Abstract
Background
The COVID-19 pandemic has become a public health emergency and raised global concerns in about 213 countries without vaccines and with limited medical capacity to treat the disease. The COVID-19 has prompted an urgent search for effective interventions, and there is little information about the money value of treatments. The present study aimed to summarize economic evaluation evidence of preventing strategies, programs, and treatments of COVID-19.
Material and methods
We searched Medline/PubMed, Cochrane Library, Web of Science Core Collection, Embase, Scopus, Google Scholar, and specialized databases of economic evaluation from December 2019 to July 2020 to identify relevant literature to economic evaluation of programs against COVID-19. Two researchers screened titles and abstracts, extracted data from full-text articles, and did their quality assessment by the Consolidated Health Economic Evaluation Reporting Standards (CHEERS) checklist. Then, quality synthesis of results was done.
Results
Twenty-six studies of economic evaluations met our inclusion criteria. The CHEERS scores for most studies (n = 9) were 85 or higher (excellent quality). Eight studies scored 70 to 85 (good quality), eight studies scored 55 to 70 (average quality), and one study < %55 (poor quality). The decision-analytic modeling was applied to twenty-three studies (88%) to evaluate their services. Most studies utilized the SIR model for outcomes. In studies with long-time horizons, social distancing was more cost-effective than quarantine, non-intervention, and herd immunity. Personal protective equipment was more cost-effective in the short-term than non-intervention. Screening tests were cost-effective in all studies.
Conclusion
The results suggested screening tests and social distancing to be cost-effective alternatives in preventing and controlling COVID-19 on a long-time horizon. However, evidence is still insufficient and too heterogeneous to allow any definite conclusions regarding costs of interventions. Further research as are required in the future.
Keywords: Economic evaluation, SARS-COV-2, COVID-19, Isolation, Lockdown, Screening
1. Introduction
The COVID-19 pandemic has influences worldwide communities with considerable morbidity and mortality caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [[1], [2], [3]]. This disease causes dry cough, fever, breath shortness, pneumonia, and lung infections [4]. Healthcare systems have raised some concerns regarding the high demand for increasing the existing capacity, additional resources, and financial support [5].
Years of Life Lost (YLLs) due to COVID-19 were 4,072,325 in 30 high-incidence countries on July 14, 2020. The largest number of total YLLs attributed to COVID-19 was in the USA, and the YLLs and Disability-Adjusted Life Years (DALYs) per 100,000 populations were the highest in Belgium [6]. In Korea, the Years Lost due to Disability (YLDs) and the YLLs constituted 10.3% and 89.7% of the DALYs, respectively [3].
YLL causes most burden of COVID-19 and suggests that decision-makers should make an effort to reduce fatality. It emphasizes the importance of early identification of incidence cases [3,6]. Global economic costs of COVID-19 are estimated from $77 billion to $2.7 trillion [7]. The direct medical cost of an asymptomatic COVID-19 patient was $3045 during the infection in the USA [5].
No vaccine or approved treatment has been found for the prevention and treatment of COVID-19. Any attempt to achieve treatment should be widely available and cost-effective to control this global pandemic [7].
Non-pharmaceutical interventions for prevention and control of COVID-19 vary between countries, including lockdowns of populations, border closures, school closures, screening of suspected cases, isolating symptomatic individuals and their contacts, and social distancing. However, these strategies could result in substantial productivity losses [8]. One of the goals of social distancing measurement is reducing the percentage of the infected population and the negative effect of the COVID-19 pandemic on economics [9]. Others have suggested a herd immunity strategy, which is indirect protection against infection transmitted to susceptible individuals if there are large numbers of immune individuals in a population [5].
Understanding whether these interventions have a positive effect on epidemic control or which interventions are necessary for disease preventing is crucial and result in high economic and social costs [8]. To the best of our knowledge, there aren't any systematic reviews regarding the cot-effectiveness of these interventions. By considering the costs and benefits of preventing and controlling strategies for the COVID-19 pandemic, decision-makers can optimize the impact of scarce healthcare resources. Therefore, the purpose of this study was to summary the cost-effectiveness of programs against COVID-19.
2. Method
This systematic review followed the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) and AMSTAR (Assessing the methodological quality of systematic reviews) guidelines [10,11]. The review protocol was registered on PROSPERO (International prospective register of systematic reviews). CRD42020199673.
A comprehensive search was performed for the literature published from December 2019 to July 2020 on Cochrane Library, Medline, Web of Science Core Collection, Scopus, Embase, Google Scholar, National Health Service Economic Evaluation Database (NHS EEDS), and Cost-Effectiveness Analysis Registry (CEA). We developed a search strategy to detect studies using a Population/Problem–Intervention–Comparison–Outcomes–Study design (PICOS) framework. We used Medical Subject Heading (Mesh) terms and keywords for “cost” and “COVID-19”. Search strategy for all databases is presented in Appendix S1. We also searched reference lists of included studies to identify relevant articles. First, the search strategy was developed for PubMed and afterward translated to other databases. The included studies specifically focused on economic analysis of strategies and programs against COVID-19. The detailed exclusion and inclusion criteria are presented in Table 1 .
Table 1.
