Abstract
Background
Femoral head fractures (FHF) are uncommon and generally caused by high-energy injuries. Surgical reduction with stable fixation of large fragments is believed to have the best outcomes. This retrospective study intended to report outcomes with surgical treatment at our institution and tried to establish treatment algorithm.
Methods
Through the 6-year period (2003–2008), 35 FHF in 35 consecutive patients (average, 30 years) were surgically treated. All FHF were caused by high-energy trauma. Patients' general condition was stabilized first and hip dislocation was manually reduced immediately. Definite fracture treatment was scheduled after admission for an average of 2.9 days (0.3–11 days). Pipkin classification was used as the treatment guide and open reduction with internal fixation was performed in all 35 FHF.
Results
These FHF included 21 type I, 7 type II, 3 type III, and 4 type IV fractures. The hip joint had been approached by either an anterior or posterior route depending on the individual surgeon. Internal fixation with screws was performed for all 35 FHF. The average admission was 13.8 days (range, 2–35 days). Thirty patients (86%, 30/35) were followed for an average of 3.3 years (at lease 6 months) and all 30 FHF healed. Avascular necrosis of the femoral head was found in 23% (7/30) patients and six patients were converted to hip arthroplasty for developing advanced stages of avascular necrosis. Heterotopic ossification occurred in 43% (13/30) patients. However, only one patient had range of motion limitation. Besides, one patient had moderate hip osteoarthritis.
Conclusions
FHF are uncommon and generally caused by high-energy injuries. Fracture healing can be attained in all femoral head fractures by using open reduction and screw fixation. Our results by using conventional approaches were associated with high complication rates. Further endeavor to improve the outcome should be taken.
Keywords: Avascular necrosis, Femoral head fracture, Heterotopic ossification, Internal fixation, Osteoarthritis
At a glance commentary
Scientific background on the subject
Femoral head fractures normally occur in high-energy injury and are uncommon. In the literature, treatment principles and outcomes are controversial due to relatively few sample sizes. Theoretically, open reduction with stable fixation of large fragments to restore original anatomy of the femoral head may achieve the best outcomes. However, the optimal approach has yet achieved a consensus. Following the advancement of modern medicine and technology, a more reasonable surgical technique may be developed.
What this study adds to the field
Fracture healing can be attained in all femoral head fractures by using open reduction and screw fixation. However, Pipkin type I and II fractures treated by conventional approaches were associated with high incidence of osteonecrosis (17%) and heterotopic ossification (43%). Further endeavor to improve the outcome should be taken.
Femoral head fractures (FHF) are uncommon and may be sometimes associated with posterior hip dislocation [1], [2]. The reported incidence of combined injuries is 5%–15% in FHF [2], [3]. From anatomic and biomechanical viewpoints, fractures of the femoral head occur the most possibly on the anterior part during injury [4]. Pipkin classification has been widely used to classify FHF and is considered valuable in predicting treatment outcomes [2], [5]. Principles for FHF treatment have been recommended in the literature [3]. The more recent literature supports the opinion: only anatomic reduction with stable fixation of fracture fragments can achieve the best long-term results [3]. Following the advancement of modern medicine and technology, theoretically the surgical outcomes may be greatly improved.
FHF are still difficult to be treated because of their intra-articular involvement with complex approaches for anatomic fixation [1], [2], [6]. Major complications of post-traumatic osteoarthritis, avascular necrosis (AVN), and heterotopic ossification (HO) may occur frequently [2], [7], [8]. Previous articles generally reported the pros and cons of different surgical approaches or fixation methods, depending on varied Pipkin's classification [9], [10]. Few studies focused on the prognosis after surgical treatment for each type of FHF. The aim of this retrospective study was to report the mid-term surgical outcomes of FHF treated at our institution, based on varied Pipkin types, and tried to establish treatment algorithm.
Methods
This study had been approved by the Institutional Review Board of our institution (No. 101-3711B).
We enrolled all patients with surgical treatment of traumatic FHF with or without hip dislocations. Patients without surgical treatment of FHF were excluded due to lack of documents (e.g. small fracture fragments). FHF which had been associated with pathologic or atypical femur fractures were also excluded [11]. Thirty-five patients who were treated at our institution by various surgeons from January 2003 to December 2008 were included in this study.
