Abstract
Researchers have proposed numerous factors that may contribute to rural adolescents’ heightened risk for tobacco use. Some of these include well-known risk factors for tobacco use, whereas others concern factors unique to rural populations, reflecting norms and values (“rural culture”) that accept and encourage tobacco use. This study aimed to test a broad range of tobacco-use risk factors to determine which were a) universal risk factors for both urban and rural adolescents vs. b) unique risk factors for rural adolescents. Data came from a prospective cohort study of 1,220 adolescent males in Ohio who were aged 11-16 (average = 14 years) when surveyed at baseline (2015-2016). Follow-up surveys occurred every 6 months. The present study examined tobacco-use outcomes—prevalent use and incident use—by the two-year follow-up (2017-2018). Findings indicated a higher prevalence of ever-use of cigarette and smokeless tobacco among rural, vs. urban, adolescents at baseline. By the two-year follow-up, the urban/rural difference was attenuated but remained. Stratified multivariable logistic regression indicated that some baseline risk factors were associated with subsequent tobacco use for both rural and urban adolescents. Having an adult tobacco user in the home (for prevalent use) and susceptibility to a male family member offer of tobacco products (for both prevalent and incident use) were associated with tobacco use only for rural adolescents. These findings align with qualitative work demonstrating that masculinity and an intergenerational tobacco culture are important to male adolescents. This unique rural profile should be considered when developing prevention efforts.
Introduction
Rural residency in the United States (U.S.) remains an important risk factor for tobacco use. Research with adults indicates that rural areas of the U.S. have an elevated prevalence of tobacco use, especially for products like cigarettes and smokeless tobacco.1,2 Moreover, this urban/rural difference in adult tobacco use appears to have expanded in the past decade3 and is present regardless of poverty level.1,2 Research with adolescents is less established, but generally indicates a similar pattern, such that rural adolescents have a higher prevalence of tobacco use than their urban counterparts.4–7 There is also some evidence that, compared to urban adolescents, rural adolescents begin using tobacco products at younger ages.4,8 Given that the majority of tobacco initiation begins during adolescence,9 addressing tobacco use among rural adolescents is essential to prevention. It is therefore critical to better understand why rural residency puts adolescents at risk for tobacco use. Only by better understanding this heightened rural risk can prevention efforts be modified or developed to be maximally impactful for rural adolescents.
Researchers have proposed numerous factors that may be contributing to rural adolescents’ risk for tobacco use. Some of these include well-known risk factors for tobacco use, such as low socioeconomic status (SES) and exposure to tobacco retail marketing. Such factors are not only well-established as predictors of adolescent tobacco initiation for the overall population, but they also tend to be more prevalent/heightened in rural populations.10–12 Research has additionally proposed that rural populations have risk factors that are unique to them, such that “rural culture” can be considered a social determinant of health.13 According to this perspective, there are distinct norms and values in rural communities, sometimes embedded in a history of growing tobacco,14 that accept and encourage tobacco use and other health-risk behaviors. Supporting this notion is the well-established finding that pro-tobacco norms within a family or broader culture promote the initiation and use of tobacco.15 Such contextual risk factors could, in addition, shape individual traits. For example, delay discounting (the preference for smaller, sooner rewards over larger, delayed rewards) is one of the three dimensions of impulsivity that has been associated with tobacco use among youth,16–18 yet it has not received much attention for its relation to urban/rural differences.
Despite these developing theories on rural adolescent tobacco use, the data to support them is still emerging. Much of the research on rural adolescent tobacco use has included only rural populations.14,19–21 These studies, which are often qualitative, are crucial for gaining in-depth information about the perceptions and behaviors of rural individuals. However, the lack of a non-rural comparison group prevents researchers from identifying risk factors that may be unique for rural adolescents. Conversely, the studies that have compared urban and rural adolescents5,22 primarily focused on basic demographic characteristics and risk factors (e.g., marketing exposure). Such an approach overlooks the potential role of social and cultural factors as determinants of health behavior.
The purpose of the present study was to merge these two areas of rural research (i.e., investigations of cultural factors vs. urban/rural comparisons), in order to better understand why rural residency puts adolescents at risk for tobacco use. Specifically, we aimed to test a broad range of tobacco-use risk factors among a sample of urban and rural adolescents in order to determine which were a) universal risk factors for both urban and rural adolescents vs. b) unique risk factors for rural adolescents. Given that the largest urban/rural disparities are often reported for smokeless tobacco, which is primarily used among men,2 the present study focused on male adolescents.
Methods
Participants
Data came from The Buckeye Teen Health Study, a prospective cohort study of 1,220 adolescent males who were between ages 11 and 16 at baseline. The original focus of this study was smokeless tobacco use, which is why only males were enrolled. Individuals were recruited from Franklin County, Ohio (where the city of Columbus is located) and nine rural Ohio Appalachian counties (Figure 1). Two methods were used to recruit the sample. First, we used address-based sampling (ABS), a probability sampling method that uses the U.S. Postal Service’s address list to select households. Second, we used convenience sampling methods: We placed advertisements in local papers, attended community events, posted flyers at youth-oriented locations, and performed snowball sampling.
Figure 1.
