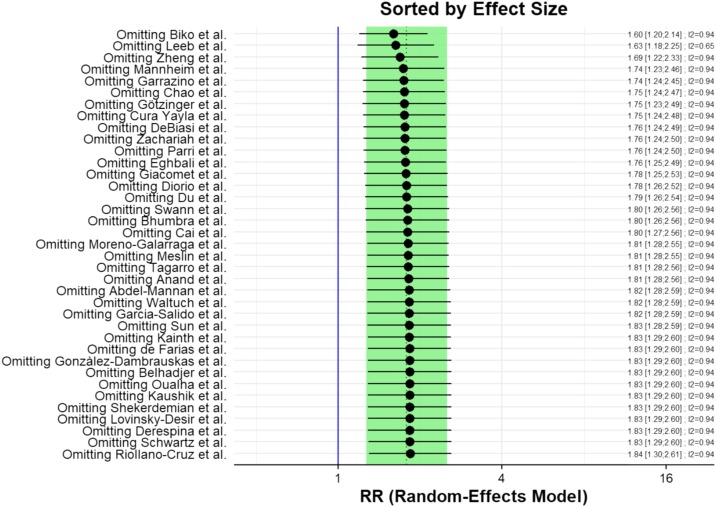
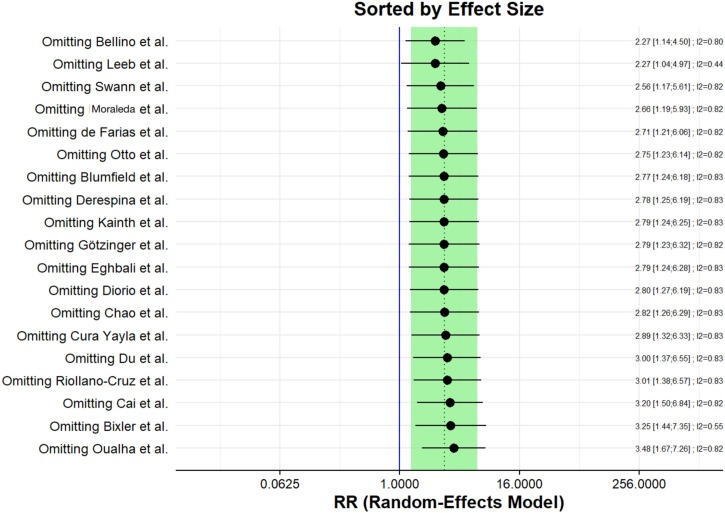
Among the 9,353 pediatric patients with SARS-CoV-2 infection and underlying comorbidities, 481 (5.1%) had severe COVID-19 and/or were admitted to a PICU (Table 1). In contrast, only 579 of the 275,661 (0.21%) pooled pediatric patients without comorbidities had a severe manifestation of COVID-19. Employing a random-effects model to examine the relative risk of severe COVID-19 and/or PICU admission among children with comorbidities, we obtained a total relative risk ratio of 1.79 (95% CI 1.27 – 2.51; 2 = 602.31 (P < 0.001); I2 = 94%) (Fig. 2 ). It is important to note that only 37 studies were included in this analysis as 5 studies only examined COVID-19-associated deaths (Bellino et al., 2020; Bixler et al., 2020; Blumfield and Levin, 2020; Moraleda et al., 2020; Otto et al., 2020). Nonetheless, 7 studies (Anand et al., 2020; Kainth et al., 2020; Meslin et al., 2020; Moreno-Galarraga et al., 2020; Riollano‐Cruz et al., 2020; Schwartz et al., 2020; Tagarro et al., 2020) had a higher risk ratio of severe COVID-19 among pediatric patients without comorbidities than those with underlying conditions (Fig. 2). Furthermore, studies such as the CDC Mortality and Morbidity Weekly Report (Leeb, 2020) had noticeably larger participant cohort populations than other reports. To examine the potential preferential bias of these studies towards the overall relative risk ratio of our analysis, we individually excluded each of the 37 studies to determine the overall effect of each singular study on the net relative risk ratio. Notably, no article significantly influenced the risk ratio in either direction (Fig. 3 ).
Fig. 2.
Pooled estimate of the relative risk of severe COVID-19 among pediatric patients with comorbidities.
Fig. 3.
Sensitivity analysis of the influence of each included study on the overall relative risk of severe COVID-19 among children with comorbidities.
