Abstract
Background
Emergencies and disasters are major threats to health care systems. Coronavirus Disease 2019 (COVID-19) is at the center of a recent emergency situation that requires increased attention from health care professionals, including pharmacists. This study was aimed at providing an overview of pharmacists’ roles in disasters and formulating a definition of expected roles and tasks through which they can perform these roles properly.
Methods
A systematic review was conducted utilizing a literature search performed on the Medline, EMBASE and PubMed databases. The last search occurred on 14 July 2020. Data were extracted and recorded on a data extraction sheet by the reviewers, then categorized using the prevention, preparedness, response, and recovery (PPRR) model. Study quality was evaluated using the Critical Appraisal Skills Program (CASP) checklist.
Results
Fifteen articles addressing pharmacists’ roles in disasters were included. Of these, three addressed pharmacists’ roles during the COVID-19 pandemic. Pharmacists’ roles in the prevention of emergencies, including COVID-19, are focused on chronic disease medication supply and education. Regarding pharmacists’ preparedness to perform their roles in disasters, they were more focused on health policy and population health planning, especially regarding the COVID-19 pandemic. Direct patient care continues to support patients through medication availability, and pharmacists’ clinical roles are examples of their response to disasters. In addition, pharmacists have an important role in disaster recovery that involves several activities, such as restocking emergency kits and reestablishing normal stock. Studies were generally of a reasonable quality. However, some limitations were noted among studies, and higher quality studies that contribute to existing knowledge are needed.
Conclusion
Health care systems’ utilization of pharmacists’ new roles can result in a well-prepared disaster response, as observed during the COVID-19 pandemic. Pharmacists’ engagement in decision-making processes and adequate demonstration of pharmacists’ nontraditional roles in the literature can facilitate the health care community’s acceptance of such roles.
Keywords: COVID-19, Disasters, Emergency, Pharmacist, PPRR
Abbreviations: PPRR, Prevention, preparedness, response and recovery risk management model
1. Introduction
People worldwide face health emergencies and disasters and suffer the repercussions associated with them. According to the World Health Organization (WHO, 2019), natural and technological hazards from emergencies impact approximately 190 million people directly, leading to more than 77,000 deaths annually. Another 172 million people are affected by conflicts. Furthermore, the WHO recorded 1200 outbreaks in 168 countries during the period 2012–2017, taking into account new or reappearing infectious diseases (WHO, 2019).
In 1918, the H1N1 virus caused an influenza pandemic that the Centers for Disease Control and Prevention (CDC) described as the harshest and most severe pandemic in recent history. It is estimated that this virus infected approximately one-third of the world’s population and caused more than 50 million deaths worldwide (CDC, 2019).
Furthermore, an additional 352 infectious disease events were tracked by the WHO in 2018. This includes the Middle East respiratory syndrome coronavirus (MERS-CoV) and Ebola virus disease (WHO, 2019).
The term “disaster” encompasses a wide range of events, including natural disasters such as infectious disease outbreaks, antimicrobial resistance, and unsafe food and water; human-made disasters such as conflicts, chemical and radiation disasters, structural collapses, transportation accidents, water and power supply shortages, and air pollution; and environmental disasters such as climate change and its consequences (WHO, 2019).
Recent catastrophic disasters and extreme events have aroused people’s interest in disaster and crisis management. Currently, Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) has caused many casualties, both in terms of clinical complications and its effects on many countries’ economies, causing fears of an economic depression. In early March 2020, COVID-19 was declared an international concern and a pandemic (WHO, 2020a). In addition, by 9 May 2020, the WHO reported that confirmed cases exceeded three million eight hundred thousand worldwide, with over two hundred sixty thousand deaths (WHO, 2020b). Such a crisis demands that key personnel play more nontraditional roles.
During a disaster, health can be affected severely for various reasons, including the performance of health care professionals and their responses to unexpected challenges. Pharmacists are communities’ most accessible health professionals, so they are in a unique position to help patients affected by disasters. Over the years, pharmacists have become known as prescription checkers and medication dispensers. As critical these roles are, however, the unique situations disaster create require pharmacists to play nontraditional roles involving decision-making in therapeutic protocols; extended authority for clinical pharmacists in hospitals; and additional services provided in community pharmacies such as administering vaccinations, medication mail delivery, and pharmaceutical care for people affected by the disaster. Hence, a proper definition of pharmacists’ roles during disasters is essential, but pharmacists’ roles in disaster health management remain formally unacknowledged.
This systematic review is aimed at providing an overview of pharmacists’ roles during disasters and formulating a definition of their expected roles and tasks through which they can perform these roles properly.
2. Materials and methods
2.1. Search strategy
A literature search was conducted using the Medline, EMBASE, and PubMed databases. The search strategy involved terms related to pharmacists’ roles, disaster, COVID-19, and SARS-CoV-2.
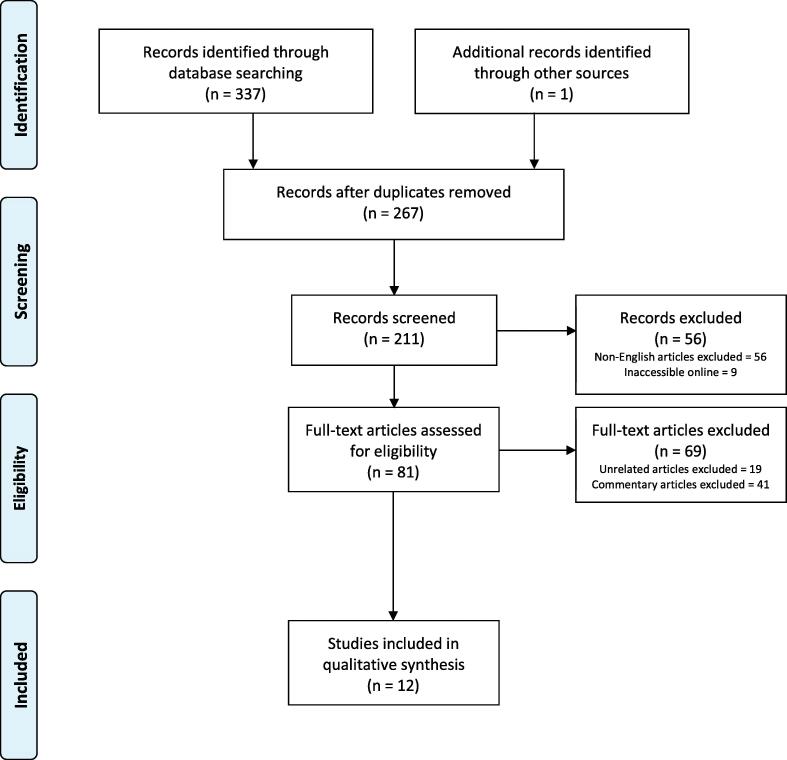
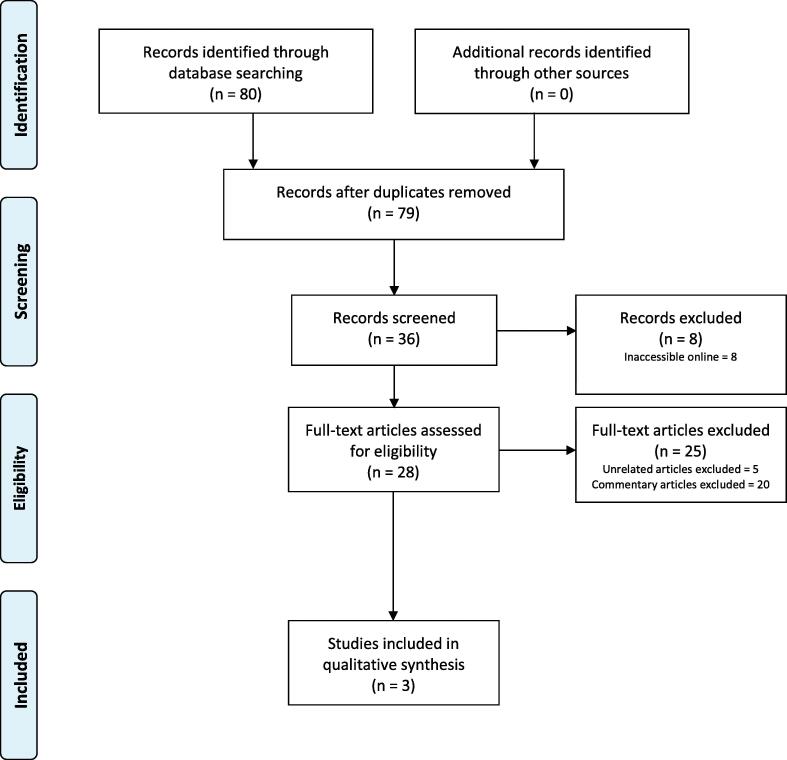
The search involved a combination of medical subject headings (MeSHs), and a search using keywords related to pharmacists, pharmacists’ roles and disaster was conducted first (Fig. 1). Another search using the keywords ‘pharmacist,’ ‘pharmacist role,’ and ‘COVID-19 or coronavirus’ was performed to retrieve as many articles related to both topics as possible (Fig. 2).
