Abstract
A territory-wide retrospective observational study was conducted in Hong Kong between January 23 to April 22, 2020 to demonstrate changes in pediatric seizure-related accident and emergency department (A&E) visits during the COVID-19 pandemic. Parallel periods from 2015 to 2019 were used as control.
All-cause A&E attendances in all paediatric age groups decreased significantly during the study period. Seizure-related attendances decreased across all pediatric age-groups in 2020 (RR 0.379, 95% CI 0.245–0.588), with a disproportionately large decrease in the 0–6 years age group (RR 0.303, 95% CI 0.174–0.526) compared with the 7–18 years age group (RR 0.534, 95% CI 0.393–0.719). Decrease in RTI-related A&E attendances was also more drastic in the 0–6 age group. The two time trends are congruent in the 0–6 years but not the 7–18 years age group. Such a trend is suggestive of the usefulness of infection control measures in seizure prevention, especially amongst young children.
Keywords: COVID19, Epilepsy, Respiratory tract infections, Medical help seek-behaviour, Febrile seizures
Introduction
The worldwide pandemic of Coronavirus Disease 2019 (COVID-19) has brought about an unprecedented public health challenge on a global basis,1 and impacted heavily on the workload of the Accident & Emergency Department around the world.2 , 3 Drops in A&E visits has been observed amongst patients seeking medical care for reasons other than suspected COVID-19,3 , 4 including that amongst children5 and patients with epilepsy.6
Seizure is one of the commonest cause for Accident & Emergency Department (A&E) visits in children.7 , 8 The pandemic offers a unique timeframe to better understand the dynamics of health seeking behaviour amongst children with seizure. We thus examined pediatric seizure-related A&E visits through conducting a territory-wide observational study during the first wave of COVID-19 pandemic in Hong Kong, during which there was relatively low burden of COVID-19 cases but a series of strict infection control measures were implemented by the health authorities.9 , 10
Methods
The Hospital Authority (HA) provides over 80% of hospital services in Hong Kong; relevant clinical data from the HA was retrieved via the Clinical Data Analysis and Reporting System (CDARS). Fourteen out of the eighteen A&Es and all inpatient services operated by HA register diagnostic codes in CDARS according with International Classification of Diseases, 9th revision (ICD-9).
The study period was defined as January 23 – April 22, 2020, i.e. the first three months after the first COVID-19 case was confirmed in Hong Kong, during which there was relatively low burden of COVID-19 cases but vigilant infection control measures were enforced within the community. Parallel intervals from 2015 to 2019 were selected as control periods. Statistics for all-cause A&E attendance, respiratory tract infections (RTIs)-related A&E attendance, and seizure-related A&E attendance and ward admissions were retrieved from CDARS (see Supplementary Table 1 for detailed search criteria). This included age of admission, diagnoses, acute ward and ICU admissions, lengths of stay (LOS), mortality rate, and early A&E readmission (within 28 days) rate. The total number of seizure-related A&E visit was further compared with that of RTI-related and all-cause A&E visits.
Linear and negative binominal regression models were used to estimate the long-term time trend and potential changes during the first three month after the first imported COVID-19 case in Hong Kong, in A&E attendances and admission parameters during the period of interest. P-values for comparison of relative risks across groups were calculated by the Monte Carlo simulation using 10,000 samples. Statistical significance is considered p < 0.05. Statistical analysis was performed with IBM SPSS 22.0 for Windows and R version 4.0.2 (R Development Core Team, Vienna, Austria).
This study was approved by the Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster.
Results
Among the hospitals with computerized A&E attendance records, there was a total of 437,111 A&E visits between January 23 and April 22 in 2015–2020, of which 2530 were seizure-related and 70,282 were related to RTIs. The number of all-cause A&E attendances has been decreasing from 2015 to 2019 (RR 0.959, 95% CI 0.921–0.999, p = 0.043), with a significant decrease in 2020 in all age groups (RR 0.331, 95% CI 0.274–0.399, p < 0.001).
