Abstract
Background and Objectives
Cognition is a known determinant of healthcare and financial decision making in old age. Social vulnerabilities also might play a role in such decisions; however, the evidence for this is less clear. Here, we examined the association of loneliness with decision making and tested the hypothesis that loneliness is associated with decision making via its interaction with global cognition.
Research Design and Methods
Participants were 1,121 nondemented older adults from the Rush Memory and Aging Project. Healthcare and financial decision making was assessed via a performance-based measure; loneliness was assessed via the De Jong Gierveld Loneliness Scale; and cognition was assessed via a 19-test neuropsychological battery.
Results
In a regression model adjusted for age, sex, and education, global cognition was associated with decision making (B = 2.43, SE = 0.14, p < .001) but loneliness was not (B = −0.04, SE = 0.11, p = .72). However, in a model including the interaction of loneliness with global cognition, the interaction was significant (B = 0.44, SE = 0.20, p = .03), such that the detrimental effect of loneliness on decision making was stronger when cognition was low. In secondary analyses examining the interaction of loneliness with 5 specific cognitive domains, the interaction between loneliness and working memory with decision making was significant (B = 0.35, SE = 0.15, p = .02).
Discussion and Implications
Our results suggest that loneliness compromises healthcare and financial decision making among older adults with lower global cognition and, more specifically, lower working memory.
Keywords: Dual-processing theory, Reserve, Social vulnerability, Working memory
Background and Objectives
Healthcare and financial decision making is fundamental to independent living but problematic for many older adults (Agarwal, Driscoll, Gabaix, & Laibson, 2009; Jacobson, Swoope, Perry, & Slosar, 2014). For example, in regard to Medicare Part D, a preponderance of older adults select prescription drug benefit plans that are inferior to other plans in terms of coverage and cost (Abaluck & Gruber, 2009; Zhou & Zhang, 2012). Similarly, with respect to financial investments, older adults often fail to choose assets that yield the best return at a given level of risk (Korniotis & Kumar, 2011). In turn, poor healthcare and financial decision making has been implicated in a variety of adverse outcomes among older adults, including overindebtedness, cost-related medication nonadherence, accelerated cognitive decline and incident Alzheimer’s dementia, and mortality (Boyle, Wilson, Yu, Buchman, & Bennett, 2013; Chung, Marottoli, Cooney, & Rhee, 2019; Lusardi & Tufano, 2009; Stewart, Yu, Wilson, Bennett, & Boyle, 2019).
While it is well established that cognition is a primary determinant of healthcare and financial decision making in old age (Boyle, Yu, Wilson, et al., 2012; Li, Baldassi, Johnson, & Weber, 2013; Li et al., 2015; Lusardi, 2012; Stewart, Yu, Wilson, Bennett, & Boyle, 2018), social factors also are posited to play an important role (Spreng, Karlawish, & Marson, 2016), although the evidence for this is less clear. Studies have associated loneliness and conceptually similar measures of social connectedness (e.g., lower perceived social support, lower social needs fulfillment) with aspects of financial decision making (e.g., financial exploitation, susceptibility to scams), but these associations have not always been observed or persisted after adjusting for covariates (Acierno et al., 2010; James, Boyle, & Bennett, 2014; Lichtenberg, Stickney, & Paulson, 2013; Liu, Wood, Xi, Berger, & Wilber, 2017). This might reflect methodological differences across studies (e.g., different social and decision making measures, different covariates) or modest associations of social connectedness with decision making among older adults in general. However, another possibility is that social connectedness is associated with decision making among some older adults more than others, depending on other relevant factors (Spreng et al., 2016). To the best of our knowledge, the only study to have examined this found that the relationship of lower perceived social support with financial exploitation was stronger among older adults with larger social networks (Beach, Schulz, & Sneed, 2018). Given the paucity of similar interaction analyses in the literature, the importance of social connectedness to decision making might go underappreciated, and opportunities to target social risk factors to bolster decision making among vulnerable older adults might be missed.
In the present study, we investigated whether the association of loneliness with healthcare and financial decision making interacts with cognition among 1,121 older adults without dementia from the Rush Memory and Aging Project (MAP; Bennett et al., 2018). We were interested in this interaction specifically because healthcare and financial decision making draws upon a diverse set of interconnected resources (Stewart et al., 2018), with cognition being a chief but declining resource in old age, even among older adults without overt cognitive impairment (Sperling et al., 2011). Additionally, evidence suggests that loneliness reduces the ability to leverage pertinent resources during decision making (i.e., reduces brain or cognitive reserve; Cacioppo, Capitanio, & Cacioppo, 2014; Wilson, Schneider, Arnold, Bienias, & Bennett, 2007) and biases decision making toward intuitive-based judgments (i.e., toward Type 1 processing in dual-processing theory; Baumeister, DeWall, Ciarocco, & Twenge, 2005; Cacioppo & Hawkley, 2009), both of which might detrimentally affect decision making when cognition is low. Thus, our central hypothesis was that loneliness is associated with decision making via its interaction with global cognition. We also were interested in exploring whether interactions of loneliness with cognition were general or specific and therefore conducted secondary analyses to determine whether loneliness is associated with decision making via its interaction with five specific cognitive domains (i.e., episodic memory, working memory, semantic memory, visuospatial ability, and perceptual speed). Although we did not have a firm hypothesis regarding the specific cognitive domains given the lack of prior work in this space, low working memory in particular has been linked to intuitive-based judgments (Evans & Stanovich, 2013); hence, the interaction between loneliness and working memory with decision making was of particular interest to us.
