Abstract
The United States currently has one of the highest numbers of cumulative COVID-19 cases globally, and Latino and Black communities have been disproportionately affected. Understanding the community-level factors that contribute to disparities in COVID-19 case and death rates is critical to developing public health and policy strategies. We performed a cross-sectional analysis of U.S. counties and found that a 10% point increase in the Black population was associated with 324.7 additional COVID-19 cases per 100,000 population and 14.5 additional COVID-19 deaths per 100,000. In addition, we found that a 10% point increase in the Latino population was associated with 293.5 additional COVID-19 cases per 100,000 and 7.6 additional COVID-19 deaths per 100,000. Independent predictors of higher COVID-19 case rates included average household size, the share of individuals with less than a high school diploma, and the percentage of foreign-born non-citizens. In addition, average household size, the share of individuals with less than a high school diploma, and the proportion of workers that commute using public transportation independently predicted higher COVID-19 death rates within a community. After adjustment for these variables, the association between the Latino population and COVID-19 cases and deaths was attenuated while the association between the Black population and COVID-19 cases and deaths largely persisted. Policy efforts must seek to address the drivers identified in this study in order to mitigate disparities in COVID-19 cases and deaths across minority communities.
1. Introduction
The United States currently has one of the highest rates of COVID-19 cases and deaths per capita compared to other high-income countries around the globe.1 Within the US, there is a growing body of evidence that demonstrates people of color account for a disproportionate number of COVID-19 cases, hospitalizations, and deaths.2 , 3 The Centers for Disease Control reports that Black Americans and Latinos have higher rates of COVID-19 cases and hospitalizations than White, non-Latino people.4 Although the racial and ethnic disparities in COVID-19 infection and severity have become increasingly clear, the drivers of these disparities among Black and Latino communities remain less clear at a national level.
Understanding whether there are specific community-level factors that are playing a role in driving COVID-19 disparities across minority communities is critically important. Education, for example, may be a key driver of these discrepancies, given the known relationship between education status and disease burden for other illnesses, such as cardiovascular disease.5 Recent data from Massachusetts demonstrated that several community-level factors, such as foreign-born non-citizen status, household size, and job type, potentially explain higher COVID-19 case rates among Latino communities, but not among Black communities.6 Other work has similarly found that crowded housing and working in essential services increases risk for COVID-19.7 , 8 Whether these factors also explain the high rates of COVID-19 cases and deaths across Latino and Black communities nationally is largely unknown. Furthermore, understanding the factors that are contributing to racial/ethnic disparities in COVID-19 death rates could potentially inform public health and policy strategies to reduce these health inequities.
Therefore, in this study, we sought to answer two questions. First, using national data, is there an association between the proportion of Black and Latino adults within a community and the reported number of COVID-19 cases and COVID-19 deaths per 100,000 people? Second, are there specific demographic, occupational, and economic factors that are associated with higher community-level COVID-19 case- and death-rates, which may be contributing to potential racial and ethnic disparities?
2. Methods
2.1. Data sources
We used the Johns Hopkins Coronavirus Resource Center data repository to obtain the number of confirmed COVID-19 cases and deaths per 100,000 residents by U.S. county between January 1, 2020 to September 12, 2020.1 For counties in Utah, Rhode Island, and two counties in Massachusetts (Nantucket and Dukes Counties), we used USA facts to determine the number of deaths per 100,000 between January 1, 2020 to September 12, 2020 since these counties were not reported in the Johns Hopkins dataset.9 We then used the 2018 American Community Survey to obtain demographic, economic, and occupational variables at the county level.10 Our study was structured similarly to a recent study that focused only on Massachusetts cities and towns.6 The primary variables of interest were the proportions of people in one of four mutually-exclusive racial/ethnic groups (based on self-report in the ACS): Hispanic or Latino ethnicity (referred to as Latino for brevity); Black non-Latino; White non-Latino; and Other non-Latino. Other variables were total population, average household size, median household income, the proportions of people who were age 60 years or older, proportion of adults who were employed as essential workers, proportion of adults who were foreign-born non-citizens, proportion of adults who completed less than a high school degree, and proportion of adults who commute using public transportation.
