Abstract
Introduction
postpartum depression (PPD) continues to become one of the major maternal health challenges across the globe but there is a paucity of recent data on its magnitude in Africa. This study was motivated by the need to update the current magnitude of PPD in Africa based on various assessment tools.
Methods
a total of 21 articles met the study criteria. Fifteen articles used the EPDS and six used other assessment tools. Postpartum depression among studies that used EPDS tool ranged from 6.9% in Morocco to 43% in Uganda and 6.1% in Uganda to 44% in Burkina Faso among studies that used other depression assessment tools. Sensitivity and specificity results of the EPDS ranged from 75%-100% and 87%-98% respectively.
Results
a total of 21 articles met the study criteria. Fifteen articles used the EPDS and six used other assessment tools. Postpartum depression among studies that used EPDS tool ranged from 6.9% in Morocco to 43% in Uganda and 6.1% in Uganda to 44% in Burkina Faso among studies that used other depression assessment tools. Sensitivity and specificity results of the EPDS ranged from 75%-100% and 87%-98% respectively.
Conclusion
despite the limited dearth of literature, the magnitude of PPD in Africa remains high which suggests that PPD is still a neglected illness and calls for immediate interventions. EPDS is an effective tool with high sensitivity and specify in varying study contexts.
Keywords: Postpartum depression, prevalence, magnitude, burden, Africa
Introduction
Postpartum depression (PPD) continues to become one of the major maternal health challenges across the globe [1-3]. A diagnostic criterion for PPD is occurrence within six weeks to six months following childbirth and symptoms must manifest for at least two weeks. PPD is one of the most challenging complications of pregnancy due to adverse effects on the health of the mother, infant, family, and community at large [4]. Detrimental consequences of PPD include diminished mother to child bonding, childhood growth impairment and underdevelopment, infanticide, and suicide [5,6]. PPD is characterized by loss of interest in usual events, sleep challenges, feelings of sadness, fatigability, problems of appetite, and difficulty in coping with daily activities [7]. Because postpartum depression is one of the most common treatable complications of the postpartum period, it is paramount that health workers identify and manage the condition promptly and effectively.
Determining the current global PPD prevalence has remained a challenge due to use of varying assessment tools, adoption of different cut-off points for those tools, the varying cultural contexts, and the dearth of studies carried out in resource-limited environments [2]. Researchers [1-3] continue to show conflicting PPD prevalence rates. Between 2012 and 2016, the global mean prevalence for PPD was reported between 15% and 25% [1-3], a higher value than the 12% to13% reported in 2007 [8], thus suggesting an increasing PPD prevalence. PPD is more rampant by 25% in low-and middle- income countries as compared to developed countries [2,9-11]. Literature reports specific countries postpartum depression rates to be 10.1 percent in Norway [12], 8 to 10 percent in Netherlands [13,14], 3.9 to 17.6 percent in Portugal [15-17] , 8 to 12.3 percent in Sweden [18-20] while in United States of America, it is estimated at 8 to 15 percent [21-24].
In Africa, studies on the magnitude of postpartum depression remain scanty [25,26].The few existing studies estimate the magnitude to be 15 to 25 percent [27-32]. Because the prevalence of PPD is projected to be higher in Africa than the global mean prevalence [33], there is still a paucity of data available in many African countries. This lack of consistent data has compromised the development of a cumulative body of knowledge regarding the multi-cultural prevalence and magnitude of PPD [34]. This review therefore aims at summarizing and synthesizing the current magnitude of postpartum depression among mothers based on various assessment tools in Africa.
Methods
A review of literature was undertaken from seven electronic databases which included PubMed, Google Scholar, CINAHL, Africa Bibliography, Bibliography of Africana Periodical Literature, African Journal On-Line, and PsychInfo. The time frame for the reviewed articles ranged from May 19, 1995 to May 18, 2020. The search identified a total of 120 articles amongst which only 21 research articles met the inclusion criteria. We started our search in 1995 to exhaust a wide range of synthesis about documented changes in magnitude over the years in Africa. Boolean strategy was used to search the databases. We used a combination of Medical Subject Heading (MeSH) and free-text terms to search the databases using the keywords: postpartum depression, prevalence, magnitude, burden, combined with Africa.
Eligibility criteria: studies were considered eligible if they were published in English, carried out within the stated time-frame, focused on the magnitude of postpartum depression in Africa, used scientific methods such as surveys, case-control, trials, prevalence and surveillance studies with sound methodological standards. These studies were further considered if they were original publications and were carried out in community and healthcare facilities. For validation studies, only articles that validated the tools of assessment were included. The review excluded articles that were not available in full text, depression assessment method not well described, and the assessment tools used were not validated.