All fractures were caused by high-energy trauma and associated injuries were multiple; however, no patients died after arrival at our institution. At the emergency room, patients' general conditions were stabilized first. All hip dislocations (9 patients, 26%) were reduced at the emergency room or operating room immediately. Definite open reduction with internal fixation (ORIF) was scheduled. Pipkin classification was used for treatment of all FHF at our institution [2], [5].
Surgical technique
Under general anesthesia with endotracheal intubation, patients were operated on according to various fracture types. Cancelous screws (Synthes, Bettlach, Switzerland) were simply used for treating type I and II fractures. For type III fractures, cannulated screws (Synthes, Bettlach, Switzerland) were chosen for treating femoral neck fixation concomitantly. ORIF with screws and plates (Synthes, Bettlach, Switzerland) was used for type IV fractures. Either an anterior (Smith-Peterson technique) or posterior approach (Gibson technique) was performed, decided by the individual surgeon. Trochanter flip osteotomy was not used because of technical unfamiliarity at this period [12]. Surgical timing was also decided by the individual surgeon depending on patient's condition or operation rooms availability. The delayed time was an average of 2.9 days (range, 0.3–11 days). In this study, timing of surgery within or without 24 h and approach route related to AVN were compared for evaluating clinical outcomes concomitantly.
We retrospectively reviewed these patients with radiographs and focused on the bony union, post-traumatic osteoarthritis, HO, and AVN. Patients were followed at the outpatient department at 4–6 weeks interval. The results were compared based on fractures of each Pipkin type. Hip function was not evaluated due to lack of documents by the individual surgeon.
Statistical analysis
For the convenience of comparison, the Fisher exact test was used for comparison of independent categorical data. P < 0.05 was considered statistically significant. Comparison among various types was not performed due to relatively few and heterogenous samples.
Results
The average admission was 13.8 days (range, 2–35 days) for 35 patients. No patient died during the whole treatment course and were discharged smoothly.
Thirty-one patients were male and four were female; ages ranged from 15 to 53 years (average, 30 years). According to Pipkin classification, there were 21 type I, 7 type II, 3 type III, and 4 type IV fractures.
Thirty patients (86%, 30/35) were followed for at least 6 months (average, 3.3 years; range, 0.5–10 years). Five patients (14%) were lost despite the maximal efforts to contact them. There was no deep infection in all FHF surgeries. The follow-up rate was 86% at 6 months with 62% at 1 year in type I FHF. The follow-up rate for type II FHF was 86% at 6 months with 71% at 1 year. The follow-up rate was 67% at 6 months or 1 year in type III FHF. In type IV FHF, the follow-up rate was 100% at 6 months or 1 year [Table 1]. All 30 FHF healed [Fig. 1]. Seven patients developed AVN in the femoral head (23%, 7/30), and 6 femoral heads needed arthroplasty treatment (3 type I, 0 type II, 2 type III, and 1 type IV fractures) for Ficat stage III AVN [Fig. 2, Fig. 3] [13]. Four of them received arthroplasty surgery within one year. One femoral head in type I FHF was Ficat stage II AVN and was observed regularly.
Table 1.
Follow-up rates after surgical treatment of femoral head fractures (n = 35).
| Follow-up |
Type I |
Type II |
Type III |
Type IV |
Total |
|---|---|---|---|---|---|
| Period | (n = 21) | (n = 7) | (n = 3) | (n = 4) | (n = 35) |
| 3 M | 19 (90%) | 6 (86%) | 2 (67%) | 4 (100%) | 31 (89%) |
| 6 M | 18 (86%) | 6 (86%) | 2 (67%) | 4 (100%) | 30 (86%) |
| 12 M | 13 (62%) | 5 (71%) | 2 (67%) | 4 (100%) | 24 (69%) |
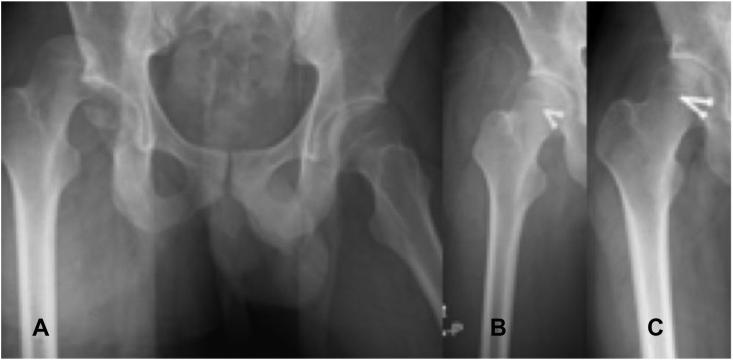
Fig. 1.
