Abstract
The purpose of this quality improvement initiative was to identify anxious/distressed lung cancer patients and address their mental health needs directly related to the COVID-19. A total of 441 patients were screened utilizing a national distress thermometer. 47% were counseled by the NP, 32% sent for referral to the social worker. Patients reported reasons for distress as fear of delaying testing, contracting the virus and changes in their lifestyle. We found that screening all patients during the pandemic, yielded a higher than normal percentage of patients who were in need of some level of mental health services.
Keywords: coronavirus, COVID-19, distress, lung cancer treatment, mental health screening
Introduction
The COVID-19 pandemic has had psychosocial impacts on our society in numerous ways, ranging from social isolation, financial loss, and seemingly negative economic impacts.1 According to the initial reports from the Centers for Disease Control and Prevention (CDC), the coronavirus has infected more than 12 million patients with close to 255,000 confirmed deaths. In August 2020, an addendum has revised noting that an excess of deaths have been reported as being COVID-19; in some cases, the patients had passed away from malignancies, trauma, chronic disease, or Alzheimer’s disease;2 although the death count may have been inflated, patients reacted to the conflicting coverage. Another major consequence of this widespread eruption of illness has been a significant increase in adverse mental health outcomes.3 Cancer patients represent an already compromised group known to have elevated levels of fear and anxiety, and introduction of the pandemic places this vulnerable population at an even higher risk for mental health consequences.
At the Stony Brook Lung Cancer Evaluation Center (LCEC), we recognized the potential for increased distress among our patients, and as such, we aimed to evaluate how the pandemic was affecting them in relation to their mental health. We wanted to ensure that all of our patients were properly screened and offered the appropriate referrals because we know that a cancer diagnosis and treatment in itself can increase anxiety and depression,4 even in the absence of a pandemic. It has been well documented that compared with healthy populations, cancer patients are at a higher risk of mental health problems.5
Over the past 6 months, the news and media have presented (sometimes conflicting) information daily on the infection, transmission, systemic and respiratory effects of the COVID-19 virus. The world shut down, and people were quarantined in their homes. Thus, for lung cancer patients or those suspected of having lung cancer, fears were likely to be heightened. Delay of diagnosis or inability to access treatment were at the forefront of concerns. Additionally, lung cancer patients have a greater predisposition to respiratory infections, immunosuppressed conditions, chronic obstructive pulmonary disease, metastatic disease, and a higher rate of mortality compared with the general population.6 These complications are thought to contribute to increased levels of fear and anxiety in our patient population. Delay of diagnosis or lack of access to treatment were at the forefront of concerns reported by patients.
The purpose of this quality improvement initiative was to identify patients for anxiety or depression that was directly related to the COVID-19 pandemic and to facilitate the acquisition of appropriate care to address their mental health needs. This initiative was originally designed to aid in the reduction of stress and anxiety in an already burdened lung cancer population during an acute health care outbreak; if successful, we aim to adapt the practice into our current multidisciplinary cancer care program.
Methods
The LCEC is housed in the Stony Brook Cancer Center and evaluates, diagnoses, and treats patients found to have concerning pulmonary nodules. The LCEC cares for a full spectrum of patients, including those with benign lesions, those under surveillance, and those with a new cancer diagnosis through treatments and survivorship.
To assess patient distress, a total of 441 patients undergoing treatment for or surveillance of lung cancer were screened between April 2020 and July 2020 utilizing the National Comprehensive Cancer Network (NCCN) Distress Thermometer.7 Patients were called individually and asked a series of questions regarding their distress levels in relation to the COVID-19 pandemic. The NCCN tool uses a numeric scale from 0 to 10 to quantify the level of distress, with 0 representing no distress and 10 indicating severe distress. A distress score of 3 alerts staff to conduct further evaluation.8 Any patient who reported a distress level between 3 and 5 was counseled by the LCEC nurse practitioner (NP) to evaluate additional needs. A score 6 or greater prompted a referral to the cancer center social worker.
