Abstract
Background
There is limited prospective evidence on possible differences in fracture risks between vegetarians, vegans, and non-vegetarians. We aimed to study this in a prospective cohort with a large proportion of non-meat eaters.
Methods
In EPIC-Oxford, dietary information was collected at baseline (1993–2001) and at follow-up (≈ 2010). Participants were categorised into four diet groups at both time points (with 29,380 meat eaters, 8037 fish eaters, 15,499 vegetarians, and 1982 vegans at baseline in analyses of total fractures). Outcomes were identified through linkage to hospital records or death certificates until mid-2016. Using multivariable Cox regression, we estimated the risks of total (n = 3941) and site-specific fractures (arm, n = 566; wrist, n = 889; hip, n = 945; leg, n = 366; ankle, n = 520; other main sites, i.e. clavicle, rib, and vertebra, n = 467) by diet group over an average of 17.6 years of follow-up.
Results
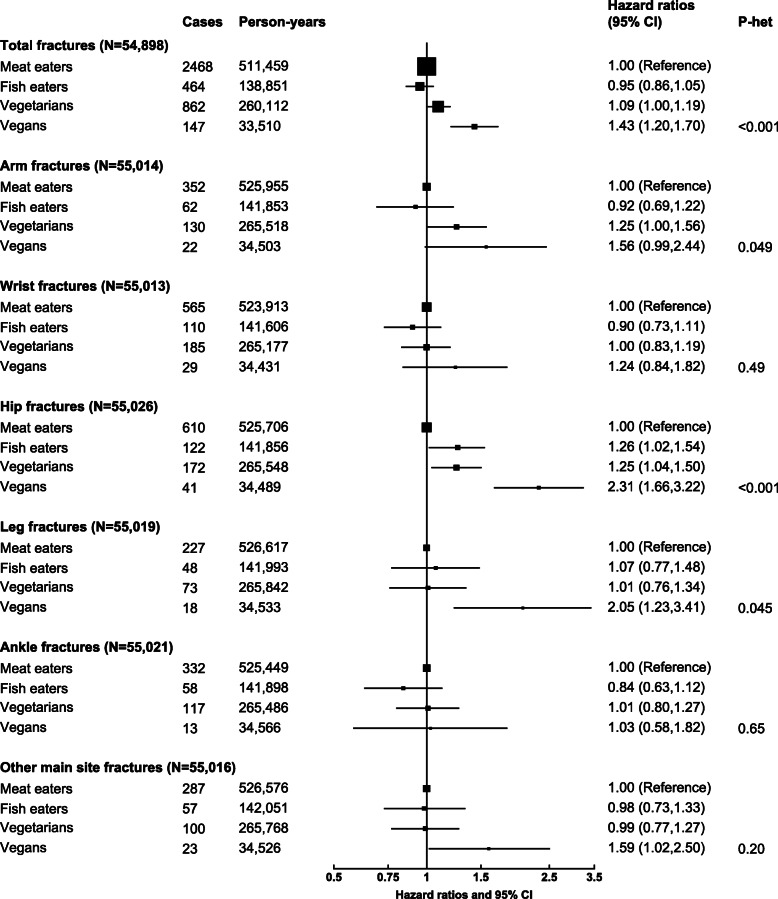
Compared with meat eaters and after adjustment for socio-economic factors, lifestyle confounders, and body mass index (BMI), the risks of hip fracture were higher in fish eaters (hazard ratio 1.26; 95% CI 1.02–1.54), vegetarians (1.25; 1.04–1.50), and vegans (2.31; 1.66–3.22), equivalent to rate differences of 2.9 (0.6–5.7), 2.9 (0.9–5.2), and 14.9 (7.9–24.5) more cases for every 1000 people over 10 years, respectively. The vegans also had higher risks of total (1.43; 1.20–1.70), leg (2.05; 1.23–3.41), and other main site fractures (1.59; 1.02–2.50) than meat eaters. Overall, the significant associations appeared to be stronger without adjustment for BMI and were slightly attenuated but remained significant with additional adjustment for dietary calcium and/or total protein. No significant differences were observed in risks of wrist or ankle fractures by diet group with or without BMI adjustment, nor for arm fractures after BMI adjustment.
Conclusions
Non-meat eaters, especially vegans, had higher risks of either total or some site-specific fractures, particularly hip fractures. This is the first prospective study of diet group with both total and multiple specific fracture sites in vegetarians and vegans, and the findings suggest that bone health in vegans requires further research.
Keywords: Vegetarian diets, Vegan diets, Fractures, Bone health, Calcium, Protein, Body mass index, Prospective study
Background
Fractures in adulthood and older ages are a common occurrence which pose a significant burden to health systems worldwide [1]. Previous epidemiological studies have shown that vegetarians had lower bone mineral density (BMD) than non-vegetarians [2, 3], but the associations of vegetarian diets with fracture risks are unclear. Potential risk differences are plausible however, owing to differences in several dietary factors, such as the substantially lower intakes of calcium in vegans [4, 5], lower intakes of dietary protein in both vegetarians and vegans [6, 7], and the lower body mass index (BMI) of non-meat eaters [2, 8].
Prior studies have linked both calcium and protein intakes to bone health, but their relationships with fracture risks are nuanced. For calcium, although previous meta-analyses have found that calcium supplements are effective in producing small increases in BMD [9], it is less clear whether this degree of improvement would be sufficient to reduce fracture risks [10]. However, a recent meta-analysis of randomised trials showed that combined vitamin D and calcium supplementation, but not vitamin D supplementation alone, was effective in fracture prevention, therefore supporting the importance of calcium [11]. For protein, while older studies suggested that high protein intake might lead to higher calcium excretion and therefore weaker bones [12], more recent evidence has suggested a positive association between protein and bone health, although this might not translate to differences in fracture risk [13]. In addition, BMI is also an important factor for fracture risk [14], and a recent study suggested that the lower BMD observed in US vegetarians might be largely explained by their lower BMI and waist circumference [15]. However, the directions of association between BMI and fracture risk differ across fracture sites, and low BMI has been associated with a higher risk of hip fracture but lower risk of ankle fracture [14].
The largest study to date on vegetarian diet group and fracture risks came from previous analyses in EPIC-Oxford on around 30,000 participants, and reported that vegans, but not vegetarians, had higher risks of total fractures, although this analysis had a short follow-up (5 years) and relied on self-reported outcome data [16]. The only two other studies on the topic included a small number of participants and did not report on site-specific fractures [17, 18]. Hence, the possible differences in fracture risks by vegetarian diet groups are still unclear, and it is not known whether the risks might differ by fracture sites.
Therefore, the aim of this study was to examine the risks of total and site-specific fractures in a prospective cohort with close to 18 years of average follow-up, including a large proportion of non-meat eaters, and with outcome data based on record linkage.
Methods
Study population
EPIC-Oxford is a prospective cohort study which recruited approximately 65,000 men and women across the UK between 1993 and 2001, via either general practices or by postal questionnaire. Details of the recruitment process and eligibility criteria for inclusion in the analyses can be found in Additional File 1: Supplementary methods [4, 19] and in the participant flow chart (Additional File 1: Fig. S1). The study has approval by a Multicentre Research Ethics Committee (Scotland A Research Ethics Committee). All participants provided written informed consent.
Classification of diet group
At recruitment, participants completed a questionnaire which asked about diet, socio-demographic characteristics, lifestyle, and medical history. A follow-up questionnaire which asked similar questions was sent to participants in 2010. Based on the responses to both questionnaires (if the participant completed the follow-up questionnaire), the participants were categorised into meat eaters, fish eaters (did not eat meat but ate fish), vegetarians (did not eat meat or fish, but ate one or both of dairy or eggs), and vegans (participants who did not eat meat, fish, dairy, and eggs) at both time points. Further details on the questionnaires, classification of diet group including agreement of diet group at baseline and follow-up, and data collection of other baseline characteristics can be found in Additional File 1: Supplementary methods [20–27].
Outcome assessment
Participants were followed up for health outcomes via record linkage to National Health Service records until 31 March 2016 in England, 31 May 2016 in Wales, and 31 October 2016 in Scotland. The outcomes of interest were the first recorded hospital admission (inpatient admissions in England, inpatient admissions and day cases in Wales and Scotland) or death from total and site-specific fractures, including fractures of the arm (i.e. humerus, radius, and ulna), wrist, hip, leg (i.e. femur [excluding neck of femur], patella, tibia, and fibula), ankle, and other main sites (i.e. clavicle, rib, or vertebra), identified by the relevant 9th or 10th revisions of the World Health Organization’s International Classification of Diseases (ICD-9/ICD-10) codes (Additional File 1: Table S1). For total fractures, incidence was defined as the first recorded occurrence of any diagnosis of any fracture; for site-specific fractures, incidence was defined as the first recorded occurrence of any fracture at that particular site, without censoring for previous fractures at other sites. Fractures at the clavicle, rib, and vertebra were examined as one composite outcome due to the small number of cases at these sites, but the three sites were examined separately in secondary analyses.
Statistical analyses
Baseline characteristics and food and nutrient intakes of the EPIC-Oxford participants were summarised by diet group. Cox proportional hazards regression models were used to estimate the hazard ratios (HRs) and 95% confidence intervals (CIs) for the associations between the four diet groups (meat eaters, fish eaters, vegetarians, vegans) and total and each site-specific fracture of interest, using meat eaters as the reference group. The underlying time variable was the age at recruitment to the age at diagnosis, death, or administrative censoring, whichever occurred first. For participants who completed both the baseline and follow-up questionnaires, diet group and relevant time-varying covariates (smoking and alcohol consumption, BMI, dietary calcium or protein) were updated at follow-up; otherwise, the baseline dietary or covariate information was carried forward.