We classified employed residents into essential workers and non-essential workers.6 The following occupations as essential: health care practitioners, technical occupations, and support services; construction and extraction; installation, maintenance, and repair; material moving occupation; production services; transportation; building and grounds cleaning and maintenance; food preparation and serving-related occupation; personal care and service occupation; and protective services.6
2.2. Statistical analysis
We constructed linear regression models to assess the association between the proportions of each racial/ethnic group with the number of COVID-19 cases and deaths per 100,000 people in each county. Models were weighted by the population size of each county. We then performed a series of univariate analyses using each community-level variable as a predictor with COVID-19 case rates as the dependent variable. We then performed multivariable linear regression to assess what factors were independently associated with differences in COVID19 case rates, and importantly, assess whether they attenuated the relationship between race/ethnicity and higher case rates. We repeated both univariate and multivariate analyses to examine the relationship between community-level variables as predictors with COVID-19 death rates. The Harvard T.H. Chan School of Public Health Institutional Review Board deemed this study non-human-subjects research given the use of aggregated publicly available data. Analyses were performed using STATA Version 14.0.
3. Results
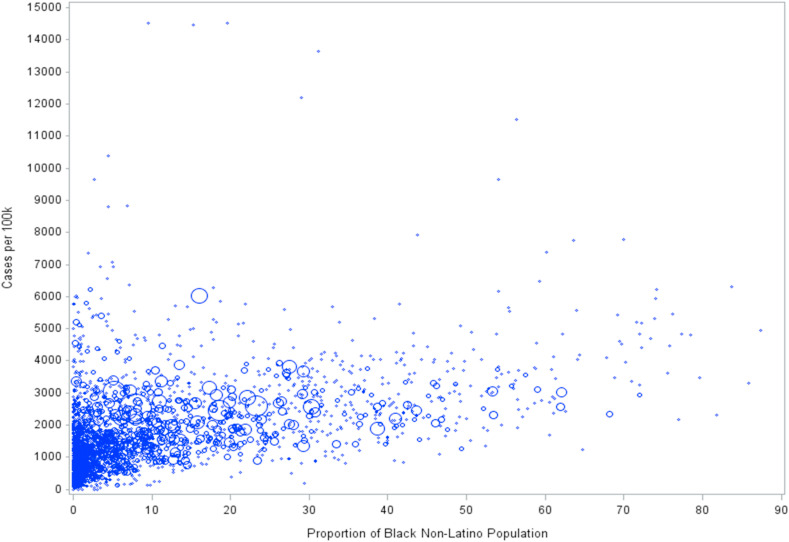
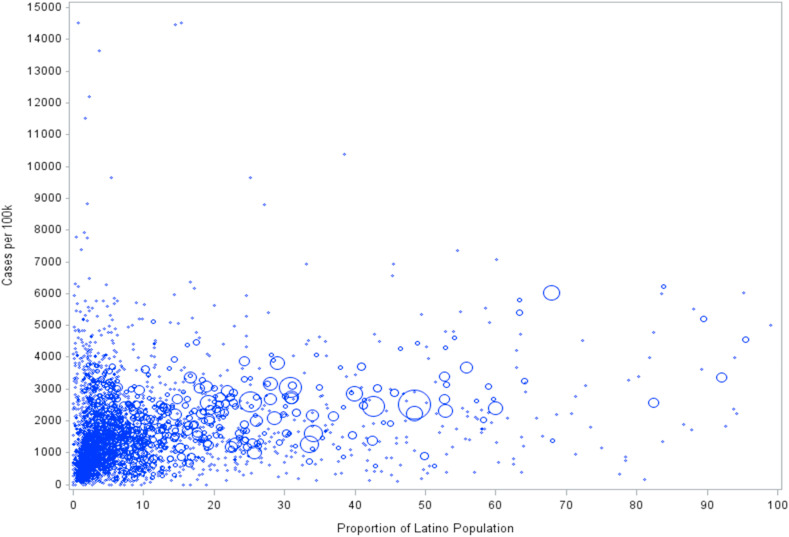
Counties with a higher proportion of Black or Latino residents generally had a higher number of COVID-19 cases per 100,000 population (Fig. 1, Fig. 2 ). In the unadjusted analyses of race/ethnicity (with White non-Latino the omitted group), a 10% point increase in the Black population was associated with an increase of 324.7 [95% CI 298.0 to 351.4, p < 0.001] cases per 100,000 people (Table 1 ). A 10% point increase in the Latino population was associated with an increase of 293.5 [95% CI 274.8 to 312.2, p < 0.001] cases per 100,000, while a 10% point increase in the Other non-Latino population was associated with a decrease of 81.0 [95% CI -125.7 to -36.2, p < 0.001] cases per 100,000.
