To the Editor,
5-Aminolevulinic acid (ALA) is utilized for photodynamic diagnosis to detect superficial bladder cancer and its adverse effect is hypotension [1–5]. Compared to general anesthesia, spinal anesthesia is not indicated as an increased risk factor for 5-ALA-induced hypotension from anesthesia induction to the start of surgery in patients undergoing transurethral resection of bladder tumor (TUR-BT) with 5-ALA [2, 3]. However, no studies exist that have investigated the precise perioperative hypotensive effects by 5-ALA under spinal anesthesia. This retrospective study assessed the hypotensive effect of 5-ALA on hemodynamic change of spinal anesthesia in patients undergoing TUR-BT not only during surgery but also after the ward admission.
The medical records of 129 patients who underwent TUR-BT under spinal anesthesia using 0.5% hyperbaric bupivacaine in Kyoto City Hospital between January 2018 and March 2019 were divided into two groups, based on whether 5-ALA was used (ALA group, n = 66) or not used (control group, n = 63). The ALA group received 5-ALA (20 mg/kg) orally 3 h before the start of surgery. The change in noninvasive blood pressure (BP) on the day of surgery and the dosage of vasopressors used during spinal anesthesia were analyzed.
No significant difference existed between the two groups in the patients’ preoperative characteristics. Intravenous fluid volume during anesthesia was significantly higher in the ALA group than in the control group (Table 1). Systolic and diastolic BP were significantly lower in the ALA group than in the control group from spinal anesthesia until 2 h after the ward admission. In the ALA group, systolic and diastolic BP significantly remained decreased from spinal anesthesia until 2 h after the ward admission (Fig. 1). The total dosage of ephedrine and phenylephrine were higher in the ALA group than in the control group (Table 1).
Table 1.
The patients’ preoperative characteristics, anesthesia profiles and the drugs administered during anesthesia
| Control group (n = 63) | ALA group (n = 66) | P value | |
|---|---|---|---|
| Age (years) | 71 ± 11 | 74 ± 10 | 0.27 |
| Height (cm) | 162 ± 15 | 161 ± 14 | 0.58 |
| Weight (kg) | 65 ± 17 | 65 ± 18 | 0.97 |
| Sex (male/female) | 59 (94%)/4 (6%) | 55 (83%)/11 (17%) | 0.07 |
| Regular use of antihypertensive drug | 24 (38%) | 23 (35%) | 0.70 |
| Regular use of renin-angiotensin system inhibitor | 14 (22%) | 11 (17%) | 0.42 |
| Duration of surgery (minutes) | 43 ± 25 | 44 ± 20 | 0.84 |
| Duration of anesthesia (minutes) | 75 ± 28 | 80 ± 22 | 0.25 |
| Dose of 0.5% hyperbaric bupivacaine of spinal anesthesia (mL) | 3.1 ± 0.3 | 3.0 ± 0.3 | 0.20 |
| Sensory block level just before surgerya | T8 (T2–T11) | T6 (T2–L1) | 0.26 |
| Sensory block level at the end of surgerya | T6 (T2–T12) | T5 (T2–T12) | 0.49 |
| Intravenous fluid volume during anesthesia (mL) | 570 ± 191 | 758 ± 284 | < 0.001 |
| Use of vasopressorsb | 10 (16%) | 47 (71%) | < 0.001 |
| Use of ephedrine | 8 (13%) | 37 (56%) | < 0.001 |
| Total dose of ephedrine (mg) | 1.0 ± 3.0 | 6.9 ± 9.0 | < 0.001 |
| Use of phenylephrine | 6 (10%) | 30 (45%) | < 0.001 |
| Total dose of phenylephrine (mg) | 0.013 ± 0.042 | 0.21 ± 0.34 | < 0.001 |
Values are presented as mean ± standard deviation or number (%)
aMedian (maximum-minimum)
bEphedrine or phenylephrine or both were used
ALA aminolevulinic acid
Fig. 1.