All analyses were stratified by sex, method of recruitment, and region of residence, and adjusted for year of recruitment, ethnicity, Townsend deprivation index [25], education level, physical activity [26], smoking, alcohol consumption, dietary supplement use, height, and in women menopausal status, hormone replacement therapy use, and parity. We tested models with and without adjustment for BMI. Details on the categorisation of covariates can be found in the Supplementary methods. The proportional hazards assumption was assessed on the basis of Schoenfeld residuals and was not violated for the variables of interest in the adjusted model for any of the outcomes. Subsequently, we estimated absolute rate differences based on the BMI adjusted model, using a previously reported method [28].
To evaluate the influence of dietary calcium and protein on the associations, we included models further adjusting for either dietary calcium or dietary protein intake, and simultaneously adjusting for both variables. Additional analyses were also performed limited to people with sufficient dietary calcium (≥ 700 mg/day) or dietary protein intake (≥ 0.75 g of protein per day/kg body weight) in accordance with UK dietary guidelines [29, 30].
As sensitivity analyses, we repeated the analyses (with adjustment for BMI) further adjusting for energy intake, excluding the first 5 years of follow-up, excluding participants with prior diseases (baseline history of diabetes, heart disease, stroke, or cancer), excluding participants who were receiving long-term treatment for any illness, and with multiple imputation for missing covariates [31]. Heterogeneity of results by age at recruitment (below and above age 50), sex, menopausal status, physical activity level (inactive/low and moderate/high activity), and BMI (below and above 22.5 kg/m2) was assessed for total and hip fractures, which had the largest numbers of cases. Cut-offs of age and BMI were chosen to ensure a reasonable distribution of number of cases in categories across all diet groups, based on analyses of total fractures.
All analyses were performed using Stata version 15.1 (StataCorp, TX, USA), and 2-sided p values < 0.05 were considered significant. The forest plot was generated using R (R Foundation for Statistical Computing, Vienna, Austria).
Results
The study population included a minimum of 54,898 participants (in analyses for total fractures), of whom 30,391 had repeated measures of diet 14 years later (details in Additional File 1: Fig. S1). Baseline characteristics in the overall cohort are tabulated by the four diet groups in Table 1, and separately for men and women in Additional File 1: Table S2. Other dietary and nutrient intakes are tabulated by the four diet groups, separately for men and women in Additional File 1: Table S3. A summary description of the baseline and dietary characteristics can be found in Additional File 1: Supplementary results.
Table 1.
Baseline characteristics of EPIC-Oxford participants by diet group
| Diet group | ||||
|---|---|---|---|---|
| Characteristics, mean (SD) or n (%) | Meat eaters (n = 29,380) | Fish eaters (n = 8037) | Vegetarians (n = 15,499) | Vegans (n = 1982) |
| Socio-demographic | ||||
| Age, years (SD) | 50.1 (13.1) | 42.7 (13.3) | 40.0 (13.5) | 38.9 (13.6) |
| Sex, women (%) | 22,591 (76.9) | 6614 (82.3) | 11,911 (76.9) | 1266 (63.9) |
| Top socio-economic quartile (%)a | 6947 (27.4) | 1534 (21.9) | 2952 (21.7) | 308 (17.6) |
| Higher education (%) | 8198 (30.8) | 3457 (45.3) | 6289 (42.7) | 797 (42.8) |
| White ethnicity (%) | 28,334 (98.6) | 7717 (97.8) | 14,764 (97.4) | 1848 (97.0) |
| Lifestyle | ||||
| Current smokers (%) | 3623 (12.4) | 805 (10.1) | 1554 (10.1) | 212 (10.8) |
| Alcohol consumption, g/day (SD) | 9.7 (12.6) | 9.8 (12.2) | 9.2 (12.6) | 8.3 (13.5) |
| Moderate or high physical activity (%) | 7516 (30.7) | 2795 (39.4) | 5400 (39.0) | 807 (45.3) |
| Dietary supplement use (%)b | 15,941 (55.4) | 5046 (64.3) | 8660 (56.9) | 1008 (51.9) |
| Health characteristics and medical history | ||||
| Body mass index, kg/m2 (SD) | 24.5 (4.0) | 23.0 (3.4) | 22.9 (3.5) | 22.1 (3.0) |
| < 20 kg/m2 (%) | 2365 (8.3) | 1178 (15.1) | 2508 (16.8) | 456 (23.8) |
| ≥ 25 kg/m2 (%) | 10,407 (36.6) | 1602 (20.6) | 3082 (20.7) | 268 (14.0) |
| Height in men, cm (SD) | 177.6 (7.0) | 178.1 (6.7) | 178.1 (7.0) | 178.1 (6.9) |
| Height in women, cm (SD) | 163.7 (6.7) | 164.6 (6.8) | 164.4 (6.8) | 164.5 (6.9) |
| Premenopausal (%)c | 9625 (44.0) | 4410 (68.2) | 8856 (75.7) | 940 (75.6) |
| Postmenopausal (%)c | 10,106 (46.2) | 1570 (24.3) | 2107 (18.0) | 235 (18.9) |
| Hormone replacement therapy use (%)c | 5945 (26.7) | 805 (12.3) | 992 (8.4) | 69 (5.6) |
| One or more children (%)c | 16,856 (75.2) | 3524 (53.8) | 5215 (44.3) | 431 (34.4) |
| Dietary information | ||||
| Energy, kJ/day (SD) | 8286 (2246) | 7940 (2208) | 7866 (2213) | 7342 (2315) |
| Dietary calcium, mg/day (SD) | 1005 (314) | 1033 (349) | 1030 (369) | 591 (237) |
| Protein, % energy (SD) | 17.0 (3.0) | 14.7 (2.4) | 13.6 (2.1) | 13.3 (2.3) |
Estimates shown are mean (SD) or numbers (%), as stated in left column. Percentages were estimated excluding participants with missing responses
aBased on Townsend deprivation index
bDefined as regularly taking any vitamins, minerals, fish oils, fibre, or other food supplements during the last 12 months
cIn women only
Over an average of 17.6 years of follow-up, we observed 3941 cases of total fractures (including 12 first reported at death; 943,934 person-years), 566 arm fractures (1 at death; 967,829 person-years), 889 wrist fractures (965,127 person-years), 945 hip fractures (1 at death; 967,599 person-years), 366 leg fractures (1 at death; 968,985 person-years), 520 ankle fractures (967,399 person-years), and 467 other main site fractures (968,921 person-years). The results of longitudinal associations between diet group and total and site-specific fractures are shown in Fig. 1 and Table 2. Absolute rate differences (AD) in the outcomes by diet group based on the BMI adjusted model are shown in Table 3.
Fig. 1.
Risks of total and site-specific fractures by diet group in EPIC-Oxford. Estimates also shown in Table 2 as model 2. All analyses were stratified by sex, method of recruitment (general practice or postal), and region (7 categories), and adjusted for year of recruitment (per year from ≤ 1994 to ≥ 1999), ethnicity (white, other, unknown), Townsend deprivation index (quartiles, unknown), education level (no qualifications, basic secondary (e.g. O level), higher secondary (e.g. A level), degree, unknown), physical activity (inactive, low activity, moderately active, very active, unknown), smoking (never, former, light, heavy, unknown), alcohol consumption (< 1 g, 1–7 g, 8–15 g, 16+ g/day), dietary supplement use (no, yes, unknown), height (5 cm categories from < 155 to ≥ 185 cm, unknown), body mass index (< 18.5, 18.5–19.9, 20–22.4, 22.5–24.9, 25–27.4, 27.5–29.9, 30–32.4, ≥ 32.5 kg/m2, unknown), and in women menopausal status (premenopausal, perimenopausal, postmenopausal, unknown), hormone replacement therapy use (never, ever, unknown), and parity (none, 1–2, ≥ 3, unknown). Other main site fractures are defined as fractures of the clavicle, rib, or vertebra
Table 2.