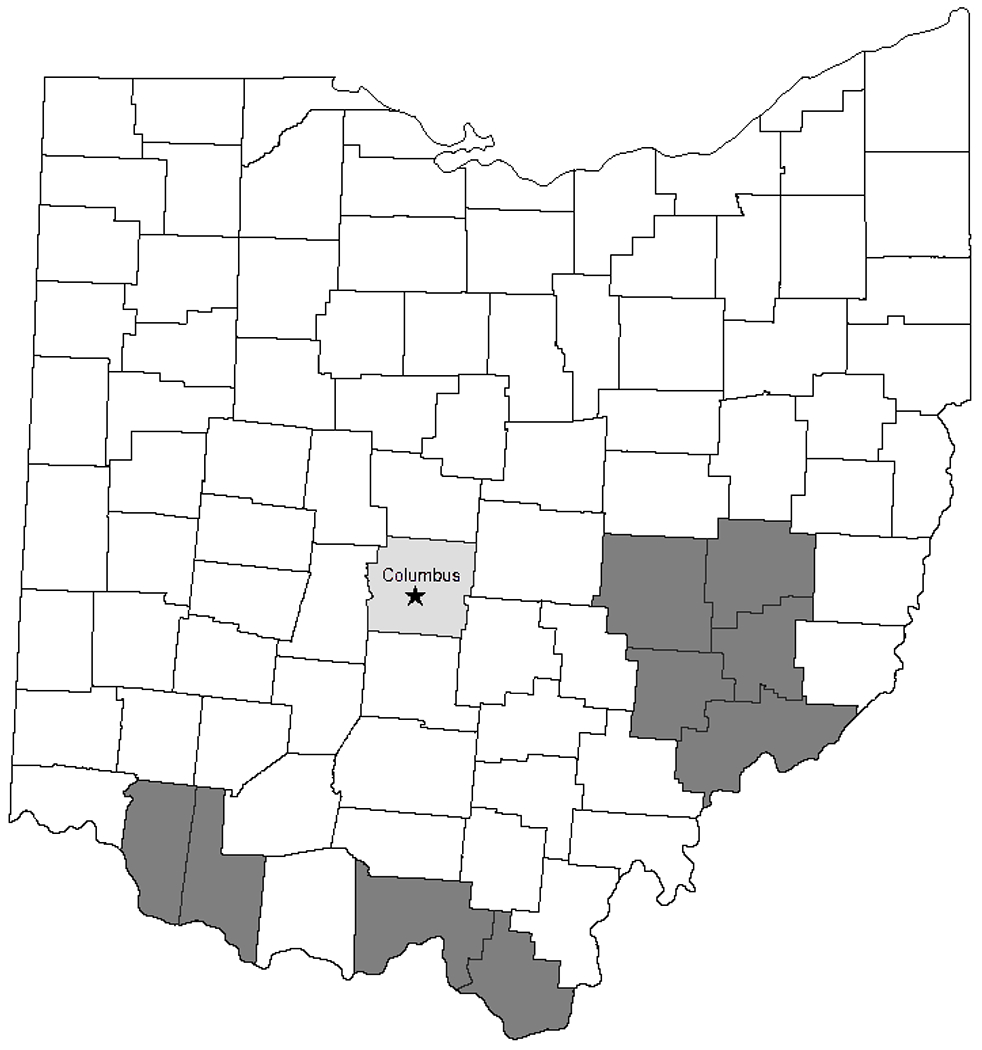
Map of Ohio counties, with shading indicating the counties from which the adolescents were recruited. The light grey indicates Franklin County (where the city of Columbus is located). All darker-shaded counties are the designated rural Appalachian counties that were sampled.
Procedures
Prior to the start of the study, the Institutional Review Board at our University approved the protocol. Each eligible household was contacted by a trained interviewer, who lived in the same region as the participants, to set up a meeting time, obtain informed permission and assent for the study, and complete the baseline session.
The baseline survey was administered in the home or at a public location, such as a library, in 2015 and 2016. Sensitive items, such as those about tobacco use, were asked using an audio-administered format. Less sensitive items were asked by the interviewer. At baseline, parents or guardians were also asked questions about their tobacco use, family income, level of education, and household smoking rules. Follow-up surveys were conducted every 6 months by telephone. After two years (2017 and 2018), another in-person assessment that was nearly identical to the baseline interview was completed in the participant’s home or at a public location.
Measures
Outcome Variable.
Our assessment of adolescent tobacco use was based on PATH items and skip patterns.23 At baseline and every follow-up survey, participants were asked about their ever use of the following tobacco products: cigarettes, smokeless tobacco, cigars/cigarillos, e-cigarettes, pipes, bidis, kreteks, and hookah. Our primary outcome of interest was use at the two-year follow-up. Participants who reported ever use to any of the aforementioned products at any follow-up survey were coded as “ever users” and all other participants were coded as “never users.” Participants who were never users at baseline but ever users at any follow-up survey were coded as “incident users.”
Risk Factors:
The urban/rural variable was assessed upon sampling and was based on whether the participant resided in Franklin County vs. Appalachian Ohio. From the parent baseline survey, we assessed whether there was an adult (i.e., someone over age 18) in the home who used tobacco; parent relationships (whether the parent had lived with ≤1 vs. >1 romantic partners within the last 5 years); and whether there were any rules about smoking inside the home (yes/no).