Fig. 1.
PRISMA flow chart. Pharmacist’s role in disasters.
Fig. 2.
PRISMA flow chart. Pharmacist’s role in COVID-19.
The included papers were quantitative or qualitative studies that analyzed pharmacists’ roles across all areas related to health care and patient management during disaster and during the COVID-19 pandemic. Non-English articles and commentary articles were excluded from the study. The last search was performed on 14 July 2020.
The prevention, preparedness, response, and recovery (PPRR) model was adopted (Disaster Management, 2018, Watson et al., 2019a); this model is a comprehensive approach to disaster management that ensures a balance between risk reduction and the enhancement of community adaptability and recovery. The model consists of four phases:
-
•
Prevention: Any regulatory and physical measures that ensure the prevention of emergencies or the amelioration of their effects
-
•
Preparedness: Any development of plans or arrangements in the full spectrum of disaster management phases based on risk assessments
-
•
Response: Appropriate response measures intended to minimize an event’s effects
-
•
Recovery: Actions taken to rapid restore and re-establish essential services
2.2. Eligibility criteria and study selection
Studies conducted to examine or report the role of pharmacists in disasters, particularly the COVID-19 pandemic, were included and deemed eligible for this review. The studied population could have been community pharmacists, hospital pharmacists, patients, those involved in the field of disaster health, or any combination of the above. Only English studies were included in the review.
Studies that did not directly address pharmacists’ roles in disasters were excluded. Commentary articles were excluded because these depend on the author or authors’ point of view. Partially available reported studies (e.g., abstracts, forms, or articles that were inaccessible online) were excluded, as were non-English studies. The two authors independently reviewed the titles and abstracts of the research findings that met the above MeSHs and keywords. The reviewers agreed to exclude articles that did not meet the aforementioned eligibility criteria, whereas those that met the eligibility criteria based on both reviewers’ assessments were included for full paper review. Full articles were reviewed independently by each reviewer against the inclusion and exclusion criteria. In case of disagreement between the two reviewers, a third reviewer who was an expert in clinical work and research was asked to review the disagreement between the two authors. However, there were no disagreements between the reviewers during the review process.
2.3. Data extraction and quality assessment
The reviewers extracted and recorded data individually on a tailored data extraction sheet. Key information such as study design, population of concern, exposure of concern, outcomes of concern, and main findings was extracted (Table 1).
Table 1.
The included articles in the systematic review with their information. .
| Author (Year) | Country | Study Design/Type | Population | Exposure | Outcomes of Interest (PPRR) | Main Findings |
|---|---|---|---|---|---|---|
| Ford et al. (2013) | USA | Review article | Articles on pharmacists’ role in disasters in peer-reviewed pharmacy journals | • Cold War-era disasters (1960–December 1991) • Post-Cold War/Preterrorism era (January 01, 1992–September 30, 2001) • Terrorism era disasters (October 01, 2001–present) |
Response | The review stated that pharmaceutical supply outweighs other roles among role reports Certain natural disasters, from regression modeling, significantly elucidate pharmacists assuming disaster roles. Pharmacists assuming roles in patient management is significantly explained by tornados and hurricanes (P = 0.0403, P = 0.0281, respectively). Decreases of 14 and 13% were noted in patient management role references for every tornado and hurricane reference, respectively (Incident rate ratios (IRR) = 0.86, IRR = 0.97, respectively). Pharmacists assuming roles in response integration significantly explained by hurricane reports (IRR = 0.96, P = 0.0138). A decrease of 4% was noted in response integration role references for every hurricane reference. Pharmacists assuming roles in policy coordination or pharmaceutical supply was not significantly explained by natural disasters. Pharmacists’ roles were also significantly explained by chemical, biological, radiological, nuclear, and explosive (CBRNE) disasters. Two categories of CBRNE disasters, radiologic dispersal devices (RDD) and nuclear terrorism, significantly explained pharmacists assuming roles in policy coordination (IRR = 0.63, P = 0.1015, IRR = 2.1, P = 0.0052, respectively). A decrease of 37% was noted in policy coordination role references for every one RDD reference increase and an increase of 110% in policy coordination references for every one nuclear terrorism reference increase. |
| Alkhalili et al. (2017) | Canada | Descriptive | Published literature describing pharmacists’ experiences in responding to or preparing for both natural and manmade disasters | (1) Planning and preparation (2) Early/acute response (3) Recovery |
Preparedness, Response, Recovery | Phase 1: The study composed a framework from a total of 505 work activities to defining the role of pharmacists in response to and in preparedness for disasters. Of work activities extracted, medical supply functions accounted for 41.2% of activities, and the remaining (n = 297) were categorized in 5 thematic areas: professional practice, population health planning, direct patient care, legislation, and communications. Phase 2: Development of a classification scheme for pharmacy personnel. By using this scheme, four categories of pharmacy personnel were defined. Distinctions between the different types of personnel were made by considering the 5 characteristics; 1) level of education; 2) experience/practical training; 3) skills not related to pharmacy; 4) dispensary tasks; and 5) level of self-government and autonomy in conducting pharmacy-related activities. Phase 3: Defining Roles and Responsibilities (Role-Mapping) The number of activities was relatively balanced through preparation for disaster, response during disasters and recovery from disasters. Personnel with primary responsibility in categories 1 and 2, carried out over the period of the emergency’s response phase, had a smaller number of activities. Conversely, personnel in category 3, during the course of the emergency response, carried out more activities, whereas personnel in category 4 carried out specialized, narrow roles. |
| Watson et al. (2019b) | Canada | Cross-sectional | 222 participants at the World Association for Disaster and Emergency Medicine’s 20th Congress in Toronto, Canada | Emerging roles of pharmacists in disasters | Preparedness, Response | Most of the respondents deemed pharmacists to have an additional role other than logistical support and supply management in disasters (96.8%, n = 122/126). A total of 87.9% believed that pharmacists’ current range of practice involved providing support in disasters. Almost half of respondents were aware of pharmacists participating in roles such as CPR, first aid/wound care roles, triaging and screening (57.1%, 68/119). Themes Identified for Pharmacists’ Roles in Preparing and Responding to Disasters Preparing for a Disaster Education, inventory management, logistical support, and vaccinations Responding to a Disaster Logistical support, medication supply, medication management, participation in disaster teams, vaccinations, education. The two main barrier themes to pharmacists being involved in disasters identified by the respondents (n = 95) were lack of comprehension of pharmacists’ value in disasters and other healthcare professionals’ biases. |
| Watson et al. (2019a) | Australia | Cross-sectional, a Delphi study | Expert panel of key opinion leaders within the field of disaster health | Pharmacists’ roles in disasters | PPRR | The study (Watson et al., 2019a) prioritized the top five pharmacists’ roles during each phase in disasters by reaching a consensus by panel of experts (n = 15). Prevention phase: enhancing chronic disease management through accommodating point of care and ensuring medication supplies, vaccination, public education on infection control and disasters’ influence on increasing the risk of adverse health outcomes Preparedness phase: ensuring essential medications procurement, having an approach to secure cold chain lines, participating in local community disaster management teams, knowledge about national stockpiles, and participating in local/state/national disaster preparedness efforts. However, consensus was not reached on developing CBRN (chemical, biological, radiological and nuclear) weapons preparedness educational tools, including signs and symptoms and drug treatments for health professionals. Response phase: dispensing, counseling, logistical support of supplies for patients with chronic diseases, medication emergency supply refills, and national stockpiles issuing and distribution. However, consensus was not reached on the following roles: altering existing therapeutic regimens where clinically necessary and offering psychological health support following a disaster. Recovery phase: restoring normal stock levels and discarding contaminated stock properly, emergency/disaster kit refills, promoting local community health, detecting and prioritizing at-risk populations, and retrieving patients and drug records if compromised |
| Jiménez-Mangual et al. (2019) | Puerto Rico | Cross-sectional | Community pharmacy patients | Hurricane Maria in Puerto Rico | Response | The study reported patients’ thoughts on the role of community pharmacists (n = 65). Access to medications from the pharmacy was the topmost medication need among participants (35.4%). Of sixty-five respondents after Hurricane Maria, (47.7%) lacked access to medications at a minimum of 1 day, and over half proceeded to lack access to medication between 1 and 7 days. Difficulty in getting in touch with the pharmacy was the most commonly noted reason to lack access to medications. Vast majority (78.5%) noted medication-related issues, and following the hurricane, almost half (47.7%) reported difficulties in getting in touch with or getting to their pharmacy. Medication supply, counseling, and counseling regarding storing medications were the top pharmacist-provided services throughout the disaster (83%, 24.6%, 23%, respectively) . Patients’ impressions about the role of pharmacists during disasters included medication supply, counseling, providing their prescription medication records, and counseling on over-the-counter products and self-care during disasters (92.3%, 73.8%, 63%, 63%, respectively). Most patients noted that pharmacists provided help in solving medication-related problems (86.2%) and that pharmacists were willing to offer help and were trustworthy (97%, 95.4%, respectively). |
