Abstract
COVID-19 spreads via aerosols, droplets, fomites and faeces. The built environment that facilitates crowding increases exposure and hence transmission of COVID-19 as evidenced by outbreaks in both cool-dry and hot-humid climates, such as in the US prison system and dormitories in Singapore, respectively. This paper explores how the built environment influences crowding and COVID-19 transmission, focusing on informal urban settlements (slums). We propose policy and practice changes that could reduce COVID-19 transmission.
There are several issues on how COVID-19 affects informal urban settlements. Slum populations tend to be younger than the overall population. Lower numbers of older people lessen the morbidity and mortality of the pandemic in slum areas. Second, many slum populations are highly mobile. By returning to their ancestral villages residents can avoid the risks of overcrowding and reduce the population density in a given area but may spread COVID-19 to other areas. Third, detection and registration of COVID-19 cases depends on patients presenting to health care providers. If the risk of visiting a health care centre outweighs the potential benefits patients may prefer not to seek treatment.
The control and prevention of COVID-19 in informal urban settlements starts with organizing community infrastructure for diagnosis and treatment and assuring that basic needs (food, water, sanitation, health care and public transport) are met during quarantine. Next, community members at highest risk need to be identified and protected. Low-income, informal settlements need to be recognized as a reservoir and source for persistent transmission. Solutions to overcrowding must be developed for this and future pandemics. In view of the constant risk that slums present to the entire population decisive steps need to be taken to rehabilitate and improve informal settlements, while avoiding stigmatization.
Keywords: Built environment, Slums, Informal settlements, Crowding, COVID-19, SARS-CoV-2
1. Introduction
Crowding occurs when the number of individuals exceeds the space available, resulting in adverse health outcomes, such as infectious diseases. Crowding may be temporary or long-term, which impacts on the intensity and duration of exposure to pathogens and the risk of transmission. For highly infectious agents, even temporary crowding in public areas such as trains and buses, can propagate an outbreak. The risk of transmission in long-term crowding, such as in densely populated urban informal settlements (slums), worker dormitories and prisons, is even higher and is often compounded by poor health and nutrition of the residents, lack of access to health care and inadequate water, sanitation and hygiene services.
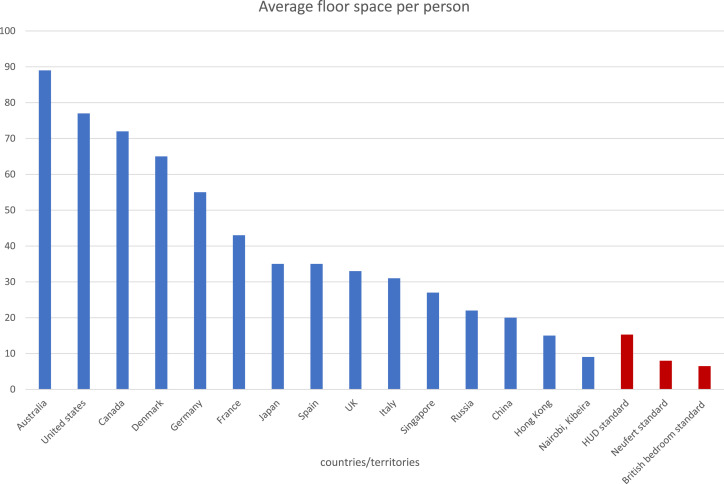
The World Health Organisation entrusts its member states to define what constitutes overcrowding [1]. UN Habitat considers overcrowding when there are more than three people per habitable room [2]. The United States Department of Housing and Urban Development (HUD) considers a household crowded if more than one person shares a room [3]. For the purposes of prevention of airborne disease transmission HUD defines overcrowding as less than 165 square feet (15.3 square meters) of living area per person. The British bedroom standard defines overcrowding by the age (child/adult) and sex of people sharing a room and also suggests that less than 70 square feet (6.5 square meters) per person constitutes overcrowding. Neufert, a reference book for spatial requirements in building design suggests residential rooms require a net minimum floor area of 86 square feet (8 square meters) and ceiling height of 7.9 feet (2.4 m) [4]. While the definition of over-crowding is subject to perception, average floor space as living area for each person can be used as an objective standard. The average floor space per person exceeds the HUD, British and Neufert standards in industrialised countries, while falling short in Kibera (Nairobi, Kenya) the largest urban slum in Africa (Fig. 1 ).
Fig. 1.
Comparison of average floor space as living area (in square meters) per person in different countries/territories. Reported average floor space (blue) minimum suggested floor space by different standards (red). (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
There is now a consensus that COVID-19 is an airborne disease in which the pathogen, SARS-CoV-2 is usually transmitted via inhalation [5]. There is no consensus whether the virus is transmitted in droplets or aerosols or both [6,7]. The primary difference between a droplet and an aerosol is the size. Particles less than <5 μm (uM) in diameter are considered aerosols while droplets have a diameter of >20 μm [8]. Particles between 5 and 20 μm diameter share some of the characterises of aerosols and droplets [9]. The difference is important in several ways. Large droplets follow a ballistic trajectory and tend to land within ≈0.16 m–0.68 m when people are speaking, ≈0.58 m–1.09 m coughing or ≈1.34 m–2.76 m sneezing (assuming an indoor environment with an air temperature of 18 °C and relative humidity of 50%) [10]. Human coronaviruses may remain viable on surfaces from 2 h to 9 days depending on the type of surface, temperature, and relative humidity [11]. People who touch such fomites are at risk of becoming infected if they subsequently touch their eyes, nose or mouth. Aerosols have long flight trajectories well beyond 2 m, can circulate in air-conditioned and ventilation systems and can penetrate human airways down to the alveolar space. Consequently, the personal protective equipment (PPE) required to prevent aerosol-borne transmission needs to be more extensive than that needed against droplet infections. While decision makers had suggested that COVID-19 is a droplet borne disease to allay concerns about insufficient PPE, the empirical evidence, such as the COVID-19 outbreak associated with air-conditioning in a restaurant in Guangzhou and a bus ride in Hubei, China, suggests that the disease is transmitted by aerosols [12,13]. The detection of aerosolized virus is further indication that a large proportion of SARS-CoV-2 infections is due to aerosolized virus [7]. Recent evidence that SARS-CoV-2 is shed in faeces and can be detected in wastewater highlights the importance of adequate sanitation in containing the pandemic [[14], [15], [16]].