Eligibility criteria.
| Inclusion criteria | Exclusion criteria | |
|---|---|---|
| Population | General population or targeted population | NA |
| Intervention | Strategies prevention or control and treatment COVID-19 pandemic | Other interventions |
| Comparator | No Intervention, standard care or any other intervention | NA |
| Outcome | Incremental cost-effectiveness ratio(ICER), Incremental cost per quality-adjusted life years(QALY), Incremental cost per disability-adjusted life years(DALY), Net monetary benefit | Cost analysis studies(i.e., studies which measured or compared costs without health outcomes) or outcomes related to effectiveness only |
| Study design | Partial economic evaluations if both costs and outcomes of one intervention, were considered | conference abstracts, review articles, animal studies and is do not find the full text. |
| full economic evaluation studies CEA, CUA or CBA (model-based or trial based) | ||
| Context | No restrictions | NA |
| Language | English language | NA |
CEA: cost-effectiveness analysis, CUA: cost-utility analysis, CBA: cost-benefit analysis.NA: not applicable.
We initially screened the title and abstract of retrieved studies based on inclusion/exclusion criteria. Then, two researchers independently evaluated the full-text of the eligible articles. In cases that the disagreement could not be resolved, the viewpoints of the third researcher used. We designed a data extraction form including country, compared interventions, study population, time horizon, type of economic evaluation (CEA, cost-utility analysis, and cost-benefit analysis), perspective, costs, and outcomes.
The reporting quality of the economic evaluation studies was assessed by the CHEERS checklist [12]. Items were scored as “fully met”, “not meet”, “partially met”, or “not applicable”. Studies that fully met each of the items of the checklist were scored as ‘1’, items that partially met the criteria 0.5 and 0 when the study did not meet the criteria.
Then a percentage score for each study was calculated. Quality scoring ≥85% were categorized as having excellent reporting quality, 70–85% as very good quality, 55–70% as good quality, and quality scoring <55% were classified as poor quality. Two researchers (A.R, A.S) independently assessed the quality of studies and was consulted a third researcher (M.T) for resolving any disagreements.
Finally, outcomes were measured by ICER (incremental cost-effectiveness ratio) as cost per life-year gained, cost per case averted, cost per quality of adjusted-life years(QALY), cost per DALY, and net marginal benefit of interventions. Then, qualitative analysis was done [13].
3. Results
3.1. Overview
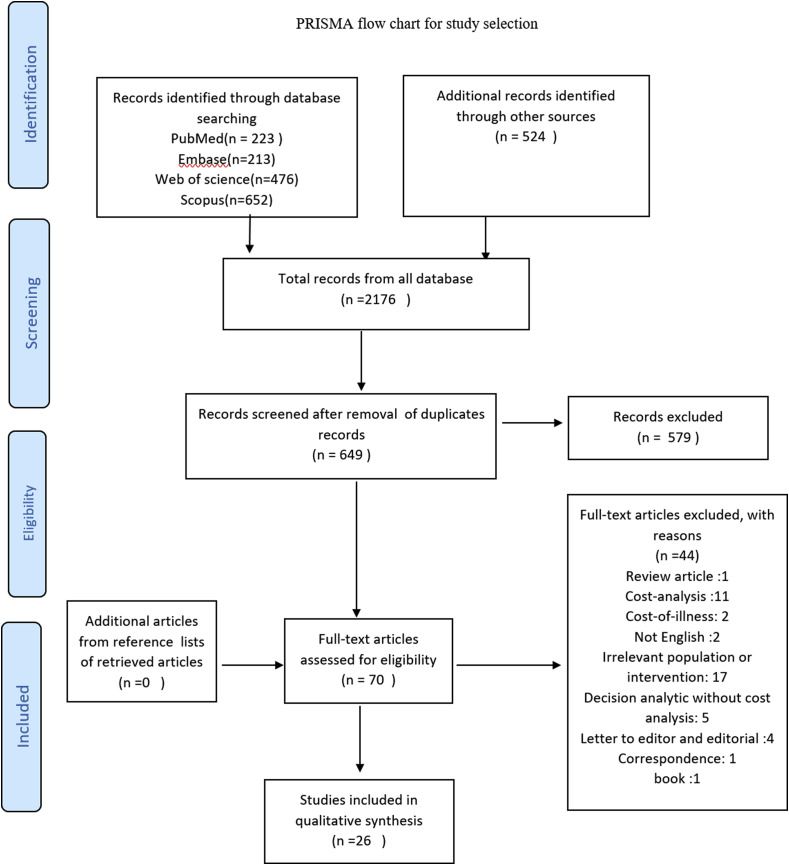
The PRISMA flow diagram of this study is given in Fig. 1 . In total, 2176 records were identified from all databases. After the removal of all duplicate records, 649 studies were eligible based on screening the titles and abstracts. Afterward, according to the inclusion criteria, 70 articles were selected for full-text evaluation. Finally, a total of 26 publications were included in the qualitative analysis, whose characteristics have been presented in Table 2 and Table 3 .
Fig. 1.
PRISMA flow chart for study selection.
Table 2.
Summary of study strategies.
| Strategies | Number of studies(%) |
|---|---|
| Screening and diagnostic tests | 8(30%) |
| Quarantine | 10 (38%) |
| Social distancing | 7(26%) |
| Isolation | 6 (23%) |
| Personal Protective equipment | 5(19%) |
| Treatment & vaccination | 3(11%) |
Table 3.