From the adolescent baseline survey, we assessed deviant/antisocial behavior (dichotomized as any vs. no deviant behaviors reported);24 sensation seeking (1-5 scale, where higher scores indicate greater liking of high-sensation experiences, like doing frightening things);25 delay discounting (assessed with a delay discounting choice task,26 which produces a k value, where higher log-transformed k values reflect a preference for more immediate reinforcers at the expense of larger but delayed reinforcers, or more impulsive behavior); any peer use of tobacco (yes/no); perceived harm of using cigarettes, e-cigarettes, and smokeless tobacco (aggregated into a single 0-10 risk perception variable, where higher scores indicate greater perceived risk); and their prototype/social image of a smoker (0-10 scale, where higher scores indicate more positive prototypes/social images of the typical same-aged peer who uses tobacco)27,28 Two items designed to assess the intergenerational culture surrounding tobacco use (“If a male family member were to offer you a cigarette[smokeless tobacco], would you smoke it?”) were also aggregated to provide a measure of susceptibility to a family member’s offer. Finally, our proxy for exposure to point-of-sale advertising was assessed by asking participants how many times in the past week they had visited various retailers (convenience stores, grocery stores, etc.) that evidence indicates have a high probability of selling tobacco.12
Demographic variables for these male participants included age, race/ethnicity (dichotomized as White non-Hispanic vs. other race/ethnicity for the present analyses), parent-reported parental education (≤ high school or GED vs. above high school/GED) and parent-reported household income (<$50,000 vs. $50,000 or more).
Statistical Analysis
All analyses were survey-weighted to reflect the sampling design; details about weighting procedures are provided elsewhere.29 In brief, we first generated weights for the ABS (probability-based) sample; we next calibrated weights for the convenience (non-probability) sample based on key covariates and combined them with the probability sample; finally, we trimmed the weights to stabilize estimates. Our analyses began with descriptive statistics to examine the prevalence of tobacco use by urban and rural residence at both baseline and by the two-year follow-up. We then used univariate logistic regressions, stratified by urban/rural status, to model the unadjusted association between baseline risk factors and (1) ever-use of tobacco and (2) incident tobacco use by the two-year follow-up survey. Finally, we entered all variables that were statistically significant in the univariate analyses into multivariable regressions to estimate the adjusted effects. Using model comparison methods recommended for complex survey data,30 we rechecked for the univariate variables with “borderline” p-values (0.05 < p < 0.2) by adding them sequentially. Thus, some “marginal” variables from the univariate analyses remained in the final multivariable models if they altered the other coefficients in the model and improved model fit. Participants who did not complete any follow-up surveys (i.e., those who only participated at baseline) were excluded from the logistic regression analyses (n = 325).
Results
At baseline, our male participants were an average of 14.1 years of age and 74.3% were Non-Hispanic White. Among the rural adolescents (n = 512), 46.5% had parents reporting incomes below $50,000 and 40.6% had an adult tobacco user living in their home. Among the urban adolescents (n = 708), 28.2% had parents reporting incomes below $50,000 and 25.4% had an adult tobacco user in the home. For the overall sample, 74.0% of participants completed at least one follow-up survey by the two-year follow-up period. Those missing data at the two-year follow-up (vs. those with data) were more likely at baseline to be non-White, from rural areas, somewhat older, and of lower socioeconomic status. Moreover, they were more likely to live with adult tobacco users, live in homes where smoking was allowed, have peers who use tobacco, have lower risk perception, and have higher exposure to point-of-sale advertising.
Table 1 presents the weighted prevalence of ever use of tobacco—both overall, and for specific products—for the participants at baseline and by the two-year follow-up. At baseline, prevalence values were generally higher among rural vs. urban adolescents. The difference was especially pronounced for smokeless tobacco, which was over five times as high among rural adolescents than urban adolescents (12.4% vs. 2.4%, respectively). Ever use of any tobacco product was nearly 23% among rural adolescents and under 14% among urban adolescents at baseline. However, by the two-year follow-up, the urban/rural difference had attenuated. Specifically, although substantial urban/rural differences remained for smokeless tobacco, differences for cigarettes and cigars/cigarillos were less pronounced; e-cigarette use had even become (non-significantly) higher among the urban adolescents. Ever use of any tobacco product was nearly 30% among the rural adolescents and over 24% among the urban adolescents at the two-year follow-up.
Table 1.
Weighted prevalence of the ever-use of various tobacco products (at baseline and by the two-year follow-up) and demographic characteristics among the adolescent males, separated by rural vs. urban residency (N = 512 and 708, respectively, at baseline).
| Tobacco Use Behavior | Rural % | Urban % |
|---|---|---|
| Ever-Use at Baseline | ||
| All tobacco products* | 23.0 | 13.9 a |
| Cigarettes | 11.2 | 6.7 a |
| Smokeless Tobacco | 12.4 | 2.4 a |
| Cigars/Cigarillos | 7.3 | 5.7 |
| e-Cigarettes | 13.0 | 7.0 a |
| Ever-Use by Two Year Follow-Up | ||
| All tobacco products* | 29.6 | 24.2 |
| Cigarettes | 12.5 | 11.1 |
| Smokeless Tobacco | 14.4 | 3.4 a |
| Cigars/Cigarillos | 13.2 | 11.2 |
| e-Cigarettes | 16.1 | 16.6 |
| Race | ||
| White | 91.3 | 63.5 a |
| Non-white | 8.7 | 36.5 |
| Parental Education | ||
| Some college or above | 75.5 | 88.0 a |
| High school or less | 24.5 | 12.0 |
| Household Income | ||
| $50,000 or more | 54.7 | 68.9 a |
| Less than $50,000 | 45.3 | 31.1 |
“All tobacco products” includes cigarettes, smokeless tobacco, cigars/cigarillos, e-cigarettes, pipes, bidis, kreteks, and hookah.
