Highlights
-
•
SARS-CoV-2 pandemic is changing the perioperative surgical practice worldwide.
-
•
Specific protocols are essential for COVID-19 patient undergoing emergency surgery.
-
•
COVID-19 asymptomatic patients can safely undergo major emergency surgeries.
-
•
The first surgery for oesophagel metastatic lesion was performed on COVID-19 patient.
-
•
Adequate resource planning for healthcare workers can minimise the risk of infection.
Keywords: COVID-19, Cerebellar metastasis, Suboccipital craniectomy, PPE, Case report
Abstract
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) outbreak has an impact on the delivery of neurosurgical care, and it is changing the perioperative practice worldwide. We present the first case in the literature of craniectomy procedure and asportation of a solitary cerebellar metastasis of the oesophagus squamous carcinoma in a 77 years old woman COVID-19 positive. In these particular circumstances, we show that adequate healthcare resources and risk assessments are essential in the management of COVID-19 patients referred to emergency surgery.
Presentation of case
The case here presented was treated in 2019 for squamous carcinoma of the oesophagus. In April 2020, she presented a deterioration of her clinical picture consisting of dysphagia, abdominal pain, hyposthenia and ataxia. A Head CT scan was performed, which showed the presence of a solitary cerebellar metastasis. Her associated SARS-CoV-2 positivity status represented the principal clinical concern throughout her hospitalisation.
Discussion
The patient underwent a suboccipital craniectomy procedure with metastasis asportation. She tested positive for SARS-CoV-2 in the pre- and post-operative phases, but she was not admitted to the intensive care unit because she did not present any respiratory complications. Her vital parameters and inflammation indexes fell within the reference ranges, and she was kept in isolation for 16 days in our neurosurgical unit following strict COVID-19 measures. She was asymptomatic and not treated for any of the specific and non-specific symptoms of COVID-19.
Conclusion
This is the first case reported of solitary cerebellar metastasis of oesophagus carcinoma operated on a COVID-19 positive patient. It shows that asymptomatic COVID-19 positive patients can undergo major emergency surgeries without the risk of infecting the operating team if adequate Personal Protection Equipment (PPE) is used. The patient remained asymptomatic and did not develop the disease’s active phase despite undergoing a stressful event such as a major emergency neurosurgical procedure. In the current crisis, a prophylactic COVID-19 screening test can identify asymptomatic patients undergoing major emergency surgery and adequate resource planning and Personal Protective Equipment (PPE) for healthcare workers can minimise the effect of the COVID-19 pandemic.
1. Introduction
1.1. Background
Oesophageal carcinoma frequently metastasises in the lungs, pleura, liver, stomach, peritoneum, kidney, adrenal gland, and bones [1]. Brain metastasis in primary oesophageal cancer patients are considered very rare, incidence estimated at between 1.4% and 6.6% according to retrospective reviews of patients treated for oesophageal and oesophagogastric junction cancers [2,3]. Surgical treatment and favourable Karnofsky Performance Status (KPS) are associated with longer survivals for selected patients with brain metastasis from oesophageal carcinoma [4]. The Chemoradiotherapy for Esophageal Cancer Followed by Surgery Study (CROSS) trial established tri-modality therapy with 49.4 months median survival in the combined treatment group [5]. During the SARS-CoV-2 pandemic, when cases often suffer severe acute respiratory syndrome, surgery should be offered only to patients with extensive lesions causing symptoms related to mass effect and vasogenic oedema, whose survival is expected to be greater than three months [6]. In the public health emergency for the COVID-19 outbreak, surgery has been reduced for urgencies and cerebral and spinal oncological cases; some of the neurosurgical unit personnel have been assigned to the COVID-19 units [7]. We report a case of a 77 years old woman, previously treated for oesophageal carcinoma in our centre, arriving at our unit with chief neurological complaints. The clinical examination revealed ataxia, nausea, vomiting and headache, which prompted us to perform urgent craniectomy and metastasis removal. During her hospitalisation, she resulted positive for COVID-19, and she has been tested for SARS-CoV-2 in the pre- and post-operative phases. The operation took place in April in -----Name of centre blinded----- in a dedicated operating theatre. This report describes for the first time in the literature a case solitary cerebellar metastasis removal of oesophageal carcinoma in a COVID-19 positive patient. This case report demonstrates that major neurological surgeries such as craniectomy and asportation of cerebellar metastasis can be performed in asymptomatic COVID-19 patients and that adequate resource planning and Personal Protective Equipment (PPE) are essential to reduce the healthcare-associated infections (HCAIs) risk in the current COVID-19 pandemic.