| Austin et al. (2007) | Canada | Cross-sectional | Pharmacists in a direct-patient care setting | The severe acute respiratory syndrome (SARS) outbreak and the electrical system failure “blackout” | Preparedness, Response | A total of 27 pharmacists were interviewed for this study. Five key themes emerged from this research: (1) During times of crisis, pharmacies are among the first-line health care facilities: Large increases in patients and severity and acuity levels of cases presented to pharmacies were reported by participants. (2) “A Vacuity of Leadership/Lack of Utility of Emergency Preparedness Guidelines and Policies”: During the SARS outbreak, the lack of comprehension of the disease, disorganization and poor communication from public health officials resulted in individuals searching for leadership at a local level. “Emergency preparedness training” was provided to several participants, ranging from fulfillment of reading requirements of guidelines and policies to workshops and lecture-based training. Participants also noted that attained knowledge and skills from such training appeared to be of limited applicability in assisting them in adapting to these crises. (3) Dependence on experience and professional judgment and their role: Individuals were obligated to make “microjudgments” in the environment where time is limited due to the sensitivity and the complicated professional practices in the best case scenario possible. Dispensing and practice management skills were arguably overlooked as a result of emphasizing clinical skills and problem solving in pharmacy education. Newer graduates found it more challenging to cope during disasters because of the lack of a solid basis in drug distribution systems management. (4) Significance of Documentation: Pharmacists participated in risky behavior that is ambiguous in medical and legal aspects due to the crisis. As crises continued, flaws and defective documentation systems were observed to be problematic to pharmacists over time. (5) “Teamness” During Times of Crisis: A determinant of successful coping with disasters was the degree of “teamness” that existed before the disaster ensued. The literature on team effectiveness has demonstrated the importance of teamwork, particularly in high-stress, highly ambiguous situations. Characteristics of high-performing teams include role flexibility, fluid boundaries, sense of shared purpose, and lack of rigid hierarchy. A key finding of this study suggests that a determinant of successful adaptation to both the SARS and blackout situations was the level of “teamness” that existed before the crisis erupted. Efficient teams are characterized as having role adaptability, fluid boundaries, a sense of common goals and aims, and flexible hierarchy. |
| Chin et al. (2004) | Canada | Review article | Pharmacy-related events and tasks | Two SARS crises that occurred in Toronto from March–June 2003 | Response | In a direct-patient care setting, pharmacists performed several tasks that were categorized into five categories: 1-Drug Information: Except for ribavirin, due to the lack of research in patients with SARS, guidelines were developed for antimicrobial intravenous administration. However, guidelines for ribavirin were assumed to be the pharmacist’s responsibility concerning oral and intravenous preparation and administration, renal impairment dosage adjustment and monitoring. For interferon alfacon-1, which was an investigational drug, pharmacists assumed responsibility of developing guidelines. SARS drug kits that offered dosing information on Ribavirin and multiple other antimicrobial agents, Ribavirin guidelines in both normal and renally impaired patients, and management algorithms for SARS were created, kept updated, and stored in the emergency department. Nebulizers were limited to all hospital patients, thereby minimizing other sources of SARS spread. A chart for conversion between nebulizer dosing and metered-dose inhalers was created by drug information pharmacists. 2-Direct Patient Care: Under the stressful conditions and the meticulous infection-control precautions, pharmacists proceeded to offer direct patient care for SARS patients. Investigational tests and direct communication between health care providers and the patients were minimized. For SARS patients, pharmacotherapy end points were monitored in modified plans compared to those used with normal patients. Weighing risk versus benefits, counseling and side effects monitoring were required during the use of investigational agents. 3-Pharmacy Operations: To transfer drugs between areas and for drugs to be returned and recycled in the pharmacy department, new procedures were provided. Entering SARS-designated areas was kept to a minimum, and unit-dose cart and ward restocking were assigned to specified pharmacy technicians. Intubation kits for SARS patients were established, and in case of use, all remainders of the kit were discarded in biohazard waste. Moreover, a designated cart for cardiopulmonary arrest codes was established. After the code, all remainders of the cart were discarded in a biohazard bag and sent for decontamination. Reminders for the staff for the new procedures were on auxiliary labels. Special Access Program, Health Canada (SAP) was utilized by drug information and research pharmacists for the procurement of ribavirin and interferon alfacon-1. 4-Collaboration and Communication: A multidisciplinary approach was taken to complete urgent tasks efficiently. Pharmacists collaborated closely with key partners and stakeholders. Treatment information was provided in a SARS binder. 5-Personnel Management: Staff were educated and deployed to high-demand areas, and situations were managed innovatively. A multidisciplinary SARS tertiary acute response team that involved pharmacists was created upon the second SARS disaster. |
| Nazar and Nazar (2020) | United Kingdom | Cross-sectional | Pharmacists involved in the humanitarian field based in England | Humanitarian field and emergency response situations | Preparedness |
Nazar and Nazar (2020) identified four descriptive themes to explore the experiences and preparedness of humanitarian pharmacists (n = 12) in response to an emergency. 1-Training and preparation Since the actuality of humanitarian crises cannot be fully predicted, no amount of training is assured to fully prepare pharmacists. Pharmacists found the most effective training for deployment preparedness to be simulation training concerning culture and existing resources and was best introduced through hospital pharmacy-based experience. All deployed participants stated that most of their learning was attained during their employment and that limited predeployment training contributed to a staggering sense of unreadiness in deployed areas. The need to have good knowledge of the culture and resources of the environment to be deployed to was expressed by most participants. 2- Required Skills Inventive and creative working, consultation skills, leadership, self-reliance and firmness in skills required to have during disasters. 3-Challenges/barriers Since humanitarian pharmacy is usually associated with medical logistical resources and support, vague roles and misunderstanding of pharmacists’ roles were reported as a result. Moreover, humanitarian organizations enlist staff through pursuing specific training and/or experience requirements, which are considered rare opportunities. 4-Profession development Pharmacists noted assertiveness in working in high-pressure environments resulting from their experiences in deployment, which also contributed to improving cultural knowledge and analytical thinking. |
| Ford et al. (2014) | USA | Review article | Pharmacy literature | Pharmacists’ roles in disasters | Response | The study reported a decreasing trend in weighted counts of patient management, followed by pharmaceutical supply pharmacist role reports and policy coordination categories in all journals. Weighted counts were analyzed using chi-square goodness-of-fit analysis. The results of analysis for pharmacists’ roles in response integration, pharmaceutical supplies, patient management, and policy coordination showed very significant differences between these roles (P < 0.001). Role categories were found to be unequally proportioned through sampled journals (P = 0.002). In the AJHP, pharmaceutical supply roles predominated other roles; however, they were emphasized to a lesser extent in other journals. In the JAPHA, commonly reported roles are patient management roles. Other possible pharmacists’ roles, policy coordination and response integration, were not emphasized to a great degree in sampled journals. Differences did not reach statistical significance in natural disasters-weighted counts (P = 0.358). The leading natural disaster recorded was hurricanes. In the sample articles, other natural disasters were not recorded, such as floods, earthquakes, and fires. In CBRN disasters, biological disasters were the leading role noted in the pharmacy journals, where documented CBRN disaster proportions were significantly different (P < 0.001). |
| Armitstead and Burton (2006) | USA | Descriptive | Licensed pharmacists | Training program for counterterrorism and disaster response | Preparedness | In the training program for Kentucky’s licensed pharmacists, (4.7%) were certified. In pre- and posttest results, a significant improvement was noted in knowledge in bioterrorism training for pharmacists trained in the period between February and August 2005. As a result of the training program, trained pharmacists in bioterrorism established a network for the state that provided name, address, and contact details of each participant to be used as first responders during bioterrorism disasters. |
| Awad and Cocchio (2015) | USA | Cross-sectional | Hospital pharmacy directors or representatives | Mass casualty scenarios | Preparedness | Most respondents are practicing in community-based hospitals (66%). Most institutions have not been classified as trauma centers (64.7%). Estimated numbers of beds and visits to emergency departments each year varied considerably among institutions. Among institutions, centralized pharmacies were common in (94.1%, 16/17), as was having a clinical pharmacist in the institution (76.5%, 13/17). Survey respondents (n = 18) indicated that they have institutional protocols for disaster preparedness at their facility, and (55.5%) had pharmacy department plans. Most respondents (55.5%) were doubtful about essential medication supplies in their hospitals. Of respondents, (27.7%) agreed to have hospitalized patient care plans during disasters for the pharmacy department, and (22.2%) agreed that the medication supply was adequate for both patients and employees. National or international guidelines determined the medication stock (16.6%). Eight participants reported on medication-stockpiling expense payments, (62.5%) reported that the medication stockpiling budget was considered in the pharmacy department budget. Eight participants reported on disaster drill frequencies. Disaster drills were conducted every six months in half of respondents’ facilities with annual disaster drills in (37.5%). |