Chi-square values indicate a statistically significant urban/rural difference in prevalence (p-value < 0.05).
Weighted univariate logistic regressions showed that numerous factors assessed at baseline were predictive of ever-use by the two-year follow-up, although the particular factors differed somewhat for rural vs. urban adolescents (Table 2). When these factors were included in a weighted multivariable logistic regression, six factors were related to a greater odds of rural tobacco use: older age, having an adult tobacco user in the home, susceptibility to a male family member’s offer, any deviant behavior, higher delay discounting (i.e., more impulsivity), and more positive smoker prototypes (Table 4). For urban adolescents, predictors were older age, any deviant behavior, higher sensation seeking, and any peer use.
Table 2.
Odds ratios and 95% confidence intervals (CIs) for weighted univariate logistic regressions testing predictors of prevalent ever-use of any tobacco product by two-year follow-up stratified by region.
| Prevalent any tobacco ever-use by two years | |||||||
|---|---|---|---|---|---|---|---|
| Variable | Rural | Urban | |||||
| Mean (SD)/% | OR | 95% CI | Mean (SD)/% | OR | 95% CI | ||
| Age | 14.69 (0.19) | 1.62 | 1.36-1.92 | 14.79 (0.23) | 1.56 | 1.32-1.83 | |
| Race | |||||||
| White | 97.0 | Ref | - | 43.2 | Ref | - | |
| Non-white | 3.0 | 1.98 | 0.67-5.88 | 56.8 | 1.01 | 0.60-1.70 | |
| Parent Education | |||||||
| Some college or above | 74.3 | Ref | - | 16.8 | Ref | - | |
| High school or less | 25.7 | 1.17 | 0.58-2.14 | 83.2 | 1.36 | 0.62-3.01 | |
| Household Income | |||||||
| $50,000 or more | 51.2 | Ref | - | 50.0 | Ref | - | |
| Less than $50,000 | 48.8 | 1.03 | 0.59-1.77 | 50.0 | 2.07 | 1.22-3.50 | |
| Parent Relationships | |||||||
| 0-1 | 97.3 | Ref | - | 80.2 | Ref | - | |
| > 1 | 2.8 | 1.65 | 0.38-7.27 | 19.8 | 3.67 | 1.2-11.17 | |
| Adult user in the house | |||||||
| Yes | 35.3 | 2.28 | 1.30-3.99 | 23.7 | 1.42 | 0.81-2.50 | |
| No | 64.7 | Ref | - | 76.3 | Ref | - | |
| Household smoking rules | |||||||
| Smoking allowed/no rules | 24.2 | 1.78 | 0.89-3.54 | 19.3 | 1.64 | 0.88-3.07 | |
| Smoking not allowed | 75.8 | Ref | - | 80.7 | Ref | - | |
| Male family member offer | |||||||
| Yes (susceptible) | 33.1 | 5.37 | 2.59-11.50 | 30.0 | 1.97 | 1.03-3.74 | |
| No (not susceptible) | 66.9 | Ref | - | 70.0 | Ref | - | |
| Peer use | |||||||
| Yes | 48.28 | 4.03 | 2.20-7.39 | 61.8 | 5.25 | 2.94-9.36 | |
| No | 51.72 | Ref | - | 38.2 | Ref | - | |
| Any deviant behavior | |||||||
| Yes | 85.2 | 3.02 | 1.52-5.99 | 98.8 | 8.22 | 3.94-17.15 | |
| No | 14.8 | Ref | - | 1.2 | Ref | ||
| Mean sensation seeking | 3.20 (0.14) | 1.56 | 1.011-2.19 | 3.31 (0.09) | 2.34 | 1.70-3.28 | |
| Delay discounting (log-transformed K-score) | −4.01 (0.30) | 1.18 | 1.02-1.38 | −3.88 (0.14) | 1.13 | 1.01-1.27 | |
| Risk perceptions | 7.57 (0.25) | 0.81 | 0.67-0.94 | 6.80 (0.23) | 0.83 | 0.73-0.94 | |
| Smoking prototypes | 1.31 (0.29) | 1.28 | 1.06-1.54 | 2.06 (0.35) | 1.19 | 1.03-1.38 | |
| Exposure to POS advertising | 4.95 (0.42) | 1.04 | 0.97-1.12 | 5.18 (0.79) | 1.09 | 1.03-1.16 | |
Table 4.