Study design and setting overview.
| Author | Country | population | Compared intervention | Type of economic evaluation | Perspective | Time horizon | Discount rate | Sensitivity analysis | CHEERS score |
|---|---|---|---|---|---|---|---|---|---|
| Zhao, Jidi | China | General population | Strategy 1: no delay Movement restriction policies Strategy 2: 1week delay Movement restriction policies Strategy 3: 2week delay Movement restriction policies Strategy 4 : 4week delay Movement restriction policies | CUA (SEIR model) | Health care and social | lifetime | 3% | Yes, one-way and PSA | 0.98 |
| Wang, Qiang | China | General population | 1.Personal protection 2.Isolation-and-quarantine 3.Gathering restriction 4.Community containment 5. no intervention | CEA (Stochastic agent-based model) | NR | 14 days | Not applicable | Yes, one-way and two-way | 0.86 |
| Thunström, Linda | US | General population | Social distancing Vs. no social distancing | CBA (SIR model) | NR | 30 years | 3% | Yes, break even analysis | 0.67 |
| Xu, Liyan | China | General population | 1.Regular epidemiological control 2. local social interaction control 3.inter-city travel restriction | CEA (STEX-SEIR model) | NR | 30 days | Not applicable | Yes, one-way | 0.59 |
| Sriwijitalai, Won | Thailand | Patients with COVID-19 | Chest CT and RT-PCR | CUA - | NR | NR | NR | NR | 0.4 |
| Shlomai, Amir | Israel | General population | Quarantine of the susceptible population vs. social distancing | CEA and CUA (SEIR model) | NR | 200 days | Not applicable | Yes,deterministic and PSA | 0.87 |
| Sharma, Naveen | India | General population | Lockdown vs. no lockdown | CBA (Decision tree) | Social | One year | Not applicable | NR | 0.69 |
| Shaker, M. S. | US | Patient with allergic rhinitis (AR) | 1.Clinical AIT 2.Home AIT 3.Discontinue AIT | CUA (Markov) | Social and health care system | 50 years | 3% | Yes,deterministic and PSA | 0.92 |
| Schonberger, R. B. | US | General population | herd immunity (full reopening) vs. Limited reopening with social distancing | CBA - | NR | NR | 3% | NR | 0.59 |
| Savitsky, L. M. | US | Health care workers | Universal COVID-19 screening vs. universal PPE use | CEA (Decision tree) | NR | NR | Not applicable | Yes,one-way,two- way and PSA | 0.78 |
| Rushworth, Stuart A | UK | General population | Mount siani covid-19 Serological assay (immunoassay) | CEA - | NR | 14 days | Not applicable | Yes,PSA | 0.81 |
| Risko, Nicholas | US | Health care workers | Full PPE supply vs. Inadequate PPE | CEA and ROI (Decision tree) | Societal | 30 weeks | Not applicable | Yes,PSA | 0.93 |
| Reddy, K. P. | South Africa | General population | 1. HT 2.HT + CT 3. HT + CT + IC + MS 4.HT + CT + IC 5. HT + CT + IC + MS + QC 6. HT + CT + IC + QC | CEA (Markov) | Health care system | Lifetime | NR | Yes, One y-way and multiway | 0.78 |
| Paltiel, A. D. | US | College student | screening strategies: 1.Weekly, test sensitivity:70, 80, 90 2.Every 3 days, test sensitivity: 70, 80,90 3.Every 2 days, test sensitivity: 70,80, 90 4. Daily: test sensitivity:70, 80,90 | CEA (SIR model) | NR | 80 days | Not applicable | NR | 0.75 |
| Padula, William V | US | General population | 1.Do nothing 2.social distance 3.Treatment 4. vaccination | CUA (Markov) | Societal | 365 days | 3% | Yes,one-way and PSA | 0.93 |
| Neilan, Anne M. | US | General population | 1.PCR-any-symptom 2.Self- screen 3.PCR-severe only 4.PCR-all 5.PCR-all-repeart | CUA (dynamic stat-transition microsimulation model) | Health care system | 180 days | Not applicable | Yes, one-way and PSA | 0.98 |
| Nannyonga, Betty K. | Uganda | General population | Facemask vs. no facemask | CEA (SEIAQRD model) | NR | 14 days | Not applicable | NR | 0.67 |
| Mahmoudi, Nader | Australia | General population | Home isolation Vs. hotel room isolation | CEA (Decision tree) | NR | 14 days | Not applicable | NR | 0.69 |
| Khajji, B. | Morocco | General population | Strategy 1: protecting susceptible individuals from contacting the infected individuals in the same region 1 Strategy 2: protecting and preventing susceptible individuals from contacting the infected individuals in the same region or in other regions.Strategy 3: protecting susceptible individuals, preventing their contact with the infected individuals and encouraging the exposed individuals to join quarantine centers.Strategy 4: protecting susceptible individuals, preventing their contact with the infected individuals, encouraging the exposed individuals to join quarantine centers and the disposal of the infected animals. | CEA (multi-region discrete time model) | NR | NR | NR | NR | 0.59 |
| Jiang, Yawen | China | Patients with covid-19 | 1.Two times test RT- PCR 2. three test times RT- PCR | CUA and NMB (SEIR model) | Health care system | 23 January 2020-6 march 2020 | Not applicable | Yes, one-way and PSA | 0.92 |
