Abstract
Identification of risk factors is crucial to find ways to reduce rabies deaths. We investigated the hospital records of rabies deceased through contact tracing of the relatives of the victims using enhanced verbal autopsies (VA) to identify why the people had to die from rabies in recent years in Bangladesh. Patients whose deaths were confirmed by physicians based on the history of animal exposure and clinical signs were taken into account for VA. Socio-demographic profile of the deceased, animal exposure, nature of the wound, and history of post-exposure prophylaxis (PEP) data were obtained and analysed. The study found 256 cases in which the cause of death was attributed to rabies, most of the victims were male (71.88%), resided in the rural community (80.47%), dependent (49.22%), and children below the age of 15 years (47.27%). Dogs were the single most responsible (81.64%); however, cats (12.11%), jackals (3.91%) and mongoose (2.34%) were also found accountable for rabies incidence (P < 0.05). Significantly, limbs were the most common (67.97%) site of exposure, and the shortest incubation period was identified in the case of bites to head and face (P < 0.05). The majority (86.72%) of the deceased did not receive any PEP; whereas, 66.80% sought treatment from traditional healers. Among the deceased (13.28%, n = 34) who had received PEP, only 8.82% of them completed the full course of the vaccination regimen (P < 0.01); however, none of them had history of taking rabies immunoglobulin (RIG). The study recommends extensive public health awareness programs in the rural community and establishing methods to improve healthcare-seeking behaviours, including receiving PEP instead of visiting traditional healers. Moreover, the availability and accessibility of PEP in the government hospital facilities are desirable, and laboratory-based surveillance with compatible rapid data reporting may be incorporated in the existing policy.
Keywords: Epidemiology, Public health, Infectious disease, Bangladesh, Rabies, Vaccine, Verbal autopsy
Epidemiology; Public health; Infectious disease; Bangladesh; Rabies; Vaccine; Verbal autopsy.
1. Introduction
Rabies is a viral disease of high public health importance and its presentation has epidemiologically evolved in different ways worldwide. Still, the problem is complex, causing around 60,000 annual deaths globally [1, 2]. According to WHO, rabies-related death ranges from the thousands in Asia and Africa to a few hundred in Latin America [3]. Bangladesh ranks third in prevalence after India and China in South-East Asia, with estimated 2,100 deaths annually before 2010 [4]. A dense canine population, many of whom are unvaccinated and poorly cared for, and poor healthcare-seeking behaviours among animal bite victims were the main factors of causing human rabies in Bangladesh [5, 6, 7]. However, a national strategic plan for the elimination of rabies in Bangladesh has been in place since June 2010 [8]. The strategies initiated by the government of Bangladesh to eliminate rabies have been focused on (i) advocacy, communication, and social mobilization (ACSM), (ii) modern management of animal bites with tissue culture vaccine for post-exposure prophylaxis (PEP), (iii) mass dog vaccination (MDV), and (iv) dog population control. Since 2011, the ongoing strategic efforts results showed a decreasing trend in the number of human rabies-related deaths in the last few years, however, the numbers of cases are still noticeable [9]. It demands inclusive investigation on rabies deceased to explore why the people had to die from rabies for further progress towards the goal of rabies elimination by 2030.
Verbal autopsy (VA) is an essential public health tool for obtaining a reasonable direct estimation of the causal structure of mortality at a community or population level [10]. VA is carried out by interviewing the family members and/or caregivers of the deceased using a structured questionnaire to elicit signs and symptoms and other pertinent information that can later be used to assign a probable cause of death [11, 12]. Consequently, in the recent era, VA has become the primary source of information about causes of death in populations lacking vital registration and medical certification [13, 14]. Typically, in developing countries like Bangladesh, detailed records with epidemiological information of every deceased people are not well documented. Therefore, the objective of this study was to investigate the hospital records of the rabies deceased through contact tracing of the relatives of the victims to identify the underlying causes of rabies death in Bangladesh. These data might be useful for designing the existing rabies elimination program in targeting both the animal source and the human population at risk.
2. Materials and methods
2.1. Study area and population
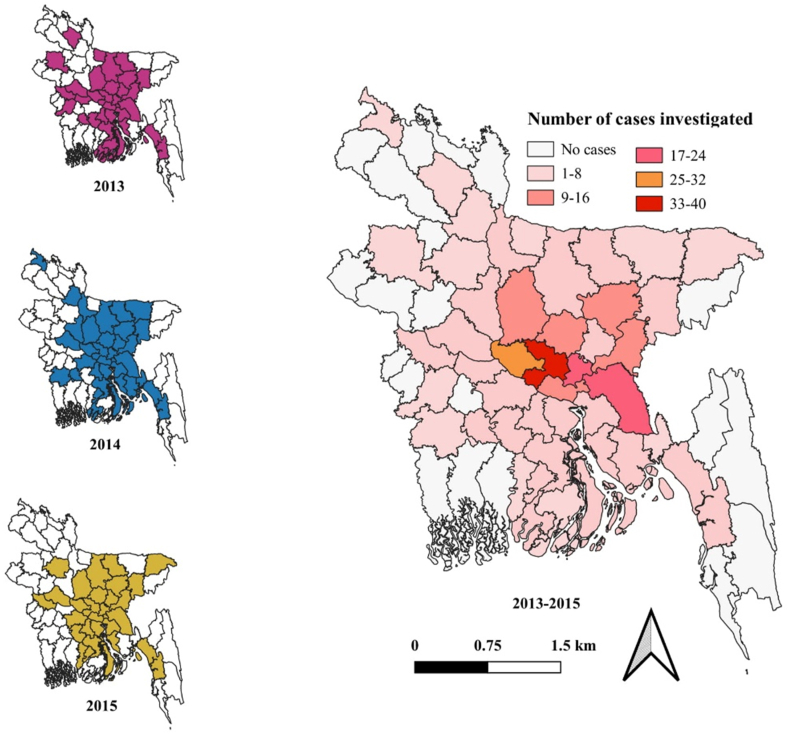
Bangladesh is administratively divided into 64 districts and 491 sub-districts and has a population of about 152.52 million [15]. There are 67 District Rabies Prevention and Control Center (DRPCC) in Bangladesh (one in each district sadar hospital and three more in the Dhaka city). According to the “National Rabies Elimination Program” guidelines, all DRPCCs refer their rabies confirmed patients (with patients and/or patient's record) to Infectious Disease Hospital (IDH), Dhaka as the central referral hospital for human rabies patients in Bangladesh. This study was conducted on the deceased who had died from rabies after being bitten by animals, registered at IDH during January 2013 to December 2015. A total of 256 human rabies death cases from IDH records were investigated subsequently in the following years (therefore, VA of human rabies death cases of 2013, 2014, and 2015 were performed in 2014, 2015, and 2016, respectively) through contact tracing of the relatives of the victims in different districts of Bangladesh and VA was performed using the standard VA tools (Figure 1).