Adjusted odds ratios and 95% confidence intervals (CIs) for weighted logistic regressions testing predictors of prevalent ever-use of any tobacco product by two-year follow-up by region.
| Prevalent any tobacco ever-use by two years | |||||
|---|---|---|---|---|---|
| Variable | Rural | Urban | |||
| OR | 95% CI | OR | 95% CI | ||
| Age | 1.56 | 1.25-1.94 | 1.32 | 1.09-1.61 | |
| Race | |||||
| White | -- | -- | -- | -- | |
| Non-white | |||||
| Parent Education | |||||
| Some college or above | -- | -- | -- | -- | |
| High school or less | |||||
| Household Income | |||||
| $50,000 or more | -- | -- | 1.90 | 0.99-3.64 | |
| Less than $50,000 | |||||
| Parent Relationships | |||||
| 0-1 | -- | -- | -- | -- | |
| > 1 | |||||
| Adult user in the house | |||||
| Yes | 2.45 | 1.15-5.22 | -- | -- | |
| No | Ref | - | |||
| Household smoking rules | |||||
| Smoking allowed/no rules | -- | -- | -- | -- | |
| Smoking not allowed | |||||
| Male family member offer | |||||
| Yes (susceptible) | 4.07 | 1.70-9.71 | -- | -- | |
| No (not susceptible) | Ref | - | |||
| Peer use | |||||
| Yes | -- | -- | 2.45 | 1.26-4.78 | |
| No | - | - | |||
| Any deviant behavior | |||||
| Yes | 2.52 | 1.16-5.46 | 4.05 | 1.77-9.29 | |
| No | Ref | - | Ref | - | |
| Mean sensation seeking | -- | -- | 1.85 | 1.27-2.69 | |
| Delay discounting (log-transformed K-score) | 1.24 | 1.01-1.54 | -- | -- | |
| Risk perceptions | -- | -- | -- | -- | |
| Smoking prototypes | 1.29 | 1.02-1.64 | -- | -- | |
| Exposure to POS advertising | -- | -- | -- | -- | |
-- Indicates where a variable was not included in the multivariable model due to it not being significant in the univariate model.
In terms of predicting incident use by the two-year follow-up, weighted univariate logistic regressions similarly showed that numerous factors were predictive for rural and urban adolescents (Table 3). The weighted multivariable logistic regression then indicated that older age, susceptibility to a male family member’s offer, and worse delay discounting were associated with greater odds of initiating tobacco use among rural adolescents (Table 5). Among urban adolescents, predictors were older age, any deviant behavior, and lower risk perceptions.
Table 3.
Odds ratios and 95% confidence intervals (CIs) for weighted univariate logistic regressions testing predictors of incident ever-use of any tobacco product by two-year follow-up stratified by region.
| Incident tobacco ever-use by two-years | |||||||
|---|---|---|---|---|---|---|---|
| Variable | Rural | Urban | |||||
| Mean (SD)/% | OR | 95% CI | Mean (SD)/% | OR | 95% CI | ||
| Age | 14.64 (0.22) | 1.61 | 1.28-2.01 | 14.56 (0.22) | 1.49 | 1.21-1.83 | |
| Race | |||||||
| White | 92.2 | Ref | - | 71.4 | Ref | - | |
| Non-white | 7.8 | 1.24 | 0.38-4.06 | 28.6 | 1.34 | 0.68-2.65 | |
| Parent Education | |||||||
| Some college or above | 80.0 | Ref | - | 91.7 | Ref | - | |
| High school or less | 20.0 | 0.92 | 0.37-2.29 | 8.3 | 0.89 | 0.31-2.60 | |
| Household Income | |||||||
| $50,000 or more | 68.6 | Ref | - | 68.4 | Ref | - | |
| Less than $50,000 | 31.4 | 0.65 | 0.31-1.40 | 31.6 | 1.41 | 0.71-2.80 | |
| Parent Relationships | |||||||
| 0-1 | 3.9 | Ref | - | 97.6 | Ref | - | |
| > 1 | 96.1 | 2.00 | 0.23-17.52 | 2.4 | 0.82 | 0.12-5.52 | |
| Adult user in the house | |||||||
| Yes | 46.1 | 2.04 | 0.95-4.41 | 33.8 | 1.78 | 0.91-3.50 | |
| No | 53.9 | Ref | - | 66.2 | Ref | - | |
| Household smoking rules | |||||||
| Smoking allowed/no rules | 12.6 | 1.05 | 0.39-2.89 | 23.4 | 1.80 | 0.83-3.91 | |
| Smoking not allowed | 87.4 | Ref | - | 76.6 | Ref | - | |
| Male family member offer | |||||||
| Yes (susceptible) | 16.4 | 3.12 | 1.17-8.31 | 15.3 | 1.34 | 0.59-3.05 | |
| No (not susceptible) | 83.6 | Ref | - | 84.7 | Ref | - | |
| Peer use | |||||||
| Yes | 26.9 | 2.30 | 1.01-5.26 | 25.1 | 2.45 | 1.17-5.17 | |
| No | 73.1 | Ref | - | 74.9 | Ref | - | |
| Any deviant behavior | |||||||
| Yes | 82.4 | 2.70 | 0.94-7.75 | 88.6 | 4.85 | 2.17-10.85 | |
| No | 17.6 | Ref | - | 11.4 | Ref | - | |
| Mean sensation seeking | 2.80 (0.15) | 1.20 | 0.80-1.81 | 3.08 (0.10) | 1.94 | 1.32-2.86 | |
| Delay discounting (log-transformed K-score) | −3.33 (0.23) | 1.41 | 1.12-1.79 | −3.91 (0.18) | 1.12 | 0.96-1.30 | |
| Risk perceptions | 7.63 (0.22) | 0.82 | 0.69-0.98 | 6.77 (0.25) | 0.83 | 0.71-0.97 | |
| Smoking prototypes | 0.97 (0.27) | 1.21 | 0.89-1.63 | 1.61 (0.27) | 1.12 | 0.94-1.34 | |
| Exposure to POS advertising | 4.58 (0.60) | 1.03 | 0.97-1.12 | 4.33 (0.49) | 1.07 | 1.00-1.15 | |
Table 5.
