Abstract
The burden of the COVID-19 pandemic upon healthcare workers necessitates a systematic effort to support their resilience. This article describes the Yale University and Yale New Haven Health System effort to unite several independent initiatives into a coherent integrated model for institutional support for healthcare workers. Here, we highlight both opportunities and challenges faced in attempting to support healthcare workers during this pandemic.
The COVID-19 pandemic is an epic public health threat and the most stressful medical crisis for healthcare workers in this era. Within months, it dramatically changed healthcare and pushed healthcare workers to the limits of their resilience. Frontline workers put themselves and their cohabitating family members at risk for infection in the service of caring for the desperately ill. They worked long, exhausting hours in rapidly changing healthcare settings; filling unfamiliar roles; making demoralizing life-and-death decisions; and battling a poorly understood new virus. Workers had limited treatment options for patients and available options had limited validation. During this pandemic, some likened healthcare delivery to war. A battle was fought at the front lines to save lives, but healthcare worker casualties were not always easy to identify.
The COVID-19 pandemic put healthcare workers at risk for stress-related symptoms [1], consistent with reports of increased levels of anxiety, depression, and posttraumatic stress disorder symptoms [[2], [3], [4], [5]]. In one sample of 657 healthcare workers, acute stress symptoms were present in 57%, depression symptoms were present in 48%, and anxiety symptoms were present in 33% [6].
Here, we describe the rapid mobilization of the Yale community to support our healthcare workers in the hope that it may be useful to other healthcare systems. Our presentation is organized into three sections: 1) a description of the team that developed our institutional support system, 2) a characterization of the three tiers of services that we developed or organized (individual-level, team-level, community-level), and 3) a report of what we learned and how it influences our plan for the future. This was a high priority mission intended to promote the overall effort to deliver optimal care to patients infected by COVID-19. It proved difficult to reach the people who were struggling the most, i.e., people whose stoicism, exhaustion, isolation, concerns about privacy, or commitment to work overshadowed their attention to self-care. To create a system that addressed these challenges, we: 1) united independent efforts across our campus into an integrated support system; 2) created an array of services to build a safety net to support struggling individuals; 3) initiated a proactive outreach program; 4) redeployed trainees and faculty; and 5) identified volunteers to provide needed services. Further, we accomplished this task quickly and without hiring new staff.
1. Creating a united campus-wide support system
When the pandemic emerged, healthcare workers reported extremely stressful conditions in many hospital areas, including the Intensive Care Units, inpatient units caring for COVID-19-infected patients, and the Emergency Department. In response, multiple programs emerged within the Yale School of Medicine (YSM) and Yale Medicine (YM), its faculty practice, as well as its affiliated hospital, Yale-New Haven Health (YNHH), which is embedded within the Yale New Haven Health System (YNHHS). These initiatives built on multiple pre-COVID initiatives within several YSM and YNHHS departments and programs. We recognized that these entities needed to collaborate in order to integrate the initiatives into a well-coordinated system. This led to thrice weekly meetings with the heads of these groups under the leadership of the chair of the Department of Psychiatry (JHK) and the emergence of a wonderfully collaborative effort that worked through a consensus process to provide supports to healthcare workers in our community.
2. Creating a tiered support system
Our greatest concern was reaching the people in the most need of support, providing them with engaging services, and supporting them in their work and home lives. The services described below emerged independently, but became linked. Here we present the system that was rapidly deployed through the collaboration among the component program leaders.
Our group developed a shared vision through collaboration. It drew on a mindfulness-informed approach to stress management [7], a resilience-promoting wellness-oriented perspective [8], a scientifically-based model for human resilience [9], a disaster-oriented brief intervention [10], a peer support model developed to support military personnel in combat [11,12], an expert approach to parenting [13,14], and other psychotherapeutic and educational perspectives. We viewed reported stress symptoms as part of a normal reaction to an extreme situation and we strove to avoid pathologizing these normal responses. We also avoided debriefing strategies that might consolidate maladaptive stress appraisals and worsen long-term outcomes [15].
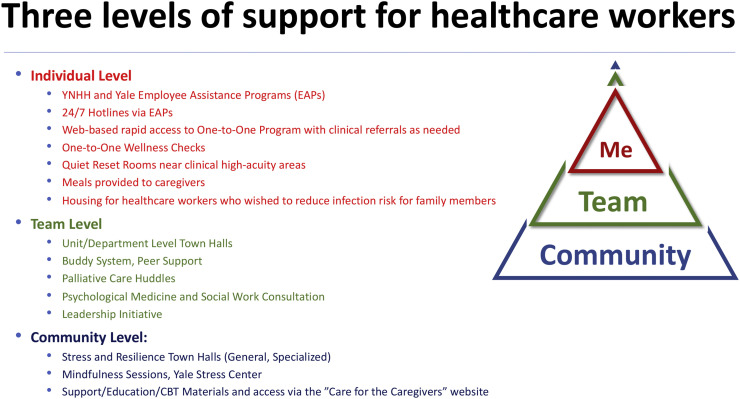
Our interventions targeted three levels: self, team, and community (see Fig. 1 ). This hierarchical model was intended to reinforce self-care and to increase engagement in psychological treatment; to bolster peer relationships and strengthen clinical teams; and to draw on the common themes of stress across our community while providing interventions that promoted resilience (see Table 1 ).