Figure 1.
Distribution of rabies cases in different districts of Bangladesh, 2013–2015.
2.2. Study method and questionnaire
A retrospective cross-sectional study was conducted by the VA investigation team comprising of at least one trained veterinarian/physician from the central level (CDC), and one public health and one animal health worker from the local district health and livestock department respectively. The local team members assisted in tracing the incidence and convincing the respondent family by briefing the purpose of the study, whereas, VA was performed by the central level trained veterinarian/physician. The team visited the households of the deceased and interviewed the caregiver of the deceased or other close relatives. The respondents selected for interviewing were adults (≥18 years of age) involved in caring of the deceased during the period of illness. A standard WHO model of the VA questionnaire was used, which was structured into different sections including open questions about the circumstances of the death, socio-demographic data about the deceased, history of animal exposure, a checklist of signs and symptoms experienced before death including their durations, healthcare-seeking practices, and any available health records. The English questionnaire was translated into the local language (Bengali) with back-translation to ensure the accuracy. Before administering the questionnaires, respondents were briefed about the purpose of the study, and a written or verbal informed consent was obtained, in addition, highlighting that participation was voluntary, and their answers would be kept confidential. Only those participants who agreed verbally were interviewed, and in each case, at least one suitable respondent was confirmed for the VA.
2.3. Verbal autopsy (VA) and assigning the cause of death
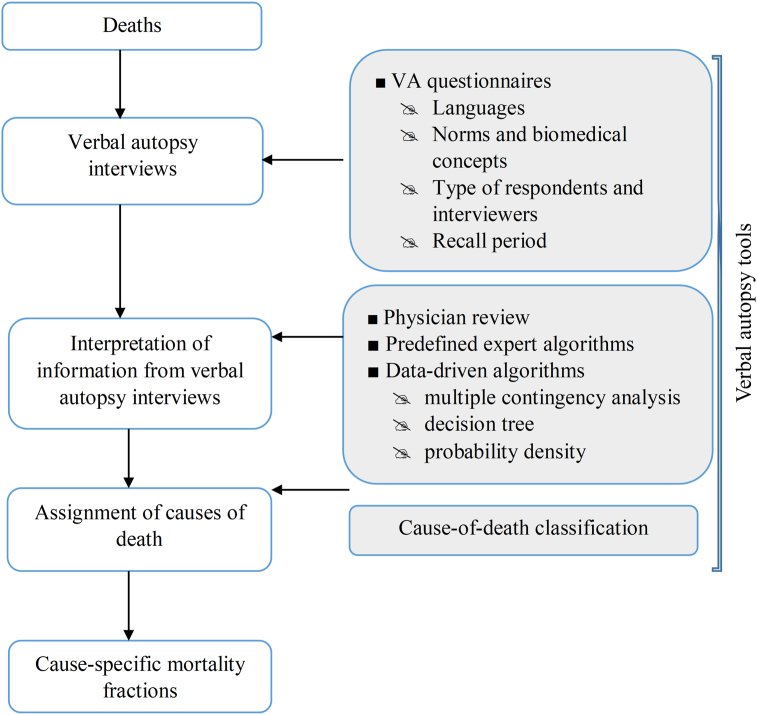
The VA process was followed as described by Soleman et al. [10] (Figure 2). To find out the possible cause of death, each questionnaire was interpreted by a qualified physician having local experience, as well as trained on reviewing the VA questionnaires and assigning the causes of death. The diagnosis of rabies was established from the history of animal exposure and clinical signs recorded by the physician's clinical diagnosis report and the VA tools data interpretation. Moreover, some specific points were set as inclusion criteria to confirm the death due to rabies by questioning the respondents including: a) whether the patient was diagnosed with rabies by a qualified physician, b) whether the patient had one or more clinical signs including hydrophobia, photophobia, aerophobia, restlessness, hyper-salivation, or limb paralysis with a history of animal bite or scratch, and c) whether the victim died within 4–10 days after the first symptoms appeared if no intensive care is instituted. Those cases found as no rabies after interpreting VA tools were excluded, whereas, the new cases that found during searching in community were included in the final analysis.
Figure 2.
Flow chart of verbal autopsy process and VA tools.
2.4. Data analysis
Data were entered into a database system of the Communicable Disease Control (CDC) unit of DGHS. After data cleaning, sorting and management, all categorical variables were analyzed through multiple contingency analysis for frequency distribution and probability testing (P > 0.05). While, regression analysis with the standard least square model for explaining the potential relationship between continuous dependent variables and independent categorical variables (P > 0.05) were carried out using the fit model platform of JMP 14 (100 SAS Campus Drive Cary, NC 27513-2414, USA) statistical software.
2.5. Ethical statements
This study was conducted under the component of operational research of Communicable Disease Control (CDC), Directorate General of Health Services (DGHS), reviewed by the Technical Working Group (TWG), and approved by the Director, Disease Control, and Line Director, CDC, DGHS, Ministry of Health and Family Welfare, Bangladesh (Memo No. DGHS/DC/Rabies/2014/2536). Before conducting the verbal autopsy, respondents (≥18-year-olds) were briefed about the purpose of the study, and a written or verbal informed consent was obtained. Verbal autopsies were performed from the appropriate respondents who were mostly involved in caring for the deceased during illness. If the most appropriate individual did not agree, then VA was taken from the next available person. Since no intervention was involved in responding to an interviewers, and all information was kept confidential, participants were not faced any study-related risks.
3. Results
Based on the primary baseline data from IDH, we found a total of 256 death cases during the study period with human rabies (86 in 2013, 104 in 2014, and 66 in 2015) that were initially aimed for VA subsequently in the following years. Based on the inclusion criteria after interpreting the VA tools, we found a cumulative total of 256 cases (87, 104, and 65 in 2013, 2014, and 2015 respectively) (Table 1). The prevalence of human rabies was present in forty-four districts out of 64 districts of Bangladesh. The highest incidence of human rabies was reported in Dhaka (n = 37) and Manikganj (n = 28) district. Both belonged to the Dhaka division (Table 2).