(A) A 19-year-old man sustained combined right posterior hip dislocation and a femoral head fracture (Pipkin type I) due to motorcycle accident. (B) The hip dislocation was closely reduced immediately and the femoral head fragment was surgically treated with screw fixation later. The fracture healed at 3 months. (C) There were no avascular necrosis and heterotopic ossification for 2-year follow-up.
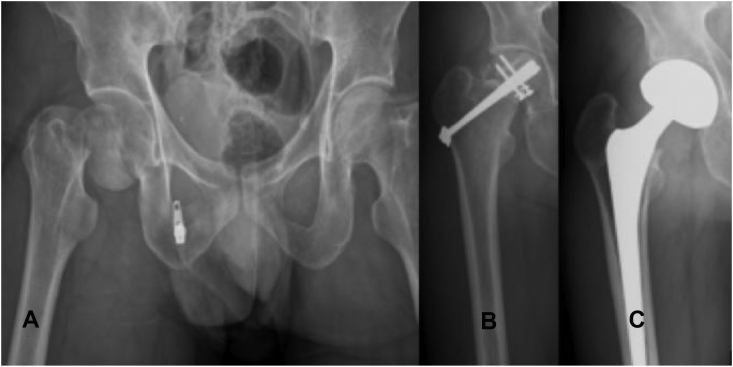
Fig. 2.
(A) A 45-year-old man sustained combined right posterior hip dislocation with a femoral head fracture (Pipkin type I) due to automobile accident. (B) The fracture fragment was stabilized with two screws but avascular necrosis with nonunion occurred at 6 moths. (C) Total hip arthroplasty was performed within one year.
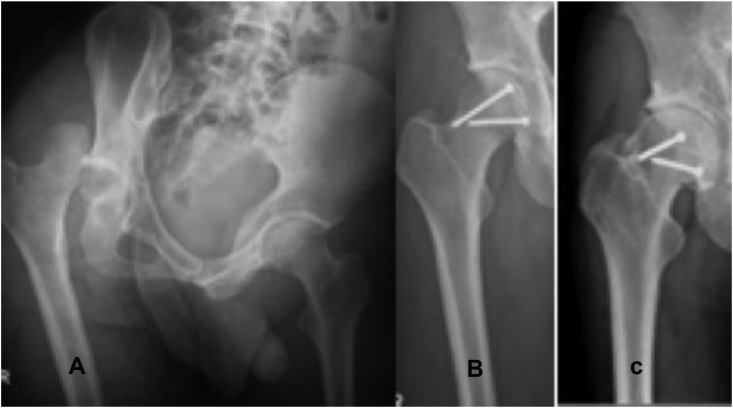
Fig. 3.
(A) A 40-year-old man sustained combined right femoral neck and head fractures (Pipkin type III) due to motorcycle accident. (B) Both fractures were stabilized with screws but avascular necrosis occurred. (C) Bipolar hemiarthroplasty was performed at 6 months.
Because 80% (24/30) patients with follow-up were type I or II fractures and both fractures were relatively homogeneous, comparison was made to represent the prognosis of FHF treatment [Table 2]. In combined Pipkin type I and II fractures (24 FHF), there were 11 patients received surgery within 24 h and 2 FHF developed AVN (18%, 2/11). Thirteen patients were treated beyond 24 h, and 2 FHF developed AVN (15%, 2/13; p = 0.20; power = 0.04). Eighteen FHF were treated using an anterior approach and 3 developed AVN (17%, 3/18). Six FHF were treated using a posterior approach and one developed AVN (17%, 1/6; p = 0.46; power = 0.04).
