Abstract
The State-Trait Anxiety Inventory — Trait version (STAI-T) was developed to measure an individual’s tendency to experience anxiety, but it may lack discriminant evidence of validity based on strong observed relationships with measures of depression. The present series of meta-analyses compares STAI-T scores among individuals with depressive disorders, anxiety disorders, and nonclinical comparison groups, as well as correlations with measures of anxiety and depressive symptom severity, in order to further examine discriminant and convergent validity. A total of 388 published studies (N = 31,021) were included in the analyses. Individuals with an anxiety disorder and those with a depressive disorder displayed significantly elevated scores on the STAI-T compared to nonclinical comparison groups. Furthermore, anxiety and depressive symptom severity were similarly strongly correlated with the STAI-T (mean r = .59 – .61). However, individuals with a depressive disorder had significantly higher STAI-T scores than individuals with an anxiety disorder (Hedges’s g = 0.27). Given these findings, along with previous factor analyses that have observed a depression factor on the STAI-T, describing the scale as a measure of ‘trait anxiety’ may be a misnomer. It is proposed that the STAI-T be considered a non-specific measure of negative affectivity rather than trait anxiety per se.
Keywords: STAI, trait anxiety, negative affectivity/neuroticism, meta-analysis, depression
Trait anxiety is an individual’s tendency to appraise situations as threatening, avoid anxiety-provoking situations, and demonstrate high baseline physiological arousal (Elwood et al., 2012). Early research identified trait anxiety as separate from, but likely contributing to, state anxiety (Cattell & Scheier, 1958; 1961; Spielberger, 1966), and ongoing research suggests that trait anxiety is an important vulnerability factor for anxiety-related psychopathology (Andrews, 1991; Eysenck, 1992; Rachman, 1998). The present review examines the cognitive, behavioral, physiological, and neural correlates of trait anxiety which may offer important insights into the mechanisms by which trait anxiety may increase vulnerability to the development and maintenance of anxiety-related psychopathology. Research evidence suggests that trait anxiety may also be associated with depression (Weger & Sandi, 2018), though the magnitude of this association is unclear.
Trait anxiety and related personality traits (negative affectivity, neuroticism, and dispositional negativity) have been extensively studied in the psychopathological literature. Barlow and colleagues (2014) suggest that trait anxiety is synonymous with neuroticism. Given these close ties, they suggest that both anxiety and depressive disorders share similar etiology and should be considered jointly under the category of emotional disorders. Operational definitions of trait anxiety have also been informed by consideration of psychological and neurobiological processes in animals and humans that contribute to a propensity to experience more frequent, intense, and/or enduring negative affect (dispositional negativity). Shackman and colleagues (2016) suggest that stable, indiscriminate, elevated negative affect is the most relevant to the development of psychopathology. In this model, trait anxiety is described as one component of anxious distress, one of two lower-level dimensions of dispositional negativity. Although the construct of trait anxiety has been a major component of etiological modes of anxiety-related disorders, much remains unknown about its measurement and associated mechanisms. The present review contributes to this broader literature by critically examining the cognitive, behavioral, and biological correlates of trait anxiety and its role in anxiety and depression, with a focus on studies that use the most commonly used measure, the State-Trait Anxiety Inventory (STAI; Spielberger et al., 1970, 1983).
What is Trait Anxiety? An Examination Across Multiple Levels of Analysis
Cognitive Correlates
Research on the cognitive mechanisms of trait anxiety suggests that individuals high in trait anxiety process and respond to threatening information differently than individuals low in trait anxiety. Trait anxiety is associated with an attentional bias toward threat (Bar-Haim et al., 2007) as well as an enhanced memory of threatening information (Mitte, 2008). Individuals high in trait anxiety also demonstrate impaired ability to inhibit distracting information, even under non-stressful conditions (Pacheco-Unguetti et al., 2010). Finally, individuals high in trait anxiety demonstrate lower cognitive flexibility, the ability to adapt one’s behavioral, emotional, and cognitive response to a situation in the face of new information (Martin & Rubin, 1995; Wang et al., 2019). In sum, individuals high in trait anxiety prioritize threatening information over non-threatening information and experience difficulty in adapting to new information. Similarly, cognitive neuroscience research has found that individuals high in trait anxiety have executive functioning and decision-making impairments even in the absence of direct threat (Basten et al., 2012; Bishop, 2009; Gawda & Szepietowska, 2016), which may predispose them to cognitive biases prevalent in anxiety and depressive disorders.
Behavioral Correlates
Anxiety-related behavior includes avoidance of perceived threat as well as a tendency to escape any situation perceived as threatening. Thus, it is reasonable to assume that individuals high in trait anxiety may display increased avoidance behavior in the laboratory. However, it is difficult to measure general avoidance in a laboratory setting. One reason is that avoidance behavior may be more characteristic of trait fear, conceptualized as an underactive fear extinction process, compared to trait anxiety, which is characterized by sustained hyperarousal and hypervigilance (Sylvers et al., 2011). Because many measures conflate trait fear and trait anxiety, important theoretical differences in these traits may be obscured in the literature (Lang et al., 2016; Sylvers et al., 2011). Although avoidance behavior may occur in trait anxious individuals, it is important to differentiate between avoidance of specific threats and avoidance of potential threats. The development of behavioral tasks that can measure responses to non-specific potential threats in the laboratory is necessary in order to more precisely examine behavioral correlates of trait anxiety.
Physiological Correlates
Given that hyperarousal is hypothesized to be a component of trait anxiety (Clark & Watson, 1991b; Sylvers et al., 2011), experimental research should demonstrate differential physiological responding between low trait-anxious and high trait-anxious individuals. Indeed, individuals high in trait anxiety demonstrate slower physiological recovery after a stressor (Calvo & Cano-Vindel, 1997; Willmann et al., 2012). Individuals with anxiety-related disorders typically show impaired fear learning in the form of increased fear acquisition or prolonged fear extinction (Mineka & Zinbarg, 2006). However, evidence of a differential physiological response to fear learning between individuals high and low in trait anxiety is mixed. Several studies have found that high trait anxiety is associated with impaired safety learning, as indexed by increased physiological responding to safety signals (Gazendam et al., 2013; Haddad et al., 2012). However, other studies have found no effect of trait anxiety on fear generalization, as measured by fear-potentiated startle and skin conductance response (Torrents-Rodas et al., 2013). Wong and Lovibond (2018) suggest that ambiguity is the key factor in increased physiological responding to safety signals. When individuals high in trait anxiety face a situation that may signal threat, they appear to demonstrate increased arousal compared to their non-anxious counterparts.
Neural Correlates
Trait anxiety is also associated with important differences in brain structure and function. For example, individuals high in trait anxiety have reduced thickness in the orbitofrontal cortex (Kühn et al., 2011), an area associated with extinction learning processes (Milad & Rauch, 2007), as well as reduced gyrification in the precuneus (Miskovich et al., 2016). Decreased gyrification and thickness may indicate less structural connectivity, and thus less efficient processing, in cortical areas (Laughlin & Sejnowski, 2003). Research suggests that activity in the bed nucleus of the stria terminalis (BNST) correlates with trait anxiety (Avery et al., 2016; Somerville et al., 2010). Neural activity in the ventromedial prefrontal cortex (vmPFC), one area centrally involved during emotion regulation, is negatively correlated with trait anxiety during fear conditioning (Marin et al., 2017). Taken together, individuals high in trait anxiety have both structural and functional differences in important cortical areas, which may impair their ability to regulate anxious responding under threat. This impairment may then confer vulnerability for the development of anxiety and related disorders.
Sociocultural Correlates
Trait anxiety may also have important sociocultural and demographic correlates that have important implications for the development of various forms of psychopathology. For example, women tend to score higher than men on the STAI-T, in both its nonclinical normative sample (Spielberger et al., 1983), and throughout the broader literature (McLean & Anderson, 2009). Gender differences in trait anxiety have been replicated in cross-cultural studies in Israel (Ben-Zur & Zeidner, 1988), Egypt, and Brazil (El-Zahhar & Hocevar, 1991). In fact, it may be the case that the gender differences in anxiety and depression may be partially explained by the gender differences in trait anxiety. Trait anxiety may also decline with age, though prospective studies are lacking. While age was not correlated with trait anxiety for neuropsychiatric patients in the STAI normative samples (Spielberger et al., 1983), a cross-sectional Japanese study found a linear decline in trait anxiety across a wide age range of adults (Nakazato & Shimonaka, 1989). Corresponding evidence suggests a decrease in anxiety and depressive disorder prevalence with age (Kessler et al., 2005), and decreases in neuroticism with age (Roberts et al., 2006). Because the majority of this research is cross-sectional in nature, some of these age-related differences in trait anxiety may be attributable to cohort effects. For example, in 1993, both adults and children in the United States endorsed significantly higher anxiety compared to adults and children in 1952 (Twenge, 2000). While self-reported trait anxiety increased worldwide from 1970 to 2010, these increases have not been observed in the United Kingdom and Australia, and increases in anxiety may be limited to students in the United States and Canada (Booth et al. 2016).
Cross-cultural differences in trait anxiety have also been observed. For example, trait anxiety scores were found to be higher among college students in the Philippines, Turkey, and Mexico compared to the United States (Baloglu et al., 2007). Additionally, high school students in Egypt reported higher trait anxiety compared to the United States and Brazil (El-Zahhar & Hocevar, 1991). A cross-cultural meta-analysis of trait anxiety, consisting of 116 samples in 24 countries, found a significant effect of country on trait anxiety, with country contributing about 31% of the variance in mean trait anxiety (Fischer & Boer, 2011). In their examination of potential explanatory variables, Fischer and Boer found that both greater wealth and greater individualism were associated with lower trait anxiety, though the relationship between wealth and trait anxiety appears to be mediated by individualism.
How Does Trait Anxiety Influence the Development of Anxiety and Depressive Disorders?
The available evidence suggests that trait anxiety may reflect a distinct pattern of responding across cognitive, behavioral, physiological, and neural levels of analysis. This pattern of responding may confer vulnerability for the development of anxiety and related disorders (Andrews, 1991; Eysenck, 1992; Rachman, 1998). As reviewed above, trait anxiety drives cognitive biases such as overestimation of threat, attention toward threat, increased perception of threat, and negative interpretations of threat (Figure 1). These biases lead to increased negative emotional experiences and maladaptive safety behaviors, which decrease immediate anxiety but maintain anxiety symptoms over the long term. For example, trait-anxious individuals may develop contamination fear if they overestimate the threat associated with contamination and interpret this threat as having a catastrophic outcome. These individuals would increasingly experience anxiety in the presence of contamination may develop specific behaviors, or compulsions, in order to reduce their anxiety in the short-term. However, these compulsions maintain the overestimation of threat and fear of contamination in the long-term, potentially leading to clinically significant symptoms of obsessive-compulsive disorder (OCD). Similarly, an individual high in trait anxiety who overestimates the threat of social evaluation, attends to others’ facial expressions and appraises them as negative and self-referential, and begins to avoid social situations may develop social anxiety disorder. Safety behaviors, such as avoidance and reassurance-seeking, reinforce cognitive biases as well as trait anxiety itself. Because trait anxiety has both stable and time-variant components (Cole et al., 2005; Olatunji & Cole, 2009; Steyer et al., 1989), occasion-specific behavioral factors may increase trait anxiety over time. A trait-anxious individual who learns that threat avoidance reduces short-term anxiety may deprive themselves of the opportunity to experience an expectancy violation that disconfirms their beliefs; over time, this individual may become increasingly anxious and avoidant as their beliefs about the nature of threat are reinforced.
Figure 1.
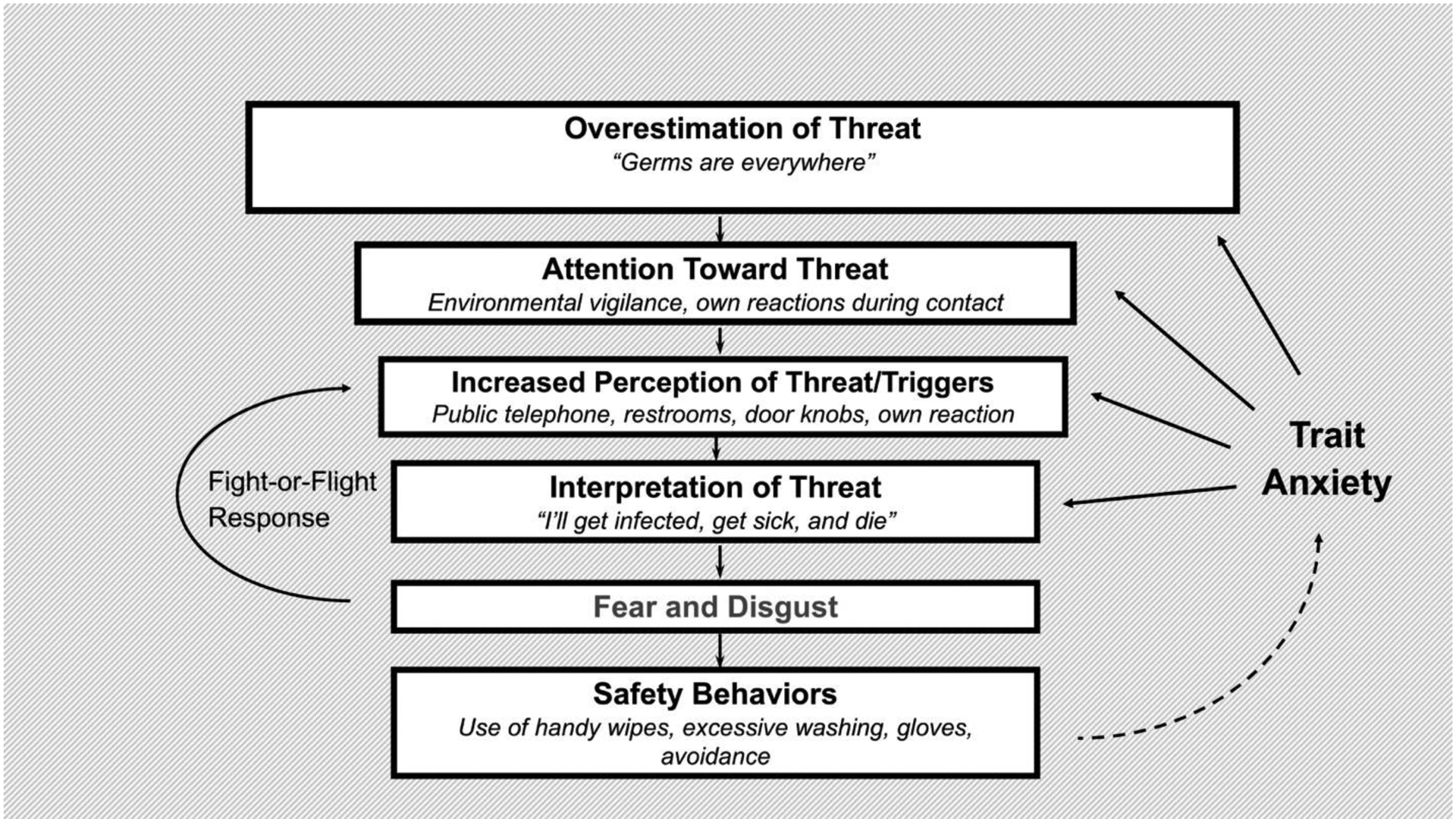
Conceptual model demonstrating how trait anxiety can lead to the development of OCD through cognitive and behavioral sequelae.
Trait Anxiety and Transdiagnostic Cognitive Vulnerabilities
Specific cognitive factors related to trait anxiety may explain how this underlying vulnerability may lead to the development of anxiety and depressive disorder symptoms. For instance, trait anxiety is strongly correlated with a tendency to overgeneralize, personalize, and catastrophize in both clinical and nonclinical groups (Muran & Motta, 1993); these cognitive distortions are a key contributing factor in the development and maintenance of anxiety and depressive disorders (Beck et al., 1979). Among individuals who had experienced a traumatic event, trait anxiety was strongly correlated with negative beliefs about the self, negative beliefs about the world, and self-blame (J. G. Beck et al., 2004; Foa et al., 1999). In a recent longitudinal study, negative metacognitive beliefs about the uncontrollability and danger of worry had a statistically significant bidirectional relation with trait anxiety, suggesting that trait anxiety both prospectively influenced and was influenced by negative metacognitive beliefs over an eight-week period (Nordahl et al., 2019). Thus, specific cognitive beliefs and biases are prevalent in individuals high in trait anxiety, which may in turn predispose these individuals to the development of psychopathology.
Trait anxiety is also associated with repetitive thinking, one cognitive mechanism associated with anxiety and depressive disorders (De Raedt et al., 2015). For example, trait anxiety has been linked with increased use of worry and decreased use of distraction (Wells & Carter, 2009). The relation between these thinking styles and trait anxiety was independent of GAD and major depressive disorder (MDD) diagnostic status, suggesting that particular thinking styles are unique determinants of trait anxiety. Similarly, trait anxiety is strongly associated with rumination, a form of repetitive negative thinking that focuses on symptoms of distress and their causes and consequences (Muris et al., 2005). Although a recent study found that repetitive negative thinking mediated the longitudinal relation between anxiety symptoms and depressive symptoms (Spinhoven et al., 2019), future studies should examine repetitive negative thinking as a potential mediator to test the hypothesized pathway from trait anxiety to later anxiety and depressive symptoms.
Finally, trait anxiety is associated with the proposed “fundamental fears”: anxiety sensitivity (the fear of anxiety symptoms and their potentially harmful consequences), illness/injury sensitivity (fears of injury, illness, and death), and fear of negative evaluation (distress associated with the expectations that others will evaluate oneself negatively; Reiss & McNally, 1985; Taylor, 1993). According to Reiss’s expectancy theory, fear reactions, such as panic attacks and phobias, can be attributed to these fundamental fears. In a factor analysis of measures of the fundamental fears, Taylor (1993) found that all three fundamental fears together contributed 41% of the variance in trait anxiety; fear of negative evaluation was moderately correlated with trait anxiety (r = .44), but zero-order relations between trait anxiety and both illness/injury sensitivity and anxiety sensitivity did not reach significance. Other studies have found statistically significant relations between anxiety sensitivity and trait anxiety (Taylor et al., 1991). Anxiety sensitivity is strongly associated with anxiety-related disorders (Naragon-Gainey, 2010); if anxiety sensitivity is a lower-order factor nested under trait anxiety (Lilienfeld et al., 1993; Olatunji & Wolitzky-Taylor, 2009), anxiety sensitivity may be one specific mechanism by which trait anxiety confers vulnerability for anxiety-related disorders. For example, while trait anxiety was associated with post-hyperventilation symptoms, it no longer significantly predicted post-hyperventilation symptoms when controlling for anxiety sensitivity (Rapee & Medoro, 1994). Similarly, in a sample of individuals high in anxiety sensitivity, trait anxiety was not significantly associated with panic attacks, anxiety diagnoses, or any clinical diagnosis at baseline or two years later, but anxiety sensitivity demonstrated a prospective relation with anxiety disorder incidence (Schmidt et al., 2006). Anxiety sensitivity may explain how an individual high in trait anxiety becomes sensitized to interpret physical symptoms of anxiety as threatening, conferring additional vulnerability for the development of a clinically significant anxiety-related disorder, especially in the case of panic disorder.