| Gandjour, Afschin | Germany | Patients with Covid-19 | Provision of additional ICU bed Vs. no intervention | CEA and ROI (Markov model) | Societal | Lifetime | %3 for costs %1 for benefits | Yes,one-way and threshold analysis | 0.89 |
| Gandjour, Afschin | Germany | General population | 1. Shutdown 2. ICU capacity exceeded by %50 3. ICU capacity exceeded by %100 4. ICU capacity exceeded by %200 5. ICU capacity exceeded by %300 6.No intervention | Economic evaluation (Decision tree) | Societal | One year | Not applicable | Yes, one-way | 0.76 |
| Dutta, Mousumi | India | General population | lockdown | CBA (SIR model) | NR | NR | NR | NR | 0.65 |
| Broughel, James | US | General population | Stay-at-Home Orders, Public School and University Closures, Any Restriction on Size of Gatherings, Legally Ordered Closure of Any Business, Legally Ordered Closure of All Nonessential Businesses and Severe Travel Restrictions | CBA model from the Institute for Health Metrics and Evaluation (IHME) | Societal | 50–91 days | 5% | NR | 0.7 |
| Asamoah, Joshua Kiddy K | Ghana | General population | 1. u1 = The effective testing and quarantine when boarders are opened. 2. u2 = Intensifying the usage of nose masks and face shields through education. 3. u3 = Cleaning of surfaces with home-based 4. u4 = Safety measures adopted by the asymptomatic and symptomatic individuals such as; practising proper cough etiquette (maintaining a distance, cover coughs and sneezes with disposable tissues or clothing and wash hands after cough or sneezes).detergents. 5. u5 = Fumigating commercial areas such as markets. Strategy 1 (which combines the use of controls ui, i = 1, 2, …, 5), Strategy 2 (u1 only), Strategy 3 (u2 only), Strategy 4 (u3 only), Strategy 5 (u4 only), and Strategy 6 (u5 only) | CEA (A deterministic model) | NR | NR | NR | Yes, one-way | 0.76 |
| Aguas, Ricardo | UK | Patients with covid-19 | Dexamethasone Vs. no dexamethasone | CEA (Stat transition model) | Provider (health system) | 6 months | Not applicable | NR | 0.71 |
NR: Not reported.HT: Healthcare Testing, CT: Contact Tracing, IC: Isolation Centers, MS: diagnostic testing for symptomatic individuals, QC Quarantine Centers, AIT: Allergen immunotherapy, CEA: cost-effectiveness, CUA cost-utility, CBA: cost-benefit, PSA: Probability sensitivity analysis, SEIR: Susceptible-Exposed-Infected-Recovered, NBA: net benefit analysis, ROI: Return on investment.
3.2. Study characteristics
Overall, 26 articles were included in this review. Most of these studies were from the US (n = 9) [[14], [15], [16], [17], [18], [19], [20], [21], [22]], followed by China (n = 4) [4,[23], [24], [25]], the UK (n = 2) [26,27], Germany(n = 2) [28,29], India (n = 2) [30,31], Australia (n = 1) [32], Israel (n = 1) [33], Morocco (n = 1) [34], Ghana (n = 1) [35], South Africa (n = 1) [36], Uganda (n = 1) [37], Thailand (n = 1) [38].
3.3. Population
Eighteen studies assessed the programs against COVID-19 in the whole population [4,14,16,[20], [21], [22], [23], [24],26,28,30,[32], [33], [34], [35], [36], [37]], four studies evaluated preventing programs among patients with COVID-19 [25,27,29,38], two studies focused on the healthcare workers (HCWs) [17,18], one study on the academic students [19] and last one on the patients with allergic rhinitis [15].
3.4. Interventions
Table 2 depicts fighting strategies for COVID-19. The three common strategies in most of the included studies were quarantine (n = 10) [4,[22], [23], [24],30,31,[33], [34], [35], [36]], screening and diagnostic tests (n = 8) [17,19,21,25,26,35,36,38], and social distancing (n = 7) [[14], [15], [16],20,24,33,35] which they were evaluated for both target groups (such as high risk or forefront healthcare workers, and academic students) and the general population. A handful of studies evaluated PPE (n = 5) [17,18,23,35,37] and isolation (n = 6) [4,22,23,32,34,36]. Three studies examined treatment and vaccination of COVID-19 [20,27,29]. Only one economic evaluation study assessed the economic value of public hygiene and cleaning surface with detergents [35].
3.5. Study perspective
The majority of included studies were from the social perspective (n = 8) [4,15,18,20,22,[28], [29], [30]]. Six studies performed from the healthcare system perspective [4,15,21,25,27,36]. Other studies have not stated any perspectives [14,16,17,19,23,24,26,[31], [32], [33], [34], [35],37,38].
3.6. Willingness-to-pay thresholds
The US studies used the following thresholds as $100000/QALY [15,21], $125000 QALY/life years gained [16], $25000/transmission preventing to an HCWs [17], and $ 10000000/reduced death risk [22]. The thresholds adopted by Chinese studies were $9595/protected humans [23], 64644/QALY [25],70892(RMB) per QALY [4], in the UK was £20000/QALY [27], Israel $150000/QALY [33], Germany €101493/life years gained [29], South African $1290/life years gained [36], and 13 studies have not stated willingness-to-pay threshold [14,18,24,26,[30], [31], [32],34,35,37,38].
