Abstract
Teenage childbearing (ages 15–19) represents a significant public health issue that can generate considerable deleterious, multigenerational consequences for teen-childbearing mothers and their offspring. However, few studies have examined the potential mediating mechanisms that may explain if and how teen childbearing is associated with the development of offspring psychopathology. The current study used a developmental model to test the mediating role of chronic child maltreatment in the relationship between teen childbearing and offspring internalizing symptoms in childhood and emerging adulthood. Participants were 384 individuals from socioeconomically-disadvantaged, ethnically-diverse backgrounds, assessed across two longitudinal waves of data (i.e., ages 10–12 and 18–20). The sample included maltreated and nonmalreated children all of whom were comparable on family income. Structural equation modeling (SEM) was conducted to test direct and indirect pathways from teen childbearing to offspring psychopathology. A multigenerational developmental cascade was found such that individuals born to mothers who began their childbearing in adolescence were more likely to experience chronic maltreatment during childhood, which in turn predicted greater internalizing symptoms throughout childhood and emerging adulthood. Using a developmental psychopathology framework, results are discussed with regard to implications for prevention and early intervention.
Keywords: teen childbearing, teen pregnancy, child maltreatment, offspring psychopathology, internalizing
Introduction
Teenage childbearing (15–19-years-old) represents a significant public health issue with substantial societal burden and deleterious, multigenerational consequences for the teenage mothers and their offspring (Coyne & D’Onofrio, 2012). The considerable toll of teen childbearing signals a need for additional research on both the immediate and long-term outcomes of this phenomenon. Despite scientific evidence that teen childbearing negatively influences offspring outcomes (Coyne & D’Onofrio, 2012; D’Onofrio et al., 2009; Fergusson & Woodward, 1999; Mollborn & Dennis, 2012; Mollborn, 2017), the empirical literature has historically focused on the effect of teen childbearing on the adolescent mothers themselves (see Coyne & D’Onofrio, 2012 for a review). For more clarity, a greater understanding of the proximal and distal factors that contribute to risk for teen pregnancy (e.g., socioeconomic disadvantage or psychopathology), as well as how teen childbearing influences the adolescent trajectories of the mother (e.g., low educational attainment or depression), are essential. However, in comparison, the extant literature has given less attention to investigating the long-term sequelae of teen childbearing on the offspring, an equally vital research area and the primary purpose of the current study.
Offspring Outcomes
The offspring of teen mothers experience a wide range of negative outcomes starting in the neonatal period and extending into adulthood (Fergusson & Woodward, 1999; Mollborn & Dennis, 2012). These outcomes encompass challenges in offspring cognition (Khatun et al., 2017), academic success (Dahinten et al., 2007; Hardy et al., 2006), interpersonal interactions (Pogarsky et al., 2006), and general life outcomes (Mok et al., 2017; Pogarsky et al., 2006). Although a range of negative academic, sociological, and economic outcomes have been identified for the offspring of teen mothers (see Coyne & D’Onofrio, 2012 for a review), the extant literature examining offspring psychopathology as a resultant adverse consequence of teen childbearing is more limited.
To date, studies on offspring psychopathology have primarily accentuated offspring externalizing psychopathology. Indeed, compared to the offspring of non-teen parents, the offspring of teen-childbearing parents demonstrate more externalizing symptoms (see Coyne & D’Onofrio, 2012 for review) including hyperkinetic disorders (e.g., Chang et al., 2014), aggression (e.g., Pogarsky et al., 2006), violent offending (Jaffee et al., 2001), criminal offending (Mok et al., 2017), and elevated levels of drug use (e.g., Coyne et al., 2013). Moreover, research suggests that these effects on offspring persist after adjusting for confounding factors associated with teen pregnancy risk, such as poverty or family-level factors (Coyne & D’Onofrio, 2012; D’Onofrio et al., 2009).
Compared to the preponderance of findings on externalizing symptoms, there is only minimal evidence for the effect of teen childbearing on offspring internalizing symptoms. Shaw et al. (2006) revealed that the offspring of teen mothers have more internalizing symptoms at 14-years-old after accounting for maternal internalizing symptoms and family characteristics (Shaw et al., 2006). Relatedly, Harden et al. (2007) employed a quasi-experimental design to control for potential confounding variables and found that adolescent motherhood significantly predicted offspring internalizing symptoms (i.e., depressive episode criteria). Further, teen childbearing is associated with increased suicide risk in offspring (Mok et al., 2017). Finally, research by Fergusson and Woodward (1999) showed that the offspring of teen mothers had approximately five times the risk of developing anxiety and depressive disorders at 18 years of age.
Mechanisms
Though there is evidence that teen childbearing is associated with offspring psychopathology, teen childbearing does not ineluctably lead to offspring mental health problems and when it does, it is still unclear exactly why or how teen childbearing may influence developmental pathways to offspring psychopathology (Mollborn, 2017; Mollborn & Dennis, 2012). Consequently, there is an unequivocal need for developmental psychopathology-guided research that further examines the putative risk for the offspring of teen childbearers to develop psychopathology by revealing possible explanatory mechanisms linking the two (Coyne & D’Onofrio, 2012). Thus, although there is existing confirmatory research evidence for teen childbearing as a risk factor for offspring psychopathology, this simply represents a starting point for further developmental psychopathology analysis to reveal mechanisms. Moreover, identifying modifiable mediators can inform and improve preventive interventions by detailing specific intervention targets.
A variety of mechanisms may plausibly mediate the association between teen childbearing and offspring psychopathology, as teen mothers are more likely to experience subsequent social disadvantage, to have lower educational attainment, to be depressed, and to be harsh, inconsistent, and unresponsive parents (Coyne & D’Onofrio, 2012; Lee & Gutterman, 2010; Mollborn, 2017), all of which can lead to psychopathology in the offspring. Though some studies have examined parenting quality or compromised parenting as a mediating mechanism in the association between teen childbearing and offspring psychopathology (Dahinten et al., 2007; Fergusson & Woodward, 1999; Jaffee et al., 2001; Mollborn & Dennis, 2012; Pogarsky et al. 2006), there is limited research on the explanatory role of the most severe form of parenting dysfunction—child maltreatment (Cicchetti, 2011). In the one study examining maltreatment as a mediator, Fergusson and Woodward (1999) found that childhood sexual abuse mediated the relationship between teen childbearing and offspring internalizing psychopathology, but the study relied on adult retrospective reports of only one type of abuse (i.e., sexual abuse) and retrospective reports of maltreatment are known to have methodological limitations (Baldwin et al., 2019). The general omission of child maltreatment as an explanatory factor is noteworthy, as research suggests that the children of teen mothers are at considerable risk for child maltreatment (MacKenzie, Nicklas, Brooks-Gunn, & Waldfogel, 2011; Putnam-Hornstein, & Needell, 2011) and maltreatment experiences are strongly associated with subsequent psychopathology (Cicchetti, 2011; Jaffee, 2017).
There are several reasons why adolescent mothers may be at risk of maltreating their children, including maternal history of being maltreated (Bartlett & Easterbrooks, 2012), maternal psychopathology (Coelho et al., 2013), developmental immaturity (Deater-Deckard, Wang, Chen, & Bell, 2012), lack of parental support, and a confluence of stressors and socioeconomic disadvantages that follow teen childbearing (see Coyne & D’Onofrio, 2012). Additionally, rather than one single factor, it may be due to a constellation of risk, whereby the mounting socioeconomic hardships that follow teen childbearing converge with other teen parenting-stressors (e.g., parenting stress, relationship strain, and depression) to impart an engulfing strain on these mothers that render their offspring more vulnerable to maltreatment victimization, whether perpetrated by the parent or others (Easterbrooks et al., 2011).
Categories of Teen Childbearing
Most previous studies examining associations between teen childbearing and offspring psychopathology have typically dichotomized the variable into two categories: 1) mothers who gave birth to the study target offspring when they were adolescents; and 2) all other mothers. However, this dichotomization fails to account for mothers who began childbearing in their adolescence, even if they birthed the study target in adulthood. Therefore, this study aims to address a limitation by examining teen childbearing as a three-category variable: Teen Parent (if the mother was less than 20-years-old when she gave birth to the study target offspring); Ever-Teen Parent (the mother of the study target had previously given birth to a child as a teenager, but was at least 20-years-old when she gave birth to the study target offspring); and Never-Teen Parent (the mother was at least 20-years-old when she gave birth to her first child and/or the study target offspring). Other studies have operationalized teen childbearing in a similar manner (e.g., Harden et al., 2007; Mollborn & Dennis, 2012; Pogarsky et al., 2006). This three-category distinction is important, as women who parent a specific child as teenagers (Teen Parents) and/or begin childbearing in their teen years (Ever-Teen Parents) may be uniquely different from women who begin childbearing in adulthood (Never-Teen Parents).