Data screening and extraction: the data screening and extraction process involved removal of duplicate articles, initial screening of the titles and abstracts based on the eligibility criteria and full-text screening of selected studies. All the articles that met our inclusion criteria were retained for data extraction using an electronic standardized data extraction template designed by the team. The data extraction template was first pilot-tested on a representative sample of articles. The characteristics of studies included the authors and year of publication, the country of study, the sample size, the type of depression assessment tool, time frame of assessment and magnitude or prevalence of depression among postpartum mothers (Table 1 and Table 2). A narrative summary of the extracted data was performed to address the research aims of the review.
Table 1.
the magnitude of postpartum depression in Africa using the EPDS as an assessment tool
| SN. | Author | Country | Sample size | Assessment tool | Time frame of assessment | Magnitude |
|---|---|---|---|---|---|---|
| 1 | Hung, 2014 [45] | South Africa | 249 | EPDS | 12 weeks | 31.7% |
| 2 | McHichi Alami et al. 2006 [46] | Morocco | 100 | EPDS | 12 weeks | 17.0% |
| 3 | Abiodun, 2006 [47] | Nigeria | 360 | EPDS | 6 weeks | 18.6% |
| 4 | Adewuya et al. 2005 [27] | Nigeria | 128 | EPDS | 6 weeks | 14.6% |
| 5 | Stellenberg, 2015 [48] | South Africa | 159 | EPDS | 6 weeks | 50.3% |
| 6 | Uwakwe, 2003 [49] | Nigeria | 225 | EPDS | 6-8 weeks | 10.7% |
| 7 | Agoub et al., 2005 [50] | Morocco | 144 | EPDS | 6 weeks | 6.9% |
| 8 | Kakyo et al.2012 [29] | Uganda | 202 | EPDS | < 12 weeks | 43% |
| 9 | Rogathi, 2017 [51] | Tanzania | 1013 | EPDS | 6 weeks | 12% |
| 10 | Chibanda, 2010 [28] | Zimbabwe | 210 | EPDS | 6 weeks | 33% |
| 11 | Chinawa, 2016 [52] | Nigeria | 214 | EPDS | 6 weeks | 22.9% |
| 12 | Khalifa, 2015 [30] | Sudan | 238 | EPDS | 12 weeks | 9.2% |
| 13 | Madeghe, 2016 [53] | Kenya | 200 | EPDS | 6 weeks | 13% |
| 14 | Ongeri, 2018 [54] | Kenya | 171 | EPDS | 6-10 weeks | 18.7% |
| 15 | Abadiga, 2019 [55] | Ethiopia | 287 | EPDS | < 12 weeks | 20.9% |
Table 2.
the magnitude of postpartum depression in Africa using other assessment tools
| SN | Author | Country | Sample size | Assessment tool | Time frame of assessment | Magnitude |
|---|---|---|---|---|---|---|
| 1 | Anokye, 2018 [56] | Ghana | 212 | PHQ-9 | 12 months | 7% |
| 2 | Baggaley, 2007[57] | Burkino Faso | 61 | K10 | 12 weeks | 44% |
| 3 | Adewuya & Afolabi, 2005 [58] | Nigeria | 480 | ZSDS | 12 weeks | 13.1% |
| 4 | Nakku, 2006 [26] | Uganda | 544 | SRQ-25 | 6 weeks | 6.1% |
| 5 | Toru, 2018 [59] | Ethiopia | 456 | PHQ-9 | 12 months | 22.9% |
| 6 | Odinka, 2019 [60] | Nigeria | 424 | HADS | 6-14 weeks | 33.3% |
Results
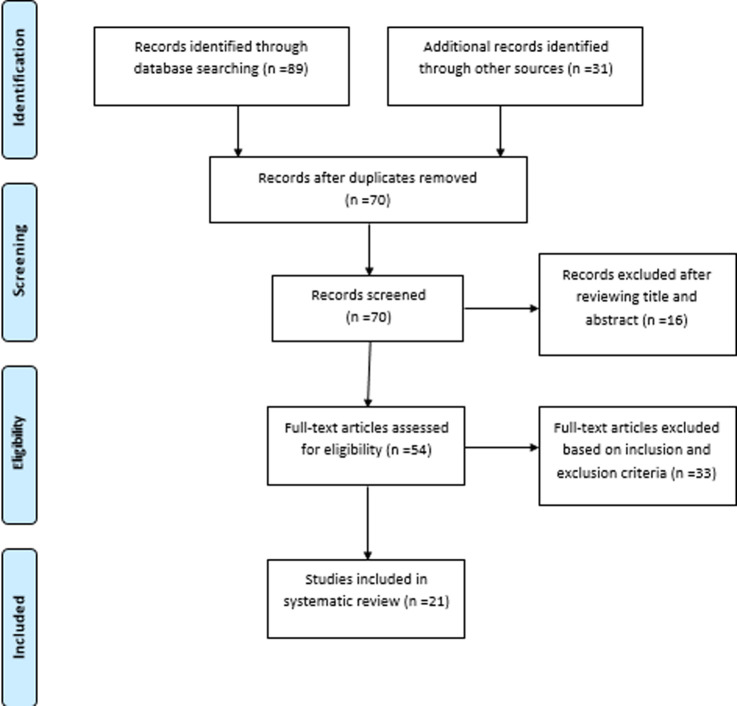
The literature search carried out on the magnitude of postpartum depression among mothers in Africa identified 21 studies. These included 15 articles on magnitude of postpartum depression among mothers in Africa using the EPDS, six articles on magnitude of postpartum depression among mothers in Africa using other PPD assessment tools and four of the articles that used the EPDS tool validated it in the African local languages and cultures as shown in Table 3. The flow diagram as shown in Figure 1 presents the inclusion and exclusion process.