Fig. 1.
This figure illustrates the three-tiered program developed at Yale to support healthcare workers and associated staff.
Table 1.
This table summarizes our interventions intended to support healthcare workers. Town Halls – General: Stress and Resilience Town Halls open to the entire community and covering themes of broad interest. Town Halls – Specific: Stress and Resilience Town Halls targeting particular groups (medical students, hospitalists, particular medical school departments, etc.). Mindfulness Courses: Weekly mindfulness courses provided by the Yale Stress Center that were open to the healthcare community. Individual Evaluations: Individuals signed up on the web, were contacted within 24 h, and received an evaluation and, if needed, referral. In-Hospital Visits were provided by the Psychological Medicine Service and YNHH Social Work Service to nearly every inpatient unit, nearly every day.
| Activity | FTE | Total number of sessions | Total number of attendees |
|---|---|---|---|
| Town Halls | Paid: 0.75 FTE Psychologist | General: 69 | General: 739 |
| Dedicated: 41 | Dedicated: 2034 | ||
| 0.25 FTE Administrative Assistant | |||
| 0.1 FTE Techical support | |||
| 0.5 FTE PhD Fellows | |||
| Volunteer: 0.3 FTE Psychologist or Psychiatrist | |||
| Mindfulness Courses | Paid: 0.5 FTE Social Worker | Free Weekly Sessions: 16 | General: 640 |
| Volunteer: 0.1 FTE Psychologist | Structured 8-week course: 3 cycles (27 sessions) | All classes: 671 | |
| Individual Brief Interventions | Paid: 0.3 FTE Psychologist (administration, website revision) | 1–4 Sessions per person | 70 Web Contact Requests |
| 51 Contacts | |||
| 0.1 FTE Psychiatrist | 19 Did not respond to outreach | ||
| 0.1 FTE Psychologist (training) | |||
| 0.2 FTE (clinical supervision, treatment for 96 sessions) | |||
| Volunteer: 34 sessions | |||
| In-Hospital Unit-based Visits⁎ | Paid: M.D. 0.8 FTE | – | – |
| M.S.W.: 11.25 FTE | |||
| Leadership Support | Paid: .4FTE Deputy Dean for Professionaism & Leadership (devoted 0.2 FTE to this effort) | Weekly Planning Meetings with Team | Between 15 and 30 in townhalls week to week |
| Weekly Town Halls (cince Apeil) | |||
| Individual coaching offered to 70 unit leaders; uptake varied from weekly to as needed | |||
| Volunteer: 0.2 FTE X2 consultants from Yale School of Management | |||
| Regular coaching sessions with individual unit leaders (nurses and MD's—usually weekly) | |||
| .2FTE X2 Yale School of Medicine faculty (MD's) | |||
| .2FTE Psychologists | |||
| Webpage Management | 0.2 FTE Administrator | 2534 webpage users | – |
| Website building/management: 80 h | |||
| Survey development/design 40 h |
FTE estimates refer to the initial 4 months following the appearance of COVID-19. FTE estimates for the Town Halls include allocations for preparation/organization and the conduct of the sessions.
The in-hospital rounding began in mid-March and ended in mid-June.
2.1. Community level interventions
Two community level interventions were initiated within two weeks of the emergence of COVID-19 infections in our community, virtual town hall meetings and virtual mindfulness courses. Both of these programs were open to the entire healthcare community (faculty, staff, trainees). Town Halls lasted one hour and were co-led by professional volunteers. Initially, group leaders were invited to volunteer for these roles on the basis of their expertise in leading therapeutic groups. Over time, a broader group of approximately 30 volunteers from the Department of Psychiatry, including psychiatry residents and psychology fellows, served as co‑leaders.
“Stress and Resilience Town Halls” blended two evidence-based approaches to help individuals cope with adversity, mutual support and psychoeducation [16,17]. They provided healthcare workers with daily opportunities to connect with others experiencing similar stresses, share their experiences, and learn resilience-building strategies. The Town Halls were interactive and co-facilitated by experienced psychiatrists and psychologists who volunteered their time. Each Town Hall began with a brief presentation relevant to stress or resilience by one of the facilitators, which was then followed by asking participants to share some of their related stresses and resilience strategies. Town Halls covered a variety of themes, such as stress management, parenting stress, isolation, guilt, relaxation techniques, and sleep hygiene.
We also provided “dedicated” Town Halls to support specific communities including departments, department sections, and other subgroups (i.e., medical students, residents, nurses, administrative staff, and clinical staff at affiliated institutions). We also conducted Town Halls tailored to support various groups including Chinese-speaking members of our community (in Mandarin); Spanish-speaking community (in Spanish); local Black and LatinX Communities (via our CTSA-supported Cultural Ambassadors Program); and elderly communities isolated in Independent Living and Nursing Home settings. To date, 110 Town Halls have been conducted with over 2700 attendees, with several individuals attending more than once. Attendence at Town Hall meetings varied enormously, from 5 to several hundred participants.
In parallel, the Yale Stress Center provided free weekly sessions in mindfulness skills coaching that were open to the community, based on ongoing Mindfulness-based Stress Reduction (MBSR) courses [18]. Since the outbreak of COVID-10, these sessions had an average of 40 enrollees weekly.