Adjusted odds ratios and 95% confidence intervals (CIs) for weighted logistic regressions testing predictors of incident ever-use of any tobacco product by two-year follow-up by region.
| Incident any tobacco ever-use by two years | |||||
|---|---|---|---|---|---|
| Variable | Rural | Urban | |||
| OR | 95% CI | OR | 95% CI | ||
| Age | 1.90 | 1.45-2.47 | 1.49 | 1.20-1.84 | |
| Race | |||||
| White | -- | -- | -- | -- | |
| Non-white | |||||
| Parent Education | |||||
| Some college or above | -- | -- | -- | -- | |
| High school or less | |||||
| Household Income | |||||
| $50,000 or more | -- | -- | -- | -- | |
| Less than $50,000 | |||||
| Parent Relationships | |||||
| 0-1 | -- | -- | -- | -- | |
| > 1 | |||||
| Adult user in the house | |||||
| Yes | 2.14 | 0.92-4.97 | -- | -- | |
| No | Ref | - | |||
| Household smoking rules | |||||
| Smoking allowed/no rules | -- | -- | -- | -- | |
| Smoking not allowed | |||||
| Male family member offer | |||||
| Yes (susceptible) | 3.39 | 1.22-9.42 | -- | -- | |
| No (not susceptible) | Ref | - | |||
| Peer use | |||||
| Yes | -- | -- | -- | -- | |
| No | |||||
| Any deviant behavior | |||||
| Yes | -- | -- | 3.36 | 1.45-7.83 | |
| No | Ref | - | |||
| Mean sensation seeking | -- | -- | 1.50 | 0.96-2.33 | |
| Delay discounting (log-transformed K-score) | 1.67 | 1.21-2.29 | -- | -- | |
| Risk perceptions | -- | -- | 0.80 | 0.66-0.98 | |
| Smoking prototypes | -- | -- | -- | -- | |
| Exposure to POS advertising | -- | -- | -- | -- | |
-- Indicates where a variable was not included in the multivariable model due to it not being significant in the univariate model.
Discussion
Consistent with the emerging research on rural adolescent tobacco use, the present study found that ever-use of tobacco was more prevalent among rural, compared to urban, adolescents in our study. These urban/rural differences were particularly pronounced for cigarette and smokeless tobacco use at baseline, where the participants were, on average, age 14 years. By the two-year follow-up, the urban/rural difference was attenuated. Thus, rural adolescent tobacco use in our sample was marked by an earlier age of onset (a finding that has likewise been found in other studies4,8). As nicotine exposure appears to influence the development of the adolescent brain,28 this has implications for long-term nicotine addiction among rural adolescents.
The primary objective of this study was to examine risk factors for adolescent tobacco use, in order to determine the extent to which use was predicted by a) universal risk factors and b) uniquely rural risk factors. Ultimately, our findings highlighted some universal risk factors. For example, our stratified multivariable logistic regression indicated that deviant behavior was associated with prevalent tobacco use by the two-year follow-up for both rural and urban adolescents. Yet we also found that having an adult tobacco user in the home (for prevalent use) and susceptibility to a male family member offer of tobacco products (for both prevalent and incident use) were only risk factors for rural adolescents in our study. Thus, although our variables assessing family influence are not measures of “rural culture” per se, our findings do provide some evidence that there are social and cultural factors that may be uniquely related to tobacco use for rural adolescent populations. These findings are consistent with work among adults, indicating that “rurality” is a unique tobacco-use risk factor that is not fully explained by differences in poverty or other risk factors.1,2 Findings also align with qualitative work demonstrating that masculinity and the intergenerational culture surrounding tobacco use are an important part of male adolescents’ tobacco culture.15 More broadly, it aligns with a well-documented kinship culture in Appalachia where the Appalachian family is cited as a critical influence on health behaviors of adults and adolescents.31–34
The fact that worse delay discounting (for prevalent and incident use) was also predictive only for the rural adolescents was an unexpected finding. As delay discounting is a measure of how much individuals value future outcomes, one possibility is that delay discounting reflects a culture of fatalism and less future orientation. It is also worth noting that, conversely, some risk factors like deviant behavior (for incident use) and sensation seeking (for both prevalent and incident use) were predictive only for the urban adolescents. It is possible that these factors were not predictive for rural youth because, in a culture where tobacco use is more normalized, youth tobacco use is not perceived to be as “deviant” and thus not exclusively sought by rebellious or high sensation-seeking youth. Such hypotheses require further exploration in future studies.