Research Design and Methods
Participants
MAP is an ongoing, longitudinal, clinical–pathological study of aging and age-related diseases (Bennett & Launer, 2012; Bennett et al., 2018). Participants are community-dwelling older adults who generally reside in northeastern Illinois. Recruitment primarily occurs in retirement communities but also takes place in Section 8 and Section 202 housing subsidized by the Department of Housing and Urban Development and local churches and other social service agencies serving minorities and low-income older adults. Participants are without known dementia upon study entry and agree to an annual assessment of risk factors, blood donation, and a detailed clinical evaluation. Participants also agree to the donation of the brain, spinal cord, and nerve and muscles at the time of death. Because the only exclusion criterion is the inability to consent to the Anatomical Gift Act, and because all clinical evaluations are performed as home visits, common comorbidities are well represented and follow-up rates are high (approximately 95%).
MAP began in 1997, and the decision-making assessment was added in 2010. Among the 2,102 participants who completed a MAP baseline evaluation, 642 died and 77 withdrew before the decision-making assessment was added. An additional 68 participants moved out of the area or were ineligible due to severe comprehension or sensory limitations; 37 declined the decision-making assessment; 87 had not yet been administered the decision-making assessment at the time of the current analyses; and 3 completed the decision-making assessment but had not yet received a clinical diagnosis. Of the remaining 1,188 participants, 66 were diagnosed with dementia and 1 had missing data. This left 1,121 nondemented participants available for the present analyses.
Informed consent was obtained from participants following an in-depth review of the risks and benefits of study participation. MAP and the decision-making substudy were approved by an Institutional Review Board of Rush University Medical Center.
Clinical Assessment and Diagnosis
Participants underwent annual structured clinical evaluations as part of their participation in MAP (Bennett et al., 2018). Alzheimer’s dementia was diagnosed according to the criteria of the National Institute of Neurologic and Communicative Disorders and Stroke and the Alzheimer’s Disease and Related Disorders Association. These criteria require a history of cognitive decline and impairment in memory and at least one other cognitive domain (McKhann et al., 1984). Participants in these analyses were without dementia at the time they underwent the assessments of decision making, loneliness, and cognition.
Assessment of Healthcare and Financial Decision Making
To assess healthcare and financial decision making, we used a modified version of a well-validated healthcare and financial decision making instrument (Finucane & Gullion, 2010; Finucane, Mertz, Slovic, & Schmidt, 2005; Stewart et al., 2018). Our adapted 12-item version was made up of a healthcare module and a financial module. Each module consisted of six items in total (three simple items and three complex items). Mimicking the types of healthcare and financial decisions older adults typically encounter, participants viewed tables displaying information about health maintenance organization (HMO) plans in the healthcare module or mutual funds in the financial module and then answered questions requiring comprehension and integration of the tabulated information. As an example, one of the simple healthcare items consisted of a table displaying five characteristics of three HMO plans (member satisfaction, preventative care strategies, access to specialists, customer service, and premium) and gave participants the following preferences: “You don’t want any HMO that is below average on member satisfaction OR below average on access to specialists. Based on the information in the table, which HMO should you choose?” One of the complex healthcare items displayed the same five characteristics for six additional HMO plans (i.e., nine plans in total) and gave participants the following preferences: “You don’t want any HMO that is below average on member satisfaction, customer service, or access to specialists, and you want an HMO that is above average on preventive care strategies. Based on the information in the table below, which HMO should you choose?” The financial module was structured similarly except that items pertained to tabulated information about the characteristics of mutual funds. The total number of healthcare and financial items answered correctly were tallied for each participant (range: 0–12, with higher scores indicating better decision making). The original decision-making measure has satisfactory short-term temporal stability, interrater reliability, and construct validity (Finucane & Gullion, 2010; Finucane et al., 2005). The current 12-item version has adequate internal consistency (Cronbach’s α = 0.75), and we have demonstrated its construct and predictive validity in prior work (i.e., it is correlated with important decision-making resources such as cognition, health and financial literacy, and risk aversion, and it is related to adverse health outcomes, including incident Alzheimer’s dementia and mortality; Boyle et al., 2013; Stewart et al., 2018, 2019).
Assessment of Loneliness
We measured loneliness via an adapted version of the De Jong Gierveld Loneliness Scale (De Jong Gierveld & Kamphuls, 1985). We made three changes to the original 11-item scale. First, because we were interested in emotional loneliness (i.e., a perceived lack of intimate relationships), we removed the five items pertaining to social loneliness (i.e., a perceived lack of a broader social network, such as friends and acquaintances). Second, to clarify item content, we combined two similar items into a single item, resulting in a five-item measure. Third, to improve sensitivity, participants rated their agreement with each item on a five-point scale rather than dichotomously. Participants’ responses to each of the five items were averaged (range: 1–5, with higher scores indicating greater loneliness). The original De Jong Gierveld Loneliness Scale is well validated (De Jong Gierveld & Kamphuls, 1985; De Jong Gierveld & Van Tilburg, 2010). The current version has satisfactory internal consistency (Cronbach’s α = 0.75) and is associated with adverse cognitive outcomes in old age (e.g., accelerated cognitive decline, incident Alzheimer’s dementia; Wilson et al., 2007).