2. Presentation of case
The presented work has been reported in line with the SCARE criteria [8], and it reports the first-in-man case intervention of a solitary cerebellar metastasis of oesophagus origin on a COVID-19 positive patient. Therefore it has been registered at the Research Registry and it has been assigned the following Research Registry unique identifying number (UIN) researchregistry6241.
2.1. Patient history and examination
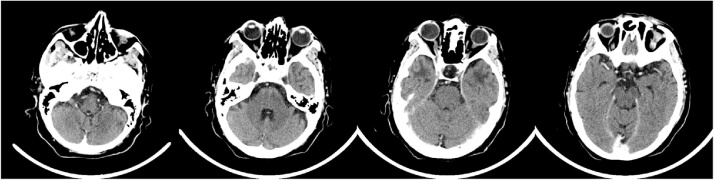
The patient was treated (September 2019) for oesophageal squamous carcinoma with radiotherapy and chemotherapy in our General Surgical and Oncology Department. On a routine CT Total Body scan performed in January 2020 for tumour follow-up, no metastasis was found (Fig. 1), and the cancer staging was T3-N0-M0.
Fig. 1.
Total Body CT scan, head images which show no tomodensitometric changes or abnormalities and no focal areas of altered intra and extra-axial enhancement. Liquor spaces are of regular density. The sagittal structures of the midline are on axis.
In April 2020, the patient walked into the Emergency Room presenting with dysphagia, abdominal pain, hyposthenia, ataxia and mild headache. In the patient’s medical history, arterial hypertension was the only co-morbidity besides the oesophageal carcinoma. The other parameters reported included the ASA Physical Status Classification System ASA Grade of III, ECOG (Eastern Cooperative Oncology Group) Performance Status of three, the Recursive Partitioning Analysis of the Radiation Therapy Oncology Group resulted in class II and the Karnofsky Performance Status (KPS) of 80 as illustrated in Table 1.
Table 1.
Patient anamnesis.
| Patient Characteristics | Data |
|---|---|
| Age | 77 years |
| Sex | F |
| ASA Gradea | III |
| Weight | 78 kg |
| BMI | 32.05 |
| ECOG PSb | 3 |
| RPA Classc | II |
| KPSd | 80 |
| Co-morbidities | Arterial Hypertension |
| Primitive Cancer | Oesophageal Squamous Carcinoma |
| Staginge | T3 N0 M1 |
| Type of COVID–19 Screening | Swab Test f |
ASA Physical Status Classification System.
ECOG (Eastern Cooperative Oncology Group) Performance Status.
Recursive Partitioning Analysis of the Radiation Therapy Oncology Group.
Karnofsky Performance Status.
American Joint Committee on Cancer (AJCC) Staging System.
Molecular Fast Track Diagnostics (FTD) SARS-CoV-2 Assay test.
In order to rule out the presence of metastatic dissemination, a chest and abdomen CT scan was performed, which did not show any signs of metastasis of the oesophagal tumour. Later, the patient developed a clinical picture of neurological symptoms such as ataxia and progressive sensorium deterioration.