Table 2.
Complications after surgical treatment of femoral head fractures (n = 30).
| Complications | Type I |
Type II |
Type III |
Type IV |
|---|---|---|---|---|
| (n = 18) | (n = 6) | (n = 2) | (n = 4) | |
| AVN (23%, 7/30) | 4 (22%) | 0 | 2 (100%) | 1 (25%) |
| HO (43%, 13/30) | 8 (44%) | 1 (17%) | 2 (100%) | 2 (50%) |
| OA (3.3%, 1/30) | 0 | 0 | 0 | 1 (25%) |
Abbreviations: AVN: avascular necrosis; HO: heterotopic ossification; OA: osteoarthritis.
All fractures healed and there were no nonunion. In addition, there were 8 HOs in type I, 1 in type II, 2 in type III, and 2 in type IV fractures [Table 2]. The incidence of HO was 43% (13/30). All except one hip with HO were in low Brooker class (class 1 or 2) and hip function was preserved [Fig. 4] [14]. No surgical treatment was performed to ameliorate hip range of motion. Only one case with moderate osteoarthritis in type IV fracture and arthroplasty treatment was suggested whenever necessary [15].
Fig. 4.
(A) A 31-year-old man sustained combined right posterior hip dislocation with a femoral head fracture (Pipkin type II) due to motorcycle accident. (B) The fragment was stabilized with two screws. (C) Low grade of heterotopic ossification (class 1) occurred without symptoms for 3-year follow-up.
Discussion
In this retrospective study, within the 6-year period 35 FHF were surgically treated. Thirty FHF (86%) were followed for at least 6 months (average, 3.3 years; range, 0.5–10 years). Complications included HO (43%) and AVN (23%). Other complications were few. Only AVN required secondary treatment and nearly all femoral heads shifted to hip arthroplasty (86%, 6/7).
Surgical treatment for injuries involving the hip joint are generally complex due to its deep location, massive soft tissues in situ, and vulnerable femoral head vascularity [2], [16], [17], [18]. To save the femoral fragments with FHF, various complications may occur. The more common delayed complications include AVN, HO, and osteoarthritis [2], [7], [8]. Because FHF are uncommon, the more favored treatment regimen has yet achieved a consensus [3], [7], [8]. In the literature, failure of surgical treatment of FHF is common. In the present study, for the 6-year period only 35 FHF were surgically treated and 30 FHF were followed. High complication rates were noted (43% HO and 23% AVN).
Traditionally, surgical treatment of FHF may use an anterior or posterior approach and each approach has unique advantages and disadvantages [2], [9], [10]. Both approaches being widely used may be closely related to familiar approaches for hip arthroplasty [19]. Anatomically and biomechanically, fragments of the femoral head are pushed anteriorly during hip injury in sitting position due to the backward forces of the femur [4], [20]. The pathomechanism of FHF may therefore be analyzed. During knee impaction on hard objects with the sitting position, the femoral head is partially covered by the acetabulum. With hip abduction, forces transferred from the knee will cause the femoral head impacting on the acetabulum and central dislocation occurs. With hip adduction, FHF below or above the fovea (type I or II fractures) may be closely related to the angles of hip flexion in sitting position. A more flexed hip will introduce FHF above the fovea (type II fractures). On the contrary, a less flexed hip may introduce FHF below the fovea (type I fractures). In this study, 21 FHF were type I (60%, 21/35) and 7 FHF were type II (20%, 7/35). Clinically, it may indicate that patients' hips are largely in less flexion during the impaction due to the knee level lower than the seat. If hip adduction is maximal, the femoral head will be pushed out of the posterior rim of the acetabulum and causes a pure posterior hip dislocation without fractures [21].
In the literature, the posterior approach is favored by some orthopedic surgeon because they believe that traumatic posterior dislocation had damaged the medial femoral circumflex artery (MFCA) [22]. The anterior approach may additionally damage the residual blood supply. However, in some current studies, the MFCA is largely preserved when posterior hip reduction is closely reduced [23]. In our study we chose either an anterior or posterior approach based on different fracture pattern in consideration of the convenience for reduction and fixation. Theoretically, an anterior approach is more convenient for fixation of fragments at the anterior part of the femoral head. The AVN rate was similar (17%, p = 0.46) in type I and II fractures. Similarly, in Chen's study an anterior approach was used for treating all Pipkin type I fractures and no AVN occurred [Table 3] [24]. This result may suggest that the anterior approach seems to be relatively safe and the approach method may be decided by fracture pattern [25].
