Abstract
The novel coronavirus disease (COVID-19) has had a significant impact on public health, economic activity, and mental health as it spread across the globe. Research from past pandemics links excessive anxiety about illness-related threats with symptoms of health anxiety and obsessive-compulsive disorder (OCD). In the present study, we investigated whether intolerance of uncertainty (IU), a psychological vulnerability factor involved in both OCD and health anxiety, accounts for a portion of the relationship between these symptoms and fear of COVID-19 during the early stages of the outbreak in the Unites States. We administered measures of concern about the spread of COVID-19 (Coronavirus Threat Scale; CTS), health anxiety, and OCD symptoms to a large sample of community adults in the United States (n = 738) recruited through Amazon MTurk. Results revealed that concern about COVID-19 was moderately and positively correlated with both OCD and health anxiety symptoms, as well as IU. Moreover, regression analyses found that IU partially accounted for the connections between concern about the spread of COVID-19 and OCD and health anxiety symptoms. These results highlight IU as a potential mechanism connecting OCD and health anxiety to anxiety about pandemic threats. Clinical implications, limitations, and future directions for research are discussed.
Keywords: Obsessive-compulsive disorder, Health anxiety, Intolerance of uncertainty, Coronavirus, COVID-19
1. Introduction
The novel coronavirus disease (COVID-19), which is caused by the SARS-CoV-2 virus, was first detected in Wuhan, China and has since been declared a global pandemic (CDC, 2020). Although the full extent of the impact of COVID-19 remains unknown, the virus has already caused major societal disruption, economic upheaval and public health burden as it spread across the globe. COVID-19 has also had significant negative effects on mental health and wellbeing. In particular, the spread of the virus has been associated with widespread anxiety among the public in many countries across the globe (Hyland et al., 2020; Ozamiz-Etxebarria, Dosil-Santamaria, Picaza-Gorrochategui, & Idoiaga-Mondragon, 2020; Shigemura, Ursano, Morganstein, Kurosawa, & Benedek, 2020; Twenge & Joiner, 2020; Wang et al., 2020). At healthy levels, anxiety can motivate protective behavioral changes. However, for some individuals the threat of a pandemic illness can lead to excessive, maladaptive levels of anxiety. In particular, recent editorials have suggested the COVID-19 outbreak may cause excessive anxiety and mental suffering for patients with obsessive-compulsive disorder (OCD; Fineberg et al., 2020) and severe health anxiety (Asmundson & Taylor, 2020).
Obsessive-compulsive disorder (OCD) is characterized by obsessions (recurring intrusive thoughts or impulses), and compulsions (repetitive behaviors and/or mental acts performed in response to an obsession or rules that must be applied rigidly) (American Psychiatric Association, 2013). OCD has a 12-month prevalence of about 1% (Ruscio, Stein, Chiu, & Kessler, 2010) and can be disabling when severe. OCD is a heterogeneous condition, but some of the most commonly reported obsessions and compulsions pertain to fears of germs and contamination coupled with compulsive washing rituals (Abramowitz et al., 2010; McKay et al., 2004). These symptoms are often motivated by fears of contracting a disease, as well as transmitting illnesses to others (Rachman, 2004; Wheaton, Abramowitz, Berman, Riemann, & Hale, 2010). Therefore, pandemic illness threats may be particularly anxiety-provoking for individuals with OCD symptoms in this dimension. Indeed, past research has found significant associations between OCD symptomatology and anxiety in response to past illness outbreaks including the 2009–2010 H1N1 “Swine Flu” (Brand, McKay, Wheaton, & Abramowitz, 2013), 2015–2016 Zika virus outbreak (Blakey & Abramowitz, 2017) and Ebola threat of 2014 (Blakey, Reuman, Jacoby, & Abramowitz, 2015). Already COVID-19 has had much more widespread impact than these past illnesses. Therefore, it is likely that COVID-19 may have particularly strong impact among individuals with OCD (Fineberg et al., 2020).
Similarly, individuals with severe health anxiety may also be especially affected by COVID-19 (Asmundson & Taylor, 2020). Whereas it is adaptive and protective to be concerned for one's health to some extent, health anxiety becomes problematic when the anxiety is chronic and excessive (Taylor & Asmundson, 2004). Some individuals experience severe health anxiety characterized by chronic worry about developing a serious illness, frequent checking one's body for signs of illness, frequent attending of medical appointments for reassurance, or avoidance of medical appointments and other areas with the fear of diagnosis or contraction of a serious illness (Taylor, McKay, & Abramowitz, 2012). Formerly such individuals would have been diagnosed with hypochondriasis, prior to the development of illness anxiety disorder and complex somatic symptom disorder in the fifth edition of the Diagnostic Manual of Mental Disorders (APA, 2013). Health anxiety and OCD share many similar features, and some have suggested that severe health anxiety belongs among a spectrum of OCD-related conditions (Murphy, Timpano, Wheaton, Greenberg, & Miguel, 2010). As with OCD symptoms, prior work has found positive relationships between levels of health anxiety and excessive fears of past pandemic illness threats including H1N1 “Swine Flu” (Brand et al., 2013; Wheaton, Abramowitz, Berman, Fabricant, & Olatunji, 2012), Zika (Blakey & Abramowitz, 2017) and Ebola (Blakey et al., 2015). Individuals with pre-existing health anxiety would likely experience elevated fears of the spread of COVID-19 given its depiction in the media as highly communicable and severe (Asmundson & Taylor, 2020; Wheaton et al., 2010; Dennis, Radnitz, & Wheaton, 2020), though this requires empirical investigation.