Trait Anxiety and Specific Anxiety Disorders
Elevated trait anxiety has been found in patients with panic disorder (Barlow, 1988; Muris et al., 2000), generalized anxiety disorder (GAD; Rapee, 1991), and social anxiety disorder (Amir et al., 2005) compared to healthy individuals. In fact, trait anxiety has been found to be associated with significantly greater odds of having an adult anxiety-related disorder even when controlling for the effects of childhood perceived stress (Mundy et al., 2015). In a study examining the specificity of disgust proneness, Muris and colleagues (1999) found that disgust proneness was correlated with a broad range of symptoms of anxiety-related disorders in children. However, results also indicated that these correlations were predominantly accounted for by trait anxiety. That is, when controlling for trait anxiety, only specific phobia symptoms and separation anxiety disorder symptoms were significantly related to disgust proneness. This finding suggests that trait anxiety underlies a broad number of childhood anxiety-related disorders and thus is an important indicator of early vulnerability for anxiety-related psychopathology. Although most studies linking trait anxiety to symptoms of anxiety-related disorders have been cross-sectional, prospective research has also examined this hypothesized causal link. For example, one such study examined patients from a GAD treatment trial 8 to 14 years after completing treatment (Chambers et al., 2004). The findings showed that pre-treatment trait anxiety was significantly correlated with the number of anxiety and depressive diagnoses at follow-up. However, after controlling for negative affect, only trait anxiety measured at long-term follow-up was significantly correlated with GAD and depression status, whereas pre-treatment trait anxiety was not. Despite its conceptualization as a stable vulnerability factor, measures of trait anxiety might also reflect current symptom severity. Although pre-treatment trait anxiety may predict comorbidity post-treatment, it does not appear to uniquely predict anxiety or depressive symptoms beyond negative affect.
Trait Anxiety and Obsessive-Compulsive Spectrum Disorders
Although obsessive-compulsive and related disorders are no longer classified with the anxiety disorders in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5; American Psychiatric Association, 2013) and the International Statistical Classification of Diseases and Related Health Problems (ICD-11; World Health Organization, 2020), evidence suggests that trait anxiety plays a significant role in obsessive-compulsive symptoms. Trait anxiety is elevated in OCD compared to both healthy individuals and to individuals with other anxiety-related disorders (Abramowitz et al., 2003). In particular, trait anxiety is significantly correlated with obsessions, but not compulsions, in OCD patients (McKay et al., 1995). Obsessions are a repetitive thought process and share features with worry and rumination, two other repetitive thinking styles that are associated with trait anxiety (Muris et al., 2005); compulsions are a set of behaviors typically performed to reduce the anxiety that arises from obsessions and are more specific to OCD than anxiety. Although there is an increased focus on the role of disgust in OCD, structural models confirm that trait anxiety remains a statistically significant predictor of obsessive-compulsive symptoms even when disgust proneness is included in the model (Olatunji et al., 2007). Finally, trait anxiety is also associated with hoarding symptoms (Tolin et al., 2011). This suggests that the stable tendency to experience negative emotions such as fears, worries, and anxiety across many situations may lead to a persistent difficulty discarding or parting with possessions because of a perceived need to save them.
Trait Anxiety and Trauma-Spectrum Disorders
The study of trauma-related disorders, including posttraumatic stress disorder (PTSD) and acute stress disorder, provides a unique opportunity to examine potential causal relations, as the experience of trauma is typically independent of premorbid trait anxiety. Several cross-sectional studies demonstrate a statistically significant relation between the experience of PTSD symptoms and trait anxiety (Casada & Roache, 2005; Orsillo et al., 1996). Trait anxiety is also correlated with acute stress disorder symptoms (Suliman et al., 2013). In two studies of children, trait anxiety was more predictive of PTSD symptom severity than the nature of the traumatic event itself, including severity of cancer diagnosis (Phipps et al., 2009) or strength of hurricane experienced (Lonigan et al., 1994). However, because these studies are cross-sectional in nature, they do not allow researchers to determine who may develop PTSD after a traumatic experience. A limited number of prospective studies attempt to answer this question. Trait anxiety, measured when patients received a cancer diagnosis, was significantly predictive of PTSD symptoms six months later (Kangas et al., 2005). Individuals high in trait anxiety, measured immediately after treatment for rectal cancer, were also more likely to endorse PTSD symptoms two to five years later (Ristvedt & Trinkaus, 2009). In a study following patients one and a half to four years after cardiac surgery, trait anxiety mediated the relation between stress exposure and PTSD, thus outlining a potential causal mechanism for how individuals who experience a stressful event later develop PTSD (Kok et al., 2016). In addition to studies of patients undergoing medical procedures, two other studies demonstrate prospective relations between trait anxiety and PTSD. For example, children’s trait anxiety measured before Hurricane Katrina predicted PTSD symptoms, as well as GAD and depression, after the hurricane (Weems et al., 2007). Finally, in a prospective study of college students who later experienced a campus shooting, anxiety sensitivity (one potential lower-order factor of trait anxiety) predicted PTSD symptoms (Boffa et al., 2016). However, given that trait anxiety itself was not specifically assessed, this study cannot differentiate between the prospective effects of trait anxiety and anxiety sensitivity on PTSD symptoms.
Trait Anxiety and Depression
Although trait anxiety refers to the stable tendency to attend to and experience fear, worry, and anxiety across many situations, there is increasing evidence that this personality trait may not be specific to anxiety-related disorders. While some studies have found comparable levels of trait anxiety in individuals with depression and anxiety-related disorders (Christopher & MacDonald, 2005), others find significantly higher trait anxiety in depressive compared to anxious clinical samples (Barlow et al., 1986; D’Avanzato et al., 2013; Power & Tarsia, 2007). In a recent study, trait anxiety was positively correlated with depression; rumination mediated the relation between trait anxiety and depressive symptoms, but cognitive flexibility buffered this association (Wang et al., 2019). This study demonstrates that the findings on cognitive biases and executive functioning impairment associated with trait anxiety, as described above, also influence depressive symptoms. Together, these findings question the extent to which trait anxiety is a vulnerability factor that is specific to anxious psychopathology.
Is Trait Anxiety a Nonspecific Vulnerability Factor?
A review of the literature suggests that trait anxiety may be implicated in both anxiety and depression as well as the cognitive factors that confer vulnerability for these disorders. This review suggests that trait anxiety may reflect a nonspecific vulnerability factor that is a product of a generalized vulnerability for anxiety and depression. For example, Clark and Watson (1991b) have argued for a tripartite model of anxiety and depression, suggesting that these disorders share a nonspecific distress factor at their core, in addition to the specific factors of hyperarousal (anxiety) and low positive affect (depression). This nonspecific distress factor has been described as negative affectivity/neuroticism, the general tendency to experience negative emotions (Watson & Clark, 1984). Negative affectivity/neuroticism is a key vulnerability factor in the development of psychopathology, of which trait anxiety may be a part (Clark et al., 1994). Although symptoms of psychopathology can change widely over time, negative affectivity/neuroticism is hypothesized to be a relatively stable construct, and measures of negative affectivity/neuroticism have high test-retest reliability over periods of years (Watson & Clark, 1984). Like trait anxiety, negative affectivity/neuroticism is a robust vulnerability factor for both anxiety and depressive disorders (Kotov et al., 2010; Shackman et al., 2016) and is associated with a biased information processing style that prioritizes safety (Van den Bergh et al., in press).
Trait Anxiety as an Indicator of Negative Affect
The existing research suggests that both trait anxiety and negative affectivity/neuroticism confer vulnerability for the development of anxiety-related disorders and depression. However, this may be because trait anxiety and negative affectivity/neuroticism are essentially the same construct. In fact, many researchers use the terms negative affectivity, neuroticism, and trait anxiety interchangeably. For example, in discussing the negative affect factor they derived within a clinically anxious sample, Zinbarg and Barlow (1996) noted:
Though these traits are defined slightly differently and given different labels in each of these models — harm avoidance (Cloninger), neuroticism (Eysenck), trait anxiety (Gray), behavioral inhibition (Kagan), and negative affectivity (Tellegen) — the conceptual and empirical overlap among these constructs far outweigh the differences.
(p. 181)
Similarly, Clark and Beck (2010) refer to trait anxiety and negative affectivity as “almost synonymous.” Further complicating this issue is how trait anxiety is often measured. Although there is a rich body of literature demonstrating the cognitive, behavioral, physiological, and neural correlates of trait anxiety, as well as its central role in both anxiety and depressive disorders, much of this research relies on the use of a single self-report measure of trait anxiety: the State-Trait Anxiety Inventory (STAI). While the STAI has a robust history, it also has a number of psychometric limitations that suggest that this widely used measure may not adequately capture the specific construct of trait anxiety.
Psychometric Properties of the State-Trait Anxiety Inventory (STAI)
Many specific measures of trait anxiety have been developed, including the Taylor Manifest Anxiety Scale (TMAS; Taylor, 1953), Adult Manifest Anxiety Scale (AMAS; Reynolds et al., 2003), Institute for Personality and Ability Testing (IPAT) Anxiety Scale (Krug et al., 1976), the Endler Multidimensional Anxiety Scales (EMAS; Endler et al., 1991), and the State-Trait Inventory for Cognitive and Somatic Anxiety (STICSA; Grös, et al., 2007). Similarly, a number of personality measures include trait anxiety scales, including the Revised NEO Personality Inventory (NEO PI-R; Costa & McRae, 1992), the HEXACO Personality Inventory-Revised (HEXACO-PI-R; Lee & Ashton, 2004, and the Jackson Personality Inventory-Revised (JPI-R; Jackson, 1994). However, the STAI is the most well-known and most cited measure of trait anxiety (Figure 2). The STAI has two subscales: state anxiety, measuring “subjective feelings of apprehension, ‘anxious’ expectation, and activation (arousal) of the autonomic nervous system” (STAI-S), and trait anxiety, measuring “individual differences in anxiety proneness” (STAI-T; Spielberger, 1966, p. 17). The STAI consists of 40 items, 20 for each subscale. Items are rated on a Likert scale from 1 (not at all/almost never) to 4 (very much so/almost always), and some items are reverse-scored. Individuals are asked to indicate how they feel “right now, at this moment” for the STAI-S and how they “generally feel” for the STAI-T.
Figure 2.
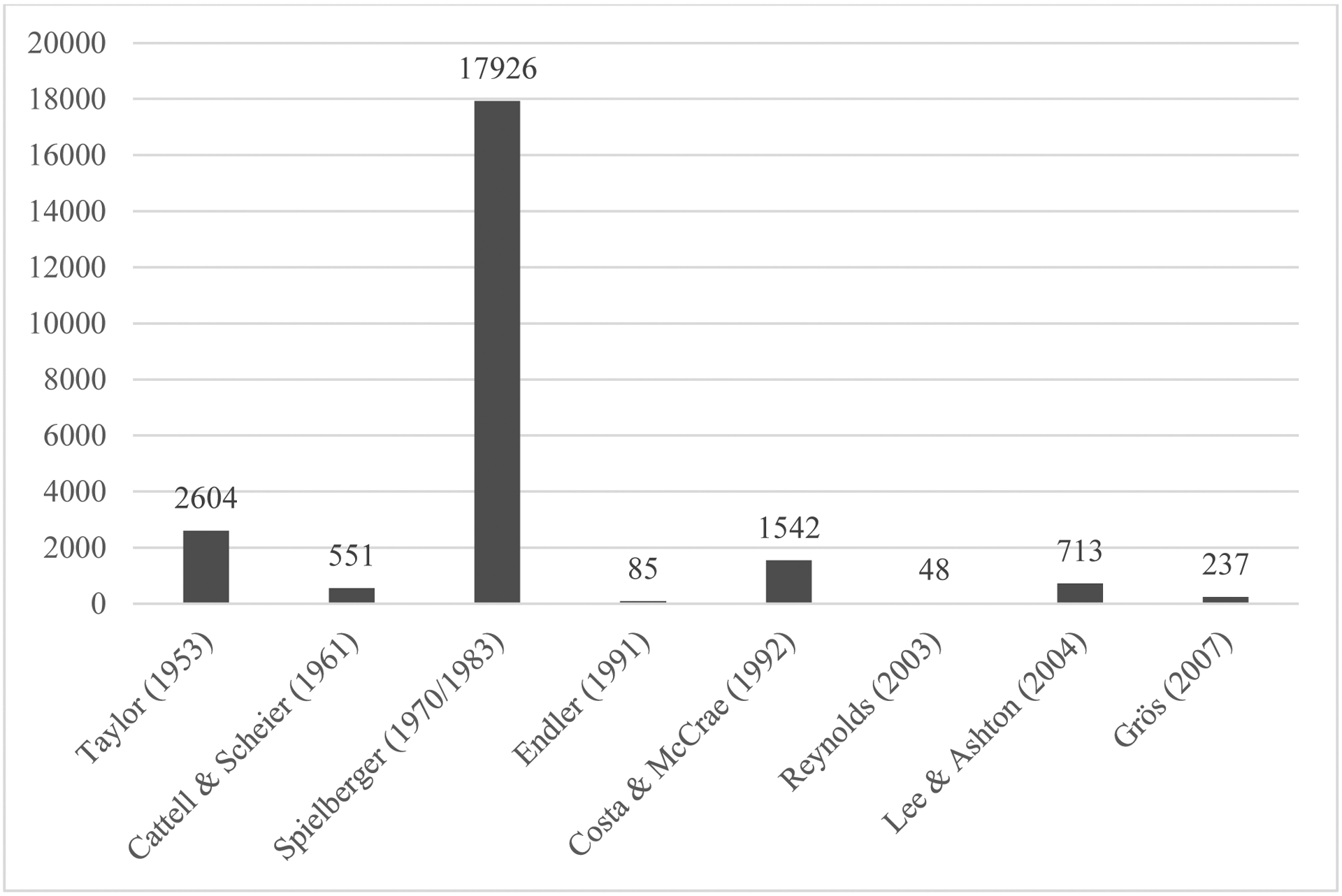
Total citations of trait anxiety measures
Source: Web of Science database search conducted March 30, 2020. Note: Costa & McRae (1992) references include only citations of the NEO-PI-R that mention anxiety; there are currently 11,109 total references citing the NEO-PI-R.
Initial reviews of the STAI were laudatory and praised the measure for being brief, inexpensive, and easy to administer, score, and interpret, with a thorough test manual (Hedberg, 1972). Although the STAI has been cited in over 31,000 articles and translated into 70 languages and dialects (Spielberger, 2010; Figure 2), it has not been without criticism for its psychometric properties. While the STAI-T demonstrated acceptable test-retest reliability in normative samples (.73 to .86; Spielberger, 1983), others have raised concerns. In an early examination, Kendall and colleagues (1976) noted that trait anxiety scores fluctuated significantly when measured across different situations, indicating poor reliability of the STAI-T. Similarly, Nixon and Steffeck (1977) found low to moderate test-retest reliability for the STAI-T in a sample of medical students across an 8 to 11-month period. A subsequent review found that the average test-retest reliability of the STAI-T was .88 across seven studies published from 1990 to 2000 (Barnes et al., 2002). Notably, however, the majority of studies using the STAI-T either do not include reliability information or only provide information on internal consistency. Similarly, few studies have examined measurement invariance, testing if the scale measures the same construct across different groups. One such study examined the STAI-T, Behavioral Inhibition Scale (BIS; Carver & White, 1994) and Fear Survey Schedule (FSS; Wolpe & Lang, 1964) among university students and community members and found evidence for distinct trait anxiety, behavioral inhibition, social fear, and tissue damage fear factors (Cooper et al., 2007). Within their sample, the model demonstrated configural invariance, full metric invariance, and scalar invariance across gender. Larger examinations of both test-retest reliability and measurement invariance across clinical populations, age groups, and nationalities are warranted.
The first published version of the STAI-T (Form X) contained six items that were “more closely related to depression than anxiety” (e.g., “I feel blue,” “I feel like crying”), leading to a subsequent revision and publication of Form Y (Spielberger, 2010; Spielberger et al., 1983). However, many published articles that have used the STAI do not specify which version of the measure was used. Furthermore, not all validated translations of the STAI use the revised Form Y; the widely used German version of the STAI is based on Form X (Laux et al., 1981). Despite efforts to revise the scale by considering items that allow for differentiation from depression, the STAI-T contains some items that do not clearly reflect a trait predisposition to the experience of anxiety; for example, items such as “I take disappointments so keenly that I can’t put them out of my mind” and “I am happy” (reverse-scored) seem to be more strongly related to a depressive state or a tendency to experience negative emotions more generally than to trait anxiety specifically. Indeed, there is concern that the STAI-T may not reliably discriminate between anxiety and depression. For example, Clark and Watson (1991b) examined four studies of over 1,600 non-clinical participants and found an average correlation of .65 between the STAI-T (Form X) and measures of depression, and an average correlation of .75 between the STAI-T and measures of anxiety. Among two studies of 281 clinical participants, the average correlation between the STAI-T and other anxiety measures reached r = .80, whereas the average correlation between the STAI and depression measures was r = .67. The strong correlation between the STAI-T and measures of depression indicates a lack of discriminant evidence of validity. In fact, some studies have even shown that the revised STAI-T (Form Y) more strongly correlates with measures of depression than with measures of anxiety. For instance, among Canadian patients with anxiety-related disorders, the STAI-T (Form Y) was strongly correlated with the Beck Depression Inventory (BDI; r = .72) and only moderately correlated with the Beck Anxiety Inventory (BAI; r = .42; Bieling et al., 1998). In a sample of Spanish students, the STAI-T (Form Y) was strongly correlated with measures of depression, rs = .62–.75, and moderately correlated with measures of anxiety, rs = .46–.61 (Bados et al., 2010). Similarly, Balsamo and colleagues (2013) found that the STAI-T (Form Y) was strongly correlated with the BDI-II in a large (N = 877) non-clinical sample of Italian adults (r = .70) and only moderately correlated with the BAI in a smaller subsample (N = 151, r = .61). Similarly, in their large clinical sample of Italian adults (N = 1124), correlations with the STAI-T were stronger with the BDI-II (r = .76) than with the BAI (r = .55).