| Watson et al. (2020) | Australia, Canada, UK, US and New Zealand | Review | Pharmacy legislation specific to disasters | Disasters | Preparedness | Disaster-specific pharmacy legislations in Australia, Canada, the UK, the US and New Zealand were reviewed. Specifically, four aspects were noted: the everyday emergency supply rule (3-day supply), emergency supply rule specific to disasters (greater than3-day supply), the vaccination rule in disasters and the mobile pharmacy rule. International legislation comparison: In (74.3%) of international pharmacy legislations, the everyday ‘3-day emergency supply’ rule was established. In only (41.9%) of cases, this rule was prolonged to account for state-declared disasters. In (15.1%) of international legislations, disaster-specific vaccination rules were implemented that declared applicability in disasters to not limit pharmacists practicing in disasters. In (23%) of international legislations, a legislation for mobile pharmacy was found. An association between everyday emergency supply legislation and a disaster-specific extension of the legislation existed (P = 0.007). Disaster-specific emergency supply legislation was found to have a relationship with disaster-specific vaccination legislation but not with mobile pharmacy legislation (Fisher’s exact test, P = 0.04, P = 0.21, respectively). Effects of disasters on pharmacy legislation: There were six models in total. The number of disasters over periods of 5 and 10 years and its association with pharmacy legislations specific to disasters were examined using a generalized estimating equation (GEE) binary logistics regression. Six models resulted. Significant associations between disaster-specific emergency supply were suggested in models 1 and 2 in both the 5- and 10-year periods. A country with a 10-year period increasing number of disasters had a 1.58-fold greater likelihood of having a disaster-specific emergency supply legislation, as suggested in model 1 (odds ratio (OR) 1.58; 95% confidence interval (CI) 1.14–2.19; P < 0.01). These odds rise to 1.78-fold more likely in a 5-year period, as suggested in model 2 (OR 1.78; 95% CI 1.58–2.01; P < 0.01). A significant association between the number of disasters in a 5-year period (2013–17) and mobile pharmacy legislation was proposed in model 6. This supports the statement of an increase in the number of disasters increasing the odds of mobile pharmacy legislation 1.05-fold (95% CI 1.01–1.09; P = 0.01). |
| Zheng et al. (2020) | China | Descriptive | Community pharmacies | COVID-19 | Prevention, Preparedness, Response | The study gathered and summarized the experience of community pharmacies during COVID-19 pandemic. Recommendations and guidance on providing pharmaceutical care: Pharmacy management Operations were actively modified in accordance with characteristics of the COVID-19 pandemic and patients’ needs. -Securing medication supply and products for COVID-19 prevention: Securing supply was thought of as a priority during the pandemic. Community pharmacists provided appropriate pharmaceutical product stock to comply with suggestions of FIP’s “Information and interim guidelines for pharmacists and the pharmacy workforce” during COVID-19. Medication purchases and delivery services real-time information were exchanged between community pharmacies to support chronic disease patients’ medication supply. Online consulting services and drug supply information were also provided through mobile apps or online. Medication supplies for cancer patients, and patients with hepatitis and irritable bowel disease were ensured through cooperation of pharmacies with drug companies. -Securing safety and efficiency of operations: Safety and efficiency of operations secured through suitable environment control staff protection and implementing emergency plan was another approach taken to prevent COVID-19. National or local regulations were followed to clean and disinfect the environment. PPE was provided to all staff for protection. Emergency plans and protocols were established alongside new pharmacy workflows for the management of COVID-19 and potential drug shortages. -Staff training: New workflow and emergency plans guidance were provided to Chinese community pharmacies staff. Staff training that ensured adequate knowledge on COVID-19 prevention was provided. Staff were also provided with training on the diagnosis and treatment of COVID-19. Pharmaceutical care services -Guiding principles of providing pharmaceutical care: Pharmaceutical care services provided principles of having COVID-19 prevention and control and safe medication use as an ultimate goal. To accomplish such goals, patients’ visits to pharmacy or any medical institutions were reduced. Pharmacies offered pharmaceutical care services that catered to patient population characteristics of their surrounding communities. -Approaches to provide PC: In addition to regular drug dispensing and patient education, online access to pharmacies through mobile apps and home delivery was considered among the approaches to minimize unnecessary pharmacy visits. Such approaches were publicized via flyers, internet notifications and text messages or emails. The model of community pharmacy services during the COVID-19 pandemic 1. Drug dispensing, patient screening and referrals A cooperative relationship was established between surrounding community pharmacies fever clinics and designated COVID-19 medical institutions to share mutual patients’ information. Suspected patients were identified by pharmacists based upon clinical symptoms (e.g., fever, cough, fatigue) and epidemiological history (e.g., travel to Wuhan city or its surrounding areas over the last 14 days). Medication reconciliation and consultation were provided by pharmacists. Home care guidance was provided to patients on home isolation. Community pharmacists focused and provided consultation on emotional situations and self-protection for patients. Therapeutic substitution was considered in case of medication shortage. 2. Chronic disease management Chronic disease patients were actively offered guidance on management to enhance medication adherence and support self-monitoring for medications’ safety and effectiveness. Patients were also advised to minimize unnecessary hospital visits. Additionally, patients were advised to check their medications expiration dates before taking them and to avoid expired medications in case of drug shortages or to avoid visits to pharmacies. Pharmacists promoted home delivery of medication to patients during the pandemic. Common adverse effects of medications and distinguishing the severity and need for medical intervention were taught to patients, along with what side effects they should monitor during their home stay. Cancer patients, irritable bowel disease or other special chronic disease patients, or patients on chronic use of a high-risk medication were offered additional guidance on the basis of their diseases or medications and were grouped using mobile apps to provide such services online. 3. Safe use of infusions Unnecessary infusions were avoided. Infusion services’ safety operation processes listed a set of strategies. Environment cleaning and disinfection, patient screening before entering the premises, reducing patient numbers to a limit, and practicing social distancing among patients were some of the strategies implemented. Community pharmacists aided infusion services care teams in establishing safety operation processes and providing regular pharmacy services. 4. Patient education Community pharmacists provided patient education and consulting services on COVID-19 prevention, early identification, and appropriate medication use. Education covered mask selection and proper use, hand and respiratory hygiene, disinfectant selection and safe use, and self-care and protection strategies. The current lack of an effective vaccine for prevention or a treatment for COVID-19 was also clearly explained to patients. Patients were provided with basic COVID-19 knowledge, particularly regarding symptom onset, routes of transmission and instructions to avoid blind use of medications. Young patients with no comorbidities and only upper respiratory symptoms were advised to be observed and isolated at home and for symptomatic treatment be given if needed. Patients were also directed to seek medical attention and comply with the treatment plan of their physician. Patients were educated on the common cold, flu and COVID-19 and how to differentiate between them and when to seek medical attention 5. Home care Pharmacists also referred to the WHO published guidelines for home care. The home environment should be prepared, cleaned and disinfected properly to comply with WHO guidelines. Isolated patients and related family members were educated on the importance of prevention and were able to implement such skills 6. Psychological support Pharmacy staff identified patients with psychological stress due to the pandemic situation (e.g., excessive anxiety, concern, fear) or blind optimism and provided psychological or emotional support for such patients, or they were referred to a psychiatrist if needed. Patient populations were educated to understand the COVID-19 pandemic properly and to view the situation in a positive light. Regular work and exercise were also promoted to the public. |
| Meghana et al. (2020) | India | Cross-sectional | Pharmacy Professionals | COVID-19 | Preparedness, Response |
The study conducted an online survey of pharmacy professionals (PP) (n = 24) regarding COVID-19 emergency preparedness and operations management. Eighty-three percent of respondents reported having a perceived preparedness for COVID-19. Additionally, (83%) of respondents reported having an adequate supply of PPE for the protection of pharmacy staff. Of respondents, (87.5%) were knowledgeable on the selection and use of masks. Respondents (41.7%) also prepared and distributed patient communication materials. COVID-19 emergency training was given by the organization to respondents (66.7%). Of those who underwent training, (87%) stated that the training was held for 1–3 h. Pharmacy professionals emphasized social distancing and isolation as infection control strategies and noted a rise in the demand for the antimalarial drugs hydroxychloroquine and chloroquine and in the demand for azithromycin and other antivirals. However, an increase in prices was not reported. Patients were screened for fever, cough, and emotional and anxiety issues (67%, 42%, 33%, respectively) by pharmacy professionals. Pharmacy professionals noted difficulties in procuring hydroxychloroquine, chloroquine, and azithromycin (20.8%) and cooperated with other pharmacies for the procurement of medications and supplies (25%). |
| Bahlol and Dewey (2020) | Egypt | Cross-sectional | Community pharmacists | COVID-19 | Preparedness | The study conducted a survey on community pharmacists’ preparedness in COVID-19. High awareness of hygiene practices, recent travel abroad risk, importance of coming into contact with infected cases, and COVID-19 symptoms was reported in respondents (97.6%–99.2%). Ninety-one percent of respondents knew all 10 possible symptoms COVID-19. Suspected COVID-19 cases were reported by (8.8%) of respondents, and (62.9%) of respondents who reported cases did not receive any pandemic training. Pharmacy staff adopted most of the recommended behaviors to prevent COVID-19 spread (up to 99.5%), except for minimizing nonessential staff (85.7%). Staff with chronic diseases or any other medical risk were informed to take a leave (Center = 91.5%, North = 97.2%, South = 97.8% and East = 97.3%; P = 0.004). Better availability of hand sanitizers, disinfectants, thermometers, face masks, antipyretic drugs, cold formulations, and disposable gloves was reported and compared to alcohol availability. However, free hand sanitizers and masks were less available for customer use (62.1%, 86.5%, respectively). Of pharmacies, (39.1%) had antimalarial drugs available. For symptomatic patients, separated areas for service and special waste disposal measures were less adopted by pharmacies (64%, 80.4%, respectively). Card payment machine availability among regions was significantly different (Center = 42.1%, North = 24.5%, South = 35.5% and East = 30.7%; P < 0.001). A significant difference was also noted in home delivery services among regions (Center = 67.1%, North = 41.0%, South = 44.1% and East = 48.0%; P < 0.001). Verbal customer education was noted to be high (90.4%). Pharmacy managers were more likely to communicate and educate patients verbally instead of providing written educational materials (98.3% vs. 78.1%) compared to junior and senior pharmacists (juniors 91.8% vs. 82%, seniors 90% vs. 86.8%) |
Study quality was evaluated using the Critical Appraisal Skills Program (CASP) checklist (Critical Appraisal Skills Program, 2018) (Table 2, Table 3).