Rapidly emerging data suggest significant links between OCD symptoms, health anxiety and reactions to COVID-19: Taylor et al. (2020a) developed the COVID-19 Stress Scale, which assesses COVID-related stress across five dimensions: (1) Danger and contamination fears, (2) fears about economic consequences, (3) xenophobia, (4) compulsive checking and reassurance seeking, and (5) traumatic stress symptoms about COVID-19. Scores on this measure were significantly correlated with OCD symptoms and health anxiety in a large community sample (Taylor et al., 2020a). However more study is needed to replicate and extend these findings.
It is also important to investigate the mechanisms that connect health anxiety and OCD symptoms to excessive fear in response to the threat of COVID-19. Existing research on anxiety in response to past pandemic illness threats has considered OCD-related factors such as disgust sensitivity (Wheaton et al., 2012) and obsessive beliefs (Brand et al., 2012). Other work has looked at factors related to illness anxiety, such as body vigilance (Wheaton et al., 2012), anxiety sensitivity (Reuman et al., 2017) and threat-related appraisals of illness severity and controllability (Scherr, Jensen, & Christy, 2017). A recent study found that fear of contracting COVID-19 was predicted by disgust propensity and anxiety sensitivity (McKay, Yang, Elhai, & Asmundson, 2020). While a range of psychological factors have been investigated as relating to fears of pandemic illnesses, an additional factor that has received limited research attention is intolerance of uncertainty (IU).
IU is defined as the “dispositional incapacity to endure the aversive response triggered by the perceived absence of salient, key, or sufficient information, and sustained by the associated perception of uncertainty.” (p. 31, Carleton, 2016). IU has been implicated as an important contributing factor to both health anxiety (Fergus & Bardeen, 2013; Fergus & Valentiner, 2011a; Wright, Levell, & Carleton, 2016) and OCD symptoms (Sarawgi, Oglesby, & Cougle, 2013; Tolin, Abramowitz, Brigidi, & Foa, 2003). At a behavioral level, individuals high in IU often attempt to avoid uncertainty, or respond to it in maladaptive ways, such as worry and excessive certainty-seeking behaviors (e.g., checking and reassurance-seeking; Carleton et al., 2012). Only a small number of studies have investigated the relationship between IU and responses to pandemic threats. A single past study found that anxiety in response to the 2009 H1N1 pandemic was linked to higher IU (Taha, Matheson, Cronin, & Anisman, 2014). A very recent study (Taylor et al., 2020b) proposed a “COVID Stress Syndrome” characterized by a broad set of distress symptoms in response to COVID-19 including: (1) Danger and contamination fears, (2) fears about economic consequences, (3) xenophobia, (4) compulsive checking and reassurance seeking, and (5) traumatic stress symptoms about COVID-19. In a large community sample, greater IU was significantly correlated with the aggregated symptoms of the symptoms of the postulated COVID-19 Stress Syndrome (Taylor et al., 2020b). However, no study has yet investigated whether IU may be a contributing factor linking fear of a pandemic illness to OCD symptoms or health anxiety.
IU may be a particularly important contributing factor to excessive anxiety during the early phases of a viral illness outbreak, when it is unclear how deadly a virus is, how far it will spread, and what, if any, treatment options will be available (Dennis, Radnitz, & Wheaton, 2020). Therefore, this study sought to investigate the relationship between excessive anxiety and behavioral responses to the COVID-19 pandemic and symptoms of OCD and health anxiety during the early phases of the outbreak. We also included a measure of IU do determine whether difficulty responding to the unknown would account for a portion of the connection between health anxiety, OCD symptoms and fear of COVID-19 during this time. We gathered data from an adult community sample in the United States during early March of 2020, a time when media reports about the potential severity of the threat were common but the extent of the illness outbreak remained unknown. We hypothesized that health anxiety symptoms and OCD symptoms (particularly fears of contamination) would both relate to concerns about the spread of COVID-19. We also predicted that IU would account for a statistically significant portion of the connections between these symptoms and COVID-19-related concerns. We elected to test our hypotheses in an unscreened adult community sample based on findings that both OCD symptoms (Olatunji, Williams, Haslam, Abramowitz, & Tolin, 2008) and health anxiety (Ferguson, 2009) occur along continuous distributions in the population.
2. Method
2.1. Participants
Participants for the present study were recruited through Amazon Mechanical Turk (MTurk), an online marketplace that connects researchers with potential participants that is frequently used in psychological research (Buhrmester, Kwang, & Gosling, 2011; Chandler et al., 2019; Coppock, 2019). Participants were required to be English-speaking residents of the United States but there were no other inclusion/exclusion criteria. In line with recommendations for online crowdsources research (Fleischer, Mead, & Huang, 2015), the survey responses were carefully screened to ensure valid responding. Multiple validation methods were utilized, including eliminating responses from participants who failed validity check “catch” items, those who completed the survey too quickly to have responded accurately, and those who completed free response questions with incomprehensible text. Of 1197 submitted responses, we analyzed data from 720 individuals who passed validity checks. The sample consisted of 362 females (50.3%), 352 males (48.9%), and 6 individuals (0.8%) who selected “other” for gender. The sample had a mean age of 36.87 years (SD = 11.87, range 18–74). Racial-ethnic composition was as follows: 68.4% non-Hispanic White, 14.7% Hispanic/Latino, 10.8% African American, 5.3% Asian/Pacific Islander, and 0.8% “other.”