Factor analytic studies have also called into question the anxiety-specific nature of the STAI. Although two subscales of the STAI are typically reported (STAI-T and STAI-S), the original factor analysis of the measure found that four factors best fit the data: state anxiety present, state anxiety absent, trait anxiety present, and trait anxiety absent (Spielberger et al., 1980). Items that load onto the “anxiety absent” factors include “I feel pleasant” and “I am calm;” their positive wording may indicate that these factors are detecting a method effect, in which reverse-scored items load onto separate factors. Indeed, a two-construct, two-method model appears to fit the measure better than both a four-factor model and a two-factor model (Vigneau & Cormier, 2008). Subsequent research by Bieling and colleagues (1998) found evidence for a hierarchical model of the STAI-T items consisting of a higher-order negative affect factor and two lower-order specific factors of depression and anxiety (named STAI-D and STAI-A). Regarding the two lower order-factors, one set of items appear to assess anxiety and worry, whereas the other items assess sadness and self-deprecation. Interestingly, the STAI-A subscale was found to be strongly correlated with both the BDI (r = .66) and the BAI (r = .50). Similarly, Bados and colleagues (2010) found that the STAI-A subscale was more strongly correlated with the depression subscales (rs = .49–.67) than with the anxiety subscales (rs = .43–.58) of three well-validated measures (BDI/BAI, DASS-21, SCL-90-R). Another factor analytic study in a French student sample found that a 3-factor solution best fit the data, corresponding to anxiety, “unsuccessfulness” or anhedonia, and happiness (Caci et al., 2003). This is further evidence that although the STAI-T is a popular measure of anxiety, it may assess depression as well as anxiety.
In fact, the STAI-T is highly correlated with measures of negative affectivity/neuroticism. Watson and Clark (1984) reported a correlation of r = .73 between the STAI-T and the Eysenck Personality Inventory Neuroticism scale in their seminal review of personality scales relevant to the construct of negative affectivity/neuroticism. Other clinical samples report similarly strong correlations (rs = .61–.86; Dammen et al., 2008; Luteijn & Bouman, 1988; Merino et al., 2016). One explanation for the high degree of overlap between the STAI-T and measures of negative affectivity/neuroticism is that the STAI-T does not actually measure a specific anxiety vulnerability factor. Rather, the evidence suggests that the STAI-T is a measure of the nonspecific distress factor that characterizes both anxiety-related disorders and depression in Clark and Watson’s tripartite model. Put another way, the STAI-T may not differentiate between anxiety-related disorders and depression because it measures general negative affectivity/neuroticism rather than the specific facet of trait anxiety.
Overview of the Present Meta-Analysis
The overall goal of this review is to evaluate the STAI-T and its association with both anxiety and depressive disorders using a meta-analytic approach. Meta-analysis is one tool by which validity evidence for a given test, such as the STAI, can be examined (American Educational Research Association, American Psychological Association, & National Council on Measurement in Education, 2014). If the STAI demonstrates strong relationships with clinical measures of anxiety symptoms or diagnostic status, this would support its convergent validity. For the STAI to be a useful measure, however, it must also demonstrate discriminant evidence of validity; relationships with measures of depressive symptoms or diagnostic status should not be as strong as those with measures of anxiety.
As is evident from the above review, it remains unclear whether trait anxiety, as assessed by the STAI-T, is a broad vulnerability factor for both anxiety and depression or a more specific vulnerability to anxiety-related disorders. Given that the STAI-T continues to be the measure most commonly used to assess trait anxiety and that the scale may reflect a broader measure of negative affectivity/neuroticism rather than a specific measure of trait anxiety, the present investigation employs a meta-analytic approach to examine the association between trait anxiety and symptoms of depression and anxiety-related disorders. Consistent with a categorical view, meta-analytic comparisons were made on STAI-T scores among those meeting diagnostic criteria for a depressive disorder, an anxiety-related disorder, and nonclinical comparisons. The purpose of this portion of the review was to answer the following three questions:
To what extent do STAI-T scores differ between nonclinical comparison groups and those with a) an anxiety-related disorder and b) a depressive disorder?
To what extent do STAI-T scores differ among those with an anxiety-related disorder compared to those with a depressive disorder?
Are differences between those with an anxiety-related disorder, those with a depressive disorder, and nonclinical comparisons influenced by anxiety and depressive disorder comorbidity?
Next, meta-analyses were performed on correlations of STAI-T scores with measures of anxiety and depressive symptoms within clinically-diagnosed individuals in order to determine the extent of the relationship between anxiety and depression severity and STAI-T scores. In addition to delineating the specific associations between STAI-T scores and depression and anxiety, gender and age were examined as moderators, given that women are 1.7 times more likely to be diagnosed with an anxiety-related disorder (McLean et al., 2011) and 1.5 times more likely to be diagnosed with a mood disorder compared to men, and rates of anxiety and depression differ by age (Kessler et al., 2005). An insufficient number of studies reported race/ethnicity, precluding further analysis. Comorbidity and medication status were also included as moderators, as rates of comorbidity (Clark & Watson, 1991a) and the degree to which symptoms are managed by medication (Soskin et al., 2012) both likely influence self-reported negative affectivity/neuroticism and thus may affect scores on the STAI-T.
Methods
Literature Base
A literature search was conducted in the PsycINFO and PubMed databases to identify empirical articles, published in English, that reported scores on the State-Trait Anxiety Inventory (STAI) within adult populations. Peer-reviewed studies published from January 1, 1970 through April 15, 2020 were included in the search, in accordance with the publication date of the STAI manual. The full search terms and specifiers are detailed in Supplementary Table 1. The initial search in PsycINFO of all peer-reviewed research articles that specified the use of the STAI in the “Tests and Measures” search field, including potential name variations, yielded 11,362 abstracts. The lead author and a team of trained undergraduate research assistants reviewed each abstract according to the following criteria: (a) included individuals aged 18 and older, who were (b) diagnosed according to DSM or ICD criteria with a current anxiety-related disorder (panic disorder, social anxiety disorder, generalized anxiety disorder, specific phobia, posttraumatic stress disorder, acute stress disorder, obsessive-compulsive disorder, illness anxiety disorder, hoarding disorder; see Asmundson, 2019) OR (c) a current depressive disorder, including major depressive disorder, minor depressive disorder, or dysthymia; (d) included a comparison group of healthy individuals OR (e) two groups of individuals diagnosed with different anxiety and depressive disorders as defined above; (f) reported scores on the 20-item Trait version of the STAI. Studies of individuals with psychotic disorders, intellectual disabilities or pervasive developmental disorder, bipolar disorder, adjustment disorder, or an anxiety or depressive disorder in remission were not included, unless separate groups of individuals with anxiety and/or depressive disorders were also reported, and individuals in these groups did not meet the exclusion criteria. After reviewing all abstracts according to these criteria, 863 eligible studies remained. The lead author reviewed all full texts according to these same inclusion criteria. Studies were excluded if they (g) did not report means and standard deviations for the STAI-T by the groups defined above or correlations with measures of anxiety or depressive symptoms, (h) only reported the state scale of the STAI, or (i) included samples overlapping with other published studies. Where the published STAI-T mean was not within the accepted range for this measure (20–80), or where the reported subscale (state or trait) of the STAI was not clear, study authors were contacted for clarifying information. Where STAI-T data was reported at multiple time points, only baseline STAI-T values were included. After review of the full-texts, 383 articles identified in PsycINFO were included in the current meta-analysis.
A literature search was also conducted in the PubMed database to identify articles published in journals not indexed within the PsycINFO database. The initial search included articles published in English and conducted with humans and contained the terms “State-Trait Anxiety Inventory” along with variations of the measure name. A complete list of search terms is included in Supplementary Table 1. A total of 3,934 abstracts were identified according to these search criteria. Of these, 2,118 abstracts were duplicate abstracts included in journals indexed in PsycINFO, leaving 1,816 unique abstracts for review according to the criteria specified above. Of these, 30 abstracts met eligibility criteria and the full texts were reviewed by the lead author. Five additional articles containing valid STAI-T data according to the specified criteria were included in the meta-analysis from the PubMed database. Thus, a total of 388 peer-reviewed articles contained valid data and were included in the current meta-analysis (Figure 3; Supplementary Tables 2 and 3).
Figure 3.

PRISMA screening diagram.
Data Analysis
Effect sizes for STAI-T scores were calculated using Comprehensive Meta-Analysis (CMA) Version 3 (Borenstein et al., 2014), comparing STAI-T means and standard deviations between (1) individuals with an anxiety-related disorder compared to a healthy comparison group, (2) individuals with a depressive disorder compared to a healthy comparison group, (3) individuals with an anxiety-related disorder compared to individuals with a depressive disorder, (4) individuals with comorbid anxiety and depression compared to individuals with an anxiety-related disorder only, and (5) individuals with comorbid anxiety and depression compared to individuals with depression only. Given heterogeneity among studies, random-effects models were used. Subgroup analyses were conducted independently by diagnosis when there were at least ten studies in a given subgroup (Higgins & Green, 2011). Hedges’s g was used as the effect size measure; Hedges’s g effect sizes can be interpreted according to the benchmarks used for Cohen’s d (0.2 = small; 0.5 = medium; 0.8 = large; Cohen, 1992). Separate meta-analyses were also conducted on the correlations between the STAI-T and (6) measures of anxiety symptoms and (7) measures of depressive symptoms. Correlations were first transformed using the Fisher’s z transformation; summary values were converted back into correlations to be reported (Borenstein et al., 2009). Mean correlations were interpreted according to Cohen’s conventions for correlation coefficients (0.1 = small; 0.3 = medium; 0.5 = large; Cohen, 1992). Observed power was > 0.99 for all meta-analyses except for the comparison between individuals with an anxiety-related disorder and those with a depressive disorder, which was 0.85 (Quintana & Tiebel, 2019).
Publication bias was assessed using multiple methods. First, funnel plots were visually inspected, and Egger’s regression analysis was used to determine the significance of asymmetry (Egger et al., 1997). Next, Rosenthal’s fail-safe N was calculated to determine the number of additional studies with an effect size of zero needed to reduce the effect size of the meta-analysis to non-significance (p > 0.05; Rosenthal, 1979). Another measure, Orwin’s fail-safe N, was also calculated in order to assess the number of studies with effects size of zero needed in order to bring the overall effect size to a trivial level, set at Hedges’s g = 0.1 and mean r = .05 (Orwin, 1983). Because observed heterogeneity was large (Table 1), potential moderators (mean age, percent female, rates of comorbid anxiety and depression, and percent of individuals on psychoactive medication) were assessed using meta-regression. For categorical moderators (region; STAI Form X vs. Form Y), dummy variables were created for use in the meta-regression model. Due to rates of missingness across studies, each potential moderator was examined in a separate meta-regression model.
Table 1.
Categorical comparisons of STAI-T scores across diagnostic groups.
| Comparison | g | k | 95% CI | p | Q | df | p | I2 | RFSN | OFSN |
|---|---|---|---|---|---|---|---|---|---|---|
| All anxiety disorders vs. nonclinical comparison groups | 1.90 | 359 | [1.81, 1.98] | <.001 | 2508.03 | 358 | <.001 | 85.73 | 999754 | 5477 |
| Anxiety disorders (excluding specific phobia) vs. nonclinical comparison groups | 2.01 | 333 | [1.92, 2.09] | <.001 | 2078.63 | 332 | <.001 | 84.03 | 957748 | 5381 |
| GAD | 2.58 | 41 | [2.33, 2.83] | <.001 | 186.01 | 40 | <.001 | 78.50 | 18882 | 934 |
| OCD | 1.82 | 79 | [1.67, 1.97] | <.001 | 373.95 | 78 | <.001 | 79.14 | 51713 | 1267 |
| PD | 1.77 | 54 | [1.58, 1.97] | <.001 | 391.19 | 53 | <.001 | 86.45 | 24517 | 666 |
| PTSD | 1.91 | 48 | [1.72, 2.11] | <.001 | 165.22 | 47 | <.001 | 71.55 | 14648 | 764 |
| SAD | 2.28 | 77 | [2.12, 2.44] | <.001 | 300.76 | 76 | <.001 | 74.73 | 60076 | 1612 |
| SP | 0.50 | 26 | [0.35, 0.64] | <.001 | 36.38 | 25 | .067 | 31.28 | 426 | 103 |
| All depressive disorders vs. nonclinical comparison groups | 2.60 | 86 | [2.37, 2.83] | <.001 | 1293.93 | 85 | <.001 | 93.43 | 113446 | 1690 |
| MDD | 2.74 | 76 | [2.49, 2.98] | <.001 | 1078.32 | 75 | <.001 | 93.05 | 94012 | 1602 |
| Anxiety disorders vs. depressive disorders | −0.27 | 24 | [−0.45, −0.08] | .005 | 79.70 | 23 | <.001 | 71.14 | 124 | 27 |
| Anxiety + depression vs. anxiety disorders | 0.75 | 11 | [0.37, 1.12] | <.001 | 46.11 | 10 | <.001 | 78.32 | 215 | 71 |
| Anxiety + depression vs. depressive disorders | 0.47 | 10 | [0.29, 0.64] | <.001 | 5.57 | 9 | .782 | 0.00 | 46 | 37 |
Note. g = Hedges’s g; k = number of studies; CI = confidence interval; RFSN = Rosenthal’s fail-safe N; OFSN = Orwin’s fail-safe N; GAD = generalized anxiety disorder; OCD = obsessive-compulsive disorder; PD = panic disorder; PTSD = posttraumatic stress disorder; SAD = social anxiety disorder (generalized); SP = specific phobia; MDD = major depressive disorder
Anxiety-related disorders include GAD, OCD, PD, PTSD, SAD, SP, acute stress disorder, hoarding disorder, illness anxiety disorder, and social anxiety disorder (performance only).
Depressive disorders include MDD, minor depression, dysthymia, and depression not otherwise specified.
Anxiety + depression includes studies where a group was designated as having a comorbid anxiety disorder and depressive disorder.
Results
Categorical Comparisons
Effect sizes for individual subgroup comparisons are listed in Supplementary Table 4.
Anxiety and Depressive Disorders Relative to Nonclinical Comparison Groups
As anticipated, individuals with anxiety-related disorders had significantly higher scores on the STAI-T compared to nonclinical comparison groups, k = 359, g = 1.90, p < .001. The magnitude of the effect was very large for GAD, OCD, panic disorder, PTSD, and social anxiety disorder, gs = 1.77 – 2.58, and medium for specific phobia, g = 0.50 (Table 1; Figure 4). When specific phobia was removed from the analyses, the overall effect for anxiety-related disorders compared to nonclinical comparison groups was slightly larger, k = 333, g = 2.01, p < .001. Individuals with depressive disorders also had significantly higher STAI-T scores than nonclinical comparison groups, k = 86, g = 2.60, p < .001. When the sample was restricted to studies of individuals who met criteria for MDD only, the effect size was slightly larger, k = 76, g = 2.74 (Table 1; Figure 4).
Figure 4.

Comparison of STAI-T scores for anxiety and depressive disorders vs. nonclinical comparison groups.
Note. CI = confidence interval; GAD = generalized anxiety disorder; OCD = obsessive-compulsive disorder; PD = panic disorder; PTSD = posttraumatic stress disorder; SAD = social anxiety disorder (generalized); SP = specific phobia; MDD = major depressive disorder
Anxiety-Related Disorders Compared to Depressive Disorders
A number of studies reported the STAI-T scores of individuals with an anxiety-related disorder compared to individuals with a depressive disorder. Individuals with anxiety-related disorders had significantly lower scores on the STAI-T compared to individuals with depressive disorders, though the effect was small, k = 24, g = −0.27, p = .005 (Table 1; Figure 4).
Comorbidity
A few studies directly compared individuals with comorbid anxiety and depressive disorders to individuals with anxiety-related disorders only, depressive disorders only, or to both groups. Individuals with comorbid anxiety and depression had significantly higher scores on the STAI-T compared to individuals with anxiety-related disorders only, k = 11, g = 0.75, p < .001, and compared to individuals with depressive disorders only, k = 10, g = 0.47, p < .001 (Table 1; Figure 5). For the remaining studies, percent comorbidity was assessed as a moderator. When comparing individuals with an anxiety-rated disorder to nonclinical comparison groups, a trend was observed such that higher rates of additional anxiety-rated disorder comorbidity were associated with higher scores on the STAI-T, Q = 2.96, p = .09. Rates of comorbid depressive disorders were significantly associated with increased STAI-T scores, Q = 10.48, p = .001, though the total variance attributed to depressive comorbidity was small, R2 analog = 0.06. The effect of comorbid depression was not statistically significant when comparing specific anxiety-related disorders with nonclinical comparison groups, although there was a trend toward increased STAI-T scores in individuals with PTSD as depressive comorbidity increased, Q = 3.50, p = .06.
Figure 5.