Table 1.
Number of human rabies death cases recorded at IDH, Dhaka, Bangladesh, 2013–2015.
| Year | Hospital Casesa | Excluded casesb | Included casesc | Total (confirmed by VA) |
|---|---|---|---|---|
| 2013 | 86 | - | 1 | 87 |
| 2014 | 104 | - | - | 104 |
| 2015 | 66 | 1 | - | 65 |
Sources: Infectious Disease Hospital (IDH), Mohakhali, Dhaka (The primary referral center for animal bites and rabies patients in Bangladesh).
Cases not found as rabies during verbal autopsy.
Cases found in the community searching during verbal autopsy but not recorded at IDH.
Table 2.
Verbal autopsy of district-wise distributed human rabies cases, 2013–2015.
| Sl. No. | District | Year |
No. of rabies cases | ||
|---|---|---|---|---|---|
| 2013 | 2014 | 2015 | |||
| 1. | Barisal | 1 | 2 | 1 | 4 |
| 2. | Bhola | 1 | 2 | 1 | 4 |
| 3. | Bogra | 0 | 0 | 1 | 1 |
| 4. | Barguna | 2 | 2 | 0 | 4 |
| 5. | Brahmanbaria | 6 | 9 | 1 | 16 |
| 6. | Chandpur | 2 | 2 | 1 | 5 |
| 7. | Chittagong | 1 | 1 | 1 | 3 |
| 8. | Comilla | 6 | 8 | 6 | 20 |
| 9. | Dhaka | 13 | 15 | 9 | 37 |
| 10. | Faridpur | 0 | 1 | 2 | 3 |
| 11. | Feni | 0 | 1 | 0 | 1 |
| 12. | Gaibandha | 0 | 1 | 0 | 1 |
| 13. | Gazipur | 4 | 6 | 1 | 11 |
| 14. | Gopalganj | 1 | 0 | 1 | 2 |
| 15. | Habiganj | 1 | 4 | 1 | 6 |
| 16. | Jamalpur | 0 | 2 | 0 | 2 |
| 17. | Jessore | 0 | 1 | 0 | 1 |
| 18. | Jhalokati | 0 | 1 | 2 | 3 |
| 19. | Jhenaidah | 1 | 0 | 0 | 1 |
| 20. | Kishoreganj | 6 | 2 | 1 | 9 |
| 21. | Kushtia | 1 | 0 | 1 | 2 |
| 22. | Lakshmipur | 1 | 1 | 1 | 3 |
| 23. | Madaripur | 2 | 2 | 2 | 6 |
| 24. | Manikganj | 12 | 9 | 7 | 28 |
| 25. | Munshiganj | 3 | 4 | 2 | 9 |
| 26. | Mymensingh | 1 | 1 | 4 | 6 |
| 27. | Naogaon | 1 | 0 | 0 | 1 |
| 28. | Narayanganj | 5 | 7 | 5 | 17 |
| 29. | Netrokona | 1 | 3 | 3 | 7 |
| 30. | Noakhali | 0 | 2 | 0 | 2 |
| 31. | Narail | 1 | 1 | 0 | 2 |
| 32. | Narsingdi | 1 | 3 | 4 | 8 |
| 33. | Pabna | 2 | 2 | 1 | 5 |
| 34. | Panchagarh | 0 | 1 | 0 | 1 |
| 35. | Patuakhali | 1 | 0 | 0 | 1 |
| 36. | Pirojpur | 0 | 0 | 1 | 1 |
| 37. | Rajbari | 2 | 0 | 0 | 2 |
| 38. | Rangpur | 1 | 0 | 0 | 1 |
| 39. | Shariatpur | 2 | 1 | 3 | 6 |
| 40. | Sherpur | 1 | 0 | 0 | 1 |
| 41. | Sirajganj | 0 | 2 | 0 | 2 |
| 42. | Sunamganj | 0 | 1 | 0 | 1 |
| 43. | Sylhet | 0 | 0 | 1 | 1 |
| 44. |
Tangail |
4 |
4 |
1 |
9 |
| Total | 87 | 104 | 65 | 256 | |
3.1. Socio-demographic profile of human rabies cases
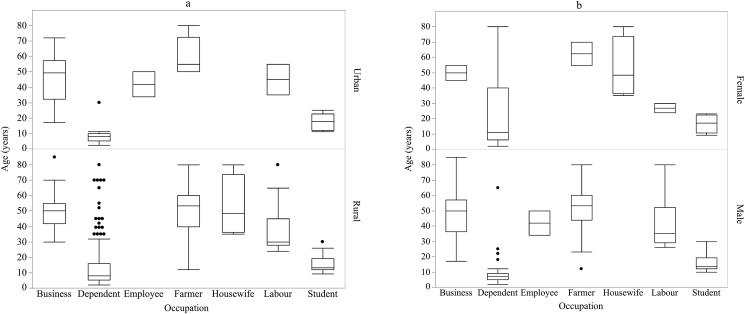
Almost half of the rabies deceased (47.27%) were under the age of 15 years with a median age of 19.05 years. The majority (80.47%) of human rabies victims resided in the rural community in comparison to urban (19.53%), and overall men constituted a higher proportion 2.6:1 (184/72) than females; however, the percentage of male victims was greater in the urban territory (80%) than rural (69.90%) in terms of rabies incidence in females (Table 3). It also found that the majority (49.22%) of victims were dependent (P = 0.002), i.e., no self-income source for their daily living expenditure except for other family members (Table 3). Most of the dependent were young and men (P > 0.0001) (Figure 3).
Table 3.