Table 3.
studies validating the EPDS in local African languages for detection of postpartum depression in Africa
| SN. | Author | Country | Language | Sample size | Diagnostic instrument Diagnostic criteria | Sensitivity (%) at different EPDS cut-off points | Specificity (%) at different EPDS cut-off points | ||
|---|---|---|---|---|---|---|---|---|---|
| 9/10 | 12/13 | 9/10 | 12/13 | ||||||
| 1 | Adewuya et al.2005[27] | Nigeria | Yoruba | 876 | DSM-III | - | 100 | - | 98 |
| 2 | Chibanda et al. 2010 [28] | Zimbabwe | Shona | 210 | DSM-IV | - | 88 | - | 87 |
| 3 | Uwakwe, 2003 [49] | Nigeria | Igbo | 225 | ICD-10 | 63 | 75 | 97 | 98 |
| 4 | Agoub et al. 2005 [50] | Morocco | Arabic | 144 | MINI | - | 92 | - | 96 |
Figure 1.
flow diagram of the article selection procedure for articles published between the year 1995 and 2020 on the magnitude of postpartum depression among mothers in Africa
Fifteen articles that used EPDS in determining the magnitude of postpartum depression in nine African countries were reviewed. Table 1 shows that the postpartum depression ranged between 6.9% to 43% percent. Findings show that the magnitude of postpartum depression in South Africa (31.7-39.6%) [35,36], Morocco (6.9-14%) [37,38], Nigeria (10.7-22.9%) [28,39-41], Uganda (43%) [27], Tanzania (12%) [42], Zimbabwe (33%) [30], Sudan (9.2%) [32], Kenya (13-18.7%) [43,44] and (19.9%) participants in Ethiopia [45]. Two studies were carried out in South Africa, Morocco, Kenya and four studies qualified to be included in Nigeria. This review targeted articles that studied postpartum mothers between six and twelve weeks following child birth. Majority of these studies ten (10) assessed PPD at six weeks whereas five (5) studies detected it at less than twelve weeks postpartum. These studies identified all postpartum mothers aged 17-49 years, who visited the health facility for routine immunization of the infants and postpartum care, during the data collection period.
Table 2 shows that there was no serious variance in the magnitude as reported in table 1 where the authors used the EPDS in detecting PPD. The review covered six studies that used other tools of assessment. These included 2 Patient Health Questionnaire (PHQ-9) [46,47], 1 Kessler (K10) [48], 1 Zung´s Self Rating Depression Scale (ZSDS) [49], 1 Self Reporting Questionnaire (SRQ-25) [25], and 1 study used Hospital Anxiety and Depression Scale (HADS) [50]. Results show that postpartum depression ranged between 6.1% and 44%. Country specific prevalence reported were Ghana (7%) [46], Burkino Faso (44%) [48], Nigeria (13.1-33.3%) [49,50], Uganda (6.1%) [25] and (22.9%) participants in Ethiopia [47]. All these countries had one study reporting the prevalence apart from Nigeria that had two studies included in this review. These six studies targeted all postpartum mothers that visited the health facility at the time of data collection and had delivered up to twelve months as opposed to the studies that detected PPD using the EPDS between six and twelve weeks following child birth.