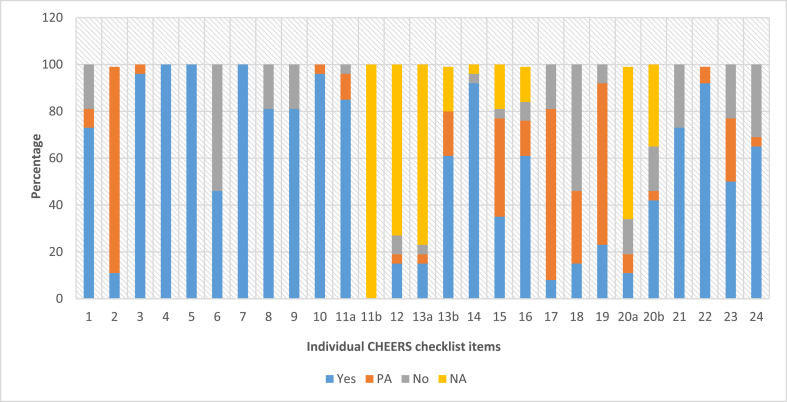
3.7. Assessment of methodological quality
Fig. 2 shows each CHEERS item; that how many ones were met by the included studies. The average quality score was %76. The maximum and minimum scores of quality were %98 and %40, respectively. Nine of the studies were scored in the range of 85 or higher as excellent quality [4,15,18,20,21,23,25,29,33], and eight studies scored within 70–85 as very good quality [17,19,22,[26], [27], [28],35,36]. Eight studies were rated as good quality [14,16,24,[30], [31], [32],34,37] and one study had poor< %55 quality [38].
Fig. 2.
Reporting Quality of included economic evaluation studies by CHEERS checklist.
The most frequent items that were not reported in the articles implied item 6 ‘study perspective’ (54% no compliant), item 18 ‘study parameters’ (54% no compliant), and item 24 ‘conflicts of interest’ (31% no compliant). Furthermore, item 21 ‘characterizing heterogeneity’ (27% no compliant) and item 23 ‘source of funding’ (23% no compliant) were the main areas of weakness for the included studies.
3.8. Modeling approaches and time horizon
Twenty-three of the studies (88%) were used decision-analytic modeling to evaluate these services [1,4,14,15,[17], [18], [19], [20], [21], [22], [23], [24], [25],[27], [28], [29], [30], [31], [32], [33], [34], [35], [36], [37]]. Most studies applied the SIR model to outcomes. Three studies applied a multi-region discrete-time [34], stochastic agent-based [23], and the Institute for Health Metrics and Evaluation(IHME) model [22]. In 11 studies (71.4%), the time horizons of the analysis were either a maximum of 1 year (42%) or between 14 days and one year [[18], [19], [20], [21], [22], [23], [24], [25], [26], [27], [28],30,32,33,37]. The four studies (15%) had time horizons of more than one year and up to a lifetime horizon [4,14,15,29,36]. Six studies (23%) have not stated time horizon [16,17,31,34,35,38]. The discounting rate for costs and benefits were at 3% to 5% annually. Five studies have not stated the discount rate [31,[34], [35], [36],38].
3.9. Summary of results in economic evaluations
The results regarding the cost-effectiveness of the interventions in prevention, control, and treatment of COVID-19 are summarized in Table 2.
3.9.1. Cost-effectiveness studies
Most of studies implied the cost-effectiveness analysis(CEA) method (%53) [[17], [18], [19],23,24,26,27,29,[32], [33], [34], [35], [36], [37]]. A Chinese study has been reported a cost-effectiveness ratio of 26426 with a negative increment for no-delay Movement Restriction Policies(MRPs) on epidemic control of COVID-19. This study compared epidemic control policies with a no-delay MRPs in four weeks [4]. The second study from China found the lowest and highest cost-effectiveness ratios for quarantine and personal protection at a cost-per-infection rate of 6.788 and 1278.438, respectively. Isolation and quarantine caused to prevent humans from infection in 1696 and 1990 with a cost of $ 12,428 and $ 58,555, respectively [23] The third study from the U.S was reported screening every two days with a sensitivity of 70% and a cost of $ 7900 per prevented case of infection as a cost-effective option among academic students [19].
One study in Australia reported that the cost of isolating a patient with COVID -19 in his/her home as $1248.00 was lower than the total cost of isolating this patient in a hotel room as $4069.80. This study has mentioned that the decision should be reversed depending on the household size and the secondary household attack rate [32]. A Moroccan study found that the strategy of protecting suspicious individuals and preventing individual contacts with the lowest cost-effectiveness ratio (3.8926) was a cost-effective option compared to other interventions [34].
In one study in Germany, the Provision of one additional ICU bed had an incremental cost-effectiveness ratio of 25,735 [29]. In a study conducted in Ghana, cleaning of surfaces with home-based detergents was the most cost-effective strategy, and then the testing and quarantine, combining all of them and increasing the use of nose masks and face shields [35]. In a South African study, the reported minimum cost-effectiveness ratio was related to isolation, household contact tracing, and mass symptom screening ($ 350/YLS). They reduced mortality by 76%, increased costs by 16% [36]. One study from the UK reported that Dexamethasone treatment was a cost-effectiveness option vs. no Dexamethasone [27].
3.9.2. Cost-utility studies
Cost-utility analysis(CUA) was performed in seven studies (%26) [4,15,20,21,25,33,38]. An American study reported the cost-effectiveness ratios of vaccination, treatment, and social distance, and non-intervention against Covid-19 at 0.892, 0.877, and 0.875, respectively [20].
Another study in China estimated the difference between the net marginal benefit of the two diagnostic strategies for Covid-19 as three times reverse transcription-polymerase chain reaction (RT-PCR(compared to two times RT-PCR with a $104 million cost. QALY loss due to mortality was found in the two-test and three-test strategies as 6563.4 and 5814, respectively. In this study, conducting three times RT- PCR test was cost-effectiveness [25]. In the American study, Home Immunotherapy Self-Administration (HITSA) had the highest net marginal benefit compared to clinic allergen immunotherapy(AIT) [15].