2.2. Procedure
Participants completed the study measures as part of an online survey that was collected using Qualtrics, an online survey development tool. MTurk workers completed the survey in exchange for monetary compensation. To prevent self-selection based on participant knowledge of and interest in COVID-19, the recruitment advertisement did not mention COVID-19. Data were collected from March 2 to March 11, 2020, which was early in the COVID-19 outbreak in the United States (i.e., less than 1300 cases had been confirmed in the country at this time). The research protocol was reviewed and approved by the local Institutional Review Board (IRB). The first page of the survey comprised the study consent form and all participants had to provide consent prior to answering study questions. Questionnaires were administered in a fixed order. To prevent the possibility that assessing COVID-19 fears would influence subsequent reporting on health anxiety and OCD symptoms, questions about COVID-19 were administered last. Statistical analyses were run using IBM SPSS (Version 26, Armonk, NY).
2.3. Measures
Intolerance of Uncertainty Scale-12 (IUS-12; Carleton, Norton, & Asmundson, 2007). The IUS-12 is a short form of the original 27-item IUS (Freeston, Rhéaume, Letarte, Dugas, & Ladouceur, 1994). Items on the IUS-12 desire for predictability, anxiety about future uncertain events, and seeking information to increase certainty. The IUS-12 is widely employed as a measure of IU and has good psychometric properties (Carleton et al., 2007; Fergus & Bardeen, 2013; Gentes & Ruscio, 2011). Higher scores indicate greater IU. In the present sample, the IUS-12 demonstrated excellent internal consistency (α = 0.91).
Dimensional Obsessive Compulsive Scale (DOCS; Abramowitz et al., 2010). The DOCS is a 20-item self-report measure that assesses the severity of the four most consistently replicated OCD symptom dimensions: contamination, responsibility for harm and mistakes, symmetry/ordering, and unacceptable thoughts. Each dimension is assessed with its own DOCS subscale, which begins with a description of the symptom dimension along with examples of representative obsessions and rituals. For each symptom dimension, five items (rated 0 to 4) assess the following parameters of severity: (a) time occupied by obsessions and compulsions, (b) avoidance, (c) distress, (d) functional impairment, and (e) difficulty disregarding the obsessions and refraining from compulsions. Higher scores on the DOCS indicate more severe OCD symptoms. The DOCS converges well with other measures of OCD symptoms and has been shown to have excellent psychometric properties (Abramowitz et al., 2010). In the present study, total scores on the DOCS demonstrated excellent internal consistency (α = 0.96). The DOCS subscales had good reliability (range in α′s = 0.88-0.92).
Short Health Anxiety Inventory (SHAI; Salkovskis, Rimes, Warwick, & Clark, 2002). The SHAI is an 18-item self-report inventory assessing severity of health anxiety, independent of physical health. It assesses worry about one's health, awareness of body sensations/changes, and fear of illness consequences. Each item utilizes a four-point ordinal scale, with higher scores indicating greater health anxiety. The SHAI has good psychometric properties and construct validity and is commonly utilized in research studies (Wheaton, Berman, Franklin, & Abramowitz, 2010). The SHAI includes 14 items pertaining to fears of becoming ill, as well as a 4-item subscale assessing beliefs about the consequences of having a severe illness. Given that past research suggests that the illness consequences subscale is less relevant to the health anxiety domain (Alberts, Sharpe, Kehler, & Hadjistavropoulos, 2011; Fergus & Valentiner, 2011b), in the present study we totaled only the first 14 items of the SHAI. Scores on these 14 items demonstrated excellent internal consistency (α = 0.90).
COVID-19 Threat Scale (CTS; Wheaton, Prikhidko, & Messner, 2020). The CTS is a self-report inventory that was developed by adapting a questionnaire developed to assess anxiety in response to the H1N1 “Swine Flu” Influenza (Wheaton et al., 2012). Items on the CTS quantify threat-related perceptions of the Coronavirus utilizing a 5-point Likert Scale (from 1-Not at all to 5-Very Much). Higher scores reflect a greater anxiety and threat-related behaviors due to COVID-19. Items asked participants to rate their fears that COVID-19 will spread widely in the United States, their fears about becoming ill or family members becoming ill, as well as behavioral changes in response to COVID-19 (e.g., decisions to be around other people, handwashing). With minor variations, these same item stems have been utilized to quantify fears of past pandemic outbreaks, including H1N1 (Brand et al., 2013; Wheaton et al., 2012), Zika Virus (Blakey & Abramowitz, 2017) and Ebola (Blakey et al., 2015). In each instance the total scores on these items have demonstrated good psychometric properties and convergent validity with anxiety-related constructs. Total scores demonstrated good internal consistency (α = 0.88).
2.4. Data analytic strategy
We first calculated descriptive statistics and Pearson's zero order correlations among the study measures. We next used regression analyses to determine whether IU accounts for a significant portion of the connections between OCD symptoms, health anxiety symptoms, and concern about COVID-19. Models were run separately for OCD and healthy anxiety symptoms. For each construct, we utilized the PROCESS SPSS macro provided by Preacher and Hayes (2008) to compare the results of simultaneous regressions in which symptoms (DOCS in Model 1 and SHAI in Model 2) and the IUS-12 were entered simultaneously as predictors of COVID-19-related concerns (CTS scores) to direct effect models in which symptoms alone were used to predict CTS scores. The significance of the indirect effect via IU was tested via bootstrapping (taking the mean of 5000 bootstrapped resamples from the data) and effect size was estimated by calculating the proportion of direct effects of symptoms on concern about COVID-19 that was accounted for by IUS-12 scores. Alpha was set at p ≤ .01.