Assessment of Cognition
Measures of global cognition and five specific cognitive domains were derived from participants’ performance on a 19-test neuropsychological battery (Bennett et al., 2018; Wilson et al., 2002). The five specific cognitive domains were as follows: (1) episodic memory (seven tests: Word List Memory, Recall, and Recognition from the CERAD neuropsychological battery; immediate and delayed recall of Logical Memory Story A and the East Boston Story), (2) working memory (three tests: Digit Span subtests [forward and backward] of the Wechsler Memory Scale—Revised and Digit Ordering), (3) semantic memory (three tests: Category Fluency, Boston Naming, and the National Adult Reading Test), (4) visuospatial ability (two tests: Judgment of Line Orientation and Standard Progressive Matrices), and (5) perceptual speed (four tests: the oral version of the Symbol Digit Modalities Test, Number Comparison, Stroop Color Naming, and Stroop Word Reading). Participants’ raw scores on individual tests were converted to z scores using the baseline mean and standard deviation of the full MAP cohort. Global cognition was calculated for each participant by averaging the z scores from all 19 tests and has good internal consistency (Cronbach’s α = 0.89). The five specific cognitive domains, which were conceptually and empirically derived, were calculated by averaging the z scores from the tests in each cognitive domain (Wilson et al., 2002).
Assessment of Covariates
Age was based on participants’ date of birth and the date that they underwent the assessment of decision making. Sex and education (years of schooling) were self-reported at participants’ initial study evaluation. Depressive symptoms were measured via a modified version of the 10-item Center for Epidemiological Studies Depression scale (Mohebbi et al., 2018). The only modification was that we removed the loneliness item (i.e., “I felt lonely”). The remaining nine items were read to participants, and participants were asked whether they experienced each symptom much of the time in the past week (range: 0–9, with higher scores indicating more depressive symptoms). Social network size was measured via standard questions that assess the number of children, family, and friends participants had seen at least once a month (Cornoni-Huntley, Brock, Ostfeld, Taylor, & Wallace, 1986). Chronic medical conditions were the total number of self-reported medical conditions, such as hypertension, diabetes, and cancer. Income was assessed by having participants choose from the following 10 categories: (1) $0–$4,999, (2) $5,000–$9,999, (3) $10,000–$14,999, (4) $15,000–$19,999, (5) $20,000–$24,999, (6) $25,000–$29,999, (7) $30,000–$34,999, (8) $35,000–$49,999, (9) $50,000–$74,999, and (10) >$75,000. We included depressive symptoms and social network size as covariates because they share similar conceptual (i.e., emotional and social) features with loneliness that need to be taken into account (Beller & Wagner, 2018; Courtin & Knapp, 2017; Wilson et al., 2007), and we included medical conditions and income as covariates because they have been associated with loneliness and/or might play a role in shaping healthcare and financial decisions (Cheung, Wright-St Clair, Chacko, & Barak, 2019; Emerson & Jayawardhana, 2016; James, Boyle, Bennett, & Bennett, 2012; Macdonald, Nixon, & Deacon, 2018).
Statistical Analysis
Bivariate associations of loneliness, cognition, and covariates with decision making were initially examined via Pearson correlations, Spearman correlations, or t tests, as appropriate. Next, in a series of multivariable linear regression models, we examined associations of loneliness, global cognition, and the interaction between loneliness and global cognition with decision making. Our initial model examined associations of loneliness and global cognition with decision making after adjusting for age, sex, and education. We then added a term for the interaction of loneliness with global cognition to the model. The interaction tested our central hypothesis that the association of loneliness with decision making depends on level of global cognition. To address potential confounding by other factors, we conducted four additional models that separately adjusted for depressive symptoms, social network size, medical conditions, and income. For each of these covariates, we adjusted for the covariate and the interaction of the covariate with global cognition. We adjusted for the latter because the relation of covariates with decision making might depend on global cognition, and we wanted to ensure that these interactions did not account for the interaction of loneliness with global cognition. In secondary analyses, we examined whether loneliness was associated with decision making via the five specific cognitive domains. To do this, we substituted global cognition with the cognitive domain under investigation and reran the above regression models (this was done separately for each of the five cognitive domains).
Results
The mean age of participants was 81.0 years (SD = 7.5, range: 58.8–100.8), and the mean score on the Mini-Mental State Examination was 28.3 (SD = 1.7, range: 17–30). Additional descriptive information is displayed in Table 1. In bivariate analyses, education, cognitive measures, social network size, and income were positively correlated with decision making, and age, loneliness, depressive symptoms, and medical conditions were negatively correlated with decision making (Table 1). Women scored lower on the decision-making measure than men (Mwomen = 7.7, SDwomen = 2.7; Mmen = 8.7, SDmen = 2.4, t = −5.0, p < .001).
Table 1.
Descriptive Characteristics of the Group and Bivariate Associations With Decision Making
| Characteristic | M (SD) or percent | r (p value) |
|---|---|---|
| Age | 81.0 (7.5) | −0.31 (<.001) |
| Female | 75.9% | −5.0 (<.001)b |
| Education | 15.6 (3.1) | 0.36 (<.001) |
| MMSE | 28.3 (1.7) | 0.40 (<.001) |
| Decision making | 8.0 (2.6) | — |
| Loneliness | 2.2 (0.6) | −0.18 (<.001) |
| Global cognition | 0.2 (0.5) | 0.57 (<.001) |
| Episodic memory | 0.3 (0.6) | 0.34 (<.001) |
| Working memory | 0.1 (0.7) | 0.36 (<.001) |
| Semantic memory | 0.2 (0.6) | 0.49 (<.001) |
| Visuospatial ability | 0.2 (0.8) | 0.45 (<.001) |
| Perceptual speed | 0.2 (0.8) | 0.55 (<.001) |
| Depressive symptoms | 0 (0–1)a | −0.10 (<.001)c |
| Social network size | 6 (3–9)a | 0.08 (.007)c |
| Medical conditions | 1.7 (1.1) | −0.14 (<.001) |
| Income | 7.5 (2.4) | 0.28 (<.001) |
Notes: Descriptive characteristics are mean (standard deviation) unless otherwise indicated. Correlation values are Pearson correlation coefficient (p value) unless otherwise indicated. MMSE = Mini-Mental State Examination.
aMedian (interquartile range).
b t value (p value).
cSpearman correlation coefficient (p value).