Table 2.
Systematic review quality assessment: Critical Appraisal Skills Program (CASP) checklist (n=15) (Critical Appraisal Skills Programme, 2018).
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |
|---|---|---|---|---|---|---|---|---|---|---|
| Ford et al. (2013) | Y | Y | Y | Y | Y | C | Y | Y | Y | Y |
| Alkhalili et al. (2017) | Y | Y | Y | N | Y | Y | C | Y | Y | Y |
| Watson et al. (2019a) | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Watson et al. (2019b) | Y | Y | Y | N | Y | Y | Y | Y | Y | Y |
| Jiménez-Mangual et al. (2019) | Y | Y | Y | Y | Y | C | Y | Y | Y | N |
| Austin et al. (2007) | Y | Y | Y | Y | Y | Y | Y | Y | N | Y |
| Chin et al. (2004) | Y | Y | Y | C | C | N | C | C | Y | C |
| Nazar and Nazar (2020) | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Ford et al. (2014) | Y | Y | Y | Y | Y | Y | C | Y | Y | Y |
| Armitstead and Burton (2006) | Y | Y | Y | Y | Y | N | N | Y | Y | C |
| Awad and Cocchio (2015) | Y | Y | Y | N | Y | N | Y | N | Y | Y |
| Watson et al. (2020) | Y | Y | Y | Y | Y | C | Y | Y | Y | Y |
| Zheng et al. (2020) | Y | Y | Y | Y | C | C | Y | C | N | Y |
| Meghana et al. (2020) | Y | Y | Y | N | N | C | C | C | Y | C |
| Bahlol and Dewey (2020) | Y | Y | Y | C | C | Y | Y | Y | Y | C |
1. Was there a clear statement of the aims of the research?
2. Is a qualitative methodology appropriate?
3. Was the research design appropriate to address the aims of the research?
4. Was the recruitment strategy appropriate to the aims of the research?
5. Was the data collected in a way that addressed the research issue?
6. Has the relationship between researcher and participants been adequately considered?
7. Have ethical issues been taken into consideration?
8. Was the data analysis sufficiently rigorous?
9. Is there a clear statement of findings?
10. How valuable is the research?
Abbreviation: N: No, Y: Yes, C: Cannot tell
Table 3.
Systematic review quality assessment total results: Critical Appraisal Skills Program (CASP) checklist (Critical Appraisal Skills Programme, 2018).
| Yes | No | Cannot tell | |
|---|---|---|---|
| 1. Was there a clear statement of the aims of the research? | 15 | 0 | 0 |
| 2. Is a qualitative methodology appropriate? | 15 | 0 | 0 |
| 3. Was the research design appropriate to address the aims of the research? | 15 | 0 | 0 |
| 4. Was the recruitment strategy appropriate to the aims of the research? | 9 | 4 | 2 |
| 5. Was the data collected in a way that addressed the research issue? | 11 | 1 | 3 |
| 6. Has the relationship between researcher and participants been adequately considered? | 7 | 3 | 5 |
| 7. Have ethical issues been taken into consideration? | 10 | 1 | 4 |
| 8. Was the data analysis sufficiently rigorous? | 11 | 1 | 3 |
| 9. Is there a clear statement of findings? | 13 | 2 | 0 |
| 10. How valuable is the research? | 10 | 1 | 4 |
3. Results
A total of 337 articles were identified as relating to pharmacists’ roles during disasters; after removing duplicate and non-English articles, 81 articles were screened for eligibility. In total, 63 articles were related to the topic, but only 11 fit the inclusion criteria. One additional study was identified through an external source (Fig. 1).
In total, 80 articles were identified as related to pharmacists’ roles during the COVID-19 pandemic; after removing duplicates and non-English articles, 36 articles were screened for eligibility. A total of 32 articles were related to the topic, but only 3 fit the inclusion criteria (Fig. 2). All studies’ key characteristics are provided in Table 1.
3.1. Quality assessment
The studies were generally of a reasonable quality. However, some limitations were noted among the studies, and higher quality studies that contribute to existing knowledge are needed. In some studies, neither the relationship between the researcher and the participants nor their influence on the research was stated explicitly. In addition, some studies did not describe the recruitment strategy in sufficient detail (Table 2, Table 3).
3.2. PPRR model during disasters
3.2.1. Prevention
Watson et al. (2019a) addressed the role of pharmacists during the disaster prevention phase. The study prioritized pharmacists’ top five roles during this phase via consensus by a panel of experts: enhancing chronic disease management through accommodating point of care and ensuring medication supplies, vaccination, public education on infection control, and the disaster’s influence on increasing the risk of adverse health outcomes.
3.2.2. Preparedness
Eight articles (Alkhalili et al., 2017, Armitstead and Burton, 2006, Austin et al., 2007, Awad and Cocchio, 2015, Nazar and Nazar, 2020, Watson et al., 2019a, Watson et al., 2019b, Watson et al., 2020) addressed the role of pharmacists during the disaster preparedness phase.
Alkhalili et al. (2017) constructed a framework from a total of 505 work activities to define pharmacists’ roles in response to disasters and disaster preparedness. Of the work activities extracted, medical supply functions accounted for 41.2% of activities, and the remaining were categorized in five thematic areas: professional practice, population health planning, direct patient care, legislation, and communications. The number of activities was relatively balanced among disaster preparation, response, and recovery.
Watson et al. (2019a) identified themes for pharmacists’ roles in disaster preparedness: education, inventory management, logistical support, and vaccinations. Watson et al. (2019b) prioritized the top five pharmacists’ roles during the disaster preparedness phase as ensuring essential medication procurement; having an approach for securing cold chain lines; participating in local community disaster management teams; having knowledge about national stockpiles; and participating in local, state, and national disaster preparedness efforts. However, consensus was not reached on developing chemical, biological, radiological and nuclear (CBRN) weapons preparedness educational tools, including signs, symptoms, and drug treatments for health professionals.
Austin et al. (2007) interviewed pharmacists (n = 27) to describe and analyze the impact of two major crises on pharmacy practice and pharmacists in Toronto, Canada. One of the study’s five key themes was “Vacuity of Leadership/Lack of Utility of Emergency Preparedness Guidelines and Policies.” During the SARS outbreak, a lack of comprehension of the disease, disorganization, and poor communication from public health officials resulted in individuals searching for local leadership. Another theme related to pharmacists’ preparedness was the importance of team cohesion. A determinant of successful coping with disasters was the degree of team cohesion that existed before the disaster ensued.
Several participants noted that they had received emergency preparedness training of some sort. Participants also noted that attained knowledge and skills from such training appeared to be of limited applicability in assisting them in adapting to these crises.
Nazar and Nazar (2020) identified four descriptive themes for exploring the experiences and preparedness of humanitarian pharmacists (n = 12) in response to an emergency. The first was training and preparation: pharmacists found the most effective training for deployment preparedness to be simulation training concerning culture and existing resources, which was best introduced through hospital pharmacy-based experience. All deployed participants stated that most of their learning was attained in the context of their employment and that limited predeployment training contributed to a staggering sense of unreadiness in deployed areas. The second theme identified inventive and creative working, consultation skills, leadership, self-reliance, and firmness as necessary skills during disasters. The third theme was challenges or barriers: because humanitarian pharmacy is usually associated with medical logistical resources and support, vague roles and misunderstandings of pharmacists’ roles were reported. Moreover, humanitarian organizations enlist staff by pursuing specific training and/or experience requirements, which participants considered rare opportunities. The final theme was professional development: pharmacists noted that assertiveness when working in high-pressure environments resulted from their deployment experiences, which also contributed to improving cultural knowledge and analytical thinking.