Socio-demographic profile of human rabies deceased (n = 256) in Bangladesh, 2013–2015 identified through VA.
| Variables | Category | Rural n (%) | Urban n (%) | Total n (%) | P- value∗ |
|---|---|---|---|---|---|
| Human rabies death | - | 206 (80.47) | 50 (19.53) | 256 | - |
| Age (years) | 0–15 | 99 (81.82) 48.05 |
22 (18.18) 44.00 |
121 (47.27) | 0.4431 |
| 16–30 | 25 (73.53) 12.14 |
9 (26.47) 18.00 |
34 (13.28) | ||
| 31–45 | 38 (88.37) 18.45 |
5 (11.63) 10.00 |
43 (16.80) | ||
| 46–60 | 30 (75.00) 14.56 |
10 (25.00) 20.00 |
40 (15.63) | ||
| 61- Above | 14 (77.78) 6.80 |
4 (22.22) 8.00 |
18 (7.03) | ||
| Gender | Male | 144 (78.26) 69.90 |
40 (21.74) 80.00 |
184 (71.88) | 0.1543 |
| Female | 62 (86.11) 30.10 |
10 (13.89) 20.00 |
72 (28.13) | ||
| Occupation |
Business | 19 (61.29) 9.22 |
12 (38.71) 24.00 |
31 (12.11) | 0.0022∗ |
| Dependent | 107 (84.92) 51.94 |
19 (15.08) 38.00 |
126 (49.22) | ||
| Employee | 0 (0.00) 0.00 |
2 (100) 4.00 |
2 (0.78) | ||
| Farmer | 30 (83.33) 14.56 |
6 (16.67) 12.00 |
36 (14.06) | ||
| Housewife | 8 (100) 3.88 |
0 (0.00) 0.00 |
8 (3.13) | ||
| Labour | 15 (88.24) 7.28 |
2 (11.76) 4.00 |
17 (6.64) | ||
| Student |
27 (75.0) 13.11 |
9 (25.0) 18.00 |
36 (14.06) |
||
| Total | 206 | 50 | 256 |
Multiple contingency analysis with α - level set as 0.05. The percentage of italics discretely represents the results within the rural and urban communities.
Figure 3.
Socio-demographic profile of human rabies deceased in Bangladesh, 2013–2015 identified through VA. a. Regression analysis with standard least square model between age and occupations by residence (P > 0.0001); b. Regression analysis with standard least square model between age and occupations by sex (P > 0.0001).
3.2. Characteristics of exposure animals
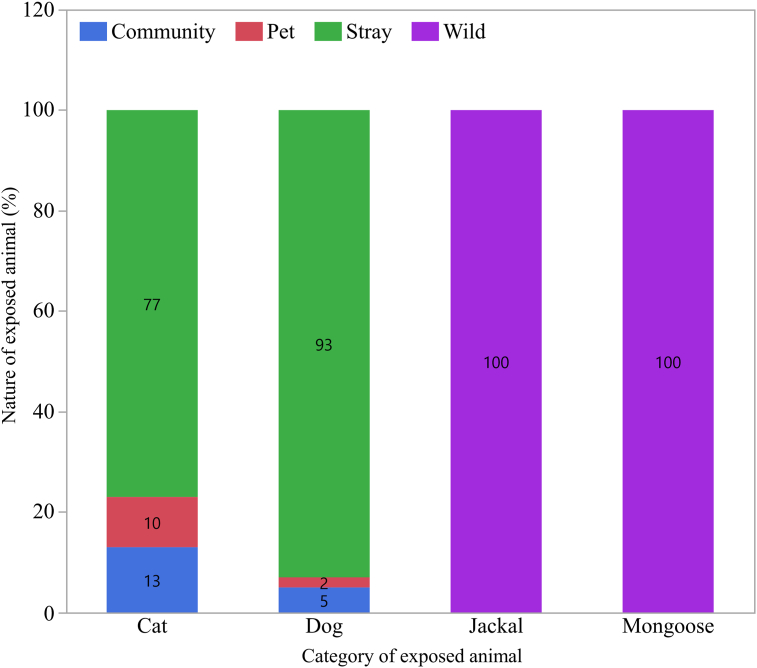
Details of animal exposure to the rabies deceased are shown in Table 4. The current study revealed that most human rabies caused by dogs (81.64%). However, cats also played a substantial role (12.11%), particularly in urban area (24%), and were followed by jackal (3.91%), and mongoose (2.34%). The majority of the biting animals were stray (free rooming, no ownership) (85.16%), while pet (confined movement, had full ownership), community (free rooming, had partial ownership as resided in the surrounding of home) and wild (predators, habited in their own nature) animals contributed 2.73%, 5.86%, and 6.25% of cases respectively. The majority (71.88%) of the animals were not found in the community after biting/scratching the victims. However, 17.58% of them were killed by the public. Among the exposed animals, dog comprised of 93% stray, 5% community, and only 2% pet; whereas, the cat was accounted for 77% stray, 13 % community and 10% pet, and all jackals and mongoose were wild in nature (Figure 4).
Table 4.
Details of animal to which human rabies deceased exposed (n = 256) in Bangladesh, 2013–2015 identified through VA.
| Variables | Category | Rural n (%) | Urban n (%) | Total n (%) | P- value∗ |
|---|---|---|---|---|---|
| Animal exposed | Cat | 19 (61.29) 9.22 |
12 (38.71) 24.00 |
31 (12.11) | 0.0242 |
| Dog | 173 (82.78) 83.98 |
36 (17.22) 72.00 |
209 (81.64) | ||
| Jackal | 8 (80.0) 3.88 |
2 (20.0) 4.88 |
10 (3.91) | ||
| Mongoose | 6 (100) 2.91 |
0 (0.00) 0.00 |
6 (2.34) | ||
| Type of animal | Community | 10 (66.67) 4.85 |
5 (33.33) 10.00 |
15 (5.86) | 0.4837 |
| Pet | 6 (85.71) 2.91 |
1 (14.29) 2.00 |
7 (2.73) | ||
| Stray | 176 (80.73) 85.44 |
42 (19.27) 84.00 |
218 (85.16) | ||
| Wild | 14 (87.50) 6.80 |
2 (12.50) 4.00 |
16 (6.25) | ||
| Fate of Animal |
Alive | 13 (81.25) 6.31 |
3 (18.75) 6.00 |
16 (6.25) | 0.2958 |
| Dead | 11 (100.00) 5.34 |
0 (0.00) 0.00 |
11 (4.30) | ||
| Killed | 38 (84.44) 18.45 |
7 (15.56) 14.00 |
45 (17.58) | ||
| Not found |
144 (78.26) 69.90 |
40 (21.74) 80.00 |
184 (71.88) |
||
| Total | 206 | 50 | 256 |
Multiple contingency analysis with α - level set as 0.05. The percentage of italics discretely represents the results within the rural and urban communities.
Figure 4.
Exposed animals and their types causing human rabies in Bangladesh, 2013–2015 identified through VA. Contingency analysis between exposed animals and their types (P > 0.0001).