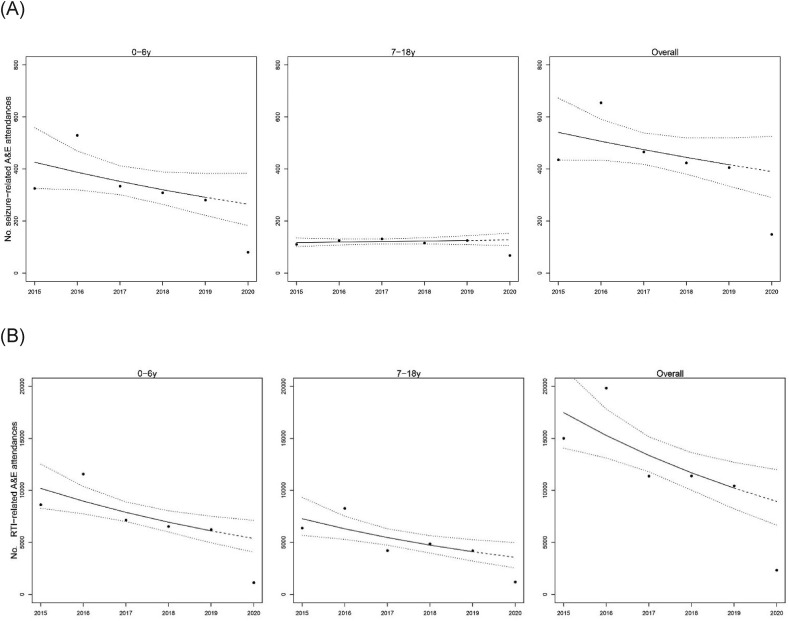
A significant drop in seizure-related A&E attendances was noted across all pediatric age groups in 2020 (RR 0.379, 95% CI 0.245–0.588, p < 0.001). Subgroup analysis showed a disproportionately larger decrease in seizure-related A&E attendances in the 0–6 years age group (RR 0.303, 95% CI 0.174–0.526, p < 0.001) than the 7–18 years age group (RR 0.534, 95% CI 0.393–0.719, p < 0.001), though the difference did not reach statistical significance (Fig. 1 A).
Figure 1.
Annual trend of seizure-related A&E attendances (A) and RTI-related A&E attendances (B) in the period from January 23 to April 22 (2015–2020). Solid lines are the fitted time trend, while dashed lines are the predicted number of attendances following the same time trend.
Similar age group discrepancies were noted in RTI-related A&E attendances. The number of RTI-related A&E attendances decreased in 2020 when compared to the overall trend from 2015 to 2019 (Fig. 1B), with a drastic decrease in the 0–6 years age group (RR 0.208, 95% CI 0.141–0.310, p < 0.001), and a smaller decrease in the 7–18 age group (RR 0.335, 95% CI 0.210–0.536, p < 0.001).
The time trends of seizure- and RTI-related A&E attendances were congruent in the 0–6 years age group (test for difference in time trends, p = 0.650) but not in the 7–18 age group (Fig. 1A and B).
In view of the above findings, seizure-related admissions from children aged 0–6 years old were further divided into febrile and afebrile subgroups for subgroup analysis. Whilst the afebrile seizure-related admissions were halved, the febrile seizure-related admission dropped to less than 20% of the previous year, and was disproportionately greater (Supplementary Fig. 1A and B).
Admission outcomes
A total of 2241 seizure-related admissions during the study period were included. The acute ward in-patient admission rate, mortality rate, and rate of early A&E re-admissions remained stable between 2015 and 2020 (Table 1 ), and the LOSs in acute ward and ICU did not change significantly during COVID-19.
Table 1.
Hospital inpatient parameters in seizure-related admissions from January 23 to April 22, 2015–2020, using linear regression.
| Coef | 95% CI | p-value | |
|---|---|---|---|
| Acute ward admission rate | |||
| Time trend (per year) | −0.010 | −0.028–0.008 | 0.182 |
| Year 2020 | −0.012 | −0.096–0.071 | 0.670 |
| Mortality rate | |||
| Time trend (per year) | 0.0003 | 0.000–0.001 | 0.182 |
| Year 2020 | −0.001 | −0.003–0.001 | 0.228 |
| Acute ward LOS | |||
| Time trend (per year) | −0.063 | −0.314–0.188 | 0.482 |
| Year 2020 | −0.210 | −1.361–0.941 | 0.603 |
| ICU LOS | |||
| Time trend (per year) | −0.027 | −0.073–0.018 | 0.152 |
| Year 2020 | 0.194 | −0.015–0.403 | 0.060 |
| Early A&E re-admission rate | |||
| Time trend (per year) | −0.003 | −0.014–0.008 | 0.437 |
| Year 2020 | −0.009 | −0.057–0.040 | 0.618 |
(Coef = coefficient; LOS = length of stay; ICU = intensive care unit).