The contrast of two types of teen parents offers a valuable comparison. For example, if the target offspring of Teen Parents have significantly higher rates of child maltreatment and internalizing psychopathology than the offspring of Ever-Teen Parents and Never-Teen Parents, then the results might suggest that the negative effects of teen childbearing may be due to age-related, developmental, or biological factors that are dependent on the specific developmental timing of the target child’s birth (Mollborn & Dennis, 2012). Thus, one might hypothesize that the effects of teen childbearing on child maltreatment risk and offspring psychopathology are transitory and would expire (Pogarsky et al., 2003) if the mother delayed childbearing until she was at least 20-years-old. Alternatively, if the offspring of both Teen Parents and Ever-Teen Parents have similar risk for child maltreatment and psychopathology, then it suggests that teen childbearing at any point in the mother’s life may impart risk on all subsequent children and that teen childbearing at any time “reflects or initiates enduring circumstances that harm the entire family’s subsequent development” (Pogarsky et al., 2003, p. 1250).
Present Study
The aim of the present study was to investigate the mediating role of chronic child maltreatment in the relationship between teen childbearing and offspring internalizing symptoms in childhood (ages 10–12) and emerging adulthood (ages 18–20) within a socioeconomically-disadvantaged, ethnically-diverse sample of children. In doing so, the study addresses multiple gaps in the literature.
First, it adds to the existing, but limited, findings regarding the association between teen childbearing and offspring internalizing symptoms. Moreover, it examines this relationship across developmental time points spanning the transition from childhood to adulthood. To date, only a few studies have observed this relationship beyond the childhood years (Fergusson & Woodward, 1999; Mok et al., 2017) and a lifespan view may be particularly important because the negative effects of teen childbearing on offspring development may worsen over time (Brooks-Gunn & Furstenberg, 1986; Jaffee et al., 2001). Additionally, some psychopathologies (e.g., depression) may not fully manifest until late adolescence or early adulthood and therefore require a longitudinal investigation (Kingsbury et al., 2016). Further, a longitudinal design allows for examination of potential continuities and discontinuities in offspring internalizing symptoms across development (Cicchetti, 2011).
Secondly, the current study addresses an empirical gap by providing a more differentiated perspective on the association between teen childbearing and offspring internalizing symptoms by illuminating the presence of an under-examined intervening variable (i.e., child maltreatment) that may signify a mechanistic pathway. And, notably, the study measures child maltreatment with documented records, rather than retrospective reports.
Thirdly, this study addresses the role of economic disadvantage in the relationship between teen childbearing, child maltreatment, and offspring internalizing symptoms by examining this relationship within an economically-disadvantaged sample of mothers and children. Unmeasured social disadvantage and poverty have been indicated as potential confounding factors in the association between teen childbearing and offspring outcomes (e.g., D’Onofrio et al. 2009; Mollborn et al., 2014) and the majority of studies that have previously examined the meditational role of parenting behavior have also found that poverty accounts for a partial effect in the association between teen childbearing and offspring symptoms (Dahinten et al., 2007; Fergusson & Woodward, 1999; Mollborn & Dennis, 2012). Thus, the current study contributes to the existing literature because it was methodologically designed to account for the potential confounding effect of poverty on teen childbearing, child maltreatment risk, and internalizing symptoms, respectively.
Methods
Participants
The participants for the current investigation included 384 economically-disadvantaged individuals who were assessed across two longitudinal waves of data collection (childhood ages 10–12 and young adult ages 18–21). Wave 1 of data collection included 680 maltreated (n= 360) and non-maltreated (n =320) children who participated in a research summer camp (see Cicchetti & Manly, 1990 for a detailed description of the research camp setting) as 10–12-year-olds (M = 11.28, SD = .97). At Wave 2, 427 of the original participants were followed up at 18–21-years old (M = 20.17, SD= 1.35) and asked to complete a series of individual interviews and research assessments. Due to missing data on the predictor variable (i.e., teen childbearing status), 384 maltreated (n= 201) and nonmaltreated (n=183) participants were included in the final analyses. The participants were racially and ethnically diverse (71.6% African-American, 11.8% Caucasian, 12.6% Hispanic, 4.0% biracial/other race) and were comparable in terms of gender (50.1% male). The families of participants were primarily headed by a single parent (68.7%) and had histories of receiving public assistance (96.1%).
Recruitment
Participants were initially recruited based on documented records of child abuse and neglect reports through the Department of Human Services (DHS). A DHS liaison reviewed Child Protective Services records and identified children who had been maltreated. Children in foster care were not recruited. A random sample of eligible families was selected for recruitment. The DHS liaison then contacted eligible families and explained the study to parents who were free to either agree to participate or to decline to have their information released to project staff. Interested participants provided project staff with informed consent for both their child’s participation in the summer camp program and for full access to any DHS records pertaining to the family.
A comprehensive and extensive review of DHS records was performed to code for maltreatment information using the Maltreatment Classification System (MCS; Barnett, Manly, & Cicchetti, 1993), a reliable and valid nosological maltreatment classification system (Bolger & Patterson, 2001; Manly, 2005; Manly, Kim, Rogosch, & Cicchetti, 2001) with operationalized determinations of child maltreatment parameters. The MCS criteria yield distinct information on multiple subtypes of child maltreatment (i.e., emotional maltreatment, neglect, physical abuse, and sexual abuse).
Maltreated children are predominantly from low-income families (Fourth National Incidence Study of Child Abuse and Neglect; Sedlak et al, 2010). Therefore, the DHS liaison identified demographically comparable families (i.e., families receiving Temporary Assistance for Needy Families) without histories of CPS involvement for recruitment for the non-maltreated comparison group. As with the maltreated group, the DHS liaison contacted a random sample of eligible non-maltreated participants to discuss study details. If participants expressed interest, their information was passed to project staff who then obtained informed consent from participants to search family DHS records and further verify the absence of maltreatment information using the MCS. Further, trained research staff completed the Maternal Child Maltreatment Interview (Cicchetti, Toth, & Manly, 2003) with all mothers to confirm the lack of maltreatment. If any conflicting information was provided that suggested the non-maltreated participants may have experienced maltreatment, they were excluded from the comparison group.
Procedures
During Wave 1 of data collection, child participants attended a weeklong, full-day summer camp where they engaged in both traditional recreational camp activities and research assessments (see Cicchetti & Manly, 1990 for a full description of research camp procedures). At camp, participants were assigned to groups of eight (four non-maltreated and four maltreated) same-age and same-sex peers. Each individual group was directed by three trained camp counselors who were unaware of participant maltreatment status and study hypotheses. The trained research staff (i.e., camp counselors) closely interacted with the participants in their respective groups for 35 hours in the weeklong camp and then rated the children on a number of assessments based on their observations, including measures on psychopathology symptoms. Camp counselors would repeat this process throughout six consecutive weeks, with new participants each week. In addition, children provided assent to participate in several individual research sessions in which they completed research assessments administered by trained research assistants.
At Wave 2, at age 18–20, former camp participants were re-recruited for a follow-up study and completed a set of individual, private, center-based research sessions. Research sessions were conducted by trained research assistants who were unaware of the participants’ maltreatment status and study hypotheses. The research assistants administered an extensive battery of assessments, including self-report measures on psychopathology symptoms and diagnostic clinical interviews.
Measures
Child maltreatment
Child maltreatment was operationalized with the Maltreatment Classification System (MCS; Barnett et al., 1993) during Wave 1. The MCS is a multidimensional classification system that is applied to official, documented CPS records. This objective measure was developed to assess child maltreatment independently from parent-report and potential bias in reporting (Manly, 2005). The MCS is a reliable and validated measure of maltreatment (Bolger & Patterson, 2001; Manly, 2005; Manly, et al., 2001). Specifically, the MCS goes beyond the CPS narratives and labels to systematically code dimensions of maltreatment including subtypes experienced, severity, developmental timing, and chronicity of maltreatment (Manly, 2005).
Based on the MCS coding system, maltreatment may occur in any or all of the following developmental periods: infancy, toddlerhood, preschool, early school age, and later school age (Manly, 2005). The number of developmental periods a child has experienced is utilized as an index of maltreatment chronicity (Manly, 2005). In this study, child maltreatment was examined as a continuous variable that indicates the number of developmental periods when maltreatment occurred. The number of developmental periods variable was coded on a scale of 0 (no maltreatment) to 5 (maltreatment in all five developmental periods). Among the maltreated children (N = 201), 55.2% experienced maltreatment in one developmental period, 23.9% in experienced maltreatment in two developmental periods, 13.9% experienced maltreatment in three developmental periods, 5.5% experienced maltreatment in four developmental periods, and 1.5% experienced maltreatment in five developmental periods. The mean score for number of developmental epochs among maltreated children is M = 1.74 (SD = 1.00).
To further characterize the maltreatment in this sample, the following indicates the percentage of each subtype of maltreatment experienced by those who had been maltreated: 81.6% neglect, 54.2% emotional maltreatment, 30.8% physical abuse, and 9.5% sexual abuse. Among the maltreated children, 42.8% experienced one form of maltreatment, 40.3% experienced two forms of maltreatment, 14.9% experienced three forms of maltreatment, and 2% experienced four forms of maltreatment. Thus, the majority of maltreated children experienced multiple subtypes Additionally, the number of maltreatment subtypes experienced was highly correlated with the number of developmental periods in which maltreatment occurred (r = .80, p < .001).