Decision Making as a Function of Loneliness, Cognition, and the Interaction of Loneliness With Cognition
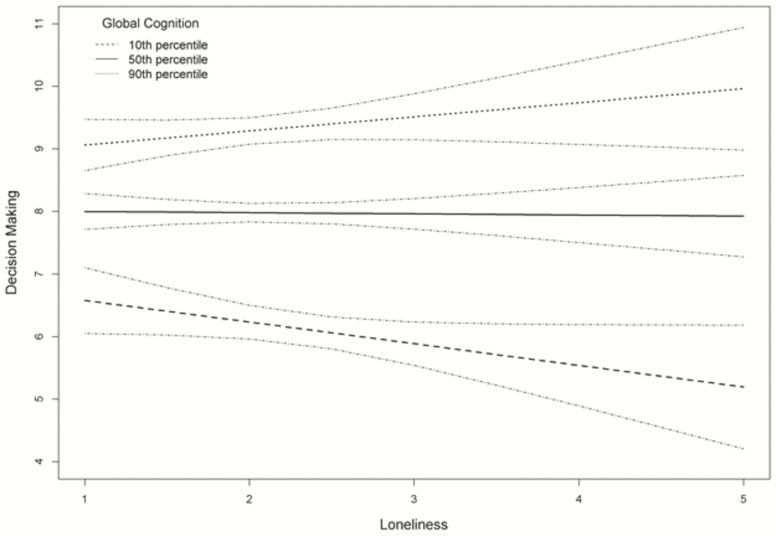
We initially examined associations of loneliness and global cognition with decision making in a linear regression model that adjusted for age, sex, and education. We found that lower global cognition was associated with poorer decision making (B = 2.43, SE = 0.14, p < .001). The regression coefficient for the relation of loneliness with decision making was negative but not significant (B = −0.04, SE = 0.11, p = .72). Next, to test our central hypothesis that the association of loneliness with decision making depends on the level of global cognition, we added a term for the interaction of loneliness with global cognition to the model. The interaction was significant (B = 0.44, SE = 0.20, p = .03; Table 2, Model A), such that the deleterious effect of loneliness on decision making was strongest among those with lower global cognition. To contextualize this interaction, for participants with average global cognition (50th percentile), a one-point increase in loneliness only corresponded to a 0.02-point reduction in decision making. By contrast, for participants with low global cognition (10th percentile), a one-point increase in loneliness corresponded to a 0.35-point reduction in decision making (Figure 1). This interaction persisted in separate models that additionally adjusted for depressive symptoms, social network size, medical conditions, and income (Table 2; for full regression results, please see Supplementary Table S1).
Table 2.
Associations of Decision Making With Loneliness, Global Cognition, and the Interaction of Loneliness With Global Cognition
| Model | Model term | Unstandardized B (SE) | p |
|---|---|---|---|
| A | Loneliness | −0.14 (0.12) | .25 |
| Global cognition | 2.33 (0.15) | <.001 | |
| Loneliness × global cognition | 0.44 (0.20) | .03 | |
| B | Loneliness | −0.12 (0.13) | .34 |
| Global cognition | 2.39 (0.16) | <.001 | |
| Loneliness × global cognition | 0.50 (0.22) | .03 | |
| C | Loneliness | −0.12 (0.12) | .33 |
| Global cognition | 2.33 (0.15) | <.001 | |
| Loneliness × global cognition | 0.44 (0.21) | .03 | |
| D | Loneliness | −0.12 (0.12) | .30 |
| Global cognition | 2.07 (0.22) | <.001 | |
| Loneliness × global cognition | 0.42 (0.20) | .04 | |
| E | Loneliness | −0.11 (0.12) | .38 |
| Global cognition | 2.22 (0.15) | <.001 | |
| Loneliness × global cognition | 0.41 (0.21) | .05 |
Notes: Model A adjusted for age, sex, and education (core model). Model B additionally adjusted for depressive symptoms and the interaction of depressive symptoms with global cognition. Model C additionally adjusted for social network size and the interaction of social network size with global cognition. Model D additionally adjusted for medical conditions and the interaction of medical conditions with global cognition. Model E additionally adjusted for income and the interaction of income with global cognition. SE = standard error.
Figure 1.
Association of loneliness with decision making at the 10th, 50th, and 90th percentiles of global cognition, with 95% confidence bands, adjusted for age, sex, and education.
In secondary analyses examining the interaction of loneliness with the five specific cognitive domains, the only significant interaction was between loneliness and working memory with decision making (B = 0.35, SE = 0.15, p = .02). Specifically, the relation of loneliness with poorer decision making was more robust when working memory was low. This interaction persisted in separate models that additionally adjusted for depressive symptoms (B = 0.42, SE = 0.16, p = .01), social network size (B = 0.39, SE = 0.16, p = .01), medical conditions (B = 0.36, SE = 0.15, p = .02), and income (B = 0.36, SE = 0.16, p = .02; for full regression results, please see Supplementary Table S2).
Discussion and Implications
The central hypothesis of this study was that loneliness is associated with healthcare and financial decision making via its interaction with global cognition. Our results were supportive. In a linear regression model adjusted for age, sex, and education, global cognition was associated with decision making but loneliness was not. Critically, however, the interaction between loneliness and global cognition with decision making was significant, such that the detrimental effect of loneliness on decision making was strongest among those with lower global cognition. This interaction persisted after further adjusting for depressive symptoms, social network size, medical conditions, and income. Secondary analyses examining the five specific cognitive domains revealed an interaction between loneliness and working memory with decision making. These findings suggest that loneliness compromises decision making among older adults with lower global cognition and, more specifically, lower working memory. They also raise possible mechanisms linking loneliness to complex decision making and have implications pertaining to how loneliness might be incorporated into interventions aiming to bolster healthcare and financial decision making.