Results
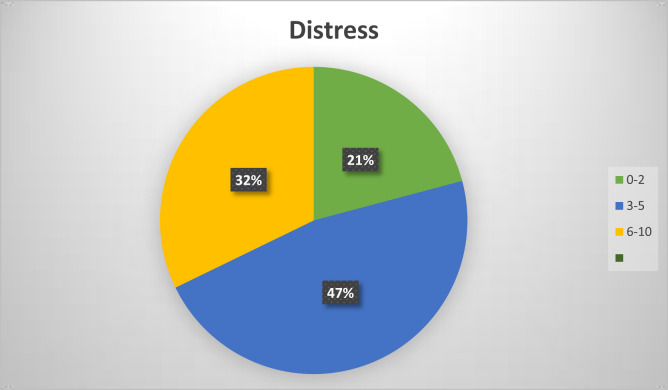
In this investigation, of the 451 patients contacted, 10 (2.2%) declined to participate. Of the 441 (see Figure) who were screened, 92 (21%) scored 2 or lower, requiring no additional action. A total of 207 (47%) scored 3–5 and were counseled by the NP, and 142 (32%) scored between 6 and 9, requiring referral to the social worker. The most common reasons reported for distress were fear of delayed testing, contracting the virus, and changes in their lifestyle (not seeing family, isolation, etc.).
Figure.
Reported distress scores among patients undergoing lung cancer treatment or surveillance between April and July 2020 (N = 441). Self-reported distress score on the National Comprehensive Cancer Network Distress Thermometer.7 NP intervention = blue; social worker intervention = yellow; no intervention = green.
Given the findings from the present investigation indicating that approximately one-third of patients were at actionable levels of distress management during the recent pandemic, it has become increasingly important to recognize and address these mental health concerns that are on the rise in this vulnerable patient population
Discussion
The Distress Management Panel of the NCCN recommends that all cancer patients be screened on a regular basis for psychological distress.8 The Distress Thermometer is a validated tool that was developed to help screen cancer patients for heightened distress quickly and efficiently.9 , 10 We know that early detection of distress can reduce the effects of suffering and the severity of symptoms.11 In a study carried out in China, the authors discuss lung cancer patients and their higher incidence and severity of COVID-19.12 Compared with the general population, lung cancer patient have a higher mortality.6 This information contributes to the increased fear and anxieties of our patient population.
It is widely known that NPs play a key role at the core of a multidisciplinary team.13, 14, 15 In fact, the NP is often the team member to triage the patient from the first contact with the organization and the consistent contact with patients throughout their cancer journey; utilizing the NP to evaluate and treat this patient population was ideal. Our team is aware of the specific cancer-related anxiety and coping techniques that are important when educating this patient population. The use of medication is sometimes necessary to assist with anxiety. Cognitive behavior therapy in conjunction with medications is considered the most effective.16 Support groups are discussed with our patients and offered on a monthly basis to provide a safe environment to share feelings with patients and families that are going through similar situations.16 In the time of COVID-19, support groups are offered online and on Zoom calls. Other tools include education on physical activity, diet, support systems, relaxation, and mindful mediations to practice that can assist with reducing stress.
Once patients who scored between 3 and 5 were identified through the screening process, the NP intervention was initiated. Studies have demonstrated that advanced practitioners improve quality and continuity of care,17 so having the NP that was already familiar with the patients make these calls and visits best suited our patients. Each patient call lasted between 15 and 45 minutes, which included evaluating the causes of the acute anxiety. The majority of the fears were related to contracting the virus, families contracting the virus, and delay of cancer treatment. During these sessions, the opportunity was taken to educate patients on precautions outlined by the CDC, and resource information including educational, community, and essential support services were offered. Patients were encouraged to participate in frequent remote contact with family, friends, and religious affiliations via telephone, email, or virtual contact. Additional time was allotted for support and to ease the fears of treatment delays. A follow-up call or a virtual or in-person visit was completed within 2–4 weeks.
Our office worked directly with the social worker to improve outcomes, decrease stress, and improve quality improvements. Patients who scored above a 6 on the Distress Thermometer were directed to the social worker intervention. This session included reaching out to patients by telephone, virtual means, or an in-person visit to explain the role of the social worker, provide emotional support, and describe the available resources. Patient history was obtained, including family support. Suicidal ideation was screened, and psychoeducation regarding common emotional reactions to COVID-19 and cancer was provided. The social worker remained available for continued support and planning.
Conclusion
We found that screening all patients (not solely those newly diagnosed with lung cancer) during the pandemic yielded a higher than normal percentage of patients who were in need of some level of mental health services. Cancer patients, particularly lung cancer patients, have increased fear due to the respiratory symptoms of COVID-19. After completion of this quality improvement initiative, we have incorporated distress assessment and triage protocols into our practice for all patients, which will continue after COVID-19.
Biographies
Denise Albano, DNP, is a nurse practitioner at Stony Brook University Medical Center, Stony Brook University Hospitals, Stony Brook, NY. She can be contacted at Denise.albano@stonybrookmedicine.edu.
Melissa Feraca, FNP, is a nurse practitioner at Stony Brook University Medical Center, Stony Brook University Hospitals, Stony Brook, NY.