3. Results
3.1. Descriptive statistics
Means and standard deviations for all study measures are presented in Table 1 . Scores on the DOCS were somewhat higher than other unscreened community samples (M = 13.73; Fergus & Carmin, 2014) but below clinical samples (M = 30.06; Abramowitz et al., 2010). Scores on the SHAI were similarly slightly elevated relative to previous studies that employed the 14-item version of this scale in adult community samples (Alberts et al., 2011; Fergus, 2013).
Table 1.
Zero order correlations among study measures.
| CTS | IUS | DOCS total | DOCS-C | DOCS-RH | DOCS-UT | DOCS-S | SHAI | Mean (SD) | |
|---|---|---|---|---|---|---|---|---|---|
| CTS | – | 30.75 (8.61) | |||||||
| IUS | .41* | – | 36.02 (9.94) | ||||||
| DOCS total | .53* | .59* | – | 20.98 (15.81) | |||||
| DOCS-C | .58* | .47* | .84* | – | 5.92 (4.39) | ||||
| DOCS-RH | .49* | .56* | .89* | .70* | – | 5.30 (4.64) | |||
| DOCS-UT | .37* | .51* | .86* | .59* | .69* | – | 5.12 (4.76) | ||
| DOSCS-S | .38* | .48* | .86* | .61* | .67* | .67* | – | 4.63 (4.54) | |
| SHAI | .44* | .45* | .63* | .50* | .59* | .53* | .57* | – | 13.01 (7.25) |
*p < .001.
Note. DOCS = Dimensional Obsessive Compulsive Scale; DOCS-C=Contamination Subscale; DOCS-RH = Responsibility for harm subscale; DOCS-UT=Unacceptable Thoughts Subscale; DOCS-S=Symmetry Subscale; IUS=Intolerance of Uncertainty Scale-12; SHAI = Short Health Anxiety Inventory; CTS=COVID-19 Threat Scale.
3.2. Zero-order correlations
We computed Pearson zero-order correlations between the study measures as shown in Table 1. As predicted, concerns about COVID-19 (CTS scores) were significantly positively correlated with health anxiety (SHAI, r = 0.44, p < .001), OCD symptoms (DOCS, r = 0.53, p < .001) and IU (IUS-12, r = 0.41, p < .001). Analysis of the DOCS subscales found that CTS scores were positively correlated with all four OCD symptoms dimensions, but most strongly for the contamination/washing symptom dimension (r = 0.58, p < .001).
3.3. Regression analyses
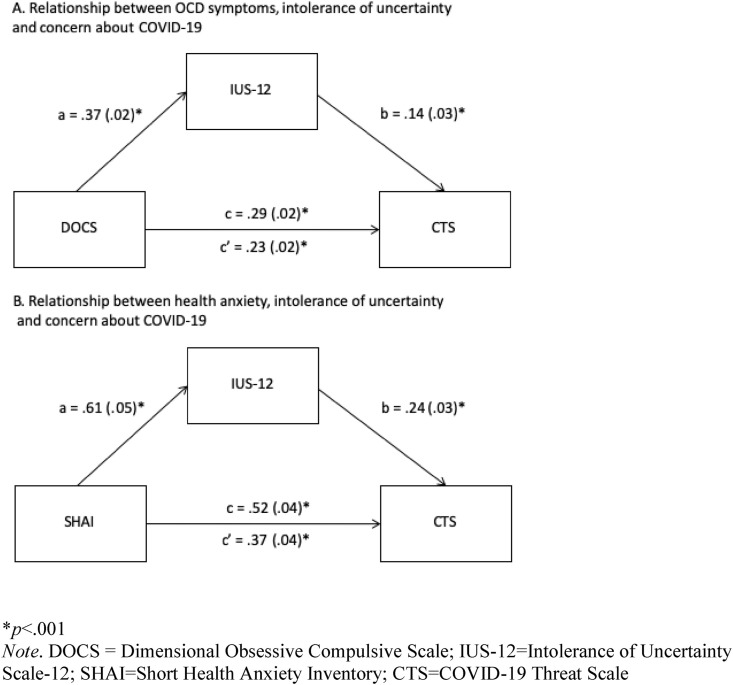
The first regression analysis considered IU as a factor in the association between OCD symptoms and concerns about COVID-19 as illustrated in Fig. 1 . The simultaneous regression accounted for 34% of the variance in CTS scores (R2 = 0.34, p < .001), with both DOCS (b = 0.23 [0.02], p < .001) and IUS-12 (b = 0.14 [0.03], p < .001) emerging as significant individual predictors. As shown, the significant direct association between DOCS total score and CTS (c path) was reduced in magnitude once IUS-12 was accounted for (c′ path). We calculated the proportion of the direct effect of DOCS scores that was accounted for via the IUS-12, which showed that 22.22% of the relationship between OCD symptoms and concern about COVID-19 was accounted for by the IUS-12. The point estimate for the indirect effect (taking the mean of 5000 bootstrapped resamples from the data) was 0.05 (SE = 0.01). The bias-corrected bootstrapped 99% confidence interval did not contain zero (99% CI = 0.02 to 0.09), indicating the effect was significant, p < .01.
Fig. 1.
*p < .001.
Note. DOCS = dimensional obsessive compulsive scale; IUS-12 = Intolerance of uncertainty Scale-12; SHAI=Short health anxiety inventory; CTS=COVID-19 threat scale.