The built environment interacts with a number of co-factors in SARS-CoV-2 transmission which include, climate, demographics, pre-existing health status and the indirect influence of the socio-economic status. Cool temperatures and low humidity facilitate CoV-19 transmission as illustrated by the emergence of the infection in Wuhan, China at the end of 2019 and spread in institutions in Illinois, USA during winter and spring of 2020. Using incidence data of confirmed COVID-19 cases in China and India, a recent modelling exercise showed that epidemics in crowded cities are more spread over time, and crowded cities have larger total attack rates than less populated cities [17]. The authors speculate that crowding sustains transmission within households resulting in a drawn-out spread of the virus through the population. The impact of population density on the COVID-19 pandemic has also been shown in India, Algeria, and Brazil [[18], [19], [20]]. The objective of this review is to investigate through the description and analysis of different examples how the built environment results in crowding and is associated with increased COVID-19 infections.
2. Material and methods
We employed a narrative approach to explore how the built environment modulates crowding and the risk of SARS-CoV-2 transmission. We searched Google, PubMed, and the authors’ personal collections for articles on specific examples of how the built environment increases the risk for crowding and COVID-19. We discuss the potential benefits of improvements in the built environment to minimise the negative impact of crowding on SARS-CoV-2 transmission. Statistical analyses were descriptive. Figures were created using Excel (Microsoft, Redmond, Washington 2018).
3. Theory
Historically, plague, smallpox, cholera and influenza epidemics have primarily affected those in the lowest socio economic strata of society [21]. Rich, privileged people can afford spacious living conditions while the poorest segments of society tend to live in the most crowded environments [22]. We hypothesise that the built environment that modulates population density increases the risk for the COVID-19 infection.
4. Results
Specific examples of crowding associated with the built environment that facilitates COVID-19 transmission are the US prison system, worker dormitories in Singapore and informal urban settlements.
4.1. The US prison system
The incarcerated population in the US comprises approximately 2.1 Mio. adults and has been disproportionally affected by COVID-19 [23]. Eight of the ten largest COVID clusters in the US, all with more than 1000 cases were in prisons or jails and the other two large clusters of COVID-19 cases were in meat processing facilities, where people work closely together shoulder-by-shoulder at low temperatures [24]. The space requirements of cell and detention rooms are regulated. For example the Illinois administrative code dictates that each cell has to have at least 50 square feet (4.6 square meters) of floorspace with a minimum ceiling height of 8 feet (2.4 m) and a maximum occupancy of two detainees per cell [25]. Despite these space regulations, the number of U.S. prison residents who tested positive for COVID-19 was 5.5 times higher than the general U.S. population, with a prisoner case rate of 3251 per 100,000 residents as compared to 587 cases per 100,000 in the general population [26]. The US prison administration including the Cook County Board responded by early release of a large number of eligible prisoners to reduce crowding [27].
4.2. Worker dormitories in Singapore
Early evidence that efficient COVID-19 transmission can occur in hot humid climates comes from Singapore, a modern city state in tropical SE Asia with about 5.6 Mio inhabitants. Mean daily temperature in Singapore ranges between 25 and 32° Centigrade, with a relative humidity of 90% in the morning and 60% mid-afternoon [28]. Singapore is a well-recognized financial centre with clean streets and modern high-rise buildings. Yet the construction of these high-rise buildings and much of the maintenance of the city depends on migrant workers housed in dormitories. The Singapore Ministry of Manpower website lists 43 state-licensed, purpose-built or converted factories serving as dormitories [29,30]. According to Singapore government regulations dormitories have to provide a minimum of 48 square feet (4.5 square meters) of living space for each worker [31]. Dormitories are generally not air conditioned.
Salaries for workers are multi-fold higher in Singapore (median Sing $15/hour plus $2488 bonus) than in other Asian cities, ensuring an influx of migrants into the city. As of December 2019, the total foreign workers in Singapore was over 1 million, with 293,300 working in construction [30]. The number of workers living in dormitories is estimated to be 323,000 [29]. Migrant workers can maximise savings by living in dormitories, which are located distant to the city centre, and affluent Singapore residents hardly come into contact with migrant workers. The parallel worlds of affluent Singaporeans and a subpopulation sleeping in dormitories was tolerated and ignored until the pandemic struck. Initially the Singapore government believed that the COVID-19 outbreak could be managed with sophisticated contact tracing and quarantining of exposed individuals. By end of April 2020 the public health department had become overwhelmed and contact tracing of all newly diagnosed cases could no longer be assured. The number of COVID-19 infections in migrant workers sleeping in dormitories has dwarfed that in the rest of the population. By September 2020, 54,399 out of 57,685 (94%) of the CoV-2 infections reported in Singapore were in migrant workers [31]. The lockdown of the entire city state that started on 21st April 2020, has cost an excess of Sin$ 10 billion and will result at least in an 8.5% contraction of the state's economy in 2020 [32,33].
Interestingly, the Singapore outbreak has a relative low mortality. As of September 2020, 27 of the 57,685 infected individuals (0.05%) died. This is much lower than the global case fatality estimates of around 3.6%. The quality of health care in Singapore plays a role but another major factor is the age of migrant workers. In the outbreak in New York 3263/6839 (48%) deaths were in people over 75 years [34]. It is now well-accepted that the risk for severe COVID-19 increases with age, often concomitant with chronic conditions. The foreign workers in Singapore tend to be under 50 years and physically fit, hence mortality in this at-risk population in Singapore is low.
4.3. Urban informal urban settlements
Since 2007, more than half of the world's population has been living in cities, and that proportion is projected to rise to 68% by 2050 [35]. Urban growth outpaces the creation of appropriate housing and infrastructure in many low- and middle-income countries. New arrivals coming into cities with minimal resources often live in informal settlements.