Strengths of this study include the relatively large, survey-weighted sample that was representative of urban and rural Appalachian adolescent males in our study counties. In addition, the study itself was able to assess many parent- and adolescent-reported risk factors for tobacco use at the individual, family, and environmental level. A limitation to this study was that it was not adequately powered to test multiple moderation effects, which would have allowed for direct urban-versus-rural comparison. Future studies with larger samples (i.e., several thousand participants) will be needed for such analyses. This study was also not designed to measure rural culture and how identification as a rural or Appalachian resident may influence tobacco use (particularly smokeless tobacco use). Attrition is an issue with all longitudinal studies, and despite using the proper statistical techniques (weighted analyses), bias cannot be ruled out; as participants without data at the two-year follow-up were more likely than those retained to be from rural areas and to have risk factors for rural tobacco use, it is possible that our findings underestimate true effects. Another important study limitation is that our sample was restricted to boys from Appalachia and we were not able to identify possible differences in predictive factors between in adolescents of differing genders or rural regions.
The higher prevalence of tobacco use among rural populations is a key contributor to many of the rural health disparities observed in the U.S. These urban/rural prevalence differences begin at an early age, and it is only by appropriately designing prevention efforts for rural adolescents that we can prevent the subsequent establishment of nicotine addiction and regular tobacco use by adulthood. Our findings highlight some of the risk factors that put rural adolescents at risk for tobacco use and initiation. This unique rural profile should be considered when developing prevention efforts both for the overall population, and for rural groups in particular.
Highlights.
Baseline ever-use of tobacco was higher among rural vs. urban adolescents (M age=14.1)
By the two-year follow-up, the urban/rural difference was attenuated but remained
Stratified multivariable analyses examined how risk factors predicted subsequent use
Only for rural was having an adult tobacco user in the home a risk factor
Only for rural was susceptibility to a male family member offer of tobacco a risk factor
Findings align with qualitative work on an intergenerational “rural culture”
Acknowledgments
Funding: This project was supported by NCI grant P50CA180908.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Roberts ME, Doogan NJ, Kurti AN, et al. Rural tobacco use across the United States: How rural and urban areas differ, broken down by census regions and divisions. Health & Place. 2016;39:153–159. doi: 10.1016/j.healthplace.2016.04.001 2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Roberts ME, Doogan NJ, Stanton CA, et al. Rural Versus Urban Use of Traditional and Emerging Tobacco Products in the United States, 2013–2014. Am J Public Health. 2017;107(10):1554–1559. doi: 10.2105/AJPH.2017.303967 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Doogan NJ, Roberts ME, Wewers ME, Stanton CA, Keith DR, Gaalema DE, Kurti AN, Redner R, Cepeda-Benito A, Bunn JY, Lopez A, & Higgins ST A growing geographic disparity: Rural and urban cigarette smoking trends in the United States. Under Review. Published online 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bernat DH, Choi K. Differences in Cigarette Use and the Tobacco Environment Among Youth Living in Metropolitan and Nonmetropolitan Areas. The Journal of Rural Health. 2018;34(1):80–87. doi: 10.1111/jrh.12194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gfroerer JC, Larson SL, Colliver JD. Drug Use Patterns and Trends in Rural Communities. The Journal of Rural Health. 2007;23 (s1): 10–15. doi: 10.1111/j.1748-0361.2007.00118.x [DOI] [PubMed] [Google Scholar]
- 6.Warren JC, Smalley KB, Barefoot KN. Recent Alcohol, Tobacco, and Substance Use Variations Between Rural and Urban Middle and High School Students. Journal of Child & Adolescent Substance Abuse. 2017;26(1):60–65. doi: 10.1080/1067828X.2016.1210550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wiggins AT, Huntington-Moskos L, Rayens EA, et al. Tobacco Use Among Rural and Urban US Middle and High School Students: National Youth Tobacco Survey, 2011–2016. The Journal of Rural Health. 2020;36(1):48–54. doi: 10.1111/jrh.12356 [DOI] [PubMed] [Google Scholar]
- 8.HarrelL JS, Bangdiwala SI, Deng S, Webb JP, Bradley C. Smoking initiation in youth: The roles of gender, race, socioeconomics, and developmental status. Journal of Adolescent Health. 1998;23(5):271–279. doi: 10.1016/S1054-139X(98)00078-0 [DOI] [PubMed] [Google Scholar]
- 9.USDHHS. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. 2014;Public Health Service, Office of the Surgeion General. [Google Scholar]
- 10.Byun S, Meece JL, Irvin MJ. Rural-Nonrural Disparities in Postsecondary Educational Attainment Revisited. Am Educ Res J. 2012;49(3):412–437. doi: 10.3102/0002831211416344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.USDA ERS - Geography of Poverty. Accessed December 17, 2016 https://www.ers.usda.gov/topics/rural-economy-population/rural-poverty-well-being/geography-of-poverty.aspx