Risks of total and site-specific fractures by diet group in EPIC-Oxford, with varying levels of adjustments
| Fracture site/diet group | N cases | Person-years | Age at eventa | Hazard ratios (95% confidence intervals) | ||||
|---|---|---|---|---|---|---|---|---|
| Model 1b | Model 2c | Model 3d | Model 4e | Model 5f | ||||
| Total fractures (N = 54,898) | ||||||||
| Meat eaters | 2468 | 511,459 | 68.5 (13.1) | Reference | Reference | Reference | Reference | Reference |
| Fish eaters | 464 | 138,851 | 64.3 (14.5) | 0.97 (0.87, 1.07) | 0.95 (0.86, 1.05) | 0.95 (0.85, 1.05) | 0.94 (0.84, 1.04) | 0.94 (0.84, 1.05) |
| Vegetarians | 862 | 260,112 | 60.7 (16.4) | 1.11 (1.02, 1.21) | 1.09 (1.00, 1.19) | 1.08 (1.00, 1.18) | 1.07 (0.97, 1.17) | 1.07 (0.97, 1.18) |
| Vegans | 147 | 33,510 | 59.9 (17.4) | 1.50 (1.26, 1.78) | 1.43 (1.20, 1.70) | 1.31 (1.10, 1.57) | 1.39 (1.16, 1.67) | 1.30 (1.08, 1.56) |
| p-heterogeneityg | < 0.001 | < 0.001 | 0.003 | 0.001 | 0.009 | |||
| Arm fractures (N = 55,014) | ||||||||
| Meat eaters | 352 | 525,955 | 69.9 (12.4) | Reference | Reference | Reference | Reference | Reference |
| Fish eaters | 62 | 141,853 | 66.1 (13.0) | 0.93 (0.71, 1.24) | 0.92 (0.69, 1.22) | 0.92 (0.69, 1.22) | 0.85 (0.64, 1.13) | 0.85 (0.64, 1.13) |
| Vegetarians | 130 | 265,518 | 63.7 (15.4) | 1.28 (1.03, 1.60) | 1.25 (1.00, 1.56) | 1.25 (1.00, 1.56) | 1.12 (0.87, 1.43) | 1.12 (0.87, 1.43) |
| Vegans | 22 | 34,503 | 58.0 (16.1) | 1.67 (1.07, 2.61) | 1.56 (0.99, 2.44) | 1.54 (0.96, 2.46) | 1.39 (0.87, 2.22) | 1.39 (0.86, 2.25) |
| p-heterogeneityg | 0.020 | 0.049 | 0.056 | 0.19 | 0.20 | |||
| Wrist fractures (N = 55,013) | ||||||||
| Meat eaters | 565 | 523,913 | 67.3 (11.4) | Reference | Reference | Reference | Reference | Reference |
| Fish eaters | 110 | 141,606 | 64.4 (13.6) | 0.93 (0.75, 1.15) | 0.90 (0.73, 1.11) | 0.90 (0.73, 1.12) | 0.92 (0.74, 1.15) | 0.94 (0.75, 1.17) |
| Vegetarians | 185 | 265,177 | 60.2 (14.4) | 1.03 (0.86, 1.24) | 1.00 (0.83, 1.19) | 1.00 (0.83, 1.20) | 1.03 (0.84, 1.26) | 1.05 (0.86, 1.29) |
| Vegans | 29 | 34,431 | 58.8 (16.2) | 1.33 (0.91, 1.96) | 1.24 (0.84, 1.82) | 1.14 (0.76, 1.70) | 1.28 (0.86, 1.90) | 1.19 (0.79, 1.79) |
| p-heterogeneityg | 0.39 | 0.49 | 0.70 | 0.49 | 0.67 | |||
| Hip fractures (N = 55,026) | ||||||||
| Meat eaters | 610 | 525,706 | 76.8 (9.5) | Reference | Reference | Reference | Reference | Reference |
| Fish eaters | 122 | 141,856 | 74.6 (11.4) | 1.33 (1.08, 1.62) | 1.26 (1.02, 1.54) | 1.26 (1.03, 1.54) | 1.24 (1.01, 1.53) | 1.25 (1.01, 1.55) |
| Vegetarians | 172 | 265,548 | 74.5 (11.9) | 1.34 (1.12, 1.61) | 1.25 (1.04, 1.50) | 1.24 (1.03, 1.49) | 1.20 (0.98, 1.47) | 1.21 (0.99, 1.49) |
| Vegans | 41 | 34,489 | 74.1 (13.3) | 2.64 (1.90, 3.67) | 2.31 (1.66, 3.22) | 1.97 (1.39, 2.79) | 2.21 (1.56, 3.12) | 1.94 (1.35, 2.77) |
| p-heterogeneityg | < 0.001 | < 0.001 | < 0.001 | < 0.001 | 0.002 | |||
| Leg fractures (N = 55,019) | ||||||||
| Meat eaters | 227 | 526,617 | 68.7 (12.3) | Reference | Reference | Reference | Reference | Reference |
| Fish eaters | 48 | 141,993 | 62.8 (13.8) | 1.06 (0.77, 1.47) | 1.07 (0.77, 1.48) | 1.06 (0.77, 1.47) | 1.06 (0.76, 1.49) | 1.05 (0.75, 1.47) |
| Vegetarians | 73 | 265,842 | 61.3 (16.0) | 1.00 (0.75, 1.33) | 1.01 (0.76, 1.34) | 1.00 (0.75, 1.33) | 0.99 (0.72, 1.37) | 0.99 (0.72, 1.36) |
| Vegans | 18 | 34,533 | 59.1 (19.3) | 2.04 (1.23, 3.38) | 2.05 (1.23, 3.41) | 1.83 (1.07, 3.14) | 2.02 (1.19, 3.44) | 1.81 (1.04, 3.15) |
| p-heterogeneityg | 0.044 | 0.045 | 0.16 | 0.053 | 0.17 | |||
| Ankle fractures (N = 55,021) | ||||||||
| Meat eaters | 332 | 525,449 | 63.0 (12.1) | Reference | Reference | Reference | Reference | Reference |
| Fish eaters | 58 | 141,898 | 56.0 (10.2) | 0.79 (0.59, 1.05) | 0.84 (0.63, 1.12) | 0.84 (0.63, 1.12) | 0.88 (0.65, 1.19) | 0.89 (0.66, 1.20) |
| Vegetarians | 117 | 265,486 | 54.7 (14.4) | 0.94 (0.75, 1.19) | 1.01 (0.80, 1.27) | 1.01 (0.80, 1.27) | 1.10 (0.85, 1.43) | 1.11 (0.85, 1.44) |
| Vegans | 13 | 34,566 | 51.1 (14.8) | 0.90 (0.51, 1.58) | 1.03 (0.58, 1.82) | 0.91 (0.50, 1.63) | 1.13 (0.63, 2.03) | 1.00 (0.55, 1.82) |
| p-heterogeneityg | 0.44 | 0.65 | 0.65 | 0.59 | 0.60 | |||
| Other main site fracturesh (N = 55,016) | ||||||||
| Meat eaters | 287 | 526,576 | 69.1 (14.1) | Reference | Reference | Reference | Reference | Reference |
| Fish eaters | 57 | 142,051 | 63.1 (15.1) | 1.01 (0.75, 1.36) | 0.98 (0.73, 1.33) | 0.98 (0.72, 1.32) | 0.98 (0.72, 1.33) | 0.96 (0.71, 1.31) |
| Vegetarians | 100 | 265,768 | 59.4 (16.7) | 1.03 (0.80, 1.32) | 0.99 (0.77, 1.27) | 0.98 (0.76, 1.26) | 0.97 (0.73, 1.28) | 0.95 (0.72, 1.26) |
| Vegans | 23 | 34,526 | 58.2 (16.2) | 1.73 (1.11, 2.70) | 1.59 (1.02, 2.50) | 1.66 (1.03, 2.67) | 1.55 (0.97, 2.48) | 1.61 (0.98, 2.62) |
| p-heterogeneityg | 0.11 | 0.20 | 0.18 | 0.23 | 0.20 | |||
aIn cases only, as mean years (SD)
bModel 1 was stratified by sex, method of recruitment (general practice or postal), and region (7 categories), and adjusted for year of recruitment (per year from ≤ 1994 to ≥ 1999), ethnicity (white, other, unknown), Townsend deprivation index (quartiles, unknown), education level (no qualifications, basic secondary (e.g. O level), higher secondary (e.g. A level), degree, unknown), physical activity (inactive, low activity, moderately active, very active, unknown), smoking (never, former, light, heavy, unknown), alcohol consumption (< 1 g, 1–7 g, 8–15 g, 16+ g/day), dietary supplement use (no, yes, unknown), height (5 cm categories from < 155 to ≥ 185 cm, unknown), and in women menopausal status (premenopausal, perimenopausal, postmenopausal, unknown), hormone replacement therapy use (never, ever, unknown), and parity (none, 1–2, ≥ 3, unknown)
cModel 2 was model 1 plus BMI (< 18.5, 18.5–19.9, 20–22.4, 22.5–24.9, 25–27.4, 27.5–29.9, 30–32.4, ≥ 32.5 kg/m2, unknown)
dModel 3 was model 2 plus dietary calcium intake (< 525, 525–699, 700–899, 900–1199, ≥ 1200 mg)
eModel 4 was model 2 plus protein intake (< 13, 13–14.4, 14.5–15.9, 16–18.0, ≥ 18.1 of % energy)
fModel 5 was model 2 plus dietary calcium intake (< 525, 525–699, 700–899, 900–1199, ≥ 1200 mg) and protein intake (< 13, 13–14.4, 14.5–15.9, 16–18.0, ≥ 18.1 of % energy)
gp-heterogeneity represents heterogeneity in risk between diet group based on Wald’s tests
hDefined as fractures of the clavicle, rib, or vertebra
Table 3.