2.2. Pre-operative care
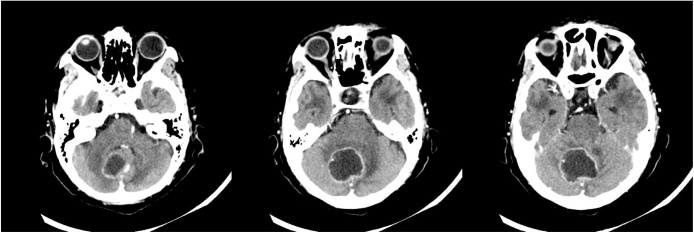
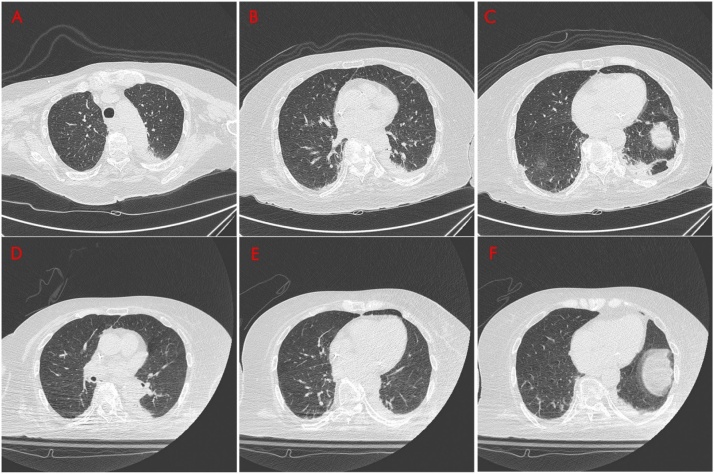
Given the rapid worsening of the neurological status, an urgent head CT was performed, which showed a solitary metastasis in the cerebellum area with compression of the 4th ventricle and hydrocephalus onset (Fig. 2). According to our hospital COVID-19 protocol, together with the Italian Ministry of Health recommendations, we proceeded with taking a swab sample to test the patient using the Molecular Fast Track Diagnostics (FTD) for the specific detection of SARS-CoV-2, this uses real-time PCR to detect RNA from this virus. The test resulted positive for the virus nucleocapsid (N) gene of COVID-19. Also, we performed a pre-operative chest CT scan; using medical imaging tools as the second approach of COVID-19 to assess the degree of the infection. The chest CT showed slight atelectasis in the left lung basal field, which was incompatible with the active phase of COVID-19 infection (Fig. 3, A-B-C). The patient showed no COVID-19 associated symptoms such as fever, low oxygen saturation, or dyspnea on clinical examination.
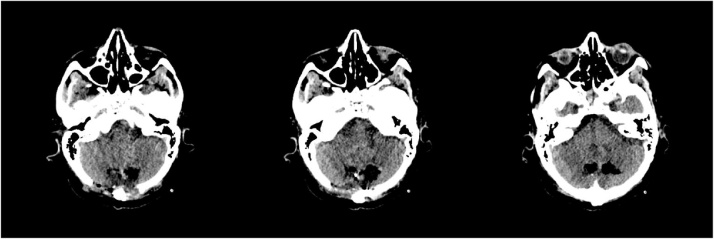
Fig. 2.
Pre-Operative enhanced axial Head-CT scan showing a median cerebellar metastatic lesion with central hypodense appearance of 3.6 × 3.3 cm and extensive mass effect causing marked compression of the 4th ventricle and the onset of hydrocephalus.
Fig. 3.
Pre- and post-operative Chest CTs show slight atelectasis in the area of the left lung’s basal field, incompatible with an active infection of COVID-19. The apical (A), the hilar (B) and the basal (C) aspect of lung four days before surgery compared to the apical (D), the hilar (E) and the basal (F) aspect of lung 48 h after surgery. The latter shows a reduction in the appreciable parenchymal consolidation at the base of the apical-dorsal segment of the upper lobe of the left lung and in the lower lobe of the homolateral one. Thin hyperdense bands are located at the base of the lower lobe of the right lung.