Fig. 1 Panel B, presents a similar model in which IU accounts for a portion of the association between health anxiety (SHAI scores) and concern about COVID-19. The simultaneous regression accounted for 25% of the variance in CTS scores (R2 = 0.25, p < .001), with both SHAI (b = 0.37 [0.04], p < .001) and IUS-12 (b = 0.24 [0.03], p < .001) emerging as significant individual predictors. As shown in the figure, the significant direct association between SHAI and CTS (c path) was reduced in magnitude once the IUS-12 was accounted for (c′ path). Calculating the proportion of the direct effect that was explained, showed that 38.75% of the relationship between health anxiety symptoms and concern about COVID-19 was accounted for by the IUS-12. The point estimate for the indirect effect was 0.15 (SE = 0.02) and the bias-corrected bootstrapped 99% confidence interval did not contain zero (99% CI = 0.09 to 0.21), indicating the effect was significant, p < .01.
4. Discussion
The present study examined the relationship between health anxiety, OCD symptoms, IU, and concern about the spread of COVID-19. As we predicted, we found significant positive correlations between OCD symptoms, health anxiety and fear of the spread of COVID-19. Our results are consistent with recent editorials that have suggested a link between excessive concern about the COVID-19 outbreak and OCD (Fineberg et al., 2015) and health anxiety (Asmundson & Taylor, 2020), as well as recently emerging data (Taylor et al., 2020a,b). These results are also consistent with past empirical reports from prior pandemic illness threats, which found that OCD and health anxiety symptoms also related to anxiety about the spread of H1N1 “Swine Flu” Influenza (Brand et al., 2013; Wheaton et al., 2012), Zika virus (Blakey & Abramowitz, 2017) and Ebola (Blakey et al., 2015). The present results comport with these findings in suggesting that pandemic illness threats are salient for individuals with OCD symptoms and health anxiety. Among the adult community members who comprised our sample, those with greater OCD symptoms and health anxiety experienced more concerns about the spread of COVID-19 during the early stages of the illness threat in the United States.
Our results also evaluated a potential mechanism connecting OCD and health anxiety symptoms to excessive concerns about COVID-19: difficulty tolerating uncertainty. Substantial past work has suggested that IU is a contributing factor to both OCD and health anxiety symptoms (Fergus & Bardeen, 2013; Fergus & Valentiner, 2011a; Sarawgi et al., 2013; Tolin et al., 2003; Wright, Levell, & Carleton, 2016). Here we also found a positive correlation between IU and fear of COVID-19 (similar to a past report linking IU to anxiety about H1N1; Taha et al., 2014 and a recent report linking IU to “COVID Stress Syndrome”; Taylor et al., 2020b). Our results extend these findings by also considering IU as a factor accounting for the connection between health anxiety and OCD symptoms and concern about COVID-19. This result should be interpreted within the context that our data was collected from March 2nd-11th 2020, which was early on in the illness outbreak in the United States. At this point in the crisis, the threat was largely an unknown possibility, as some media reports from the time included both dire projects about the potential impact of the disease, whereas others downplayed the potential threat. Thus, the tendency to have aversive responses to uncertainty and ambiguity could amplify concerns about COVID-19 during this time given the extent that the threat was unknown.
Although data for the present study came from an unscreened community sample, the present results may have clinical implications. Evidence suggests that IU is malleable (Dugas & Ladouceur, 2000) and specific treatment techniques have been developed to enhance patients’ ability to cope with uncertainty via cognitive behavioral therapy (Robichaud & Dugas, 2006). It is therefore possible that utilizing interventions targeting IU might help to ameliorate excessive anxiety in light of a pandemic threat. That is, interventions designed to help individuals tolerate and accept uncertainty might be beneficial in working with patients with OCD and health anxiety concerns under the extraordinary circumstances involved in a pandemic disease threat. However, this possibility requires empirical testing via a treatment trial.
It should be noted that although IU accounted for a portion of the links between health anxiety, OCD symptoms, and concern about COVID-19, we did not formally evaluate mediation. Mediation implies cause-and-effect relationships that occur sequentially over time and analysis of cross-sectional data can yield biased estimates of mediational effects (Maxwell & Cole, 2007; Maxwell, Cole, & Mitchell, 2011). Therefore, concluding mediation would require a longitudinal design (i.e., assessing IU prior to a disease outbreak and subsequently assessing pandemic-related anxiety). Yet, cross-sectional studies can be useful in demonstrating when potential third variables share outcome variance with predictors to develop mediational hypotheses to be evaluated longitudinally (Shrout, 2011). Within this framework, the present results highlight the possibility that IU may be a shared mechanism linking OCD, health anxiety and fear of pandemics, though future longitudinal work is needed. In addition, IU accounted for only a portion of the direct links between these symptoms and pandemic fears. This suggests that other factors are likely to be important in the connections between health anxiety, OCD symptoms and COVID-19 related fears. For example, past work on pandemic fears has implicated factors such as anxiety sensitivity (Blakey et al., 2015), body vigilance (Wheaton et al., 2012) disgust sensitivity (Blakey & Abramowitz, 2017) and obsessive beliefs (Brand et al., 2013). Similarly, a recent study (McKay et al., 2020) found that disgust sensitivity and anxiety sensitivity predicted anxiety in response to COVID-19, both independently and interactively. Thus, there may be multiple pathways connecting these constructs, and helping individuals experiencing excessive fears of a pandemic illness may require a multipronged effort. Importantly, it is also necessary to determine whether IU and these other factors overlap in variance accounted for. Unfortunately, the survey we administered did not include these measures and so we are unable to control for them here, leaving an important direction for future research.