Teen childbearing
The mother’s age at the birth of her child(ren) was determined based on information obtained from Department of Human Services records and substantiated via maternal self report. Specifically, the mother’s age at birth was calculated by subtracting each child’s date of birth (DOB) from her DOB. Teen childbearing was then coded into a trichotomous categorical variable: Teen Parent (the mother was < 20-years-old when she gave birth to the study target offspring); Ever-Teen Parent (the mother of the study target had previously given birth to a child as a teenager, but was > 20-years-old when she gave birth to the study target offspring); and Never-Teen Parent (the mother was > 20-years-old when she gave birth to her first child and/or the study target offspring). We elected to map onto the classification of teen childbearing (i.e., < 20yrs) defined by the Centers for Disease Control and Prevention (CDC, 2019). Our ultimate aim is for the findings of this study to translate to actionable prevention efforts and early intervention programs designed to provide young mothers with the supports to help them recognize their inherent strengths and have resilient outcomes for their families.
Child internalizing symptoms (Wave 1)
Child Depression Inventory (CDI; Kovacs, 1982; 2004)
The CDI was utilized to assess self-reported child depressive symptoms at the first wave. The CDI is a 27-item questionnaire designed to assess depressive symptoms in school-aged children. Children are asked to respond to a series of items (e.g., feelings of worthlessness) by selecting the response that best describes their feelings within the past two weeks. The CDI is a widely-used measure with strong psychometric properties (Kovacs, 2004). The current study relied on a summary score of the 27 items as an indicator of internalizing pathology. A total sum score equal to or greater than 19 indicates clinical-level depressive symptoms (Kovacs, 2004). In the current sample, 7.8% of children had sum scores that met the clinical threshold.
Revised Children’s Manifest Anxiety Scale (RCMAS; Reynolds & Richmond, 1978)
The RCMAS is a widely used 37-item self-report instrument designed to assess manifest anxiety reactions in children and adolescents. Participants were asked to respond to each of the 28 anxiety items (e.g., “I worry about what other people think about me”) and 9 Lie items (e.g., “I am always kind”) by indicating if the statement was true (yes = 1) or not true (no = 0). The RCMAS has extensive evidence indicating its reliability and validity properties (Reynolds & Richmond, 1985). The measure produces a total anxiety score and three subscale scores (worry-oversensitivity, physiological arousal, and concentration). The present study used the total anxiety score as an indicator of childhood internalizing symptomology. In the current sample, 9.8% of children had sum scores that met the clinical threshold.
Child Behavior Checklist Teacher Report Form (TRF; Achenbach, 1991)
Children’s internalizing symptomatology was assessed by camp counselors using the TRF at Wave 1. Camp counselors relied on weeklong observations of the children (35 hours) to provide an assessment of behavioral disturbance from a non-related adult. The TRF is a well-validated and reliable measure (Achenbach, 1991; Achenbach, Dimenci, & Rescorla, 2003) that assesses internalizing and externalizing symptom domains across 118 items. The TRF can yield validated syndrome subscales and DSM-oriented subscales (Achenbach, 1991; Achenbach et al., 2003). Children were independently rated by two separate camp counselors and the counselor scores were averaged to create one T score for each symptom dimension (i.e., internalizing) and counselors had an average interrater reliability of (k) 0.68. The internalizing subscale T-score was used as an other-informant indicator for childhood internalizing pathology. In the current sample, 8% of children had sum scores that met the borderline or greater clinical threshold.
Adult internalizing symptoms (Wave 2)
Adult Self-Report (ASR; Achenbach, 1991)
The ASR is a self-report measure of internalizing and externalizing symptoms for adult participants (18–35-years). The questionnaire asks participants to rate their symptoms over the last six months across 120-items on a 3-point scale (0 = not at all; 1 = sometimes; 2 = always). The ASR produces normed scales for adaptive functioning, psychological syndromes, internalizing problems, externalizing problems, and DSM-oriented scales. All scales are normed for gender and age based on nationally-representative samples. The ASR has strong psychometric properties, including strong test-retest reliability (r = .80 or greater on all scales; Achenbach, 1991). The DSM-oriented subscales for anxiety and depressive disorders were used as indicators for adult internalizing pathology. Within the sample, 11.7% of participants met the threshold for borderline (or higher) clinical symptoms of depression and 11.1% met that threshold for anxiety symptoms.
Beck Depression Inventory-II (BDI-II; Beck, Steer, & Brown, 1996)
The BDI is a commonly used 21-item self-report measure of depressive symptoms. Participants were asked to respond to each item (e.g., “I feel sad”) by choosing one of four statements (0 = never, 1 = sometimes, 2 = often, 3 = always) that best represented their symptomatology over the past two weeks. Clinical-range symptoms are indicated by sum scores of 20 or greater (Beck et al., 1996). In the current sample, 20.7% of the young adults reported sum scores in the clinical range. The BDI-II has good psychometric properties (Wang & Gorenstein, 2013), including test-retest reliability scores ranging from 0.73–0.96 and strong convergent validity with other depression measures (Wang & Gorenstein, 2013). A sum score of all 21 items was used as an indicator of adult internalizing pathology in the current study.
Diagnostic Interview Schedule (DIS-IV: Robins et al., 1995)
The DIS-IV is a structured clinical interview designed to be administered by lay interviewers, via computer software, to provide clinical psychiatric diagnoses based on Diagnostic and Statistical Manual of Mental Disorders-IV criteria (DSM-IV; APA, 1994). The total counts of Major Depressive Disorder (MDD) and Generalized Anxiety Disorder (GAD) symptoms in the past year were used as indicators of adult internalizing pathology. In the current sample, 20.3% of participants met diagnostic criteria for Major Depressive Disorder and 6.5% met diagnostic criteria for Generalized Anxiety Disorder.
Data Analytic Plan
Descriptive data analyses were performed using SPSS 25 and structural equation models (SEMs) were conducted using Mplus Version 8.1 (Muthén & Muthén, 2017). Measurement modeling was conducted to confirm the factor structure of the three proposed indicators of childhood internalizing symptoms (CDI sum score, RCMAS total anxiety score, and the TRF internalizing subscale t-score) and the five proposed indicators of adult internalizing symptoms (BDI sum score, ASR:DSM-oriented subscales for anxiety and depression, and the DIS symptom counts for MDD and GAD). The robust maximum likelihood estimator was used for this confirmatory factor analysis (CFA) because one of the indicator variables was non-normally distributed. The results of the CFA were used to inform SEM model specification.
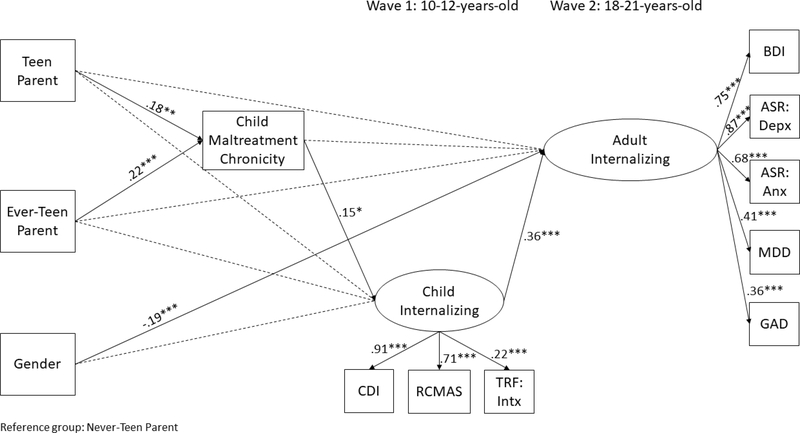
The SEM was specified as follows: two teen childbearing variables (dummy coded, with Never-Teen Parent as the reference group; see Table 1) were entered as exogenous variables; chronicity of child maltreatment was specified as a mediating variable predicted by teen childbearing dummy codes; offspring internalizing symptoms in childhood (Wave 1) was modeled as a latent factor predicted by teen childbearing and child maltreatment; and offspring internalizing symptoms in adulthood (Wave 2) was modeled as an endogenous latent factor predicted by teen childbearing, child maltreatment, and childhood offspring internalizing (see Figure 1). Sex (coded as Female = 0 and Male= 1) was entered as a covariate predicting offspring internalizing symptoms in childhood and adulthood. The SEM was assessed using a resampling (i.e., bootstrapping) method with 1,000 sample replications so that sequential mediation significance (i.e., indirect effects) could be determined via the bootstrapping technique (MacKinnon, Fairchild, & Fritz, 2007).
Table 1.
Descriptive statistics for teen childbearing among parents
| Teen Parent | Ever-Teen Parent | Never-Teen Parent | ||||
|---|---|---|---|---|---|---|
| N | % | N | % | N | % | |
| 118 | 31.0% | 119 | 31.0% | 147 | 38.0% | |
|
| ||||||
| HS diploma | 52.0% | 42.0% | 69.0% | |||
|
| ||||||
| First-time Parent | 68.6% | 0.00% | 47.3% | |||
|
| ||||||
| Employment (past year) | 38.1% | 32.8% | 38.5% | |||
|
| ||||||
| Living with partner (past year) | 31.4% | 26.1% | 31.1% | |||
|
| ||||||
| Race | ||||||
| Black | 76.1% | 71.3% | 63.5% | |||
| White | 11.1% | 12.2% | 30.0% | |||
| Other | 12.8% | 16.5% | 15.5% | |||
Note. Percentages for HS diploma, first-time parent (i.e., the mother was a first-time parent of the target offspring), employment (i.e., if parent was employed at Wave 1 or at any point in the year prior), living with partner (i.e., if parent reported living with a partner at Wave 1 or in the 12 prior months), and race represent the percentages within each category of teen childbearing status.