2.2. Unit level interventions
To engage many people who needed help, we needed to reach them where they were working. The Town Halls were not effectively engaging many of the members of our healthcare community, particularly physicians, who were working in the Intensive Care Units, Emergency Departments, and units caring for COVID-19 patients. In discussions with the leaders of our medical community, we learned that healthcare workers in these areas were very stressed, but also exhausted and feeling too depleted to reach out for support. We suspected that aspects of our healthcare culture reduced help-seeking, particularly the premium placed on self-reliance and the prioritization of the healthcare needs of others over self-care. Many of these highly dedicated people working on the frontlines were not sure that they needed resilience support and perhaps some were not inclined to seek help even if they sensed their need for it.
As a result, we developed three levels of site-specific outreach directed to the units with the greatest need. The first level involved peer-support, building on the experiences of the YNNHS Chief of Social Work during years of service in the National Guard. We developed a “buddy system,” that encouraged people to check-in regulary with each other and to give extra attention to those who seemed to be struggling. This inititiave complemented peer-support efforts within particular YSM Departments.
We then targeted multidisciplinary clinical teams using both “bottom-up” (targeting frontline staff) and “top-down” (targeting unit leadership) approaches. With regards to the former, the YNHH Psychological Medicine and Social Workers rounded on every unit of the hospital nearly every day with the objective of “checking in” with frontline staff to monitor stress levels and to assist with difficult situations. The time needed by these professionals to provide these services was freed up from their roles in Ambulatory Care, which were put on hold during COVID-19, and redeployed from Inpatient Units, where reduced referral rates during the peak of the pandemic. It was particularly challenging to gain entre to the Intensive Care Units for several reasons: 1) staff were too busy to make time for debriefing or support meetings, 2) there was reluctance to expend precious personal protective equipment (PPE) to support on-site consultations, and 3) we wanted to make sure that our support interventions were sufficiently impactful to justify the risk of COVID-19 exposure to our team. Instead, we instituted virtual support (“decompression”) huddles and included mental health expertise in these regular meetings.
The “top down” interventions came in the form of a Leadership Development Program supported by faculty from YSM and the School of Management. At the peak, nearly 40% of YNHH patients were infected with COVID-19. This surge required rapid repurposing of hospital units and the creation of new intensive care units. The new COVID-19 Units were led by physicians and nurses from medicine, pediatrics, and surgery, some with relatively limited leadership experience or limited familiarity with working in these settings. Further, new physician-nursing leadership dyads were learning to work together, managing rapidly evolving treatment protocols, leading staff who had not worked together previously, providing guidance to their staff about PPE and COVID-19, and managing ethical issues with patients at the end of life. Twice weekly one hour group leadership meetings were supplemented with individual coaching to enhance crisis management skills. This Program faculty also met thrice weekly to plan the interventions.
We learned that the disruption of ongoing work roles, the assumption of new roles, and the the establishment of new work relationships was extremely stressful for the leadership dyads on the new COVID-19 units. This stress significantly augmented the distress intrinsic to working with extremely ill patients suffering from a poorly understood disorder. Also, it was extremely important to support the collaboration among the leadership dyads as the distinct stresses of the doctor and nurse roles on the COVID-19 Units had the potential to create resentment, mistrust, and to break down communication and collaboration. One of the common sources of resentment was related to tasks that could or could not be conducted remotely. Many of the physician tasks could be performed remotely, while fewer of the nurses' tasks could be performed remotely. Worse, since nurses were in the hospital while some physicians were at home, remote interviewing of patients by physicians often required nursing staff to hold the tablet computer during the interview. This meant that the disparity in the burden of care was worsened. As the leadership dyads settled into their new roles, they were better able to support their clinical teams and to help them manage overall stress levels. These observations have a very important implication. If there is a second wave of COVID-19 or another disaster or pandemic, it would be extremely valuable, to the extent possible, to reconstitute the earlier COVID-19 Unit Teams rather than to assemble new teams.
2.3. Individual level interventions
We created a resource for one-to-one support. Community- and unit-level interventions were not sufficient to adequately engage or support healthcare workers. However, limitations in access to one-to-one support created gaps in our “safety net.” The existing Employee Assistance Programs (EAPs), which included 24/7 hotlines, were not not optimally utilized by our community. Although, when utilized, they were reported to be helpful.
We created a confidential web-based system rapid-response system whereby healthcare workers could sign up on-line and be contacted by a mental health professional within 24 h. Users of this service received a 2–3 session (45–60 min) acute traumatic stress intervention developed within the Yale Child Study Center [10] that focused on assessment and coping skills. The intervention was delivered by trained clinician volunteers, advertised as confidential, and provided without charge. Treaters were volunteers from the faculty and trainees of the Departments of Psychiatry and Child Study Center, the YNHHS Department of Social Work, YNHHS and CMHC the YNHHS Nursing Service (advanced practice nurses), and the Western New England Psychoanalytic Institute. We referred patients needing longer-term care to the appropriate EAP or directly to community-based clinicians.
In addition, YSM and YNHH addressed structural contributors to stress by providing housing to healthcare workers who were concerned about exposing their families to the COVID-19 virus and delivering meals to healthcare workers who required quarantine due to COVID-19 exposure or infection.