Awad and Cocchio (2015) found that all of their survey respondents (n = 18) indicated that they had institutional protocols for disaster preparedness at their facility, and most (55.5%) had a pharmacy department plan. Most respondents (55.5%) were doubtful about essential medication supplies in their hospitals, 27.7% agreed to have a hospitalized patient’s care plan for the pharmacy department during disasters, and 22.2% agreed that the medication supply was adequate for patients and employees. For 16.6%, national or international guidelines determined the medication stock. Eight participants reported on medication stockpiling expense payments, and for 62.5%, medication stockpiling budgets were considered in the pharmacy department budget. Eight participants reported on disaster drill frequency. Disaster drills were conducted every six months in half of the respondents’ facilities, with annual disaster drills were conducted in 37.5%.
Armitstead and Burton (2006) reported that in the counterterrorism and disaster response training program implemented in the United States, among Kentucky’s licensed pharmacists, only 4.7% were certified. In pretest and posttest results, significant improvements were noted in bioterrorism training knowledge for pharmacists trained during the period February–August 2005. As a result of the training program, pharmacists trained in bioterrorism established a network for the state that provided each participant’s name, address, and contact details for use as a first responder during bioterrorism disasters.
Watson et al. (2020) reviewed international disaster pharmacy legislation. In 74.3% of international pharmacy legislations, the everyday three-day emergency supply rule was established. In only 41.9% of cases, this rule was extended to account for state-declared disasters. In 15.1% of international legislation, disaster-specific vaccination rules were implemented to avoid limiting pharmacists practicing during disasters. Mobile pharmacy legislation appeared in 23% of international legislation. An association between everyday emergency supply legislation and disaster-specific extensions of the legislation existed (P = 0.007). Disaster-specific emergency supply legislation had a relationship with disaster-specific vaccination legislation but not with mobile pharmacy legislation (Fisher’s exact test, P = 0.04 and P = 0.21, respectively). Watson et al. (2020) also assessed the effects of disasters on pharmacy legislation. There were six models in total. A significant association between disaster-specific emergency supplies was suggested in Models 1 and 2 during both the five- and 10-year periods. A country in which the number of disasters increased over a 10-year period had a 1.58-fold higher likelihood of having disaster-specific emergency supply legislation, as suggested in Model 1. These odds increased to 1.78-fold more likely in a period of 5 years, as suggested in model 2. A significant association between the five-year period (2013–17), number of disasters, and mobile pharmacy legislation was proposed in Model 6. This supports the statement that an increased number of disasters increases the odds of mobile pharmacy legislation by 1.05-fold.
3.2.3. Response
Eight articles (Alkhalili et al., 2017, Austin et al., 2007, Chin et al., 2004, Ford et al., 2013, Ford et al., 2014, Jiménez-Mangual et al., 2019, Watson et al., 2019a, Watson et al., 2019b) addressed the role of pharmacists during the disaster response phase.
Ford et al. (2013) stated that pharmaceutical supply outweighs other roles among role reports. Certain natural disasters require pharmacists to assume significant disaster roles. Pharmacists’ assumption of patient management roles is explained significantly by tornados and hurricanes (P = 0.0403 and P = 0.0281, respectively). In addition, pharmacists’ assumption of roles in response integration is explained significantly by hurricane reports (IRR = 0.96, P = 0.0138). However, pharmacists’ assumption of roles in policy coordination or pharmaceutical supply was not explained significantly by natural disasters. Pharmacists’ roles were explained significantly by chemical, biological, radiological, nuclear, and explosive (CBRNE) disasters. Two categories of CBRNE disasters, radiologic dispersal devices and nuclear terrorism, explained pharmacists’ assumption of policy coordination roles significantly (IRR = 0.63, P = 0.1015 and IRR = 2.1, P = 0.0052, respectively).
Alkhalili et al. (2017) developed a classification scheme that defined four categories of pharmacy personnel. Distinctions between the different types of personnel were made by considering five characteristics (Table 1). Personnel with primary responsibility in Categories 1 and 2 carried out a smaller number of activities during the emergency response phase. Conversely, personnel in Category 3 carried out more activities during the emergency response, whereas personnel in Category 4 carried out narrow, specialized roles.
Watson et al. (2019a) identified themes for pharmacists’ roles during disaster response: logistical support, medication supply, medication management, participation in disaster teams, vaccinations, and education. The two main barriers to pharmacists’ involvement in disasters, as identified by the respondents, were lack of comprehension of the pharmacist’s value in disasters and other health care professionals’ biases.
Watson et al. (2019b) prioritized the top five pharmacists’ roles during the disaster response phase as dispensing, counseling, logistical support related to supplies for patients with chronic diseases, medication emergency supply refills, and national stockpile issuing and distribution. However, consensus was not reached on the following roles: altering existing therapeutic regimens where clinically necessary and offering psychological health support following a disaster.
Following Hurricane Maria in Puerto Rico, Jiménez-Mangual et al. (2019) reported patients’ thoughts on the roles of community pharmacists. Access to medications from the pharmacy was the topmost medication need among participants (35.4%). Of 65 respondents, after Hurricane Maria, 47.7% lacked access to medications for a minimum of one day, and over half lacked access to medication for one to seven days. Difficulty getting in touch with the pharmacy was the most commonly noted reason for lacking access to medications. The majority of participants (78.5%) noted medication-related issues, and following the hurricane, almost half (47.7%) reported difficulty getting in touch with or getting to their pharmacy. Medication supply, counseling, and counseling regarding medication storage were the top pharmacist-provided services throughout the disaster (83%, 24.6%, and 23%, respectively). Patients’ impressions of pharmacists’ roles during disasters included medication supply, counseling, providing their prescription medication records, and counseling on over-the-counter products and self-care during disasters (92.3%, 73.8%, 63%, and 63%, respectively).
Austin et al. (2007) reported the emergence of five key themes, four of which addressed the response phase. In the first theme, during times of crisis, pharmacies are among the first-line health care facilities. The second theme addressed dependence on and the role of experience and professional judgment. The third dealt with the significance of documentation: as crises continued, flaws and defective documentation systems became problematic to pharmacists over time. The fourth theme was the importance of team cohesion in enabling successful coping during disasters. Efficient teams are characterized as having role adaptability, fluid boundaries, a sense of common goals and aims, and a flexible hierarchy.
Chin et al. (2004) also addressed the Canadian response to the SARS outbreak. In a direct patient care setting, pharmacists performed several tasks that were assigned to five categories: providing direct patient care, providing information on drugs, pharmacy operational activities, communication, and staff management.
Ford et al. (2014) reported a decreasing trend in all journals in terms of weighted counts of patient management, followed by pharmaceutical supply pharmacist role reports and policy coordination categories. Weighted counts were analyzed using chi-square goodness-of-fit analysis. The results of analysis for pharmacists’ roles in response integration, pharmaceutical supplies, patient management, and policy coordination showed very significant differences between these roles (P < 0.001). Role categories were unequally proportioned throughout the sampled journals (P = 0.002). For example, in the American Journal of Health-System Pharmacy (AJHP), pharmaceutical supply roles dominated other roles; however, they were less emphasized in other journals. In the Journal of the American Pharmacists Association (JAPHA), patient management roles were commonly reported. Other possible pharmacists’ roles, including policy coordination and response integration, were not emphasized to a great degree in the sampled journals.
3.2.4. Recovery
Two articles (Alkhalili et al., 2017, Watson et al., 2019a) addressed pharmacists’ role during the disaster recovery phase.
As mentioned above, Alkhalili et al. (2017) extracted various work activities, and when defining roles, they found that the number of activities was relatively balanced among disaster preparation, response, and recovery.
Watson et al. (2019a) prioritized the top five pharmacist roles during the recovery phase in disasters as follows: restoring normal stock levels and discarding contaminated stock properly, refiling emergency and disaster kits, promoting local community health, detecting and prioritizing at-risk populations, and retrieving patient and drug records if compromised.
3.3. PPRR model during the COVID-19 pandemic
Three articles (Bahlol and Dewey, 2020, Meghana et al., 2020, Zheng et al., 2020) addressed pharmacists’ role in COVID-19 prevention, preparedness, and response. However, no articles addressed the recovery phase after the COVID-19 pandemic.
3.3.1. Prevention
Zheng et al. (2020) focused on the prevention phase during the COVID-19 pandemic by gathering and summarizing the experiences of community pharmacies. Securing medication supplies and products was among the approaches taken to prevent COVID-19. In addition, medication purchase and delivery service information were exchanged between community pharmacies in real time to support chronic disease patients’ medication supplies.
To prevent COVID-19, operational safety and efficiency was secured through suitable environment control, staff protection, and the implementation of an emergency plan. In addition, national or local regulations were followed to clean and disinfect the environment, and personal protective equipment (PPE) was provided to all staff for protection. Emergency plans and protocols were also established alongside new pharmacy workflows to manage COVID-19 and potential drug shortages. Staff training that ensured adequate information about COVID-19 prevention was provided.