Figure 1.
Standardized path coefficients are reported. CDI = Child Depression Inventory sum score; RCMAS = Total anxiety symptom T score; TRF: Intx = Teacher Report Form internalizing subscale T score; BDI = Beck Depression Inventory-II sum score; DSM: Depx = Adult Self Report DSM-oriented depressive symptom subscale T score; DSM: Anx = Adult Self Report DSM-oriented anxiety symptom subscale T score; GAD = Diagnostic Interview Schedule—General Anxiety Disorder symptom count; MDD = Diagnostic Interview Schedule—Major Depressive Disorder symptoms; Gender is coded 0 = female, 1 = male; *p < .05, **p < .01, ***p < .001.
Model fit for the CFA and SEM were determined using the following criteria: Comparative fit index (CFI), root mean square error of approximation (RMSEA), and standardized root mean square residual (SRMR; Yu & Muthen, 2002). Acceptable model fit was determined by RMSEA values less than 0.06, CFI greater than 0.95, and SRMR less than 0.08 (Kline, 2011; Yu & Muthen, 2002). The sequential mediation from teen childbearing—to child maltreatment—to offspring child internalizing symptoms—to adult internalizing symptoms was tested with the distribution of the product of the coefficients method with 95% confidence intervals (MacKinnon, Lockwood, & Williams, 2004). Confidence intervals that did not include the value of zero determined significant sequential mediation.
Descriptive Statistics and Preliminary Analysis
Table 1 describes the demographic characteristics of Teen Parents, Ever-Teen Parents, and Never-Teen Parents. Table 2 provides the zero-order correlations among study variables. Table 3 provides the descriptive information for study variables. An ANOVA was conducted to test whether the teen-childbearing groups significantly differed on mean scores of offspring maltreatment chronicity (i.e., number of developmental periods in which maltreatment occurred). The groups significantly differed on the mean number of developmental periods in which maltreatment occurred as determined by a one-way ANOVA, F (2, 383) = 8.77, p < .001. A Bonferroni post hoc test revealed that maltreatment chronicity was significantly greater in the offspring of Teen Parents (p < .01) and Ever-Teen Parents (p < .001) compared to the offspring of Never-Teen Parents. There was no statistically significant difference between the offspring of Teen Parents and Ever-Teen Parents (p = 0.99). These results informed our decision to use Never-Teen Parents as the reference group in the SEM.
Table 2.
Zero-order correlations among study variables (N = 384)
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Maltreatment Chronicity | ||||||||||
| 2. CDI | .16** | |||||||||
| 3. RCMAS | .11* | .64*** | ||||||||
| 4. TRF | .05 | .21*** | .12* | |||||||
| 5. BDI | .11* | .27*** | .22*** | .09 | ||||||
| 6. ASR: Depx | .12* | .25*** | .25*** | .11* | .65*** | |||||
| 7. ASR: Anx | .08 | .26*** | .21*** | .06 | .48*** | .61*** | ||||
| 8. DIS: GAD | .09 | .11* | .09 | −.04 | .27*** | .30*** | .27*** | |||
| 9. DIS: MDD | .03 | .16** | .19*** | .02 | .31*** | .35*** | .27*** | .20*** | ||
| 10. Gender | .03 | .03 | −.01 | −.05 | −.22** | −.14** | −.01 | -.11** | −.13* | |
| Mean/SD NTP | .62/1.1 | 7.2/6.1 | 45.4/10 | 47.3/8.9 | 11.7/8.6 | 55.4/7.0 | 55.6/5.9 | .30/1.2 | 2.4/3.3 | |
| Mean/SD TP | 1.1/1.1 | 8.8/7.8 | 47.3/11 | 48.0/7.8 | 13.0/8.8 | 56.4/7.3 | 57.3/7.0 | .21/.95 | 1.8/3.0 | |
| Mean/SD ETP | 1.0/1.1 | 7.9/6.4 | 46.6/11 | 47.2/8.0 | 12.1/8.4 | 55.6/6.7 | 56.6/6.8 | .50/1.5 | 2.3/3.2 | |
| n | 384 | 382 | 380 | 382 | 384 | 379 | 379 | 379 | 379 | 384 |
Notes: CDI = Child depression; RCMAS = Child anxiety; TRF = Child internalizing; BDI = Beck Depression Inventory-II sum score; ASR Depx and ASR Anx = Adult Self Report depression and anxiety; DIS: GAD and DIS: MDD = Diagnostic Interview Schedule—general anxiety and major depressive symptoms; Gender is coded 0 = female, 1 = male; NTP = Never-Teen Parent; TP = Teen parent; ETP = Ever-Teen Parent.
p < .05
p < .01
p < .001.
Table 3.
Descriptive statistics of offspring study variables
| N | Minimum | Maximum | M | SD | Skewness | Kurtosis | |
|---|---|---|---|---|---|---|---|
| CDI | 382 | 00.00 | 42.00 | 7.91 | 6.76 | 1.43 | 2.58 |
| RCMAS | 380 | 18.00 | 78.00 | 46.36 | 10.35 | 0.34 | 0.60 |
| TRF | 384 | 36.00 | 76.00 | 47.47 | 8.29 | 0.68 | −0.01 |
| BDI | 384 | 0.00 | 44.00 | 12.20 | 8.58 | 0.84 | 0.30 |
| DSM: Depx | 379 | 50.00 | 84.00 | 55.75 | 7.00 | 1.40 | 1.50 |
| DSM: Anx | 379 | 50.00 | 77.00 | 56.35 | 6.54 | 1.00 | 0.06 |
| DIS:GAD | 379 | 0.00 | 6.00 | 0.33 | 1.23 | 3.61 | 3.65 |
| DIS: MDD | 379 | 0.00 | 9.00 | 3.15 | 1.15 | 0.13 | −0.40 |
Notes: CDI = Child Depression Inventory sum score; RCMAS = Total anxiety symptom T score; TRF = Teacher Report Form internalizing subscale T score; BDI = Beck Depression Inventory-II sum score; DSM: Depx = Adult Self Report DSM-oriented depressive symptom subscale T score; DSM: Anx= Adult Self Report DSM-oriented anxiety symptom subscale T score; DIS: GAD = Diagnostic Interview Schedule—General Anxiety Disorder symptoms; DIS: MDD = Diagnostic Interview Schedule—Major Depressive Disorder symptoms.
Test of Measurement Model
CFAs were conducted to determine the factor structure of both latent variables (child and adult internalizing). Results suggested good model fit χ2 (19) = 17.55 p = .60, CFI = 1.00, RMSEA = .00 (90% CI: .00–.04), SRMR = .02 and standardized factor loadings were all statistically significant (λ = .22–.87) and mostly large (>.70).
Test of Structural Model
The fit indices for the SEM indicated good fit χ2 (44) = 61.25, p = .04, RMSEA=.03 (90% CI: .01–.05), CFI=.98, SRMR=.03 (see Figure 1 for graphical representation of model and results). Results suggested that compared to being the child of a Never-Teen Parent (i.e., reference group), being born to a Teen Parent (b = .18, p < .01)1 and Ever-Teen Parent (b = .22, p < .001) predicted greater maltreatment chronicity for offspring. However, there were no significant direct effects of teen childbearing (Teen Parent or Ever-Teen Parent) on offspring internalizing symptoms in either childhood or young adulthood.
Regarding the effects of maltreatment, more chronic maltreatment was associated with greater offspring internalizing symptoms in childhood (b = .15, p < .05), but not in young adulthood (b = .09, ns). However, results indicated symptom continuity, as higher levels of offspring childhood internalizing symptoms predicted greater levels of internalizing symptoms in adulthood (b = .36, p < .001). Finally, female offspring reported more internalizing symptoms in young adulthood than did male offspring (b = −.20, p < .001); gender did not have a significant effect on childhood internalizing symptoms2.
To examine whether child maltreatment chronicity represents a mechanism by which teen childbearing affects offspring internalizing symptoms, 95% bootstrap confidence intervals were calculated (MacKinnon et al., 2004). Comparing the offspring of Teen Parents to Never-Teen Parents (reference group), teen childbearing indirectly affected offspring childhood internalizing symptoms through chronic child maltreatment [LCL = .003, UCL = .06]. Moreover, there was significant two-sequence mediation from teen childbearing→child maltreatment→offspring child internalizing symptoms→adult internalizing symptoms [LCL = .001, UCL = .02]. Similarly, comparing the offspring of Ever-Teen Parents to Never-Teen Parents (reference group), teen childbearing exhibited an indirect effect on offspring internalizing symptoms in childhood via chronic child maltreatment [LCL=.004, UCL=.08] and in adulthood via multiple mediators (chronic child maltreatment and offspring child internalizing) [LCL=.02, UCL= .40].