Relative Risk of Pediatric Comorbidities on Mortality Associated with COVID-19 Infection
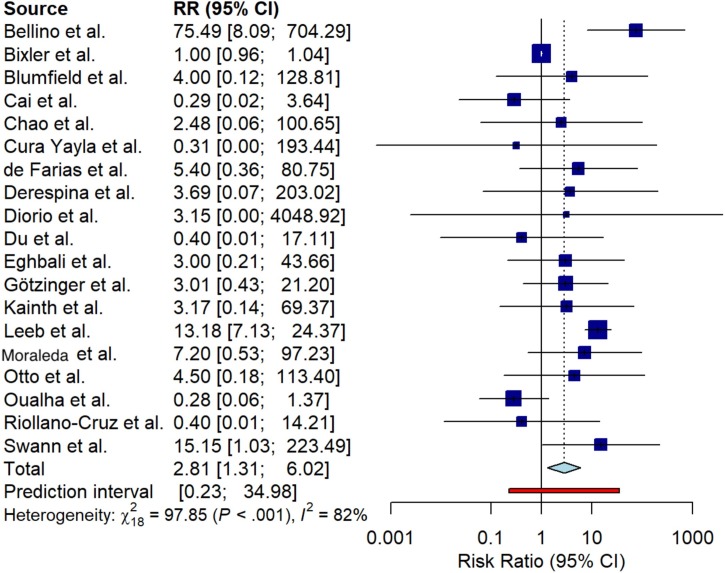
Nineteen of the 42 articles included in this meta-analysis reported children who died while being infected with SARS-CoV-2 (Fig. 4 ). Across the 19 articles, of the 274,647 pediatric patients with COVID-19 infection without comorbidities, only 77 (0.03%) died across 8 studies (Bixler et al., 2020; Cai et al., 2020; Du et al., 2020; Götzinger et al., 2020; Leeb, 2020; Oualha et al., 2020; Riollano‐Cruz et al., 2020; Yayla, 2020). In contrast, 134 (1.5%) of the 8960 children with pre-existing conditions died during the course of their SARS-CoV-2 infection across 15 studies (Bellino et al., 2020; Bixler et al., 2020; Blumfield and Levin, 2020; Chao et al., 2020; Derespina et al., 2020; Diorio et al., 2020; Eghbali et al., 2020; de Farias et al., 2020; Götzinger et al., 2020; Kainth et al., 2020; Leeb, 2020; Moraleda et al., 2020; Otto et al., 2020; Oualha et al., 2020; Swann et al., 2020) (Table 1). The random effects model used to determine the risk of mortality among children with comorbidities and COVID-19 relative to pediatric patients without comorbidities revealed a total risk ratio of 2.81 (95% CI 1.31 – 6.02; 2 = 97.85 (P < 0.001); I2 = 82%) (Fig. 4). In only five of the studies (Cai et al., 2020; Du et al., 2020; Oualha et al., 2020; Riollano‐Cruz et al., 2020; Yayla, 2020) did children with comorbidities have a lower risk of mortality during the course of COVID-19 (Fig. 4). Notably, subsequent sensitivity analysis confirmed that no one article significantly affected the relative risk ratio of mortality among children with pre-existing conditions (Fig. 5 ).
Fig. 4.
Pooled estimate of the relative risk of COVID-19-associated mortality among pediatric patients with comorbidities.
Fig. 5.
Sensitivity analysis of the relative contributions of each study toward the relative risk of mortality during COVID-19 infection in pediatric patients with comorbidities.
Relative Risks of Various Pediatric Comorbidities on Severe COVID-19 Manifestations
Our previously presented analyses hinted at a higher risk of severe COVID-19 infection and associated mortality among pediatric patients with underlying comorbidities (Fig. 2, Fig. 4). We next sought to examine the potential impact of specific comorbidities on the risks of severe SARS-CoV-2 manifestations. For details on the underlying conditions represented among all 9,353 children with comorbidities regardless of COVID-19 severity, see Supplement S3. In the 42 studies included in this meta-analysis, we found that among children with severe COVID-19, 64 children were obese (Abdel-Mannan et al., 2020; Chao et al., 2020; DeBiasi et al., 2020; Derespina et al., 2020; de Farias et al., 2020; Giacomet et al., 2020; González-Dambrauskas et al., 2020; Kaushik et al., 2020; Lovinsky-Desir et al., 2020; Shekerdemian et al., 2020; Swann et al., 2020; Waltuch et al., 2020; Zachariah et al., 2020), 58 had chronic respiratory disease (Belhadjer et al., 2020; Chao et al., 2020; DeBiasi et al., 2020; Diorio et al., 2020; González-Dambrauskas et al., 2020; Götzinger et al., 2020; Kaushik et al., 2020; Lovinsky-Desir et al., 2020; Mannheim et al., 2020; Riollano‐Cruz et al., 2020; Shekerdemian et al., 2020; Swann et al., 2020; Waltuch et al., 2020; Yayla, 2020; Zachariah et al., 2020), 45 had cardiovascular disease (Chao et al., 2020; DeBiasi et al., 2020; Derespina et al., 2020; Diorio et al., 2020; Eghbali et al., 2020; Garazzino et al., 2020; Giacomet et al., 2020; González-Dambrauskas et al., 2020; Götzinger et al., 2020; Kainth et al., 2020; Kaushik et al., 2020; Mannheim et al., 2020; Schwartz et al., 2020, Shekerdemian et al., 2020, Swann et al., 2020, Zachariah et al., 2020, Zheng et al., 2020), 33 had neurologic disorders (Cai et al., 2020, Chao et al., 2020, DeBiasi et al., 2020, Diorio et al., 2020, Giacomet et al., 2020, González-Dambrauskas et al., 2020, Götzinger et al., 2020, Kainth et al., 2020, Oualha et al., 2020, Shekerdemian et al., 2020, Zachariah et al., 2020), 26 had immune disorders (Belhadjer et al., 2020, Chao et al., 2020, Kainth et al., 2020, Mannheim et al., 2020, Shekerdemian et al., 2020, Swann et al., 2020, Zachariah et al., 2020), and 19 had metabolic disease (DeBiasi et al., 2020, Derespina et al., 2020, Riollano‐Cruz et al., 2020, Shekerdemian et al., 2020, Waltuch et al., 2020, Zachariah et al., 2020, Zheng et al., 2020). Additionally, 12 had hematologic disorders (Eghbali et al., 2020, García-Salido et al., 2020, Kaushik et al., 2020, Oualha et al., 2020, Shekerdemian et al., 2020, Yayla, 2020, Zachariah et al., 2020), and 11 had cancer (Chao et al., 2020, Diorio et al., 2020, Du et al., 2020, González-Dambrauskas et al., 2020, Götzinger et al., 2020, Kainth et al., 2020, Sun et al., 2020). Five children had renal disease (Cai et al., 2020, Götzinger et al., 2020, Oualha et al., 2020), and 2 had GI comorbidities (Giacomet et al., 2020) respectively. Seventy-one children had other conditions (Diorio et al., 2020, Garazzino et al., 2020, González-Dambrauskas et al., 2020, Götzinger et al., 2020, Kainth et al., 2020, Kaushik et al., 2020, Mannheim et al., 2020, Schwartz et al., 2020, Shekerdemian et al., 2020, Swann et al., 2020, Zachariah et al., 2020) including prematurity, trisomy 21, or other genetic abnormalities. Finally, only 1 child presented with allergies (Du et al., 2020) and hepatobiliary disease (Riollano‐Cruz et al., 2020) respectively.