For pharmaceutical care services, COVID-19 prevention and control and safe medication use were the ultimate goals. To accomplish such goals, patients’ visits to pharmacies and medical institutions were reduced. Pharmacies offered pharmaceutical care services that catered to patient population characteristics in their surrounding communities. Infusion services’ safety operation processes included strategies such as cleaning and disinfecting the environment, screening patients before they entered the premises, limiting patient numbers, and practicing social distancing among patients.
Community pharmacists provided patient education and consulting services related to COVID-19 prevention, early identification, and appropriate medication use. Education covered mask selection and proper use, hand and respiratory hygiene, disinfectant selection and safe use, and self-care and protection strategies. The current lack of an effective vaccine or treatment for COVID-19 was also explained to patients.
3.3.2. Preparedness
Zheng et al. (2020) also addressed the preparedness of Chinese community pharmacies in the face of COVID-19. New workflows and emergency plan guidance were provided to Chinese community pharmacy staff, as was training on the diagnosis and treatment of COVID-19. A cooperative relationship was established between surrounding community pharmacies, fever clinics, and designated COVID-19 medical institutions to share mutual patients’ information. Pharmacists also referred to the WHO published guidelines for home care.
Meghana et al. (2020) conducted a survey on pharmacy professionals (n = 24) regarding COVID-19 emergency preparedness and operations management. Eighty-three percent of respondents reported feeling prepared for COVID-19. In addition, 83% of respondents reported having an adequate supply of PPE for the protection of pharmacy staff. Among the respondents, 87.5% were knowledgeable about the selection and use of masks. In addition, 41.7% of respondents prepared and distributed patient communication materials. COVID-19 emergency training was given by the 66.7% of respondents’ organizations. Of those who underwent training, 87% stated that it lasted 1–3 h.
Bahlol and Dewey (2020) also surveyed community pharmacists’ preparedness in COVID-19. High awareness of hygiene practices, recent travel abroad risk, the importance of contacting infected cases, and COVID-19 symptoms were reported by 97.6%–99.2% of respondents. In addition, 91% of respondents knew all 10 possible symptoms of COVID-19. Suspected COVID-19 cases were reported by 8.8% of respondents, and 62.9% of respondents who reported cases did not receive pandemic training. Up to 99.5% of pharmacy staff adopted most recommended behaviors to prevent the spread of COVID-19, except for minimizing nonessential staff (85.7%). Staff with chronic diseases or any other medical risks were required to take a leave (Central = 91.5%, North = 97.2%, South = 97.8%, and East = 97.3%; P = 0.004). Better availability of hand sanitizers, disinfectants, thermometers, face masks, antipyretic drugs, cold formulations, and disposable gloves was reported and compared to alcohol availability. However, free hand sanitizer supplies and masks were less available for customer use (62.1% and 86.5%, respectively). Of pharmacies, only 39.1% had antimalarial drugs available. However, pharmacies adopted separate areas for service and special waste disposal measures for symptomatic patients less frequently (64% and 80.4%, respectively). Card payment machine availability among regions was significantly different (Central = 42.1%, North = 24.5%, South = 35.5%, and East = 30.7%; P < 0.001). A significant difference was also noted in home delivery services among regions (Central = 67.1%, North = 41.0%, South = 44.1%, and East = 48.0%; P < 0.001).
3.3.3. Response
Zheng et al. (2020) reported on Chinese community pharmacies’ response to the COVID-19 pandemic. Operations were modified actively in accordance with the pandemic’s characteristics and patients’ needs. Pharmacists identified suspected patients based on clinical symptoms (e.g., fever, cough, fatigue) and epidemiological history (e.g., travel to Wuhan City or its surrounding area in the past 14 days). Patients were also directed to seek medical attention and to comply with their physicians’ treatment plans. Young patients with no comorbidities and only upper respiratory symptoms were advised to be observed and isolated at home and receive symptomatic treatment if necessary. Patients were provided with basic COVID-19 knowledge, particularly regarding symptom onset, routes of transmission, and instructions to avoid blind use of medications. Pharmacists provided medication reconciliations and consultations. Home care guidance was provided to patients in home isolation. Patients with chronic diseases receive active guidance on management to enhance medication adherence and support self-monitoring for medication safety and effectiveness. Patients were also advised to minimize unnecessary hospital visits. Cancer patients, patients with irritable bowel disease or other special chronic diseases, and patients who used high-risk medications frequently received additional guidance on the basis of their diseases or medications. Online consulting services and drug supply information were also provided. Unnecessary infusions were avoided, and community pharmacists aided infusion services care teams in establishing operational safety processes and providing regular pharmacy services. Pharmacy staff identified patients with psychological stress due to the pandemic situation (e.g., excessive anxiety, concern, fear) or blind optimism and provided psychological or emotional support for such patients, as well as referrals to psychiatrists if needed.
Meghana et al. (2020) conducted a survey on pharmacists regarding COVID-19 operations management. Pharmacists emphasized social distancing and isolation as infection control strategies and noted a rise in the demand for the antimalarial drugs hydroxychloroquine and chloroquine, as well as increased demand for azithromycin and other antivirals. However, an increase in prices was not reported. Pharmacists screened patients for fever, cough, and emotional and anxiety issues (67%, 42%, 33%, respectively).
Pharmacists also noted difficulties in procuring hydroxychloroquine, chloroquine, and azithromycin (20.8%) and cooperated with other pharmacies to procure medications and supplies (25%).
4. Discussion
This review evaluates pharmacists’ roles during health emergencies and disasters, including the current COVID-19 pandemic. We reviewed studies critically to assess and define the role of pharmacists in disaster prevention, preparedness, response, and recovery, particularly in terms of the COVID-19 pandemic. We identified 15 studies conducted in multiple countries that provided an in-depth and comprehensive assessment of pharmacists’ role in disasters and during the COVID-19 pandemic.
In the prevention phase, only Watson et al. (2019a) assessed pharmacists’ roles in disasters and focused mainly on medication supply, vaccination, and education. Regarding COVID-19, Zheng et al. (2020) summarized methods and strategies used by Chinese pharmacies, which applied roles with characteristics similar to those mentioned by Watson et al. (2019a).
Eight articles assessed pharmacists’ disaster preparedness. It was obvious that pharmacists should have more specific training courses that use simulation approaches rather than nonspecific, lecture-based training. Failure to receive proper training could give pharmacists an overwhelming sense of unpreparedness. The COVID-19 pandemic was used as an example of a rapidly changing scenario mandating proper, thorough, and frequent training sessions to keep pharmacists briefed on the latest updates. That said, Meghana et al. (2020) reported that 66.7% of pharmacy professionals underwent COVID-19 emergency training provided by an organization. Of those, 87% stated that the training lasted only 1–3 h. Even though Awad and Cocchio (2015) found that institutional disaster preparedness protocols existed at 55.5% of their respondents’ facilities, other studies (Austin et al., 2007, Nazar and Nazar, 2020) reported a lack in guidelines and protocols. Hence, proper guidelines and protocols that pharmacists could use to be better prepared and organized during disasters should be established and reviewed by a multidisciplinary team. Chinese pharmacies during the COVID-19 pandemic immediately resorted to national and international guidelines (Zheng et al., 2020). An opinion paper from the Saudi society of clinical pharmacy recommended health care institutions to involve pharmacists in emergency preparedness and disaster planning, as they are essential and integral during epidemic and pandemic situations (Badreldin et al., 2020). The ease with which the public can access pharmacists gives them the advantage of providing services that can reduce unnecessary hospital visits. For example, licensing pharmacists to provide vaccinations has proven successful whether they serve as immunizers, facilitators, or educators (Burson et al., 2016, Isenor et al., 2016, Isenor and Bowles, 2018).
In eight studies that assessed pharmacists’ roles during the disaster response phase, pharmaceutical supply was the most common (Ford et al., 2014, Watson et al., 2019a, Watson et al., 2019b, Watson et al., 2020). Using the personnel categories described by Alkhalili et al. (2017) (Table 1), Category 3 personnel performed more activities during periods of disaster. Additionally, Ford et al. (2013) implied that although policy coordination and response integration are possible roles for pharmacists during disasters, they are not emphasized in pharmaceutical journals, which implies that pharmacists still perform traditional roles during disasters, even though nontraditional roles have been advocated.
This shift in pharmacists’ roles toward pharmaceutical supply sends the wrong message of a narrow spectrum of roles and encourages people to fall back into the traditional, one-sided view of pharmacists. In fact, pharmacists can claim a diverse set of roles, including policy coordination, response integration, and patient management.
Debate continues regarding which “nontraditional” roles of pharmacists are considered suitable by other health care professionals. For example, Watson et al. (2019a) did not reach a consensus regarding pharmacists offering psychological health support after a disaster. However, in describing Chinese pharmacists’ experiences during the COVID-19 pandemic, Zheng et al. (2020) reported that pharmacy staff identified patients with psychological stress due to the pandemic situation (e.g., excessive anxiety, concern, fear) or blind optimism, provided psychological or emotional support for such patients, and referred them to psychiatrists if necessary.