Table 3.
Comparison of clinical outcomes in surgical treatment of Pipkin type I and II fractures.
| Series | Case No. | Approach | Union rate (%) | AVN (%) | HO (%) | OA (%) | F–U (yr) |
|---|---|---|---|---|---|---|---|
| Chen, 2011 [24] | 12 | Ant | 100 | 0 | 42 | – | >2 |
| Mostafa, 2014 [10] | 12 | Troch | 97 | 8.1 | 33 | – | 2.5 |
| 11 | Post | 100 | 18 | 18 | – | 2.5 | |
| Gavaskar, 2015 [12] | 26 | Troch | 100 | 0 | 0 | 0 | 3.0 |
| Masse, 2015 [30] | 13 | Troch | 100 | 10 | 15 | 8 | 7.4 |
| Trikha, 2018 [33] | 32 | Troch | 100 | 3.1 | 6.2 | 6.2 | >2 |
| Present 2019 | 24 | Ant or Post | 100 | 17 | 38 | 0 | 3.3 |
Abbreviations: Ant: anterior; AVN: avascular necrosis; F–U: follow-up; HO: heterotopic ossification; OA: osteoarthritis; Post: posterior; Troch: trochanteric; –: unavailable.
Some studies showed that early treatment within 48 h has better outcomes because blood supply can be restored earlier [26]. However, our result did not support this finding. Patients who underwent surgery within 24 h did not have a lower AVN rate as compared to those beyond 24 h. Because post-hoc power in this comparison was only 0.04. The accuracy could not be confirmed. The reasons of no difference may include the small sample size in all studies, which deeply affects statistical comparison. In addition, the femoral head vascularity (the MFCA) may have been preserved after closed reduction [23]. As long as fragment fixation is not delayed for a long time, the AVN rate may not be increased. The free fragment may achieve revascularization after it is reattached and stabilized on the main femoral head. If the free fragment is far-displaced for a long time, it will become dead bone because of being deprived of blood supply. However, we will suggest that treatment should still be performed as early as possible if patient's condition is stabilized. Delayed operation may cause the care difficulty and even elevate a complication rate.
The incidence of HO was reported 35%–80% in reported studies [27]. In our studies, the incidence of HO is 43%. Among these patients, only one patient (in type IV fractures) developed class 4 HO and others were no more than class 2 [14]. Although HO occurred, patients were usually asymptomatic.
Despite that FHF with or without a hip dislocation is a high-energy trauma, no patients died after arrival at our institution. Generally speaking, surgical outcome is better in types I and II as compared to types III and IV FHF regarding to AVN and HO [Table 2]. Although some articles encourage excision of fragment in Pipkin I fractures; in respect of maintaining joint congruency we generally performed ORIF for type I instead of excision and the clinical result seemed acceptable [3], [10], [25]. The incidence of AVN is still high in type III fractures and the majority of these cases need arthroplasty treatment later. Initial treatment with hip arthroplasty may be considered as another treatment option [2], [28]. In this study [Table 2], AVN occurs in type I (22%), type II (0%), type III (100%), and type IV (25%) fractures. The contradicted incidence in type I and type II fractures may be due to small sample sizes. Type III or type IV fractures normally had a higher incidence of AVN. This study used plain X ray with a minimal follow-up of 6 months to detect the occurrence of AVN. We did not know whether to increase the follow-up duration or to use advanced image modalities such as CT, MRI, or bone scan would increase the incidence of AVN. However, the incidence of AVN is still not low in Pipkin type I and II fractures, and it means that the current treatment techniques still require further improvement.
In the literature, type I or II FHF are favored by ORIF and excision of large fragments is reported to have poor hip function [3], [29], [30], [31]. In the current study, ORIF for FHF in both types has introduced 17% (4/24) AVN and 38% (9/24) HO. The hip function was affected in 17% patients (4/24). Practically, this result may be acceptable.