Some of the review studies translated and validated the EPDS tool to the local language. Such studies were scanty and as indicated in Table 3 include four articles reviewed from three countries namely: Nigeria in Igbo and Yoruba, Zimbabwe in Shona and Morocco in Arabic language. One (1) of the studies used EPDS cut-offs of 9/10 and 12/13 cutoff for sensitivity and specificity [40] while the other three (3) studies used cutoff point of only 12/13 for both the sensitivity and specificity [28,30,38]. All the studies reported high sensitivity and specificity rates of 75%-100% and 87%-98% of 12/13.
Discussion
Postpartum Depression has been established by several studies [2,51,52] to have significant consequences for women´s health outcomes and their quality of life. Additional impacts of PPD include maternal bonding, child health and development. The prevalence of PPD varies among countries, regions, and socioeconomic settings [2,24,51,52]. Many studies have shown the prevalence of postpartum depression around the world, but there is no universal prevalence rate that the literature indicates. The prevalence rates are higher in low and middle- income countries as compared to developed countries [1,9-11,53]. Most of these studies have used western screening tools for PPD assessment without validating them for local contexts yet PPD may be perceived in different ways across cultures. Secondly, most of the studies reviewed used self-report measures which may lead some communities in over-estimating or underestimating according to their beliefs, perceptions, and social contexts. It would be more accurate if the mothers are screened using a self-reporting questionnaire augmented with further clinical diagnostic evaluation to confirm the validity of the screening tools. Some researchers have pointed out that PPD prevalence peaks between six and twelve weeks if the EPDS is used but may increase to twelve months if other tools of assessment like the PHQ-9 are used [5]. This therefore emphasizes the need to consistently consider the uniform time frame while assessing for PPD.
In developed countries, many studies examining the prevalence of postpartum depression using the EPDS show low prevalence rates compared to low and middle-income countries, which have prevalence variations [22,54-57]. The PPD rate is estimated to range from 3.9 to 17.6 percent in five countries hence: Norway, Netherlands, Portugal, Sweden and the United States of America [12-24]. The intense attention to PPD in developed countries may have contributed to awareness and policy interventions to address PPD. This could explain the lower prevalence rate than in low and middle income countries. Secondly, the available screening tools have been developed in the context of western cultures and thus reflect the cultural perceptions and understanding in those settings. The discrepancies point to the urgency of a locally validated tool to screen for PPD. The few existing studies estimate higher prevalence of PPD in the African countries. The paucity of consistent PPD prevalence data in African countries [25,26] may be due to the in-availability of screening tools developed within the context of local cultures that reflect the African cultural perceptions and understanding. Other prevalence studies that were carried out were excluded because they were not specifically screening for PPD but were directed to high risk categories like HIV infected women, pregnant women, pregnant women with eclampsia and mothers of children with malnutrition [27,58-60].
Conclusion
In conclusion, the literature review shows that primary studies examining the magnitude of PPD are very few which means the condition is under reported. The magnitude of PPD in Africa using EPDS ranges from 6.9% to 50.3% and 6.1% to 47.7% among studies that used other tools. EPDS tool is an effective tool for assessing PPD as results showed sensitivity and specificity results ranged from 75%-100% and 75%-98% respectively in different settings. Recommendations: 1) African countries need to consider postpartum depression as a public health problem that is neglected among postpartum mothers. 2) Need to determine the actual prevalence of postpartum depression using a validated Edinburgh Postnatal Depression Scale (EDPS) against a clinical diagnosis based on a DSM-V, MINI or ICD-11 among the African population. 3) The actual burden of PPD will encourage early screening, diagnosis and treatment of postpartum depression as an integral component of maternal postpartum care in Africa.
What is known about this topic
The articles reviewed have provided great insights into what is already known about the magnitude of PPD and the existing limitations and knowledge gaps have also been identified;
Validation of screening tools into local contexts is very important in appropriately determining the actual prevalence of PPD among mothers;
The use of western developed standardized screening tools may not be appropriate for application across variable cultural groups requiring researchers to be culturally sensitive; the Edinburgh Postnatal Depression Scale is one of the most reliable and simple tools for screening PPD among mothers with a high level of acceptability.
What this study adds
The review of the literature has found that there are limited studies carried out to determine the magnitude of postpartum depression in Africa;
Available studies on the prevalence of PPD have given contradicting variable results. These differences are attributed to the different tools used, varying cutoff points, timing, and cultural settings.
Footnotes
Cite this article: Catherine Atuhaire et al. The magnitude of postpartum depression among mothers in Africa: a literature review. Pan African Medical Journal. 2020;37(89). 10.11604/pamj.2020.37.89.23572
Competing interests
The authors declare no competing interest.