While it has been theorized that social connectedness interplays with other relevant factors to affect healthcare and financial decision making in old age (Spreng et al., 2016), we are only aware of one study examining this issue. Beach and colleagues (2018) reported that the relationship of lower perceived social support with financial exploitation was stronger among older adults with larger social networks. This finding supports a “quality not quantity” maxim regarding social connections and decision making, and the current interaction of loneliness with cognition, which persisted beyond social network size, further underscores the importance of quality social connections (or lack thereof) to decision making. More broadly, the present study justifies additional study of interactions between cognition and other social or contextual factors with healthcare and financial decision making. We suspect that such interactions exist because cognition is central to decision making but declines even among older adults without significant cognitive impairment (Sperling et al., 2011). Thus, as cognition diminishes, other resources or vulnerabilities might move toward the forefront of decision making. Conversely, social connectedness might play a lesser role among older adults whose decision making is dominated by strong cognitive abilities. If borne out, this would help explain why associations of social connectedness with decision making tend to be modest among older adults in general (Acierno et al., 2010; James et al., 2014; Lichtenberg et al., 2013; Liu et al., 2017).
Although this study does not elucidate the mechanism or mechanisms underlying the interaction between loneliness and cognition with decision making, a couple of possibilities warrant discussion. One is that lonely older adults have less social capital available, and this detrimentally affects decision making among those with lower cognition. While possible, one issue with this explanation is that we used a performance-based measure of healthcare and financial decision making, whereas most prior studies examined self-reported financial exploitation. Performance-based measures have several advantages (e.g., they provide highly granular information and avoid underreporting of poor decisions due to stigma; Ghesquiere, McAfee, & Burnett, 2019; Lichtenberg, Campbell, Hall, & Gross, 2020; Marson, 2015), but they do not reflect individuals’ social milieu in the way that self-reported financial exploitation does (DeLiema, 2018; DeLiema, Yon, & Wilber, 2016). Thus, whereas it makes intuitive sense that loneliness and low social capital would increase the risk of financial exploitation, it is not entirely clear how these factors would directly influence performance on the current decision-making measure.
A second possible explanation is that loneliness decreases older adults’ capacity to leverage compensatory resources in the face of accumulating age-related neuropathologies and cognitive loss. Such compensation is likely critical in aging because healthcare and financial decision making draws upon varied resources in addition to cognition, particularly domain-specific health and financial literacy and numeracy (Boyle, Yu, Buchman, & Bennett, 2012; Chin et al., 2017; Li et al., 2013; Lichtenberg et al., 2020; Stewart et al., 2018), and these other resources might be enlisted to offset the detrimental effect of age-related cognitive decline on decision making. This notion is akin to brain or cognitive reserve (Stern, 2017), except here reserve is in reference to decision making. Notably, animal studies have associated social isolation with neurobiological changes that might lessen brain reserve (e.g., reduced neurogenesis and brain-derived neurotrophic factor in the hippocampus; Cacioppo et al., 2014). Also, we previously associated loneliness with adverse cognitive outcomes in old age but not Alzheimer’s disease pathology or cerebral infarctions, suggesting that loneliness depletes cognitive reserve (Wilson et al., 2007). The current findings align with this literature because reduced reserve due to loneliness should detrimentally affect decision making when compensatory processes are needed, namely, when cognition is low.
Another, complimentary explanation of the current findings is that loneliness skews information processing in a manner that is ill-fitted for healthcare and financial decision making. This idea stems from dual-processing theory, which posits a rapid mode of decision making that supports intuitive-based judgments (Type 1 processing) and an analytic mode of decision making specifically linked to working memory (Type 2 processing; Evans & Stanovich, 2013; Sanfey & Chang, 2008). While analytic Type 2 processing is likely a much better fit for complex healthcare and financial decision making, loneliness has been shown to decrease self-regulation and increase prepotent responding (Baumeister et al., 2005; Cacioppo et al., 2000) and thus should skew decision making toward intuitive-based Type 1 processing (Cacioppo & Hawkley, 2009). The present findings may suggest that this skewing is detrimental to complex decision making when cognition is low. That is, lonely older adults with weaker cognitive abilities—weaker working memory in particular—might be especially reliant on intuitive-based Type 1 processing, which is maladaptive to healthcare and financial decision making.
Regarding policy and program intervention, this study raises some interesting avenues worth consideration. One is that an assessment of loneliness could be used to stratify risk of poor decision making among older adults who are already vulnerable due to low cognition. This information could then be used to prioritize the deployment of interventions to those most in need. Our findings also could be used to determine when loneliness, a modifiable factor, should be a focus of decision-making interventions. If cognition is high, then a loneliness intervention would not be indicated from a decision-making perspective even if the individual is lonely. On the contrary, if cognition is low and loneliness is high, then a loneliness intervention would be indicated. Interestingly, cognitive-behavioral interventions are particularly efficacious in reducing loneliness (Masi, Chen, Hawkley, & Cacioppo, 2011). These interventions teach individuals to identify and challenge maladaptive automatic thoughts about social situations through an objective analysis of the situation. In dual-processing parlance, this means learning to supplant intuitive-based Type 1 processing with analytic-based Type 2 processing. Given the potential importance of this shift in processing, cognitive-behavioral interventions for loneliness might be especially well suited to bolster healthcare and financial decision making.