2.3. Surgical procedure
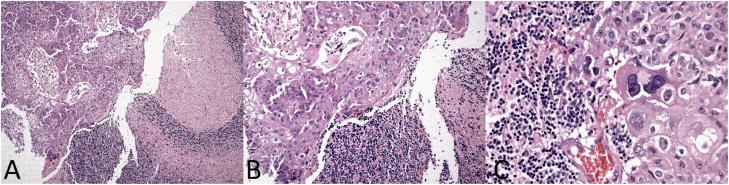
We performed a paramedian suboccipital craniectomy approach in the Concorde position; the paramedian exposure is the most suitable exposure for the resection of midline tumours of the posterior fossa [9]. After the opening of the Magna Cistern, we isolated the lesion from parenchyma tissue. Once removed the lesion with the ultrasonic aspirator, we performed a watertight dural closure. General anaesthesia was used in this case for the posterior fossa operation; anaesthesia duration was 240 min; drugs and intraoperative parameters are shown in detail in Table 2. Histological examination of the lesion confirmed the metastasis of keratinising oesophageal squamous cell carcinoma (ESCC) (Fig. 4).
Table 2.
Surgery management data.
| Intraoperative | Type | Dose |
|---|---|---|
| Drugs | Propofol | 250 mg a |
| Rocuronium | 60 mg a | |
| Fentanyl | 150 μg a | |
| Remifentanil | 4 mg a | |
| Antibiotic Prophylaxisb | Cefazolin | 2 g |
| Arterial Blood data | FiO2 | 50% |
| pCO2 | 25–26 mmHg | |
| pO2 | 98–99 mmHg | |
| Halogen Ethers | Sevoflurane | 3–2.7% |
| Duration | Surgery | 170 minutes |
| General Anesthesia | 240 min | |
| Recovery Room c | 100 min |
Total dose of anaesthetics during general anaesthesia.
Started within one hour before surgical incision.
Recovery phase after surgery is in the Recovery Room.
Fig. 4.
Histological images of keratinising oesophageal squamous cell carcinoma (ESCC) localised in the cerebellar tissue. Infiltrating squamous cell carcinoma cells in the cerebellar cortex (left side) (A: ×10, H&E). Diffuse infiltration in the cerebral cortex (B: ×20, H&E). Polymorphic, atypical and poorly differentiated cells with hyperchromatic nuclei (C: ×40, H&E).
2.4. Post-operative care
Post-operative care was regular and uneventful, with no residual neurological deficits found at the neurological examination. The patient was not presenting dyspnea or desaturation and was admitted to the warm isolation room. Inflammation indexes such as C-Reactive Protein (CRP), fever, White Blood Cell count (WBC) markedly increased after surgery (Table 3) but normalised after a few days in the range of 12.03 103/mmc for WBC and 0.31 × 103μl Lymphocytes. Post-operative Chest CT shows no relevant signs of COVID-19 associated abnormalities. Post-operative Head CT scan showed no residual lesion and re-expansion of the 4th ventricle returning to normal (Fig. 5).
Table 3.
Pre-operative and post-operative examinations.
| Patient Characteristics | Pre-operative a | Post-operative b |
|---|---|---|
| Symptoms | Vomiting, Dysphagia Headache and Ataxia Gait | Headache |
| Symptoms of Coronavirus Infection | Asymptomatic | Asymptomatic |
| AVPU score (Alert – Verbal – Pain – Unresponsive)c | Verbally Responsive | Verbally Responsive |
| The Highest Recorded Body Temperature | 36.6 C° (97.88 F) | 37.2 C° (98.96 F) |
| Average Respiratory Rate | 18 | 20 |
| Average Heart Rate | 65 bpm | 74 bpm |
| Average Blood Pression (Syst/Diast) | 135/75 mmHg | 130/80 mmHg |
| Average SpO2 (FiO2) | 95% (28%) | 95% (32%) |
| Haemoglobin | 14.2 g/L | 13.3 g/L |
| WBCd | 6.48 109/L | 15.22 109/L |
| CRPe | 4.00 mg/L | 17.81 mg/L |
| Creatinin | 0.71 mg/dL | 0.71 mg /dL |
12 h before surgery.
12 h after surgery.
Glasgow Coma Scale (GCS) 12–13 ∼ Verbally Responsive.
White blood cell (WBC) count.
C-reactive protein (CRP).
Fig. 5.
