Abstract
This case series study evaluates head and neck injuries caused by electric scooters in Paris, 2017-2019, focusing on user behavior and injury types.
Introduction
Recent studies have highlighted the dramatic increase in injuries and admissions associated with electric scooter (e-scooter) use in several countries.1,2,3,4,5,6 Although self-service e-scooters have been available in Paris since June 22, 2018, in our department we have recently observed a trend toward an increase in severe head and neck injuries caused by the use of e-scooters.
The aim of this case series study was to assess the epidemiology of head and neck and dental trauma related to e-scooter use in Paris, focusing on user behavior and injury type.
Methods
We performed an observational retrospective and prospective case series study between January 1, 2017, and October 31, 2019. The local ethics committee, Comité Scientifique et Ethique de l’Entrepôt de Données de Santé, approved the study, and all patients gave verbal informed consent. After study approval, we retrospectively requested 2 facial trauma centers to search their databases to retrieve all electronic medical records including the keyword e-scooter for the period between January 1, 2017, and June 30, 2019. Then one of us (Q.H.) manually screened medical records to identify patients treated for e-scooter–related head and neck trauma.
Data on age, sex, site, type (fractures, soft-tissue wounds, and dental lesions) of injured patients were collected from medical records by one of us (Q.H.). Mandibular fractures were described as unifocal (1 mandibular site) or plurifocal (>1 mandibular site).
We constructed a questionnaire including 9 items related to the circumstances of the accidents: alcohol or drug consumption (items 1 and 2), high-speed driving (3), driving on sidewalks (4), tandem riding (5), riding without a helmet (6), level of experience (>10 uses) with riding an e-scooter (7), experience with motorcycle driving (8), and possession of a driver’s license (9). A rider’s behavior was defined as risky if 1 of the 6 first items was answered as positive. From July 1 to October 31, 2019, items were prospectively collected by the surgeon who initially managed the patient’s care. Before July 1, 2019, items were retrospectively collected during a telephone call from one of us (Q. H.). This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline for observational studies.
Results
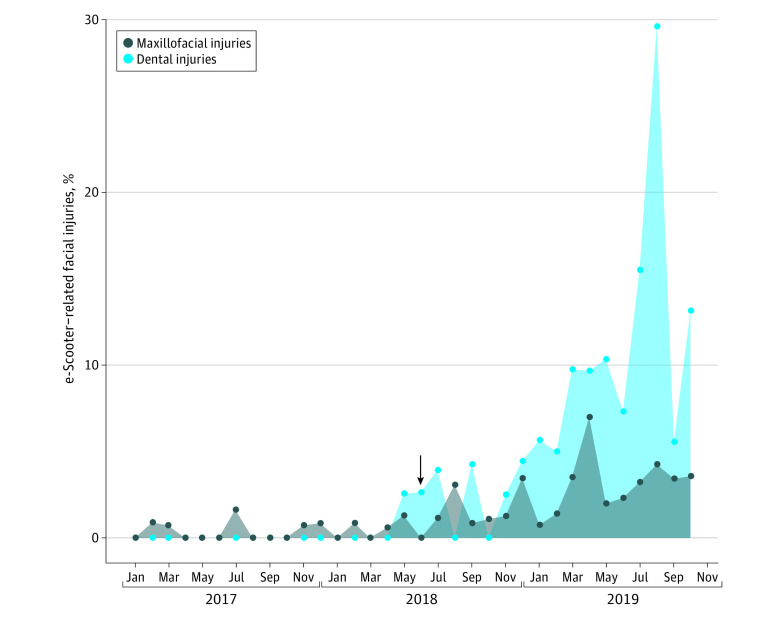
Of the total of 125 patients, 49 (39%) were included prospectively and 76 (61%) were included retrospectively for facial (n = 92) or dental (n = 33) trauma associated with use of an e-scooter. An increase in such injuries was observed over the study period (Figure). The questionnaire was completed by 43 of 49 patients (88%) and 42 of 76 patients (55%) during the prospective and retrospective parts of the study, respectively. Only 11 injuries (9%) occurred over the time span of the study before the introduction of e-scooter self-service providers. The mean (SD) patient age was 32.5 (12.7) years, and 46 patients (37%) were women (Table). Two patients (2%) were pedestrians struck by e-scooters, including the oldest member of the study cohort (95 years). Only 10 patients (12%) used a helmet while riding. High-speed and sidewalk riding were noted in 44 of 87 patients (51%) and 26 of 84 patients (31%), respectively, during the 2 parts of the study. Alcohol consumption was reported in 45 of 92 cases (49%). Overall, a risky behavior was observed in 80 of 92 cases (87%).
Figure. Time Trends of Electric Scooter (e-Scooter)–Related Head and Neck Injuries.
The arrow indicates the introduction of self-service e-scooters in Paris, France, on June 22, 2018.