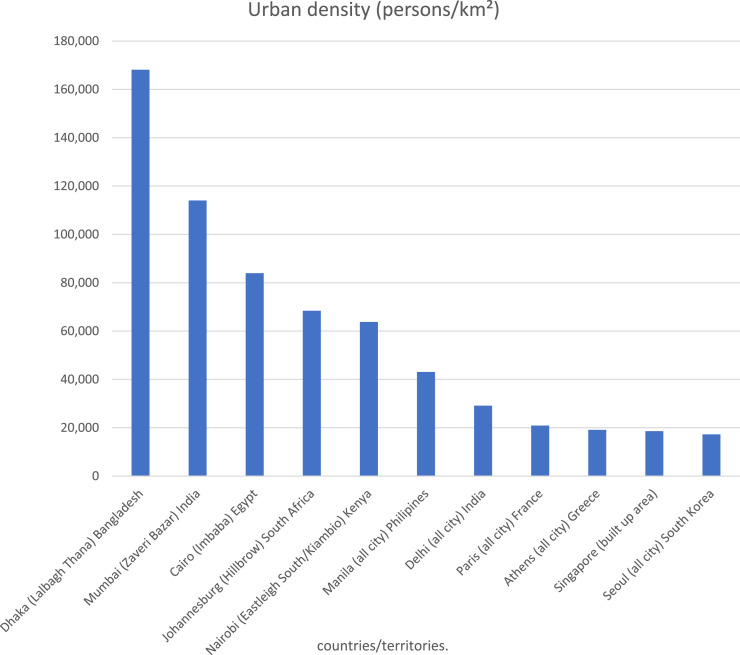
Slum areas are defined as informal settlements where half or more of the households lack access to safe water and improved sanitation, sufficient living space, durable housing, or secure tenure. In 2014 about 30% of urban populations were living in slums; these estimates are uncertain and may vary from 25% to 80% [36]. In many cities especially in Southern Asia and sub-Saharan Africa, slums no longer consist of a small proportion of marginalized neighbourhoods but instead may be home to large proportions of the urban population. In Dar es Salaam, Tanzania 28% of residents are living at least three to a room and in Abidjan, the figure is 50% [37]. Population density in Lalbagh Thana, Dhaka, Bangladesh is 168,151 people per km [2] compared with 27,000 people per km [2] in Manhattan and there are no high rises in Lalbagh Thana (Fig. 2 ) [38]. Urban density on its own is a poor predictor for COVID-19 risk, since this may be mitigated by other factors, as found in New York. Very high-income areas such as the Upper East Side of Manhattan, have a relatively high urban density (27,000/km2) but extensive floor space per person (112 sqm) related to the ubiquity of high-rise buildings. In contrast West Queens has less floor space per person (29sqm), lower urban density (20,907/km2), lower income, but a higher COVID-19 incidence [39,40]. People living in urban slums where floor space is limited, tend to have high infectious disease transmission rates and poor morbidity and mortality indicators resulting in poor outcomes [41]. Under pandemic situations, social distancing and self-isolation are impossible and residents are often forced to leave their abode to earn their daily living. In hot and humid tropical regions slum dwellings often made from corrugated metal sheets may become unbearably uncomfortable especially during the middle of the day forcing the residents to leave their home at least for a few hours each day.
Fig. 2.
Urban densities (person/km2).
Reports suggest high COVID-19 incidence in urban slums in Asia and South America but only seroprevalence studies can provide a quantitative assessment of the disease burden in informal settlements [42,43]. A survey carried out in the capital New Delhi and found that 24% of more than 20,000 people tested had Covid-19 antibodies and seropositivity in Mumbai's slums approached the 60% [44]. Several characteristics modify the impact of COVID-19 on slum populations:
4.3.1. Demographics
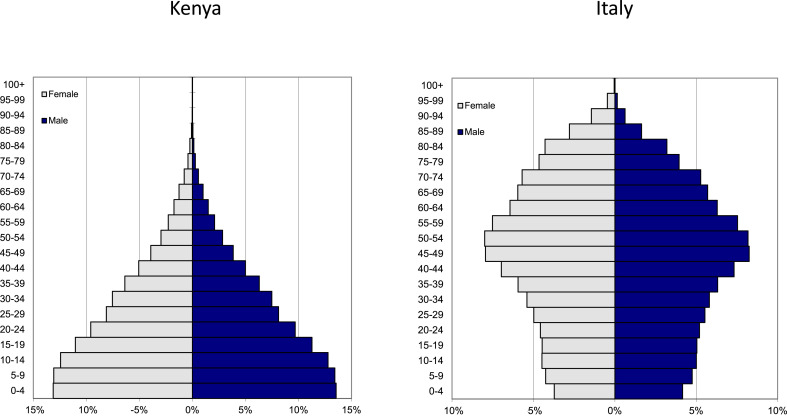
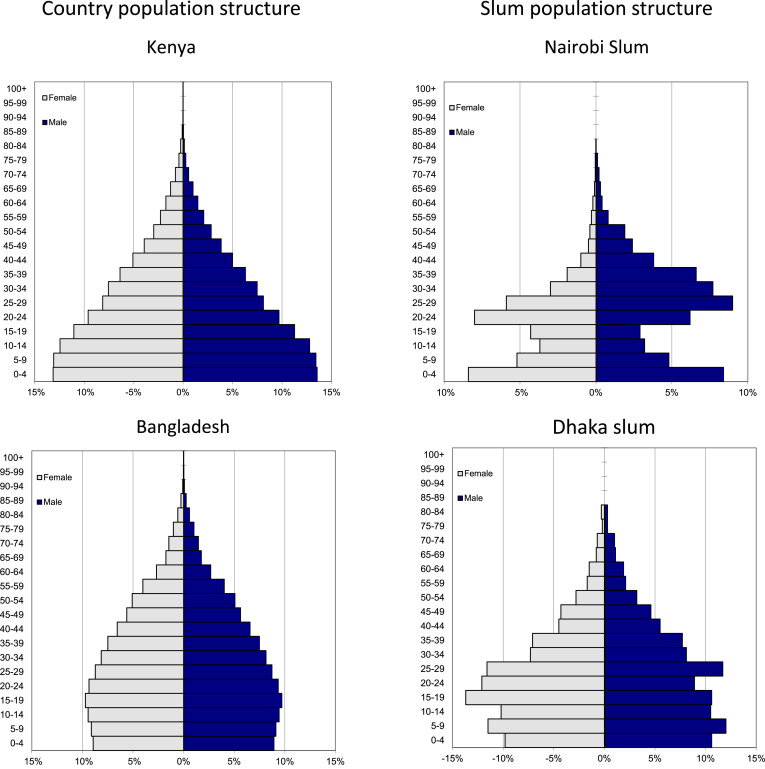
The demography of slums may be relevant to the impact of COVID-19 for slum populations. The population age structure in low-income countries, is pyramidal with a broad base representing the younger people and a relatively small older population compared with industrialised nations where the COVID-19 pandemic struck hardest, described as column- or onion-shaped. The demographic differences in the population structures of Kenya and Italy are shown in Fig. 3 (data source PopulationPyramid.net [45]). Kenya has a broad base of young people while in Italy a large proportion of the population is over 50 years and thus at an increased risk for COVID-19 with poor outcome compared to Kenya. Roughly 24% of the population of Italy is over 65 years, by contrast this percentage in Kenya is 2% (Fig. 3). The slum population structure may also differ from the overall country population (Fig. 4 ). Younger people may become infected, but they are much less likely to become severely ill and die than older people. Comorbidities including obesity, hypertension and diabetes have been identified as predictors for poor outcome of COVID-19 [46]. Slum populations may have some distinguishing features compared with the overall country population (Fig. 4). The overall national population structure (e.g. Kenya, Bangladesh) [45] is not representative for slum populations which tend to be younger (Kenya [47] and Bangladesh [48]) and predominantly male (Kenya [47] only). Reflecting the purpose of slum areas, which is to house predominantly males of working age seeking a livelihood in the city, younger children and females of all ages may be comparatively less represented in slum population. The low numbers of older adults lessen some of the morbidity and mortality of the pandemic in slum areas [49].