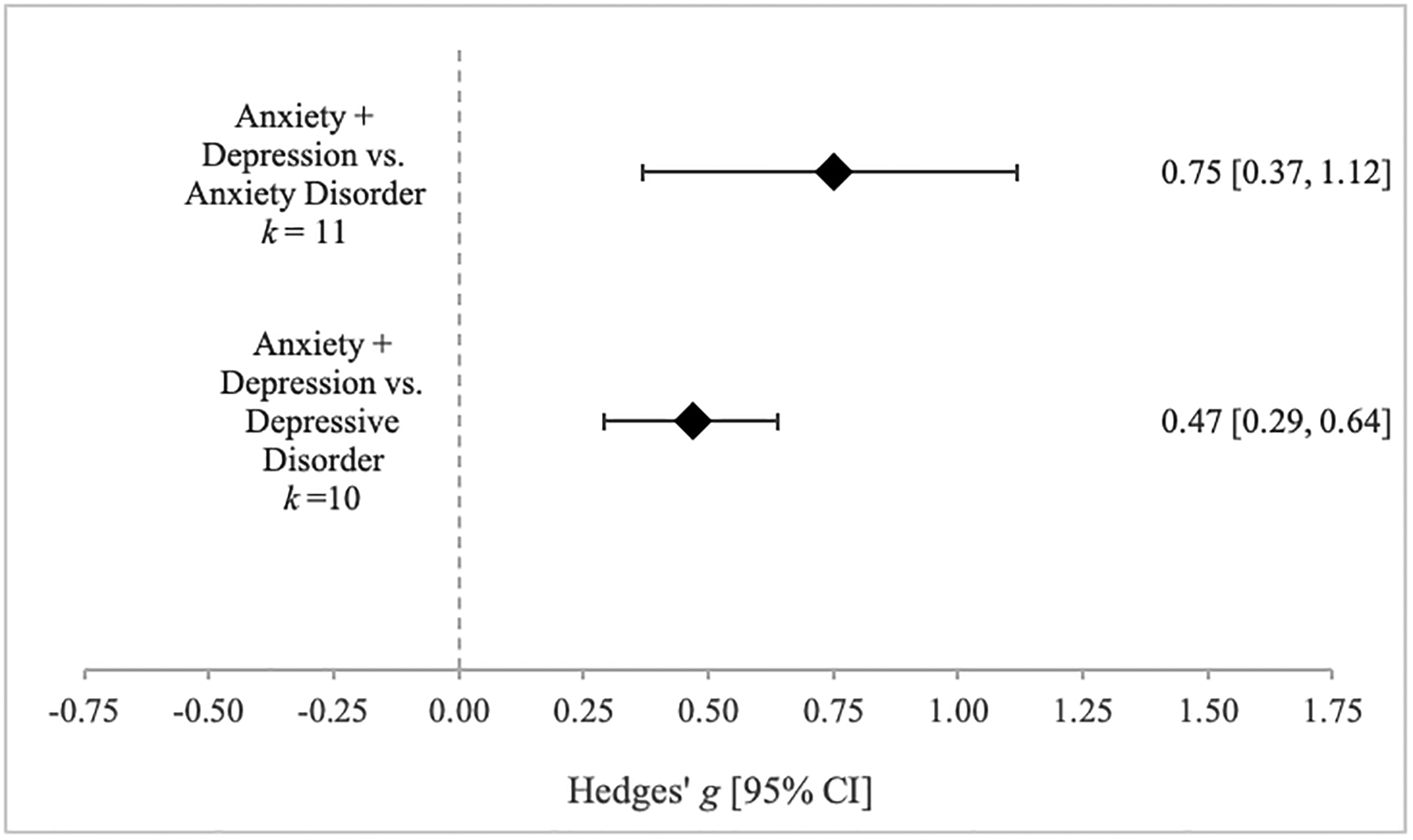
Comparison of STAI-T scores for comorbid anxiety + depressive disorders vs. single disorder.
Note. CI = confidence interval
When comparing individuals with a depressive disorder with nonclinical comparison groups, rates of comorbid anxiety-related disorders did not significantly affect STAI-T scores, Q = 0.21, p = .65. In addition, there was a trend observed for individuals with depressive disorders to have increased STAI-T scores as the percentage of other comorbid depressive disorders (i.e., MDD and dysthymia) increased, Q = 3.76, p = .05. Anxiety comorbidity did not moderate the difference in STAI-T scores between individuals with anxiety-related disorders and individuals with depressive disorders, Q = 0.22, p = .90, and depressive comorbidity also did not did not moderate the difference in STAI-T scores between these groups, Q = 0.02, p = .99. Table 2 displays the results of these comorbidity moderation analyses.
Table 2.
Moderation analyses.
| Moderator | β | SE | Q | df | p |
|---|---|---|---|---|---|
| Anxiety Disorder vs. Nonclinical Comparison Group | |||||
| Comorbid Anxiety | 0.00 | 0.00 | 2.96 | 1 | .09# |
| Comorbid Depression | 0.01 | 0.00 | 10.48 | 1 | .001* |
| Medication | 0.00 | 0.00 | 0.00 | 1 | .98 |
| Gender | 0.00 | 0.00 | 1.54 | 1 | .21 |
| Age | 0.01 | 0.01 | 1.93 | 1 | .17 |
| Form (X vs. Y) | −0.24 | 0.09 | 6.58 | 1 | .01* |
| Region (vs. United States) | 42.05 | 16 | <.001* | ||
| Asia (other) | −0.91 | 0.54 | .09# | ||
| Australia/New Zealand | 0.10 | 0.33 | .77 | ||
| Canada | −0.44 | 0.32 | .17 | ||
| China | −0.56 | 0.18 | .001* | ||
| Europe (other) | −0.69 | 0.29 | .02* | ||
| Germany/Austria | −0.54 | 0.12 | <.001* | ||
| Israel | −0.51 | 0.24 | .04* | ||
| Italy | −0.64 | 0.21 | .002* | ||
| Japan | −0.65 | 0.21 | .002* | ||
| South America | −0.62 | 0.47 | .19 | ||
| South Korea | −0.61 | 0.27 | .02* | ||
| Spain | −0.73 | 0.26 | .005* | ||
| Switzerland | −0.08 | 0.24 | .74 | ||
| Turkey | −0.30 | 0.27 | .26 | ||
| United Kingdom | −0.15 | 0.18 | .39 | ||
| Western Europe | −0.60 | 0.22 | .01* | ||
| GAD vs. Nonclinical Comparison Group | |||||
| Moderator | β | SE | Q | df | p |
| Comorbid Anxiety | 0.00 | 0.01 | 0.05 | 1 | .82 |
| Comorbid Depression | 0.00 | 0.01 | 0.18 | 1 | .67 |
| Medication | −0.01 | 0.00 | 2.87 | 1 | .09# |
| Gender | 0.02 | 0.01 | 4.39 | 1 | .04* |
| Age | 0.01 | 0.01 | 0.15 | 1 | .70 |
| OCD vs. Nonclinical Comparison Group | |||||
| Moderator | β | SE | Q | df | p |
| Comorbid Anxiety | 0.00 | 0.01 | 0.13 | 1 | .72 |
| Comorbid Depression | 0.00 | 0.00 | 0.22 | 1 | .64 |
| Medication | 0.00 | 0.00 | 0.00 | 1 | .97 |
| Gender | 0.01 | 0.01 | 4.43 | 1 | .04* |
| Age | 0.01 | 0.01 | 0.96 | 1 | .33 |
| Panic Disorder vs. Nonclinical Comparison Group | |||||
| Moderator | β | SE | Q | df | p |
| Comorbid Anxiety | 0.00 | 0.00 | 0.66 | 1 | .42 |
| Comorbid Depression | 0.01 | 0.01 | 0.86 | 1 | .35 |
| Medication | 0.00 | 0.00 | 0.01 | 1 | .94 |
| Gender | 0.01 | 0.01 | 3.12 | 1 | .08# |
| Age | −0.05 | 0.02 | 5.51 | 1 | .02* |
| PTSD vs. Nonclinical Comparison Group | |||||
| Moderator | β | SE | Q | df | p |
| Comorbid Anxiety | 0.01 | 0.01 | 0.84 | 1 | .36 |
| Comorbid Depression | 0.01 | 0.01 | 3.50 | 1 | .06# |
| Medication | 0.00 | 0.00 | 0.54 | 1 | .46 |
| Gender | 0.00 | 0.00 | 2.00 | 1 | .16 |
| Age | −0.01 | 0.02 | 0.33 | 1 | .57 |
| SAD vs. Nonclinical Comparison Group | |||||
| Moderator | β | SE | Q | df | p |
| Comorbid Anxiety | 0.00 | 0.01 | 0.03 | 1 | .87 |
| Comorbid Depression | 0.00 | 0.00 | 0.17 | 1 | .68 |
| Medication | 0.01 | 0.01 | 0.98 | 1 | .32 |
| Gender | 0.00 | 0.00 | 0.04 | 1 | .84 |
| Age | −0.02 | 0.02 | 0.90 | 1 | .34 |
| Specific Phobia vs. Nonclinical Comparison Group | |||||
| Moderator | β | SE | Q | df | p |
| Comorbid Anxiety | −0.01 | 0.07 | 0.03 | 1 | .87 |
| Gender | 0.00 | 0.01 | 0.05 | 1 | .83 |
| Age | 0.04 | 0.01 | 8.91 | 1 | .003* |
| Depressive Disorder vs. Nonclinical Comparison Group | |||||
| Moderator | β | SE | Q | df | p |
| Comorbid Anxiety | 0.00 | 0.01 | 0.21 | 1 | .65 |
| Comorbid Depression | 0.02 | 0.01 | 3.76 | 1 | .05# |
| Medication | 0.00 | 0.00 | 0.03 | 1 | .87 |
| Gender | −0.01 | 0.01 | 2.31 | 1 | .13 |
| Age | −0.01 | 0.02 | 0.65 | 1 | .42 |
| Form | 0.11 | 0.25 | 0.18 | 1 | .67 |
| Region (vs. United States) | 27.35 | 8 | <.001* | ||
| Asia | −1.11 | 0.38 | .003* | ||
| Australia | 0.11 | 0.60 | .86 | ||
| Canada | 0.03 | 0.73 | .97 | ||
| Europe | −0.40 | 0.31 | .20 | ||
| Germany/Austria | 0.16 | 0.32 | .61 | ||
| Middle East | −0.94 | 0.59 | .11 | ||
| South America | 0.47 | 0.59 | .42 | ||
| United Kingdom | 0.90 | 0.38 | .02* | ||
| MDD vs. Nonclinical Comparison Group | |||||
| Moderator | β | SE | Q | df | p |
| Comorbid Anxiety | 0.01 | 0.01 | 1.89 | 1 | .17 |
| Comorbid Depression | 0.02 | 0.01 | 2.42 | 1 | .12 |
| Medication | 0.00 | 0.00 | 0.34 | 1 | .56 |
| Gender | 0.00 | 0.01 | 0.26 | 1 | .61 |
| Age | −0.05 | 0.02 | 4.67 | 1 | .03* |
| Form | 0.09 | 0.26 | 0.12 | 1 | .73 |
| Anxiety Disorder vs. Depressive Disorder | |||||
| Moderator | β | SE | Q | df | p |
| Comorbid Anxiety | 0.22 | 2 | .90 | ||
| Anxiety | 0.00 | 0.02 | |||
| Depression | 0.00 | 0.01 | |||
| Comorbid Depression | 0.02 | 2 | .99 | ||
| Anxiety | 0.00 | 0.01 | |||
| Depression | 0.00 | 0.03 | |||
| Gender | 0.68 | 2 | .71 | ||
| Anxiety | 0.00 | 0.01 | |||
| Depression | 0.00 | 0.01 | |||
| Age | 3.21 | 2 | .20 | ||
| Anxiety | −0.01 | 0.02 | |||
| Depression | 0.03 | 0.00 | |||
| Form | −0.04 | 0.22 | 0.03 | 1 | .86 |
Note. SE = standard error; df = degrees of freedom; GAD = generalized anxiety disorder; OCD = obsessive-compulsive disorder; PTSD = posttraumatic stress disorder; SAD = social anxiety disorder (generalized); MDD = major depressive disorder
significant moderation (p < .05);
trend level moderation (p < .10)
Studies were coded by country, and countries were combined into regions when only a small number of studies were conducted within a given country. For example, many European countries were combined, with the exception of countries that contributed a large number of studies to the meta-analysis. Because most studies did not specify whether the STAI X or Y was used, this moderator was coded based on the version of the STAI that was cited in the study. If a study cited a non-English translation of the STAI, that citation was reviewed to determine if the translated version of the STAI was based on X or Y.
Other Moderators
All other moderation analyses are displayed in Table 2. The gender composition of the groups did not affect the difference in STAI-T scores between individuals with an anxiety-related disorder compared to nonclinical comparison groups, Q = 1.54, p = .21, or individuals with a depressive disorder compared to nonclinical comparison groups, Q = 2.31, p = .13. Gender also did not moderate the difference in STAI-T scores between individuals with anxiety-related disorders and individuals with depressive disorders, Q = 0.68, p = .71. However, gender did moderate the effect size between nonclinical comparison groups and specific anxiety-related disorders. For individuals with GAD and OCD, an increased percent of women in the sample was associated with a significantly higher STAI-T score compared to nonclinical comparison groups, QGAD = 4.39, p = .04, R2 analog = 0.12; QOCD = 4.43, p = .04, R2 analog = 0.17. This trend was also observed for individuals with panic disorder but did not reach significance, QPD = 3.12, p = .08.
Age did not significantly moderate the difference in STAI-T scores between individuals with an anxiety-related disorder compared to nonclinical comparison groups, Q = 1.93, p = .17, or individuals with a depressive disorder compared to nonclinical comparison groups, Q = 0.65, p = .42. However, specific disorders did show relations with age. For individuals with panic disorder, younger individuals had significantly higher STAI-T scores compared to nonclinical comparison groups, Q = 5.51, p = .02, R2 analog = 0.12. For individuals with a specific phobia, age had the opposite effect; older individuals had significantly higher STAI-T scores compared to nonclinical comparison groups, Q = 8.91, p < .01, R2 analog = 0.80. For individuals with MDD, younger individuals had higher STAI-T scores than non-clinical comparison groups, Q = 4.67, p = .03, R2 analog = 0.00. Age did not moderate the difference in STAI-T scores between individuals with anxiety-related disorders and individuals with depressive disorders, Q = 3.21, p = .20.
Rates of psychoactive medication did not moderate differences in STAI-T scores between individuals with anxiety-related disorders, Q = 0.00, p = .98, or individuals with depressive disorders compared to nonclinical comparison groups, Q = 0.03, p = .87. However, a trend was observed for individuals with GAD compared to nonclinical comparison groups, such that higher rates of medication use in the sample were associated with lower STAI-T scores, Q = 2.87, p = .09. An insufficient number of studies included medication information to allow for comparison between individuals with anxiety and depressive disorders.
Because there are significant differences between Form X and Form Y of the STAI, comparisons were conducted between studies that used each form. For comparisons between individuals with anxiety-related disorders and nonclinical comparison groups, the form of the STAI used was a statistically significant moderator. Studies using Form Y (k = 180, g = 1.99) showed significantly higher STAI-T scores for individuals with anxiety-related disorders compared to nonclinical comparison groups than studies using Form X (k = 141, g = 1.75), Q = 6.58, p = .01. The form of the STAI used did not significantly affect differences in STAI-T scores between individuals with depressive disorders and nonclinical comparison groups, Q = 0.18, p = .67, or between individuals with anxiety-related disorders and individuals with depressive disorders, Q = 0.08, p = .86.
Regional differences in STAI-T scores were also found. For studies comparing individuals with an anxiety-related disorder and nonclinical comparison groups, the region in which the study was conducted significantly moderated the difference in STAI-T scores, Q = 42.05, p < .001. Specifically, studies conducted in China (k = 25), Germany and Austria (k = 75), Israel (k = 12), Italy (k = 17), Japan (k = 16), South Korea (k = 9), Spain (k = 10), Western Europe (k = 15, includes France, the Netherlands, and Belgium), and other European countries (k = 8, includes Hungary, Poland, Croatia, Greece, Sweden, and Norway) had significantly smaller differences in STAI-T scores between individuals with an anxiety-related disorder and nonclinical comparison groups than studies conducted in the United States (k = 97), all ps < .04. Studies comparing individuals with anxiety-related disorders and nonclinical comparison groups that were conducted in Australia and New Zealand (k = 7), Canada (k = 7), South America (k = 3), Switzerland (k = 14), Turkey (k = 10), and the United Kingdom (k = 27) did not significantly differ from studies conducted in the United States, all ps > .16 (see Table 2 for full results). For studies comparing individuals with a depressive disorder and nonclinical comparison groups, the region in which the study was conducted significantly moderated the difference in STAI-T scores, Q = 27.35, p < .001. Specifically, studies conducted in Asia (k = 9), including China, Japan, South Korea, and Russia (Siberia), had significantly smaller differences in STAI-T scores between individuals with a depressive disorder and nonclinical comparison groups than studies conducted in the United States (k = 21), β = −1.11, SE = 0.38, p < .01. Studies conducted in the United Kingdom (k = 10) had a larger effect than studies conducted in the United States, β = 0.90, SE = 0.38, p = .02. For all other regions (Australia, Canada, Europe, Germany and Austria, the Middle East, and South America), effect sizes did not differ from studies conducted in the United States.
Correlational Meta-Analyses
STAI-T and Anxiety Symptom Severity
Correlations were examined between the STAI-T and measures of anxiety symptoms, including the Penn State Worry Questionnaire (PSWQ; Meyer et al., 1990), Obsessive Compulsive Inventory — Revised (OCI-R; Foa et al., 2002), the Yale-Brown Obsessive-Compulsive Scale (Y-BOCS; Goodman et al., 1989), the Hypochondriasis Y-BOCS (H-YBOCS; Skritskaya et al., 2012), the Davidson Trauma Scale (DTS; Davidson et al., 1997), the Acute Stress Disorder Interview (ASDI; Bryant et al.,1998), the Liebowitz Social Anxiety Scale (LSAS; Liebowitz, 1987), the Social Interaction Anxiety Scale (SIAS; Rodebaugh et al., 2007), the Social Phobia Inventory (SPIN; Connor et al., 2000), and the Symptoms Rating Scale for Depression and Anxiety, Anxiety subscale (SRSDA; Bech, 1993). Correlations were included if they were measured within clinically anxious or depressed samples (k = 15). The STAI-T was strongly correlated with anxiety symptom severity, mean r = 0.59 (Table 3, Figure 6).
Table 3.
Correlations of STAI-T scores with measures of anxiety and depressive symptom severity.
| Measures | Mean r | k | 95% CI | p | Q | df | p | I2 | RFSN | OFSN |
|---|---|---|---|---|---|---|---|---|---|---|
| STAI-T + measures of anxiety | 0.59 | 15 | [0.49, 0.68] | <.001 | 50.92 | 14 | <.001 | 72.51 | 1180 | 175 |
| STAI-T + measures of depression | 0.61 | 13 | [0.53, 0.68] | <.001 | 18.67 | 12 | .10 | 35.73 | 767 | 170 |
Note. Measures of anxiety symptoms include the ASDI, DTS, H-YBOCS, LSAS, OCI-R, PSWQ, SIAS, SPIN, SRSDA, and Y-BOCS. Measures of depression include the BDI and BDI-II.
k = number of studies; CI = confidence interval; RFSN = Rosenthal’s fail-safe N; OFSN = Orwin’s fail-safe N; ASDI = Acute Stress Disorder Interview; BDI = Beck Depression Inventory; BDI-II = Beck Depression Inventory-II; DTS = Davidson Trauma Scale; H-YBOCS = Hypochondriasis Yale-Brown Obsessive-Compulsive Scale; LSAS = Liebowitz Social Anxiety Scale; OCI-R = Obsessive Compulsive Inventory — Revised; PSWQ = Penn State Worry Questionnaire; SIAS = Social Interaction Anxiety Scale; SPIN = Social Phobia Inventory; SRSDA = Symptoms Rating Scale for Depression and Anxiety (Anxiety subscale); Y-BOCS = Yale-Brown Obsessive-Compulsive Scale.