Post-operative Head CT scan showing the outcomes of a suboccipital craniotomy with minimal hyperdense residual blood tissue located in the area of the surgical cavity at the left paramedian level where the lesion was removed. Air spaces along the surgical access indicating the re-expansion process of the 4th ventricle returning to normal.
3. Discussion
We report the case of a 77 years old woman with oesophagus carcinoma diagnosed in September 2019 and treated at our centre with chemotherapy and radiotherapy. In January 2020, she underwent a Total Body CT scan to assess the staging, grading and spread of the tumour resulting in the absence of metastatic disease. Later she underwent KPS evaluation resulting in 80 and Recursive Partitioning Analysis (RPA) Class II. In April, she presented symptoms associated with hypertension in the posterior fossa (dysphagia, headache, ataxia, and progressive sensorium deterioration). An urgent enhanced head-CT scan was performed which showed a solitary cerebellar metastasis in the paramedian aspect of the right cerebellum hemisphere causing compression of the 4th ventricle. The patient was found positive for COVID-19 infection at molecular screening without respiratory symptoms. Therefore she has not been treated for any specific and non-specific symptoms of COVID-19. We hypothesise that the metastatic lesion’s mass effect would have resulted in acute obstructive hydrocephalus with rapid coma and death if we did not promptly proceed with emergency surgery [10].
Patients with esophageal carcinoma and brain metastasis have an overall survival (OS) of 2 weeks after metastasis diagnosis to 25 months after treatment [11]. On the other hand, patients with oesophageal cancer and solitary solid and stable organ metastases have an OS of 54 months after surgery, which was superior compared to chemotherapy only [12]. A case series of surgeries for posterior fossa metastases demonstrates a median OS of 6 months for all posterior fossa brain metastasis [11]. According to the priority criteria defined for neurological surgeries during the COVID-29 pandemic, the case under discussion was evaluated as a Class A ++ grade, indicating cases requiring immediate treatment. This class of priority comprises patients with intracranial or spinal tumours requiring urgent treatment such as rapidly evolving intracranial hypertension with deteriorating state of consciousness, spinal cord compression, hydrocephalus. [13].
Our hospital is one of the largest designated COVID-19 centres with theatres dedicated to COVID-19 positive patients, with appropriately trained staff on COVID-19 emergency and specific protocols. Our team joined an international research to study the disruption of elective cancer surgeries and the outcomes of COVID-19 patients undergoing surgery (COVIDSurg of the NIHR Global Surgery Group) which suggested that, for patients undergoing surgery with perioperative SARS-CoV-2 infection, postponing non-urgent procedures and promoting non-operative treatment (to delay or avoid the need for surgery) should be taken in consideration to avoid mortality and pulmonary complications [14]. For major elective cancer procedures, recent evidence indicates that delaying surgery following a positive SARS-CoV-2 swab test by at least four weeks will minimise post-operative complications in infected asymptomatic patients [15]. Regarding the importance of COVID-19 pre-operative testing, in a recent international cohort study of patients undergoing elective cancer surgery for ten different types of cancer. There were 87,484 patients included in the analysis, run in 432 hospitals over 53 countries worldwide; the overall pulmonary complication rate was 3.9%. This was higher in patients with no test (4.2%) or CT only (4.8%, Adjusted OR 1.27) compared to those who underwent a swab test (2.8%, AOR 0.68, 95 percent c.i. 0.47 to 0.98, P = 0.040) or swab test and CT (2.5%, AOR 0.57). Overall it has been found that pre-operative nasopharyngeal swab testing in asymptomatic patients was associated with a reduced rate of post-operative pulmonary complication and the main benefit was seen in patients undergoing major surgeries in high incidence areas [16].
Other Italian centres have reported a total of 15 cases of COVID-19 positive patients who have undergone neurosurgery treatments; 9 of these had a regular course and did not present any COVID-19 associated complications during their hospitalisation [17]. This shows that symptomatic COVID-19 patients can undergo major surgery. Interventions must be carried out with dedicated routes and appropriate individual protection equipment for healthcare workers [18].