The model was re-specified with Ever-Teen Parents as the reference group, allowing for direct comparisons between Teen Parents and Ever-Teen Parents in the prediction of child maltreatment chronicity. The fit indices for this model indicated good fit χ2 (44) = 59.70, p = .06, RMSEA=.03 (90% CI: .01-.05), CFI=.98, SRMR=.04. Results suggested that compared to being the child of an Ever-Teen Parent (i.e., reference group), being born to a Never-Teen Parent predicted significantly less maltreatment chronicity for offspring (b = −0.22, p < .001). The offspring of Teen Parents did not experience significantly greater maltreatment chronicity compared to Ever-Teen Parents (b = −0.05, p = 0.50). There were no significant direct effects of teen childbearing status on offspring internalizing symptoms in either childhood or young adulthood. Regarding the effects of maltreatment, greater maltreatment chronicity was associated with greater offspring internalizing symptoms in childhood (b = .15, p < .05), but not in young adulthood (b = .09, ns). However, results indicated symptom continuity, as higher levels of offspring childhood internalizing symptoms predicted greater levels of internalizing symptoms in adulthood (b = .36, p < .001).
Discussion
The aims of the current investigation were to use a longitudinal design to examine whether teen childbearing imparts an enduring effect on offspring internalizing symptoms in both childhood (ages 10–12) and into young adulthood (ages 18–21) and to examine the role of offspring child maltreatment chronicity as a mediating factor within a socioeconomically-disadvantaged, ethnically-diverse sample. The current findings buttress existing literature on the association between teen childbearing and offspring psychopathology outcomes (Coyne & D’Onofrio, 2012) and expand on previously explored mediating mechanisms, such as ineffective or impaired caregiving behavior (e.g., Dahinten et al., 2007; Jaffee et al., 2001), by examining chronic child maltreatment—an extreme form of impaired caregiving (Cicchetti, 2011)—as an intervening variable. Moreover, although prior studies have established a predictive relationship between teen childbearing and offspring maltreatment (Bartlett & Easterbrooks, 2012; Lee, 2009; Putnam-Hornstein, & Needell, 2011) and between chronic maltreatment and offspring internalizing psychopathology (Cicchetti & Toth, 2016), this study unpacks the processes by which offspring of young mothers may be at risk for internalizing symptoms throughout development—namely, via heightened maltreatment risk.
Teen childbearing and offspring internalizing
A direct effect of teen childbearing on offspring internalizing symptoms was not supported. This is not surprising, given the mixed findings regarding the isolated and independent effect of maternal age at birth on offspring outcomes (D’Onofrio et al., 2009; Geronimus et al., 1994; Harden et al., 2007). Rather, the results further support the second aim of the study, which was to identify potential mediating or indirect effects that initiate a cascading link from teen childbearing to offspring symptoms.
Teen childbearing and child maltreatment
Regarding the first path of the two-mediator sequential chain, we found that the offspring of teen-childbearing parents (both Teen Parents and Ever-Teen Parents) were predictably more likely to experience child maltreatment that persisted across more developmental periods than the offspring of Never-Teen Parents. Although the link between teen childbearing and offspring maltreatment chronicity is not deterministic, this finding aligns with other studies that have similarly found a probabilistic relationship between the two phenomena (e.g., Bartlett & Easterbrooks, 2012; Putnam-Hornstein, & Needell, 2011).
According to complex ecological-transactional perspectives on the development of child maltreatment, no single risk factor, such as teen childbearing, could entirely account for the etiology of maltreatment (Cicchetti & Lynch, 1993). Although child maltreatment has been shown to be multiply determined (Cicchetti & Toth, 2016), there are a variety of explanations for why teen childbearing may be a salient risk factor for the chronic offspring maltreatment observed in this study. Though speculative, some of these determinants will be briefly reviewed to further contextualize the study findings.
Development
One explanation may be that having a child during a developmentally vulnerable time (i.e., adolescence), when the mother is less prepared to navigate the challenges of parenting, may result in a coalescence of adversity, stress, and developmental immaturity (e.g., weaker executive function skills and more emotional volatility) that compounds and impairs her capacity to provide a salubrious caregiving environment and exacerbates the propensity for chronic maltreatment exposure for her offspring. A unique finding of this study is that the offspring of Teen Parents and Ever-Teen Parents are both at risk for more chronic maltreatment.This suggests that simply beginning childbearing during the teen years may initiate a set of enduring conditions that place subsequent children at risk for chronic maltreatment, even by adult parents, as is seen with the offspring of Ever-Teen Parents in this study.
Early entry into parenting during the teen years may disrupt development and the achievement of stage-salient developmental tasks associated with high-quality caregiving. Individuals who successfully master stage-salient tasks integrate those adaptations into an internalized hierarchy and are more equipped to adaptively negotiate future life challenges; individuals who struggle to resolve stage-salient tasks may develop liabilities in their internal resources and increase the likelihood of maladaptive responses to subsequent life challenges (Cicchetti & Rogosch, 2002). Applied to Ever-Teen Parents, the internal parenting resources (e.g., emotional autonomy and affect regulation) that Ever-Teen Parents have available for their offspring during adulthood depends substantially on how they were able to negotiate stage-salient tasks during their prior teen years (Cicchetti & Rogosch, 2002)—the very time when they began childbearing. It is possible that teen childbearing thwarted the successful resolution of stage-salient tasks (e.g., emotional autonomy or competence) for these mothers, suspending their developmental growth and compromising their caregiving ability, fixing a maladaptive parenting pattern that persists with future children (Geeraert, Van den Noortgate, Grietens, & Onghena, 2004).
Identity shift
The precipitous shift in identity from adolescent to parent may also contribute to maltreatment risk for the offspring of teen-childbearing mothers. That is, the dependent needs of the child may compete with a teen mother’s stage-salient efforts to establish her own autonomy and independence (Feldman, 2012). The dissonance that arises from these competing demands may impede the formation of a healthy attachment with the child (Osofsky et al., 1993), increasing the risk for maltreatment (Stith et al., 2009). For example, the majority of teen pregnancies are unwanted (OAH, 2016) and teen parents may develop ambivalent feelings towards the child (e.g., “I love you and I resent being a parent”) and/or negative representations (e.g., “My child stole my teen years”) that leave them feeling resentful of, and less emotionally connected to, the child (Berlin et al., 2002; Fergusson & Woodward, 1999), which are strong predictors of offspring maltreatment (Berlin et al., 2002; Lee & Gutterman, 2010; Stith et al., 2009). For Ever-Teen Parents, it may be that they experienced these processes during their initial experiences of child rearing in adolescence and have unresolved or unprocessed grief pertaining to the loss of their adolescence that emerges in their dyadic interactions with all their children. The activiation of these previously established negative representations of the caregiving relationship may then result in maltreatment (Stith et al., 2009).
Pre-existing factors
Similarly, although this study demonstrated an association between teen childbearing and offspring maltreatment, it is certainly possible that factors which predate teen childbearing contribute to this association (e.g., socioeconomic disadvantage, maternal maltreatment history, or maternal characteristics). For example, instead of a causal relationship between teen childbearing and offspring maltreatment, it may be that adolescent girls with pre-existing psychopathology or traits such as impulsivity and risk-taking are selected into teen childbearing (Coyne et al., 2013), and then it is these same propensities—which predate teen childbearing—that directly predict offspring maltreatment (Mulder et al., 2018). Thus, the individuals who are most likely to have offspring who experience maltreatment (i.e., individuals with risky traits; Mulder et al., 2018) are also most likely to be selected into teen childbearing (Jaffee et al., 2001).
Child Maltreatment and Offspring Internalizing Symptoms
Chronicity of child maltreatment predicted greater offspring internalizing symptoms in childhood. This finding is consistent with a robust literature establishing a link between child maltreatment and risk for internalizing symptoms (see Li, D’Arcy, & Meng, 2016 for review). Indeed, some have even suggested that the majority of internalizing disorders are related to child maltreatment histories (see Jaffee, 2017 for review). Exposure to the aberrant conditions of chronic child maltreatment compromises development and likely initiates the emergence of lasting vulnerabilities that dramatically elevate the risk for internalizing symptoms that extends from childhood to emerging adulthood (Cicchetti & Toth, 2016). Further, childhood internalizing symptoms predicted subsequent internalizing symptoms ten years later during the transition into emerging adulthood. This developmental symptom continuity is in accordance with other findings on the unfolding of internalizing symptoms across development (Jaffee, 2017).
Sequential Mediation
Taken together, our results support a two-mediator, developmental sequence in which teen childbearing potentiates chronicity of child maltreatment for offspring, which in turn acts as a catalyst for these same children to develop emergent internalizing symptoms in childhood that continues and endures into young adulthood. Further, this indirect pathway exists over and above the sex differences that are commonly observed in the development of internalizing and depressive symptoms during the transition from adolescence to adulthood (Cyranowski, Frank, Young, & Shear, 2000). Therefore, our results suggest that although teen childbearing may not be the reason for offspring psychopathology, it may act as an initial push that results in a cascade toward disorder (Hyde, 2015). In other words, the pathway to offspring internalizing symptoms may be initiated as a result of the mother beginning childbearing in adolescence; however, the path is then sustained and maintained by subsequent mechanisms (i.e., child maltreatment).