Table. Patient Characteristics and Description of Facial Injuries Associated With Electric Scooters (e-Scooters).
| Characteristic | No. (%)a |
|---|---|
| Patients | |
| Female | 46 (37) |
| Age, y | |
| Mean (SD) | 32.5 (12.7) |
| Median (range) | 30 (10-95) |
| <18 | 3 (2.4) |
| Pedestrian hit by an e-scooter | 2 (1.6) |
| Alcohol consumption | 45 (49) |
| Drug consumption | 5 (6) |
| Speed at the time of the accidentb | |
| Low or medium | 43 (49) |
| High | 44 (51) |
| Driving on the sidewalk at the time of the accident | 26 (31) |
| Tandem riding | 12 (14) |
| User level (>10 e-scooter uses before the accident) | 51 (60) |
| Previous experience with motorcycle driving | 23 (27) |
| Driver’s license | 51 (60) |
| Helmet use | 10 (12) |
| Facial injuries | |
| Mandibular fracturesc | 66 (55) |
| No. of injured patients | 36 (47) |
| Type | |
| Unifocal | 4 (72) |
| Plurifocal | 22 (28) |
| Site | |
| Dentulous portion | 21 (32) |
| Condylar process | 45 (68) |
| Midface fractures | 53 (45) |
| No. of injured patients | 43 (56) |
| Site | |
| Nasal bones | 20 (26) |
| Zygoma | 13 (17) |
| Occlusofacial fracture (Le Fort) | 4 (5) |
| Orbital fracture | 7 (9) |
| Craniofacial fractures | |
| No. of injured patients | 7 (9) |
| Site | |
| Fronto-orbito-ethmoidal fracture | 1 (1) |
| Frontal sinus | 7 (9) |
| Facial wounds | 90 |
| No. of injured patients | 78 (62) |
| Site | |
| Supraorbital rim/forehead | 16 (18) |
| Nose | 10 (11) |
| Cheek | 3 (3) |
| Lips | 25 (28) |
| Tongue | 1 (1) |
| Chin | 36 (40) |
| Dental trauma | 115 |
| No. of injured patients | 55 (44) |
| Type | |
| Crown fractures | 69 (60) |
| Dental dislocation | 40 (35) |
| Alveolodental fractures | 6 (5) |
| Site | |
| Incisors | 92 (80) |
| Other teeth | 23 20) |
Denominators to calculate percentages may vary according to available data retrieved from the questionnaire as well as the medical records.
Patients were divided into 3 groups according to the speed at time of the accident: low (<10 kph), medium (10-20 kph), and high (>20 kph).
Each mandibular site of fracture in a patient was recorded as 1 fracture.
Two intracranial lesions, including a subdural hematoma and a subarachnoid hemorrhage, were reported. A surgical procedure with the patient under general anesthesia was performed in 36 of 77 patients (47%) with facial fractures.
Discussion
Although trauma caused by e-scooters is poorly described in the literature, recently there has been an increased number of scientific publications on e-scooter–related injuries.1,2,3,4,5,6 Most published articles were retrospective observational studies from the United States.
Although the retrospective part of our study could bias the interpretation of our results, we noted that 87% of traumatic injuries were associated with risky behavior. e-Scooter companies explicitly do not recommend consumption of drugs or alcohol while riding. We believe that further information campaigns could help raise awareness of risky behavior during e-scooter riding to prevent e-scooter accidents and decrease related hospital admissions in emergency departments.
In summary, e-scooter accidents are increasing in the streets of Paris. Engaging all public authorities in the prevention of e-scooter–related accidents is urgently needed.
References
- 1.Faraji F, Lee JH, Faraji F, et al. Electric scooter craniofacial trauma. Laryngoscope Investig Otolaryngol. 2020;5(3):390-395. doi: 10.1002/lio2.380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Störmann P, Klug A, Nau C, et al. Characteristics and injury patterns in electric-scooter related accidents—a prospective two-center report from Germany. J Clin Med. 2020;9(5):1569. doi: 10.3390/jcm9051569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vernon N, Maddu K, Hanna TN, Chahine A, Leonard CE, Johnson J-O. Emergency department visits resulting from electric scooter use in a major southeast metropolitan area. Emerg Radiol. 2020;27(5):469-475. doi: 10.1007/s10140-020-01783-4 [DOI] [PubMed] [Google Scholar]
- 4.Blomberg SNF, Rosenkrantz OCM, Lippert F, Collatz Christensen H. Injury from electric scooters in Copenhagen: a retrospective cohort study. BMJ Open. 2019;9(12):e033988. doi: 10.1136/bmjopen-2019-033988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Trivedi TK, Liu C, Antonio ALM, et al. Injuries associated with standing electric scooter use. JAMA Netw Open. 2019;2(1):e187381-e187381. doi: 10.1001/jamanetworkopen.2018.7381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Namiri NK, Lui H, Tangney T, Allen IE, Cohen AJ, Breyer BN. Electric scooter injuries and hospital admissions in the United States, 2014-2018. JAMA Surg. 2020;155(4):357-359. doi: 10.1001/jamasurg.2019.5423 [DOI] [PMC free article] [PubMed] [Google Scholar]