This study has strengths and limitations. Its strengths include a large group of well-characterized, community-dwelling older adults and the use of established measures of loneliness, cognition, and healthcare and financial decision making. We also adjusted for depressive symptoms, social network size, medical conditions, and income, which increases confidence in our findings. A limitation is that our group of participants was fairly homogenous in terms of race and education (93% of participants were non-Hispanic White; years of schooling: M = 15.6, SD = 3.1). We are collecting decision-making data among more diverse groups of older adults and will investigate generalization of the current results in future work. Another limitation is that the present analyses are cross-sectional and do not establish the causal effects of loneliness and cognition on decision making. Longitudinal data collection in MAP is ongoing, and once sufficient data have amassed, we will examine whether the interaction of loneliness with low cognition is associated with subsequent decline in decision making. Additional work also is needed to determine whether other specific cognitive abilities, particularly reasoning and problem solving—which are often subsumed with working memory under executive functioning—interact with loneliness in relation to decision making.
Other research questions stimulated by the current work pertain to the intersection of loneliness with brain/cognitive reserve and dual-processing theory. For example, if loneliness hinders the recruitment of compensatory processes and/or skews decision making toward rapid, intuitive-based Type 1 processing, then lonely older adults with weaker cognitive abilities should not only make worse healthcare and financial decisions (as demonstrated here), they also might make these decisions impulsively (i.e., quickly). Similarly, healthcare and financial decision making among lonely older adults with weaker cognitive abilities should be less reliant on brain systems implicated in compensatory processes (e.g., working memory networks involving the dorsolateral prefrontal cortex) and more reliant on brain systems implicated in Type 1 processing (e.g., reward circuits involving the ventral striatum; Cacioppo, Norris, Decety, Monteleone, & Nusbaum, 2009; Cacioppo et al., 2014; Powers, Wagner, Norris, & Heatherton, 2013; Sanfey & Chang, 2008). We already collect response time on our decision-making measure and have neuroimaging for many participants and thus can examine these hypotheses in future research. This work has the potential to clarify why loneliness interacts with cognition to affect healthcare and financial decision making and further inform the design of interventions that support decision making in the face of age-related cognitive decline.
Funding
This work was supported by the National Institute on Aging (R01 AG017917 to D. A. Bennett and R01 AG033678, R01 AG034374, and R01 AG060376 to P. A. Boyle).
Conflict of Interest
None reported.
Supplementary Material
Acknowledgments
This study could not be conducted without the dedication of the thousands of participants in the Rush Memory and Aging Project (MAP) and the staff of the Rush Alzheimer’s Disease Center (RADC). We extend our heartfelt thanks to them. Please visit the RADC’s Research Resource Sharing Hub to request data from MAP for research purposes, including with respect to the current analyses (www.radc.rush.edu).
References
- Abaluck J T, & Gruber J (2009). Choice inconsistencies among the elderly: Evidence from plan choice in the Medicare Part D program. American Economic Review, 101(4), 1180–1210. doi: 10.1257/aer.101.4.1180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Acierno R, Hernandez M A, Amstadter A B, Resnick H S, Steve K, Muzzy W, & Kilpatrick D G (2010). Prevalence and correlates of emotional, physical, sexual, and financial abuse and potential neglect in the United States: The National Elder Mistreatment Study. American Journal of Public Health, 100(2), 292–297. doi: 10.2105/AJPH.2009.163089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agarwal S, Driscoll J C, Gabaix X, & Laibson D (2009). The age of reason: Financial decisions over the life cycle and implications for regulation. Brookings Papers on Economic Activity, 2009 (Fall 2009), 51–101. doi: 10.1353/eca.0.0067 [DOI] [Google Scholar]
- Baumeister R F, DeWall C N, Ciarocco N J, & Twenge J M (2005). Social exclusion impairs self-regulation. Journal of Personality and Social Psychology, 88(4), 589–604. doi: 10.1037/0022-3514.88.4.589 [DOI] [PubMed] [Google Scholar]
- Beach S R, Schulz R, & Sneed R (2018). Associations between social support, social networks, and financial exploitation in older adults. Journal of Applied Gerontology, 37(8), 990–1011. doi: 10.1177/0733464816642584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beller J, & Wagner A (2018). Disentangling loneliness: Differential effects of subjective loneliness, network quality, network size, and living alone on physical, mental, and cognitive health. Journal of Aging and Health, 30(4), 521–539. doi: 10.1177/0898264316685843 [DOI] [PubMed] [Google Scholar]