To date, only one prior study has examined a maltreatment-mediated pathway from teen childbearing to offspring internalizing symptoms into emerging adulthood (Fergusson & Woodward, 1999). In their study, Fergusson and Woodward (1999) relied on retrospective reports of sexual abuse to measure child maltreatment, whereas this study utilized documented reports to record chronic child maltreatment via multiple forms of abuse and neglect to advance the current understanding of the mediating role of child maltreatment.
Strengths and Limitations
This study should be interpreted within the context of the strengths and limitations inherent in its design. First, although we have offered several speculative explanations for why teen childbearing increases risk for offspring maltreatment based on existing literature, the current study was unable to systematically explore explanatory mechanisms of this aspect of the developmental cascade, such as maternal representational models, maternal mental health, and cumulative maternal stress. Second, and relatedely, it should be noted that the study sample represents a high-risk sample (i.e., low-income, maltreated/nonmaltreated children) that was enriched for child maltreatment and is not representative of the entire population of teen-childbearing parents. Thus, it is possible that the effects of teen childbearing on offspring maltreatment may be inflated or amplified in this sample. The results of this study are not intended to generate incidence data and the association between teen childbearing and offspring maltreatment may not be as robust when using a nationally-representative sample of teen childbearing parents. An alternative approach would be a prospective design that identified a representative sample of low-income participants based on teen-childbearing status (rather than offspring maltreatment status) and then followed parents and offspring to examine the developmental cascade to subsequent offspring maltreatment and offspring internalizing pathology in childhood and into emerging adulthood. This design would allow for the exploration of additional demographic risks that may be operating for teen-childbearing parents and allow for the examination of mechanisms underlying the relationship between teen childbearing and offspring maltreatment.
Additionally, we were unable to control for a variety of maternal factors known to influence offspring symptoms that may confound results, such as maternal depression or maternal maltreatment history, the wantedness of the pregnancy, cultural views of teen pregnancy, prenatal environmental factors, infant birthweight, and gestational age (Cornelius et al., 2009; Rogers, Lenze, & Luby, 2013). Also, we relied on record data from the child welfare system to determine maltreatment chronicity and it is possible that children in the nonmaltreated group experienced maltreatment that did not come to the attention of Child Protective Services (CPS). Relatedly, we were unable to subsequently examine CPS records at Wave 2 of the study to determine if maltreatment continued into adolescence. Future studies would ideally continue to track subjects’ involvement with CPS throughout adolescence. Finally, the associations between teen parenthood and negative offspring outcomes are not deterministic, and many children experience resilient, positive outcomes. Although it was beyond the scope of the present study, future research should aim to examine buffering factors (e.g., family support; Mollborn, 2017) that may interrupt negative cascades.
Even with the limitations, this study contains a range of methodological strengths. The multi-informant measurement design is an example. Rather than over-relying on self-report measures that are prone to have validity issues (e.g., response bias), the current study draws on a multi-informant approach including self- and other-reports, as well as objective records. Specifically, the use of documented records to prospectively measure child maltreatment addresses the recognized limitations of retrospective self-reports of abuse (Baldwin et al., 2019; Manly, 2005). Additionally, the use of a multi-informant latent construct to measure childhood internalizing symptoms is a principal strength, as research suggests that the self-directed nature of internalizing symptoms tends to result in variations and discrepancies between reporters (Tandon, Cardeli, & Luby, 2009).
The developmental longitudinal design and recruitment procedures also confer substantial methodological advantages. For instance, the temporal ordering of variables facilitated the examination of a sequential-mediational chain across the life course into emerging adulthood. Also, because nonmaltreated comparisons were recruited to be comparable on economic status to the maltreated sample, we were able to observe the impact of teen childbearing on offspring symptoms (via child maltreatment) within a low-income population, neutralizing income as a major confounding factor related to all three study constructs (i.e., teen childbearing, child maltreatment, offspring internalizingy symptoms) in the extant literature.
Implications
Internalizing psychopathology (i.e., depression and anxiety) is one of the leading causes of disability in the United States (National Institutes of Health, 2019) and elucidating its developmental origin to inform intervention is critical. We have presented a developmental model of psychopathology that traces the roots of child and adult internalizing symptoms to chronic child maltreatment that is influenced by the timing of the mother’s initiation of childbearing. This perspective can inform preventive interventions that are developmentally-timed in a way that can prevent or ameliorate psychopathology outcomes for at-risk individuals.
For example, though a variety of programs exist to effectively prevent teen pregnancy (Koh, 2014), this is not the only way to prevent risk pathways and ensure healthy offspring development, as many teen parents and their children experience resilient outcomes (Easterbrooks et al., 2013). Rather, the current findings can be translated into early interventions designed to interrupt the detrimental pathway from teen childbearing to child maltreatment within these vulnerable dyads, thereby reducing the emergence of psychopathology before risks accumulate and the pathway becomes further entrenched (Toth, Petrenko, Davis, & Handley, 2016).
Delivering home-based and/or relational interventions that empower teen parents, promote emotionally sensitive parenting, and foster secure attachment relationships may stall or suppress the detrimental cascade presented in this study before it can engulf the offspring’s development (Cicchetti, 2011; Masten & Cicchetti, 2010). For example, insight-oriented relational interventions that address parental trauma histories, psychopathology, and maladaptive representational models about caregiving—all common in teen parents—are effective in preventing child maltreatment (e.g., Valentino, 2017). Similarly, comprehensive intervention programs for teen mothers that utilize home-visiting (reducing treatment barriers for teen parents) to seamlessly integrate services addressing the socioeconomic (e.g., employment and educational support), psychological (e.g., maternal mental health and abuse history), and parenting needs of teen mothers may alleviate the cumulative burdens and challenges facing teen parents and minimize the risk for maltreatment in offspring (Paradis et al., 2013; Toth & Manly, 2011)
Furthermore, this study also has important implications for screening vulnerable individuals for prevention services. Because the results of this study demonstrate that the offspring of both Teen Parents and Ever-Teen Parents are at risk for chronic maltreatment and subsequent internalizing psychopathology, teen childbearing history should be considered as an indicator for the need for prevention services for families. Although prevention services exist for teen parents and their children (Olds, 2006; Paradis et al., 2013), programs rarely consider a history of teen childbearing when working with adult mothers and their later-born children. However, the current findings suggest teen-childbearing history should be assessed with all pregnant women because it represents an excellent screening tool to identify families who may benefit from preventive services.
The screening process could potentially be modeled after the new 2018 recommendations by the U.S. Preventive Services Task Force for screening pregnant women and new mothers for depression (U.S. Preventive Services Task Force, 2018). The Task Force recommends that physicians screen all pregnant women and new mothers for depression risk factors (e.g., unwanted pregnancy, abuse history, stressful live events, and teen pregnancy) so that these women can be offered preventive services, before the onset of symptoms, during the prenatal and postnatal periods. Similarly, based on the results of the current study, we would recommend that pregnant women and new mothers are screened for teen-childbearing histories so that they may be offered preventive services that may avert chronic maltreatment and psychopathology for their offspring.
Conclusion
In conclusion, the present study illuminates a lesser studied mechanism (i.e., child maltreatment), with implications for lifespan development, involved in the relationship between teen childbearing and offspring internalizing symptoms. Reaching back to explore the risk mechanisms that initiate (i.e., teen childbearing) and sustain (i.e., child maltreatment) the developmental path to offspring internalizing symptoms can help direct the allocation of resources to more effective interventions that target appropriate etiological constructs. Informed by this research, practitioners will be better able to screen pregnant women and new mothers for teen childbearing histories and direct developmentally-timed preventive services, which may prevent offspring maltreatment and psychopathology and promote positive, resilient trajectories for mothers and their children following teen childbearing.
Acknowledgments
We are grateful to the National Institute on Drug Abuse (R01-DA01774 to Fred A. Rogosch and Dante Cicchetti) for their support of this work. Address correspondence to Justin Russotti, Mt. Hope Family Center, 187 Edinburgh Street, Rochester, NY 14608.
Footnotes
Standardized effects are reported.
The model was re-estimated to include maternal demographic factors (i.e., high school education, whether they were a first-time parent, and race) as covariates predicting offspring maltreatment. Because the pattern of results remained unchanged and because of missing data on these maternal variables, the decision was made to trim the covarites from the final model and present the more parsimonious model.
References
- Achenbach TM (1991). Manual for the Teacher’s Report Form and 1991 profile. Vermont: University of Vermont Department Psychiatry. [Google Scholar]
- Achenbach TM, Dumenci L, & Rescorla LA (2003). DSM-oriented and empirically based approaches to constructing scales from the same item pools. Journal of Clinical Child and Adolescent Psychology, 32(3), 328–340. doi: 10.1207/S15374424JCCP3203_02 [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders (4th Edition-Revised). Washington, DC: American Psychiatric Association. [Google Scholar]
- Baldwin JR, Reuben A, Newbury JB, & Danese A (2019). Agreement between prospective and retrospective measures of childhood maltreatment: a systematic review and meta-analysis. JAMA psychiatry. doi: 10.1001/jamapsychiatry.2019.0097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartlett JD, & Easterbrooks MA (2012). Links between physical abuse in childhood and child neglect among adolescent mothers. Children and Youth Services Review, 34(11), 2164–2169. doi: 10.1016/j.childyouth.2012.07.011 [DOI] [Google Scholar]
- Barnett D, Manly JT, Cicchetti D, & Toth SL (1993). Child abuse, child development, and social policy.