Fig. 1.
Proportion of Black Non-Latino Population and Number of COVID-19 Cases per 100,000 Across U.S. Counties.
Figure shows the relationship between proportion of Black Non-Latinos residing in a county and COVID-19 case rates. The size of each circle reflects the total population of each county.
Fig. 2.
Proportion of Latino Population and Number of COVID-19 Cases per 100,000 Across U.S. Counties.
Figure shows the relationship between proportion of Latinos residing in a county and COVID-19 case rates. The size of each circle reflects the total population of each county.
Table 1.
Association of race/ethnicity, demographic, economic, and occupational factors with COVID-19 case rates across U.S. Counties.
| County Characteristics | Increases in cases per 100,000 people |
|||||
|---|---|---|---|---|---|---|
| Univariate Analyses |
Multivariable Analyses |
|||||
| Estimate | 95% CI | P-value | Estimate | 95% CI | P-value | |
| Proportion of Black non-Latino Population | 324.7 | 298.0 to 351.4 | <0.001 | 278.1 | 252.2 to 303.9 | <0.001 |
| Proportion of Latino Population | 293.5 | 274.8 to 312.2 | <0.001 | 23.8 | -13.5 to 61.2 | 0.21 |
| Proportion of Other Non-Latino Population | -81.0 | -125.7 to -36.2 | <0.001 | -268.9 | -310.5 to -227.3 | <0.001 |
| City/town population size | 1.3 | 1.1 to 1.5 | <0.001 | -0.5 | -0.6 to -0.3 | <0.001 |
| Age, Proportion age >60 years | -600.3 | -673.8 to -526.9 | <0.001 | 155.8 | 84.1 to 227.6 | <0.001 |
| Average Household size (per 1 person increase) | 1559.5 | 1433.9 to 1685.1 | <0.001 | 1117.3 | 934.4 to 1300.2 | <0.001 |
| Proportion with < HS education | 990.8 | 933.2 to 1048.5 | <0.001 | 208.8 | 106.5 to 311.1 | <0.001 |
| Median income | -108.6 | -129.4 to -87.7 | <0.001 | -112.7 | -143.1 to -82.2 | <0.001 |
| Proportion of essential workers | 138.0 | 89.6 to 186.3 | <0.001 | -102.9 | -176.8 to -29.1 | 0.01 |
| Proportion of foreign-born non-citizens | 903.4 | 843.4 to 963.4 | <0.001 | 803.7 | 682.8 to 924.6 | <0.001 |
| Proportion of workers that commute using public transportation | 185.8 | 150.0 to 221.6 | <0.001 | 3.8 | -28.9 to 36.5 | 0.82 |
For univariate and multivariate analyses.
-Changes in case rates reflect a per 10% point increase in the following variables: Proportion Black, Latino, Other non-Latino population, age over 60 years, people with less than a high school education, essential workers, foreign-born non-citizens, proportion of people who commute to work by public transportation.
-For county population size, changes in case rates reflect a per 10,000 people increase.
-For average household size, changes in case rates reflect a per 1 person increase.
-For median income, changes in case rates reflect a per $10,000 increase.