Figure 6.

Correlations between the STAI-T and measures of anxiety and depressive symptom severity.
Note. CI = confidence interval
STAI-T and Depressive Symptom Severity
Correlations were also available between the STAI-T and the Beck Depression Inventory (BDI; Beck et al., 1961) and Beck Depression Inventory-II (BDI-II; Beck et al., 1996) within clinically anxious or depressed samples (k = 13). The STAI-T was strongly correlated with depressive symptom severity, mean r = 0.61 (Table 3, Figure 6).
Publication Bias
Publication bias was also assessed for each of these analyses. Funnel plots are displayed in Supplementary Figures 1–5. The funnel plots for the meta-analyses comparing STAI-T scores between individuals with an anxiety-related disorder and individuals with a depressive disorder, individuals with comorbid anxiety and depression and individuals with an anxiety-related disorder only, and individuals with comorbid anxiety and depression and individuals with a depressive disorder only were not asymmetrical, ps = .13–.31, suggesting that these meta-analyses were not significantly affected by publication bias (Egger et al., 1997). Similarly, the funnel plots for the correlations between the STAI-T and measures of depression and measures of anxiety were not asymmetrical (ps = .22–.52). However, the meta-analyses comparing individuals with an anxiety-related disorder and individuals with a depressive disorder to nonclinical comparison groups were significantly asymmetrical (both ps < .001).
Discussion
The present meta-analysis showed that individuals with an anxiety-related disorder and those with a depressive disorder displayed significantly elevated scores on the STAI-T compared to nonclinical comparison groups. Furthermore, measures of depression and anxiety symptom severity were similarly strongly correlated with the STAI-T in these samples. These findings are consistent with research that has implicated trait anxiety in anxiety and depression (Andrews, 1991; Rachman, 1998; Weger & Sandi, 2018). Although the effect size was small, the present findings also showed that individuals with a depressive disorder had significantly higher STAI-T scores than individuals with an anxiety-related disorder. This finding is contrary to what would be expected if the STAI-T is to be considered a measure of the stable tendency to attend to, experience, and report fears, worries, and anxiety across many situations. Furthermore, the findings showed that comorbidity influenced differences in STAI-T scores. More specifically, individuals with comorbid anxiety and depression had higher STAI-T scores than individuals with either anxiety or depression alone. In particular, the addition of comorbid depression increased STAI-T scores for individuals with anxiety-related disorders, whereas the addition of comorbid anxiety did not affect STAI-T scores for individuals with depressive disorders.
The STAI-T is a Nonspecific Measure of Negative Affect
The findings of the present meta-analysis suggest that the STAI-T may not exclusively measure trait anxiety as it purports to do but rather captures a higher-order trait such as negative affectivity/neuroticism that characterizes both anxiety and depression. For example, based on an extensive review of the literature, Mineka and colleagues (1998) concluded that the DSM-IV mood and anxiety disorders contain a shared component representing “broad individual differences in general distress and Negative Affect; it is a pervasive higher order factor that is common to both the mood and anxiety disorders and is primarily responsible for the overlap among these disorders” (p. 397). Given factor analytic studies of the STAI that identify anxiety and depression factors (Bieling et al., 1998) and the wording of specific items that reflect depressive rather than anxious content (e.g., “I take disappointments so keenly that I can’t put them out of my mind”), the STAI-T appears to capture a broad negative affective vulnerability that may confer risk for both anxiety and depression.
Attempts to develop a valid measure of trait anxiety via self-report are not new; sixty years ago, there were at least 120 personality tests that purported to measure anxiety (Cattell & Scheier, 1958). Traits are descriptive and useful ways to categorize behavior, but psychometrically, they cannot be measured directly and are instead inferred from systematic covariation (Cattell, 1946). Accordingly, concerns about validity are not unique to the STAI (Dobson, 1985; Feldman, 1993; Gotlib, 1984). Indeed, many self-report scales of anxiety and depression suffer from similar psychometric limitations (Gotlib & Cane, 1989). However, due to its widespread use (see Figure 2), the STAI-T’s limited discriminant evidence of validity has important implications for the inferences made in the psychopathology literature. For example, many of the previously reviewed studies that discuss relations between trait anxiety and behavioral, cognitive, physiological, and neural processes may need to be reconceptualized. Given that the STAI-T appears to be a measure of negative affectivity/neuroticism, these studies demonstrate an association between various processes and negative affectivity/neuroticism more broadly rather than trait anxiety per se.
Although the STAI-T appears to be a measure of negative affect, it is important to note that it is imperfect in this regard as well. For example, the STAI-T does not appear to assess negative emotions other than anxiety and depression. Indeed, guilt, shame, disgust, and anger are all negative emotions, yet the items included in the STAI-T do not reflect these emotions. Other measures of negative affectivity/neuroticism, such as the Positive Affect and Negative Affect Scales (PANAS; Watson et al., 1988), do include items assessing guilt, shame, hostility, and irritability and evince a moderate degree of stability and predictive power across a 6-year period in their trait form (Watson & Walker, 1996). Although the PANAS does not capture any behavioral, cognitive, or somatic correlates of affective experiences and strictly asks individuals to report to what extent they “generally” feel, it is clearly a more comprehensive measure of negative affect. In sum, the STAI-T lacks discriminant evidence of validity and thus is not an appropriate measure of trait anxiety. However, the STAI-T also underrepresents the construct of negative affect due to its limited scope.
Anxiety and Depressive Disorders Differ in Negative Affect
If the STAI-T is better described as a measure of negative affect than trait anxiety, the findings of the present meta-analysis suggest that individuals with depressive disorders demonstrate higher trait negative affectivity than individuals with anxiety-related disorders. Although a meta-analysis examining personality traits and psychopathology did not find significantly higher negative affectivity/neuroticism in depression compared to anxiety-related disorders (Kotov et al., 2010), symptoms of depression correlate more strongly with negative affectivity/neuroticism than symptoms of social anxiety, panic, agoraphobia, and specific phobia in other studies (Brown, 2007; Brown et al., 1998; Brown & Naragon-Gainey, 2013; Gamez et al., 2007; Naragon-Gainey & Watson, 2018; Paulus et al., 2015; Watson et al., 2005). Notably, in studies examining negative affectivity/neuroticism and symptoms of psychopathology, GAD has stronger relations with negative affectivity/neuroticism than other anxiety-related disorders. In structural models of psychopathology, GAD loads onto a distress/anxious-misery factor along with MDD, dysthymia, and sometimes PTSD, whereas other anxiety disorders (panic disorder, agoraphobia, social anxiety disorder, and specific phobia) load onto a fear disorder factor (Krueger, 1999; Vollebergh et al., 2001; Watson, 2005; Watson et al., 2008; Wright et al., 2013). In the present meta-analysis, studies comparing individuals with GAD to nonclinical comparison groups had a similar effect size as studies comparing individuals with depressive disorders and nonclinical comparison groups. Although these effect sizes cannot be directly compared1, the 95% confidence interval of the effect size of the difference in STAI-T scores between individuals with a depressive disorder and nonclinical comparison groups overlaps with the 95% confidence interval for GAD as well as for social anxiety disorder, but not with the effect sizes for other anxiety-related disorders. A small number of studies (k = 7) were available directly comparing STAI-T scores between individuals with GAD and individuals with a depressive disorder; this effect size was small (Hedges’s g = −0.23) and did not reach significance (p = .26). A direct comparison of STAI-T scores between individuals with social anxiety disorder and individuals with a depressive disorder suggests that there is a small but significant difference in these groups’ mean STAI-T scores (k = 5, Hedges’s g = −0.45, p < .001). Together, these results suggest that individuals with GAD and individuals with a depressive disorder do not differ in negative affectivity/neuroticism; individuals with social anxiety disorder have significantly lower negative affectivity/neuroticism than individuals with depression. These results are consistent with existing evidence that individuals with distress disorders have a higher level of negative affectivity compared to individuals with fear disorders.
Negative affectivity/neuroticism may be the core common feature of internalizing disorders, as demonstrated by findings from a large-scale study of adolescents that identified a single internalizing factor common to mood and anxiety-related disorder diagnostic status that correlated almost perfectly (r = .98) with a measure of neuroticism (Griffith et al., 2010). Even though negative affectivity/neuroticism contributes a large proportion of symptom variance in structural models of psychopathology, the inclusion of measures of cognitive vulnerabilities may provide additional specificity and predictive power. Multiple candidates for specific cognitive vulnerability factors that may be either cumulative or synergistic with negative affectivity/neuroticism in structural models of psychopathology have been evaluated. For example, anxiety sensitivity and intolerance of uncertainty explained unique variance in OCD, social anxiety, and worry symptoms in an undergraduate sample (Norton & Mehta, 2007). Another study in an undergraduate sample found that specific cognitive vulnerabilities fully mediated the relation between negative affectivity/neuroticism and symptoms of psychopathology, including intolerance of uncertainty and ruminative style for depression and worry symptoms, and anxiety sensitivity for panic and social anxiety symptoms (Hong, 2013). In a sample of treatment-seeking outpatients with anxiety and depressive disorders, negative affectivity/neuroticism explained a large portion of the variance in panic symptoms indirectly through anxiety sensitivity, and also explained a statistically significant portion of the variance in OCD, social anxiety, GAD, and depression indirectly through intolerance of uncertainty (Paulus et al., 2015). A second study in a large clinical sample identified negative affectivity/neuroticism as a core biological vulnerability for internalizing disorders along with specific cognitive vulnerabilities, including perceived control for both GAD and OCD as well as thought-action fusion for OCD alone (Brown & Naragon-Gainey, 2013). Finally, a study of psychiatric outpatients found that although a model including higher-order negative affectivity/neuroticism and multiple lower-order cognitive vulnerabilities (anxiety sensitivity, intolerance of uncertainty, perfectionism, and experiential avoidance) fit the data, only anxiety sensitivity and perfectionism contributed significant variance to internalizing psychopathology, with the latter only specifically contributing variance in OCD2 (Naragon-Gainey & Watson, 2018). These results suggest that employing measures of specific cognitive vulnerabilities may have increment (or complement) negative affectivity/neuroticism when examining vulnerability factors for various forms of psychopathology.
The present meta-analysis also suggests that negative affectivity is higher in comorbid anxiety and depression compared to either anxiety or depression alone. Other studies have also found an association between increased negative affectivity/neuroticism and increased prevalence and number of comorbid disorders in MDD (Jylh et al., 2009; Xia et al. 2011), and a previous study of individuals with anxiety and depressive disorders demonstrated a trend toward increased comorbidity with increased negative affectivity/neuroticism (Bienvenu et al., 2001). The nature of comorbidity within anxiety and depression has been extensively examined, and negative affectivity/neuroticism likely accounts for much of this overlap, as individuals high in negative affectivity are more likely to experience high levels of multiple negative emotions (Mineka et al., 1998; Watson, 2005). The present study suggests that depressive disorders are associated with higher negative affectivity than anxiety-related disorders; thus, increased comorbid depression in an anxious sample leads to significantly higher STAI-T scores, whereas the addition of comorbid anxiety in a depressive disorder sample does not have a statistically significant effect on STAI-T scores.
Importantly, though individuals with depressive disorders endorsed a small but significantly higher mean level of negative affect than individuals with anxiety-related disorders, the STAI-T correlated equally strongly with anxiety and depressive symptom severity. That is, while there was a strong relationship between overall symptom severity and STAI-T scores within these clinical samples, the relationship between STAI-T scores and anxiety symptom severity did not differ from the relationship between STAI-T scores and depressive symptom severity. Although there were fewer studies included in the correlational analyses compared to the diagnostic comparisons, observed power (> 0.99) was still sufficient to detect small differences in the relationship between negative affect and anxiety and depressive symptoms.
Moderators of STAI-T Effects
Statistically significant moderators of the difference in STAI-T scores between clinically anxious and depressed individuals and nonclinical comparison groups were also detected. For instance, gender moderated the difference in STAI-T scores between nonclinical comparison groups and individuals with GAD and OCD, with samples with a higher percentage of women having higher STAI-T scores than nonclinical comparison groups. In nonclinical normative samples, women tended to have higher scores than men on the STAI-T (Spielberger et al., 1983); a meta-analysis of cross-cultural gender differences in personality traits among nonclinical individuals found that women tended to score significantly higher on measures of negative affectivity/neuroticism compared to men (Schmitt et al., 2008). For both GAD and OCD, women are more likely than men to meet criteria for comorbid depression (Hallion et al., 2015; Vesga-López et al., 2008), which may account for higher reported negative affect as indexed by the STAI-T. However, it is unclear why higher negative affect would only be found for women with GAD and OCD, but not for women with other anxiety-related or depressive disorders. Similarly, age effects were not detected at the broad categorical level but did emerge for specific disorders. In studies comparing individuals with panic disorder and individuals with major depressive disorder with nonclinical comparison groups, as mean participant age increased, the difference in STAI-T scores between the clinical and nonclinical groups decreased. However, in specific phobia, older individuals had higher STAI-T scores compared to nonclinical comparison groups than younger individuals. It is unclear why this pattern would be reversed in individuals with specific phobia; it is possible that individuals whose specific phobias persist into later adulthood are more likely to be generally anxious than individuals whose specific phobias resolve earlier in life. Among older adults, individuals with current specific phobia had higher rates of comorbid depression and other anxiety-related disorders than older individuals without specific phobia, but this study did not compare older and younger adults with specific phobia (Chou, 2009).
Lastly, studies conducted in the United States tended to have larger differences in STAI-T scores between clinically anxious and depressed individuals and nonclinical comparison groups compared to most other regions, especially non-English-speaking countries. Importantly, these cross-national variations in negative affect may not be attributable to cross-national differences in the nature or validity of negative affect (Simon et al., 2002), as all studies used the STAI-T. Accordingly, using the STAI-T may be revealing different levels of negative affect in different countries. Coupled with recent research showing that some forms of negative affect have significantly increased in the United States (Weinberger et al., 2018), the present findings suggest that there may be utility in programmatic research designed to better understanding the macro-level, micro-level, and individual factors that are contributing to increased negative affect in the United States compared to other countries.
The present findings also show that studies using Form Y of the STAI demonstrate larger effects for individuals with anxiety-related disorders compared to nonclinical comparison groups than studies that used Form X, but no differences were found when comparing individuals with depressive disorders and nonclinical comparison groups. This finding supports the use of the revised Form Y and demonstrates its increased specificity to detect anxiety compared to Form X. There were no statistically significant moderators in the meta-regression model comparing individuals with anxiety-related disorders to individuals with depressive disorders, though these analyses may have been limited due to a smaller number of studies that conducted these direct comparisons.
Treatment Implications
Evidence that traits, or at minimum the behavioral manifestations of traits, can change over the lifespan has influenced the conceptualization and treatment of personality disorders (Clark, 2009). If traits can change over time, perhaps traits that influence anxiety and depression are malleable to treatment. Pharmacological research has found that antidepressant medication leads to significant changes in emotional temperament, which subsequently affect changes at the symptom level (Soskin et al., 2012). More specifically, a population-based cohort study in Finland found a small but statistically significant decrease in STAI-T scores over a seven- to ten-year period for individuals taking an antidepressant (Nabi et al., 2013). Multiple psychotherapy studies also demonstrate reductions in STAI-T for patients undergoing treatment. In a review of six studies, Fisher and Durham (1999) found that GAD patients’ STAI-T scores consistently decreased after a variety of therapeutic approaches to treatment (anxiety management training, analytical psychotherapy, behavior therapy, cognitive therapy, and non-directive therapy), though the strongest effects were found for individuals receiving cognitive-behavioral therapy (CBT) or applied relaxation. More recent studies have found statistically significant decreases in STAI-T scores for GAD patients receiving CBT (Newman et al., 2011) and meta-cognitive therapy (Wells et al., 2010), with reductions maintained over one- to two-year follow-up. In a sample of individuals with heterogenous anxiety-related disorders, STAI-T scores significantly decreased after mindfulness-based stress reduction, and this decrease was maintained at six-month follow-up (Vøllestad et al., 2011). Taken together, these results show that STAI-T scores are malleable, which would suggest that negative affectivity/neuroticism does respond to treatment.
Although negative affectivity/neuroticism decreases after psychological and pharmacological interventions, few treatments directly target this this trait. However, Barlow and colleagues (2014) have suggested that psychological interventions should specifically target negative affectivity/neuroticism, rather than features of emotional disorders such as anxiety and depression. The Unified Protocol (UP) for the Treatment of Mental Disorders was developed with this goal in mind. Initial evidence suggests that this treatment can reduce negative affectivity/neuroticism compared to a waitlist control group, and this decrease in negative affectivity/neuroticism predicted decreases in anxiety and depressive symptoms and functional impairment (Carl et al., 2013). Although head-to-head tests of the protocol compared to other treatments will be needed to demonstrate any relative strengths of the UP in decreasing negative affectivity/neuroticism, these results demonstrate promise that psychological interventions can effectively target negative affectivity, and the STAI-T may be a useful outcome measure in such studies.
Study Limitations and Suggestions for Future Research
The results of these meta-analyses must be considered in light of several limitations. First, although direct comparisons between individuals with anxiety and depressive disorders and correlational examinations between the STAI-T and measures of anxiety and depression were robust to publication bias according to several applied metrics (funnel plot inspection and fail-safe N’s), comparisons of STAI-T scores between nonclinical comparison groups and individuals with anxiety-related disorders and with individuals with depressive disorders had significantly asymmetric funnel plots. Egger et al. (1998) have suggested that funnel plots are less useful in observational meta-analyses due to the extensive degree of heterogeneity between studies that may affect the results. Funnel plots are typically used as a depiction of publication bias, but they actually depict small-study effects (Sterne et al., 2000). It is possible that the sampling of the nonclinical comparison group varied systematically between large and small studies; for example, larger studies may have conducted less rigorous screening of nonclinical comparison groups due to the substantial time these procedures may take in large samples, whereas smaller neuroimaging studies may have nonclinical comparison groups that were precisely matched and screened to exclude any history of anxiety or depression. Given that the STAI-T was not the main outcome reported in the vast majority of these studies, but rather included as part of the descriptive statistics of the samples, it is unlikely that these asymmetrical funnel plots are due to a bias toward publishing statistically significant results, as might be the case in meta-analyses comparing the effects of interventions. Additionally, the fail-safe N’s for both meta-analyses are extremely large (Tables 1 and 3), suggesting that a huge number of studies with nonsignificant differences in STAI-T scores between clinically anxious or depressed individuals and nonclinical comparison groups would need to be missing from the present analyses in order for the estimated effect sizes to be nonsignificant.