- 12.Burgoon ML, Albani T, Keller-Hamilton B, et al. Exposures to the tobacco retail environment among adolescent boys in urban and rural environments. The American Journal of Drug and Alcohol Abuse. 2019;45(2):217–226. doi: 10.1080/00952990.2018.1549562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hartley D Rural Health Disparities, Population Health, and Rural Culture. Am J Public Health. 2004;94(10):1675–1678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nemeth JM, Liu ST, Klein EG, Ferketich AK, Kwan M-P, Wewers ME. Factors Influencing Smokeless Tobacco Use in Rural Ohio Appalachia. J Community Health. 2012;37(6):1208–1217. doi: 10.1007/sl0900-012-9556-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.US Department of Health and Human Services. Preventing tobacco use among youth and young adults: a report of the Surgeon General. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2012;3. [Google Scholar]
- 16.Barlow P, McKee M, Reeves A, Galea G, Stuckler D. Time-discounting and tobacco smoking: a systematic review and network analysis. Int J Epidemiol. 2017;46(3):860–869. doi: 10.1093/ije/dyw233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Reynolds B A review of delay-discounting research with humans: relations to drug use and gambling. Behavioural Pharmacology. 2006;17(8):651–667. doi: 10.1097/FBP.0b013e3280115f99 [DOI] [PubMed] [Google Scholar]
- 18.Reynolds B, Penfold RB, Patak M. Dimensions of impulsive behavior in adolescents: Laboratory behavioral assessments. Experimental and Clinical Psychopharmacology. 2008; 16(2): 124–131. doi: 10.1037/1064-1297.16.2.124 [DOI] [PubMed] [Google Scholar]
- 19.Couch ET, Darius E, Walsh MM, Chaffee BW. Smokeless Tobacco Decision-Making Among Rural Adolescent Males in California. J Community Health. 2017;42(3):544–550. doi: 10.1007/s10900-016-0286-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cultural Perspectives Concerning Adolescent Use of Tobacco and Alcohol in the Appalachian Mountain Region - Meyer - 2008 - The Journal of Rural Health - Wiley Online Library. Accessed January 31, 2020 https://onlinelibrary.wiley.eom/doi/full/10.1111/j.1748-0361.2008.00139.x [DOI] [PMC free article] [PubMed]
- 21.Hart JL, Walker KL, Sears CG, et al. The ‘state’ of tobacco: Perceptions of tobacco among Appalachian youth in Kentucky. Tob Prev Cessat. 2018;4. doi: 10.18332/tpc/81857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pesko MF, Robarts AMT. Adolescent Tobacco Use in Urban Versus Rural Areas of the United States: The Influence of Tobacco Control Policy Environments. Journal of Adolescent Health. 2017;61(1):70–76. doi: 10.1016/j.jadohealth.2017.01.019 [DOI] [PubMed] [Google Scholar]
- 23.Hyland A, Ambrose BK, Conway KP, et al. Design and methods of the Population Assessment of Tobacco and Health (PATH) Study. Tob Control. Published online August 8, 2016:tobaccocontrol-2016-052934. doi: 10.1136/tobaccocontrol-2016-052934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Barrera M, Biglan A, Ary D, Li F. Replication of a Problem Behavior Model with American Indian, Hispanic, and Caucasian Youth. The Journal of Early Adolescence. 2001. ;21 (2): 133–157. doi: 10.1177/0272431601021002001 [DOI] [Google Scholar]
- 25.Stephenson MT, Hoyle RH, Palmgreen P, Slater MD. Brief measures of sensation seeking for screening and large-scale surveys. Drug and Alcohol Dependence. 2003;72(3):279–286. doi: 10.1016/j.drugalcdep.2003.08.003 [DOI] [PubMed] [Google Scholar]
- 26.Kirby KN, MarakoviC NN, Delay-discounting probabilistic rewards: Rates decrease as amounts increase. Psychonomic Bulletin & Review. 1996;3(1): 100–104. doi: 10.3758/BF03210748 [DOI] [PubMed] [Google Scholar]
- 27.Gibbons FX, Gerrard M, Lane DJ. A social reaction model of adolescent health risk In: Suls J, Wallston KA, eds. Social Psychological Foundations of Health and Illness. Blackwell series in health psychology and behavioral medicine Blackwell Publishing; 2003:107–136. [Google Scholar]
- 28.Gerrard M, Gibbons FX, Stock ML, Lune LSV, Cleveland MJ. Images of Smokers and Willingness to Smoke Among African American Pre-adolescents: An Application of the Prototype/Willingness Model of Adolescent Health Risk Behavior to Smoking Initiation. J Pediatr Psychol. 2005;30(4):305–318. doi: 10.1093/jpepsy/jsi026 [DOI] [PubMed] [Google Scholar]
- 29.Friedman KL, Roberts ME, Keller-Hamilton B, et al. Attitudes toward Tobacco, Alcohol, and Non-Alcoholic Beverage Advertisement Themes among Adolescent Boys. Substance Use & Misuse. 2018;53(10):1706–1714. doi: 10.1080/10826084.2018.1429473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lewis T. Modeling complex survey data. Proceedings of the 2012 MidWest SAS Users Group Conference Published online 2012. [Google Scholar]
- 31.Keefe SE Appalachian family ties. Appalachian mental health. Published online 1988:24–35. [Google Scholar]
- 32.Elam C. Culture, Poverty and Education in Appalachian Kentucky. Education and Culture. 2002;18(1):10–13. [Google Scholar]
- 33.Coyne CA, Demian-Popescu C, Friend D. Social and Cultural Factors Influencing Health in Southern West Virginia: A Qualitative Study. Prev Chronic Dis. 2006;3(4). Accessed February 3, 2020 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1779288/ [PMC free article] [PubMed] [Google Scholar]
- 34.Gulley T The Effects of Fatalism, Faith and Family Dynamics on Health among Appalachian Youth. Public health in Appalachia: Essays from the clinic and the field [Google Scholar]