Our findings should be evaluated in light of several additional study limitations. First, all data were collected online via Amazon Mturk. Although this approach allowed for rapid collection of a community sample of adults, sole reliance on self-report questionnaires may have inflated the relationship between variables due to shared methods variance. In addition, use of an unscreened community sample allowed us to study the full range of OCD and healthy anxiety symptom severity, as these variables are continuously distributed in the population. However, no formal diagnoses were made and so future research is needed replicate these results in clinical samples of patients with OCD and health anxiety. Future research also might consider studying the relationship between IU and other alternative measures related to the COVID-19 pandemic, including the COVID Stress Scales (Taylor et al., 2020b) and Fear of COVID-19 Scale (Ahorsu et al., 2020). Specifically, these scales might be utilized to tap into other dimensions of COVID-19's impact on mental health (e.g., worry about finances and traumatic stress symptoms), to determine whether IU is related to specific distress reactions to COVID-19.
Notwithstanding these limitations, the present report highlights the possibility that IU contributes to illness fears during a pandemic outbreak, particularly in the context of OCD symptoms and health healanxiety. Our results suggest a need for further exploration in this area. For example, studies in clinical populations might be used to verify the possibility that difficulty tolerating uncertainty contributes to excessive anxiety about a pandemic illness threat in patients with OCD and severe health anxiety. In addition, future work might explore whether interventions tailored to address IU might help these patients to cope with the uncertainties involved an epidemic outbreak and thereby reduce excessive anxiety.
Informed consent
All participants provided informed consent and the study protocol was reviewed and approved by the local IRB.
Animal rights statements
No animal studies were carried out for this study.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
The authors declare that they have no conflict of interest.
References
- Abramowitz J.S., Deacon B.J., Olatunji B.O., Wheaton M.G., Berman N.C., Losardo D., Björgvinsson T. Assessment of obsessive-compulsive symptom dimensions: Development and evaluation of the dimensional obsessive-compulsive scale. Psychological Assessment. 2010;22(1):180–198. doi: 10.1037/a0018260. [DOI] [PubMed] [Google Scholar]
- Ahorsu D.K., Lin C.Y., Imani V., Saffari M., Griffiths M.D., Pakpour A.H. The fear of COVID-19 scale: Development and initial validation. International Journal of Mental Health and Addiction. 2020:1–9. doi: 10.1007/s11469-020-00270-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alberts N.M., Sharpe D., Kehler M.D., Hadjistavropoulos H.D. Health anxiety: Comparison of the latent structure in medical and non-medical samples. Journal of Anxiety Disorders. 2011;25(4):612–614. doi: 10.1016/j.janxdis.2011.01.011. [DOI] [PubMed] [Google Scholar]
- Dennis D., Radnitz C., Wheaton M.G. International Journal of Cognitive Therapy; 2020. A perfect storm? Health and contamination anxiety and COVID-19: Lessons from past pandemics and current challenges. In press. [Google Scholar]
- American Psychiatric Association . American Psychiatric Publishing; Arlington: 2013. Diagnostic and statistical manual of mental disorders. [Google Scholar]
- Asmundson G.J., Taylor S. How health anxiety influences responses to viral outbreaks like COVID-19: What all decision-makers, health authorities, and health care professionals need to know. Journal of Anxiety Disorders. 2020;71:102211. doi: 10.1016/j.janxdis.2020.102211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blakey S.M., Abramowitz J.S. Psychological predictors of health anxiety in response to the Zika virus. Journal of Clinical Psychology in Medical Settings. 2017;24(3–4):270–278. doi: 10.1007/s10880-017-9514-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blakey S.M., Reuman L., Jacoby R.J., Abramowitz J.S. Tracing “fearbola”: Psychological predictors of anxious responding to the threat of Ebola. Cognitive Therapy and Research. 2015;39(6):816–825. doi: 10.1007/s10608-015-9701-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brand J., McKay D., Wheaton M.G., Abramowitz J.S. The relationship between obsessive compulsive beliefs and symptoms, anxiety and disgust sensitivity, and Swine Flu fears. Journal of Obsessive-Compulsive and Related Disorders. 2013;2(2):200–206. doi: 10.1016/j.jocrd.2013.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buhrmester M., Kwang T., Gosling S.D. Amazon's Mechanical Turk a new source of inexpensive, yet high-quality, data? Perspectives on Psychological Science. 2011;6(1):3–5. doi: 10.1177/1745691610393980. [DOI] [PubMed] [Google Scholar]
- Carleton R.N. The intolerance of uncertainty construct in the context of anxiety disorders: Theoretical and practical perspectives. Expert Review of Neurotherapeutics. 2012;12:937–947. doi: 10.1586/ern.12.82. [DOI] [PubMed] [Google Scholar]
- Carleton R.N. Into the unknown: A review and synthesis of contemporary models involving uncertainty. Journal of Anxiety Disorders. 2016;39:30–43. doi: 10.1016/j.janxdis.2016.02.007. [DOI] [PubMed] [Google Scholar]