Although a large number of studies were included in the present meta-analyses, some analyses included a small number of studies. In particular, Field (2001) suggests that meta-analyses of correlation coefficients should be conducted only when there are 30 samples or more due to the degree of heterogeneity among the studies and inflated Type I error rate. The correlational meta-analyses conducted in the present study contained 12 and 15 samples, largely because these studies were limited to individuals with clinically diagnosed anxiety and/or depression. Multiple large-scale studies have been conducted demonstrating stronger correlations between the STAI-T and measures of depression than between the STAI-T and measures of anxiety in nonclinical samples (Bados et al., 2010; Balsamo et al., 2013). However, future research could extend this work by using a meta-analytic approach to examine correlations among the STAI-T and measures of anxiety and depression in both clinical and nonclinical samples.
Other study sampling limitations may have affected the results of this meta-analytic review. For example, unpublished studies and dissertations were not included. Additionally, only peer-reviewed studies published in English were included. Because region was a statistically significant moderator of the differences in STAI-T scores between clinical and nonclinical groups, it is likely that the inclusion of studies published in languages other than English may have influenced the findings. It is unclear whether these regional differences are due to differences in translations of the STAI-T or due to true population-level differences. Although the present meta-analysis is strengthened by the examination of multiple potential moderators, some studies did not include information regarding comorbidity, medication use, or the form of the STAI-T used, which prevented testing of multiple moderators within a single meta-regression model. In addition, the racial and ethnic identities of participants were usually not reported, precluding analysis of these potentially important moderators.
Finally, a number of other unmeasured variables (IQ, genetic background/family history, previous mental health history) could have impacted these results. Such variables were often not included in the studies used in the present meta-analyses. Further investigation into the effects of these various factors on scores on the STAI may be warranted. In addition, due to the meta-analytic techniques employed in the present study, other methods of assessing a measure’s psychometric properties could not be used, such as the use of informant reports or social desirability scales or examinations of concordance with behavioral and psychophysiological measures. There is much left to understand about the construct of trait anxiety as a whole, but the existing evidence suggests that the STAI-T may not be a valid measure of trait anxiety.
Despite the study limitations, the present findings have important implications for future research. The deeply established research background of the STAI suggests that this measure will not fade into obscurity. Indeed, the existence of thousands of studies that provide comparative STAI-T scores in varied populations is informative and should not be discarded. However, future studies that use the STAI-T must consider the measure in light of the available validity evidence. Studies that choose to employ the STAI-T must be careful to specify that the measure reflects trait negative affectivity/neuroticism, rather than trait anxiety. Researchers that are interested in the construct of trait anxiety as a measure of individual differences in the predisposition to experience fear, worry, and anxiety should consider measures such as the STICSA (Grös et al., 2007) that have better discriminant evidence of validity with measures of depression.
Conclusion
These findings suggest that trait anxiety may be a clinically meaningful construct that is in search of a more valid measure. Although the STAI-T cannot be considered a valid, specific measure of trait anxiety, these results do not diminish the value of the construct. Earlier, we defined trait anxiety as “an individual’s tendency to appraise situations as threatening, avoid anxiety-provoking situations, and demonstrate high baseline physiological arousal,” based on Elwood and colleagues’ review of the measurement and correlates of anxious traits (Elwood et al., 2012). There is utility in examining this pattern of responding to and preparing for threat separately from the tendency to experience negative emotions. The National Institute of Mental Health’s Research Domain Criteria (RDoC; Insel et al., 2010; Sanislow et al., 2010) provide one avenue by which to consider the measurement of trait anxiety. In the RDoC matrix, anxiety is referred to as Potential Threat:
Activation of a brain system in which harm may potentially occur but is distant, ambiguous, or low/uncertain in probability, characterized by a pattern of responses such as enhanced risk assessment (vigilance). These responses to low imminence threats are qualitatively different than the high imminence threat behaviors that characterize fear (https://www.nimh.nih.gov/research/research-funded-by-nimh/rdoc/constructs/potential-threat-anxiety.shtml).
The RDoC matrix was specifically created to examine potential mechanisms underlying psychopathology. It aims to study psychological constructs across multiple levels of analysis, including self-report, neural circuits, and physiological responses to established paradigms. Self-report measures of Potential Threat included in the RDoC matrix assess anxiety sensitivity, fear of negative evaluation, intolerance of uncertainty, and behavioral inhibition, as well as responses to stressful life events. Hierarchical measures of anxiety (Carleton, 2016; Lilienfeld et al., 1993; Olatunji & Wolitzky-Taylor, 2009) suggest that these are lower-order factors nested under trait anxiety, which itself is subsumed under negative affectivity/neuroticism. Although these measures are useful in examining specific aspects of responses to Potential Threat, there is not yet a valid measure that captures an individual’s overall trait responsivity to Potential Threat. Even the STICSA, which has better discriminant evidence of validity than the STAI-T, does not directly assess an individual’s typical response to Potential Threat. The STICSA contains questions that assess cognitive and somatic aspects of anxiety in reference to an individual’s “general mood state,” such as “My heart beats fast” and “I can’t get some thought out of my mind” (Grös et al., 2007), but it does not ask individuals to reflect on how they evaluate or respond to potential threats in their environment. A comprehensive self-report measure of potential threat would include items about hypervigilance, checking behavior, freezing, and repetitive thinking in the context of uncertain situations. Informant reports would also be useful, especially when examining the responses of children or for individuals who have limited insight into their own thoughts and behavior in uncertain, potentially threatening situations.
Potential Threat is unlikely to be fully captured or understood based on self-reported measures alone. Behavioral tasks that can assess in vivo behavior in ecologically valid, potentially threatening situations are also needed. Theories of trait anxiety and responses to Potential Threat should integrate available evidence from genetic, neurobiological, psychophysiological, and behavioral research along with self- and informant reports for a more complete understanding of this construct. In one such model, Weger and Sandi (2018) propose a stress-diathesis model that demonstrates how trait anxiety can lead to depression, integrating genetic and epigenetic risk factors identified through animal and human research with an understanding of the impacts of environmental conditions and stress. In suboptimal environmental conditions, individuals may be more likely to employ maladaptive behavioral strategies to cope with stress, leading to the development of anxiety and depression. For example, an individual with a biological predisposition toward trait anxiety raised in a highly stressful environment with a lack of parental support or modeling of effective coping is more likely to develop an anxiety-related disorder compared to an individual with a similar biological predisposition raised in a lower stress environment with supportive, non-accommodating parents. However, this model does not distinguish between contexts and strategies that predispose an individual to developing anxiety vs. depression. Figure 1 outlines one potential pathway from maladaptive coping strategies to clinically significant anxiety, with an emphasis on relevant cognitive biases and maladaptive behavioral strategies. Such integrative models outline the proposed pathway from high trait anxiety to the development and maintenance of anxiety-related psychopathology and suggest the Potential Threat framework to guide future multimodal research on trait anxiety.
Supplementary Material
Highlights.
Depressed individuals have higher STAI-T scores than anxious individuals.
Anxiety and depressive symptoms are both strongly correlated with STAI-T scores.
The STAI-T does not appear to specifically measure trait anxiety.
The STAI-T should be considered a nonspecific measure of negative affectivity.
Acknowledgements
The authors would like to thank the undergraduate research assistants in the Emotion and Anxiety Research Laboratory for their assistance in reviewing abstracts for inclusion in the meta-analysis. In addition, the authors would like to thank Maria Sanin and Max Luber for their assistance in article review and data entry. Finally, the authors would like to thank Drs. Jennifer Blackford, David Cole, and Steve Hollon for their helpful feedback.
Role of Funding Sources
The lead graduate student author (K. Knowles) was supported by a predoctoral fellowship training grant awarded by the National Institute of Mental Health (T32 MH018921-29). The funding agency had no role in conducting the synthesis or in deciding to publish the results.
Author Biography
Kelly A. Knowles, M.A., is a PhD candidate in Clinical Psychology at Vanderbilt University. She is broadly interested in the dissemination of clinical science and evidence-based treatment for anxiety and obsessive-compulsive disorders. Her work focuses on potential mechanisms of the development, maintenance, and treatment of anxiety and OCD.
Bunmi O. Olatunji, Ph.D., is the Gertrude Conaway Vanderbilt Professor of Psychology at Vanderbilt University. His primary research interest involves multilevel examination of cognitive behavioral theory, assessment, and therapy for anxiety disorders. He is currently adopting an experimental psychopathology framework to examine the role of basic emotions, especially disgust, as they relate to the assessment, etiology, and maintenance of anxiety-related disorders.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest: The authors reported no conflict of interest.
The effect sizes cannot be directly compared as they were calculated based on studies of samples that are not fully independent (i.e., some studies included a group with anxiety-related disorders, a group with depressive disorders, and the same nonclinical comparison was used for both groups; Lipsey & Wilson, 2001).
In structural models of psychopathology, OCD sometimes loads onto a separate thought disorder factor rather than an internalizing factor (Caspi et al., 2014).
References
- American Educational Research Association, American Psychological Association, and National Council on Measurement in Education. (2014). Standards for educational and psychological testing. Washington, DC: American Psychological Association. [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author. [Google Scholar]
- Andrews G (1991). Anxiety, personality and anxiety disorders. International Review of Psychiatry, 3, 293–302. doi: 10.3109/09540269109110408 [DOI] [Google Scholar]
- Asmundson GJG (2019). A rose by any other name…How should we refer to the collective of conditions characterized by clinically significant anxiety? Journal of Anxiety Disorders. doi: 10.1016/j.janxdis.2019.102143 [DOI] [PubMed] [Google Scholar]
- Avery SN, Clauss JA, & Blackford JU (2016). The human BNST: Functional role in anxiety and addiction. Neuropsychopharmacology, 41(1), 126–141. doi: 10.1038/npp.2015.185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bados A, Gómez-Benito J, & Balaguer G (2010). The state-trait anxiety inventory, trait version: Does it really measure anxiety? Journal of Personality Assessment, 92(6), 560–567. doi: 10.1080/00223891.2010.513295 [DOI] [PubMed] [Google Scholar]
- Baloglu M, Abbasi A, & Masten WG (2007). A cross-cultural comparison of anxiety among college students. College Student Journal, 41(4), 977–985. [Google Scholar]
- Bar-Haim Y, Lamy D, Pergamin L, Bakermans-Kranenburg MJ, & van IJzendoorn MH (2007). Threat-related attentional bias in anxious and nonanxious individuals: A meta-analytic study. Psychological Bulletin, 133(1), 1–24. doi: 10.1037/0033-2909.133.1.1 [DOI] [PubMed] [Google Scholar]
- Barlow DH (1988). Anxiety and its disorders: The nature and treatment of anxiety and panic. New York: Guilford Press. [Google Scholar]
- Barlow DH, DiNardo PA, Vermilyea BB, Vermilyea J, & Blanchard E (1986). Comorbidity and depression among the anxiety disorders. Journal of Nervous and Mental Disease, 174, 63–72. [DOI] [PubMed] [Google Scholar]
- Barlow DH, Sauer-Zavala S, Carl JR, Bullis JR, & Ellard KK (2014). The nature, diagnosis, and treatment of neuroticism: Back to the future. Clinical Psychological Science, 2(3), 344–365. doi: 10.1177/2167702613505532 [DOI] [Google Scholar]
- Basten U, Stelzel C, & Fiebach CJ (2012). Trait anxiety and the neural efficiency of manipulation in working memory. Cognitive, Affective and Behavioral Neuroscience, 12(3), 571–588. doi: 10.3758/s13415-012-0100-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bech P (1993). Rating scales for psychopathology, health status and quality of life (pp. 325–340). New York: Springer. [Google Scholar]
- Beck AT, Rush J, & Shaw BF (1979). Cognitive therapy of depression. New York: Guilford Press. [Google Scholar]
- Beck AT, Steer RA, & Brown GK (1996). Manual for the Beck Depression Inventory, 2nd edition The Psychological Association, San Antonio, TX. [Google Scholar]
- Beck AT, Ward CH, Mendelson M, Mock J, & Erbaugh J (1961). An inventory for measuring depression. Archives of General Psychiatry, 4(6), 561–571. doi: 10.1001/archpsyc.1961.01710120031004 [DOI] [PubMed] [Google Scholar]
- Beck JG, Coffey SF, Palyo SA, Gudmundsdottir B, Miller LM, & Colder CR (2004). Psychometric properties of the Posttraumatic Cognitions Inventory (PTCI): A replication with motor vehicle accident survivors. Psychological Assessment, 16(3), 289–298. doi: 10.1037/1040-3590.16.3.289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ben-Zur H, & Zeidner M (1988). Sex differences in anxiety, curiosity, and anger: A cross-cultural study. Sex Roles, 19(5–6), 335–347. 10.1007/BF00289841 [DOI] [Google Scholar]
- Bienvenu OJ, Brown C, Samuels JF, Liang KY, Costa PT, Eaton WW, & Nestadt G (2001). Normal personality traits and comorbidity among phobic, panic and major depressive disorders. Psychiatry Research, 102(1), 73–85. doi: 10.1016/S0165-1781(01)00228-1 [DOI] [PubMed] [Google Scholar]
- Bishop SJ (2009). Trait anxiety and impoverished prefrontal control of attention. Nature Neuroscience, 12(1), 92–98. doi: 10.1038/nn.2242 [DOI] [PubMed] [Google Scholar]
- Boffa JW, Norr AM, Raines AM, Albanese BJ, Short NA, & Schmidt NB (2016). Anxiety sensitivity prospectively predicts posttraumatic stress symptoms following a campus shooting. Behavior Therapy, 47, 367–376. doi: 10.1016/j.beth.2016.02.006 [DOI] [PubMed] [Google Scholar]
- Booth RW, Sharma D, & Leader TI (2016). The age of anxiety? It depends where you look: Changes in STAI trait anxiety, 1970–2010. Social Psychiatry and Psychiatric Epidemiology, 51(2), 193–202. 10.1007/s00127-015-1096-0 [DOI] [PubMed] [Google Scholar]
- Borenstein M, Hedges LV, Higgins JP, & Rothstein HR (2009). Effect sizes based on correlations Introduction to meta-analysis (pp. 41–43). West Sussex, United Kingdom: John Wiley & Sons. [Google Scholar]
- Borenstein M, Hedges L, Higgins J, & Rothstein H (2014). Comprehensive meta-analysis version 3.3 Biostat: Englewood, New Jersey. [Google Scholar]
- Brown TA (2007). Temporal course and structural relationships among dimensions of temperament and DSM-IV anxiety and mood disorder constructs. Journal of Abnormal Psychology, 116(2), 313–328. doi: 10.1037/0021-843X.116.2.313 [DOI] [PubMed] [Google Scholar]
- Brown TA, Chorpita BF, & Barlow DH (1998). Structural relationships among dimensions of the DSM-IV anxiety and mood disorders and dimensions of negative affect, positive affect, and autonomic arousal. Journal of Abnormal Psychology, 107(2), 179–192. [DOI] [PubMed] [Google Scholar]
- Brown TA, & Naragon-Gainey K (2013). Evaluation of the unique and specific contributions of dimensions of the triple vulnerability model to the prediction of DSM-IV anxiety and mood disorder constructs. Behavior Therapy, 44(2), 277–292. doi: 10.1016/j.beth.2012.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryant RA, Harvey AG, Dang ST, & Sackville T (1998). Assessing acute stress disorder: Psychometric properties of a structured clinical interview. Psychological Assessment, 10, 215–220. doi: 10.1037/1040-3590.10.3.215 [DOI] [Google Scholar]