Barbara Nemesure, PhD, is a researcher at Stony Brook University Medical Center, Stony Brook University Hospitals, Stony Brook, NY.
Footnotes
In compliance with national ethical guidelines, the authors report no relationships with business or industry that would pose a conflict of interest.
References
- 1.Dubey S., Biswas P., Ghosh R., et al. Psychosocial impact of COVID-19. Diabetes Metab Syndr. 2020;14(5):779–788. doi: 10.1016/j.dsx.2020.05.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Excess deaths associated with COVID-19. 2020. https://www.cdc.gov/nchs/nvss/vsrr/covid19/excess_deaths.htm
- 3.Rajkumar R.P. COVID-19 and mental health: a review of the existing literature. Asian J Psychiatry. 2020;52 doi: 10.1016/j.ajp.2020.102066. 102066-102066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.O’Hea E., Kroll-Desrosiers A., Cutillo A.S., et al. Impact of the mental health and dynamic referral for oncology (MHADRO) program on oncology patient outcomes, health care utilization, and health provider behaviors: A multi-site randomized control trial. Patient Educ Counsel. 2020;103:607–616. doi: 10.1016/j.pec.2019.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ng H.S., Roder D., Koczwara B., Vitry A., et al. Comorbidity, physical and mental health among cancer patients and survivors: An Australian population-based study. Asia-Pacific J Clin Oncol. 2018;14(2):e181–e192. doi: 10.1111/ajco.12677. [DOI] [PubMed] [Google Scholar]
- 6.Rogado J., Pangua C., Serrano-Montero G., et al. COVID-19 and lung cancer: a greater fatality rate? Lung Cancer. 2020;146:19–22. doi: 10.1016/j.lungcan.2020.05.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.National Comprehensive Cancer Network NCCN Distress Thermometer. 2020. https://www.nccn.org/patients/resources/life_with_cancer/pdf/nccn_distress_thermometer.pdf
- 8.Distress management. Clinical practice guidelines. J Natl Compr Canc Netw. 2003;1:344–374. doi: 10.6004/jnccn.2003.0031. [DOI] [PubMed] [Google Scholar]
- 9.Cutillo A., O’Hea E., Person S., Lessard D., Harralson T., Boudreaux E. The Distress Thermometer: cutoff points and clinical use. Oncol Nurs Forum. 2017;44(3):329–336. doi: 10.1188/17.ONF.329-336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Roth A.J., Kornblith A.B., Batel-Copel L., Peabody E., Scher H.I., Holland J.C. Rapid screening for psychologic distress in men with prostate carcinoma: a pilot study. Cancer. 1998;82(10):1904–1908. doi: 10.1002/(sici)1097-0142(19980515)82:10<1904::aid-cncr13>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- 11.Faller H., Schuler M., Richard M., Heckl U., Weis J., Küffner R. Effects of psycho-oncologic interventions on emotional distress and quality of life in adult patients with cancer: systematic review and meta-analysis. J Clin Oncol. 2013;31(6):782–793. doi: 10.1200/JCO.2011.40.8922. [DOI] [PubMed] [Google Scholar]
- 12.Yu J., Ouyang W., Chua M.L.K., Xie C. SARS-CoV-2 transmission in patients with cancer at a tertiary care hospital in Wuhan, China. JAMA Oncol. 2020;6:1108–1110. doi: 10.1001/jamaoncol.2020.0980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Abdulrahman G.O. The effect of multidisciplinary team care on cancer management. Pan African Med J. 2011;9:20. doi: 10.4314/pamj.v9i1.71195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ko C., Chaudhry S. The need for a multidisciplinary approach to cancer care. J Surg Res. 2002;105(1):53–57. doi: 10.1006/jsre.2002.6449. [DOI] [PubMed] [Google Scholar]
- 15.Reid A.E., Tanoue L., Detterbeck F., Michaud G.C., McCorkle R. The role of the advanced practitioner in a comprehensive lung cancer screening and pulmonary nodule program. J Adv Pract Oncol. 2014;5:440–446. doi: 10.6004/jadpro.2014.5.6.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bates G.E., Mostel J.L., Hesdorffer M. Cancer-related anxiety. JAMA Oncol. 2017;3:1007. doi: 10.1001/jamaoncol.2017.0254. [DOI] [PubMed] [Google Scholar]
- 17.Oliveria S.A., Altman J.F., Christos P.J., Halpern A.C. Use of nonphysician health care providers for skin cancer screening in the primary care setting. Prev Med. 2002;34:374–379. doi: 10.1006/pmed.2001.0995. [DOI] [PubMed] [Google Scholar]