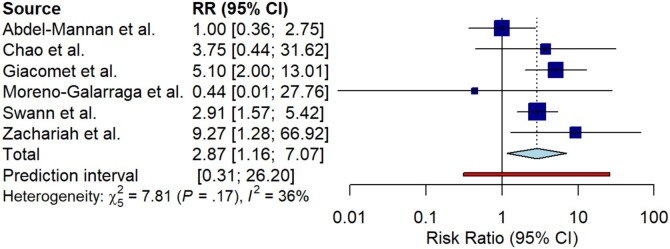
We next analyzed the relative contribution of childhood obesity to pediatric COVID-19 severity. We chose to focus primarily on obesity as it has an easily definable metric (i.e. BMI) that can be compared across multiple studies. Although 64 pediatric patients with underlying obesity presented with severe COVID-19 across 13 studies (Abdel-Mannan et al., 2020, Chao et al., 2020, DeBiasi et al., 2020, Derespina et al., 2020, de Farias et al., 2020, Giacomet et al., 2020, González-Dambrauskas et al., 2020, Kaushik et al., 2020, Lovinsky-Desir et al., 2020, Shekerdemian et al., 2020, Swann et al., 2020, Waltuch et al., 2020, Zachariah et al., 2020), we chose to perform a meta-analysis only on the studies that included case-control participants (Abdel-Mannan et al., 2020, Chao et al., 2020, Giacomet et al., 2020, Moreno-Galarraga et al., 2020, Swann et al., 2020, Zachariah et al., 2020). Examining the risk of obesity on COVID-19 severity in relation to children without comorbidities, we obtained a relative risk ratio of 2.87 (95% CI 1.16 – 7.07; 2 = 7.81 (P = 0.17); I2 = 36%) (Fig. 6 ). We also examined the relative risk of childhood cancer on severe COVID-19 (Supplement S4), from which we were not able to draw any conclusions due to the confidence interval of the relative risk ratio spanning a value of 1.0. Taken together, these results indicate that childhood obesity likely increases risk of severe COVID-19. However, more case-controlled, well-defined studies are needed to examine the effects that other childhood comorbidities such as cancer have on risk of severe manifestations of SARS-CoV-2.
Fig. 6.
Relative risk of childhood obesity on severe manifestations of COVID-19
Discussion
Current meta-analyses of publications involving children with COVID-19 infection primarily examine the overall characteristics, symptoms, and outcomes of SARS-CoV-2 infection regardless of comorbidity status (Ding et al., 2020, Hoang et al., 2020, Ludvigsson, 2020). Studies suggest that children typically have a milder infection course than adults, with an overall good prognosis. However, the effects of comorbidities on COVID-19 severity in children remain unclear. Although a previous correspondence suggested a worse SARS-CoV-2 infection course in children with comorbidities (Harman et al., 2020), the small sample size precludes definitive conclusions. In this systematic review and meta-analysis of 42 articles, we report that children with comorbidities are at higher risk for severe manifestations of COVID-19 and associated mortality relative to previously healthy children. Furthermore, we also note that childhood obesity probably leads to a worse COVID-19 prognosis. To our knowledge, we are the first to report these findings.
Early analyses in adults with COVID-19 indicated that older age (Zhou et al., 2020) and comorbidities such as diabetes, hypertension, malignancies, chronic respiratory disease and obesity are significant risk factors for severe infection (Caussy et al., 2020, Guan et al., 2020, Yang et al., 2020). As such, the early lockdown measures implemented across the world in the spring of 2020 were aimed at protecting vulnerable populations (i.e., the elderly, and people with comorbid conditions) from COVID-19 infection, as well as preventing the overburdening of hospitals. In contrast, early epidemiological studies of pediatric populations (Dong et al., 2020) cited high rates of mild and asymptomatic COVID-19 infection, with certain publications advocating for their return to school (Munro and Faust, 2020, van Bruwaene et al., 2020). The results from our study suggest that children with specific comorbidities are a vulnerable population at risk for potentially life-threatening consequences of COVID-19 infection.
We report that childhood obesity is likely associated with a worsened prognosis of COVID-19 infection. This is in keeping with several adult studies noting that patients who had a BMI greater than or equal to 35 kg/m2 required invasive mechanical ventilation due to SARS-CoV-2 infection more frequently than their leaner counterparts (Caussy et al., 2020, Simonnet et al., 2020). The effects of childhood obesity in potentiating severe COVID-19 are unsurprising. The high visceral adiposity present in obese individuals is known to induce higher levels of local and systemic inflammatory cytokines such as Interleukin-6 (IL-6), and C-reactive protein (CRP) (Fontana et al., 2007). The increased baseline of these cytokines in obesity are also likely the result of increased pro-inflammatory macrophage populations that have been observed in this population (Russo and Lumeng, 2018). These cytokines have been positively correlated with COVID-19 severity (Zeng et al., 2020) and their higher levels in obese individuals may contribute to their increased susceptibility to severe infection. However, childhood obesity likely contributes to severe COVID-19 infection in additional ways.