- Calvo MG, & Cano-Vindel A (1997). The nature of trait anxiety: Cognitive and biological vulnerability. European Psychologist, 2(4), 301–312. doi: 10.1027/1016-9040.2.4.301 [DOI] [Google Scholar]
- Carleton RN (2016). Fear of the unknown: One fear to rule them all? Journal of Anxiety Disorders, 41, 5–21. doi: 10.1016/j.janxdis.2016.03.011 [DOI] [PubMed] [Google Scholar]
- Carver CS, & White TL (1994). Behavioral inhibition, behavioral activation, and affective responses to impending reward and punishment: The BIS/BAS scales. Journal of Personality and Social Psychology, 67, 319–333. [Google Scholar]
- Caspi A, Houts RM, Belsky DW, Goldman-Mellor SJ, Harrington H, Israel S, … Moffitt TE (2014). The p factor: One general psychopathology factor in the structure of psychiatric disorders? Clinical Psychological Science, 2(2), 119–137. doi: 10.1177/2167702613497473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cattell RB (1946). The description and measurement of personality. Yonkers-on-Hudson, NY: World Book. [Google Scholar]
- Cattell RB, & Scheier IH (1958). The nature of anxiety: A review of thirteen multivariate analyses comprising 814 variables. Psychological Reports, 4(3), 351–388. [Google Scholar]
- Cattell RB, & Scheier IH (1961). The meaning and measurement of neuroticism and anxiety. New York: The Ronald Press Company. [Google Scholar]
- Chambers JA, Power KG, & Durham RC (2004). The relationship between trait vulnerability and anxiety and depressive diagnoses at long-term follow-up of generalized anxiety disorder. Journal of Anxiety Disorders, 18(5), 587–607. doi:/ 10.1016/j.janxdis.2003.09.001 [DOI] [PubMed] [Google Scholar]
- Chou K (2009). Specific phobia in older adults: Evidence from the National Epidemiologic Survey on Alcohol and Related Conditions. The American Journal of Geriatric Psychiatry, 17(5), 376–386. doi: 10.1097/JGP.0b013e3181943214 [DOI] [PubMed] [Google Scholar]
- Clark DA, & Beck AT (2010). Cognitive therapy of anxiety disorders: Science and practice. New York, NY: Guilford Press. [Google Scholar]
- Clark LA (2009). Stability and change in personality disorder. Current Directions in Psychological Science, 18(1), 27–31. doi: 10.1111/j.1467-8721.2009.01600.x [DOI] [Google Scholar]
- Clark LA, & Watson D (1991a). Theoretical and empirical issues in differentiating depression from anxiety In Becker J & Kleinman A (Eds.), Psychosocial aspects of depression (pp. 39–65). Hillsdale, NJ, US: Lawrence Erlbaum Associates, Inc. [Google Scholar]
- Clark LA, & Watson D (1991b). Tripartite model of anxiety and depression: Psychometric evidence and taxonomic implications. Journal of Abnormal Psychology, 100(3), 316–336. [DOI] [PubMed] [Google Scholar]
- Clark LA, Watson D, & Mineka S (1994). Temperament, personality, and the mood and anxiety disorders. Journal of Abnormal Psychology, 103(1), 103–116. [PubMed] [Google Scholar]
- Cohen J (1992). A power primer. Psychological Bulletin, 112(1), 155–159. doi: 10.1037/0033-2909.112.1.155 [DOI] [PubMed] [Google Scholar]
- Cole DA, Martin NC, & Steiger JH (2005). Empirical and conceptual problems with longitudinal trait–state models: Support for a trait–state–occasion model. Psychological Methods, 10, 3–20. doi: 10.1037/1082-989X.10.1.3 [DOI] [PubMed] [Google Scholar]
- Connor KM, Davidson JR, Churchill LE, Sherwood A, Weisler RH, & Foa E (2000). Psychometric properties of the Social Phobia Inventory (SPIN): New self-rating scale. The British Journal of Psychiatry, 176(4), 379–386. doi: 10.1192/bjp.176.4.379 [DOI] [PubMed] [Google Scholar]
- Cooper AJ, Perkins AM, & Corr PJ (2007). A confirmatory factor analytic study of anxiety, fear, and behavioral inhibition system measures. Journal of Individual Differences, 28(4), 179–187. doi: 10.1027/1614-0001.28.4.179 [DOI] [Google Scholar]
- Costa PTJ, & McCrae RR (1992). Revised NEO Personality Inventory (NEO-PI-R) and the Five Factor Inventory (NEO-FFI): Professional Manual. Psychological Assessment Resources, Inc., Odessa, FL. [Google Scholar]
- Dammen T, Ekeberg Ø, Arnesen H, & Friis S (2008). Health-related quality of life in non-cardiac chest pain patients with and without panic disorder. The International Journal of Psychiatry in Medicine, 38(3), 271–286. doi: 10.2190/PM.38.3.d [DOI] [PubMed] [Google Scholar]
- Davidson JR, Book SW, Colket JT, Tupler LA, Roth S, David D, … & Davison RM (1997). Assessment of a new self-rating scale for post-traumatic stress disorder. Psychological Medicine, 27(1), 153–160. doi: 10.1017/S0033291796004229 [DOI] [PubMed] [Google Scholar]
- De Raedt R, Hertel PT, & Watkins ER (2015). Mechanisms of repetitive thinking: Introduction to the special series. Clinical Psychological Science, 3(4), 568–573. Doi: 10.1177/2167702615584309 [DOI] [Google Scholar]
- Dobson KS (1985). An analysis of anxiety and depression scales. Journal of Personality Assessment, 49(5), 522–527. doi: 10.1207/s15327752jpa4905_10 [DOI] [PubMed] [Google Scholar]
- Egger M, Schneider M, & Smith GD (1998). Spurious precision? Meta-analysis of observational studies. BMJ, 316, 140–144. doi: 10.1136/bmj.316.7125.140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egger M, Smith GD, Schneider M, & Minder C (1997). Bias in meta-analysis detected by a simple, graphical test. BMJ, 315, 629–634. doi: 10.1136/bmj.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elwood LS, Wolitzky-Taylor K, & Olatunji BO (2012). Measurement of anxious traits: A contemporary review and synthesis. Anxiety, Stress and Coping, 25(6), 647–666. doi: 10.1080/10615806.2011.582949 [DOI] [PubMed] [Google Scholar]
- El-Zahhar NE, & Hocevar D (1991). Cultural and sexual differences in test anxiety, trait anxiety and arousability: Egypt, Brazil, and the United States. Journal of Cross-Cultural Psychology, 22(2), 238–249. 10.1177/0022022191222005 [DOI] [Google Scholar]
- Endler NS, Parker JD, Bagby RM, & Cox BJ (1991). Multidimensionality of state and trait anxiety: Factor structure of the Endler Multidimensional Anxiety Scales. Journal of Personality and Social Psychology, 60(6), 919–926. [DOI] [PubMed] [Google Scholar]
- Eysenck MW (1992). Anxiety The cognitive perspective. Hove: Erlbaum. doi: 10.4324/9780203775677 [DOI] [Google Scholar]
- Feldman LA (1993). Distinguishing depression and anxiety in self-report: Evidence from confirmatory factor analysis on nonclinical and clinical samples. Journal of Consulting and Clinical Psychology, 61(4), 631–638. doi: 10.1037/0022-006X.61.4.631 [DOI] [PubMed] [Google Scholar]
- Field AP (2001). Meta-analysis of correlation coefficients: A Monte Carlo comparison of fixed-and random-effects methods. Psychological Methods, 6(2), 161–180. doi: 10.1037/1082-989X.6.2.161 [DOI] [PubMed] [Google Scholar]
- Fisher PL, & Durham RC (1999). Recovery rates in generalized anxiety disorder following psychological therapy: An analysis of clinically significant change in the STAI-T across outcome studies since 1990. Psychological Medicine, 29(6), 1425–1434. doi: 10.1017/S0033291799001336 [DOI] [PubMed] [Google Scholar]
- Foa EB, Huppert JD, Leiberg S, Langner R, Kichic R, Hajcak G, & Salkovskis PM (2002). The Obsessive-Compulsive Inventory: Development and validation of a short version. Psychological Assessment, 14, 485–495. doi: 10.1037/1040-3590.14.4.485 [DOI] [PubMed] [Google Scholar]
- Foa EB, Tolin DF, Ehlers A, Clark DM, & Orsillo SM (1999). The Posttraumatic Cognitions Inventory (PTCI): Development and validation. Psychological Assessment, 11(3), 303–314. doi: 10.1037/1040-3590.11.3.303 [DOI] [Google Scholar]
- Gamez W, Watson D, & Doebbeling BN (2007). Abnormal personality and the mood and anxiety disorders: Implications for structural models of anxiety and depression. Journal of Anxiety Disorders, 21(4), 526–539. doi: 10.1016/j.janxdis.2006.08.003 [DOI] [PubMed] [Google Scholar]
- Gawda B, & Szepietowska E (2016). Trait anxiety modulates brain activity during performance of verbal fluency tasks. Frontiers in Behavioral Neuroscience, 10, 1–15. doi: 10.3389/fnbeh.2016.00010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gazendam FJ, Kamphuis JH, & Kindt M (2013). Deficient safety learning characterizes high trait anxious individuals. Biological Psychology, 92(2), 342–352. doi: 10.1016/j.biopsycho.2012.11.006 [DOI] [PubMed] [Google Scholar]
- Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischmann RL, Hill CL … & Charney DS (1989). The Yale-Brown Obsessive-Compulsive Scale. I. Development, use, and reliability. Archives of General Psychiatry, 46, 1006–1011. [DOI] [PubMed] [Google Scholar]
- Gotlib IH (1984). Depression and general psychopathology in university students. Journal of Abnormal Psychology, 93(1), 19–30. doi: 10.1037/0021-843X.93.1.19 [DOI] [PubMed] [Google Scholar]
- Gotlib IH, & Cane DB (1989). Self-report assessment of depression and anxiety In Kendall EC & Watson D (Eds.), Anxiety and depression: Distinctive and overlapping features (pp. 131–169). New York: Academic Press. [Google Scholar]
- Griffith JW, Zinbarg RE, Craske MG, Mineka S, Rose RD, Waters AM, & Sutton JM (2010). Neuroticism as a common dimension in the internalizing disorders. Psychological Medicine, 40, 1125–1136. doi: 10.1017/S0033291709991449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grös DF, Antony MM, Simms LJ, & McCabe RE (2007). Psychometric Properties of the State-Trait Inventory for Cognitive and Somatic Anxiety (STICSA): Comparison to the State-Trait Anxiety Inventory (STAI). Psychological Assessment, 19(4), 369–381. doi: 10.1037/1040-3590.19.4.369 [DOI] [PubMed] [Google Scholar]
- Haddad ADM, Pritchett D, Lissek S, & Lau JYF (2012). Trait anxiety and fear responses to safety cues: Stimulus generalization or sensitization? Journal of Psychopathology and Behavioral Assessment, 34(3), 323–331. doi: 10.1007/s10862-012-9284-7 [DOI] [Google Scholar]
- Hallion LS, Sockol LE, & Wilhelm S (2015). Obsessive-compulsive disorder In Stein DJ, & Vythilingum B (Eds.), Anxiety disorders and gender (pp. 69–87). Springer International Publishing, New York, NY. doi: 10.1007/978-3-319-13060-6_4 [DOI] [Google Scholar]
- Higgins JP, & Green S (Eds.). (2011). Cochrane handbook for systematic reviews of interventions (Vol. 5.1). Available from www.handbook.cochrane.org. [Google Scholar]
- Hong RY (2013). From dispositional traits to psychopathological symptoms: Social-cognitive vulnerabilities as intervening mechanisms. Journal of Psychopathology and Behavioral Assessment, 35(4), 407–420. doi: 10.1007/s10862-013-9350-9 [DOI] [Google Scholar]
- Insel T, Cuthbert B, Garvey MA, Heinssen R, Pine DS, Quinn K, … Wang P (2010). Research Domain Criteria (RDoC): Toward a new classification framework for research on mental disorders. American Journal of Psychiatry, 167(7), 748–751. doi: 10.1176/appi.ajp.2010.09091379 [DOI] [PubMed] [Google Scholar]
- Jackson DN (1994). Jackson Personality Inventory-Revised. Sigma Assessment Systems, Research Psychologists Press Division. [Google Scholar]
- Jylhä P, Melartin T, & Isometsä E (2009). Relationships of neuroticism and extraversion with axis I and II comorbidity among patients with DSM-IV major depressive disorder. Journal of Affective Disorders, 114(1–3), 110–121. doi: 10.1016/j.jad.2008.06.011 [DOI] [PubMed] [Google Scholar]
- Kangas M, Henry JL, & Bryant RA (2005). Predictors of posttraumatic stress disorder following cancer. Health Psychology, 24, 579–585. [DOI] [PubMed] [Google Scholar]
- Kendall PC, Finch AJ, Auerbach SM, Hooke JF, & Mikulka PJ (1976). The State-Trait Anxiety Inventory: A systematic evaluation. Journal of Consulting and Clinical Psychology, 44(3), 406–412. doi: 10.1037/0022-006X.44.3.406 [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, & Walters EE (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62, 593–602. doi: 10.1001/archpsyc.62.6.593 [DOI] [PubMed] [Google Scholar]
- Kok L, Sep MS, Veldhuijzen DS, Cornelisse S, Nierich AP, van der Maaten J, … Hillegers MH (2016). Trait anxiety mediates the effect of stress exposure on post-traumatic stress disorder and depression risk in cardiac surgery patients. Journal of Affective Disorders, 206, 216–223. doi: 10.1016/j.jad.2016.07.020 [DOI] [PubMed] [Google Scholar]
- Kotov R, Gamez W, Schmidt F, & Watson D (2010). Linking “big” personality traits to anxiety, depressive, and substance use disorders: a meta-analysis. Psychological Bulletin, 136(5), 768–821. doi: 10.1037/a0020327 [DOI] [PubMed] [Google Scholar]
- Krueger RF (1999). The structure of common mental disorders. Archives of General Psychiatry, 56(10), 921–926. doi: 10.1001/archpsyc.56.10.921 [DOI] [PubMed] [Google Scholar]
- Krug SE, Scheier IH, & Cattell RB (1976). Handbook for the IPAT Anxiety Scale. Champaign, IL: Institute for Personality and Ability Testing. [Google Scholar]
- Kühn S, Schubert F, & Gallinat J (2011). Structural correlates of trait anxiety: Reduced thickness in medial orbitofrontal cortex accompanied by volume increase in nucleus accumbens. Journal of Affective Disorders, 134(1–3), 315–319. doi: 10.1016/j.jad.2011.06.003 [DOI] [PubMed] [Google Scholar]
- Lang PJ, McTeague LM, & Bradley MM (2016). RDoC, DSM, and the reflex physiology of fear: A biodimensional analysis of the anxiety disorders spectrum. Psychophysiology, 53(3), 336–347. doi: 10.1111/psyp.12462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laughlin SB, & Sejnowski TJ (2003). Communication in neuronal networks. Science, 301(5641), 1870–1874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laux L, Glanzmann P, Schaffner P, & Spielberger CD (1981). Das State-Trait-Angstinventar Theoretische Grundlagen und Handanweisung [State-Trait Anxiety Inventory. Theoretical foundations and manual] Weinheim: Beltz. [Google Scholar]
- Lee K, & Ashton MC (2004). Psychometric properties of the HEXACO Personality Inventory. Multivariate Behavioral Research, 39, 329–358. doi: 10.1207/s15327906mbr3902_8 [DOI] [PubMed] [Google Scholar]
- Liebowitz MR (1987). Social phobia. Modern Problems of Pharmacopsychiatry, 22, 141–173. [DOI] [PubMed] [Google Scholar]
- Lilienfeld S, Turner SM, & Jacob RG (1993). Anxiety sensitivity: An examination of theoretical and methodological issues. Advances in Behaviour Research and Therapy, 15, 147–183. [Google Scholar]
- Lipsey MW, & Wilson DB (2001). Practical Meta-Analysis. Thousand Oaks: SAGE Publications, Inc. [Google Scholar]
- Lonigan CJ, Shannon MP, Taylor CM, Finch AJ, & Sallee FR (1994). Children exposed to disaster: II. Risk factors for the development of post-traumatic symptomatology. Journal of the American Academy of Child & Adolescent Psychiatry, 33(1), 94–105. [DOI] [PubMed] [Google Scholar]
- Luteijn F, & Bouman TK (1988). The concepts of depression, anxiety, and neuroticism in questionnaires. European Journal of Personality, 2, 113–120. [Google Scholar]
- Marin MF, Zsido RG, Song H, Lasko NB, Killgore WDS, Rauch SL, … Milad MR (2017). Skin conductance responses and neural activations during fear conditioning and extinction recall across anxiety disorders. JAMA Psychiatry, 74(6), 622–631. doi: 10.1001/jamapsychiatry.2017.0329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin MM, & Rubin RB (1995). A new measure of cognitive flexibility. Psychological Reports, 76, 623–626. doi: 10.2466/pr0.1995.76.2.623 [DOI] [Google Scholar]
- McKay D, Danyko S, Neziroglu F, & Yaryura-Tobias JA (1995). Factor structure of the Yale-Brown Obsessive-Compulsive Scale: A two-dimensional measure. Behaviour Research and Therapy, 33(7), 865–869. [DOI] [PubMed] [Google Scholar]
- McLean CP, & Anderson ER (2009). Brave men and timid women? A review of the gender differences in fear and anxiety. Clinical Psychology Review, 29(6), 496–505. 10.1016/j.cpr.2009.05.003 [DOI] [PubMed] [Google Scholar]
- McLean CP, Asnaani A, Litz BT, & Hofmann SG (2011). Gender differences in anxiety disorders: Prevalence, course of illness, comorbidity and burden of illness. Journal of Psychiatric Research, 45(8), 1027–1035. doi: 10.1016/j.jpsychires.2011.03.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer TJ, Miller ML, Metzger RL, & Borkovec TD (1990). Development and validation of the Penn State Worry Questionnaire. Behaviour Research and Therapy, 28, 487–495. doi: 10.13072/midss.158 [DOI] [PubMed] [Google Scholar]
- Milad MR, & Rauch SL (2007). The role of the orbitofrontal cortex in anxiety disorders. Annals of the New York Academy of Sciences, 1121, 546–561. doi: 10.1196/annals.1401.006 [DOI] [PubMed] [Google Scholar]
- Mineka S, Watson D, & Clark LA (1998). Comorbidity of anxiety and unipolar mood disorders. Annual Review of Psychology, 49, 377–412. doi: 10.1146/annurev.psych.49.1.377 [DOI] [PubMed] [Google Scholar]
- Mineka S, & Zinbarg R (2006). A contemporary learning theory perspective on the etiology of anxiety disorders: It’s not what you thought it was. American Psychologist, 61(1), 10–26. doi: 10.1037/0003-066X.61.1.10 [DOI] [PubMed] [Google Scholar]
- Miskovich TA, Pedersen WS, Belleau EL, Shollenbarger S, Lisdahl KM, & Larson CL (2016). Cortical gyrification patterns associated with trait anxiety. PLoS One, 11(2). doi: 10.1371/journal.pone.0149434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitte K (2008). Memory bias for threatening information in anxiety and anxiety disorders: A meta-analytic review. Psychological Bulletin, 134(6), 886–911. doi: 10.1037/a0013343 [DOI] [PubMed] [Google Scholar]
- Mundy EA, Weber M, Rauch SL, Killgore WDS, Simon NM, Pollack MH, & Rosso IM (2015). Adult anxiety disorders in relation to trait anxiety and perceived stress in childhood. Psychological Reports, 117(2), 473–489. doi: 10.2466/02.10.PR0.117c17z6 [DOI] [PubMed] [Google Scholar]