Discussion
The COVID-19 pandemic has deeply affected many aspects of people's lives, including personal hygiene practices, suspension of schools and social activities, quarantine policies and travel restrictions. This study demonstrated change in seizure-related health seeking behavior, and the possible effect of social distancing on the incidence of seizure-related complaints in children during this global public health crisis.
We found that seizure-related A&E attendances decreased significantly during the periods of vigilant social distancing under COVID-19, with a disproportionately large effect on the 0–6 years age group compared to older pediatric age groups. A similar trend was found for A&E attendances for RTI during the same period.
The observed trend may be due to both an actual reduction in seizure occurrences and changes in health-seeking behavior. Social distancing and hygienic precautions reduced the risk of virus transmission, as evident by the significantly reduction in RTI occurrences. The disproportionate drop in seizure-related admissions in children 0–6 years, particularly febrile seizure-related admissions during this period of increased infection control suggests that intercurrent illnesses are a more significant risk factor of seizure occurrences in younger children, amongst whom the predominant cause of seizures is febrile seizure that are frequently associated with respiratory infections.11 , 12 It is therefore a reasonable postulation that strict infection control measures, including the use of facemasks, improved personal hygiene, social distancing, and homestay measures reduced RTI incidences and hence lowered incidences of febrile seizures.13 , 14 While it is beyond of scope of this observational study to demonstrate a causal relationship between the drop in RTI and febrile seizures during the COVID-19 pandemic, these findings may shed light on how febrile seizures and other related epileptic disorders can be prevented using approaches focusing on infection control measures and immunization programs.
Infection outbreaks, in particular pandemics, are a cause for altered medical help seeking behaviour,15, 16, 17 and large drops in A&E visits have also been observed in other pediatric populations around the world during the current pandemic.5 The possibility of nosocomial COVID-19 cross-infections, prohibition of family visits, and attempts to avoid overloading the healthcare system may have discouraged patients or parents from attending the A&E. While the spectrum of seizure severities did not show significant changes during the COVID-19 outbreak, it is not known whether these unmet medical needs may emerge later, causing a surge in service demand after the epidemic. Moreover, the COVID-19 pandemic is ongoing; our observations raise the need for further studies to better understand the trends observed and their causes in relation to the severity of the pandemic.
Conclusion
We demonstrated a significant reduction in emergency service utilization for seizures during the first wave of COVID-19 pandemic in Hong Kong, during which there was relatively low burden of COVID-19 cases but strict infection control measures were in place within the community. This reduction was more drastic in children aged 0–6 years old, who are prone to febrile seizures. This trend was congruent with that of RTI-related A&E attendances. Future studies are warranted to explore the approaches of infection control measures and immunization programs in preventing febrile seizures in younger children.
Sponsorship or funding
This study does not involve sponsorship or funding.
Declaration of competing interest
All authors have nothing to disclose.