Unfortunately, we were unable to determine whether other comorbidities increase risk of severe COVID-19. This is in part due to the paucity of case-controlled literature examining the outcomes of children with COVID-19 who have well-defined comorbid conditions. Towards this aim, various international Surveillance Epidemiology of Coronavirus (COVID-19) Under Research Exclusion (SECURE) databases and registries are set up to prospectively collect data, and will be particularly helpful in defining risk of COVID-19 infection and severity in patients with comorbidities. However, to date the available data remain quite limited. Apart from a recent article (Brenner et al., 2020a) and the SECURE-IBD database (Brenner et al., 2020b), a multi-national database examining the outcomes of patients with IBD and COVID-19, limited literature examining the effects of GI diseases on COVID-19 outcomes in children has been published. Furthermore, although recent approaches have begun examining the effects of COVID-19 infection on diseases such as sickle-cell disease (SSD) (McCloskey et al., 2020, Hussain et al., 2020), limited data exist for other systemic diseases. For example, for rheumatic diseases, apart from a retrospective report (Zhong et al., 2020), only a speculative review on the topic has been published (Licciardi et al., 2020). With reports of MIS-C occurring in cohorts of children with COVID-19 infection (Riphagen et al., 2020, Verdoni et al., 2020) the dynamics and underlying characteristics of severe infection in the context of autoinflammatory comorbidities in children require further study.
Study Strengths
Our study has several important strengths. To our knowledge, this is the first systematic review and meta-analysis that examines the relative risk of severe COVID-19 and associated mortality among children with comorbidities. Furthermore, our study is the first to show that childhood obesity likely increases the risk of severe COVID-19 infection course. Lastly, our study has a relatively large sample size of 9,353 children with comorbidities among 42 articles. This relatively large sample size and study number allows for high statistical power, enabling accurate conclusions to be drawn from the study results.
Study Limitations
Our systematic review and meta-analysis have several potential limitations. Most importantly, there likely exists variations in PICU admission criteria across the studies, particularly regarding children with comorbidities and COVID-19 infection. We cannot ascertain whether admission to the PICU was primarily due to problems with underlying comorbidities in some children, with COVID-19 infection being subsequently discovered. Therefore, the increased risk of severe COVID-19 infection among children with comorbidities addressed in this meta-analysis could be the result of a selection bias of PICU admission in favor of children with underlying conditions. Furthermore, our study is subject to a high degree of study heterogeneity due to the small sample size in some of the included studies. In addition, based on the large body of rapidly-published literature surrounding COVID-19 infection, some studies may have used similar participants. Therefore, we cannot be certain that patients were not duplicated in our study. Our meta-analysis was also not able to capture the relative risk that comorbidities other than obesity contribute to severe SARS-CoV-2 viral infection. This is due to the sub-population heterogeneity of comorbidities that limits the ability to draw accurate comparisons between studies. Lastly, our meta-analysis amplifies the ascertainment bias of the primary literature. Asymptomatic COVID-19 infections among children with comorbidities do occur (Poli et al., 2020), however in most jurisdictions at this time, testing of asymptomatic or pauci-symptomatic children is very limited outside of outbreak settings. Consequently, such mild cases among children with comorbidities are likely less represented in the primary literature and therefore in our analysis. We therefore call for further availability of data on pediatric patients with comorbidities and COVID-19 outcomes, regardless of illness severity. Such broader representation within the literature would increase the accuracy of relative risk computation within this population by future meta-analyses.
Conclusions
To our knowledge, this is the first systematic review and meta-analysis examining the severity of COVID-19 infection among pediatric patients with comorbidities. We report that children with pre-existing conditions are at a greater risk of severe COVID-19 and associated mortality. In particular, childhood obesity is likely positively correlated with COVID-19 severity. However, further cross-sectional, case-controlled studies examining the effects of specific well-defined comorbidities are required to examine the effects that pediatric underlying conditions play in COVID-19 severity.
Author Contributions
BKT: study concept and design; literature review, acquisition of data; literature grading; analysis and interpretation of data; statistical analysis; drafting of the manuscript; approval of final manuscript.
JMA: study concept and design; critical revision of the manuscript for important intellectual content; approval of final manuscript.
MAI: statistical analysis, analysis and interpretation of data; critical revision of the manuscript for important intellectual content; approval of final manuscript.
AAL: literature review; critical revision of the manuscript for important intellectual content; approval of final manuscript.
LJS: critical revision of the manuscript for important intellectual content; approval of final manuscript.
BAV: study concept and design; critical revision of the manuscript for important intellectual content; approval of final manuscript.
KJ: study concept and design; literature grading; review and interpretation of data; drafting of the manuscript, critical revision of the manuscript for important intellectual content; approval of final manuscript.
Ethics Approval
No ethics approval was required for this publication.
Potential competing interest
None declared.
Financial Support
KJ has received research support from Janssen, AbbVie and adMare Bioinnovations (formerly the Center for Drug Research and development -CDRD). KJ has served on the advisory boards of Janssen, AbbVie, and Merck and participates in the speaker’s bureau for AbbVie and Janssen.
The remaining authors disclose no conflicts of interest.
Acknowledgements
K.J. is a Senior Clinician Scientist supported by the Children with Intestinal and Liver Disorders (CHILD) Foundation and the BC Children’s Hospital Research Institute Clinician Scientists Award Program, University of British Columbia. B.A.V. holds the CHILD Foundation Chair in Pediatric Gastroenterology. B.K.T. was supported by a Natural Sciences and Engineering Research Council of Canada Undergraduate Student Research Award (NSERC-USRA). J.A. is supported by a Canadian Institute for Health Research (CIHR)/Canadian Association of Gastroenterology and Michael Smith Foundation for Health Research (MSFHR) research fellowships.
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.ijid.2020.11.163.