- Beck AT, Steer RA, & Brown GK (1996). Manual for Beck Depression Inventory—II. San Antonio, TX: Psychological Corporation. [Google Scholar]
- Berlin LJ, Brady-Smith C, & Brooks-Gunn J (2002). Links between childbearing age and observed maternal behaviors with 14-month-olds in the Early Head Start Research and Evaluation Project. Infant Mental Health Journal: Official Publication of the World Association for Infant Mental Health, 23(1–2), 104–129. doi: 10.1002/imhj.10007. [DOI] [Google Scholar]
- Bolger KE, & Patterson CJ (2001). Developmental pathways from child maltreatment to peer rejection. Child Development, 72, 549–568. doi: 10.1111/1467-8624.00296. [DOI] [PubMed] [Google Scholar]
- Chang Z, Lichtenstein P, D’Onofrio BM, Almqvist C, Kuja-Halkola R, Sjölander A, & Larsson H (2014). Maternal age at childbirth and risk for ADHD in offspring: A population-based cohort study. International Journal of Epidemiology, 43(6), 1815 1824. doi: 10.1093/ije/dyu204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicchetti D (2011). Developmental psychopathology. In Lerner RM, Freund AM, & Lamb ME (Eds.), Lifespan development (Vol. 2, pp. 511–589). Hoboken, NJ: Wiley & Sons. [Google Scholar]
- Cicchetti D, & Manly JT (1990). A personal perspective on conducting research with maltreating families: Problems and solutions. In Brody G & Sigel I (Eds.), Methods of family research: Families at risk (Vol. 2, pp. 87–133). Hillsdale, NJ: Erlbaum. [Google Scholar]
- Cicchetti D, & Rogosch FA (2002). A developmental psychopathology perspective on adolescence. Journal of Consulting and Clinical Psychology, 70(1), 6.doi: 10.1037/0022-006X.70.1.6. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, & Lynch M (1993). Toward an ecological/transactional model of community violence and child maltreatment: Consequences for children’s development. Psychiatry, 56, 96–118. doi: 10.1080/00332747.1993.11024624. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, & Toth SL (2016). Child maltreatment and developmental psychopathology: A multilevel perspective. In Cicchetti D (Ed.), Developmental psychopathology: Maladaptation and psychopathology (3rd ed., pp. 457–512). Hoboken, NJ: Wiley. [Google Scholar]
- Cicchetti D, Toth SL, & Manly JT (2003). Maternal maltreatment classification interview. Unpublished manuscript, Mt. Hope Family Center, Rochester, NY. [Google Scholar]
- Coelho FMDC, Pinheiro RT, Silva RA, Quevedo LDÁ, Souza LDDM, Castelli RD, … & Pinheiro KAT (2013). Major depressive disorder during teenage pregnancy: Socio-demographic, obstetric and psychosocial correlates. Revista Brasileira de Psiquiatria, 35(1), 51–56. doi: 10.1016/j.rbp.2012.03.006. [DOI] [PubMed] [Google Scholar]
- Cornelius M, Goldschmidt L, DeGenna N, & Day N (2007). Smoking during teenage pregnancies: Effects on behavioral problems in offspring. Nicotine & Tobacco Research, 9(7), 739–750. doi: 10.1080/14622200701416971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coyne CA, & D’Onofrio BM (2012). Some (but not much) progress toward understanding teenage childbearing: A review of research from the past decade. In Advances in child development and behavior (Vol. 42, pp. 113–152). JAI.doi: 10.1016/B978-0-12-394388-0.00004-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cyranowski JM, Frank E, Young E, & Shear MK (2000). Adolescent onset of the gender difference in lifetime rates of major depression: a theoretical model. Archives of General Psychiatry, 57(1), 21–27. doi: 10.1001/archpsyc.57.1.21. [DOI] [PubMed] [Google Scholar]
- Coyne CA, Långström N, Lichtenstein P, & D’Onofrio BM (2013). The association between teenage motherhood and poor offspring outcomes: A national cohort study across 30 years. Twin Research and Human Genetics, 16(3), 679–689. doi: 10.1017/thg.2013.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Onofrio BM, Goodnight JA, Van Hulle CA, Rodgers JL, Rathouz PJ, Waldman ID, & Lahey BB (2009). Maternal age at childbirth and offspring disruptive behaviors: Testing the causal hypothesis. Journal of Child Psychology and Psychiatry, 50(8), 1018–1028. doi: 10.1111/j.1469-7610.2009.02068.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahinten VS, Shapka JD, & Willms JD (2007). Adolescent children of adolescent mothers: The impact of family functioning on trajectories of development. Journal of Youth and Adolescence, 36(2), 195–212. doi: 10.1007/s10964-006-9140-8. [DOI] [Google Scholar]
- Deater-Deckard K, Wang Z, Chen N, & Bell MA (2012). Maternal executive function, harsh parenting, and child conduct problems. Journal of Child Psychology and Psychiatry, 53(10), 1084–1091. doi: 10.1111/j.1469-7610.2012.02582.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Easterbrooks MA, Chaudhuri JH, Bartlett JD, & Copeman A (2011). Resilience in parenting among young mothers: Family and ecological risks and opportunities. Children and Youth Services Review, 33(1), 42–50. doi: 10.1016/j.childyouth.2010.08.010 [DOI] [Google Scholar]
- Easterbrooks MA, Bartlett JD, Raskin M, Goldberg J, Contreras MM, Kotake C, … & Jacobs FH (2013). Limiting home visiting effects: maternal depression as a moderator of child maltreatment. Pediatrics, 132(Supplement 2), S126–S133. doi: 10.1542/peds.2013-1021K. [DOI] [PubMed] [Google Scholar]
- Feldman JB (2012). Best practice for adolescent prenatal care: Application of an attachment theory perspective to enhance prenatal care and diminish birth risks. Child and Adolescent Social Work Journal, 29(2), 151–166. [Google Scholar]
- Fergusson DM, & Woodward LJ (1999). Maternal age and educational and psychosocial outcomes in early adulthood. The Journal of Child Psychology and Psychiatry and Allied Disciplines, 40(3), 479–489. doi: 10.1111/1469-7610.00464 [DOI] [PubMed] [Google Scholar]
- Geeraert L, Van den Noortgate W, Grietens H, & Onghena P (2004). The effects of early prevention programs for families with young children at risk for physical child abuse and neglect: A meta-analysis. Child maltreatment, 9(3), 277–291. doi:10.1177%2F1077559504264265. [DOI] [PubMed] [Google Scholar]
- Geronimus AT, Korenman S, & Hillemeier MM (1994). Does young maternal age adversely affect child development? Evidence from cousin comparisons in the United States. Population and Development Review, 585–609. doi: 10.2307/2137602. [DOI] [Google Scholar]
- Harden KP, Lynch SK, Turkheimer E, Emery RE, D’onofrio BM, Slutske WS, … & Martin NG (2007). A behavior genetic investigation of adolescent motherhood and offspring mental health problems. Journal of Abnormal Psychology, 116(4), 667. doi: 10.1037/0021-843X.116.4.667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardy JB, Sharpiro S, Astone NM, Miller TL, Brooks-Gunn J, & Hilton SC (2006). Adolescent childbearing revisited: The age of inner-city mothers at delivery is a determinant of their children’s self-sufficiency at age 27 to 33. Pediatrics, 100, 802– 809. doi: 10.1542/peds.100.5.802. [DOI] [PubMed] [Google Scholar]
- Hyde LW (2015). Developmental psychopathology in an era of molecular genetics and neuroimaging: A developmental neurogenetics approach. Development and Psychopathology, 27(02), 587–613. doi: 10.1017/S0954579415000188. [DOI] [PubMed] [Google Scholar]
- Jaffee SR (2017). Child maltreatment and risk for psychopathology in childhood and adulthood. Annual Review of Clinical Psychology, 13, 525–551. doi: 10.1146/annurevclinpsy-032816-045005. [DOI] [PubMed] [Google Scholar]
- Jaffee S, Caspi A, Moffitt TE, Belsky JAY, & Silva P (2001). Why are children born to teen mothers at risk for adverse outcomes in young adulthood? Results from a 20-year longitudinal study. Development and Psychopathology, 13(2), 377–397. doi: 10.1017/S0954579401002103. [DOI] [PubMed] [Google Scholar]
- Khatun M, Al Mamun A, Scott J, William GM, Clavarino A, & Najman JM (2017). Do children born to teenage parents have lower adult intelligence? A prospective birth cohort study. PloS One, 12(3), e0167395. doi: 10.1371/journal.pone.0167395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kingsbury M, Weeks M, MacKinnon N, Evans J, Mahedy L, Dykxhoorn J, & Colman I (2016). Stressful life events during pregnancy and offspring depression: Evidence from a prospective cohort study. Journal of the American Academy of Child & Adolescent Psychiatry, 55(8), 709–716. doi: 10.1016/j.jaac.2016.05.014. [DOI] [PubMed] [Google Scholar]
- Kline RB (2011). Convergence of structural equation modeling and multilevel modeling. In Williams M & Vogt WP (Eds.), Handbook of methodological innovation (pp. 562–589). London, England: Sage. [Google Scholar]
- Kovacs M (1982). The Children’s Depression Inventory: A self-rated depression scale for school-aged youngsters. Unpublished manuscript.