Another study in the US pointed out that the PCR-all-repeat strategy leads to the most effective results, and PCR-only-only leads to the worst results. It occurs when effective reproduction numbers (Re)≥1.8 PCR-any-symptom was cost-saving compared to other strategies [21]. An Israeli study reported the cost-effectiveness ratio of the global quarantine of suspects compared to social distance as 751,000 for preventing death [33]. In a Thai study, the cost per PCR adjusted quality of life was 71.53 [38].
3.9.3. Cost-benefit studies
The (cost-benefit analysis)CBA technique was applied in four studies(%15) [14,16,30,31]. In an Indian study, lockdown was found to be cost-saving as 2.7 trillion [30]. In another Indian study, the net benefit of lockdown was reported in all scenarios ranging from 667.25 to 10038.69 [31].
In one American study, the value of life lost by social distance and its net benefit were $ 21.8 and $ 5.9 trillion, respectively [14]. Another American study regarding the monetary value of QALY gained from social distancing was 1143.9 billion compared to herd immunity [16].
4. Discussion
The present study is the first systematic review focused on the economic evaluations of interventions against COVID-19. We identified 26 studies regarding the cost-effectiveness of preventing and treating interventions for COVID-19, which they evaluated six different strategies. These studies generally had good quality.
The included economic evaluation studies were different vastly based on type of interventions, used methods, setting, perspectives, and populations. For this reason, direct comparing the results of studies was difficult (e.g., preventive and diagnostic procedures, also drug therapies).
Results of the present study showed that in research with long-time horizons, the social distancing was more cost-effective than quarantine, non-intervention, and herd immunity. For example, the result of a study in China showed that isolation-and-quarantine was the most cost-effective intervention in the control of COVID-19 [23]. The other research in Israel estimated that the cost of isolating one person per day was $70 [33]. However, personal protection, isolation, and quarantine was an effective strategy to prevent further contamination than isolation or quarantine alone. In this study, the community containment was more efficient and cost-effective when the quarantine delay-time was more than the latent period. Thunström et al. conducted a cost-benefit analysis for the present value of saved lives based on the current difference in Gross domestic product(GDP) regarding social distancing and non-social distancing. This study indicated that social distancing through decreasing the average contact rate by 38% among individuals could keep the average mortality rate at the lower level of 0.5%, and the present value of net benefits by $5.16 trillion [14].
Sharma's study has illustrated that by lockdown in India, 1.86% of GDP based on evaluated Indian GDP of February 2019–20 at current prices has saved [30]. However, another study in India indicated that the net benefits of lockdown were negative [31]. One study in the US noted the social distancing is a cost-effective strategy relative to herd immunity if an effective therapy or vaccine can be introduced within 11.1 months of late May 2020 [14]. Reddy showed that the strategy of isolation, household contact tracing, and mass symptom screening would reduce COVID-19 mortality [34]. Similarly, the study by Khajji et al. indicated that protecting susceptible individuals, preventing contact with the infected individuals, and encouraging the exposed individuals to join quarantine centers provides the most cost-effective strategy for controlling the disease [34].
Also, Zhao's study suggests the early implementation of MRPs in response to COVID-19 that reduced both of the health burden and societal cost [4]. Another study showed that a successful cessation increases the years of life by 0.02 and 0.08 per person significantly, also an economic value between 1543 and 8027 euros per person in the German population. However, if herd immunity is achieved through natural infecting, it is expected to lose 0.42 years of life per capita compared to the pre-epidemic situation [28].
Personal protective equipment was more cost-effective in the short-time than non-intervention. There was no long-term study regarding the cost-effectiveness of personal protective equipment. Screening tests have been cost-effective in all studies. One study in the HCWs population of the US showed that COVID-19 screening was the cost-effective option relative to universal PPE also, in areas with high COVID-19 prevalence, PPE may be preferred [17]. Other studies suggest that investing 9557 million dollars in PPE production for HCWs results in an economic gain of 755314 million dollars. The intervention will save 2,299,543 lives in low and middle-income countries, costing $ 59 per HCW for disease prevention and $ 4309 per life saved [18].
The present review had several potential limitations. The results was limited to articles published in English that representing a potential limitation. The used model structure, sources of information, and time horizons varied across studies, and as a result, it was difficult to generalize the results of a study to other settings. A significant proportion of the studies has not reported the perspective in the analysis and funding disclosures. Most studies were conducted in the United States and China. Just less than %10 of the studies investigated treatment and vaccination, and approximately %88 of them focused on preventing and controlling interventions of COVID-19.
5. Conclusion
The results suggested the screening and social distancing as cost-effective alternatives to prevent and control COVID-19 in the long-time horizon. This study can help to choose the best strategies against COVID-19 pandemic.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Data statement
As this article is a systematic review, all research data are available in the tables, figures and articles cited in the references.
Ethical approval
This study requires formal ethical approval because it will not involve the collection of primary data.
Sources of funding
This paper was written independently; no company or institution supported it financially.
Author contribution
Conceptualization: Aziz Rezapour, Aghdas Souresrafil.
Project administration: Aziz Rezapour.
Data extraction: Aziz Rezapour, Aghdas Souresrafil.
Quality assessment: Aziz Rezapour, Aghdas Souresrafil.
Analysis: Aghdas Souresrafil, Mahsa Tashakori-Miyanroudi, Mona Heidarali, Mohammad Mehdi Peighambari.
Writing – original & editing: Aziz rezapour, Aghdas Souresrafil, Mona Heidarali, Mahsa Tashakori-Miyanroudi, Mohammad Mehdi Peighambari.
All authors read and approved the final manuscript.
Trial registry number
-
1.