Appendix A. Supplementary data
The following are Supplementary data to this article:
References
- Abdel-Mannan O., Eyre M., Löbel U., Bamford A., Eltze C., Hameed B., et al. Neurologic and Radiographic Findings Associated With COVID-19 Infection in Children. JAMA Neurol. 2020 doi: 10.1001/jamaneurol.2020.2687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anand P., Yadav A., Debata P., Bachani S., Gupta N., Gera R. Clinical profile, viral load, management and outcome of neonates born to COVID 19 positive mothers: a tertiary care centre experience from India. Eur J Pediatr. 2020:1–13. doi: 10.1007/s00431-020-03800-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balduzzi S., Rücker G., Schwarzer G. How to perform a meta-analysis with R: a practical tutorial. Evidence-Based Mental Health. 2019;22:153–160. doi: 10.1136/ebmental-2019-300117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belhadjer Zahra, Mathilde Méot, Fanny Bajolle, Diala Khraiche, Antoine Legendre, Samya Abakka, et al. Acute Heart Failure in Multisystem Inflammatory Syndrome in Children in the Context of Global SARS-CoV-2 Pandemic. Circulation. 2020;142:429–436. doi: 10.1161/CIRCULATIONAHA.120.048360. [DOI] [PubMed] [Google Scholar]
- Bellino S., Punzo O., Rota M.C., Del Manso M., Urdiales A.M., Andrianou X., et al. COVID-19 Disease Severity Risk Factors for Pediatric Patients in Italy. Pediatrics. 2020;146 doi: 10.1542/peds.2020-009399. e2020009399. [DOI] [PubMed] [Google Scholar]
- Bhumbra S., Malin S., Kirkpatrick L., Khaitan A., John C.C., Rowan C.M., et al. 2020. Clinical Features of Critical Coronavirus Disease 2019 in Children. Pediatric Critical Care Medicine. Publish Ahead of Print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biko D.M., Ramirez-Suarez K.I., Barrera C.A., Banerjee A., Matsubara D., Kaplan S.L., et al. Imaging of children with COVID-19: experience from a tertiary children’s hospital in the United States. Pediatr Radiol. 2020 doi: 10.1007/s00247-020-04830-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bixler D., Miller A.D., Mattison C.P., Taylor B., Komatsu K., Peterson Pompa X., et al. SARS-CoV-2-Associated Deaths Among Persons Aged <21 Years - United States, February 12-July 31, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1324–1329. doi: 10.15585/mmwr.mm6937e4. [DOI] [PubMed] [Google Scholar]
- Blumfield E., Levin T.L. COVID-19 in pediatric patients: a case series from the Bronx. NY. Pediatr Radiol. 2020;50:1369–1374. doi: 10.1007/s00247-020-04782-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brenner E.J., Ungaro R.C., Gearry R.B., Kaplan G.G., Kissous-Hunt M., Lewis J.D., et al. Corticosteroids, But Not TNF Antagonists, Are Associated With Adverse COVID-19 Outcomes in Patients With Inflammatory Bowel Diseases: Results From an International Registry. Gastroenterology. 2020 doi: 10.1053/j.gastro.2020.05.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brenner E.J., Ungaro R.C., Colombel J.F., Kappelman M.D. 2020. SECURE-IBD Database Public Data Update. covidibd.org. Accessed on November 9, 2020. [Google Scholar]
- Cai X., Ma Y., Li S., Chen Y., Rong Z., Li W. Clinical Characteristics of 5 COVID-19 Cases With Non-respiratory Symptoms as the First Manifestation in Children. Front Pediatr. 2020;8:258. doi: 10.3389/fped.2020.00258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caussy C., Wallet F., Laville M., Disse E. Obesity is Associated with Severe Forms of COVID-19. Obesity. 2020;28:1175. doi: 10.1002/oby.22842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chao J.Y., Derespina K.R., Herold B.C., Goldman D.L., Aldrich M., Weingarten J., et al. Clinical Characteristics and Outcomes of Hospitalized and Critically Ill Children and Adolescents with Coronavirus Disease 2019 at a Tertiary Care Medical Center in New York City. The Journal of Pediatrics. 2020;223 doi: 10.1016/j.jpeds.2020.05.006. 14-19.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- COVID-19 Map . 2020. Johns Hopkins Coronavirus Resource Center n.d. https://coronavirus.jhu.edu/map.html (accessed August 17, 2020) [Google Scholar]
- Cucinotta D., Vanelli M. WHO Declares COVID-19 a Pandemic. Acta Bio Medica Atenei Parmensis. 2020;91:157–160. doi: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Farias E.C.F., Pedro Piva J., de Mello M.L.F.M.F., do Nascimento L.M.P.P., Costa C.C., Machado M.M.M., et al. Multisystem Inflammatory Syndrome Associated With Coronavirus Disease in Children: A Multi-centered Study in Belém, Pará, Brazil. Pediatr Infect Dis J. 2020;39:e374–e386. doi: 10.1097/INF.0000000000002865. [DOI] [PubMed] [Google Scholar]
- DeBiasi R.L., Song X., Delaney M., Bell M., Smith K., Pershad J., et al. Severe Coronavirus Disease-2019 in Children and Young Adults in the Washington, DC, Metropolitan Region. The Journal of Pediatrics. 2020;223 doi: 10.1016/j.jpeds.2020.05.007. 199-203.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Defining Childhood Obesity . 2019. Overweight & Obesity | CDC.https://www.cdc.gov/obesity/childhood/defining.html (accessed August 19, 2020) [Google Scholar]