3.3. Nature of wound and healthcare-seeking behaviours
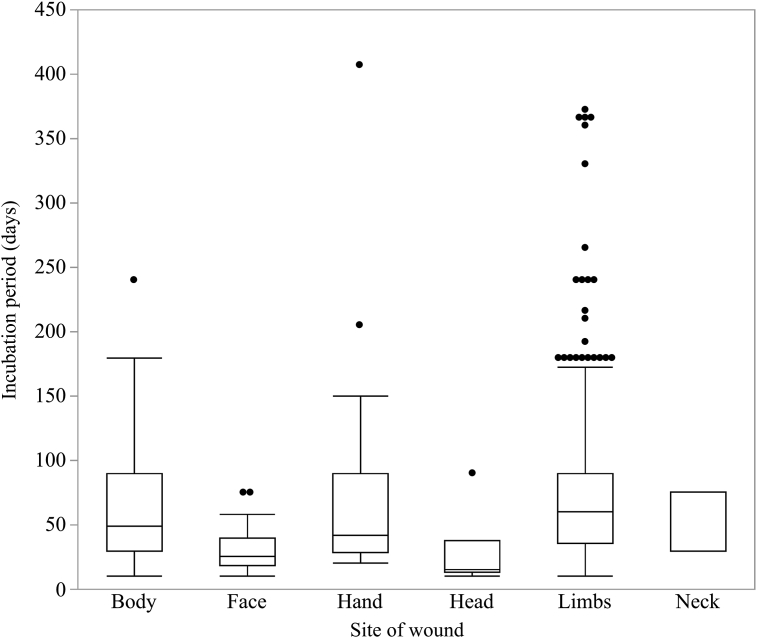
Over 90% of the cases, animal bites were accounted for causing rabies regardless of scratching, and only a single bite attributed for death in 50% cases (Table 5). The most common site for bites was one of the limbs (67.97%), and the majority (92.58%) of the bites were WHO category III exposure (Table 5). The incubation period ranged from 10 (lowest incubation period) to 407 days (highest incubation period) with a median of 59 days (Figure 5). The incubation period was lowest (0–30 days) for bites to the head and face, 83.33% and 71.43% respectively. While, the highest incubation period (>90 days) was found in the case of bites to the limbs in 24.14% cases (P = 0.002) (Table 5).
Table 5.
Nature of the wound and incubation period (n = 256) of human rabies deceased in Bangladesh, 2013–2015 identified through VA.
| Variable | Category | Incubation period (days) |
Total n (%) | P-value∗ | |||
|---|---|---|---|---|---|---|---|
| 0–30 | 31–60 | 61–90 | 90 -Above | ||||
| Nature of exposure | Bite | 75 (31.91) | 65 (27.66) | 50 (21.28) | 45 (19.15) | 235 (91.80) | 0.8762 |
| Scratch | 7 (33.33) | 6 (28.57) | 3 (14.29) | 5 (23.81) | 21 (8.20) | ||
| Site of wound | Body | 5 (33.33) | 4 (26.67) | 3 (20.00) | 3 (20.00) | 15 (5.86) | 0.0019 |
| Face | 15 (71.43) | 4 (19.05) | 2 (9.52) | 0 (0.00) | 21 (8.20) | ||
| Hand | 15 (40.54) | 11 (29.73) | 6 (16.22) | 5 (13.51) | 37 (14.45) | ||
| Head | 5 (83.33) | 0 (0.00) | 1 (16.67) | 0 (0.00) | 6 (2.34) | ||
| Limbs | 40 (22.99) | 52 (29.89) | 40 (22.99) | 42 (24.14) | 174 (67.97) | ||
| Neck | 2 (66.67) | 0 (0.00) | 1 (33.33) | 0 (0.00) | 3 (1.17) | ||
| Category of wound | Cat-II | 6 (31.58) | 5 (26.32) | 5 (26.32) | 3 (15.79) | 19 (7.42) | 0.9242 |
| Cat-III | 76 (32.07) | 66 (27.85) | 48 (20.25) | 47 (19.83) | 237 (92.58) | ||
| Number of wound | Multiple | 45 (35.43) | 35 (27.56) | 25 (19.69) | 22 (17.32) | 127 (49.61) | 0.6439 |
| Single | 37 (28.68) | 36 (27.91) | 28 (21.71) | 28 (21.71) | 129 (50.39) | ||
| Severity of wound |
Mild | 3 (25.00) | 4 (33.33) | 4 (33.33) | 1 (8.33) | 12 (4.69) | 0.7690 |
| Moderate | 17 (26.98) | 19 (30.16) | 14 (22.22) | 13 (20.63) | 63 (24.61) | ||
| Severe |
62 (34.25) |
48 (26.52) |
35 (19.34) |
36 (19.89) |
181 (70.70) |
||
| Total | 82 | 71 | 53 | 50 | 256 | ||
Multiple contingency analysis with α - level set as 0.05.
Figure 5.
Relationship between site of wounds and incubation period of rabies in the human rabies deceased in Bangladesh, 2013–2015 identified through VA. Regression analysis with standard least square model between incubation periods and site of wounds (P = 0.0038).
The majority (86.72%) of the deceased did not visit the hospital and had not received any rabies vaccine (Table 6). Among the victims who received PEP (13.28%) with intradermal rabies vaccine (IDRV) [commercial tissue culture vaccines, Rabipur® (Renata Pharmaceuticals, Ltd., Bangladesh)], but none of them had history of taking rabies immunoglobulin (RIG). In addition to that, only 8.82% of them received the complete vaccination series (4 doses, ID) [WHO approved Thai Red Cross (TRC) ID regimen] (Table 6). The study also reported that most of them (52.94%) had visited nearby DRPCC after experiencing animal bites to receive rabies vaccine free of cost (Table 6). On the other hand, approximately 68.80% of victims had resorted to treatment from traditional healers who approaches different magico-religious practices following a bite in the community (Table 6).
Table 6.