2.3.1. Implementing a proactive outreach strategy
Underutilization of support services in traumatized individuals is a problem common among the military [19], veterans [20], and civilian populations after disasters [21]. We needed an outreach strategy to engage healthcare workers. The first step was to develop a common site for all support resources provided within our community, the “Care for the Caregivers” Website (https://medicine.yale.edu/caregivers/). This website provided a wide range of resources intended to promote self-care, enhance management of work-related stress, and to promote overall wellness and resilience. From April 12, 2020, when it was created, to July 7, 2020, when this article was prepared, 2534 users accessed this website. The five most highly visited pages on this website were “Building Resilience” (1955 page views, it provides information on Town Halls, One-to-One Support, EAPs, and web-based self-guided care), “Home” (1945 pageviews, provides information about sleep, nutrition, relaxation, childcare), “Self-Guided Care” (413 page views, it provides information about meditation exercises, quiet rooms, managing emotions, online CBT programs, contact information for accessing individual treatment via particular insurance plans, and links to assessment and recovery resources provided by the VA's National Center for PTSD).
We then linked a pro-active stress self-assessment to referral for one-to-one services or alternative resilience-promoting programs. We developed a web-based version of a brief stress self-assessment, The Yale Stress Self-Assessment for COVID-19 (YSSA-COVID-19; Table 2 ), with items selected from established sources [[22], [23], [24], [25]]. This questionnaire typically took approximately 3 min to complete (https://yalesurvey.ca1.qualtrics.com/jfe/form/SV_esb27uCIL5PFse9). The scale provided feedback on the level of stress (low, medium, high) and asked participants whether they would like to “talk to someone.” If the answer was yes, a direct link took them to the “Care for the Caregivers” Website. There, they could enroll in one-to-one services, support materials, and other resources. These resources were also made available in our Quiet Reset Rooms, which were set up near high acuity work-units.
Table 2.
The Yale Stress Self-Assessment for COVID-19 (YSSA-COVID-19). Overall stress scores: 0–9 (mild), 10–15 (moderate), 16–20 (high). Overall stress was assessed using the following items: loss of confidence in managing work, family, and life demands; exposure to death or threat of death for self and loved ones; feeling out of control; feeling guilty or ashamed; and blaming others for their distress. Stress symptom scores: 0–4 (mild), 5–9 (moderate), 10–17 (high). Participants were asked to rate increases in symptoms associated with the pandemic and reflect a degree of increased level of stress above the usual level of stress.
| Overall stress during Covid-19 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Stress signs |
| Check-in with yourself – have you noticed an increase in any of the following stress signs, three or more times per week? Please check all that you have notices: |
| □ Tired, exhausted or fatigued |
| □ Sleep difficulties |
| □ Forgetting things |
| □ Irritable, frustrated or emotional |
| □ Anxious, tense, nervous |
| □ Racing or slowing thoughts |
| □ Losing focus or concentration |
| □ Feeling down or hopeless |
| □ Feeling of grief or loss |
| □ Distant and cut off from people |
| □ Headaches |
| □ Aches and pains |
| □ Alcohol use |
| □ Dwelling on past events |
| □ Other signs specific to you |
The third step was to disseminate the stress self-assessment to all YSM and YNHH faculty, staff, and trainees, which revealed high levels of stress. Three waves of survey distribution to over 40,000 individuals resulted in 8299 people completing the assessment. We enabled repeated self-assessment to detect persisting stress symptoms, a predictor of the later development of post-traumatic stress disorder [26]. Topline results from this survey are presented in Table 3 . As can be seen, the sample was predominately female, mostly non-physicians, and were predominately hospital employees. The key findings were: 1) over half (53.4%) of respondents were experiencing a moderate-to-severe increase in stress-related symptoms above their usual level of stress; 2) 30.2% of respondents reported moderate-to-high levels of overall stress (see Table 2 for details); and 3) on average, i.e., regardless of their role, respondents experienced mild-to-moderate levels of overall stress and stress symptoms. A future report will share findings arising from the analyses of the stress questionnaire data. These concerning numbers suggest significant rates and levels of COVID-19-related distress that were increased from those of the usual high-stress healthcare work environment.
Table 3.
Top-line Yale Stress Self-Assessment for COVID-19 (YSSA-COVID-19) results from 8299 respondents, approximately 20% of the sample invited to complete the questionnaire.
| Age: Mean (SD) [N] | 45.1 (12.9) (n = 7850) |
|---|---|
| Gender | |
| Women (N[%]) | 6547 [78.9] |
| Men (N[%]) | 1603 [19.3] |
| Non-Binary (N[%]) | 19 [0.2] |
| Other/Missing (N[%]) | 130 [1.6] |
| Staff discipline | |
| Physician (N[%]) | 710 [8.6] |
| Non-Physician (N[%]) | 7544 [90.9] |
| Missing (N[%]) | 45 [0.5] |
| Affiliation | |
| Yale School of Medicine (N[%]) | 1342 [16.2] |
| Yale Medicine (N[%]) | 581 [7.0] |
| Yale New Haven Health System (N[%]) | 6261 [75.4] |
| Missing (N[%]) | 115 [1.4] |
| Mean overall stress scores | |
| Overall Stress: Mean (SD) | 7.6 (4.0) |
| Stress Symptoms: Mean (SD) | 5.52 (3.9) (n = 7253) |
| Moderate/High Stress Scores (N[%]) | 2505 [30.2] |
| Moderate/High Stress Symptoms (N[%]) | 3871 [53.4] (n = 7253) |
The fourth step, was to reach out to YSM Department chairs and Clinical Section Chiefs to encourage department-specific Town Hall Meetings. This was a group that was not accustomed to discussing mental illness or its treatment. However, we knew that they would be critical for increasing awareness about stress and resilience, reducing stigma associated with help-seeking, and promoting utilization of the resources throughout our physician community. We used the Town Halls to learn about the stress that people were experiencing, to advocate for completion of the stress self-assessments, and to invite faculty, if desired, to make use of the other support resources.