- Bennett D A, Buchman A S, Boyle P A, Barnes L L, Wilson R S, & Schneider J A (2018). Religious orders study and rush memory and aging project. Journal of Alzheimer’s disease, 64(s1), S161–S189. doi: 10.3233/JAD-179939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett D A, & Launer L J (2012). Longitudinal epidemiologic clinical–pathologic studies of aging and Alzheimer’s disease. Current Alzheimer Research, 9(6), 617–620. doi: 10.2174/156720512801322645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyle P A, Wilson R S, Yu L, Buchman A S, & Bennett D A (2013). Poor decision making is associated with an increased risk of mortality among community-dwelling older persons without dementia. Neuroepidemiology, 40(4), 247–252. doi: 10.1159/000342781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyle P A, Yu L, Buchman A S, & Bennett D A (2012). Risk aversion is associated with decision making among community-based older persons. Frontiers in Psychology, 3, 205. doi: 10.3389/fpsyg.2012.00205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyle P A, Yu L, Wilson R S, Gamble K, Buchman A S, & Bennett D A (2012). Poor decision making is a consequence of cognitive decline among older persons without Alzheimer’s disease or mild cognitive impairment. PLoS One, 7(8), e43647. doi: 10.1371/journal.pone.0043647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo J T, Ernst J M, Burleson M H, McClintock M K, Malarkey W B, Hawkley L C,...Berntson G G (2000). Lonely traits and concomitant physiological processes: The MacArthur social neuroscience studies. International Journal of Psychophysiology, 35(2–3), 143–154. doi: 10.1016/s0167-8760(99)00049-5 [DOI] [PubMed] [Google Scholar]
- Cacioppo J T, & Hawkley L C (2009). Perceived social isolation and cognition. Trends in Cognitive Sciences, 13(10), 447–454. doi: 10.1016/j.tics.2009.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo J T, Norris C J, Decety J, Monteleone G, & Nusbaum H (2009). In the eye of the beholder: Individual differences in perceived social isolation predict regional brain activation to social stimuli. Journal of Cognitive Neuroscience, 21(1), 83–92. doi: 10.1162/jocn.2009.21007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo S, Capitanio J P, & Cacioppo J T (2014). Toward a neurology of loneliness. Psychological Bulletin, 140(6), 1464–1504. doi: 10.1037/a0037618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheung G, Wright-St Clair V, Chacko E, & Barak Y (2019). Financial difficulty and biopsychosocial predictors of loneliness: A cross-sectional study of community dwelling older adults. Archives of Gerontology and Geriatrics, 85, 103935. doi: 10.1016/j.archger.2019.103935 [DOI] [PubMed] [Google Scholar]
- Chin J, Madison A, Gao X, Graumlich J F, Conner-Garcia T, Murray M D, . . . Morrow D G (2017). Cognition and health literacy in older adults’ recall of self-care information. The Gerontologist, 57(2), 261–268. doi: 10.1093/geront/gnv091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung G C, Marottoli R A, Cooney L M Jr, & Rhee T G (2019). Cost-related medication nonadherence among older adults: Findings from a nationally representative sample. Journal of the American Geriatrics Society, 67(12), 2463–2473. doi: 10.1111/jgs.16141 [DOI] [PubMed] [Google Scholar]
- Cornoni-Huntley J, Brock D B, Ostfeld A M, Taylor J O, & Wallace R B (1986). Established populations for epidemiologic studies of the elderly resource data book. U.S. Department of Health and Human Services. [Google Scholar]
- Courtin E, & Knapp M (2017). Social isolation, loneliness and health in old age: A scoping review. Health & Social Care in the Community, 25(3), 799–812. doi: 10.1111/hsc.12311 [DOI] [PubMed] [Google Scholar]
- De Jong Gierveld J, & Kamphuls F (1985). The development of a Rasch-type loneliness scale. Applied Psychological Measurement, 9(3), 289–299. doi: 10.1177/014662168500900307 [DOI] [Google Scholar]
- De Jong Gierveld J, & Van Tilburg T (2010). The De Jong Gierveld short scales for emotional and social loneliness: Tested on data from 7 countries in the UN generations and gender surveys. European Journal of Ageing, 7(2), 121–130. doi: 10.1007/s10433-010-0144-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeLiema M. (2018). Elder fraud and financial exploitation: Application of routine activity theory. The Gerontologist, 58(4), 706–718. doi: 10.1093/geront/gnw258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeLiema M, Yon Y, & Wilber K H (2016). Tricks of the trade: Motivating sales agents to con older adults. The Gerontologist, 56(2), 335–344. doi: 10.1093/geront/gnu039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emerson K G, & Jayawardhana J (2016). Risk factors for loneliness in elderly adults. Journal of the American Geriatrics Society, 64(4), 886–887. doi: 10.1111/jgs.14053 [DOI] [PubMed] [Google Scholar]
- Evans J S, & Stanovich K E (2013). Dual-process theories of higher cognition: Advancing the debate. Perspectives on Psychological Science, 8(3), 223–241. doi: 10.1177/1745691612460685 [DOI] [PubMed] [Google Scholar]
- Finucane M L, & Gullion C M (2010). Developing a tool for measuring the decision-making competence of older adults. Psychology and Aging, 25(2), 271–288. doi: 10.1037/a0019106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finucane M L, Mertz C K, Slovic P, & Schmidt E S (2005). Task complexity and older adults’ decision-making competence. Psychology and Aging, 20(1), 71–84. doi: 10.1037/0882-7974.20.1.71 [DOI] [PubMed] [Google Scholar]
- Ghesquiere A R, McAfee C, & Burnett J (2019). Measures of financial capacity: A review. The Gerontologist, 59(2), e109–e129. doi: 10.1093/geront/gnx045 [DOI] [PubMed] [Google Scholar]
- Jacobson G, Swoope C, Perry M, & Slosar M C (2014). How are seniors choosing and changing health insurance plans? Findings from focus groups with Medicare beneficiaries . Kaiser Family Foundation; https://www.kff.org/medicare/report/how-are-seniors-choosing-and-changing-health-insurance-plans/ [Google Scholar]
- James B D, Boyle P A, & Bennett D A (2014). Correlates of susceptibility to scams in older adults without dementia. Journal of Elder Abuse & Neglect, 26(2), 107–122. doi: 10.1080/08946566.2013.821809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- James B D, Boyle P A, Bennett J S, & Bennett D A (2012). The impact of health and financial literacy on decision making in community-based older adults. Gerontology, 58(6), 531–539. doi: 10.1159/000339094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korniotis G M, & Kumar A (2011). Do older investors make better investment decisions? Review of Economics and Statistics, 93(1), 244–265. doi: 10.1162/REST_a_00053 [DOI] [Google Scholar]