Healthcare-seeking behaviours by the human rabies deceased (n = 256) in Bangladesh, 2013–2015 identified through VA.
| Variables | Category | Rural n (%) | Urban n (%) | Total n (%) | P-value∗ |
|---|---|---|---|---|---|
| Treatment received | Traditional healer (Kabiraj) | 141 (68.45) | 30 (60.00) | 171 (66.80) | 0.6347 |
| Local doctor | 4 (1.94) | 2 (4.00) | 6 (2.34) | ||
| Physician (vaccine) | 26 (12.62) | 8 (16.00) | 34 (13.28) | ||
| Not taken | 35 (16.99) | 10 (20.00) | 45 (17.58) | ||
| History of vaccination |
Absent | 180 (87.38) | 42 (84.00) | 222 (86.72) | 0.5277 |
| Present |
26 (12.62) |
8 (16.00) |
34 (13.28) |
||
| Total |
206 |
50 |
256 |
||
| Frequency of vaccination | Complete | 0 (0.00) | 3 (37.50) | 3 (8.82) | 0.0011 |
| Incomplete | 26 (100.00) | 5 (62.50) | 31 (91.18) | ||
| Place of vaccination |
DRPCC | 12 (46.15) | 6 (75.00) | 18 (52.94) | 0.3067 |
| Municipality | 3 (11.54) | 0 (0.00) | 3 (8.82) | ||
| Pharmacy |
11 (42.31) |
2 (25.00) |
13 (38.24) |
||
| Total | 26 | 8 | 34 |
Multiple contingency analysis with α - level set as 0.05.
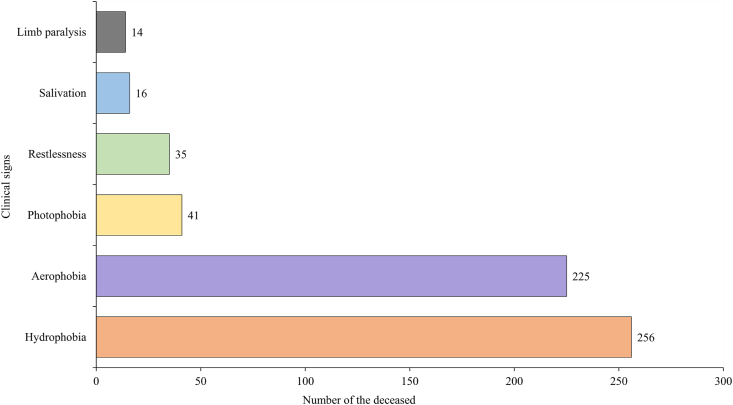
3.4. Clinical signs and symptoms, and reporting of death
All the victims had history of developing hydrophobia, which was accompanied by aerophobia in 87.89% victims, photophobia in 16.02%, and followed by restlessness (13.67%), drooling of saliva (6.25%), and limb paralysis (5.47%) (Figure 6). Almost all the patients (n = 255) were referred to the IDH, treated as outpatients, and reported only after confirming their death by follow-up contact through the medical team. However, due to lack of laboratory facility, medical autopsy was not undertaken in any of the cases; hence, no laboratory confirmation was possible.
Figure 6.
Clinical signs developed in the human rabies deceased in Bangladesh, 2013–2015 identified through VA.
4. Discussion
Human rabies remained an endemic disease in Bangladesh for the last few decades. However, the prevalence of human rabies appeared to be in decreasing trend in recent years [9]. It might be due to the potential effects of government initiative as targeted for rabies elimination by 2030. In this study, we traced 256 human rabies deceased in 44 different districts and performed VA from the caregivers of the victims. The VA conducted on rabies-related fatalities revealed that the majority of the victims were male (71.88%), under 15 years old (47.27%), and from a rural setting (80.47%) (Table 3). This result corresponded with some previous studies in Bangladesh and some other South-Asian countries [4, 6, 16, 17]. Almost half (49.2%) of the deceased were dependent and young men who relied on others, especially a family member, for financial support (Figure 3). This indicated that the deceased might be not have had the financial means for the vaccine cost, when unable to access at no cost from a government facility [18]. This also suggests a higher number (84.92%) of the dependent came from poor sections of the community. Some other studies reported that males constituted 67.1% in rabies deaths, of which 89.4% occurrence among the rural people in Bangladesh [19]; also rural incidence reported 71.1% in India [16] and 62% in Bhutan [17]. In our study, we found dogs were mainly (81.64%) responsible for rabies and the majority (93%) of them were stray. However, cats also played a significant role (12.11%), of which 77% was stray, 13% community and 10% pets. The remaining few deaths could be attributed to wild jackals and mongoose (Figure 4). Similarly, other studies have identified dogs as being the main responsible animal (>90%) for human rabies deaths in developing countries [2, 5, 17, 20, 21]. This difference with the current study might be due to effective results of mass scaling up of dog vaccination [9]. The vaccination status of the exposing animals was unknown, which indicates that a higher number of free-roaming/stray dogs with no registration and vaccination records were remained prevailing in Bangladesh.
The majority (91.80%) of the deceased were exposed by animal bite rather than a scratch with WHO category III. However, the site of bite/scratch mostly (67.97%) took place on the patient's limb region, followed by hands, face, body, head, and neck. Similar findings were also documented from some other studies that lower limbs were principal site of the animal's bite [16, 17]. In our study, we found a significance difference in the incubation period depending on the sites of exposure. The rabies cases from bites to the head and face had a shorter incubation period (Table 5). This result was consistent with previous findings suggesting the incubation period varied depending on a wide range of factors, including the wound location, nature of bite, virus inoculum dose, and host associated factors [16, 22, 23, 24, 25]. Our study reported the longest incubation period as 407 days in case of bite in the hand; however, the incubation period varied between 13 and 367 days when victims were bitten on their limbs (Figure 5). Some previous studies also reported much longer incubation periods than usual, depending on the location of animal exposure [16, 26]. So, considering the maximum incubation period, the study suggests the necessity of taking PEP for the person who has a history of animal exposure fall in with WHO wound category II and III, but did not receive PEP even after a long period.
Despite the lack of laboratory facilities in Bangladesh for confirmatory diagnosis for human rabies, the clinical signs of rabies included hydrophobia, aerophobia, photophobia, restlessness, hyper-salivation, and/or limb paralysis along with the appearances of a rapidly fatal encephalopathy. These factors along with evidence of animal exposure history provided the basis for establishing that rabies virus was the causal agent in the fatal cases of this study. In our study, we found hydrophobia in 100% of the cases; we also observed a high proportion (87.89%) of the deceased manifested with aerophobia, which is another hallmark feature of rabies. A substantial number of deceased had developed photophobia (16.02%), followed by restlessness (13.67%), drooling of saliva (6.25%), and limb paralysis (5.47%) during the time of their illness (Figure 6). These findings also supported other study results of clinical symptoms developed in rabies patients [19, 27].