After multivariable adjustment, the association between the Black population and case rates persisted. A 10% point increase in the Black population was associated with an additional 278.1 [95% CI 252.2 to 303.9, p < 0.001] cases per 100,000. In contrast, the association between the Latino population and case rates was substantially attenuated and no longer statistically significant (23.8 [95% CI -13.5 to 61.2, p = 0.2108] cases per 100,000). The association between the Other non-Latino population and cases remained significantly negative – a 10% point higher population was associated with fewer cases per 100,000 (-268.9 [95% CI -310.5 to -227.3, p < 0.001]).
3.1. Race/ethnicity and COVID-19 deaths
In the unadjusted analyses of race/ethnicity, a 10% point increase in the Black population was associated with an increase of 14.5 [95% CI 12.9 to 16.0, p < 0.001] deaths per 100,000 (Table 2 ). A 10% point increase in the Latino population was associated with an increase of 7.6 [95% CI 6.5 to 8.8, p < 0.001] deaths per 100,000, while a 10% point increase in the Other non-Latino population was associated with an increase of 5.7 [95% CI 3.1 to 8.2, p < 0.001] deaths per 100,000.
Table 2.
Association of race/ethnicity, demographic, economic, and occupational factors with COVID-19 deaths across U.S. Counties.
| County Characteristics | Increases in deaths per 100,000 people |
|||||
|---|---|---|---|---|---|---|
| Univariate Analyses |
Multivariable Analyses |
|||||
| Estimate | 95% CI | P-value | Estimate | 95% CI | P-value | |
| Proportion of Black non-Latino Population | 14.5 | 12.9 to 16.0 | <0.001 | 9.3 | 8.0 to 10.6 | <0.001 |
| Proportion of Latino Population | 7.6 | 6.5 to 8.8 | <0.001 | 0.4 | -1.5 to 2.4 | 0.69 |
| Proportion of Other Non-Latino Population | 5.7 | 3.1 to 8.2 | <0.001 | -11.9 | -14.0 to -9.7 | <0.001 |
| City/town population size | 0.0 | 0.0 to 0.1 | <0.001 | 0.0 | 0.0 to 0.0 | 0.001 |
| Age, Proportion age >60 years | -6.8 | -11.2 to -2.5 | 0.002 | 28.0 | 24.2 to 31.7 | <0.001 |
| Average Household size (per 1 person increase) | 30.0 | 22.3 to 37.6 | <0.001 | 56.4 | 46.9 to 66.0 | <0.001 |
| Proportion with < HS education | 31.5 | 27.8 to 35.1 | <0.001 | 13.8 | 8.4 to 19.1 | <0.001 |
| Median income | 1.1 | -0.1 to 2.3 | 0.084 | 1.6 | 0.0 to 3.2 | 0.047 |
| Proportion of essential workers | -5.2 | -8.0 to -2.5 | <0.001 | -2.5 | -6.3 to 1.4 | 0.206 |
| Proportion of foreign-born non-citizens | 40.4 | 36.8 to 44.0 | <0.001 | 0.9 | -5.4 to 7.2 | 0.773 |
| Proportion of workers that commute using public transportation | 40.4 | 38.9 to 41.9 | <0.001 | 41.0 | 39.3 to 42.7 | <0.001 |
For univariate and multivariate analyses.
-Changes in death rates reflect a per 10% point increase in the following variables: Proportion Black, Latino, Other non-Latino population, age over 60 years, people with less than a high school education, essential workers, foreign-born non-citizens, commute to work by public transportation.
-For county population size, changes in death rates reflect a per 10,000 people increase.
-For average household size, changes in death rates reflect a per 1 person increase.
-For median income, changes in death rates reflect a per $10,000 increase.
After multivariable adjustment, the association between the Black population and death rates persisted. A 10% point increase in the Black population was associated with an additional 9.3 [95% CI 8.0 to 10.6, p < 0.001] deaths per 100,000. In contrast, the association between the Latino population and death rates was substantially attenuated and no longer statistically significant (0.4, [95% CI -1.5 to 2.4, p = 0.6859]). The relationship between the proportion of the Other non-Latino population and death rates became significantly negative, with a 10% point higher population associated with a decrease of 11.9 [95% CI -14.0 to -9.7, p < 0.001] deaths per 100,000.