Consensus was also not reached regarding pharmacists’ altering of existing therapeutic regimens where clinically necessary. Even though clinical pharmacy is a relatively new professional discipline, it is presented to a lesser extent during disasters. Clinical pharmacists can provide their knowledge and experience during disasters. For example, during the COVID-19 pandemic, many proposed medications were experimental and needed clinical pharmacists to better assess the safety and clinical efficacy of such medications.
Only two articles assessed the role of pharmacists during the recovery phase. Alkhalili et al. (2017) assessed number of activities during periods of disaster and concluded that activities were relatively balanced across all three time periods: before, during, and after the disaster. Watson et al. (2019a) prioritized the top five pharmacists’ roles during the recovery phase, which mainly consisted of a rehabilitative effort to restore balance and normal activities and to arrange for community and vulnerable patients’ needs to be fulfilled. We believe pharmacists should be more involved in patients’ therapeutic plans and in clinical team management to evaluate all patient situations, including the pharmacists’ main role of providing medication. In addition, several roles have been assumed by pharmacists working in various places such as pharmaceutical companies; such pharmacists have a crucial role to ensure the quality of these medications and to ensure the presence of a sufficient medication supply for use during emergencies. For the health care system to accept pharmacists’ new nontraditional roles, the proper presentation in the literature and the involvement of pharmacists in policy coordination are warranted.
4.1. Implications
This review provides decision-makers with an overview of pharmacists’ roles during disasters using the PPRR risk management model, which can be readily adopted during disasters and emergencies. By using the COVID-19 pandemic as an example of a very recent disaster, this review offers a proper presentation of pharmacists’ responsibilities and capabilities, as well as policymakers’ perceptions of pharmacists’ roles during disasters.
4.2. Strengths and limitations
The study has advantages that, to the best of our knowledge, this is the first systematic review of the role of pharmacists during disasters in which the ongoing COVID-19 pandemic is used as an example to reflect the results. We also used the PPRR risk management model that helped us organize the findings of this systematic review. A comprehensive process was employed that included the critical appraisal of the included studies. However, we have limitation that despite the comprehensiveness of the searches, we excluded non-English articles, taking into account the valuable data they may hold.
5. Conclusions
The COVID-19 pandemic has revealed the need for well-prepared, regulated health care system responses to disasters that adopt new roles that have emerged in recent years. Pharmacists have proven their ability to fill multiple roles that allow them to use their knowledge and experience at the front lines of disasters. However, current evidence does not reflect pharmacists’ full abilities. Most of the studies conducted in community pharmacies showed slight variations in pharmacists’ roles that still fall under the umbrella of a traditional role; however, some of these studies were of inferior quality.
Role of the funding source
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contributions
WA design the methodology, conduct the study, review the included articles, writing the manuscript, TM has started the research idea, design the methodology, part of reviewing the included articles, edit the manuscript and supervise the whole process.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Peer review under responsibility of King Saud University.
References
- Alkhalili M., Ma J., Grenier S. Defining roles for pharmacy personnel in disaster response and emergency preparedness. Disaster Med. Public Health Prep. 2017;11:496–504. doi: 10.1017/dmp.2016.172. [DOI] [PubMed] [Google Scholar]
- Armitstead J.A., Burton D.C. Enhanced pharmacy training for counter-terrorism and disaster response. J. Telemed. Telecare. 2006;12(Suppl 1):3–5. doi: 10.1258/135763306777978498. [DOI] [PubMed] [Google Scholar]
- Austin Z., Martin J.C., Gregory P.A.M. Pharmacy practice in times of civil crisis: the experience of SARS and the blackout in Ontario. Canada. Res. Soc. Adm. Pharm.: RSAP. 2007;3:320–335. doi: 10.1016/j.sapharm.2006.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Awad N.I., Cocchio C. Assessment of hospital pharmacy preparedness for mass casualty events. P T: Peer-Rev. J. Formul. Manag. 2015;40:264–267. [PMC free article] [PubMed] [Google Scholar]
- Badreldin H.A., Raslan S., Almudaiheem H., Alomari B., Almowaina S., Joharji H., Alawagi M., Al-Jedai A. Pharmacists roles and responsibilities during epidemics and pandemics in Saudi Arabia: an opinion paper from the Saudi Society of clinical pharmacy. Saudi Pharm. J. 2020;28:1030–1034. doi: 10.1016/j.jsps.2020.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bahlol M., Dewey R.S. Pandemic preparedness of community pharmacies for COVID-19. Res. Soc. Adm. Pharm. 2020 doi: 10.1016/j.sapharm.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burson R.C., Buttenheim A.M., Armstrong A., Feemster K.A. Community pharmacies as sites of adult vaccination: A systematic review. Human Vac. Immunotherapeutics. 2016;12(12):3146–3159. doi: 10.1080/21645515.2016.1215393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC), 2019. 1918 pandemic (H1N1 virus) pandemic influenza (Flu). http://www.cdc.gov/flu/pandemic-resources/1918-pandemic-h1n1.html.
- Chin T.W., Chant C., Tanzini R., Wells J. Severe acute respiratory syndrome (SARS): the pharmacist's role. Pharmacotherapy. 2004;24:705–712. doi: 10.1592/phco.24.8.705.36063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Critical Appraisal Skills Programme, 2018. CASP qualitative checklist. http://casp-uk.net/wp-content/uploads/2018/03/CASP-Qualitative-Checklist-2018_fillable_form.pdf (accessed 04 July 2020).
- Disaster Management, 2018. Prevention preparedness, response and recovery disaster management guideline. http://www.disaster.qld.gov.au/dmg/Pages/default.aspx.
- Ford H., Dallas C.E., Harris C. Examining roles pharmacists assume in disasters: a content analytic approach. Disaster Med. Public Health Prep. 2013;7:563–572. doi: 10.1017/dmp.2013.99. [DOI] [PubMed] [Google Scholar]
- Ford H., von Waldner T., Perri M., 3rd Pharmacists' roles in post-september 11th disasters: a content analysis of pharmacy literature. J. Pharm. Pract. 2014;27:350–357. doi: 10.1177/0897190013507081. [DOI] [PubMed] [Google Scholar]
- Isenor J.E., Bowles S.K. Evidence for pharmacist vaccination. Can. Pharmacists J. CPJ Revue des pharmaciens du Canada : RPC. 2018;151(5):301–304. doi: 10.1177/1715163518783000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isenor J.E., Edwards N.T., Alia T.A., Slayter K.L., MacDougall D.M., McNeil S.A., Bowles S.K. Impact of pharmacists as immunizers on vaccination rates: A systematic review and meta-analysis. Vaccine. 2016;34(47):5708–5723. doi: 10.1016/j.vaccine.2016.08.085. [DOI] [PubMed] [Google Scholar]
- Jiménez-Mangual B.C., Cuevas-Acevedo D.M., Quiles-Alves N., Rodríguez-Nazario I., Melin K.R. Description of patients medications needs and the community pharmacist's role in Puerto Rico following a natural disaster. J. Prim. Care Community Health. 2019;10 doi: 10.1177/2150132719842701. 2150132719842701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meghana A., Aparna Y., Chandra S.M., Sanjeev S. Emergency preparedness and response (EP&R) by pharmacy professionals in India: lessons from the COVID-19 pandemic and the way forward. Res. Soc. Adm. Pharm. 2020 doi: 10.1016/j.sapharm.2020.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nazar Z., Nazar H. Exploring the experiences and preparedness of humanitarian pharmacists in responding to an emergency-response situation. Res. Soc. Adm. Pharm. 2020;16:90–95. doi: 10.1016/j.sapharm.2019.03.146. [DOI] [PubMed] [Google Scholar]
- Watson K.E., Singleton J.A., Tippett V., Nissen L.M. Do disasters predict international pharmacy legislation? Aust. Health Rev. 2020;44:392–398. doi: 10.1071/AH19093. [DOI] [PubMed] [Google Scholar]
- Watson K.E., Singleton J.A., Tippett V., Nissen L.M. Defining pharmacists' roles in disasters: a Delphi study. PLoS One. 2019;14:e0227132. doi: 10.1371/journal.pone.0227132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson K.E., Tippett V., Singleton J.A., Nissen L.M. Disaster health management: do pharmacists fit in the team? Prehosp. Disaster Med. 2019;1–8 doi: 10.1017/s1049023x18001152. [DOI] [PubMed] [Google Scholar]
- World Health Organization, 2020a. WHO coronavirus disease (COVID-19) dashboard. http://covid19.who.int.
- World Health Organization, 2020b. WHO Timeline - COVID-19. https://www.who.int/news-room/detail/27-04-2020-who-timeline-covid-19.
- WHO, 2019. Health Emergency and Disaster Risk Management Framework. World Health Organization, Geneva.
- Zheng S.Q., Yang L., Zhou P.X., Li H.B., Liu F., Zhao R.S. Recommendations and guidance for providing pharmaceutical care services during COVID-19 pandemic: a China perspective. Res. Soc. Adm. Pharm.: RSAP. 2020;S1551–7411(1520):30284–30289. doi: 10.1016/j.sapharm.2020.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]