Authors' contributions
Catherine Atuhaire conceived and designed the study. Catherine Atuhaire, Laura Brennaman, Godfrey Zari Rukundo and Grace Nambozi contributed to the analysis and interpretation of the data. Catherine Atuhaire, Samuel Nambile Cumber and Godfrey Zari Rukundo were involved in writing the first manuscript and all authors were involved in reviewing this manuscript. All the authors have read and agreed to the final manuscript.
References
- 1.Gelaye B, Rondon MB, Araya R, Williams MA. Epidemiology of maternal depression, risk factors, and child outcomes in low-income and middle-income countries. Lancet Psychiatry. 2016;3(10):973–982. doi: 10.1016/S2215-0366(16)30284-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Norhayati MN, Hazlina NH, Asrenee AR, Emilin WM. Magnitude and risk factors for postpartum symptoms: a literature review. Journal of Affective Disorders. 2015;175:34–52. doi: 10.1016/j.jad.2014.12.041. [DOI] [PubMed] [Google Scholar]
- 3.Fisher J, Cabral de Mello M, Patel V, Rahman A, Tran T, Holton S, et al. Prevalence and determinants of common perinatal mental disorders in women in low-and lower-middle-income countries: a systematic review. Bulletin of the World Health Organization. 2012;90(2):139G–149G. doi: 10.2471/BLT.11.091850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stewart DE Vigod S. Postpartum Depression. New England Journal of Medicine. 2016;375(22):2177–2186. doi: 10.1056/NEJMcp1607649. [DOI] [PubMed] [Google Scholar]
- 5.Khubaib Ammar Ayoub. Prevalence of postpartum depression among recently delivering mothers in Nablus District and its associated factors. Thesis for master of public health an-Najah National University. 2014. Palestine.
- 6.Henderson C, Evans-Lacko S, Thornicroft G. Mental illness stigma, help seeking, and public health programs. American Journal of Public Health. 2013;103(5):777–80. doi: 10.2105/AJPH.2012.301056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sulyman D, Ayanda K, Dattijo L,Aminu B. Postnatal depression and its associated factors among Northeastern Nigerian women. Annals of Tropical Medicine and Public Health. 2016;9(3):184–190. [Google Scholar]
- 8.Segre LS, O'Hara MW, Arndt S, Stuart S. The prevalence of postpartum depression: the relative significance of three social status indices. Social Psychiatry and Psychiatric Epidemiology. 2007;42(4):316–21. doi: 10.1007/s00127-007-0168-1. [DOI] [PubMed] [Google Scholar]
- 9.Ferda Ozbaşaran, Ayden Coban, Mert Kucuk. Prevalence and risk factors concerning postpartum depression among women within early postnatal periods in Turkey. Archives of Gynecology and Obstetrics. 2011;283(3):483–90. doi: 10.1007/s00404-010-1402-8. [DOI] [PubMed] [Google Scholar]
- 10.Tachibana Y, Koizumi T, Takehara K, Kakee N, Tsujii H, Mori R, et al. Antenatal risk factors of postpartum depression at 20 weeks gestation in a Japanese sample: psychosocial perspectives from a cohort study in Tokyo. PLoS One. 2015;10(12):e0142410. doi: 10.1371/journal.pone.0142410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Falah-Hassani K, Shiri R,Dennis CL. Prevalence and risk factors for comorbid postpartum depressive symptomatology and anxiety. Journal of Affective Disorders. 2016;198:142–7. doi: 10.1016/j.jad.2016.03.010. [DOI] [PubMed] [Google Scholar]
- 12.Glavin K, Smith L, Sørum R. Prevalence of postpartum depression in two municipalities in Norway. Scand J Caring Sci. 2009;23(4):705–10. doi: 10.1111/j.1471-6712.2008.00667.x. [DOI] [PubMed] [Google Scholar]
- 13.Blom EA, Jansen PW, Verhulst FC, Hofman A, Raat H, Jaddoe VW, et al. Perinatal complications increase the risk of postpartum depression. The Generation R Study. BJOG: an international journal of obstetrics and gynaecology. 2010;117(11):1390–8. doi: 10.1111/j.1471-0528.2010.02660.x. [DOI] [PubMed] [Google Scholar]
- 14.Van Son M, Verkerk G, van der Hart O, Komproe I, Pop V. Prenatal depression, mode of delivery and perinatal dissociation as predictors of postpartum posttraumatic stress: an empirical study. Clinical Psychology & Psychotherapy. 2005;12(4):297–312. [Google Scholar]