- Li Y, Baldassi M, Johnson E J, & Weber E U (2013). Complementary cognitive capabilities, economic decision making, and aging. Psychology and Aging, 28(3), 595–613. doi: 10.1037/a0034172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y, Gao J, Enkavi A Z, Zaval L, Weber E U, & Johnson E J (2015). Sound credit scores and financial decisions despite cognitive aging. Proceedings of the National Academy of Sciences of the United States of America, 112(1), 65–69. doi: 10.1073/pnas.1413570112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lichtenberg P A, Campbell R, Hall L, & Gross E Z (2020). Context matters: Financial, psychological, and relationship insecurity around personal finance is associated with financial exploitation. The Gerontologist. Advance online publication. doi: 10.1093/geront/gnaa020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lichtenberg P A, Stickney L, & Paulson D (2013). Is psychological vulnerability related to the experience of fraud in older adults? Clinical Gerontologist, 36(2), 132–146. doi: 10.1080/07317115.2012.749323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu P J, Wood S, Xi P, Berger D E, & Wilber K (2017). The role of social support in elder financial exploitation using a community sample. Innovation in Aging, 1(1), igx016. doi: 10.1093/geroni/igx016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lusardi A. (2012). Numeracy, financial literacy, and financial decision-making. National Bureau of Economic Research, Article Working Paper 17821. doi: 10.3386/w17821 [DOI] [Google Scholar]
- Lusardi A, & Tufano P (2009). Debt literacy, financial experiences, and overindebtedness. National Bureau of Economic Research, Article Working Paper 14808. doi: 10.3386/w14808 [DOI] [Google Scholar]
- Macdonald S J, Nixon J, & Deacon L (2018). ‘Loneliness in the city’: Examining socio-economics, loneliness and poor health in the North East of England. Public Health, 165, 88–94. doi: 10.1016/j.puhe.2018.09.003 [DOI] [PubMed] [Google Scholar]
- Marson D. (2015). Investigating functional impairment in preclinical Alzheimer’s disease. The Journal of Prevention of Alzheimer’s Disease, 2(1), 4–6. doi: 10.14283/jpad.2015.44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masi C M, Chen H Y, Hawkley L C, & Cacioppo J T (2011). A meta-analysis of interventions to reduce loneliness. Personality and Social Psychology Review, 15(3), 219–266. doi: 10.1177/1088868310377394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKhann G, Drachman D, Folstein M, Katzman R, Price D, & Stadlan E M (1984). Clinical diagnosis of Alzheimer’s disease: Report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer’s Disease. Neurology, 34(7), 939–944. doi: 10.1212/wnl.34.7.939 [DOI] [PubMed] [Google Scholar]
- Mohebbi M, Nguyen V, McNeil J J, Woods R L, Nelson M R, Shah R C,...Berk M; ASPREE Investigator Group (2018). Psychometric properties of a short form of the Center for Epidemiologic Studies Depression (CES-D-10) scale for screening depressive symptoms in healthy community dwelling older adults. General Hospital Psychiatry, 51, 118–125. doi: 10.1016/j.genhosppsych.2017.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powers K E, Wagner D D, Norris C J, & Heatherton T F (2013). Socially excluded individuals fail to recruit medial prefrontal cortex for negative social scenes. Social Cognitive and Affective Neuroscience, 8(2), 151–157. doi: 10.1093/scan/nsr079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanfey A G, & Chang L J (2008). Multiple systems in decision making. Annals of the New York Academy of Sciences, 1128, 53–62. doi: 10.1196/annals.1399.007 [DOI] [PubMed] [Google Scholar]
- Sperling R A, Aisen P S, Beckett L A, Bennett D A, Craft S, Fagan A M, . . . Phelps C H (2011). Toward defining the preclinical stages of Alzheimer’s disease: Recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimer’s & Dementia, 7(3), 280–292. doi: 10.1016/j.jalz.2011.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spreng R N P, Karlawish J M, & Marson D C M (2016). Cognitive, social, and neural determinants of diminished decision-making and financial exploitation risk in aging and dementia: A review and new model. Journal of Elder Abuse & Neglect, 28(4–5), 320–344. doi: 10.1080/08946566.2016.1237918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stern Y. (2017). An approach to studying the neural correlates of reserve. Brain Imaging and Behavior, 11(2), 410–416. doi: 10.1007/s11682-016-9566-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart C C, Yu L, Wilson R S, Bennett D A, & Boyle P A (2018). Correlates of healthcare and financial decision making among older adults without dementia. Health Psychology, 37(7), 618–626. doi: 10.1037/hea0000610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart C C, Yu L, Wilson R S, Bennett D A, & Boyle P A (2019). Healthcare and financial decision making and incident adverse cognitive outcomes among older adults. Journal of the American Geriatrics Society, 67(8), 1590–1595. doi: 10.1111/jgs.15880 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson R S, Beckett L A, Barnes L L, Schneider J A, Bach J, Evans D A, & Bennett D A (2002). Individual differences in rates of change in cognitive abilities of older persons. Psychology and Aging, 17(2), 179–193. doi: 10.1037/0882-7974.17.2.179 [DOI] [PubMed] [Google Scholar]
- Wilson R S, Schneider J A, Arnold S E, Bienias J L, & Bennett D A (2007). Conscientiousness and the incidence of Alzheimer disease and mild cognitive impairment. Archives of General Psychiatry, 64(10), 1204–1212. doi: 10.1001/archpsyc.64.10.1204 [DOI] [PubMed] [Google Scholar]
- Zhou C, & Zhang Y (2012). The vast majority of Medicare Part D beneficiaries still don’t choose the cheapest plans that meet their medication needs. Health Affairs (Project Hope), 31(10), 2259–2265. doi: 10.1377/hlthaff.2012.0087 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.