The study revealed that the majority of the rabies deceased (86.72%) had not received any rabies prophylaxis following animal exposure. It also established that most of the victims (68.80%) primarily sought treatment from traditional healers (Kabiraj) instead of visiting the hospital. These sorts of treatment-seeking behaviour remained common among the community, due to lack of proper awareness and belief in different kinds of myths and dogmas or uncertainty of getting vaccine due to shortage of accessibility in the government facilities [6, 7]. However, a smaller number (13.28%) of cases had history of receiving rabies vaccine, but a large number of them (91.18%) did not complete the full course of vaccination regimen and the use of RIG was absent (Table 6). Although this study did not assess the exact reasons of having incompletion of PEP course, however, this might be due to the shortage of free vaccine accessibility and the inability of purchasing the vaccine as of high price, in addition, treatment delays after being exposed to a suspected rabid animal may cause the RIG not to be used. Song et al. [24] reported that 66.3% of people did not take any measure for PEP, 27.6% received inadequate PEP, and only 6.0% received a full regime of PEP in China. Another study by Tenzin et al. [28] revealed that 40% of the rabies victims received an incomplete vaccine course in Bhutan; whereas, approximately 33% of the patient with dog bite cases ignored to come for the last dose of the PEP series and failed to finish a complete series of PEP recorded in Thailand by Sriaroon et al. [29]. This might be driven by a gross negligence among the people, reflect their poor socio-economic conditions [30], distance between hospital facilities and victims' residence as one center in one district in Bangladesh as well as lack of adequate focal points for vaccine accessibility like in other developing countries [26, 31, 32]. Although over the last few years, there has been a significant improvement in the overall healthcare system in this country; a budget deficiency for the prevention and control of rabies program for availability and accessibility of rabies vaccine in the tertiary health facility centers remains. With the adequate amount of modern tissue culture vaccine and RIG, particularly in the rural areas, it is expected that the incidence of human rabies deaths will decline. Simultaneously, extensive awareness program through ACSM for rabies, particularly for the rural community, children's intercommunication with dogs and their pets, inclusion of cats with current mass dog vaccination (MDV) program, and the promotion of responsible dog ownership to control stray animal population burden and bite incidence is equally important for reducing rabies mortality in Bangladesh.
5. Limitation of the study
The present study was not beyond the limitations. Foremost one was that the diagnosis of rabies was confirmed by clinical signs and history of animal exposure; no laboratory confirmation was done in any of the cases. Next, there is always a risk that the respondent sometimes did not correctly recall the events during the autopsy. To minimize this, we tried to collect accurate data by interviewing the most appropriate personnel as a respondent who had engaged in caring for the patients very closely at the time of the deceased illness. Regardless of these weaknesses, we firmly believe that our study has revealed some valuable information about the causes exists for the prevailing of rabies in Bangladesh and it could be helpful to improve the overall situation towards the elimination of rabies in developing countries like Bangladesh.
6. Conclusion
It is necessary to arrange the extensive public health awareness program for rabies through education and information materials (EIM) and strongly address traditional healer's role for the burden of rabies in the rural community. Besides, availability and accessibility of adequate WHO pre-qualified tissue culture rabies vaccine are desirable to ensure the free provision of PEP in the government hospital facilities throughout the country. Moreover, laboratory-based surveillance, compatible rapid data reporting, and an adequate risk assessment system might be helpful for strengthening the rabies elimination program towards zero rabies transmission by 2030.
Declarations
Author contribution statement
M.S. Rana: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data; Wrote the paper.
U.R. Siddiqi: Conceived and designed the experiments; Wrote the paper.
B. Ahmed: Conceived and designed the experiments; Contributed reagents, materials, analysis tools or data.
S. Ghosh: Conceived and designed the experiments; Performed the experiments.
M.K. Islam., M.R.A. Shah and S.M. Ullah: Performed the experiments.
S.M.E. Ali: Performed the experiments; Contributed reagents, materials, analysis tools or data.
A.A. Jahan: Analyzed and interpreted the data; Wrote the paper.
A.K.M. Shamsuzzaman: Contributed reagents, materials, analysis tools or data.
Funding statement
This work was supported by the operational research budget of the Communicable Disease Control (CDC) unit, Directorate General of Health Services, Ministry of Health and Family Welfare, Bangladesh.
Declaration of interests statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
Acknowledgements
The authors are grateful to the respective district Civil Surgeon (CS) and District Livestock Officer (DLO) for their staff support to find out the specific household during the verbal autopsy. The authors sincerely appreciate the support of the In-Charge and Staff of the IDH for the collection of baseline data for this study. The authors also thank Peter Krawczel, Helsinki One Health, University of Helsinki, Helsinki, Finland for English proofreading of this manuscript.