- 15.Pereira AT, Bos S, Marques M, Maia BR, Soares MJ, Valente J, et al. The Portuguese version of the postpartum depression screening scale. J Psychosom Obstet Gynaecol. 2010;31(2):90–100. doi: 10.3109/0167482X.2010.481736. [DOI] [PubMed] [Google Scholar]
- 16.Figueiredo B, Pacheco A, Costa R. Depression during pregnancy and the postpartum period in adolescent and adult Portuguese mothers. Arch Womens Ment Health. 2007;10(3):103–9. doi: 10.1007/s00737-007-0178-8. [DOI] [PubMed] [Google Scholar]
- 17.Berta Maia, Ana Pereira T, Mariana Marques, Sandra Bos, Maria Soares J, José Valente, et al. The role of perfectionism in postpartum depression and symptomatology. Archives of Womens Mental Health. 2012;15(6):459–68. doi: 10.1007/s00737-012-0310-2. [DOI] [PubMed] [Google Scholar]
- 18.Wickberg B, Hwang CP. Screening for postnatal depression in a population-based Swedish sample. Acta Psychiatr Scand. 1997;95(1):62–6. doi: 10.1111/j.1600-0447.1997.tb00375.x. [DOI] [PubMed] [Google Scholar]
- 19.Sara Sylvén, Fotios Papadopoulos C, Vassilios Mpazakidis, Lisa Ekselius, Inger Sundström-Poromaa, Alkistis Skalkidou. Newborn gender as a predictor of postpartum mood disturbances in a sample of Swedish women. Arch Womens Ment Health. 2011;14(3):195–201. doi: 10.1007/s00737-011-0211-9. [DOI] [PubMed] [Google Scholar]
- 20.Rubertsson C, Waldenström U, Wickberg B, Rådestad I, Hildingsson I. Depressive mood in early pregnancy and postpartum: prevalence and women at risk in a national Swedish sample. Journal of Reproductive and Infant Psychology. 2005;23(2):155–166. [Google Scholar]
- 21.Drake E, Howard E, Kinsey E. Online screening and referral for postpartum depression: an exploratory study. Community Mental Health Journal. 2014;50(3):305–11. doi: 10.1007/s10597-012-9573-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Howell EA, Bodnar-Deren S, Balbierz A, Loudon H, Mora PA, Zlotnick C, et al. An intervention to reduce postpartum depressive symptoms: a randomized controlled trial. Archives of women's mental health. 2014;17(1):57–63. doi: 10.1007/s00737-013-0381-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Moses-Kolko EL, Roth EK. Antepartum and postpartum depression: healthy mom, healthy baby. J Am Med Womens Assoc (1972) 2004;59(3):181–91. [PubMed] [Google Scholar]
- 24.Halbreich U Karkun S. Cross-cultural and social diversity of prevalence of postpartum depression and depressive symptoms. Journal of Affective Disorders. 2006;91(2-3):97–111. doi: 10.1016/j.jad.2005.12.051. [DOI] [PubMed] [Google Scholar]
- 25.Nakku JEM, Nakasi G, Mirembe F. Postpartum major depression at six weeks in primary health care: prevalence and associated factors. African Health Sciences. 2006;6(4):207–214. doi: 10.5555/afhs.2006.6.4.207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ferrari AJ, Charlson FJ, Norman RE, Patten SB, Freedman G, Murray CJ, et al. Burden of depressive disorders by country, sex, age, and year: findings from the global burden of disease study 2010. PLoS medicine. 2013;10(11):e1001547. doi: 10.1371/journal.pmed.1001547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kakyo TA, Muliira JK, Mbalinda SN, Kizza IB, Muliira RS. Factors associated with depressive symptoms among postpartum mothers in a rural district in Uganda. Midwifery. 2012;28(3):374–9. doi: 10.1016/j.midw.2011.05.001. [DOI] [PubMed] [Google Scholar]
- 28.Adewuya AO, Eegunranti AB, Lawal AM. Prevalence of postnatal depression in Western Nigerian women: a controlled study. International Journal of Psychiatry in Clinical Practice. 2005;9(1):60–4. doi: 10.1080/13651500510018211. [DOI] [PubMed] [Google Scholar]
- 29.Owoeye AO, Aina OF, Morakinyo O. Risk factors of postpartum depression and EPDS scores in a group of Nigerian women. Tropical Doctor. 2006;36(2):100–3. doi: 10.1258/004947506776593341. [DOI] [PubMed] [Google Scholar]
- 30.Chibanda D, Mangezi W, Tshimanga M, Woelk G, Rusakaniko P, Stranix-Chibanda L, et al. Validation of the Edinburgh postnatal depression scale among women in a high HIV prevalence area in urban Zimbabwe. Archives of Womens Mental Health. 2010;13(3):201–6. doi: 10.1007/s00737-009-0073-6. [DOI] [PubMed] [Google Scholar]