3.2. Association of demographic, economic, and other factors with COVID-19 cases
Several factors were associated with higher COVID-19 case rates across counties nationally in our unadjusted models: higher average household size; lower median household income; a larger share of individuals with less than a high school diploma, essential workers, and foreign-born non-citizens; and a higher proportion of workers who commute using public transportation (Table 1). After multivariable adjustment, average household size, share of individuals with less than a high school diploma, median household income, and percentage of foreign-born non-citizens remained significantly associated with COVID-19 case rates. The multivariate model demonstrated that average household size was the strongest predictor of COVID-19 cases (1117.3 additional cases per a 1 person increase in the household size, 95% CI 934.4 to 1300.2, p < 0.001), followed by percentage of foreign-born non-citizens (803.7 additional cases per 10% point increase in proportion of foreign-born non-citizens, 95% CI 682.8 to 924.6, p < 0.001).
3.3. Association of demographic, economic, and other factors with COVID-19 deaths
In univariate analyses of COVID-19 deaths, several factors were significantly associated with higher COVID-19 mortality rates across counties: higher average household size; a larger share of individuals with less than a high school diploma, essential workers, and foreign-born non-citizens; and a higher proportion of workers who commute using public transportation (Table 2). After multivariable adjustment, average household size, percentage of the population with less than a high school diploma, and percentage of workers that commute using public transportation remained significantly associated with COVID-19 death rates. In the multivariate analyses, average household size was the strongest predictor of COVID-19 deaths (56.4 additional deaths per 10% point increase in household size, 95% CI 46.9 to 66.0, p < 0.001), followed by percentage of workers that commute using public transportation (41.0 additional deaths per 10% point increase in proportion of workers, 95% CI 39.3 to 42.7, p < 0.001).
4. Discussion
Across the United States, Black and Latino communities are experiencing higher rates of COVID-19 cases and deaths. Several community-level factors, such as low educational attainment, household size, and foreign-born non-citizen status, were independently associated with risk of COVID-19 infection and death. Similar to a recent study in Massachusetts,6 these factors appear to explain the higher COVID-19 case and mortality rates in Latino communities but only partially account for the disproportionately higher rates in Black communities.
Our findings shed important insights into the key community-level factors associated with a higher risk of COVID-19 infection and mortality. One key predictor was a low level of educational attainment within a community. During the pandemic, individuals with a high school diploma or less are less likely than those with at least some college education to telework, or more broadly, work in low contact positions in response to COVID-19.11 Furthermore, persons with lower levels of educational attainment are more likely to be specific types of essential workers (e.g. food service workers), who may not have the option to work from home. Given the risks of essential jobs and in-person work during the pandemic, this may at least partially be driving some of the educational disparities in COVID-19 cases.12 For this reason, it is crucial that employers and states ensure adequate paid sick leave, especially for low-wage, essential workers, to reduce the potential exposure risk to COVID-19 that may be associated with differences in educational attainment.
Other community-level factors, such as crowded housing and high use of public transportation were also independently associated with higher rates of COVID-19 cases and deaths. This aligns with prior research that found that in urban communities, factors such as unemployment, crowded housing, and vehicle access were associated with increased diagnosis of and mortality from COVID-19.13 Interestingly, a greater proportion of essential workers was not associated with more COVID-19 cases after adjustment. In fact, it appeared to confer protection. However, it is important to note that the variable of essential service jobs includes many high-income occupations like healthcare workers and other relatively well-paying jobs like those in protective services. In a recent study, only occupation in the food service preparation industry was associated with high case rates.6
We also found that foreign-born non-citizen status is an important driver of increased case rates in these communities, especially among Latino communities. Given the Trump Administration's recent revision to the “Public Charge” Rule, which aims to prevent immigrants who utilize public benefits, like Medicaid, from gaining permanent residency status, as well as general mistrust in the medical field, immigrant communities may be hesitant to seek testing or medical care for COVID-19.14 This may prevent individuals from receiving the kind of public health guidance necessary to quarantine in a safe and timely manner, which may lead to further spread of the disease and worsen patient outcomes.15 While initially there was a ruling in July 2020 that stated the public charge rule would not go into effect until after the federal declaration of a national emergency related to COVID-19 was over,16 the Trump administration unfortunately overturned this decision, thereby allowing the public charge rule to continue being applied for immigrants seeking residency.17 Therefore, containment efforts will continue to be compromised until the new public charge rule is eliminated permanently.