Absolute rate differences of total and site-specific fractures by diet group in EPIC-Oxford
| Fracture site/diet group | Predicted incidencea | Absolute rate differenceb | ||
|---|---|---|---|---|
| Per 1000 person-years | Per 1000 people over 10 years | Per 1000 person-years | Per 1000 people over 10 years | |
| Total fractures | ||||
| Meat eaters | 4.8 (4.6, 5.1) | 47.2 (44.9, 49.7) | Reference | Reference |
| Fish eaters | 4.6 (4.2, 5.0) | 44.8 (41.0, 49.0) | − 0.2 (− 0.6, 0.2) | − 2.4 (− 6.2, 1.8) |
| Vegetarians | 5.3 (4.9, 5.6) | 51.3 (48.0, 54.8) | 0.4 (0.1, 0.8) | 4.1 (0.8, 7.6) |
| Vegans | 6.9 (5.8, 8.1) | 66.6 (56.8, 78.1) | 2.0 (1.0, 3.3) | 19.4 (9.6, 30.9) |
| Total fractures in men | ||||
| Meat eaters | 3.9 (3.4, 4.4) | 37.9 (33.4, 42.8) | Reference | Reference |
| Fish eaters | 3.6 (2.9, 4.5) | 35.5 (28.5, 44.3) | − 0.2 (− 1.0, 0.7) | − 2.3 (− 9.4, 6.4) |
| Vegetarians | 4.1 (3.5, 4.7) | 40.0 (34.9, 45.8) | 0.2 (− 0.3, 0.8) | 2.1 (− 3.0, 7.9) |
| Vegans | 4.5 (3.4, 6.1) | 44.3 (33.2, 59.1) | 0.7 (− 0.5, 2.2) | 6.5 (− 4.7, 21.3) |
| Total fractures in women | ||||
| Meat eaters | 5.1 (4.8, 5.4) | 49.9 (47.2, 52.7) | Reference | Reference |
| Fish eaters | 4.9 (4.4, 5.4) | 47.5 (43.1, 52.3) | − 0.3 (− 0.7, 0.3) | − 2.4 (− 6.8, 2.4) |
| Vegetarians | 5.6 (5.2, 6.0) | 54.5 (50.5, 58.8) | 0.5 (0.1, 0.9) | 4.6 (0.6, 8.9) |
| Vegans | 7.8 (6.4, 9.5) | 75.1 (62.0, 90.9) | 2.7 (1.3, 4.4) | 25.2 (12.1, 41.0) |
| Arm fractures | ||||
| Meat eaters | 0.7 (0.6, 0.8) | 6.7 (5.8, 7.6) | Reference | Reference |
| Fish eaters | 0.6 (0.5, 0.8) | 6.1 (4.8, 7.9) | − 0.1 (− 0.2, 0.1) | − 0.5 (− 1.9, 1.2) |
| Vegetarians | 0.8 (0.7, 1.0) | 8.3 (7.0, 9.9) | 0.2 (0.0, 0.3) | 1.6 (0.3, 3.2) |
| Vegans | 1.0 (0.7, 1.6) | 10.4 (6.8, 15.8) | 0.4 (0.0, 0.9) | 3.7 (0.1, 9.2) |
| Wrist fractures | ||||
| Meat eaters | 1.1 (1.0, 1.2) | 10.7 (9.7, 11.9) | Reference | Reference |
| Fish eaters | 1.0 (0.8, 1.2) | 9.7 (8.0, 11.6) | − 0.1 (− 0.3, 0.1) | − 1.1 (− 2.7, 0.9) |
| Vegetarians | 1.1 (0.9, 1.2) | 10.7 (9.2, 12.4) | 0.0 (− 0.1, 0.2) | 0.0 (− 1.5, 1.7) |
| Vegans | 1.3 (0.9, 1.9) | 13.2 (9.2, 19.1) | 0.3 (− 0.2, 0.8) | 2.5 (− 1.6, 8.4) |
| Hip fractures | ||||
| Meat eaters | 1.2 (1.0, 1.3) | 11.5 (10.4, 12.8) | Reference | Reference |
| Fish eaters | 1.5 (1.2, 1.7) | 14.5 (12.1, 17.3) | 0.3 (0.1, 0.6) | 2.9 (0.6, 5.7) |
| Vegetarians | 1.5 (1.2, 1.7) | 14.4 (12.4, 16.8) | 0.3 (0.1, 0.5) | 2.9 (0.9, 5.2) |
| Vegans | 2.7 (2.0, 3.7) | 26.5 (19.4, 36.0) | 1.5 (0.8, 2.5) | 14.9 (7.9, 24.5) |
| Leg fractures | ||||
| Meat eaters | 0.4 (0.4, 0.5) | 4.3 (3.6, 5.1) | Reference | Reference |
| Fish eaters | 0.5 (0.3, 0.6) | 4.6 (3.5, 6.1) | 0.0 (− 0.1, 0.2) | 0.3 (− 0.8, 1.8) |
| Vegetarians | 0.4 (0.3, 0.5) | 4.3 (3.4, 5.5) | 0.0 (− 0.1, 0.1) | 0.0 (− 0.9, 1.2) |
| Vegans | 0.9 (0.5, 1.4) | 8.8 (5.5, 14.1) | 0.5 (0.1, 1.0) | 4.5 (1.2, 9.8) |
| Ankle fractures | ||||
| Meat eaters | 0.6 (0.5, 0.7) | 6.3 (5.5, 7.2) | Reference | Reference |
| Fish eaters | 0.5 (0.4, 0.7) | 5.3 (4.1, 6.8) | − 0.1 (− 0.2, 0.1) | − 1.0 (− 2.2, 0.5) |
| Vegetarians | 0.6 (0.5, 0.8) | 6.4 (5.3, 7.7) | 0.0 (− 0.1, 0.1) | 0.1 (− 1.0, 1.4) |
| Vegans | 0.7 (0.4, 1.1) | 6.5 (3.7, 11.2) | 0.0 (− 0.3, 0.5) | 0.2 (− 2.6, 4.9) |
| Other main site fracturesc | ||||
| Meat eaters | 0.5 (0.5, 0.6) | 5.4 (4.7, 6.3) | Reference | Reference |
| Fish eaters | 0.5 (0.4, 0.7) | 5.4 (4.1, 6.9) | 0.0 (− 0.1, 0.1) | − 0.1 (− 1.3, 1.5) |
| Vegetarians | 0.5 (0.4, 0.7) | 5.4 (4.4, 6.5) | 0.0 (− 0.1, 0.1) | − 0.1 (− 1.0, 1.1) |
| Vegans | 0.9 (0.6, 1.3) | 8.7 (5.7, 13.1) | 0.3 (0.0, 0.8) | 3.2 (0.3, 7.7) |
aFor meat eaters, calculated as (1 − Sr) × 1000, where Sr = (1 − observed incidence in meat eaters), representing the average survival (or non-incidence) rate in the meat eaters, or Sr = (1 − observed incidence in meat eaters)10, representing the predicted 10-year survival rate in the meat eaters. For all other diet groups, calculated as (1 − SrHR) × 1000, where HR represents the hazard ratio or confidence intervals of the hazard ratio for each outcome in that diet group, and SrHR represents either the predicted average survival or the predicted 10-year survival rate in the diet group, as indicated in the column heading. Hazard ratios and confidence intervals were based on covariate adjustment as listed for Table 2 model 2 or Table 5 (for total fractures in men and women), and expressed as floating absolute risks
bCalculated as the difference between the predicted incidence per 1000 person-years or per 1000 people over 10 years between each diet group and the meat eaters
cDefined as fractures of the clavicle, rib, or vertebra
Compared with meat eaters, vegetarians (HR 1.11; 95% CI 1.02, 1.21) and vegans (1.50; 1.26, 1.78) had higher risks of total fractures after adjustment for confounders (Table 2 model 1). The associations attenuated with additional adjustment of BMI (vegetarians—1.09; 1.00, 1.19; vegans—1.43; 1.20, 1.70), but remained clearly significant in vegans (Table 2 model 2, Fig. 1). The equivalent rate differences were 4.1 (0.8, 7.6) more cases in vegetarians and 19.4 (9.6, 30.9) more cases in vegans for every 1000 people over 10 years. The associations were attenuated further but remained significant in vegans with additional adjustment for dietary calcium (1.31; 1.10, 1.57, Table 2 model 3), total dietary protein (1.39; 1.16, 1.67, Table 2 model 4), or both dietary factors simultaneously (1.30; 1.08, 1.56, Table 2 model 5).
For site-specific fractures (Fig. 1 and Table 2), the largest magnitudes in risk difference by diet group were observed for hip fractures. After adjustment for BMI, the risks were higher in fish eaters (HR 1.26; 1.02, 1.54, or AD 2.9; 0.6, 5.7), vegetarians (HR 1.25; 1.04, 1.50, or AD 2.9; 0.9, 5.2), and vegans (HR 2.31; 1.66, 3.22, or AD 14.9; 7.9, 24.5) than meat eaters. Similar to the findings for total fractures, the associations appeared stronger before BMI adjustment and attenuated but remained strongly significant in vegans after further adjustment for both calcium and protein.
For the other sites, after adjustment for BMI, the vegans had a higher risk of leg fractures (2.05; 1.23, 3.41) and other main site fractures (clavicle, rib, vertebra, 1.59; 1.02, 2.50) than the meat eaters (Fig. 1 and Table 2). When the other main site fractures were examined separately, a significantly higher risk was observed in the vegans for vertebral fracture (2.42; 2.31, 4.48), but not for the other two sites (Additional File 1: Table S4). No significant differences in risks between diet groups were observed for arm, wrist, or ankle fracture, after adjustment for BMI (Fig. 1 and Table 2), although a higher risk of arm fractures was observed in both vegetarians (1.28; 1.03, 1.60) and vegans (1.67; 1.07, 2.61) in the multivariable model before BMI adjustment (Table 2 model 1).
Results from secondary analyses are reported in more detail in the Supplementary results. Overall, results were consistent when the analyses were restricted to participants with sufficient intakes of calcium and protein (Table 4), and also in other secondary analyses, including with further adjustment for energy intake, excluding the first 5 years of follow-up, excluding participants with prior diseases or receiving long-term treatment for any illness, or with multiple imputation for missing covariates (Additional File 1: Table S5).
Table 4.