- Carleton R.N., Norton M.P.J., Asmundson G.J. Fearing the unknown: A short version of the intolerance of uncertainty scale. Journal of Anxiety Disorders. 2007;21(1):105–117. doi: 10.1016/j.janxdis.2006.03.014. [DOI] [PubMed] [Google Scholar]
- CDC . 2020. Coronavirus disease 2019 (COVID-19) in the U.S. Centers for disease control and prevention.https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html [Google Scholar]
- Chandler J., Rosenzweig C., Moss A.J., et al. Online panels in social science research: Expanding sampling methods beyond Mechanical Turk. Behav Res. 2019;51:2022–2038. doi: 10.3758/s13428-019-01273-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coppock A. Generalizing from survey experiments conducted on mechanical Turk: A replication approach. Political Science Research and Methods. 2019;7(3):613–628. [Google Scholar]
- Dugas M.J., Ladouceur R. Treatment of GAD targeting intolerance of uncertainty in two types of worry. Behavior Modification. 2000;24(5):635–657. doi: 10.1177/0145445500245002. [DOI] [PubMed] [Google Scholar]
- Fergus T.A. Repetitive thought and health anxiety: Tests of specificity. Journal of Psychopathology and Behavioral Assessment. 2013;35(3):366–374. [Google Scholar]
- Fergus T.A., Bardeen J.R. Anxiety sensitivity and intolerance of uncertainty: Evidence of incremental specificity in relation to health anxiety. Personality and Individual Differences. 2013;55(6):640–644. [Google Scholar]
- Fergus T.A., Carmin C.N. The validity and specificity of the short-form of the Obsessive Beliefs Questionnaire (OBQ) Journal of Psychopathology and Behavioral Assessment. 2014;36(2):318–328. [Google Scholar]
- Ferguson E. A taxometric analysis of health anxiety. Psychological Medicine. 2009;39(2):277–285. doi: 10.1017/S0033291708003322. [DOI] [PubMed] [Google Scholar]
- Fergus T.A., Valentiner D.P. Intolerance of uncertainty moderates the relationship between catastrophic health appraisals and health anxiety. Cognitive Therapy and Research. 2011;35(6):560–565. [Google Scholar]
- Fergus T.A., Valentiner D.P. The short health anxiety inventory and multidimensional inventory of hypochondriacal traits: A comparison of two self-report measures of health anxiety. Cognitive Therapy and Research. 2011;35(6):566–574. [Google Scholar]
- Fineberg N.A., Van Ameringen M., Drummond L., Hollander E., Stein D.J., Geller D., Rodriguez C.I. How to manage obsessive-compulsive disorder (OCD) under COVID-19: A clinician’s guide from the international college of obsessive compulsive spectrum disorders (ICOCS) and the obsessive-compulsive research network (ocrn) of the European college of neuropsychopharmacology. Comprehensive Psychiatry. 2020;100 doi: 10.1016/j.comppsych.2020.152174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fleischer A., Mead A.D., Huang J. Inattentive responding in MTurk and other online samples. Industrial and Organizational Psychology. 2015;8(2):196–202. [Google Scholar]
- Freeston M.H., Rhéaume J., Letarte H., Dugas M.J., Ladouceur R. Why do people worry? Personality and Individual Differences. 1994;17(6):791–802. [Google Scholar]
- Gentes E.L., Ruscio A.M. A meta-analysis of the relation of intolerance of uncertainty to symptoms of generalized anxiety disorder, major depressive disorder, and obsessive–compulsive disorder. Clinical Psychology Review. 2011;31(6):923–933. doi: 10.1016/j.cpr.2011.05.001. [DOI] [PubMed] [Google Scholar]
- Hyland P., Shevlin M., McBride O., Murphy J., Karatzias T., Bentall R.P., et al. Anxiety and depression in the Republic of Ireland during the COVID‐19 pandemic. Acta Psychiatrica Scandinavica. 2020 doi: 10.1111/acps.13219. [DOI] [PubMed] [Google Scholar]
- Maxwell S.E., Cole D.A. Bias in cross-sectional analyses of longitudinal mediation. Psychological Methods. 2007;12(1):23. doi: 10.1037/1082-989X.12.1.23. [DOI] [PubMed] [Google Scholar]
- Maxwell S.E., Cole D.A., Mitchell M.A. Bias in cross-sectional analyses of longitudinal mediation: Partial and complete mediation under an autoregressive model. Multivariate Behavioral Research. 2011;46(5):816–841. doi: 10.1080/00273171.2011.606716. [DOI] [PubMed] [Google Scholar]
- McKay D., Abramowitz J.S., Calamari J.E., Kyrios M., Radomsky A., Sookman D., Wilhelm S. A critical evaluation of obsessive–compulsive disorder subtypes: Symptoms versus mechanisms. Clinical Psychology Review. 2004;24(3):283–313. doi: 10.1016/j.cpr.2004.04.003. [DOI] [PubMed] [Google Scholar]
- McKay D., Yang H., Elhai J., Asmundson G. Anxiety regarding contracting COVID-19 related to interoceptive anxiety sensations: The moderating role of disgust propensity and sensitivity. Journal of Anxiety Disorders. 2020:102233. doi: 10.1016/j.janxdis.2020.102233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy D.L., Timpano K.R., Wheaton M.G., Greenberg B.D., Miguel E.C. Obsessive-compulsive disorder and its related disorders: A reappraisal of obsessive-compulsive spectrum concepts. Dialogues in Clinical Neuroscience. 2010;12(2):131–148. doi: 10.31887/DCNS.2010.12.2/dmurphy. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olatunji B.O., Williams B.J., Haslam N., Abramowitz J.S., Tolin D.F. The latent structure of obsessive‐compulsive symptoms: A taxometric study. Depression and Anxiety. 2008;25(11):956–968. doi: 10.1002/da.20387. [DOI] [PubMed] [Google Scholar]