Of note, while adjustment for community-level factors examined in this study seemed to account for most of the COVID-19 disparities in Latino communities, disparities among Black communities largely persisted. This finding highlights the need for further research to understand the key drivers of higher case and death rates in Black communities. One potential reason may be poor access to high-quality care, such as delayed access to diagnostic testing.18 , 19 Other important reasons may be related to longstanding issues of structural racism and systemic inequities among the Black community, which can contribute to higher rates of morbidity and mortality among people of color.20 , 21 Neighborhood segregation in dense living areas and poor living environments, such as greater exposure to air pollution,22, 23, 24 may also be playing an important role.
4.1. Limitations
There are important limitations to this study. First, individual-level data by race/ethnicity and other socioeconomic variables are not currently publicly available across all US counties. Therefore, we are limited to community-level analyses, which may be subject to ecological fallacy. However, our findings closely match individual-level disparities reported in studies that used patient-level data.25 , 26 Second, currently not all states report COVID-19 testing data by race.27 Given the evidence of racial and ethnic disparities in diagnostic testing access,18 it is possible that our study is underestimating disparities in case rates.
5. Conclusion
Across U.S. counties, there are significant racial and ethnic disparities in COVID-19 case rates and mortality rates. Important community-level factors—like crowded housing, recent immigrant status, low-level of educational attainment, and public transportation use—are significantly associated with higher COVID-19 case and/or death rates within communities. While these factors explain the disparities among Latino communities, further research is needed to understand how socioeconomic factors, as well as structural inequities and racism, have contributed to the higher burden of COVID-19 in Black communities.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Johns Hopkins University Centers for Systems Science and Engineering (CSSE) 2020. Coronavirus COVID-19 Global Cases.https://coronavirus.jhu.edu/map.html Accessed. [Google Scholar]
- 2.Kendi I.X. The Atlantic. 2020. What the racial data show.https://www.theatlantic.com/ideas/archive/2020/04/coronavirus-exposing-our-racial-divides/609526/ Accessed. [Google Scholar]
- 3.Wadhera R.K., Wadhera P., Gaba P., et al. Variation in COVID-19 hospitalizations and deaths across New York city boroughs. J Am Med Assoc. 2020;323(21):2192–2195. doi: 10.1001/jama.2020.7197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.COVID-19 hospitalization and death by race/ethnicity. Center for Disease Control and Prevention. August 18, 2020:2020. [Google Scholar]
- 5.Kubota Y., Heiss G., MacLehose R.F., Roetker N.S., Folsom A.R. Association of educational attainment with lifetime risk of cardiovascular disease: the atherosclerosis risk in communities study. JAMA Intern Med. 2017;177(8):1165–1172. doi: 10.1001/jamainternmed.2017.1877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Figueroa J.F., Wadhera R.K., Lee D., Yeh R.W., Sommers B.D. Community-level factors associated with racial and ethnic disparities in COVID-19 rates in Massachusetts. Health Aff. 2020 doi: 10.1377/hlthaff.2020.01040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lofquist D.A. United States Census Bureau; October 1, 2012 2012. Multigenerational Households: 2009-2011. ACSBR/11-03. [Google Scholar]
- 8.Labor Force Characteristics by Race and Ethnicity. U.S. Bureau of Labor Statistics; October: 2018. p. 1082. 2019 2019. [Google Scholar]
- 9.USAFacts U.S. 2020. Coronavirus Cases and Deaths: Track COVID-19 Data Daily by State and County.https://usafacts.org/visualizations/coronavirus-covid-19-spread-map/ [Google Scholar]
- 10.Bureau USC. American Community Survey. Washington DC2020.