Risks of total and site-specific fractures by diet group in EPIC-Oxford, in participants with adequate levels of dietary calcium or protein
| Fracture site/diet group | Hazard ratios (95% confidence intervals)a | |||||
|---|---|---|---|---|---|---|
| N cases | Dietary calcium ≥ 700 mg/day | N cases | Dietary protein ≥ 0.75 g per day/kg body weight | N cases | Dietary calcium ≥ 700 mg/day plus dietary protein ≥ 0.75 g per day/kg body weight | |
| Total fractures | ||||||
| Meat eaters | 2077 | Reference | 2188 | Reference | 1925 | Reference |
| Fish eaters | 377 | 0.92 (0.82, 1.03) | 376 | 0.92 (0.82, 1.03) | 332 | 0.90 (0.80, 1.02) |
| Vegetarians | 700 | 1.08 (0.98, 1.19) | 648 | 1.07 (0.97, 1.18) | 583 | 1.06 (0.96, 1.18) |
| Vegans | 49 | 1.50 (1.12, 1.99) | 103 | 1.52 (1.24, 1.87) | 44 | 1.45 (1.07, 1.97) |
| p-heterogeneityb | 0.003 | < 0.001 | 0.009 | |||
| Arm fractures | ||||||
| Meat eaters | 300 | Reference | 304 | Reference | 273 | Reference |
| Fish eaters | 54 | 0.96 (0.71, 1.30) | 49 | 0.89 (0.65, 1.21) | 46 | 0.91 (0.66, 1.26) |
| Vegetarians | 107 | 1.27 (0.99, 1.62) | 98 | 1.24 (0.97, 1.59) | 90 | 1.25 (0.96, 1.62) |
| Vegans | 8 | 1.76 (0.86, 3.61) | 15 | 1.58 (0.92, 2.70) | 7 | 1.61 (0.75, 3.46) |
| p-heterogeneityb | 0.10 | 0.091 | 0.18 | |||
| Wrist fractures | ||||||
| Meat eaters | 475 | Reference | 503 | Reference | 436 | Reference |
| Fish eaters | 89 | 0.88 (0.70, 1.11) | 96 | 0.93 (0.74, 1.16) | 82 | 0.91 (0.71, 1.16) |
| Vegetarians | 146 | 0.96 (0.79, 1.18) | 140 | 0.97 (0.79, 1.19) | 126 | 0.99 (0.80, 1.23) |
| Vegans | 9 | 1.14 (0.58, 2.22) | 21 | 1.35 (0.86, 2.12) | 9 | 1.29 (0.66, 2.52) |
| p-heterogeneityb | 0.71 | 0.47 | 0.74 | |||
| Hip fractures | ||||||
| Meat eaters | 507 | Reference | 536 | Reference | 463 | Reference |
| Fish eaters | 95 | 1.21 (0.96, 1.52) | 97 | 1.19 (0.95, 1.49) | 85 | 1.22 (0.96, 1.55) |
| Vegetarians | 136 | 1.25 (1.02, 1.54) | 130 | 1.22 (0.99, 1.50) | 115 | 1.25 (1.01, 1.56) |
| Vegans | 14 | 2.39 (1.39, 4.11) | 31 | 2.71 (1.85, 3.95) | 13 | 2.43 (1.38, 4.28) |
| p-heterogeneityb | 0.003 | < 0.001 | 0.004 | |||
| Leg fractures | ||||||
| Meat eaters | 191 | Reference | 197 | Reference | 179 | Reference |
| Fish eaters | 38 | 0.98 (0.68, 1.42) | 38 | 1.04 (0.73, 1.50) | 34 | 0.97 (0.66, 1.42) |
| Vegetarians | 61 | 1.00 (0.73, 1.37) | 51 | 0.95 (0.68, 1.32) | 46 | 0.87 (0.62, 1.24) |
| Vegans | 7 | 2.50 (1.15, 5.42) | 16 | 2.90 (1.68, 4.99) | 6 | 2.32 (1.00, 5.34) |
| p-heterogeneityb | 0.13 | 0.001 | 0.17 | |||
| Ankle fractures | ||||||
| Meat eaters | 277 | Reference | 296 | Reference | 263 | Reference |
| Fish eaters | 49 | 0.84 (0.61, 1.15) | 44 | 0.79 (0.57, 1.10) | 40 | 0.77 (0.55, 1.09) |
| Vegetarians | 88 | 0.91 (0.70, 1.19) | 79 | 0.97 (0.74, 1.27) | 72 | 0.92 (0.69, 1.23) |
| Vegans | 3 | 0.73 (0.23, 2.31) | 9 | 1.19 (0.60, 2.36) | 3 | 0.85 (0.27, 2.69) |
| p-heterogeneityb | 0.66 | 0.50 | 0.54 | |||
| Other main site fracturesc | ||||||
| Meat eaters | 249 | Reference | 254 | Reference | 229 | Reference |
| Fish eaters | 49 | 0.97 (0.70, 1.34) | 47 | 0.95 (0.68, 1.31) | 44 | 0.95 (0.68, 1.34) |
| Vegetarians | 84 | 0.97 (0.74, 1.27) | 75 | 0.93 (0.70, 1.24) | 70 | 0.93 (0.69, 1.25) |
| Vegans | 11 | 2.30 (1.23, 4.28) | 18 | 1.82 (1.10, 3.01) | 11 | 2.40 (1.28, 4.50) |
| p-heterogeneityb | 0.06 | 0.08 | 0.03 | |||
aAll analyses were stratified by sex, method of recruitment (general practice or postal), and region (7 categories), and adjusted for year of recruitment (per year from ≤ 1994 to ≥ 1999), ethnicity (white, other, unknown), Townsend deprivation index (quartiles, unknown), education level (no qualifications, basic secondary (e.g. O level), higher secondary (e.g. A level), degree, unknown), physical activity (inactive, low activity, moderately active, very active, unknown), smoking (never, former, light, heavy, unknown), alcohol consumption (< 1 g, 1–7 g, 8–15 g, 16+ g/day), dietary supplement use (no, yes, unknown), height (5 cm categories from < 155 to ≥ 185 cm, unknown), BMI (< 18.5, 18.5–19.9, 20–22.4, 22.5–24.9, 25–27.4, 27.5–29.9, 30–32.4, ≥ 32.5 kg/m2, unknown), and in women menopausal status (premenopausal, perimenopausal, postmenopausal, unknown), hormone replacement therapy use (never, ever, unknown), and parity (none, 1–2, ≥ 3, unknown)
bRepresents heterogeneity in risk between diet groups based on Wald’s tests
cDefined as fractures of the clavicle, rib, or vertebra
In stratified analyses of total (Table 5) and hip fractures (Additional File 1: Table S6), a significantly higher risk of both total and hip fractures was only observed in vegetarians over age 50 at recruitment, although vegans had higher risks in both age groups, and a significant p for interaction was only observed for total fractures. For both types of fractures, the significant associations in vegans appeared stronger in women, particularly those who were postmenopausal, and participants with low physical activity and lower BMI, possibly partly due to the larger number of participants in most of these subgroups, but a higher risk of hip fracture was only observed in the fish eaters and vegetarians in the higher BMI category. Because the numbers of cases in these subgroup analyses were often very small, it is likely that we did not have sufficient power to identify possible differences.
Table 5.
Risks of total fractures by diet group, stratified by age, sex, menopausal status, physical activity, and BMI
| Stratifying variable | N cases in strata, hazard ratios (95% confidence intervals)a | Test of interactionb | |||
|---|---|---|---|---|---|
| Age at recruitment | < 50 years | ≥ 50 years | |||
| Meat eaters | 690 | Reference | 1778 | Reference | |
| Fish eaters | 204 | 0.86 (0.73, 1.01) | 260 | 0.99 (0.87, 1.14) | |
| Vegetarians | 459 | 1.00 (0.88, 1.13) | 403 | 1.14 (1.01, 1.27) | χ2 = 23.07 |
| Vegans | 80 | 1.31 (1.03, 1.67) | 67 | 1.50 (1.17, 1.93) | p < 0.001 |
| p-heterogeneityc | 0.016 | 0.003 | |||
| Sex | Men | Women | |||
| Meat eaters | 440 | Reference | 2028 | Reference | |
| Fish eaters | 76 | 0.94 (0.73, 1.21) | 388 | 0.95 (0.85, 1.06) | |
| Vegetarians | 202 | 1.06 (0.88, 1.28) | 660 | 1.09 (0.99, 1.20) | χ2 = 6.39 |
| Vegans | 47 | 1.18 (0.85, 1.62) | 100 | 1.53 (1.24, 1.88) | p = 0.09 |
| p-heterogeneityc | 0.64 | < 0.001 | |||
| Menopausal statusd | Premenopausal | Postmenopausal | |||
| Meat eaters | 167 | Reference | 1500 | Reference | |
| Fish eaters | 54 | 0.64 (0.47, 0.87) | 231 | 1.01 (0.88, 1.17) | |
| Vegetarians | 161 | 0.91 (0.73, 1.15) | 325 | 1.13 (0.99, 1.28) | χ2 = 3.74 |
| Vegans | 27 | 1.41 (0.93, 2.15) | 52 | 1.62 (1.22, 2.16) | p = 0.44 |
| p-heterogeneityc | 0.004 | 0.004 | |||
| Physical activity | Inactive/low | Moderate/high | |||
| Meat eaters | 1437 | Reference | 561 | Reference | |
| Fish eaters | 253 | 0.94 (0.82, 1.08) | 144 | 0.96 (0.79, 1.16) | |
| Vegetarians | 495 | 1.09 (0.98, 1.22) | 257 | 1.03 (0.88, 1.22) | χ2 = 0.69 |
| Vegans | 79 | 1.43 (1.13, 1.80) | 50 | 1.34 (0.98, 1.82) | p = 0.88 |
| p-heterogeneityc | 0.006 | 0.25 | |||
| Body mass index | < 22.5 kg/m2 | ≥ 22.5 kg/m2 | |||
| Meat eaters | 762 | Reference | 1593 | Reference | |
| Fish eaters | 210 | 0.95 (0.81, 1.11) | 237 | 0.97 (0.84, 1.11) | |
| Vegetarians | 428 | 1.17 (1.02, 1.33) | 396 | 1.04 (0.92, 1.17) | χ2 = 4.71 |
| Vegans | 95 | 1.66 (1.32, 2.08) | 43 | 1.10 (0.80, 1.49) | p = 0.19 |
| p-heterogeneityc | < 0.001 | 0.76 | |||
aResults shown were for subset analyses by the stratifying variable. Analyses were stratified by sex, method of recruitment (general practice or postal), and region (7 categories), and adjusted for year of recruitment (per year from ≤ 1994 to ≥ 1999), ethnicity (white, other, unknown), Townsend deprivation index (quartiles, unknown), education level (no qualifications, basic secondary (e.g. O level), higher secondary (e.g. A level), degree, unknown), physical activity (inactive, low activity, moderately active, very active, unknown), smoking (never, former, light, heavy, unknown), alcohol consumption (< 1 g, 1–7 g, 8–15 g, 16+ g/day), dietary supplement use (no, yes, unknown), height (5 cm categories from < 155 to ≥ 185 cm, unknown), BMI (< 18.5, 18.5–19.9, 20–22.4, 22.5–24.9, 25–27.4, 27.5–29.9, 30–32.4, ≥ 32.5 kg/m2, unknown), and in women menopausal status (premenopausal, perimenopausal, postmenopausal, unknown), hormone replacement therapy use (never, ever, unknown), and parity (none, 1–2, ≥ 3, unknown), except the stratifying variable where appropriate
bInteractions by age at recruitment, sex, menopausal status, physical activity, and body mass index were investigated by including both strata in the model (e.g. both men and women) and comparing Cox models with and without the appropriate interaction term using likelihood ratio tests
cRepresents heterogeneity in risk between diet groups based on Wald tests
dPremenopausal women included women who were below age 50 years at recruitment if they were perimenopausal or had unknown menopausal status; analyses in premenopausal women were censored at age 50. Postmenopausal women included women above age 50 years at recruitment if perimenopausal or had unknown perimenopausal status
Discussion
Summary of findings
Overall, vegans in this study had higher risks of total and some site-specific fractures (hip, leg, vertebra) than meat eaters. The strongest associations were observed for hip fractures, for which fish eaters, vegetarians, and vegans all had higher risks. These risk differences might be partially explained by the lower average BMI, and lower average intakes of calcium and protein in the non-meat eaters. However, because the differences remained, especially in vegans, after accounting for these factors, other unaccounted for factors may be important.