- Ozamiz-Etxebarria N., Dosil-Santamaria M., Picaza-Gorrochategui M., Idoiaga-Mondragon N. Stress, anxiety, and depression levels in the initial stage of the COVID-19 outbreak in a population sample in the northern Spain. Cadernos de Saúde Pública. 2020;36 doi: 10.1590/0102-311X00054020. [DOI] [PubMed] [Google Scholar]
- Preacher K.J., Hayes A.F. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40(3):879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Rachman S. Fear of contamination. Behaviour Research and Therapy. 2004;42(11):1227–1255. doi: 10.1016/j.brat.2003.10.009. [DOI] [PubMed] [Google Scholar]
- Robichaud M., Dugas M.J. 2006. A cognitive-behavioral treatment targeting intolerance of uncertainty. Worry and its psychological disorders: Theory, assessment and treatment. [Google Scholar]
- Ruscio A.M., Stein D.J., Chiu W.T., Kessler R.C. The epidemiology of obsessive-compulsive disorder in the national comorbidity survey replication. Molecular Psychiatry. 2010;15(1):53–63. doi: 10.1038/mp.2008.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salkovskis P.M., Rimes K.A., Warwick H.M.C., Clark D.M. The health anxiety inventory: Development and validation of scales for the measurement of health anxiety and hypochondriasis. Psychological Medicine. 2002;32(5):843–853. doi: 10.1017/s0033291702005822. [DOI] [PubMed] [Google Scholar]
- Sarawgi S., Oglesby M.E., Cougle J.R. Intolerance of uncertainty and obsessive-compulsive symptom expression. Journal of Behavior Therapy and Experimental Psychiatry. 2013;44(4):456–462. doi: 10.1016/j.jbtep.2013.06.001. [DOI] [PubMed] [Google Scholar]
- Scherr C.L., Jensen J.D., Christy K. Dispositional pandemic worry and the health belief model: Promoting vaccination during pandemic events. Journal of Public Health. 2017;39(4):e242–e250. doi: 10.1093/pubmed/fdw101. [DOI] [PubMed] [Google Scholar]
- Shigemura J., Ursano R.J., Morganstein J.C., Kurosawa M., Benedek D.M. Public responses to the novel 2019 coronavirus (2019‐nCoV) in Japan: Mental health consequences and target populations. Psychiatry and Clinical Neurosciences. 2020;74(4):281. doi: 10.1111/pcn.12988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrout P.E. Commentary: Mediation analysis, causal process, and cross-sectional data. Multivariate Behavioral Research. 2011;46(5):852–860. doi: 10.1080/00273171.2011.606718. [DOI] [PubMed] [Google Scholar]
- Taha S., Matheson K., Cronin T., Anisman H. Intolerance of uncertainty, appraisals, coping, and anxiety: The case of the 2009 H 1 N 1 pandemic. British Journal of Health Psychology. 2014;19(3):592–605. doi: 10.1111/bjhp.12058. [DOI] [PubMed] [Google Scholar]
- Taylor S., Asmundson . Guilford; New York: 2004. Treating health anxiety: A cognitive behavioral approach. [Google Scholar]
- Taylor S., Landry C., Paluszek M., Fergus T.A., McKay D., Asmundson G.J. Development and initial validation of the COVID stress scales. Journal of Anxiety Disorders. 2020:102232. doi: 10.1016/j.janxdis.2020.102232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor S., Landry C.A., Paluszek M.M., Fergus T.A., McKay D., Asmundson G.J. 2020. COVID stress syndrome: Concept, structure, and correlates. Depression and anxiety. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor S., McKay D., Abramowitz J.S. In: Handbook of evidence-based practice in clinical psychology,. II. Sturmey P., Herson M., editors. New York Wiley: Adult disorders); 2012. Hypochondriasis and health-related anxiety; pp. 603–619. [Google Scholar]
- Tolin D.F., Abramowitz J.S., Brigidi B.D., Foa E.B. Intolerance of uncertainty in obsessive-compulsive disorder. Journal of Anxiety Disorders. 2003;17(2):233–242. doi: 10.1016/s0887-6185(02)00182-2. [DOI] [PubMed] [Google Scholar]
- Twenge J.M., Joiner T.E. 2020. US Census Bureau‐assessed prevalence of anxiety and depressive symptoms in 2019 and during the 2020 COVID‐19 pandemic. Depression and anxiety. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. International Journal of Environmental Research and Public Health. 2020;17(5):1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wheaton M.G., Abramowitz J.S., Berman N.C., Fabricant L.E., Olatunji B.O. Psychological predictors of anxiety in response to the H1N1 (swine flu) pandemic. Cognitive Therapy and Research. 2012;36(3):210–218. [Google Scholar]
- Wheaton M.G., Abramowitz J.S., Berman N.C., Riemann B.C., Hale L.R. The relationship between obsessive beliefs and symptom dimensions in obsessive-compulsive disorder. Behaviour Research and Therapy. 2010;48(10):949–954. doi: 10.1016/j.brat.2010.05.027. [DOI] [PubMed] [Google Scholar]
- Wheaton M.G., Berman N.C., Franklin J.C., Abramowitz J.S. Health anxiety: Latent structure and associations with anxiety-related psychological processes in a student sample. Journal of Psychopathology and Behavioral Assessment. 2010;32(4):565–574. [Google Scholar]
- Wheaton M.G., Prikhidko A., Messner G.R. Frontiers in Psychology; 2020. Is fear of COVID-19 contagious? The effects of emotion contagion and social media use on anxiety in response to the coronavirus pandemic. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright K.D., Lebell M.A.A., Carleton R.N. Intolerance of uncertainty, anxiety sensitivity, health anxiety, and anxiety disorder symptoms in youth. Journal of Anxiety Disorders. 2016;41:35–42. doi: 10.1016/j.janxdis.2016.04.011. [DOI] [PubMed] [Google Scholar]