Acknowledgement
The authors would like to acknowledge Mrs. R. Wong for her assistance with English editing.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jfma.2020.11.006.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Sohrabi C., Alsafi Z., O'Neill N., Khan M., Kerwan A., Al-Jabir A. World Health Organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19) Int J Surg. 2020;76:71–76. doi: 10.1016/j.ijsu.2020.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bjornsen L.P., Naess-Pleym L.E., Dale J., Laugsand L.E. Patient visits to an emergency department in anticipation of the COVID-19 pandemic. Tidsskr Nor Laegeforen. 2020;140(8) doi: 10.4045/tidsskr.20.0277. [DOI] [PubMed] [Google Scholar]
- 3.Hartnett K.P., Kite-Powell A., DeVies J., Coletta M.A., Boehmer T.K., Adjemian J. Impact of the COVID-19 pandemic on emergency department visits - United States. MMWR Morb Mortal Wkly Rep. 2020;69(23):699–704. doi: 10.15585/mmwr.mm6923e1. January 1, 2019-may 30, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Metzler B., Siostrzonek P., Binder R.K., Bauer A., Reinstadler S.J. Decline of acute coronary syndrome admissions in Austria since the outbreak of COVID-19: the pandemic response causes cardiac collateral damage. Eur Heart J. 2020;41(19):1852–1853. doi: 10.1093/eurheartj/ehaa314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li H., Yu G., Duan H., Fu J., Shu Q. Changes in children's healthcare visits during COVID-19 pandemic in Hangzhou, China. J Pediatr. 2020 doi: 10.1016/j.jpeds.2020.05.013. [published Online First: 2020/05/18] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Granata T., Bisulli F., Arzimanoglou A., Rocamora R. Did the COVID-19 pandemic silence the needs of people with epilepsy? Epileptic Disord. 2020 doi: 10.1684/epd.2020.1175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wong V. Study of seizure and epilepsy in Chinese children in Hong Kong: period prevalence and patterns. J Child Neurol. 2004;19(1):19–25. doi: 10.1177/088307380401900104011. [DOI] [PubMed] [Google Scholar]
- 8.Sogawa Y., Maytal J. Emergency department admission of children with unprovoked seizure: recurrence within 24 hours. Pediatr Neurol. 2006;35(2):98–101. doi: 10.1016/j.pediatrneurol.2006.01.007. [published Online First: 2006/08/01] [DOI] [PubMed] [Google Scholar]
- 9.Centre of Health Protection DoH The Government of the Hong Kong special administrative region. Latest situation of coronavirus Disease (COVID-19) in Hong Kong. https://chp-dashboard.geodata.gov.hk/covid-19/en.html Available from:
- 10.Authority HKH Press Releases. https://www.ha.org.hk/visitor/ha_visitor_text_index.asp?Content_ID=254422&Lang=ENG&Dimension=100&Parent_ID=10000&Ver=TEXT Available from:
- 11.Francis J.R., Richmond P., Robins C., Lindsay K., Levy A., Effler P.V. An observational study of febrile seizures: the importance of viral infection and immunization. BMC Pediatr. 2016;16(1):202. doi: 10.1186/s12887-016-0740-5. [published Online First: 2016/12/05] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Carman K.B., Calik M., Karal Y., Isikay S., Kocak O., Ozcelik A. Viral etiological causes of febrile seizures for respiratory pathogens (EFES Study) Hum Vaccines Immunother. 2019;15(2):496–502. doi: 10.1080/21645515.2018.1526588. [published Online First: 2018/09/21] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.MacIntyre C.R., Chughtai A.A. Facemasks for the prevention of infection in healthcare and community settings. BMJ. 2015;350:h694. doi: 10.1136/bmj.h694. [published Online First: 2015/04/11] [DOI] [PubMed] [Google Scholar]
- 14.Jefferson T., Del Mar C., Dooley L., Ferroni E., Al-Ansary L.A., Bawazeer G.A. Physical interventions to interrupt or reduce the spread of respiratory viruses: systematic review. BMJ. 2009;339:b3675. doi: 10.1136/bmj.b3675. [published Online First: 2009/09/24] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Feng S., Grepin K.A., Chunara R. Tracking health seeking behavior during an Ebola outbreak via mobile phones and SMS. NPJ Digit Med. 2018;1:51. doi: 10.1038/s41746-018-0055-z. [published Online First: 2019/07/16] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Person B., Sy F., Holton K., Govert B., Liang A., National Center for Infectious Diseases SCOT Fear and stigma: the epidemic within the SARS outbreak. Emerg Infect Dis. 2004;10(2):358–363. doi: 10.3201/eid1002.030750. [published Online First: 2004/03/20] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lau J.T., Yang X., Tsui H., Kim J.H. Monitoring community responses to the SARS epidemic in Hong Kong: from day 10 to day 62. J Epidemiol Community Health. 2003;57(11):864–870. doi: 10.1136/jech.57.11.864. [published Online First: 2003/11/06] [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.