Despite these efforts, we failed to engage many people who were suffering and who wanted help. In particular, as reflected in Table 2, we were less successful in getting males and M.D.s to complete the stress self-assessments. Our initial concern was that our infrastructure would be overwhelmed by large numbers of people seeking help. However, utilization of the individual support program was quite less than expected. Of the 8299 survey completers, 660 people completed an additional question and indicated an interest in seeking counseling, while 2573 people chose not respond to this question. Thus, we expected far more than the 70 people who completed an additional screening questionnaire and signed up for one-to-one support. Of those who completed the questionnaire, 19 did not respond to outreach. Thus, as of July 7, only 51 individuals, received support, i.e., 7.7% of the people who expressed an interest in counseling.
3. Lessions learned
3.1. Focusing on the Dedicated Town Halls
The General Town Halls initially attracted reasonably high levels of attendance from diverse elements of our community (50–70 attendees every day). However, over time, attendance dwindled for the General Town Halls but remained high for the Dedicated Town Halls. Given our experience, if we experience a “second wave” of COVID-19, we would focus our efforts on the Dedicated Town Halls.
3.1.1. Mobilizing broader institutional support for the one-to-one support sessions
Many people who were suffering and who expressed a desire for counseling were reluctant to follow through with treatment for reasons that are not clear. Informal discussions with healthcare workers suggested that some were embarrassed about seeking mental health support, perhaps as a consequence of stigma. Others were concerned about their privacy and that reporting difficulties might trigger obligatory reporting to the Department of Public Health, potentially threatening their medical licenses. As a result, it is possible that the “sign up questionnaire” that we created to enable access to one-to-one support served as a barrier to engagement. However, we saw a similar pattern when we offered physicians in two hospitals the opportunity to “touch base” with a counselor; most simply failed to show up for appointments that they had scheduled. It is possible that the gap is not as serious as it seems, as some individuals may have utilized the self-help resources provided by our website or obtained support through alternative venues, particularly via the EAPs and the university health service. In retrospect, it may have been helpful to mobilize Department and Section leaders as advocates for one-to-one car earlier in the pandemic to obtain higher rates of physician participation.
3.2. Childcare: a critical unmet need
The COVID-19 pandemic put many healthcare working parents in a nearly unmanageable position. In order to live up to their work commitments, they needed to spend a great deal of time away from home, sometimes upredictably, while their children were sheltering in place at home. The closure of childcare programs and schools necessitated home schooling. The closure of summer camps and continued limits on center-based childcare will add further stress. Further, healthcare workers in hospital settings increased their risk of COVID-19 exposure for their families. Solutions that quarantined healthcare workers from their families reduced the risk of transmitting infections at the cost of increasing other aspects of family stress, including separation from their children and increasing childcare burden on other family members.
Parenting stress is a common problem for healthcare workers in the pandemic era. Data suggest that 29% of healthcare provider households in the U.S. have at least one child between the ages of 3–12, while 7% involve single parents [27]. Further, childcare resources were significantly constrained by the impact of sheltering in place, worsening the burden on healthcare worker parents. Even prior to COVID, the shortage of quality center-based childcare capacity placed significant burdens on the families of healthcare workers and society, broadly.
Childcare stresses are among the most common concerns expressed by men and women in the one-to-one, unit-based, and community-based interventions. Counseling and support to parents can be helpful. However, the lack of adequate childcare resources for healthcare workers is a structural, not a psychological, problem. The real solution is to expand in-home childcare resources (including a central coordination and training of in-home childcare professionals) now and in advance of the emergence of any future pandemic so that healthcare working parents can obtain the support they need.
Currently, with support from Yale University, we are creating an in-home provider network comprised of professionals who will receive additional training in child development and who will be supported by experts who provide consultation as needed. These in-home services would provide care, school programming, and infection control practices for younger children.
3.3. The impact of racism
For most healthcare workers, responding to COVID-19 proved to be only one of several painful and concurrent challenges. The cumulative impact of several tragic murders by police of African-Americans including George Floyd, Breonna Taylor, Daniel Prude, and Murbarak Sulemane shook our community. These events coincided with the disproportionate impact of COVID-19 in our local Black Community. Both of these issues highlighted longstanding tensions in our community related to disparities in the racial composition of our faculties, leadership groups, and in many of our training programs. The result was heightened distress experienced across our healthcare community, particularly so for our Healthcare Workers of Color. We found that refocusing our support efforts to encompass the impact of racism and health disparities was critically important to our overall support for healthcare workers.