Name of the registry: PROSPERO
-
2.
Unique Identifying number or registration ID: CRD42020199673
-
3.
Hyperlink to your specific registration (must be publicly accessible and will be checked): https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42020199673
Guarantor
Aghdas Souresrafil.
Declaration of competing interest
The authors declare that they have no conflict of interest.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijsu.2020.11.015.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Li Y., Mutchler J.E. Older adults and the economic impact of the COVID-19 pandemic. J. Aging Soc. Pol. 2020;32(4–5):477–487. doi: 10.1080/08959420.2020.1773191. [DOI] [PubMed] [Google Scholar]
- 2.Li X.-Z., Jin F., Zhang J.-G., Deng Y.-F., Shu W., Qin J.-M., et al. Treatment of coronavirus disease 2019 in Shandong, China: a cost and affordability analysis. Infect. Dis. Poverty. 2020;9(1):78. doi: 10.1186/s40249-020-00689-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jo M.W., Go D.S., Kim R., Lee S.W., Ock M., Kim Y.E., et al. The burden of disease due to COVID-19 in korea using disability-adjusted life years. J. Kor. Med. Sci. 2020;35(21):e199. doi: 10.3346/jkms.2020.35.e199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhao J., Jin H., Li X., Jia J., Zhang C., Zhao H., et al. Disease burden attributable to the first wave of COVID-19 in China, and the effect of timing on the cost-effectiveness of movement restriction policies. https://ssrncom/abstract=3605199. 2020 Available at: SSRN: [DOI] [PMC free article] [PubMed]
- 5.Sarah M., Bartsch M.C.F., McKinnell James A., O'Shea Kelly J., Wedlock Patrick T., Siegmund Sheryl S., Lee Bruce Y. The potential health care costs and resource use associated with COVID-19 in the United States. Health Aff. 2020;39(6):927–935. doi: 10.1377/hlthaff.2020.00426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Oh I.H., Ock M., Jang S.Y., Go D.S., Kim Y.E., Jung Y.S., et al. Years of life lost attributable to COVID-19 in high-incidence countries. J. Kor. Med. Sci. 2020;35(32) doi: 10.3346/jkms.2020.35.e300. e300-e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Forsythe S., Cohen J., Neumann P., Bertozzi S.M., Kinghorn A. The economic and public health imperatives around making potential coronavirus disease–2019 treatments available and affordable. Value Health. 2020;23(11):1427–1431. doi: 10.1016/j.jval.2020.04.1824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Flaxman S., Mishra S., Gandy A., Unwin H.J.T., Mellan T.A., Coupland H., et al. Estimating the effects of non-pharmaceutical interventions on COVID-19 in Europe. Nature. 2020;584(7820):257–261. doi: 10.1038/s41586-020-2405-7. [DOI] [PubMed] [Google Scholar]
- 9.Block P., Hoffman M., Raabe I.J., Dowd J.B., Rahal C., Kashyap R., et al. Social network-based distancing strategies to flatten the COVID-19 curve in a post-lockdown world. Nat. Human Behav. 2020;4(6):588–596. doi: 10.1038/s41562-020-0898-6. [DOI] [PubMed] [Google Scholar]
- 10.Moher D., Liberati A., Tetzlaff J., Altman D.G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ (Clin. Res. ed) 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shea B.J., Reeves B.C., Wells G., Thuku M., Hamel C., Moran J., et al. Amstar 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ (Clin. Res. ed) 2017;358:j4008. doi: 10.1136/bmj.j4008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Husereau D., Drummond M., Petrou S., Carswell C., Moher D., Greenberg D., et al. Consolidated health economic evaluation reporting Standards (CHEERS) statement. Value Health : J. Int. Soc. Pharm. Outcomes Res. 2013;16(2):e1–5. doi: 10.1016/j.jval.2013.02.010. [DOI] [PubMed] [Google Scholar]
- 13.van Mastrigt G.A.P.G., Hiligsmann M., Arts J.J.C., Broos P.H., Kleijnen J., Evers S.M.A.A., et al. How to prepare a systematic review of economic evaluations for informing evidence-based healthcare decisions: a five-step approach (part 1/3) Expert Rev. Pharmacoecon. Outcomes Res. 2016;16(6):689–704. doi: 10.1080/14737167.2016.1246960. [DOI] [PubMed] [Google Scholar]
- 14.Thunström L., Newbold S.C., Finnoff D., Ashworth M., Shogren J.F. The benefits and costs of using social distancing to flatten the curve for COVID-19. J. Benefit-Cost Anal. 2020:1–17. [Google Scholar]
- 15.Shaker M.S., Mosnaim G., Oppenheimer J., Stukus D., Abrams E.M., Greenhawt M. Health and economic outcomes of home maintenance allergen immunotherapy in select patients with high health literacy during the COVID-19 pandemic: a cost-effectiveness analysis during exceptional times. J. Allergy Clin. Immunol. Practice. 2020;8(7):2310–23121 e4. doi: 10.1016/j.jaip.2020.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schonberger R.B., Listokin Y.J., Ayres I., Yaesoubi R., Shelley Z.R. 2020. Cost Benefit Analysis of Limited Reopening Relative to a Herd Immunity Strategy or Shelter in Place for SARS-CoV-2 in the United States. medRxiv. [Google Scholar]