- Derespina K.R., Kaushik S., Plichta A., Conway E.E., Bercow A., Choi J., et al. Clinical Manifestations and Outcomes of Critically Ill Children and Adolescents with Coronavirus Disease 2019 in New York City. The Journal of Pediatrics. 2020;226 doi: 10.1016/j.jpeds.2020.07.039. 55-63.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ding Y., Yan H., Guo W. Clinical Characteristics of Children With COVID-19: A Meta-Analysis. Front Pediatr. 2020:8. doi: 10.3389/fped.2020.00431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diorio C., Henrickson S.E., Vella L.A., McNerney K.O., Chase J., Burudpakdee C., et al. Multisystem inflammatory syndrome in children and COVID-19 are distinct presentations of SARS–CoV-2. J Clin Invest. 2020:130. doi: 10.1172/JCI140970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong Y., Mo X., Hu Y., Qi X., Jiang F., Jiang Z., et al. Epidemiology of COVID-19 Among Children in China. Pediatrics. 2020:145. doi: 10.1542/peds.2020-0702. [DOI] [PubMed] [Google Scholar]
- Du H., Dong X., Zhang J., Cao Y., Akdis M., Huang P., et al. Clinical characteristics of 182 pediatric COVID‐19 patients with different severities and allergic status. Allergy. 2020 doi: 10.1111/all.14452. all.14452. https://doi.org/10.1111/all.14452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eghbali A., Shokrollahi S., Mahdavi N.S., Mahdavi N.S.A., Dabbagh A. COVID-19 in pediatric patients: A case series. 1. 2020;5:3–5. doi: 10.22037/jcma.v5i1.29690. [DOI] [Google Scholar]
- Fontana L., Eagon J.C., Trujillo M.E., Scherer P.E., Klein S. Visceral Fat Adipokine Secretion Is Associated With Systemic Inflammation in Obese Humans. Diabetes. 2007;56:1010–1013. doi: 10.2337/db06-1656. [DOI] [PubMed] [Google Scholar]
- Garazzino S., Montagnani C., Donà D., Meini A., Felici E., Vergine G., et al. Multicentre Italian study of SARS-CoV-2 infection in children and adolescents, preliminary data as at 10 April 2020. Eurosurveillance. 2020;25:2000600. doi: 10.2807/1560-7917.ES.2020.25.18.2000600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- García-Salido A., Leoz-Gordillo I., Martínez de Azagra-Garde A., Nieto-Moro M., Iglesias-Bouzas M.I., García-Teresa MÁ, et al. Children in Critical Care Due to Severe Acute Respiratory Syndrome Coronavirus 2 Infection: Experience in a Spanish Hospital. Pediatric Critical Care Medicine. 2020 doi: 10.1097/PCC.0000000000002475. Publish Ahead of Print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giacomet V., Barcellini L., Stracuzzi M., Longoni E., Folgori L., Leone A., et al. Gastrointestinal Symptoms in Severe COVID-19 Children. The Pediatric Infectious Disease Journal. 2020;39:e317. doi: 10.1097/INF.0000000000002843. [DOI] [PubMed] [Google Scholar]
- González-Dambrauskas S., Vásquez-Hoyos P., Camporesi A., Díaz-Rubio F., Piñeres-Olave B.E., Fernández-Sarmiento J., et al. Pediatric Critical Care and COVID-19. Pediatrics. 2020:146. doi: 10.1542/peds.2020-1766. [DOI] [PubMed] [Google Scholar]
- Götzinger F., Santiago-García B., Noguera-Julián A., Lanaspa M., Lancella L., Calò Carducci F.I., et al. COVID-19 in children and adolescents in Europe: a multinational, multicentre cohort study. The Lancet Child & Adolescent Health. 2020;4:653–661. doi: 10.1016/S2352-4642(20)30177-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guan W., Liang W., Zhao Y., Liang H., Zi-sheng Chen, Li Y., et al. Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis. European Respiratory Journal. 2020;55 doi: 10.1183/13993003.00547-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harman K., Verma A., Cook J., Radia T., Zuckerman M., Deep A., et al. Ethnicity and COVID-19 in children with comorbidities. The Lancet Child & Adolescent Health. 2020;4:e24–e25. doi: 10.1016/S2352-4642(20)30167-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoang A., Chorath K., Axel Moreira, Evans M., Burmeister-Morton F., Burmeister F., et al. COVID-19 in 7780 pediatric patients: A systematic review. EClinicalMedicine. 2020:24. doi: 10.1016/j.eclinm.2020.100433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan. China. The Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussain F.A., Njoku F.U., Saraf S.L., Molokie R.E., Gordeuk V.R., Han J. COVID-19 infection in patients with sickle cell disease. Br J Haematol. 2020;189:851–852. doi: 10.1111/bjh.16734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IntHout J., Ioannidis J.P., Borm G.F. The Hartung-Knapp-Sidik-Jonkman method for random effects meta-analysis is straightforward and considerably outperforms the standard DerSimonian-Laird method. BMC Medical Research Methodology. 2014;14:25. doi: 10.1186/1471-2288-14-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kainth M.K., Goenka P.K., Williamson K.A., Fishbein J.S., Subramony A., Barone S., et al. Early Experience of COVID-19 in a US Children’s Hospital. Pediatrics. 2020;146 doi: 10.1542/peds.2020-003186. e2020003186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaushik S., Aydin S.I., Derespina K.R., Bansal P.B., Kowalsky S., Trachtman R., et al. Multisystem Inflammatory Syndrome in Children Associated with Severe Acute Respiratory Syndrome Coronavirus 2 Infection (MIS-C): A Multi-institutional Study from New York City. The Journal of Pediatrics. 2020;224:24–29. doi: 10.1016/j.jpeds.2020.06.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leeb R.T. COVID-19 Trends Among School-Aged Children — United States, March 1–September 19, 2020. MMWR Morb Mortal Wkly Rep. 2020:69. doi: 10.15585/mmwr.mm6939e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Licciardi F., Giani T., Baldini L., Favalli E.G., Caporali R., Cimaz R. COVID-19 and what pediatric rheumatologists should know: a review from a highly affected country. Pediatric Rheumatology. 2020;18:35. doi: 10.1186/s12969-020-00422-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovinsky-Desir S., Deshpande D.R., De A., Murray L., Stingone J.A., Chan A., et al. Asthma among hospitalized patients with COVID-19 and related outcomes. Journal of Allergy and Clinical Immunology. 