Fig. 3.
Demographic differences in the population structures of Kenya and Italy. Kenya has a broad base of young people while in Italy a large proportion is over of the population is over 50 years and thus at an increased risk for COVID-19 with poor outcome compared to Kenya. The y-axis indicates the percentage to the male and female population respectively. (data source PopulationPyramid.net 42).
Fig. 4.
A comparison of country and slum-area population structures. The overall national population structure (e.g. Kenya, Bangladesh)42is not representative for slum populations which tend to be younger (Kenya 44and Bangladesh 45) and predominantly male (Kenya 44only).
4.3.2. Mobility
Slum populations are mobile. Young people who see limited opportunities to gain an income in their rural homes, migrate to low-cost informal, housing close to urban centres. Young migrants try to generate sufficient income to afford trips to their rural ancestral villages. Rural households may still depend on migrating household members for seasonal agricultural activities such as harvesting, leading to circular rural-to-urban-to-rural migration patterns. For example in two urban slums in Nairobi a quarter of the total population and a third of the younger population (15–30 years) are renewed annually [50]. Once there is a threat of an outbreak or perhaps even more worrying a lockdown, migrants may prefer to return to their village homes. Urban to rural flight has the potential to reduce the crowding in urban centres and provide a form of self-quarantine for slum dwellers in rural villages but mass urban to rural migration carries the risk of spreading the disease. Outbreak-related, urban to rural migration has been documented in Thailand during the COVID-19 outbreak. The announcement of wide-ranging business closures by the governor of Bangkok on 21 March 2020 triggered a mass movement of migrants from Bangkok, to their ancestral provinces or countries [51]. Although the spread of COVID-19 infections from urban to rural areas was not detected in Thailand, it is of concern in India [52].
4.3.3. Treatment seeking behaviour
The detection of COVID-19 related morbidity and mortality, (outside of active case detection studies) depends on the patient coming forward to present to a health care provider. Treatment seeking behaviour depends not only on availability, i.e. the healthcare infrastructure but also on socio-economic, demographic, and geographic factors. The prevalence of childhood illnesses is often higher in urban slums than rural areas, but those living in urban slums have easier access to health care and are more willing to seek treatment for childhood illnesses than those living in rural areas [41]. Less is known about the treatment seeking behaviour for adult illness. This is critical for COVID-19 as morbidity and mortality increases with age. An analysis of the Indian national sample survey found that only a fraction of people over 60 sought medical assistance for medical complaints [53]. A study in Bangladesh found that older people considered many diseases an integral part of ageing which cannot and should not be treated [54]. It stands to reason that a variable fraction of COVID-19 related morbidity affecting the elderly goes undetected simply because the patients do not come forward. In a number of countries annualised mortality data will show increased mortality in 2020 compared to earlier and later years attributable to COVID-19. This may be especially true if health care providers cannot provide curative treatment and the consequences, extended isolation in unfamiliar settings appear worse than the status quo.
5. Discussion
The government response to COVID-19 in many informal settlements has been strict lockdown [42,55]. In areas defined by mobile populations and those dependent on a daily wage, this strategy may not be feasible for a sufficiently long period of time to make an impact on transmission. Until the SARS-CoV-2 is controlled by herd immunity and hopefully vaccines there remains a risk that outbreaks will flare up in informal settlements. We look here at short and longer-term approaches to minimise the risk of urban outbreaks and strategies to minimise the impact once outbreaks are ongoing.
5.1. Immediate practice
5.1.1. Community organisation
To be effective communities have to be organised existing committees should be activated to include COVID-19 issues or new ones elected to inform and network the residents, represent community interests in the larger municipality and advocate for the community's welfare [56]. Historically, top-down directives have been less than successful in informal settlements where they are ignored or even suspected to be a government ruse to clear the area. At the very least for the duration of the lockdown it is vital for evictions to be suspended and to provide the basic needs for residents in informal residents. Planning committees need to organise donations including foodbanks and assure a fair distribution of essential foodstuff. The committee needs to encourage the community to abide with feasible precautionary measures (e.g. face masks) and negotiate with the municipality government to ensure that there is no interruption in the provision of basic utilities, namely electricity, water supply, sanitation, and solid waste removal. The committee has to assure the training and deployment of community health workers who liaise with the quarantine stations (below) to facilitate the appropriate and safe transfer to the quarantine stations and return to their homes.