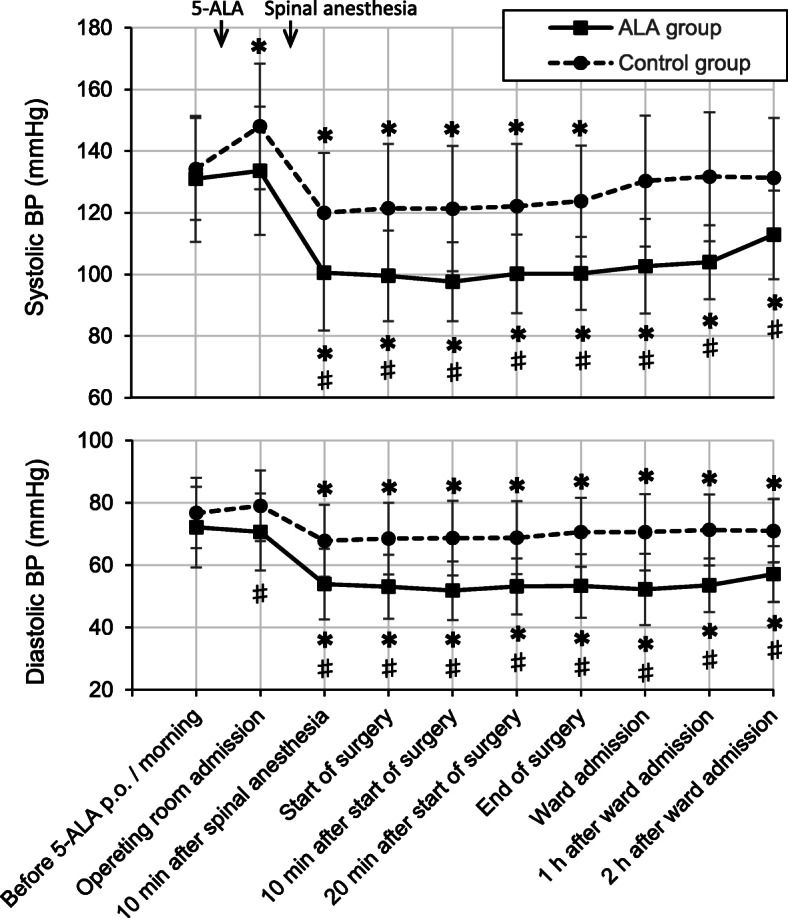
Time courses of systolic blood pressure and diastolic blood pressure. Values are presented as mean ± standard deviation. *P < 0.05, post-operating room admission versus before 5-ALA p.o./morning. #P < 0.05, the ALA group versus the control group. ALA aminolevulinic acid, BP blood pressure, p.o. per os
Additive hypotensive effect induced by spinal anesthesia and 5-ALA was prominent after spinal anesthesia induction not only during surgery but also for 2 h after the ward admission, as shown by the BP changes in our ALA group. Since the duration of the hypotensive effect by 5-ALA is longer than that of hyperbaric bupivacaine of spinal anesthesia, the systolic BP in the ALA group did not return to the baseline level even 2 h after the ward admission, unlike in the control group. We cannot easily state that spinal anesthesia using hyperbaric bupivacaine is a safe technique from our result, when considering the postoperative period. Our reflection point is that hypotension may be encouraged by hypovolemia in the ALA group, because all patients did not have intravenous fluids after 5-ALA administration before spinal anesthesia. Other risk factors that increase the incidence of 5-ALA-induced hypotension have been reported to be the regular use of antihypertensive drugs, particularly renin-angiotensin system inhibitor drugs [2, 4] and a history of ALA-induced hypotension [5].
In conclusion, orally administered 5-ALA before TUR-BT under spinal anesthesia induced significant hypotension after spinal anesthesia induction until 2 h after surgery and an increased need for vasopressors and intravenous volume. Anesthesiologists should have a strategy for safe anesthetic management against long-lasting hypotension by 5-ALA.
Acknowledgements
Not applicable
Abbreviations
- ALA
Aminolevulinic acid
- TUR-BT
Transurethral resection of bladder tumor
- BP
Blood pressure
Authors’ contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by MS, TY, and SM. The first draft of the manuscript was written by MS and supervised by TA. All authors read and approved the final manuscript.
Funding
None
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
This study was approved by the institutional ethics committee of Kyoto City Hospital (approval no. 514) and the requirement for informed consent was waived according to the retrospective nature of the study.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Masami Sato, Email: masami@kb3.so-net.ne.jp.
Tsutomu Yanagisawa, Email: sppc21hv06@yahoo.co.jp.
Sonoko Minamino, Email: higasono@gmail.com.
Toshiyuki Arai, Email: arai@kuhp.kyoto-u.ac.jp.
References
- 1.Herman MA, Webber J, Fromm D, Kessel D. Hemodynamic effects of 5-aminolevulinic acid in humans. J Photochem Photobiol B. 1998;43:61–65. doi: 10.1016/S1011-1344(98)00086-4. [DOI] [PubMed] [Google Scholar]
- 2.Nohara T, Kato Y, Nakano T, Nakagawa T, Iwamoto H, Yaegashi H, et al. Intraoperative hypotension caused by oral administration of 5-aminolevulinic acid for photodynamic diagnosis in patients with bladder cancer. Int J Urol. 2019;26:1064–1068. doi: 10.1111/iju.14099. [DOI] [PubMed] [Google Scholar]
- 3.Yatabe T, Karashima T, Kume M, Kawanishi Y, Fukuhara H, Ueba T, et al. Identification of risk factors for post-induction hypotension in patients receiving 5-aminolevulinic acid: a single-center retrospective study. JA Clin Rep. 2020;6:35. doi: 10.1186/s40981-020-00340-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chung IW, Eljamel S. Risk factors for developing oral 5-aminolevulinic acid-induced side effects in patients undergoing fluorescence guided resection. Photodiagn Photodyn Ther. 2013;10:362–367. doi: 10.1016/j.pdpdt.2013.03.007. [DOI] [PubMed] [Google Scholar]
- 5.Bondad J, Aboumarzouk OM, Moseley H, Kata SG. Oral 5-aminolevulinic acid induced photodynamic diagnostic ureterorenoscopy - does the blood pressure require monitoring? Photodiagn Photodyn Ther. 2013;10:39–41. doi: 10.1016/j.pdpdt.2012.06.004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.