- 17.Savitsky L.M., Albright C.M. Preventing COVID-19 transmission on labor and delivery: a decision analysis. Am. J. Perinatol. 2020;37(10):1031–1037. doi: 10.1055/s-0040-1713647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Risko N., Werner K., Offorjebe O.A., Vecino-Ortiz A.I., Wallis L.A., Razzak J. Cost-effectiveness and return on investment of protecting health workers in low- and middle-income countries during the COVID-19 pandemic. PLoS One. 2020;15(10) doi: 10.1371/journal.pone.0240503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Paltiel A.D., Zheng A., Walensky R.P. medRxiv; 2020. COVID-19 Screening Strategies that Permit the Safe Re-opening of College Campuses. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Padula W.V., Malaviya S., Reid N.M., Tierce J., Alexander GJAaS. Economic value of treatment and vaccine to address the COVID-19 pandemic: a US cost-effectiveness and budget impact analysis. https://ssrncom/abstract=3586694. 2020 Available at: SSRN: [DOI] [PMC free article] [PubMed]
- 21.Neilan A.M., Losina E., Bangs A.C., Flanagan C., Panella C., Eskibozkurt G.E., et al. medRxiv; 2020. Clinical Impact, Costs, and Cost-Effectiveness of Expanded SARS-CoV-2 Testing in Massachusetts. 2020.07.23.20160820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Broughel J. The benefits of coronavirus suppression: a cost-benefit analysis of the response to the first wave of COVID-19. https://ssrncom/abstract=3636090. 2020 Available at: SSRN: [DOI] [PMC free article] [PubMed]
- 23.Wang Q., Shi N., Huang J., Cui T., Yang L., Ai J., et al. medRxiv; 2020. Effectiveness and Cost-Effectiveness of Public Health Measures to Control COVID-19: a Modelling Study. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Xu L, Zhang H, Deng Y, Wang K, Li F, Lu Q, et al. Cost-effectiveness Analysis of Antiepidemic Policies and Global Situation Assessment of COVID-19. arXiv. 2020.
- 25.Jiang Y., Cai D., Chen D., Jiang S. The cost-effectiveness of conducting three versus two reverse transcription-polymerase chain reaction tests for diagnosing and discharging people with COVID-19: evidence from the epidemic in Wuhan, China. BMJ Global Health. 2020;5(7) doi: 10.1136/bmjgh-2020-002690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rushworth S., Johnson B., Ashurst K., Davidson R., Paddy P., Mistry J., et al. medRxiv; 2020. Performance and Health Economic Evaluation of the Mount Sinai COVID-19 Serological Assay Identifies Modification of Thresholding as Necessary to Maximise Specificity of the Assay. [Google Scholar]
- 27.Aguas R., Mahdi A., Shretta R., Horby P., Landray M., White L.J. medRxiv; 2020. The Potential Health and Economic Impact of Dexamethasone Treatment for Patients with COVID-19. 2020.07.29.20164269. [Google Scholar]
- 28.Gandjour A. medRxiv; 2020. The Clinical and Economic Value of a Successful Shutdown during the SARS-CoV-2 Pandemic in Germany. 2020.05.12.20098996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gandjour A. medRxiv; 2020. How Much Reserve Capacity Is Justifiable for Hospital Pandemic Preparedness? A Cost-Effectiveness Analysis for COVID-19 in Germany. 2020.07.27.20162743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sharma N., Mishra P. Cost benefit analysis of COVID-19 lockdown in India. Int. J. Innovat. Med. Health Sci. 2020;12:34–40. [Google Scholar]
- 31.Dutta M., Husain Z. medRxiv; 2020. What Cost Decisiveness? A Cost Benefit Analysis of the Lockdown to Contain COVID-19 in India. 2020.07.07.20148338. [Google Scholar]
- 32.Mahmoudi N., Melia A., Lee D., Dalton C., FJAaS Paolucci. Cost-effectiveness analysis of COVID-19 case isolation. https://ssrncom/abstract=3603711 2020 Available at: SSRN:
- 33.Shlomai A., Leshno A., Sklan E.H., Leshno M. medRxiv; 2020. Cost-effectiveness Analysis of Social Distancing Strategies to Prevent SARS-CoV2 Spread. 2020.03.30.20047860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Khajji B., Kada D., Balatif O., Rachik M. A multi-region discrete time mathematical modeling of the dynamics of Covid-19 virus propagation using optimal control. J. Applied Math. Comput. 2020:1–27. doi: 10.1007/s12190-020-01354-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Asamoah J.K.K., Owusu M., Jin Z., Oduro F., Abidemi A., Gyasi E.O.J.C., Solitons, et al. Global stability and cost-effectiveness analysis of COVID-19 considering the impact of the environment: using data from Ghana. Chaos, Solit. Fractals. 2020:110103. doi: 10.1016/j.chaos.2020.110103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Reddy K.P., Shebl F.M., Foote J.H.A., Harling G., Scott J.A., Panella C., et al. medRxiv; 2020. Cost-effectiveness of Public Health Strategies for COVID-19 Epidemic Control in South Africa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nannyonga B.K., Wanyenze R.K., Kaleebu P., Ssenkusu J.M., Lutalo T., Makumbi F.E., et al. medRxiv; 2020. Estimating the Effect and Cost-Effectiveness of Facemasks in Reducing the Spread of the Severe Acute Respiratory Syndrome-Coronavirus 2 (SARS-CoV-2) in Uganda. 2020.06.11.20128272. [Google Scholar]
- 38.Sriwijitalai W., Wiwanitkit V. Cost-utility analysis for chest CT versus RT-PCR for COVID-19 detection. Int. J. Prev. Med. 2020;11(1):67. doi: 10.4103/ijpvm.IJPVM_83_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.