Hip osteoarthritis may be caused by malunited FHF with the poor acetabular congruence. A malunited fragment of the femoral head may be treated early either by open or arthroscopic osteochondroplasty, especially in active young patients with type I or type II FHF in non-arthritic condition. In such cases, CT or MRI (arthrography) would be necessary.
Recently, Ganz trochanter flip osteotomy was supported by some orthopedic surgeons and satisfactory results were reported [12], [32], [33]. This approach was considered to be able to minimize soft tissue and vascular injuries. However, some orthopedic surgeons had concerned about nonunion of trochanteric fragments after osteotomy [34]. The present study did not include this kind of approach because of unfamiliarity the procedures at that time. Further studies should be necessary.
Using hip arthroscopy to fix the femoral head fractures is rarely reported. Because femoral head fractures are often associated with unstable acetabular fractures, open duction with fixing both fractures are normally necessary. Although simple fixation of the type 1 or type II femoral head fragments is generally effective, it is performed only in 6/144 cases [35].
The limitations of this study may include (1) It is a retrospective study. Many related data are lack and valuable comparison cannot be concluded. Because FHF are uncommon, individual surgeon cannot collect sufficient cases by himself. Moreover, other surgeons may refuse to proceed the similar protocol. (2) The sample size is small. Once it is divided to 4 types, comparison is not convincing. Therefore, we mainly focused on Pipkin type I and II fractures. Even so, the power of this study is still small (0.04). (3) The long-term follow-up rate is low (only a 69% follow-up rate at 1 year). For joint degeneration, at least 2 years is advised [30], [36]. Therefore, an osteoarthritis rate cannot be accurately evaluated in this study.
Conclusion
FHF are uncommon and generally caused by high-energy injuries. Fracture healing can be attained in all femoral head fractures by using open reduction and screw fixation. Our results by using conventional approaches were associated with high complication rates. Further endeavor to improve the outcome should be taken.
Conflicts of interest
There are no conflicts of interest in this study.
Footnotes
Peer review under responsibility of Chang Gung University.
References
- 1.Droll K.P., Broekhuyse H., O'Brien P. Fracture of the femoral head. J Am Acad Orthop Surg. 2007;15:716–727. doi: 10.5435/00124635-200712000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Romeo N.M., Firoozabadi R. Classification in brief: the Pipkin classification of femoral head fractures. Clin Orthop Relat Res. 2008;476:1114–1119. doi: 10.1007/s11999.0000000000000045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Henle P., Kloen P., Siebenrock K.A. Femoral head injuries: which treatment strategy can be recommended? Injury. 2007;38:478–488. doi: 10.1016/j.injury.2007.01.023. [DOI] [PubMed] [Google Scholar]
- 4.Hankin M.H., Morse D.E., Bennett-Clerke C.A. McGraw-Hill Medical; New York, NY: 2013. Clinical anatomy: a case study approach; pp. 350–355. [Google Scholar]
- 5.Pipkin G. Treatment of grade IV fracture-dislocation of the hip. J Bone Joint Surg Am. 1957;39:1027–1042. [PubMed] [Google Scholar]
- 6.Zelken J.A. First-person long-term follow-up using autologous mosaicplasty for osteochondral lesion accompanying femoral head fracture. J Orthop Trauma. 2016;30:e70–e74. doi: 10.1097/BOT.0000000000000439. [DOI] [PubMed] [Google Scholar]
- 7.Asghar F.A., Karunakar M.A. Femoral head fractures: diagnosis, management, and complications. Orthop Clin N Am. 2004;35:463–472. doi: 10.1016/j.ocl.2004.05.004. [DOI] [PubMed] [Google Scholar]