- Muran EM, & Motta RW (1993). Cognitive distortions and irrational beliefs in post-traumatic stress, anxiety, and depressive disorders. Journal of Clinical Psychology, 49(2), 166–176. [DOI] [PubMed] [Google Scholar]
- Muris P, Merckelbach H, & Rassin E (2000). Monitoring, trait anxiety, and panic disorder symptomatology in normal subjects. Journal of Behavior Therapy and Experimental Psychiatry, 31, 21–28. [DOI] [PubMed] [Google Scholar]
- Muris P, Merckelbach H, Schmidt H, & Tierney S (1999). Disgust sensitivity, trait anxiety and anxiety disorders symptoms in normal children. Behaviour Research and Therapy, 37, 953–961. doi: 10.1016/S0005-7967(99)00045-5 [DOI] [PubMed] [Google Scholar]
- Muris P, Roelofs J, Rassin E, Franken I, & Mayer B (2005). Mediating effects of rumination and worry on the links between neuroticism, anxiety, and depression. Personality and Individual Differences, 39, 1105–1111. doi: 10.1016/j.paid.2005.04.005 [DOI] [Google Scholar]
- Nabi H, Virtanen M, Singh-Manoux A, Hagger-Johnson G, Pentti J, Kivimäki M, & Vahtera J (2013). Trait anxiety levels before and after antidepressant treatment: A 3-wave cohort study. Journal of Clinical Psychopharmacology, 33(3), 371–377. doi: 10.1097/JCP.0b013e31828b26c2 [DOI] [PubMed] [Google Scholar]
- Nakazato K, & Shimonaka Y (1989). The Japanese State-Trait Anxiety Inventory: Age and sex differences. Perceptual and Motor Skills, 69(2), 611–617. doi: 10.2466/pms.1989.69.2.611 [DOI] [PubMed] [Google Scholar]
- Naragon-Gainey K (2010). Meta-analysis of the relations of anxiety sensitivity to the depressive and anxiety disorders. Psychological Bulletin, 136(1), 128–150. doi: 10.1037/a0018055 [DOI] [PubMed] [Google Scholar]
- Naragon-Gainey K, & Watson D (2018). What lies beyond neuroticism? An examination of the unique contributions of social-cognitive vulnerabilities to internalizing disorders. Assessment, 25(2), 143–158. doi: 10.1177/1073191116659741 [DOI] [PubMed] [Google Scholar]
- Newman MG, Castonguay LG, Borkovec TD, Fisher AJ, Boswell JF, Szkodny LE, & Nordberg SS (2011). A randomized controlled trial of cognitive-behavioral therapy for generalized anxiety disorder with integrated techniques from emotion-focused and interpersonal therapies. Journal of Consulting and Clinical Psychology, 79(2), 171–181. doi: 10.1037/a0022489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nixon GF, & Steffeck JC (1977). Reliability of the State-Trait Anxiety Inventory. Psychological Reports, 40, 357–358. [DOI] [PubMed] [Google Scholar]
- Nordahl H, Hjemdal O, Hagen R, Nordahl HM, & Wells A (2019). What lies beneath trait-anxiety? Testing the self-regulatory executive function model of vulnerability. Frontiers in Psychology, 10, 1–8. doi: 10.3389/fpsyg.2019.00122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norton PJ, & Mehta PD (2007). Hierarchical model of vulnerabilities for emotional disorders. Cognitive Behaviour Therapy, 36(4), 240–254. doi: 10.1080/16506070701628065 [DOI] [PubMed] [Google Scholar]
- Olatunji BO, & Cole DA (2009). The longitudinal structure of general and specific anxiety dimensions in children: Testing a latent trait–state–occasion model. Psychological Assessment, 21(3), 412–424. doi: 10.1037/a0016206 [DOI] [PubMed] [Google Scholar]
- Olatunji BO, Williams NL, Lohr JM, Connolly KM, Cisler JM, & Meunier SA (2007). Structural differentiation of disgust from trait anxiety in the prediction of specific anxiety disorder symptoms. Behaviour Research and Therapy, 45(12), 3002–3017. doi: 10.1016/j.brat.2007.08.011 [DOI] [PubMed] [Google Scholar]
- Olatunji BO, & Wolitzky-Taylor KB (2009). Anxiety sensitivity and the anxiety disorders: A meta-analytic review and synthesis. Psychological Bulletin, 135(6), 974–999. doi: 10.1037/a0017428 [DOI] [PubMed] [Google Scholar]
- Orsillo SM, Weathers FW, Litz BT, Steinberg HR, Huska JA, & Keane TM (1996). Current and lifetime psychiatric disorders among veterans with war zone-related posttraumatic stress disorder. Journal of Nervous and Mental Disease, 184(5), 307–313. doi: 10.1097/00005053-199605000-00007 [DOI] [PubMed] [Google Scholar]
- Orwin R (1983). A fail-safe N for effect size in meta-analysis. Journal of Educational Statistics, 8(2), 157–159. doi: 10.2307/1164923 [DOI] [Google Scholar]
- Pacheco-Unguetti A, Acosta A, Marqués E, & Lupiáñez J (2011). Alterations of the attentional networks in patients with anxiety disorders. Journal of Anxiety Disorders, 25(7), 888–895. doi: 10.1016/j.janxdis.2011.04.010 [DOI] [PubMed] [Google Scholar]
- Paulus DJ, Talkovsky AM, Heggeness LF, & Norton PJ (2015). Beyond negative affectivity: A hierarchical model of global and transdiagnostic vulnerabilities for emotional disorders. Cognitive Behaviour Therapy, 44(5), 389–405. doi: 10.1080/16506073.2015.1017529 [DOI] [PubMed] [Google Scholar]
- Quintana DS, & Tiebel J (2019, August 20). How to calculate statistical power for your meta-analysis. 10.17605/OSF.IO/5C7UZ [DOI]
- Rachman SJ (1998). Anxiety. Hove: Psychology Press. [Google Scholar]
- Rapee RM (1991). Generalized anxiety disorder: A review of clinical features and theoretical concepts. Clinical Psychology Review, 11, 419–440. [Google Scholar]
- Rapee RM, & Medoro L (1994). Fear of physical sensations and trait anxiety as mediators of the response to hyperventilation in nonclinical subjects. Journal of Abnormal Psychology, 103(4), 693–699. doi: 10.1037/0021-843X.103.4.693 [DOI] [PubMed] [Google Scholar]
- Reiss S, & McNally RJ (1985). The expectancy model of fear In Reiss S & Bootzin RR (Eds.), Theoretical issues in behavior therapy (pp. 107–121). New York: Academic Press. [Google Scholar]
- Reynolds CR, Richmond BO, & Lowe PA (2003). The Adult Manifest Anxiety Scale: Manual. Los Angeles: Western Psychological Services. [Google Scholar]
- Ristvedt SL, & Trinkaus KM (2009). Trait anxiety as an independent predictor of poor health-related quality of life and post-traumatic stress symptoms in rectal cancer. British Journal of Health Psychology, 14(4), 701–715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts BW, Walton KE, & Viechtbauer W (2006). Patterns of mean-level change in personality traits across the life course: A meta-analysis of longitudinal studies. Psychological Bulletin, 132(1), 1–25. 10.1037/0033-2909.132.1.1 [DOI] [PubMed] [Google Scholar]
- Rodebaugh TL, Woods CM, & Heimberg RG (2007). The reverse of social anxiety is not always the opposite: The reverse-scored items of the Social Interaction Anxiety Scale do not belong. Behavior Therapy, 38(2), 192–206. doi: 10.1016/j.beth.2006.08.001 [DOI] [PubMed] [Google Scholar]
- Rosenthal R (1979). The file drawer problem and tolerance for null results. Psychological Bulletin, 86(3), 638–641. doi: 10.1037/0033-2909.86.3.638 [DOI] [Google Scholar]
- Sanislow CA, Pine DS, Quinn KJ, Kozak MJ, Garvey MA, Heinssen RK, … Cuthbert BN (2010). Developing constructs for psychopathology research: Research domain criteria. Journal of Abnormal Psychology, 119(4), 631–639. doi: 10.1037/a0020909 [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Zvolensky MJ, & Maner JK (2006). Anxiety sensitivity: Prospective prediction of panic attacks and Axis I pathology. Journal of Psychiatric Research, 40, 691–699. doi: 10.1016/j.jpsychires.2006.07.009 [DOI] [PubMed] [Google Scholar]
- Schmitt DP, Realo A, Voracek M, & Allik J (2008). Why can’t a man be more like a woman? Sex differences in big five personality traits across 55 cultures. Journal of Personality and Social Psychology, 94(1), 1168–182. doi: 10.1037/0022-3514.94.1.168 [DOI] [PubMed] [Google Scholar]
- Simon GE, Goldberg DP, Von Korff M, & Üstün TB (2002). Understanding cross-national differences in depression prevalence. Psychological Medicine, 32(4), 585–594. doi: 10.1017/S0033291702005457 [DOI] [PubMed] [Google Scholar]
- Skritskaya NA, Carson-Wong AR, Moeller JR, Shen S, Barsky AJ, & Fallon BA (2012). A clinician-administered severity rating scale for illness anxiety: Development, reliability, and validity of the H-YBOCS-M. Depression and Anxiety, 29(7), 652–664. doi: 10.1002/da.21949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Somerville LH, Whalen PJ, & Kelley WM (2010). Human bed nucleus of the stria terminalis indexes hypervigilant threat monitoring. Biological Psychiatry, 68(5), 416–424. doi: 10.1016/j.biopsych.2010.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soskin DP, Carl JR, Alpert J, & Fava M (2012). Antidepressant effects on emotional temperament: Toward a biobehavioral research paradigm for major depressive disorder. CNS Neuroscience and Therapeutics, 18(6), 441–451. doi: 10.1111/j.1755-5949.2012.00318.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spielberger CD (1966). Theory and research on anxiety In Spielberger CD (Ed.). Anxiety and behavior. New York: Academic Press. [Google Scholar]
- Spielberger CD (2010). State‐Trait Anxiety Inventory In Weiner IB & Craighead WE, (Eds.). The Corsini Encyclopedia of Psychology (Vol. 4, pp. 1698–1699). Hoboken, NJ: John Wiley & Sons. [Google Scholar]
- Spielberger CD, Gorsuch RL, & Lushene RE (1970). STAI: Manual for the State-Trait Anxiety Inventory. Palo Alto: Consulting Psychologists Press. [Google Scholar]
- Spielberger CD, Gorsuch RL, Lushene RE, Vagg PR, & Jacobs GA (1983). Manual for the State-Trait Anxiety Inventory (Form Y). Palo Alto, CA: Consulting Psychologists Press. [Google Scholar]
- Spielberger CD, Vagg PR, Barker LR, Donham GW & Westberry LG (1980). The factor structure of the State-Trait Anxiety Inventory In Sarason IG and Spielberger CD (Eds.), Stress and anxiety (Vol. 7, pp. 95–109). New York: Hemisphere/Wiley. [Google Scholar]
- Spinhoven P, van Hemert AM, & Penninx BW (2019). Repetitive negative thinking as a mediator in prospective cross-disorder associations between anxiety and depression disorders and their symptoms. Journal of Behavior Therapy and Experimental Psychiatry, 63, 6–11. doi: 10.1016/j.jbtep.2018.11.007 [DOI] [PubMed] [Google Scholar]
- Sterne JA, Gavaghan D, & Egger M (2000). Publication and related bias in meta-analysis: power of statistical tests and prevalence in the literature. Journal of Clinical Epidemiology, 53(11), 1119–1129. doi: 10.1016/S0895-4356(00)00242-0 [DOI] [PubMed] [Google Scholar]
- Steyer R, Majcen A-M, Schwenkmezger P, & Buchner A (1989). A latent state-trait anxiety model and its application to determine consistency and specificity coefficients. Anxiety Research, 1(4), 281–299. doi: 10.1080/08917778908248726 [DOI] [Google Scholar]
- Sylvers P, Lilienfeld SO, & LaPrairie JL (2011). Differences between trait fear and trait anxiety: Implications for psychopathology. Clinical Psychology Review, 31(1), 122–137. doi: 10.1016/j.cpr.2010.08.004 [DOI] [PubMed] [Google Scholar]
- Taylor JA (1953). A personality scale of manifest anxiety. The Journal of Abnormal and Social Psychology, 48(2), 285–290. [DOI] [PubMed] [Google Scholar]
- Taylor S (1993). The structure of fundamental fears. Journal of Behavior Therapy and Experimental Psychiatry, 24(4), 289–299. [DOI] [PubMed] [Google Scholar]
- Taylor S, Koch WJ, & Crockett DJ (1991). Anxiety sensitivity, trait anxiety, and the anxiety disorders. Journal of Anxiety Disorders, 5, 293–311. [Google Scholar]
- Torrents-Rodas D, Fullana MA, Bonillo A, Caseras X, Andión O, & Torrubia R (2013). No effect of trait anxiety on differential fear conditioning or fear generalization. Biological Psychology, 92(2), 185–190. doi: 10.1016/j.biopsycho.2012.10.006 [DOI] [PubMed] [Google Scholar]
- Tolin DF, Meunier SA, Frost RO, & Steketee G (2011). Hoarding among patients seeking treatment for anxiety disorders. Journal of Anxiety Disorders, 25, 43–48. doi: 10.1016/j.janxdis.2010.08.001 [DOI] [PubMed] [Google Scholar]
- Twenge JM (2000). The age of anxiety? Birth cohort change in anxiety. Journal of Personality and Social Psychology, 79(6), 1007–1021. [DOI] [PubMed] [Google Scholar]
- Vesga-López O, Schneier FR, Wang S, Heimberg RG, Liu S, Hasin DS, & Blanco C (2008). Gender differences in generalized anxiety disorder: Results from the national epidemiologic survey on alcohol and related conditions (NESARC). The Journal of Clinical Psychiatry, 69(10), 1606–1616. doi: 10.4088/JCP.v69n1011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vigneau F, & Cormier S (2008). The factor structure of the State-Trait Anxiety Inventory: An alternative view. Journal of Personality Assessment, 90(3), 280–285. doi: 10.1080/00223890701885027 [DOI] [PubMed] [Google Scholar]
- Vollebergh WAM, Iedema J, Bijl RV, De Graaf R, Smit F, & Ormel J (2001). The structure and stability of common mental disorders: The NEMESIS Study. Archives of General Psychiatry, 58(6), 597–603. doi: 10.1001/archpsyc.58.6.597 [DOI] [PubMed] [Google Scholar]
- Vøllestad J, Sivertsen B, & Nielsen GH (2011). Mindfulness-based stress reduction for patients with anxiety disorders: Evaluation in a randomized controlled trial. Behaviour Research and Therapy, 49, 281–288. doi: 10.1016/j.brat.2011.01.007 [DOI] [PubMed] [Google Scholar]
- Wang T, Li M, Xu S, Liu B, Wu T, Lu F, … Wang J (2019). Relations between trait anxiety and depression: A mediated moderation model. Journal of Affective Disorders, 244, 217–222. doi: 10.1016/j.jad.2018.09.074 [DOI] [PubMed] [Google Scholar]
- Watson D (2005). Rethinking the mood and anxiety disorders: A quantitative hierarchical model for DSM-V. Journal of Abnormal Psychology, 114(4), 522–536. doi: 10.1037/0021-843X.114.4.522 [DOI] [PubMed] [Google Scholar]
- Watson D, & Clark LA (1984). Negative affectivity: The disposition to experience aversive emotional states. Psychological Bulletin, 96(3), 465–490. [PubMed] [Google Scholar]
- Watson D, Clark LA, & Tellegen A (1988). Development and validation of brief measures of positive and negative affect. Journal of Personality and Social Psychology, 54(6), 1063–1070. [DOI] [PubMed] [Google Scholar]
- Watson D, Gamez W, & Simms LJ (2005). Basic dimensions of temperament and their relation to anxiety and depression: A symptom-based perspective. Journal of Research in Personality, 39, 46–66. doi: 10.1016/j.jrp.2004.09.006 [DOI] [Google Scholar]
- Watson D, O’Hara MW, & Stuart S (2008). Hierarchical structures of affect and psychopathology and their implications for the classification of emotional disorders. Depression and Anxiety, 25(4), 282–288. doi: 10.1002/da.20496 [DOI] [PubMed] [Google Scholar]
- Watson D, & Walker LM (1996). The long-term stability and predictive validity of trait measures of affect. Journal of Personality and Social Psychology, 70(3), 567–577. doi: 10.1037/0022-3514.70.3.567 [DOI] [PubMed] [Google Scholar]
- Weems CF, Pina AA, Costa NM, Watts SE, Taylor LK, & Cannon MF (2007). Predisaster trait anxiety and negative affect predict posttraumatic stress in youths after Hurricane Katrina. Journal of Consulting and Clinical Psychology, 75(1), 154–159. doi: 10.1037/0022-006X.75.1.154 [DOI] [PubMed] [Google Scholar]
- Weger M, & Sandi C (2018). High anxiety trait: A vulnerable phenotype for stress-induced depression. Neuroscience and Biobehavioral Reviews, 87, 27–37. 10.1016/j.neubiorev.2018.01.012 [DOI] [PubMed] [Google Scholar]
- Weinberger AH, Gbedemah M, Martinez AM, Nash D, Galea S, & Goodwin RD (2018). Trends in depression prevalence in the USA from 2005 to 2015: Widening disparities in vulnerable groups. Psychological Medicine, 48(8), 1308–1315. doi: 10.1017/S0033291717002781 [DOI] [PubMed] [Google Scholar]
- Wells A, & Carter KEP (2009). Maladaptive thought control strategies in generalized anxiety disorder, major depressive disorder, and nonpatient groups and relationships with trait anxiety. International Journal of Cognitive Therapy, 2(3), 224–234. doi: 10.1521/ijct.2009.2.3.224 [DOI] [Google Scholar]
- Wells A, Welford M, King P, Papageorgiou C, Wisely J, & Mendel E (2010). A pilot randomized trial of metacognitive therapy vs applied relaxation in the treatment of adults with generalized anxiety disorder. Behaviour Research and Therapy, 48(5), 429–434. doi: 10.1016/j.brat.2009.11.013 [DOI] [PubMed] [Google Scholar]
- Willmann M, Langlet C, Hainaut JP, & Bolmont B (2012). The time course of autonomic parameters and muscle tension during recovery following a moderate cognitive stressor: Dependency on trait anxiety level. International Journal of Psychophysiology, 84(1), 51–58. doi: 10.1016/j.ijpsycho.2012.01.009 [DOI] [PubMed] [Google Scholar]
- Wolpe J, & Lang PJ (1964). A Fear Survey Schedule for use in behaviour therapy Behaviour Research and Therapy, 2, 27–30. 10.1016/0005-7967(64)90051-8 [DOI] [PubMed] [Google Scholar]
- Wong AHK, & Lovibond PF (2018). Excessive generalisation of conditioned fear in trait anxious individuals under ambiguity. Behaviour Research and Therapy, 107, 53–63. doi: 10.1016/j.brat.2018.05.012 [DOI] [PubMed] [Google Scholar]
- World Health Organization; (2020). International statistical classification of diseases and related health problems (11th ed.). https://icd.who.int/ [Google Scholar]
- Wright AGC, Krueger RF, Hobbs MJ, Markon KE, Eaton NR, & Slade T (2013). The structure of psychopathology: Toward an expanded quantitative empirical model. Journal of Abnormal Psychology, 122(1), 281–294. doi: 10.1037/a0030133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xia J, He Q, Li Y, Xie D, Zhu S, Chen J, … Wang X (2011). The relationship between neuroticism, major depressive disorder and comorbid disorders in Chinese women. Journal of Affective Disorders, 135(1–3), 100–105. doi: 10.1016/j.jad.2011.06.053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zinbarg RE, & Barlow DH (1996). Structure of anxiety and the anxiety disorders: A hierarchical model. Journal of Abnormal Psychology, 105(2), 181–193. doi: 10.1037/0021-843X.105.2.181 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