Comparison with previous studies
Few previous studies have examined the associations of vegetarian diets with fracture risk. In previous EPIC-Oxford analyses of self-reported fractures with short follow-up, vegans, but not fish eaters or vegetarians, were reported to have 30% (HR 1.30; 1.02, 1.66) higher risks of total fractures, but in contrast to the current findings, the association attenuated completely when restricted to participants who reported consuming at least 525 mg/day of calcium [16]. This apparent inconsistency might be explained by several differences between the current and previous analysis; while the current analysis included close to 4000 hospital-admitted cases over more than 17 years of average follow-up on around 55,000 participants, the previous study included under 2000 self-reported fracture cases over 5 years of follow-up on around 35,000 participants. Given the difference in case ascertainment method, the current analysis is less prone to reporting error and is not susceptible to selective drop-out. It is also possible that there was insufficient power to detect a difference after stratifying by calcium intake status in the previous analysis, which also did not examine site-specific fractures.
The only other studies which reported on risks of fractures by diet groups were one small prospective study in Vietnam of 210 women (105 vegans) which found no significant difference in fracture incidence (10 cases in total) between vegans and omnivores over 2 years [17], and one prospective study in India which reported a higher crude rate of stress fractures (604 cases in total) among 2131 vegetarian than 6439 non-vegetarian army recruits [18]. Separately, previous findings from the Adventist Health Study 2, which has a large proportion of vegetarians, showed that participants who ate meat more than three times a week had lower risks of hip fractures (HR 0.60; 0.41, 0.87) than participants who ate meat less than once a week [32], while combined analyses of peri- and postmenopausal women from Adventist Health Study 1 and 2 found that participants who ate meat more than four times a week had lower risks of wrist fractures (HR 0.44; 0.23, 0.84) than participants who never ate meat [33], but these results cannot be used to infer risks in fish eaters, vegetarians, or vegans as separate diet groups.
Interpretation of results and implications
The higher observed risks of fractures in non-meat eaters were usually stronger before BMI adjustment, which suggests that the risk differences were likely partially due to differences in BMI. Vegetarians and vegans generally have lower BMI than meat eaters [2, 8], and previous studies have reported an inverse association between BMI and some fractures, particularly hip fractures, possibly due to reasons including the cushioning against impact force during a fall, enhanced oestrogen production with increased adiposity, or stronger bones from increased weight-bearing [14, 34]. However, a positive association between BMI and fracture risk has been observed for some other sites, including ankle fractures, possibly as a result of higher torques from twisting of the ankle in people with higher BMI [14]. No significant differences in the risks of ankle fractures by diet group were observed in our study, but the point estimates were directionally consistent with a lower risk in all non-meat eaters before BMI adjustment, and the results might reflect a counterbalance between a protective effect from lower BMI but higher risk due to lower intakes of nutrients related to bone health in the non-meat eaters.
In our stratified analyses, there is limited evidence of heterogeneity in fracture risk by BMI categories. Although a statistically significant higher risk of total and hip fractures was only observed in vegans in the lower BMI category (< 22.5 kg/m2), our interpretation is limited by the small numbers of cases in each stratum in these analyses, especially because of the strong correlation between diet group and BMI, which results in very few vegans in the higher BMI category, and vice versa comparatively small numbers of meat eaters with a low BMI. In addition to BMI, previous studies have reported that muscle strength is an important risk factor which is protective against fall risk and subsequently fractures in older adults [35]. A previous study in the UK found lower lean mass and grip strength in vegetarians and vegans compared to meat eaters [2]; therefore, the possible influences of muscle strength and fall risk in addition to bone health on fracture risk in vegetarian and vegan populations should be further investigated. Fractures at some sites, especially at the hip, may also be more related to osteoporosis than fractures at some other sites, which might be more likely to be the result of violent impacts in accidents [36, 37]. We were unable to differentiate fragility and traumatic fractures in this study, since data were not available on the causes of the fractures.
In this study and previous studies, vegans had substantially lower intakes of calcium than other diet groups since they do not consume dairy, a major source of dietary calcium [4, 5], while both vegetarians and vegans had lower protein intakes on average [6, 7]. In the human body, 99% of calcium is present in bones and teeth in the form of hydroxyapatite, which in cases of calcium deficiency gets resorbed to maintain the metabolic calcium balance, and thus, osteoporosis could occur if the calcium was not restored [38–40]. A recent meta-analysis reported that increasing calcium intake from either dietary sources or supplements resulted in small increases in BMD [9], but the evidence on fracture risk has been less consistent. Previous analyses in EPIC-Oxford found a higher risk of self-reported fractures in women, but not men, with calcium intakes below 525 mg/day compared with over 1200 mg/day [41]. A recent meta-analysis of both randomised trials and prospective studies concluded that there was no evidence of an association between calcium intake from diet and fracture risk, but a possible weak protective association between calcium supplement use and some fractures [10]. More recently however, a separate meta-analysis showed a protective effect against fractures of combined vitamin D and calcium supplements, but not vitamin D supplements alone [11].
For protein, some older studies suggested that excessive protein intake would lead to an increased metabolic acid load, subsequently buffered by bone resorption and calciuria, and thus poorer bone health [12, 42]. However, more recent experimental evidence has shown that high protein intake also increases intestinal calcium absorption [43], and stimulates the production of insulin-like growth factor (IGF)-I [44], which in turn is associated with better bone health [45, 46]. Two meta-analyses, which included different studies, both reported a possible protective effect of higher protein intake on lumbar spine BMD [13, 47]; several epidemiological studies have reported inverse associations between protein intake and fracture risks [48–50], though a recent meta-analysis found no significant association between protein intake and osteoporotic fractures [51].
The higher risks of fractures especially in the vegans remained significant after adjustment for dietary calcium and protein, which suggests that these factors may at most only partly explain the differences in fracture risks by diet group, and other factors may also contribute. However, estimation of intakes of these nutrients by questionnaires has substantial error, and we were only able to account for differences in dietary calcium but not differences in calcium supplement use, since data on the latter were not available. A detailed analysis of the associations of specific foods, such as meat or dairy, with fracture risk is beyond the scope of the current study, but should be explored in further studies. Future research should also focus on possible effects of other nutrients or biological markers on fracture risks, for example circulating vitamin D, vitamin B12, or IGF-I, which may vary by degree of animal-sourced food intake [52–54]. The value of incorporating habitual dietary habits in addition to established parameters for predicting fracture risks in clinical settings should also be further explored.
Strengths and limitations
The strengths of this study were that it included a large number of non-meat eaters with a long follow-up, and studied both total and site-specific fractures, after accounting for a range of confounders. We updated diet group and relevant confounders where possible, to account for changes over the period of follow-up. There was little evidence of reverse causality, as results were similar after excluding the first 5 years of follow-up. The outcome data were ascertained based on hospital records, which reduced misreporting and selective loss to follow-up, although a possible limitation of this approach was that less serious fractures that did not require hospitalisation would not have been captured.
Of other limitations, while we excluded known cases of fractures before baseline based on hospital records, this may not be a complete exclusion, since no questions on previous diagnosis of fractures (prior to the earliest available hospital data) or osteoporosis were asked at baseline, and no data on the use of anti-osteoporosis medication were available. Repeat measures of diet were not available in all participants, and the exact date of dietary change during follow-up was also not recorded, but considering the good agreement of diet group in participants who did provide a repeat measure, and the fact that a dietary change may only influence fracture risk after a period of time, we do not expect substantial misclassification. As with all observational studies, residual confounding from both dietary and non-dietary factors may be present; for example, the role of calcium might have been underestimated due to measurement error. As the study predominantly includes white European participants, generalisability to other populations or ethnicities may be limited, which could be important considering previously observed differences in BMD [2, 55] and fracture risks [56] by ethnicity. We also observed only a small number of cases in many subgroup analyses, and thus, it is likely we had insufficient power to reliably assess whether there might be any heterogeneity by these subgroups including age, sex, menopausal status, or BMI; additional data are therefore needed to confirm or refute possible differences. In particular, because the EPIC-Oxford cohort consists predominantly of women (77%), further work should be conducted in cohorts with a larger proportion of men to explore heterogeneity by sex and to derive reliable sex-specific estimates.