- 31.Weobong B, Ten Asbroek AH, Soremekun S, Danso S, Owusu-Agyei S, Prince M, et al. Determinants of postnatal depression in rural ghana: findings from the don population based cohort study. Depression and Anxiety. 2015;32(2):108–19. doi: 10.1002/da.22218. [DOI] [PubMed] [Google Scholar]
- 32.Khalifa DS, Glavin K, Bjertness E, Lien L. Determinants of postnatal depression in Sudanese women at 3 months postpartum: a cross-sectional study. BMJ Open. 2016;6(3):e009443. doi: 10.1136/bmjopen-2015-009443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Villegas L, McKay K, Dennis CL, Ross LE. Postpartum depression among rural women from developed and developing countries: a systematic review. Journal of Rural Health. 2011;27(3):278–88. doi: 10.1111/j.1748-0361.2010.00339.x. [DOI] [PubMed] [Google Scholar]
- 34.Dennis CL McQueen K. The relationship between infant-feeding outcomes and postpartum depression: a qualitative systematic review. Pediatrics. 2009;123(4):e736–51. doi: 10.1542/peds.2008-1629. [DOI] [PubMed] [Google Scholar]
- 35.Hung KJ, Tomlinson M, le Roux IM, Dewing S, Chopra M,Tsai AC. Community-based prenatal screening for postpartum depression in a South African township. Int J Gynaecol Obstet. 2014;126(1):74–7. doi: 10.1016/j.ijgo.2014.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ethelwynn Stellenberg L, Johanna Abrahams M. Prevalence of and factors influencing postnatal depression in a rural community in South Africa. Afr J Prim Health Care Fam Med. 2015;7(1):874. doi: 10.4102/phcfm.v7i1.874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McHichi Alami K, Kadri N, Berrada S. Prevalence and psychosocial correlates of depressed mood during pregnancy and after childbirth in a Moroccan sample. Archives of Women's Mental Health. 2006;9(6):343–346. doi: 10.1007/s00737-006-0154-8. [DOI] [PubMed] [Google Scholar]
- 38.Agoub M, Moussaoui D, Battas O. Prevalence of postpartum depression in a Moroccan sample. Arch Womens Ment Health. 2005;8(1):37–43. doi: 10.1007/s00737-005-0069-9. [DOI] [PubMed] [Google Scholar]
- 39.Abiodun OA. Postnatal depression in primary care populations in Nigeria. Gen Hosp Psychiatry. 2006;28(2):133–6. doi: 10.1016/j.genhosppsych.2005.11.002. [DOI] [PubMed] [Google Scholar]
- 40.Uwakwe R, Okonkwo JE. Affective (depressive) morbidity in puerperal Nigerian women: validation of the Edinburgh Postnatal Depression Scale. Acta Psychiatr Scand. 2003;107(4):251–9. doi: 10.1034/j.1600-0447.2003.02477.x. [DOI] [PubMed] [Google Scholar]
- 41.Chinawa JM, Odetunde OI, Ndu IK, Ezugwu EC, Aniwada EC, Chinawa AT, et al. Postpartum depression among mothers as seen in hospitals in Enugu, South-East Nigeria: an undocumented issue. Pan African Medical Journal. 2016;23(1):180. [Google Scholar]
- 42.Rogathi JJ, Manongi R, Mushi D, Rasch V, Sigalla GN, Gammeltoft T, et al. Postpartum depression among women who have experienced intimate partner violence: A prospective cohort study at Moshi, Tanzania. J Affect Disord. 2017;218:238–245. doi: 10.1016/j.jad.2017.04.063. [DOI] [PubMed] [Google Scholar]
- 43.Madeghe BA, Kimani VN, Vander Stoep A, Nicodimos S, Kumar M. Postpartum depression and infant feeding practices in a low income urban settlement in Nairobi-Kenya. BMC Res Notes. 2016;9(1):506. doi: 10.1186/s13104-016-2307-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ongeri L, Wanga V, Otieno P, Mbui J, Juma E, Stoep AV, et al. Demographic, psychosocial and clinical factors associated with postpartum depression in Kenyan women. BMC Psychiatry. 2018;18(1):318. doi: 10.1186/s12888-018-1904-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Abadiga M. Magnitude and associated factors of postpartum depression among women in Nekemte town, East Wollega zone, west Ethiopia 2019 a community-based study. PLoS One. 2019;14(11):e0224792. doi: 10.1371/journal.pone.0224792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Anokye R, Acheampong E, Budu-Ainooson A, Obeng EI, Akwasi AG. Prevalence of postpartum depression and interventions utilized for its management. Ann Gen Psychiatry. 2018;17:18. doi: 10.1186/s12991-018-0188-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Toru T, Chemir F, Anand S. Magnitude of postpartum depression and associated factors among women in Mizan Aman town, Bench Maji zone, Southwest Ethiopia. BMC Pregnancy Childbirth. 2018;18(1):442. doi: 10.1186/s12884-018-2072-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Baggaley RF, Ganaba R, Filippi V, Kere M, Marshall T, Sombié I, et al. Detecting depression after pregnancy: the validity of the K10 and K6 in Burkina Faso. Trop Med Int Health. 2007;12(10):1225–9. doi: 10.1111/j.1365-3156.2007.01906.x. [DOI] [PubMed] [Google Scholar]