In the pre- and post-operative management, specific planning and control measures were adopted for healthcare personnel involved in managing the patient undergoing surgery (Table 4). In the post-operative phase, the patient was not admitted into the intensive care unit (ICU) because, according to COVID-19 local protocol the, ICU is currently reserved for critical patients with acute respiratory. Sixteen days after surgery, on clinical and laboratory examination, the patient recovered quickly and in good condition; the inflammatory markers were within the reference ranges and the post-operative head CT showed no abnormalities and the normalisation of the 4th ventricle spaces.
Table 4.
COVID-19 patient management.
| Team | Transporting the patient to the OR | 2 Nurse aids b |
| Procedure Room | 2 Surgeons | |
| 2 Anesthesiologists | ||
| 2 Nurses | ||
| Clean Room | 2 Nurses | |
| COVID-19 screening for the surgical team | COVID-19 Swab test | Performed twice; 3 days befor surgery 3 days after surgery |
| Measures adopteda | For all the staff having contact with patient | Medical mask FFP3 |
| Gown | ||
| Gloves | ||
| Eye protection | ||
| Apron | ||
| For the operating theatre | Near Entrance Block | |
| High OR air exchange cycles (> 25 exchanges/h). |
Staff involved in the intervention not to leave the OR during the procedure.
Staff nurses aids involved in transporting the patient to the Operating Room (same nurses for taking the patients to the theatre and returning).
4. Conclusions
We presented the first reported case of solitary cerebellar metastasis of keratinising squamous cell carcinoma operated in a COVID-19 patient. This case report shows that major neurological surgeries can be considered for asymptomatic COVID-19 patients with adequate resource planning and PPE in order to reduce the healthcare-associated infections (HCAIs) risk, and no treatment for any specific and non-specific symptoms of COVID-19 was necessary. It is interesting to notice that our patient remained asymptomatic, not developing an active phase after a significant stressor like a major procedure. Therefore, COVID-19 screening tests can help identify asymptomatic patients undergoing major emergency surgery to set up adequate standards of care and protection for these patients and reduce the risk of transmission in surgical units during the current crisis. Hospitals, governments and policymakers need to introduce routine pre-operative SARS-CoV-2 swab testing for patients undergoing major surgery, especially given future waves of COVID-19 outbreaks.
Declaration of Competing Interest
None.
Funding
None.
Ethical approval
This study is exempt from ethical approval in my institution.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
PL: Study Design, Data Collection, Statistical Analysis, Data Interpretation, Manuscript Preparation, Literature Search
PF: Data Collection, Funds Collection
PB: Study Design, Data Collection, Statistical Analysis, Data Interpretation, Literature Search
RA: Data Collection
RM: Data Interpretation
AF: Funds Collection
GD: Data Interpretation, Funds Collection
AS: Funds Collection
Registration of research studies
-
1.
Name of the registry: Research Registry
-
2.
Unique identifying number or registration ID: researchregistry6241
-
3.
Hyperlink to your specific registration (must be publicly accessible and will be checked): https://www.researchregistry.com/browse-the-registry#home/registrationdetails/5fa9e5e0c5ea22001526ac18/
Guarantor
Pietro Familiari.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Acknowledgements
This study was supported by Sapienza University of Rome; Department of Anatomical, Histological, Medical Legal Sciences and Locomotor Apparatus.