- Kovacs M (2004). Children’s depression inventory (CDI). North Tonawanda, NY: Multi Health Systems. [Google Scholar]
- Koh H (2014). The Teen Pregnancy Prevention Program: An evidence-based public health program model. Journal of Adolescent Health, 54(3), S1–S2. doi: 10.1016/j.jadohealth.2013.12.031. [DOI] [PubMed] [Google Scholar]
- Lee Y (2009). Early motherhood and harsh parenting: The role of human, social, and cultural capital. Child Abuse & Neglect, 33(9), 625–637. doi: 10.1016/j.chiabu.2009.02.007 [DOI] [PubMed] [Google Scholar]
- Lee Y, & Gutterman N (2010). Young mother–father dyads and maternal harsh parenting behavior. Child Abuse and Neglect, 34(11), 874–885. doi: 10.1016/j.chiabu.2010.06.001. [DOI] [PubMed] [Google Scholar]
- Li M, D’arcy C, & Meng X (2016). Maltreatment in childhood substantially increases the risk of adult depression and anxiety in prospective cohort studies: Systematic review, meta analysis, and proportional attributable fractions. Psychological Medicine, 46(4), 717–730. doi: 10.1017/S0033291715002743. [DOI] [PubMed] [Google Scholar]
- MacKenzie MJ, Nicklas E, Brooks-Gunn J, & Waldfogel J (2011). Who spanks infants and toddlers? Evidence from the fragile families and child well-being study. Children and Youth Services Review, 33(8), 1364–1373. doi: 10.1016/j.childyouth.2011.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, & Williams J (2004). Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivariate Behavioral Research, 39(1), 99–128. doi: 10.1207/s15327906mbr3901_4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Fairchild AJ, & Fritz MS (2007). Mediation analysis. Annual Reviews Psychology, 58, 593–614. doi: 10.1146/annurev.psych.58.110405.085542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manly JT (2005). Advances in research definitions of child maltreatment. Child Abuse & Neglect, 29, 425–439. doi: 10.1016/j.chiabu.2005.04.001. [DOI] [PubMed] [Google Scholar]
- Manly JT, Kim JE, Rogosch FA, & Cicchetti D (2001). Dimensions of child maltreatment and children’s adjustment: Contributions of developmental timing and subtype. Development and Psychopathology, 13(4), 759–782. doi: 10.1017/S0954579401004023 [DOI] [PubMed] [Google Scholar]
- Masten AS, & Cicchetti D (2010). Developmental cascades. Development and Psychopathology, 22(3), 491–495. doi: 10.1017/S0954579410000222 [DOI] [PubMed] [Google Scholar]
- Mok PL, Antonsen S, Pedersen CB, & Webb RT (2017). Younger or older parental age and risk of suicidality, premature death, psychiatric illness, and criminality in offspring. Journal of Affective Disorders, 208, 130–138. doi: 10.1016/j.jad.2016.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mollborn S (2017). Teenage mothers today: What we know and how it matters. Child Development Perspectives, 11(1), 63–69. doi: 10.1111/cdep.12205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mollborn S, & Dennis JA (2012). Explaining the early development and health of teen mothers’ children. In Sociological Forum (Vol. 27, No. 4, pp. 1010–1036). Blackwell Publishing Ltd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mollborn S, & Dennis JA (2012). Investigating the life situations and development of teenage mothers’ children: Evidence from the ECLS-B. Population Research and Policy Review, 31(1), 31–66. doi: 10.1007/s11113-011-9218-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mollborn S, Lawrence E, James-Hawkins L, & Fomby P (2014). How resource dynamics explain accumulating developmental and health disparities for teen parents’ children. Demography, 51(4), 1199–1224. doi: 10.1007/s13524-014-0301-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulder TM, Kuiper KC, van der Put CE, Stams GJJ, & Assink M (2018). Risk factors for child neglect: A meta-analytic review. Child Abuse & Neglect, 77, 198– 210. doi: 10.1016/j.chiabu.2018.01.006. [DOI] [PubMed] [Google Scholar]
- Muthén LK and Muthén BO (1998–2017). Mplus User’s Guide (8th Edition). Los Angeles, CA: Muthén & Muthén [Google Scholar]
- Olds DL (2006). The nurse–family partnership: An evidence-based preventive intervention. Infant Mental Health Journal, 27(1), 5–25. doi: 10.1002/imhj.20077. [DOI] [PubMed] [Google Scholar]
- Osofsky JD, Hann DM, & Peebles C (1993). Adolescent parenthood: Risks and opportunities for mothers and infants. In Zeanah CH (Ed.) Handbook of Infant Mental Health, New York: Guilford. [Google Scholar]
- Paradis HA, Sandler M, Manly JT, & Valentine L (2013). Building healthy children: Evidence-based home visitation integrated with pediatric medical homes. Pediatrics, 132(Supplement 2), S174–S179. doi: 10.1542/peds.2013-1021R. [DOI] [PubMed] [Google Scholar]
- Pogarsky G, Lizotte AJ, & Thornberry TP (2003). The delinquency of children born to young mothers: Results from the Rochester Youth Development Study. Criminology, 41(4), 1249–1286. doi: 10.1111/j.1745-9125.2003.tb01019.x. [DOI] [Google Scholar]
- Pogarsky G, Thornberry TP, & Lizotte AJ (2006). Developmental outcomes for children of young mothers. Journal of Marriage and Family, 68(2), 332–344. doi: 10.1111/j.1741-3737.2006.00256.x. [DOI] [Google Scholar]
- Putnam-Hornstein E, & Needell B (2011). Predictors of child protective service contact between birth and age five: An examination of California’s 2002 birth cohort. Children and Youth Services Review, 33(8), 1337–1344. doi: 10.1016/j.childyouth.2011.04.006. [DOI] [Google Scholar]
- Reynolds CR, & Richmond BO (1978). What I think and feel: A revised measure of children’s manifest anxiety. Journal of Abnormal Child Psychology, 6(2), 271–280. [DOI] [PubMed] [Google Scholar]
- Robins L, Cottler L, Bucholz K, & Compton W (1995). Diagnostic interview schedule for dsm-iv (dis-iv). Washington University School of Medicine: St Louis, MO. [Google Scholar]
- Rogers CE, Lenze SN, & Luby JL (2013). Late preterm birth, maternal depression, and risk of preschool psychiatric disorders. Journal of the American Academy of Child & Adolescent Psychiatry, 52(3), 309–318. doi.org/ 10.1016/j.jaac.2012.12.005.s [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sedlak AJ, Mettenburg J, Basena M, Petta I, McPherson K, & Greene A (2010). Fourth national incidence study of child abuse and neglect (NIS-4): Report to congress. Washington, DC: US Department of Health and Human Services, Administration for Children, Youth and Families. [Google Scholar]
- Shaw M, Lawlor DA, & Najman JM (2006). Teenage children of teenage mothers: Psychological, behavioural and health outcomes from an Australian prospective longitudinal study. Social Science & Medicine, 62(10), 2526–2539. doi: 10.1016/j.socscimed.2005.10.007. [DOI] [PubMed] [Google Scholar]
- Stith SM, Liu T, Davies LC, Boykin EL, Alder MC, Harris JM, … & Dees JEMEG (2009). Risk factors in child maltreatment: A meta-analytic review of the literature. Aggression and Violent Behavior, 14(1), 13–29. doi: 10.1016/j.avb.2006.03.006. [DOI] [Google Scholar]
- Tandon M, Cardeli E, & Luby J (2009). Internalizing disorders in early childhood: A review of depressive and anxiety disorders. Child and Adolescent Psychiatric Clinics, 18(3), 593–610. doi: 10.1016/j.chc.2009.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toth SL, & Manly JT (2011). Bridging research and practice: Challenges and successes in implementing evidence-based preventive intervention strategies for child maltreatment. Child Abuse & Neglect, 35(8), 633–636. doi: 10.1016/j.chiabu.2011.05.003. [DOI] [PubMed] [Google Scholar]
- Toth SL, Petrenko CLM, Gravener Davis J, & Handley ED (2016). Chapter 16: Advances in prevention Science: A developmental psychopathology perspective. In Cicchetti D, (Ed.). Developmental Psychopathology (Vol. 4). New York: Wiley. [Google Scholar]
- U.S. Preventive Services Task Force. (2018). Perinatal depression: Preventive interventions. Retrieved from: https://www.uspreventiveservicestaskforce.org/Page/Document/draftrecommendation-statement/perinatal-depression-preventive-interventions
- Valentino K (2017). Relational interventions for maltreated children. Child Development, 88(2), 359–367. doi: 10.1111/cdev.12735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang YP, & Gorenstein C (2013). Psychometric properties of the Beck Depression Inventory—II: A comprehensive review. Revista Brasileira de Psiquiatria, 35, 416–431. doi: 10.1590/1516-4446-2012-1048. [DOI] [PubMed] [Google Scholar]