2020 doi: 10.1016/j.jaci.2020.07.026. S0091674920311003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ludvigsson J.F. Systematic review of COVID‐19 in children shows milder cases and a better prognosis than adults. Acta Paediatr. 2020 doi: 10.1111/apa.15270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mannheim J., Gretsch S., Layden J.E., Fricchione M.J. Characteristics of Hospitalized Pediatric Coronavirus Disease 2019 Cases in Chicago, Illinois, March–April 2020. Journal of the Pediatric Infectious Diseases Society. 2020 doi: 10.1093/jpids/piaa070. piaa070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mantel N., Haenszel W. Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst. 1959;22:719–748. [PubMed] [Google Scholar]
- McCloskey K.A., Meenan J., Hall R., Tsitsikas D.A. COVID-19 infection and sickle cell disease: a UK centre experience. Br J Haematol. 2020;190:e57–8. doi: 10.1111/bjh.16779. [DOI] [PubMed] [Google Scholar]
- Meslin P., Guiomard C., Chouakria M., Porcher J., Duquesne F., Tiprez C., et al. Coronavirus Disease 2019 in Newborns and Very Young Infants: a Series of Six Patients in France. The Pediatric Infectious Disease Journal. 2020;39:e145. doi: 10.1097/INF.0000000000002743. [DOI] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman D.G., Group T.P. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLOS Medicine. 2009;6 doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moraleda C., Serna-Pascual M., Soriano-Arandes A., Simó S., Epalza C., Santos M., et al. Multi-inflammatory Syndrome in Children Related to Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) in Spain. Clinical Infectious Diseases. 2020 doi: 10.1093/cid/ciaa1042. ciaa1042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moreno-Galarraga L., Urretavizcaya-Martínez M., Alegría Echauri J., García Howard M., Ruperez García E., Aguilera-Albesa S., et al. SARS-CoV-2 infection in children requiring hospitalization: the experience of Navarra, Spain. World J Pediatr. 2020;16:614–622. doi: 10.1007/s12519-020-00393-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munro A.P.S., Faust S.N. Children are not COVID-19 super spreaders: time to go back to school. Archives of Disease in Childhood. 2020;105:618–619. doi: 10.1136/archdischild-2020-319474. [DOI] [PubMed] [Google Scholar]
- Otto W.R., Geoghegan S., Posch L.C., Bell L.M., Coffin S.E., Sammons J.S., et al. The Epidemiology of Severe Acute Respiratory Syndrome Coronavirus 2 in a Pediatric Healthcare Network in the United States. Journal of the Pediatric Infectious Diseases Society. 2020 doi: 10.1093/jpids/piaa074. piaa074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oualha M., Bendavid M., Berteloot L., Corsia A., Lesage F., Vedrenne M., et al. Severe and fatal forms of COVID-19 in children. Archives de Pédiatrie. 2020;27:235–238. doi: 10.1016/j.arcped.2020.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parri N., Lenge M., Cantoni B., Arrighini A., Romanengo M., Urbino A., et al. COVID-19 in 17 Italian Pediatric Emergency Departments. Pediatrics. 2020 doi: 10.1542/peds.2020-1235. [DOI] [PubMed] [Google Scholar]
- Poli P., Timpano S., Goffredo M., Padoan R., Badolato R. Asymptomatic case of Covid-19 in an infant with cystic fibrosis. Journal of Cystic Fibrosis. 2020;19:e18. doi: 10.1016/j.jcf.2020.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riollano‐Cruz M., Akkoyun E., Briceno‐Brito E., Kowalsky S., Reed J., Posada R., et al. Multisystem inflammatory syndrome in children related to COVID‐19: A New York City experience. J Med Virol. 2020:26224. doi: 10.1002/jmv.26224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riphagen S., Gomez X., Gonzalez-Martinez C., Wilkinson N., Theocharis P. Hyperinflammatory shock in children during COVID-19 pandemic. The Lancet. 2020;395:1607–1608. doi: 10.1016/S0140-6736(20)31094-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robins J., Breslow N., Greenland S. Estimators of the Mantel-Haenszel Variance Consistent in Both Sparse Data and Large-Strata Limiting Models. Biometrics. 1986;42:311. doi: 10.2307/2531052. [DOI] [PubMed] [Google Scholar]
- Russo L., Lumeng C.N. Properties and functions of adipose tissue macrophages in obesity. Immunology. 2018;155:407–417. doi: 10.1111/imm.13002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sankar J., Dhochak N., Kabra S.K., Lodha R. COVID-19 in Children: Clinical Approach and Management. Indian J Pediatr. 2020;87:433–442. doi: 10.1007/s12098-020-03292-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz D.A., Mohagheghi P., Beigi B., Zafaranloo N., Moshfegh F., Yazdani A. Spectrum of neonatal COVID-19 in Iran: 19 infants with SARS-CoV-2 perinatal infections with varying test results, clinical findings and outcomes. The Journal of Maternal-Fetal & Neonatal Medicine. 2020:1–10. doi: 10.1080/14767058.2020.1797672. [DOI] [PubMed] [Google Scholar]
- Schwarzer G., Carpenter J.R., Rücker G. Springer International Publishing; 2015. Meta-Analysis with R. [DOI] [Google Scholar]