5.1.2. Quarantine stations
People known to be infected or highly likely to be infected need to be provided immediately with adequate space for quarantine to avoid disincentives to testing and reporting of COVID-19 infections. Adjacent facilities such as schools and gyms can be repurposed to provide triage and “community care centres”. These community care centres have to be clean, dry, warm, and soulful – yes, soulful spaces where infection control is feasible [57,58]. South Africa, with an extensive experience in the community management of TB and HIV infections, is leading the way on how such centres can and should be structured [59]. There is a need for an integrated community kitchen, space to process community donations and distribute surplus with the neediest. Quarantine stations have to be structured in a way that the healthy (using practical personal protective equipment) can interact with patients without risking becoming infected which is a major challenge. If the quarantined feel punished it is unlikely that they will agree to complete their quarantine nor recommend others to undergo the experience. How this can be achieved remains a major challenge but deserves prioritisation.
5.1.3. Urban infrastructure
In view of potential disease transmission via fomites and the well-recognized importance of hand hygiene, the provision of safe water and sanitation takes on a new importance public transport can be a critical transmission point and providing more spacious public transport is needed. More people around the world are willing to bicycle to work. Athens, Greece has allocated 50,000 square kilometres of public space for cyclists and pedestrians [60]. Dublin, Ireland, has implemented the Dublin City Covid Mobility Programme [61] and Bogota, Columbia has opened 76 km of bicycle lanes [62]. In the current situation appropriate public transport may be lifesaving. More flexible working hours can reduce the risk of exposure by allowing employees to travel during the least crowded hours of the day. Similarly regulating markets and communal spaces can help minimise crowding.
5.2. Intermediate requirements to control outbreaks
5.2.1. Define the current exposure
It is important to estimate how many people in geographically defined, high-risk communities are infected. Detecting ongoing COVID-19 cases requires that patients come forward and present at health care centres. This will only happen if the population is aware of the signs and symptoms of COVID-19 and the sum of benefits of a visit to a health care provider outweigh the potential negative consequences of a COVID-19 diagnosis. Providing appropriate centres where patients can be tested for acute SARS-CoV-19 infection by RT-PCR should be a priority.
5.2.2. Understanding the exposure
It is critical to understand which proportion of slum populations had exposure to SARS-CoV-19 as manifested by antibody seroconversion. Although COVID-19 serologic tests are under development, many questions remain about the characteristics and duration of antibody response. The WHO has developed a population-based age-stratified seroepidemiological investigation protocol for SARS-CoV-19 infection [63]. But there is little guidance regarding the specific sampling frameworks that could investigate real exposure including high risk individuals such as health care workers compared with lower risk individuals. It would be most helpful if standardized sampling frameworks for informal urban settlements would become available to allow the comparisons between populations in different regions.
5.2.3. Understanding the population
The traditional approach to understand the dimensions of a community have been mapping and census. Both activities may provide useful information in well-established settlements but can be of more limited value in highly dynamic, mobile populations. Several approaches are now available for rapid mapping such as remote sensing with the use of LIDAR [64]. Especially multi-storey structures present a challenge for rapid assessment of potential COVID-19 hotpots that can be addressed 3D-terrain models [37]. Alternative low-tech approaches include community mapping, which is more time consuming but can be combined with census activities and thus not only provide a map but also estimates of the population size [65]. Ideally high- and low-tech approaches could be combined. Remote sensing provides a map which is then ground-truthed by community mappers who regularly update the census. Community mappers would be critical to detect urban to rural flight/migration and follow older community members. Potential civil, political and consent issues need to be taken into consideration in the conduct of population mapping and census.
5.3. Longer-term changes to physical planning and structure
There is no shortage of practical ideas how to improve and redesign urban slums blocked by a fundamental clash of private versus public interests. Not only do the residents want to stay where they are, powerful interests such as landlords and middlemen reselling basic utilities stand to lose if slums are moved or even disappear. Kibera, in Nairobi, Kenya perhaps one of the best studied slums globally has been slated for clearance since 2009 which at the present rate has been estimated to take 1178 years [66].
Pandemics have been historic triggers for urban renewal and rehabilitation. The second plague pandemic is thought to have started in 1347 and killed roughly a third of the European population [67]. But the bubonic plague was also a unique opportunity to introduce the radical urban improvements of the Renaissance including the clearing of squalid and cramped living quarters [68]. Paris was ravaged by cholera epidemics in 1832 and 1848. At the time the population density in the highly affected quarters, Arcis and Saint-Avoye (currently the third Arrondissement), was estimated to be 3m2/resident [69]. The dangerously unhygienic conditions in the highly affected quarters were important reasons for Napoleon III to appoint Georges-Eugène Haussmann to rebuild Paris. Between 1853 and 1867 Haussmann not only replaced the old overcrowded quarters with large boulevards to provide “air and open space” and lined the boulevards with large “Haussmann buildings” for which Paris is known today, he also ensured that an appropriate infrastructure including a safe water supply and sanitation was available [69].
Cities can become accustomed to their slums to the point that affluent residents do not see the slum dwellers any longer. The COVID-19 pandemic has changed the urban landscape. Affluent residents have to realise how deeply they are inter-connected and ultimately dependent on people living in informal settlements who are at high risk for disease transmission. Social distancing may well be practiced by the residents in affluent homes but will be of limited success if for example, young, physically fit, domestic helpers sleep in a slum and bring the virus into the home without realizing it. Slums may seem to be an intractable problem, but instead accepting that there will always be slums, the communities have to asked what they want and what they need. The next step is to find solutions. Jason Corburn a slum expert from Berkeley, California suggests “placing cities' highest budget, best designed, most beautiful new projects in the poorest, most neglected areas” [70]. A related strategy was used in Paris during the 1980's with urban renewals focusing on green public spaces as drivers for urban regeneration. Some of the best known examples of this strategy are perhaps Parc Citroen, a former car factory and Parc de la Villette, the site of the huge Parisian abattoirs [71]. COVID-19 can mobilize an unprecedented willingness to overcomes vested interests and invest resources into the improvement of slums resulting in better living conditions.
This paper does not attempt to be a systematic literature review but is a response to the evolving COVID-19 pandemic in the second and third quarter of 2020. More complete and accurate data will become available in coming months and years and may require revision of some of the ideas presented in this paper. Many aspects touched upon in this paper deserve a systematic literature review in the months to come but this is beyond the scope of the present paper. Similarly, the planning of facilities for intensive care, oxygen, ventilators etc. is beyond the scope of this article.