References
- 1.DVV T., Hellman S., Rosenberg S.A. vol. 2. Lippincott-Raven; Philadelphia: 1997. (Cancer: Principles and Practice of Oncology). [Google Scholar]
- 2.Ogawa K., Toita T., Sueyama H. Brain metastases from esophageal carcinoma. Cancer. 2002;94(3):759–764. doi: 10.1002/cncr.10271. [DOI] [PubMed] [Google Scholar]
- 3.Kanemoto A., Hashimoto T., Harada H. Occurrence and clinical features of brain metastasis after chemoradiotherapy for esophageal carcinoma. J. Radiat. Res. 2011;52(4):509–515. doi: 10.1269/jrr.10184. [DOI] [PubMed] [Google Scholar]
- 4.Song Z., Lin B., Shao L., Zhang Y. Brain metastases from esophageal cancer: clinical review of 26 cases. World Neurosurg. 2014;81(1):131–135. doi: 10.1016/j.wneu.2013.02.058. [DOI] [PubMed] [Google Scholar]
- 5.Hagen P.V., Hulshof M., Lanschot J.V. Pre-operative chemoradiotherapy for esophageal or junctional cancer. N. Engl. J. Med. 2012;366(22):2074–2084. doi: 10.1056/nejmoa1112088. [DOI] [PubMed] [Google Scholar]
- 6.Ramakrishna R., Zadeh G., Sheehan J.P., Aghi M.K. Inpatient and outpatient case prioritisation for patients with neuro-oncologic disease amid the COVID-19 pandemic: general guidance for neuro-oncology practitioners from the AANS/CNS tumor section and society for neuro-oncology. J. Neurooncol. 2020;(September) doi: 10.1007/s11060-020-03488-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bernucci C., Brembilla C., Veiceschi P. Effects of the COVID-19 outbreak in Northern Italy: perspectives from the bergamo neurosurgery department. World Neurosurg. 2020;137 doi: 10.1016/j.wneu.2020.03.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Agha R.A., Borrelli M.R., Farwana R., Koshy K., Fowler A., Orgill D.P., For the SCARE Group The SCARE 2018 statement: updating consensus Surgical CAse REport (SCARE) Guidelines. Int. J. Surg. 2018;60:132–136. doi: 10.1016/j.ijsu.2018.10.028. [DOI] [PubMed] [Google Scholar]
- 9.Salcman M., Heros R.C., Laws E.R., Sonntag V.K.H. Kempe’s Operative Neurosurgery. Springer; New York, NY: 2004. Suboccipital craniectomy: midline and paramedian approach. [DOI] [Google Scholar]
- 10.Nanda A. Thieme; New York, NY: 2012. Principles of Posterior Fossa Surgery. [Google Scholar]
- 11.Gabrielsen T.O., Eldevik O.P., Orringer M.B., Marshall B.L. Esophageal carcinoma metastatic to the brain: clinical value and cost-effectiveness of routine enhanced head CT before esophagectomy. AJNR Am. J. Neuroradiol. 1995;16:1915–1921. [PMC free article] [PubMed] [Google Scholar]
- 12.Depypere L., Lerut T., Moons J. Isolated local recurrence or solitary solid organ metastasis after esophagectomy for cancer is not the end of the road. Dis. Esophagus. 2016 doi: 10.1111/dote.12508. [DOI] [PubMed] [Google Scholar]
- 13.Zoia C., Bongetta D., Veiceschi P. Neurosurgery during the COVID-19 pandemic: update from Lombardy, northern Italy. Acta Neurochir. 2020 doi: 10.1007/s00701-020-04305-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.CovidSurg Collaborative Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. Lancet. 2020;396(10243):27–38. doi: 10.1016/s0140-6736(20)31182-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.COVIDSurg Collaborative Elective cancer surgery in COVID-19-free surgical pathways during the SARS-CoV-2 pandemic: an international, multicenter, comparative cohort study. J. Clin. Oncol. 2020;(October) doi: 10.1200/JCO.20.01933. Epub ahead of print. PMID: 33021869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.COVIDSurg Collaborative Pre-operative nasopharyngeal swab testing and post-operative pulmonary complications in patients undergoing elective surgery during the SARS-CoV-2 pandemic. Br. J. Surg. 2020:znaa051. doi: 10.1093/bjs/znaa051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cenzato M., DiMeco F., Fontanella M., Locatelli D., Servadei F. Editorial. Neurosurgery in the storm of COVID-19: suggestions from the Lombardy region, Italy (ex malo bonum) J. Neurosurg. JNS. 2020;133(1):33–34. doi: 10.3171/2020.3.JNS20960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lapolla P., Mingoli A., Lee R. Deaths from COVID-19 in healthcare workers in Italy—what can we learn? Infect. Control Hosp. Epidemiol. 2020:1–2. doi: 10.1017/ice.2020.241. [DOI] [PMC free article] [PubMed] [Google Scholar]