- 11.Daly M.C., Buckman S.R., Seitelman L.M. Federal Reserve Bank of San Francisco; 2020. The Unequal Impact of COVID-19: Why Education Matters. [Google Scholar]
- 12.Selden T.M., Berdahl T.A. COVID-19 and racial/ethnic disparities in health risk, employment, and household composition. Health Aff. 2020;39(9):1624–1632. doi: 10.1377/hlthaff.2020.00897. [DOI] [PubMed] [Google Scholar]
- 13.Khazanchi R., Beiter E.R., Gondi S., Beckman A.L., Bilinski A., Ganguli I. County-level association of social vulnerability with COVID-19 cases and deaths in the USA. J Gen Intern Med. 2020;35(9):2784–2787. doi: 10.1007/s11606-020-05882-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sommers B.D., Allen H., Bhanja A., Blendon R.J., Orav E.J., Epstein A.M. Assessment of perceptions of the public charge rule among low-income adults in Texas. JAMA Netw Open. 2020;3(7) doi: 10.1001/jamanetworkopen.2020.10391. e2010391-e2010391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wen L.S., Sadeghi N.B. Health Affairs; 2020. Addressing Racial Health Disparities in the COVID-19 Pandemic: Immediate and Long-Term Policy Solutions. [Google Scholar]
- 16.Soronen L. Public Charge Rule No Longer in Effect until the End of COVID-19. CitiesSpeak2020.
- 17.Peck A.L., Neifach M.H. DHS may resume public charge rule, federal appeals court rules. The National Law Review. 2020 [Google Scholar]
- 18.Farmer B. Long-standing racial and income disparities seen creeping into COVID-19 care. Kaiser Health News. April 6, 2020:2020. [Google Scholar]
- 19.Lieberman-Cribbin W., Tuminello S., Flores R.M., Taioli E. Disparities in COVID-19 testing and positivity in New York city. Am J Prev Med. 2020;59(3):326–332. doi: 10.1016/j.amepre.2020.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ford C.L., Airhihenbuwa C.O. Critical Race Theory, race equity, and public health: toward antiracism praxis. Am J Publ Health. 2010;100(Suppl 1):S30–S35. doi: 10.2105/AJPH.2009.171058. Suppl 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Boyd R.W., Lindo E.G., Weeks L.D., McLemore M.R. Health Affairs; 2020. On Racism: A New Standard for Publishing on Racial Health Inequities. [Google Scholar]
- 22.Bennett J.E., Tamura-Wicks H., Parks R.M., et al. Particulate matter air pollution and national and county life expectancy loss in the USA: a spatiotemporal analysis. PLoS Med. 2019;16(7) doi: 10.1371/journal.pmed.1002856. e1002856-e1002856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hajat A., Hsia C., O'Neill M.S. Socioeconomic disparities and air pollution exposure: a global Review. Curr Environ Health Rep. 2015;2(4):440–450. doi: 10.1007/s40572-015-0069-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wu X., Nethery R.C., Sabath B.M., Braun D., Dominici F. Exposure to Air Pollution and COVID-19 Mortality in the United States: A Nationwide Cross-Sectional Study. medRxiv. 2020 doi: 10.1101/2020.04.05.20054502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Richardson S., Hirsch J.S., Narasimhan M., et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York city area. J Am Med Assoc. 2020;323(20):2052–2059. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Price-Haywood E.G., Burton J., Fort D., Seoane L. Hospitalization and mortality among Black patients and white patients with covid-19. N Engl J Med. 2020;382(26):2534–2543. doi: 10.1056/NEJMsa2011686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Center JHUMCR Racial data transparency. 2020. https://coronavirus.jhu.edu/data/racial-data-transparency Accessed.