- 8.Giannoudis P.V., Kontakis G., Christoforakis Z., Akula M., Tosounidis T., Koutras C. Management, complications and clinical results of femoral head fractures. Injury. 2009;40:1245–1251. doi: 10.1016/j.injury.2009.10.024. [DOI] [PubMed] [Google Scholar]
- 9.Chen Z.W., Lin B., Zhai W.L., Guo Z.M., Liang Z., Zheng J.P. Conservative versus surgical management of Pipkin type I fractures associated with posterior dislocation of the hip: a randomized controlled trial. Int Orthop. 2011;35:1077–1081. doi: 10.1007/s00264-010-1087-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mostafa M.F., El-Adl W., El-Sayed M.A. Operative treatment of displaced Pipkin type I and II femoral head fractures. Arch Orthop Trauma Surg. 2014;134:637–644. doi: 10.1007/s00402-014-1960-5. [DOI] [PubMed] [Google Scholar]
- 11.Ward Sr W.G., Carter C.J., Wilson S.C., Emory C.L. Femoral stress fractures associated with long-term bisphosphonate treatment. Clin Orthop Relat Res. 2012;470:759–765. doi: 10.1007/s11999-011-2194-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gavaskar A.S., Tummala N.C. Ganz surgical dislocation of the hip is a safe technique for operative treatment of Pipkin fractures. Results of a prospective trial. J Orthop Trauma. 2015;29:544–548. doi: 10.1097/BOT.0000000000000399. [DOI] [PubMed] [Google Scholar]
- 13.Jawad M.U., Haleem A.A., Scully S.P. In brief: Ficat classification: avascular necrosis of the femoral head. Clin Orthop Relat Res. 2012;470:2636–2639. doi: 10.1007/s11999-012-2416-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hug K.T., Alton T.B., Gee A.O. Classifications in brief: Brooker classification of heterotopic ossification after total hip arthroplasty. Clin Orthop Relat Res. 2015;473:2154–2157. doi: 10.1007/s11999-014-4076-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Terjesen T., Gunderson R.B. Radiographic evaluation of osteoarthritis of the hip: an inter-observer study of 61 hips treated for late-detected developmental hip dislocation. Acta Orthop. 2012;83:185–189. doi: 10.3109/17453674.2012.665331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stannard J.P., Harris H.W., Volgas D.A., Alonso J.E. Functional outcome of patients with femoral head fractures associated with hip dislocations. Clin Orthop Relat Res. 2000;377:44–56. doi: 10.1097/00003086-200008000-00008. [DOI] [PubMed] [Google Scholar]
- 17.Siebenrock K.A., Gautier E., Woo A.K., Ganz R. Surgical dislocation of the femoral head for joint debridement and accurate reduction of the acetabulum. J Orthop Trauma. 2002;16:543–552. doi: 10.1097/00005131-200209000-00002. [DOI] [PubMed] [Google Scholar]
- 18.Gardner M.J., Suk M., Pearle A., Buly R.L., Helfet D.L., Lorich D.G. Surgical dislocation of the hip for fractures of the femoral head. J Orthop Trauma. 2005;19:334–342. [PubMed] [Google Scholar]
- 19.Petis S., Howard J.L., Lanting B.L., Vasarhelyi E.M. Surgical approach in primary total hip arthroplasty: anatomy, technique and clinical outcomes. Can J Surg. 2015;58:128–139. doi: 10.1503/cjs.007214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kelley L.L., Petersen C.M. 4th ed. Elsevier; St. Louis, MO: 2018. Sectional anatomy for imaging professionals; pp. 660–687. [Google Scholar]
- 21.Kellam P., Ostrum R.F. Systemic review and meta-analysis of avascular necrosis and posttraumatic arthritis after traumatic hip dislocation. J Orthop Trauma. 2016;30:10–16. doi: 10.1097/BOT.0000000000000419. [DOI] [PubMed] [Google Scholar]
- 22.Gautier E., Ganz K., Krugel N., Gill T., Ganz R. Anatomy of the medial femoral circumflex artery and its surgical implications. J Bone Joint Surg Br. 2000;82:679–683. doi: 10.1302/0301-620x.82b5.10426. [DOI] [PubMed] [Google Scholar]