3.3.1. Peristing COVID-19-related stress
The peak of the COVID-19 infection in Connecticut has passed for now. There is a feeling of tremendous urgency to put COVID-19 behind us. However, the cumulative impact of exhaustion, daily confrontation with death, persisting threat of infection, and feelings of isolation persist. The acute stress of the pandemic has transformed into chronic stress. Healthcare workers, like society at large, are depleted by the persisting disruption of routines, social isolation, and uncertainty regarding the subsequent waves of COVID-19 infection.
Most people are rebounding from stresses experiences at the peak of the pandemic. However, it will be important to identify people with persisting stress-related problems arising from the pandemic. For these people, promoting a healthy lifestyle, such as a healthy diet, exercise, and reengaging in meaningful activities can facilitate resilience. Counseling or formal treatment can also be an essential part of resuming a full and rewarding life. After extremely stressful events, approximately 5%–10% of people will experience a delayed onset of stress symptoms [28,29]. Two groups, in particular, are at increased risk for persisting or delayed symptoms. People with psychiatric disorders may experience COVID-19 related stress more intensely [30], increasing their risk for illness exacerbation. Also, COVID-19 infection may trigger a persisting pro-inflammatory state that contributes to persisting depression-like symptoms [31,32].
3.3.2. Sustainability
The support infrastructure that we created cannot be sustained without institutional investment is not yet clear. COVID-19 increased the visibility and acuity of the stress problems, but it did not create them. Stress and burnout levels were always higher than we would want in our community of healers. Levels of job satisfaction and engagement were similarly lower than desired. COVID-19 helped us demonstrate that a limited re-allocation of resources could have a meaningful impact on the resilience of our healthcare community. It is our hope that our community will learn from this experience and support the infrastructure necessary to continue this work.
3.3.3. Culture change
Our experience highlights a need for culture and policy change in medical schools and hospitals [33]. Managing mental illness had not been an explicit priority in medical school or hospital initiatives aimed at increasing wellness, reducing burnout, or increasing institutional alignment. However, symptoms of mental illness were a common consequence of serving as a healthcare worker, with 30–40% manifesting moderate-to-severe symptoms on our questionnaire. Yet, as was evident in the 20% completion rate for the stress self-assessment questionnaires and the paltry utilization of one-to-one support, we have a long way to go to create a culture where active engagement in self-care is considered an obligation of membership in the healthcare community. Further, we need to do a better job of engaging leaders, at all levels, in promoting the mental health self-care of their teams. High rates of people were suffering emotionally during the COVID-19 pandemic and many continue to suffer. Prior to COVID-19, we were not well-prepared to deal with the psychological impact of a disaster on our community, or its overall mental health. Our experience attempting to respond to this need highlighted both opportunities and continuing challenges. The COVID-19 pandemic has been a time for transformative change in healthcare. Perhaps this crisis is an opportunity to create better infrastructure and culture change so that we can do a better job of addressing the ongoing mental health needs of healthcare workers.
Financial disclosures
The Individual Consultant Agreements listed below are less than $10,000 per year: Consultant: Aptinyx, Inc., AstraZeneca Pharmaceuticals, Biogen, Idec, MA, Biomedisyn Corporation, Bionomics, Limited (Australia), Boehringer Ingelheim International, COMPASS Pathways, Limited, United Kingdom, Concert Pharmaceuticals, Inc., Epiodyne, Inc. EpiVario, Inc. Heptares Therapeutics, Limited (UK) Janssen Research & Development Otsuka America Pharmaceutical, Inc., Perception Neuroscience Holdings, Inc. Spring Care, Inc., Sunovion Pharmaceuticals, Inc., Takeda Industries, Taisho Pharmaceutical Co., Ltd.
Scientific Advisory Board: Bioasis Technologies, Inc., Biohaven Pharmaceuticals, BioXcel Therapeutics, Inc. (Clinical Advisory Board) BlackThorn Therapeutics, Inc. Cadent Therapeutics (Clinical Advisory Board) Cerevel Therapeutics, LLC., EpiVario, Inc., Eisai, Inc., Lohocla Research Corporation, Novartis Pharmaceuticals Corporation, PsychoGenics, Inc., Terran Biosciences, Inc., Stock: Biohaven Pharmaceuticals, Sage Pharmaceuticals, Spring Care, Inc. Stock Options: Biohaven Pharmaceuticals Medical Sciences, BlackThorn Therapeutics, Inc., EpiVario, Inc., Terran Life Sciences Income Greater than $10,000 - Editorial Board: Editor - Biological Psychiatry. Patents and Inventions: 1) Seibyl JP, Krystal JH, Charney DS. Dopamine and noradrenergic reuptake inhibitors in treatment of schizophrenia. US Patent #:5,447,948.September 5, 1995. 2) Vladimir, Coric, Krystal, John H, Sanacora, Gerard – Glutamate Modulating Agents in the Treatment of Mental Disorders US Patent No. 8,778,979 B2 Patent Issue Date: July 15, 2014. US Patent Application No. 15/695,164: Filing Date: 09/05/2017..3) Charney D, Krystal JH, Manji H, Matthew S, Zarate C., − Intranasal Administration of Ketamine to Treat Depression United States Application No. 14/197,767 filed on March 5, 2014; United States application or Patent Cooperation Treaty (PCT) International application No. 14/306,382 filed on June 17, 2014.. 4) Zarate, C, Charney, DS, Manji, HK, Mathew, Sanjay J, Krystal, JH, Department of Veterans Affairs “Methods for Treating Suicidal Ideation”, Patent Application No. 14/197.767 filed on March 5, 2014 by Yale University Office of Cooperative Research. 5) Arias A, Petrakis I, Krystal JH. – Composition and methods to treat addiction. Provisional Use Patent Application no.61/973/961. April 2, 2014. Filed by Yale University Office of Cooperative Research. 6) Chekroud, A., Gueorguieva, R., & Krystal, JH. “Treatment Selection for Major Depressive Disorder” [filing date 3rd June 2016, USPTO docket number Y0087.70116US00]. Provisional patent submission by Yale University. 7) Gihyun, Yoon, Petrakis I, Krystal JH – Compounds, Compositions and Methods for Treating or Preventing Depression and Other Diseases. U. S. Provisional Patent Application No. 62/444,552, filed on January10, 2017 by Yale University Office of Cooperative Research OCR 7088 US01. 8) Abdallah, C, Krystal, JH, Duman, R, Sanacora, G. Combination Therapy for Treating or Preventing Depression or Other Mood Diseases. U.S. Provisional Patent Application No. 62/719,935 filed on August 20, 2018 by Yale University Office of Cooperative Research OCR 7451 US01. NON Federal Research Support: AstraZeneca Pharmaceuticals provides the drug, Saracatinib, for research related to NIAAA grant “Center for Translational Neuroscience of Alcoholism [CTNA-4]. Novartis provides the drug, Mavoglurant, for research related to NIAAA grant “Center for Translational Neuroscience of Alcoholism [CTNA-4]”.