6. Conclusions
The COVID-19 pandemic has touched nearly everybody, but some have been more affected than others. Older people are at increased risk for severe disease, while socially and economically disadvantaged populations are at an increased risk of becoming infected. Among the factors modulating the infection risk, crowding stands out but is difficult to quantify and even more difficult to address. Crowding is in many ways linked to socio-economic status and should be defined in terms of floor space/person rather than population density. Well-off people can afford more floor-space, can avoid public transport and work from home. Low-income populations do not have this freedom. People residing in informal settlements have to earn their daily wages or just leave their home during the hottest hours of the day to avoid the oppressive heat in their home. The built environment can play a critical role in minimising crowding and facilitating social distancing. The built environment has played historically a key role in the control of epidemics. The second plague pandemic led to the radical urban improvements of the Renaissance. Cholera outbreaks in the 19th century led to the Hausmann's renewal of Paris. Improvements that can be achieved immediately including community organisation, opening of quarantine station, and better public transport by providing more trains and buses and increasing bicycle lanes. To interrupt transmission, it is critical to identify the populations and the geographic areas at highest risk for infections in order to direct interventions where they are needed most. Reducing the infection risks in the most affected populations ultimately serves the entire population. Only when the transmission in the entire population is interrupted can life return to normal otherwise there remains the lingering risk of another wave. The Ebola Virus Disease epidemic taught us that the key to control and elimination of outbreaks is a community working together [72]. A fractured, divided population cannot fight a pandemic.
Funding
No specific funding was obtained for the drafting of this paper.
Declaration of competing interest
The authors declare that they have no competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
We thank our colleagues at MORU, KADK, and UNHABITAT for discussions and suggestions.
References
- 1.WHO . 2018. Housing and Health Guidelines.https://wwwwhoint/publications-detail/who-housing-and-health-guidelines [PubMed] [Google Scholar]
- 2.UN. Principles Recommendations Population Housing Censuses. Statistical papers Series M No 67/Rev2. 2008. [Google Scholar]
- 3.HUD, US Department of Housing and Urban Development . 2007. Office of Policy Development and Research Measuring Overcrowding in Housing.https://wwwhudusergov/publications/pdf/Measuring_Overcrowding_in_Hsgpdf [Google Scholar]
- 4.Neufert E., Neufert P., Kister J. fourth ed. Wiley-Blackwell; 2012. Neufert Architects' Data. [Google Scholar]
- 5.Khamsi R. 2020. They Say Coronavirus Isn't Airborne—But It's Definitely Borne by Air.https://wwwwiredcom/story/they-say-coronavirus-isnt-airborne-but-its-definitely-borne-by-air/?utm_source=Nature+Briefing&utm_campaign=e09b649635-briefing-dy-20200317&utm_medium=email&utm_term=0_c9dfd39373-e09b649635-42806647 WIRED. [Google Scholar]
- 6.van Doremalen N., Bushmaker T., Morris D.H., et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N. Engl. J. Med. 2020;382(16):1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liu Y., Ning Z., Chen Y., et al. Aerodynamic analysis of SARS-CoV-2 in two Wuhan hospitals. Nature. 2020 doi: 10.1038/s41586-020-2271-3. [DOI] [PubMed] [Google Scholar]
- 8.Tellier R., Li Y., Cowling B.J., Tang J.W. Recognition of aerosol transmission of infectious agents: a commentary. BMC Infect. Dis. 2019;19(1):101. doi: 10.1186/s12879-019-3707-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mao N., An C.K., Guo L.Y., et al. Transmission risk of infectious droplets in physical spreading process at different times: a review. Build. Environ. 2020:185. doi: 10.1016/j.buildenv.2020.107307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cheng C.H., Chow C.L., Chow W.K. Trajectories of large respiratory droplets in indoor environment: a simplified approach. Build. Environ. 2020;183 doi: 10.1016/j.buildenv.2020.107196. 107196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kampf G., Todt D., Pfaender S., Steinmann E. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J. Hosp. Infect. 2020;104(3):246–251. doi: 10.1016/j.jhin.2020.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lu J., Gu J., Li K., et al. COVID-19 outbreak associated with air conditioning in restaurant, Guangzhou, China, 2020. Emerg. Infect. Dis. 2020;26(7) doi: 10.3201/eid2607.200764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shen Y., Li C., Dong H., et al. Community outbreak investigation of SARS-CoV-2 transmission among bus riders in eastern China. JAMA Intern. Med. 2020 doi: 10.1001/jamainternmed.2020.5225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chen Y., Chen L., Deng Q., et al. The presence of SARS-CoV-2 RNA in the feces of COVID-19 patients. J. Med. Virol. 2020 doi: 10.1002/jmv.25825. [DOI] [PubMed] [Google Scholar]
- 15.Santos V.S., Gurgel R.Q., Cuevas L.E., Martins-Filho P.R. Prolonged fecal shedding of SARS-CoV-2 in pediatric patients. A quantitative evidence synthesis. J. Pediatr. Gastroenterol. Nutr. 2020 doi: 10.1097/MPG.0000000000002798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Orive G., Lertxundi U., Barcelo D. Early SARS-CoV-2 outbreak detection by sewage-based epidemiology. Sci. Total Environ. 2020;732 doi: 10.1016/j.scitotenv.2020.139298. 139298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rader B., Scarpino S.V., Nande A., et al. Crowding and the shape of COVID-19 epidemics. Nat. Med. 2020 doi: 10.1038/s41591-020-1104-0. [DOI] [PubMed] [Google Scholar]
- 18.Bhadra A., Mukherjee A., Sarkar K. Impact of population density on Covid-19 infected and mortality rate in India. Model. Earth Syst. Environ. 2020:1–7. doi: 10.1007/s40808-020-00984-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kadi N., Khelfaoui M. Population density, a factor in the spread of COVID-19 in Algeria: statistic study. Bull. Natl. Res. Cent. 2020;44(1):138. doi: 10.1186/s42269-020-00393-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pequeno P., Mendel B., Rosa C., et al. Air transportation, population density and temperature predict the spread of COVID-19 in Brazil. PeerJ. 2020;8 doi: 10.7717/peerj.9322. e9322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wade L. From Black Death to fatal flu, past pandemics show why people on the margins suffer most. Science. 2020 https://wwwsciencemagorg/news/2020/05/black-death-fatal-flu-past-pandemics-show-why-people-margins-suffer-most?utm_campaign=news_daily_2020-05-14&et_rid=247859539&et_cid=3326859 [Google Scholar]
- 22.Baldassare M. University of California Press; Berkeley: 1979. Residential Crowding in Urban America. [Google Scholar]
- 23.Wallace M., Hagan L., Curran KG ea. 2020. COVID-19 in Correctional and Detention Facilities — United States. February–April 2020. . ePub: 6 May 2020, MMWR Morb Mortal Wkly Rep. [DOI] [PubMed] [Google Scholar]
- 24.New_York_Times T . 2020. Coronavirus in the U.S.: Latest Map and Case Count.https://wwwnytimescom/interactive/2020/us/coronavirus-us-caseshtml#clusters 18 june 2020. [Google Scholar]
- 25._Rules JCoA Ill. Admin. Code Tit. 20 § 701.80. 2020. https://casetextcom/regulation/illinois-administrative-code/title-20-corrections-criminal-justice-and-law-enforcement/part-701-county-jail-standards/section-70180-housing (Housing) vol. 44, 6, 80.