Conclusions
Overall, we found that compared with meat eaters, vegans had higher risks of total, hip, leg, and vertebral fractures, while fish eaters and vegetarians had higher risk of hip fractures. These risk differences were likely partly due to their lower BMI, and possibly to lower intakes of calcium and protein. More studies are needed especially from non-European and contemporary populations to examine the generalisability of our findings and to explore possible heterogeneity by factors including age, sex, menopausal status, and BMI. Future work might benefit from examining possible biological pathways by investigating serum levels of vitamin D, vitamin B12, or IGF-1, or in assessing the possible roles of other nutrients that are abundant in animal-sourced foods.
Supplementary information
Additional file 1: Supplementary results. Fig. S1. Participant flow chart. Table S1. ICD codes for incident fractures. Table S2. Baseline characteristics by diet group and sex. Table S3. Food and nutrient intake by diet group and sex. Table S4. Risks of subtypes of main site fractures. Table S5-Sensitivity analyses. Table S6. Risks of hip fractures by age, sex, menopausal status, physical activity and BMI.
Acknowledgements
We thank all participants in the EPIC-Oxford cohort for their invaluable contribution.
Abbreviations
- BMD
Bone mineral density
- BMI
Body mass index
- EPIC
European Prospective Investigation into Cancer and Nutrition
- ICD
International Classification of Diseases
- IGF-1
Insulin-like growth factor-1
Authors’ contributions
TYNT and TJK conceived and designed the research question. TYNT analysed the data and wrote the first draft of the manuscript. All authors provided input on data analysis and interpretation of results. All authors revised the manuscript critically for important intellectual content, and read and approved the final manuscript. TYNT is the guarantor. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Funding
The work is supported by the UK Medical Research Council MR/M012190/1 and Wellcome Trust Our Planet Our Health (Livestock, Environment, and People, LEAP 205212/Z/16/Z). The funders had no role on the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Availability of data and materials
The data access policy for the EPIC-Oxford study is available via the study website (www.epic-oxford.org/data-access-sharing-and-collaboration/).
Ethics approval and consent to participate
The study has approval by a Multicentre Research Ethics Committee (Scotland A Research Ethics Committee). All participants provided written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information accompanies this paper at 10.1186/s12916-020-01815-3.
References
- 1.Odén A, McCloskey EV, Kanis JA, Harvey NC, Johansson H. Burden of high fracture probability worldwide: secular increases 2010–2040. Osteoporos Int. 2015;26:2243–2248. doi: 10.1007/s00198-015-3154-6. [DOI] [PubMed] [Google Scholar]
- 2.Tong TY, Key TJ, Sobiecki JG, Bradbury KE. Anthropometric and physiologic characteristics in white and British Indian vegetarians and nonvegetarians in the UK Biobank. Am J Clin Nutr. 2018;107:909–920. doi: 10.1093/ajcn/nqy042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ho-Pham LT, Nguyen ND, Nguyen TV. Effect of vegetarian diets on bone mineral density: a Bayesian meta-analysis. Am J Clin Nutr. 2009;90:943–950. doi: 10.3945/ajcn.2009.27521. [DOI] [PubMed] [Google Scholar]
- 4.Davey GK, Spencer EA, Appleby PN, Allen NE, Knox KH, Key TJ. EPIC-Oxford: lifestyle characteristics and nutrient intakes in a cohort of 33 883 meat-eaters and 31 546 non meat-eaters in the UK. Public Health Nutr. 2003;6:259–268. doi: 10.1079/PHN2002430. [DOI] [PubMed] [Google Scholar]
- 5.Sobiecki JG, Appleby PN, Bradbury KE, Key TJ. High compliance with dietary recommendations in a cohort of meat eaters, fish eaters, vegetarians, and vegans: results from the European Prospective Investigation into Cancer and Nutrition-Oxford study. Nutr Res. 2016;36:464–477. doi: 10.1016/j.nutres.2015.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Papier K, Tong TY, Appleby PN, Bradbury KE, Fensom GK, Knuppel A, et al. Comparison of major protein-source foods and other food groups in meat-eaters and non-meat-eaters in the EPIC-Oxford cohort. Nutrients. 2019;11:1–18. doi: 10.3390/nu11040824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bradbury KE, Tong TYN, Key TJ. Dietary intake of high-protein foods and other major foods in meat-eaters, poultry-eaters, fish-eaters, vegetarians, and vegans in UK Biobank. Nutrients. 2017;9:1317. doi: 10.3390/nu9121317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Spencer EA, Appleby PN, Davey GK, Key TJ. Diet and body mass index in 38 000 EPIC-Oxford meat-eaters, fish-eaters, vegetarians and vegans. Int J Obes. 2003;27:728–734. doi: 10.1038/sj.ijo.0802300. [DOI] [PubMed] [Google Scholar]
- 9.Tai V, Leung W, Grey A, Reid IR, Bolland MJ. Calcium intake and bone mineral density: systematic review and meta-analysis. BMJ. 2015;351:h4183. doi: 10.1136/bmj.h4183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bolland MJ, Leung W, Tai V, Bastin S, Gamble GD, Grey A, et al. Calcium intake and risk of fracture: systematic review. BMJ. 2015;351:h4580. 10.1136/bmj.h4580. [DOI] [PMC free article] [PubMed]
- 11.Yao P, Bennett D, Mafham M, Lin X, Chen Z, Armitage J, et al. Vitamin D and calcium for the prevention of fracture: a systematic review and meta-analysis. JAMA Netw Open. 2019;2:e1917789. doi: 10.1001/jamanetworkopen.2019.17789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Allen LH, Oddoye EA, Margen S. Protein-induced hypercalciuria: a longer term study. Am J Clin Nutr. 1979;32:741–749. doi: 10.1093/ajcn/32.4.741. [DOI] [PubMed] [Google Scholar]
- 13.Darling AL, Millward DJ, Torgerson DJ, Hewitt CE, Lanham-New SA. Dietary protein and bone health: a systematic review and meta-analysis. Am J Clin Nutr. 2009;90:1674–1692. doi: 10.3945/ajcn.2009.27799. [DOI] [PubMed] [Google Scholar]
- 14.Armstrong MEG, Cairns BJ, Banks E, Green J, Reeves GK, Beral V. Different effects of age, adiposity and physical activity on the risk of ankle, wrist and hip fractures in postmenopausal women. Bone. 2012;50:1394–1400. doi: 10.1016/j.bone.2012.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Karavasiloglou N, Selinger E, Gojda J, Rohrmann S, Kühn T. Differences in bone mineral density between adult vegetarians and nonvegetarians become marginal when accounting for differences in anthropometric factors. J Nutr. 2020;:1–6. 10.1093/jn/nxaa018. [DOI] [PubMed]
- 16.Appleby P, Roddam A, Allen N, Key T. Comparative fracture risk in vegetarians and nonvegetarians in EPIC-Oxford. Eur J Clin Nutr. 2007;61:1400–1406. doi: 10.1038/sj.ejcn.1602659. [DOI] [PubMed] [Google Scholar]
- 17.Ho-Pham LT, Vu BQ, Lai TQ, Nguyen ND, Nguyen TV. Vegetarianism, bone loss, fracture and vitamin D: a longitudinal study in Asian vegans and non-vegans. Eur J Clin Nutr. 2012;66:75–82. doi: 10.1038/ejcn.2011.131. [DOI] [PubMed] [Google Scholar]
- 18.Dash N, Kushwaha A. Stress fractures-a prospective study amongst recruits. Med J Armed Forces India. 2012;68:118–122. doi: 10.1016/S0377-1237(12)60021-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Appleby PN, Thorogood M, Mann JI, Key TJ. The Oxford Vegetarian Study: an overview. Am J Clin Nutr. 1999;70(3 Suppl):525S–531S. doi: 10.1093/ajcn/70.3.525s. [DOI] [PubMed] [Google Scholar]
- 20.Bingham SA, Gill C, Welch A, Day K, Cassidy A, Khaw KT, et al. Comparison of dietary assessment methods in nutritional epidemiology: weighed records v. 24 h recalls, food-frequency questionnaires and estimated-diet records. Br J Nutr. 1994;72:619. 10.1079/BJN19940064. [DOI] [PubMed]
- 21.Bingham S, Cassidy A, Cole TJ, Welch A, Runswick S, Black a E, et al. Validation of weighed records and other methods of dietary assessment using the 24 h urine nitrogen technique and other biological markers. Br J Nutr. 1995;73:531–50. 10.1079/BJN19950057. [DOI] [PubMed]
- 22.Bingham SA, Gill C, Welch A, Cassidy A, Runswick SA, Oakes S, et al. Validation of dietary assessment methods in the UK arm of EPIC using weighed records, and 24-hour urinary nitrogen and potassium and serum vitamin C and carotenoids as biomarkers. Int J Epidemiol. 1997;26(Suppl 1):S137–S151. doi: 10.1093/ije/26.suppl_1.s137. [DOI] [PubMed] [Google Scholar]
- 23.Ministry of Agriculture Fisheries and Food . Food portion sizes. 2. London: Her Majesty’s Stationary Office; 1993. [Google Scholar]
- 24.Holland B, Welch A, Unwin I, Buss D, Paul A, Southgate DAT. McCance and Widdowson’s the composition of foods. 5. Cambridge: Royal Society of Chemistry; 1991. [Google Scholar]
- 25.Townsend P. Poverty in the United Kingdom: a survey of household resources and standards of living. London, UK; 1979.