Acknowledgements
Our Task Force acknowledges the administrative support provided by Ms. Halppen Donoghoe and the intellectual contributions of Steven M. Southwick, M.D. We also thank Ms. Lisa Maturo and Ms. Lucy Ruangvoravat for technical support. J.H.K. was supported by 2P50AA012870-20; 5UL1TR001863; and 1U01MH121766; K.Y. was supported by PCORI ID # 12891, R01AA026596, R21MD012697, R21HD102174.
References
- 1.Krystal J.H. Responding to the hidden pandemic for healthcare workers: stress. Nat Med. 2020 May;26(5):639. doi: 10.1038/s41591-020-0878-4. [DOI] [PubMed] [Google Scholar]
- 2.Rossi R., Socci V., Pacitti F., Di Lorenzo G., Di Marco A., Siracusano A., et al. Mental health outcomes among frontline and second-line health care workers during the coronavirus disease 2019 (COVID-19) pandemic in Italy. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.10185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pappa S., Ntella V., Giannakas T., Giannakoulis V.G., Papoutsi E., Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun. 2020 Aug;88:901–907. doi: 10.1016/j.bbi.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sharov K.S. Adaptation to SARS-CoV-2 under stress: role of distorted information. Eur J Clin Investig. 2020 Sep;50(9) doi: 10.1111/eci.13294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wu K., Wei X. Analysis of psychological and sleep status and exercise rehabilitation of front-line clinical staff in the fight against COVID-19 in China. Med Sci Monit Basic Res. 2020;26 doi: 10.12659/MSMBR.924085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shechter A., Diaz F., Moise N., Anstey D.E., Ye S., Agarwal S., et al. Psychological distress, coping behaviors, and preferences for support among New York healthcare workers during the COVID-19 pandemic. Gen Hosp Psychiatry. 2020;66:1–8. doi: 10.1016/j.genhosppsych.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kober H., Brewer J.A., Height K.L., Sinha R. Neural stress reactivity relates to smoking outcomes and differentiates between mindfulness and cognitive-behavioral treatments. Neuroimage. 2017;151:4–13. doi: 10.1016/j.neuroimage.2016.09.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Olson K., Marchalik D., Farley H., Dean S.M., Lawrence E.C., Hamidi M.S., et al. Organizational strategies to reduce physician burnout and improve professional fulfillment. Curr Probl Pediatr Adolesc Health Care. 2019;49:100664. doi: 10.1016/j.cppeds.2019.100664. [DOI] [PubMed] [Google Scholar]
- 9.Southwick S.M., Charney D.S. Cambridge University Press; Cambridge, UK: 2012. Resilience: The Science of Mastering Life’s Greatest Challenges. [Google Scholar]
- 10.Berkowitz S.J., Stover C.S., Marans S.R. The Child and Family Traumatic Stress Intervention: secondary prevention for youth at risk of developing PTSD. J Child Psychol Psychiatry. 2011;52:676–685. doi: 10.1111/j.1469-7610.2010.02321.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Keller R.T., Greenberg N., Bobo W.V., Roberts P., Jones N., Orman D.T. Soldier peer mentoring care and support: bringing psychological awareness to the front. Mil Med. 2005;170:355–361. doi: 10.7205/milmed.170.5.355. [DOI] [PubMed] [Google Scholar]
- 12.Nevarez M.D., Yee H.M., Waldinger R.J. Friendship in war: camaraderie and prevention of posttraumatic stress disorder prevention. J Trauma Stress. 2017;30:512–520. doi: 10.1002/jts.22224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rutherford H.J., Wallace N.S., Laurent H.K., Mayes L.C. Emotion regulation in parenthood. Dev Rev. 2015;36:1–14. doi: 10.1016/j.dr.2014.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Suchman N., Pajulo M., Decoste C., Mayes L. Parenting interventions for drug-dependent mothers and their young children: the case for an attachment-based approach. Fam Relat. 2006;55:211–226. doi: 10.1111/j.1741-3729.2006.00371.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mayou R.A., Ehlers A., Hobbs M. Psychological debriefing for road traffic accident victims. Three-year follow-up of a randomised controlled trial. Br J Psychiatry. 2000;176:589–593. doi: 10.1192/bjp.176.6.589. [DOI] [PubMed] [Google Scholar]