- 23.Zlotorowicz M., Czubak J., Caban A., Kozinski P., Boguslawska-Walecka R. The blood supply to the femoral head after posterior fracture/dislocation of the hip, assessed by CT angiography. Bone Joint J. 2013;95-B:1453–1457. doi: 10.1302/0301-620X.95B11.32383. [DOI] [PubMed] [Google Scholar]
- 24.Chen Z.W., Zhai W.L., Ding Z.O., Lian K.J., Kang L.Q., Guo L.X. Operative versus nonoperative management of Pipkin type-II fractures associated with posterior hip dislocation. Orthopedics. 2011;34:350. doi: 10.3928/01477447-20110317-09. [DOI] [PubMed] [Google Scholar]
- 25.Wang C.G., Li Y.M., Zhang H.F., Li H., Li Z.J. Anterior approach versus posterior approach for Pipkin I and II femoral head fractures: a systemic review and meta-analysis. Int J Surg. 2016;27:176–181. doi: 10.1016/j.ijsu.2016.02.003. [DOI] [PubMed] [Google Scholar]
- 26.Lin D., Lian K., Chen Z., Wang L., Hao J., Zhang H. Emergent surgical reduction and fixation for Pipkin type I femoral fractures. Orthopedics. 2013;36:778–782. doi: 10.3928/01477447-20130523-24. [DOI] [PubMed] [Google Scholar]
- 27.d'Heurle A., Archdeacon M.T., Hiratzka S., Casstevens C., Finnan R., McCoy B. Do surrogates of injury severity influence the occurrence of heterotopic ossification in fractures of the acetabulum? J Orthop Trauma. 2016;30:213–216. doi: 10.1097/BOT.0000000000000490. [DOI] [PubMed] [Google Scholar]
- 28.Tosounidis T., Aderinto J., Giannoudis P.V. Pipkin Type-III fractures of the femoral head: fix it or replace it? Injury. 2017;48:2375–2378. doi: 10.1016/j.injury.2017.10.002. [DOI] [PubMed] [Google Scholar]
- 29.Tonetti J., Ruatti S., Lafontan V., Loubignac F., Chiron P., Sari-Ali H. Is femoral head fracture-dislocation management improvable: a retrospective study in 110 cases. Orthop Traumatol Surg Res. 2010;96:623–631. doi: 10.1016/j.otsr.2010.03.020. [DOI] [PubMed] [Google Scholar]
- 30.Masse A., Aprato A., Alluto C., Favuto M., Ganz R. Surgical hip dislocation is a reliable approach for treatment of femoral head fractures. Clin Orthop Relat Res. 2015;473:3744–3751. doi: 10.1007/s11999-015-4352-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Park K.S., Lee K.B., Na B.R., Yoon T.R. Clinical and radiographic outcomes of femoral head fractures: excision vs. fixation of fragment in Pipkin type I: what is the optimal choice for femoral head fracture? J Orthop Sci. 2015;20:702–707. doi: 10.1007/s00776-015-0732-6. [DOI] [PubMed] [Google Scholar]
- 32.Solberg B.D., Moon C.N., Franco D.P. Use of trochanteric flip osteotomy improves outcomes in Pipkin IV fractures. Clin Orthop Relat Res. 2009;467:929–933. doi: 10.1007/s11999-008-0505-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Trikha V., Das S., Madegowda A., Agrawal P. Midterm results of trochanteric flip osteotomy technique for management of fractures around the hip. Hip Int. 2018;28:148–155. doi: 10.5301/hipint.5000539. [DOI] [PubMed] [Google Scholar]
- 34.Schoeniger R., LaFrance A.E., Oxland T.R., Ganz R., Leunig M. Does trochanteric step osteotomy provide greater stability than classic slide osteotomy? A preliminary study. Clin Orthop Relat Res. 2009;467:775–782. doi: 10.1007/s11999-008-0668-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Niroopan G., de Sa D., MacDonald A., Burrow S., Larson C.M., Ayeni O.R. Hip arthroscopy in trauma: a systemic review of indications, efficacy, and complications. Arthroscopy. 2016;32:692–703. doi: 10.1016/j.arthro.2015.12.029. [DOI] [PubMed] [Google Scholar]
- 36.Anderson D.D., Chubinskaya S., Guilak F., Martin J.A., Oegema T.R., Olson S.A. Post-traumatic osteoarthritis: improved understanding and opportunities for early intervention. J Orthop Res. 2011;29:802–809. doi: 10.1002/jor.21359. [DOI] [PMC free article] [PubMed] [Google Scholar]