- 49.Adewuya AO, Afolabi OT. The course of anxiety and depressive symptoms in Nigerian postpartum women. Arch Womens Ment Health. 2005;8(4):257–9. doi: 10.1007/s00737-005-0089-5. [DOI] [PubMed] [Google Scholar]
- 50.Odinka P, Odinka J, Ezeme M, Ndukuba A, Amadi K, Muomah R, et al. Socio-demographic correlates of postpartum psychological distress among apparently healthy mothers in two tertiary hospitals in Enugu, South-East Nigeria. Afr Health Sci. 2019;19(3):2515–2525. doi: 10.4314/ahs.v19i3.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Gulamani SS, Shaikh K, Chagani J. Postpartum depression in Pakistan: a neglected issue. Nursing for Womens Health. 2013;17(2):147–52. doi: 10.1111/1751-486X.12024. [DOI] [PubMed] [Google Scholar]
- 52.Davies T, Schneider M, Nyatsanza M, Lund C. "The sun has set even though it is morning": experiences and explanations of perinatal depression in an urban township, Cape Town. Transcultural Psychiatry. 2016;53(3):286–312. doi: 10.1177/1363461516632389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Surkan PJ, Ettinger AK, Hock RS, Ahmed S, Strobino DM, Minkovitz CS. Early maternal depressive symptoms and child growth trajectories: a longitudinal analysis of a nationally representative US birth cohort. BMC Pediatrics. 2014;14:185. doi: 10.1186/1471-2431-14-185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Edhborg M, Nasreen HE, Kabir ZN. Impact of postpartum depressive and anxiety symptoms on mothers' emotional tie to their infants 2-3 months postpartum: a population-based study from rural Bangladesh. Archives of Womens Mental Health. 2011;14(4):307–16. doi: 10.1007/s00737-011-0221-7. [DOI] [PubMed] [Google Scholar]
- 55.Bottino MN, Nadanovsky P, Moraes CL, Reichenheim ME, Lobato G. Reappraising the relationship between maternal age and postpartum depression according to the evolutionary theory: empirical evidence from a survey in primary health services. Journal of Affective Disorders. 2012;142(1-3):219–24. doi: 10.1016/j.jad.2012.04.030. [DOI] [PubMed] [Google Scholar]
- 56.Lobato G, Moraes CL, Dias AS, Reichenheim ME. Postpartum depression according to time frames and sub-groups: a survey in primary health care settings in Rio de Janeiro, Brazil. Archives of Womens Mental Health. 2011;14(3):187–93. doi: 10.1007/s00737-011-0206-6. [DOI] [PubMed] [Google Scholar]
- 57.Yurdagül Yağmur, Neşe Ulukoca. Social support and postpartum depression in low-socioeconomic level postpartum women in Eastern Turkey. International Journal of Public Health. 2010;55(6):543–9. doi: 10.1007/s00038-010-0182-z. [DOI] [PubMed] [Google Scholar]
- 58.Kaida A, Matthews LT, Ashaba S, Tsai AC, Kanters S, Robak M, et al. Depression during pregnancy and the postpartum among HIV-infected women on antiretroviral therapy in Uganda. Journal of Acquired Immune Deficiency Syndromes. 2014;67(Suppl 4 Suppl 4):S179–87. doi: 10.1097/QAI.0000000000000370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kinyanda E, Woodburn P, Tugumisirize J, Kagugube J, Ndyanabangi S, Patel V. Poverty, life events and the risk for depression in Uganda. Social psychiatry and psychiatric epidemiology. 2011;46(1):35–44. doi: 10.1007/s00127-009-0164-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ashaba S, Rukundo GZ, Beinempaka F, Ntaro M, LeBlanc JC. Maternal depression and malnutrition in children in southwest Uganda: a case control study. BMC Public Health. 2015;15:1303. doi: 10.1186/s12889-015-2644-y. [DOI] [PMC free article] [PubMed] [Google Scholar]