- 26.Saloner B., Parish K., Ward J.A., DiLaura G., Dolovich S. COVID-19 cases and deaths in federal and state prisons. J. Am. Med. Assoc. 2020 doi: 10.1001/jama.2020.12528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Williams T., Weiser B., Rashbaum W. 2020. ‘Jails Are Petri Dishes’: Inmates Freed as the Virus Spreads behind Bars.https://wwwnytimescom/2020/03/30/us/coronavirus-prisons-jailshtml [Google Scholar]
- 28.Meteorological_Service_Singapore . 2020. Climate of Singapore.http://wwwweathergovsg/climate-climate-of-singapore/ [Google Scholar]
- 29.Han K. 2020. Singapore Is Trying to Forget Migrant Workers Are People.https://foreignpolicycom/2020/05/06/singapore-coronavirus-pandemic-migrant-workers/ Foreign Policy. [Google Scholar]
- 30.Ministry_of_Manpower . 2020. Foreign Workforce Numbers.https://wwwmomgovsg/documents-and-publications/foreign-workforce-numbers (last accessed 02/06/2020) [Google Scholar]
- 31.Cai W., Lai K.K.R. 2020. Packed with Migrant Workers, Dormitories Fuel Coronavirus in Singapore.https://wwwnytimescom/interactive/2020/04/28/world/asia/coronavirus-singapore-migrantshtml?searchResultPosition=1 (last accessed 13/05/2020) [Google Scholar]
- 32.Vishnoi A. 2020. Singapore Partial Lockdown to Cost Economy S$10 Billion.https://wwwbloombergcom/news/articles/2020-04-09/singapore-s-partial-lockdown-seen-costing-economy-s-20-billion?srnd=markets-vp (last accessed 13/052020) [Google Scholar]
- 33.Straitstimes Singapore economy to shrink by steeper 8.5% this year with extended circuit breaker period: Citigroup. 2020. https://wwwstraitstimescom/business/economy/singapore-economy-to-shrink-by-steeper-85-with-extended-circuit-breaker-period (last accessed 13/05/2020)
- 34.NYC-Health . 2020. Coronavirus Disease 2019 (COVID-19) Daily Data Summary.https://www1nycgov/assets/doh/downloads/pdf/imm/covid-19-daily-data-summary-deaths-04152020-1pdf (last accessed 13/05/2020) [Google Scholar]
- 35.Affairs UNDoEaS . 2018. 68% of the World Population Projected to Live in Urban Areas by 2050, Says UN.https://wwwunorg/development/desa/en/news/population/2018-revision-of-world-urbanization-prospectshtml [Google Scholar]
- 36.UNHABITAT . 2014. Population Living in Slums (% of Urban Population)https://dataworldbankorg/indicator/ENPOPSLUMURZS [Google Scholar]
- 37.Bhardwaj G., Esch T., Lall S.V., Marconcini M., Soppelsa M.E., Wahba S. 2020. Cities, Crowding, and the Coronavirus: Predicting Contagion Risk Hotspots1.http://documentsworldbankorg/curated/en/206541587590439082/pdf/Cities-Crowding-and-the-Coronavirus-Predicting-Contagion-Risk-Hotspotspdf last accessed 18th June 2020. [Google Scholar]
- 38.Wikipedia . 2020. List of City Districts by Population Density.https://enwikipediaorg/wiki/List_of_city_districts_by_population_density#cite_note-CitypopulationBD-1 [Google Scholar]
- 39.Lall S., Wahba S. 2020. No Urban Myth: Building Inclusive and Sustainable Cities in the Pandemic Recovery.https://wwwworldbankorg/en/news/immersive-story/2020/06/18/no-urban-myth-building-inclusive-and-sustainable-cities-in-the-pandemic-recovery [Google Scholar]
- 40.Fang W., Wahba S. 2020. Urban Density Is Not an Enemy in the Coronavirus Fight: Evidence from China.https://blogsworldbankorg/sustainablecities/urban-density-not-enemy-coronavirus-fight-evidence-china [Google Scholar]
- 41.Mberu B.U., Haregu T.N., Kyobutungi C., Ezeh A.C. Health and health-related indicators in slum, rural, and urban communities: a comparative analysis. Glob. Health Action. 2016;9 doi: 10.3402/gha.v9.33163. 33163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gutierrez J.A.J. NYT; 2020. ‘Will We Die Hungry?’ A Teeming Manila Slum Chafes under Lockdown.https://wwwnytimescom/2020/04/15/world/asia/manila-coronavirus-lockdown-slumhtml [Google Scholar]
- 43.Coronavirus D.W. 2020. Brazil Headed for Catastrophe.https://wwwdwcom/en/coronavirus-brazil-headed-for-catastrophe/a-53502907 [Google Scholar]
- 44.Ministry_of_Health_and_Family_Welfare . June 2020. Sero-prevalence Study Conducted by National Center for Disease Control NCDC, MoHFW, in Delhi.https://pibgovin/PressReleasePageaspx?PRID=1640137 2020 [Google Scholar]
- 45.PopulationPyramid.net. https://www.populationpyramid.net/world/2019/.2020
- 46.Argenziano M.G., Bruce S.L., Slater C.L., et al. Characterization and clinical course of 1000 patients with coronavirus disease 2019 in New York: retrospective case series. BMJ. 2020;369 doi: 10.1136/bmj.m1996. m1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Archambault C., de Laat J., Zulu E. Urban services and child migration to the slums of Nairobi. World Dev. 2012;40(9) [Google Scholar]