References
- 1.Taylor L. Eliminating canine rabies: the role of public–private partnerships. Antivir. Res. 2013;98:314–318. doi: 10.1016/j.antiviral.2013.03.002. [DOI] [PubMed] [Google Scholar]
- 2.Hampson K., Coudeville L., Lembo T. Estimating the global burden of endemic canine rabies. PLoS Neglected Trop. Dis. 2015;9 doi: 10.1371/journal.pntd.0003709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.WHO . 2018. WHO Expert Consultation on Rabies, Third Report: WHO Technical Series Report No. 1012, Geneva.https://www.who.int/rabies/resources/who_trs_1012/en/ Available at: [Google Scholar]
- 4.Hossain M., Ahmed K., Bulbul T. Human rabies in rural Bangladesh. Epidemiol. Infect. 2012;140:1964–1971. doi: 10.1017/S095026881100272X. [DOI] [PubMed] [Google Scholar]
- 5.Hossain M., Bulbul T., Ahmed K. Five-year (January 2004-December 2008) surveillance on animal bite and rabies vaccine utilization in the Infectious Disease Hospital, Dhaka, Bangladesh. Vaccine. 2011;29:1036–1040. doi: 10.1016/j.vaccine.2010.11.052. [DOI] [PubMed] [Google Scholar]
- 6.Ghosh S., Chowdhury S., Haider N. Awareness of rabies and response to dog bites in a Bangladesh community. Vet. Med. Sci. 2016;2:161–169. doi: 10.1002/vms3.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alam A.N., Siddiqua M., Casal J. Knowledge and attitudes about rabies in dog-bite victims in Bangladesh. One Health. 2020;9:100126. doi: 10.1016/j.onehlt.2020.100126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.MIS, Health Bulletin . Directorate General of Health Services, Ministry of Health and Family Welfare; Bangladesh: 2018. Management Information System.https://dghs.gov.bd/images/docs/Publicaations/HB%202018%20final.pdf Available at: [Google Scholar]
- 9.Sumon G., Sohel R.M., Kamrul I.M. Trends and clinico-epidemiological features of human rabies cases in Bangladesh 2006–2018. Sci. Rep. 2020;10 doi: 10.1038/s41598-020-59109-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Soleman N., Chandramohan D., Shibuya K. Verbal autopsy: current practices and challenges. Bull. World Health Organ. 2006;84:239–245. doi: 10.2471/blt.05.027003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mobley C.C., Boerma J.T., Titus S. Validation study of a verbal autopsy method for causes of childhood mortality in Namibia. J. Trop. Pediatr. 1996;42:365–369. doi: 10.1093/tropej/42.6.365. [DOI] [PubMed] [Google Scholar]
- 12.Mirza N.M., Macharia W., Wafula E. Verbal autopsy: a tool for determining cause of death in a community, East Afr. Med. J. 1990;67:693–698. [PubMed] [Google Scholar]
- 13.Fottrell E., Byass P. Verbal autopsy: methods in transition. Epidemiol. Rev. 2010;32:38–55. doi: 10.1093/epirev/mxq003. [DOI] [PubMed] [Google Scholar]
- 14.Murray C.J., Lopez A.D., Feehan D.M. Validation of the symptom pattern method for analyzing verbal autopsy data. PLos Med. 2007;4:e327. doi: 10.1371/journal.pmed.0040327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.BBS . Bangladesh Burea of Statistics; 2012. Population and Housing Census 2011; p. 4.http://www.bbs.gov.bd/site/page/47856ad0-7e1c-4aab-bd78-892733bc06eb/Population-and-Housing-Census Available at: [Google Scholar]
- 16.Sudarshan M.K., Madhusudana S.N., Mahendra B.J. Assessing the burden of human rabies in India: results of a national multi-center epidemiological survey. Int. J. Infect. Dis. 2007;11:29–35. doi: 10.1016/j.ijid.2005.10.007. [DOI] [PubMed] [Google Scholar]
- 17.Tenzin, Dhand N.K., Gyeltshen T. Dog bites in humans and estimating human rabies mortality in rabies endemic areas of Bhutan. PLoS Neglected Trop. Dis. 2011;5 doi: 10.1371/journal.pntd.0001391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Knobel D.L., Cleaveland S., Coleman P.G. Re-evaluating the burden of rabies in Africa and Asia. Bull. World Health Organ. 2005;83:360–368. [PMC free article] [PubMed] [Google Scholar]
- 19.Haque M.S., Yeasmin T., Islam M.M. Epidemiological characteristics of human rabies at infectious disease hospital, Dhaka, Bangladesh. J. Child Health. 2011;35:102–107. [Google Scholar]
- 20.Digafe R.T., Kifelew L.G., Mechesso A.F. Knowledge, attitudes and practices towards rabies: questionnaire survey in rural household heads of Gondar Zuria District, Ethiopia. BMC Res. Notes. 2015;8:400. doi: 10.1186/s13104-015-1357-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rahman M.M., Salimuzzaman M., Alam M.B. Human rabies in Bangladesh - A study of 684 cases. J. Med. 2007;8:3–6. [Google Scholar]
- 22.Qi L., Su K., Shen T. Epidemiological characteristics and post-exposure prophylaxis of human rabies in Chongqing, China. BMC Infect. Dis. 2018;18:6. doi: 10.1186/s12879-017-2830-x. 2007–2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Susilawathi N.M., Darwinata A.E., Dwija I.B. Epidemiological and clinical features of human rabies cases in Bali 2008-2010. BMC Infect. Dis. 2012;12:81. doi: 10.1186/1471-2334-12-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Song M., Tang Q., Wang D.M. Epidemiological investigations of human rabies in China. BMC Infect. Dis. 2009;9:210. doi: 10.1186/1471-2334-9-210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hampson K., Dushoff J., Cleaveland S. Transmission dynamics and prospects for the elimination of canine rabies. PLoS Biol. 2009;7 doi: 10.1371/journal.pbio.1000053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dimaano E.M., Scholand S.J., Alera M.T.P. Clinical and epidemiological features of human rabies cases in the Philippines: a review from 1987 to 2006. Int. J. Infect. Dis. 2011;15:e495–e499. doi: 10.1016/j.ijid.2011.03.023. [DOI] [PubMed] [Google Scholar]
- 27.Chowdhury J., Modak K. Report on rabies in West Bengal. J. Indian Med. Assoc. 1983;81:69–74. [PubMed] [Google Scholar]
- 28.Tenzin, Dhand N.K., Ward M.P. Human rabies post exposure prophylaxis in Bhutan, 2005-2008: trends and risk factors. Vaccine. 2011;29:4094–4101. doi: 10.1016/j.vaccine.2011.03.106. [DOI] [PubMed] [Google Scholar]
- 29.Sriaroon C., Jaijaroensup W., Tantawichien T. Common dilemmas in managing rabies exposed subjects. Travel Med. Infect. Dis. 2005;3:1–7. doi: 10.1016/j.tmaid.2004.05.003. [DOI] [PubMed] [Google Scholar]
- 30.Penjor K., Tenzin T., Jamtsho R.K. Determinants of health seeking behavior of animal bite victims in rabies endemic South Bhutan: a community-based contact-tracing survey. BMC Publ. Health. 2019;19:237. doi: 10.1186/s12889-019-6559-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hampson K., Dobson A., Kaare M. Rabies exposures, post-exposure prophylaxis and deaths in a region of endemic canine rabies. PLoS Neglected Trop. Dis. 2008;2:e339. doi: 10.1371/journal.pntd.0000339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Permpalung N., Wongrakpanich S., Korpaisarn S. Trend of human rabies prophylaxis in developing countries: toward optimal rabies immunization. Vaccine. 2013;31:4079–4083. doi: 10.1016/j.vaccine.2013.06.083. [DOI] [PubMed] [Google Scholar]