- 16.Pistrang N., Barker C., Humphreys K. Mutual help groups for mental health problems: a review of effectiveness studies. Am J Community Psychol. 2008;42:110–121. doi: 10.1007/s10464-008-9181-0. [DOI] [PubMed] [Google Scholar]
- 17.Van Daele T., Hermans D., Van Audenhove C., Van den Bergh O. Stress reduction through psychoeducation: a meta- analytic review. Health Educ Behav. 2012;39:474–485. doi: 10.1177/1090198111419202. [DOI] [PubMed] [Google Scholar]
- 18.Crane R.S., Brewer J., Feldman C., Kabat-Zinn J., Santorelli S., Williams J.M., et al. What defines mindfulness-based programs? The warp and the weft. Psychol Med. 2017;47:990–999. doi: 10.1017/S0033291716003317. [DOI] [PubMed] [Google Scholar]
- 19.Hoge C.W., Castro C.A., Messer S.C., McGurk D., Cotting D.I., Koffman R.L. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care.[see comment] N Engl J Med. 2004;351:13–22. doi: 10.1056/NEJMoa040603. [DOI] [PubMed] [Google Scholar]
- 20.Spoont M.R., Murdoch M., Hodges J., Nugent S. Treatment receipt by veterans after a PTSD diagnosis in PTSD, mental health, or general medical clinics. Psychiatr Serv. 2010;61:58–63. doi: 10.1176/ps.2010.61.1.58. [DOI] [PubMed] [Google Scholar]
- 21.Kung W.W., Wang X., Liu X., Goldmann E., Huang D. Unmet mental health care needs among Asian Americans 10−11 years after exposure to the world trade center attack. Int J Environ Res Public Health. 2019;16 doi: 10.3390/ijerph16071302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cohen S., Kamarck T., Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- 23.Association AP . American Psychiatric Association; Arlington, VA: 2013. Acute Stress Disorder, Section II. Diagnostic and statistical manual of mental disorders. [Google Scholar]
- 24.Association AP . 2010. Stress in America Survey: National Report - Key Findings. [Google Scholar]
- 25.Greenberg N., Langston V., Jones N. Trauma risk management (TRiM) in the UK Armed Forces. J R Army Med Corps. 2008;154:124–127. doi: 10.1136/jramc-154-02-11. [DOI] [PubMed] [Google Scholar]
- 26.Zatzick D.F., Kang S.M., Müller H.G., Russo J.E., Rivara F.P., Katon W., et al. Predicting posttraumatic distress in hospitalized trauma survivors with acute injuries. Am J Psychiatry. 2002;159:941–946. doi: 10.1176/appi.ajp.159.6.941. [DOI] [PubMed] [Google Scholar]
- 27.Bayham J., Fenichel E.P. Impact of school closures for COVID-19 on the US health-care workforce and net mortality: a modelling study. Lancet Public Health. 2020;5:e271–e278. doi: 10.1016/S2468-2667(20)30082-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Galatzer-Levy I.R., Huang S.H., Bonanno G.A. Trajectories of resilience and dysfunction following potential trauma: a review and statistical evaluation. Clin Psychol Rev. 2018;63:41–55. doi: 10.1016/j.cpr.2018.05.008. [DOI] [PubMed] [Google Scholar]
- 29.Utzon-Frank N., Breinegaard N., Bertelsen M., Borritz M., Eller N.H., Nordentoft M., et al. Occurrence of delayed-onset post-traumatic stress disorder: a systematic review and meta-analysis of prospective studies. Scand J Work Environ Health. 2014;40:215–229. doi: 10.5271/sjweh.3420. [DOI] [PubMed] [Google Scholar]
- 30.Hao F., Tan W., Jiang L., Zhang L., Zhao X., Zou Y., et al. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? Brain Behav Immun. 2020 Jul;87:100–106. doi: 10.1016/j.bbi.2020.04.069. A case-control study with service and research implications for immunopsychiatry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Troyer E.A., Kohn J.N., Hong S. Are we facing a crashing wave of neuropsychiatric sequelae of COVID-19? Neuropsychiatric symptoms and potential immunologic mechanisms. Brain Behav Immun. 2020 Jul;87:34–39. doi: 10.1016/j.bbi.2020.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lyons D., Frampton M., Naqvi S., Donohoe D., Adams G., Glynn K. Fallout from the Covid-19 pandemic - should we prepare for a tsunami of post viral depression? Ir J Psychol Med. 2020:1–10. doi: 10.1017/ipm.2020.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Moreno C., Wykes T., Galderisi S., Nordentoft M., Crossley N., Jones N., et al. How mental health care should change as a consequence of the COVID-19 pandemic. Lancet Psychiatry. 2020 Sep;7(9):813–824. doi: 10.1016/S2215-0366(20)30307-2. [DOI] [PMC free article] [PubMed] [Google Scholar]