- 48.Razzaque A. 2019. Slum Health in Bangladesh.https://wwwgooglecom/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&ved=2ahUKEwiwoc6tverpAhVCOSsKHWXxBJYQFjAAegQIAhAB&url=http%3A%2F%2Fdspaceicddrborg%2Fjspui%2Fbitstream%2F123456789%2F9298%2F1%2Ficddrb-SP154pdf&usg=AOvVaw3Umxh71eFUgSAY4K9Ncuyp 2019 [Google Scholar]
- 49.Dowd J.B., Andriano L., Brazel D.M., et al. Demographic science aids in understanding the spread and fatality rates of COVID-19. Proc. Natl. Acad. Sci. U. S. A. 2020;117(18):9696–9698. doi: 10.1073/pnas.2004911117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Beguy D., Bocquier P., Zulu E.M. Circular migration patterns and determinants in Nairobi slum settlements. Demogr. Res. 2010;23(20):549–586. [Google Scholar]
- 51.IOM . 2020. Movement Overview: Thailand to Cambodia, Lao People's Democratic Republic (The) and Myanmar.https://reliefwebint/sites/reliefwebint/files/resources/COVID%2019%20Response%20-%20Flash%20Update%20-%20Migration%20Movement%20in%20the%20Greater%20Mekong%20Sub%20Region%20%28GMS%29%20-%2026%20March%202020pdf [Google Scholar]
- 52.Mishra S.V., Haque S.M., Gayen A. COVID-19 in India transmits from the urban to the rural. Int. J. Health Plann. Manag. 2020 doi: 10.1002/hpm.3047. [DOI] [PubMed] [Google Scholar]
- 53.Srivastava S., Gill A. Untreated morbidity and treatment-seeking behaviour among the elderly in India: analysis based on National Sample Survey 2004 and 2014. SSM Popul. Health. 2020;10 doi: 10.1016/j.ssmph.2020.100557. 100557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Biswas P., Kabir Z.N., Nilsson J.A., Zaman S.M. Dynamics of health care seeking behaviour of elderly people in rural Bangladesh. Int. J. Ageing Later Life. 2006;1(1):69–89. [Google Scholar]
- 55.Gettleman J. 2020. India's ‘Maximum City’ Engulfed by Coronavirus.https://wwwnytimescom/2020/05/14/world/asia/mumbai-lockdown-coronavirushtml last [Google Scholar]
- 56.Corburn J., Vlahov D., Mberu B., et al. Slum health: arresting COVID-19 and improving well-being in urban informal settlements. J. Urban Health. 2020 doi: 10.1007/s11524-020-00438-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Brady L., Notywala A., Ryklief A., Swartbooi N., van_Ryneveld M., Whyle E. 2020. The Power of People Caring for Those Affected by Covid-19. Maverick Citizen.https://wwwdailymaverickcoza/article/2020-04-13-the-power-of-people-caring-for-those-affected-by-covid-19/last [Google Scholar]
- 58.Doherty K. 2014. Ebola Epidemic: what Can Architecture Do?https://wwwarchitectural-reviewcom/essays/ebola-epidemic-what-can-architecture-do/8670622article last The Architectural Review. [Google Scholar]
- 59.Howell E.M., Kigozi N.G., Heunis J.C. Community-based directly observed treatment for TB patients to improve HIV services: a cross-sectional study in a South African province. BMC Health Serv. Res. 2018;18(1):255. doi: 10.1186/s12913-018-3074-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.ekathimerini . 2020. Grand Walk of Athens to Be Pilot-Tested on Thursday.https://wwwekathimerinicom/253549/article/ekathimerini/community/grand-walk-of-athens-to-be-pilot-tested-on-thursday [Google Scholar]
- 61.Dublin_City_Council Dublin city Covid mobility Programme. 2020. http://wwwdublincityie/covidmobilityprogramme
- 62.Wray S. Bogotá expands bike lanes to curb coronavirus spread. https://wwwsmartcitiesworldnet/news/news/bogota-expands-bike-lanes-overnight-to-curb-coronavirus-spread-5127 2020
- 63.WHO Population-based age-stratified seroepidemiological investigation protocol for COVID-19 virus infection. 2020. https://appswhoint/iris/handle/10665/332188 06/06/20202.
- 64.Kuffer M., Pfeffer K., Sliuzas R. Slums from space—15 Years of slum mapping using remote sensing. Rem. Sens. 2016;8(6):455. https://doiorg/103390/rs8060455 [Google Scholar]
- 65.MapKibera. 2020. https://mapkibera.org/ accessed 17th May 2020.
- 66.Wikipedia Kibera. 2020. https://enwikipediaorg/wiki/Kibera
- 67.Cohn S. The black death: end of a paradigm. Am. Hist. Rev. 2002;107(3):703–737. doi: 10.1086/532493. [DOI] [PubMed] [Google Scholar]
- 68.Lubell S. Past pandemics changed the design of cities. Six ways COVID-19 could do the same LA Times. https://wwwlatimescom/entertainment-arts/story/2020-04-22/coronavirus-pandemics-architecture-urban-design last accessd 03/06/2020 2020.
- 69.De Moncan P., Heurteux C. 2002. Le Paris d'Haussmann: Editions du Mécène. [Google Scholar]
- 70.Ellis E. How smart city planning could slow future pandemics. 2020. https://wwwwiredcom/story/coronavirus-covid-19-urban-planning-health/last
- 71.Tschumi B. Princeton Architectural Pr; New York, USA: 1988. Cinegram Folie: Le Parc De LA Villette. Hudson. [Google Scholar]
- 72.Richards P. ZED Books; London: 2016. Ebola/How a People's Science Helped End an Epidemic. [Google Scholar]