- Shekerdemian L.S., Mahmood N.R., Wolfe K.K., Riggs B.J., Ross C.E., McKiernan C.A., et al. Characteristics and Outcomes of Children With Coronavirus Disease 2019 (COVID-19) Infection Admitted to US and Canadian Pediatric Intensive Care Units. JAMA Pediatr. 2020;174:868–873. doi: 10.1001/jamapediatrics.2020.1948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi H., Han X., Jiang N., Cao Y., Alwalid O., Gu J., et al. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. The Lancet Infectious Diseases. 2020;20:425–434. doi: 10.1016/S1473-3099(20)30086-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simonnet A., Chetboun M., Poissy J., Raverdy V., Noulette J., Duhamel A., et al. High Prevalence of Obesity in Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) Requiring Invasive Mechanical Ventilation. Obesity. 2020;28:1195–1199. doi: 10.1002/oby.22831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Study Quality Assessment Tools . 2020. NHLBI, NIH. n.d.https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (accessed July 26, 2020) [Google Scholar]
- Sun D., Li H., Lu X.-X., Xiao H., Ren J., Zhang F.-R., et al. Clinical features of severe pediatric patients with coronavirus disease 2019 in Wuhan: a single center’s observational study. World J Pediatr. 2020;16:251–259. doi: 10.1007/s12519-020-00354-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swann O.V., Holden K.A., Turtle L., Pollock L., Fairfield C.J., Drake T.M., et al. Clinical characteristics of children and young people admitted to hospital with covid-19 in United Kingdom: prospective multicentre observational cohort study. BMJ. 2020:m3249. doi: 10.1136/bmj.m3249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sweeting M.J., Sutton A.J., Lambert P.C. What to add to nothing? Use and avoidance of continuity corrections in meta-analysis of sparse data. Stat Med. 2004;23:1351–1375. doi: 10.1002/sim.1761. [DOI] [PubMed] [Google Scholar]
- Szablewski C.M. SARS-CoV-2 Transmission and Infection Among Attendees of an Overnight Camp — Georgia, June 2020. MMWR Morb Mortal Wkly Rep. 2020:69. doi: 10.15585/mmwr.mm6931e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tagarro A., Epalza C., Santos M., Sanz-Santaeufemia F.J., Otheo E., Moraleda C., et al. Screening and Severity of Coronavirus Disease 2019 (COVID-19) in Children in Madrid, Spain. JAMA Pediatr. 2020 doi: 10.1001/jamapediatrics.2020.1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Team, R Core, and others . 2020. “R: A Language and Environment for Statistical Computing.” Vienna, Austria. [Google Scholar]
- van Bruwaene L., Mustafa F., Cloete J., Goga A., Green R.J. What are we doing to the children of South Africa under the guise of COVID-19 lockdown? SAMJ: South African Medical Journal. 2020;110:1–2. doi: 10.7196/SAMJ.2020.v110i7.14932. [DOI] [PubMed] [Google Scholar]
- Verdoni L., Mazza A., Gervasoni A., Martelli L., Ruggeri M., Ciuffreda M., et al. An outbreak of severe Kawasaki-like disease at the Italian epicentre of the SARS-CoV-2 epidemic: an observational cohort study. The Lancet. 2020;395:1771–1778. doi: 10.1016/S0140-6736(20)31103-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waltuch T., Gill P., Zinns L.E., Whitney R., Tokarski J., Tsung J.W., et al. Features of COVID-19 post-infectious cytokine release syndrome in children presenting to the emergency department. The American Journal of Emergency Medicine. 2020 doi: 10.1016/j.ajem.2020.05.058. S0735675720304034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wickham H., Averick M., Bryan J., Chang W., McGowan L.D., François R., et al. Welcome to the Tidyverse. Journal of Open Source Software. 2019;4:1686. doi: 10.21105/joss.01686. [DOI] [Google Scholar]
- Wu Z., McGoogan J.M. 2020. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese. [DOI] [PubMed] [Google Scholar]
- Yang J., Zheng Y., Gou X., Pu K., Chen Z., Guo Q., et al. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. International Journal of Infectious Diseases. 2020;94:91–95. doi: 10.1016/j.ijid.2020.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yayla B.C.C. 2020. Characteristics and Management of Children with COVID-19 in Turkey. Balkan Med J n.d.;37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zachariah P., Johnson C.L., Halabi K.C., Ahn D., Sen A.I., Fischer A., et al. Epidemiology, Clinical Features, and Disease Severity in Patients With Coronavirus Disease 2019 (COVID-19) in a Children’s Hospital in New York City, New York. JAMA Pediatr. 2020;174:e202430. doi: 10.1001/jamapediatrics.2020.2430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeng F., Huang Y., Guo Y., Yin M., Chen X., Xiao L., et al. Association of inflammatory markers with the severity of COVID-19: A meta-analysis. International Journal of Infectious Diseases. 2020;96:467–474. doi: 10.1016/j.ijid.2020.05.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng F., Liao C., Fan Q., Chen H., Zhao X., Xie Z., et al. Clinical Characteristics of Children with Coronavirus Disease 2019 in Hubei, China. CURR MED SCI. 2020;40:275–280. doi: 10.1007/s11596-020-2172-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhong J., Shen G., Yang H., Huang A., Chen X., Li Dong, et al. COVID-19 in patients with rheumatic disease in Hubei province, China: a multicentre retrospective observational study. The Lancet Rheumatology. 2020 doi: 10.1016/S2665-9913(20)30227-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z., et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. The Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmermann P., Curtis N. Coronavirus Infections in Children Including COVID-19: An Overview of the Epidemiology, Clinical Features, Diagnosis, Treatment and Prevention Options in Children. The Pediatric Infectious Disease Journal. 2020;39:355–368. doi: 10.1097/INF.0000000000002660. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.