- 26.Wareham NJ, Jakes RW, Rennie KL, Schuit J, Mitchell J, Hennings S, et al. Validity and repeatability of a simple index derived from the short physical activity questionnaire used in the European Prospective Investigation into Cancer and Nutrition (EPIC) study. Public Health Nutr. 2003;6:407–413. doi: 10.1079/PHN2002439. [DOI] [PubMed] [Google Scholar]
- 27.Spencer EA, Appleby PN, Davey GK, Key TJ. Validity of self-reported height and weight in 4808 EPIC–Oxford participants. Public Health Nutr. 2002;5:561–565. doi: 10.1079/PHN2001322. [DOI] [PubMed] [Google Scholar]
- 28.Tong TYN, Appleby PN, Bradbury KE, Perez-Cornago A, Travis RC, Clarke R, et al. Risks of ischaemic heart disease and stroke in meat eaters, fish eaters, and vegetarians over 18 years of follow-up: results from the prospective EPIC-Oxford study. BMJ. 2019;366:l4897. doi: 10.1136/bmj.l4897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Public Health England. Government Dietary Recommendations: Government recommendations for food energy and nutrients for males and females About Public Health England. 2016. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/618167/government_dietary_recommendations.pdf.
- 30.Department of Health. Dietary reference values: a guide. 1991. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/743790/Dietary_Reference_Values_-_A_Guide__1991_.pdf.
- 31.White IR, Royston P, Wood AM. Multiple imputation using chained equations: issues and guidance for practice. Stat Med. 2011;30:377–399. doi: 10.1002/sim.4067. [DOI] [PubMed] [Google Scholar]
- 32.Lousuebsakul-Matthews V, Thorpe DL, Knutsen R, Beeson WL, Fraser GE, Knutsen SF. Legumes and meat analogues consumption are associated with hip fracture risk independently of meat intake among Caucasian men and women: the Adventist Health Study-2. Public Health Nutr. 2013;17:2333–2343. doi: 10.1017/S1368980013002693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Thorpe DL, Knutsen SF, Lawrence Beeson W, Rajaram S, Fraser GE. Effects of meat consumption and vegetarian diet on risk of wrist fracture over 25 years in a cohort of peri- and postmenopausal women. Public Health Nutr. 2008;11:564–572. doi: 10.1017/S1368980007000808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.De Laet C, Kanis JA, Odén A, Johanson H, Johnell O, Delmas P, et al. Body mass index as a predictor of fracture risk: a meta-analysis. Osteoporos Int. 2005;16:1330–1338. doi: 10.1007/s00198-005-1863-y. [DOI] [PubMed] [Google Scholar]
- 35.Moreland JD, Richardson JA, Goldsmith CH, Clase CM. Muscle weakness and falls in older adults: a systematic review and meta-analysis. J Am Geriatr Soc. 2004;52:1121–1129. doi: 10.1111/j.1532-5415.2004.52310.x. [DOI] [PubMed] [Google Scholar]
- 36.Warriner AH, Patkar NM, Curtis JR, Delzell E, Gary L, Kilgore M, et al. Which fractures are most attributable to osteoporosis? J Clin Epidemiol. 2011;64:46–53. doi: 10.1016/j.jclinepi.2010.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Appleby PN, Allen NE, Roddam AW, Key TJ. Physical activity and fracture risk: a prospective study of 1898 incident fractures among 34 696 British men and women. J Bone Miner Metab. 2008;26:191–198. doi: 10.1007/s00774-007-0806-4. [DOI] [PubMed] [Google Scholar]
- 38.Heaney RP, Gallagher JC, Johnston CC, Neer R, Parfitt AM, Whedon GD. Calcium nutrition and bone health in the elderly. Am J Clin Nutr. 1982;36:986–1013. doi: 10.1093/ajcn/36.5.986. [DOI] [PubMed] [Google Scholar]
- 39.Nordin BE. Calcium and osteoporosis. Nutrition. 1997;13:664–686. doi: 10.1016/S0899-9007(97)83011-0. [DOI] [PubMed] [Google Scholar]
- 40.Tucker KL. Vegetarian diets and bone status. Am J Clin Nutr. 2014;100(Suppl):329S–335S. doi: 10.3945/ajcn.113.071621. [DOI] [PubMed] [Google Scholar]
- 41.Key TJ, Appleby PN, Spencer EA, Roddam AW, Neale RE, Allen NE. Calcium, diet and fracture risk: a prospective study of 1898 incident fractures among 34696 British women and men. Public Health Nutr. 2007;10:1314–1320. doi: 10.1017/S1368980007696402. [DOI] [PubMed] [Google Scholar]
- 42.Barzel US, Massey LK. Excess dietary protein can adversely affect bone. J Nutr. 1998;128:1051–1053. doi: 10.1093/jn/128.6.1051. [DOI] [PubMed] [Google Scholar]
- 43.Kerstetter JE, O’Brien KO, Insogna KL. Dietary protein, calcium metabolism, and skeletal homeostasis revisited. Am J Clin Nutr. 2003;78(3 Suppl):584S–592S. doi: 10.1093/ajcn/78.3.584S. [DOI] [PubMed] [Google Scholar]
- 44.Bonjour J-P. The dietary protein, IGF-I, skeletal health axis. Horm Mol Biol Clin Investig. 2016;28:39–53. doi: 10.1515/hmbci-2016-0003. [DOI] [PubMed] [Google Scholar]
- 45.Locatelli V, Bianchi VE. Effect of GH/IGF-1 on bone metabolism and osteoporsosis. Int J Endocrinol. 2014;2014:1–25. doi: 10.1155/2014/235060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ohlsson C, Mellström D, Carlzon D, Orwoll E, Ljunggren Ö, Karlsson MK, et al. Older men with low serum IGF-1 have an increased risk of incident fractures: the MrOS Sweden study. J Bone Miner Res. 2011;26:865–872. doi: 10.1002/jbmr.281. [DOI] [PubMed] [Google Scholar]
- 47.Shams-White MM, Chung M, Du M, Fu Z, Insogna KL, Karlsen MC, et al. Dietary protein and bone health: a systematic review and meta-analysis from the National Osteoporosis Foundation. Am J Clin Nutr. 2017;105:1528–1543. doi: 10.3945/ajcn.116.145110. [DOI] [PubMed] [Google Scholar]
- 48.Fung TT, Meyer HE, Willett WC, Feskanich D. Protein intake and risk of hip fractures in postmenopausal women and men age 50 and older. Osteoporos Int. 2017;28:1401–1411. doi: 10.1007/s00198-016-3898-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Munger RG, Cerhan JR, Chiu BC. Prospective study of dietary protein intake and risk of hip fracture in postmenopausal women. Am J Clin Nutr. 1999;69:147–152. doi: 10.1093/ajcn/69.1.147. [DOI] [PubMed] [Google Scholar]
- 50.Langsetmo L, Shikany JM, Cawthon PM, Cauley JA, Taylor BC, Vo TN, et al. The association between protein intake by source and osteoporotic fracture in older men: a prospective cohort study. J Bone Miner Res. 2017;32:592–600. doi: 10.1002/jbmr.3058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Darling AL, Manders RJF, Sahni S, Zhu K, Hewitt CE, Prince RL, et al. Dietary protein and bone health across the life-course: an updated systematic review and meta-analysis over 40 years. Osteoporos Int. 2019;30:741–761. doi: 10.1007/s00198-019-04933-8. [DOI] [PubMed] [Google Scholar]
- 52.Crowe FL, Steur M, Allen NE, Appleby PN, Travis RC, Key TJ. Plasma concentrations of 25-hydroxyvitamin D in meat eaters, fish eaters, vegetarians and vegans: results from the EPIC-Oxford study. Public Health Nutr. 2011;14:340–346. doi: 10.1017/S1368980010002454. [DOI] [PubMed] [Google Scholar]
- 53.Ma J, Giovannucci E, Pollak M, Chan JM, Gaziano JM, Willett W, et al. Milk intake, circulating levels of insulin-like growth factor-I, and risk of colorectal cancer in men. JNCI J Natl Cancer Inst. 2001;93:1330–1336. doi: 10.1093/jnci/93.17.1330. [DOI] [PubMed] [Google Scholar]
- 54.Gilsing AMJ, Crowe FL, Lloyd-Wright Z, Sanders TAB, Appleby PN, Allen NE, et al. Serum concentrations of vitamin B12 and folate in British male omnivores, vegetarians and vegans: results from a cross-sectional analysis of the EPIC-Oxford cohort study. Eur J Clin Nutr. 2010;64:933–939. doi: 10.1038/ejcn.2010.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Popp KL, Hughes JM, Martinez-Betancourt A, Scott M, Turkington V, Caksa S, et al. Bone mass, microarchitecture and strength are influenced by race/ethnicity in young adult men and women. Bone. 2017;103:200–208. doi: 10.1016/j.bone.2017.07.014. [DOI] [PubMed] [Google Scholar]
- 56.Barrett-Connor E, Siris ES, Wehren LE, Miller PD, Abbott TA, Berger ML, et al. Osteoporosis and fracture risk in women of different ethnic groups. J Bone Miner Res. 2005;20:185–194. doi: 10.1359/JBMR.041007. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Supplementary results. Fig. S1. Participant flow chart. Table S1. ICD codes for incident fractures. Table S2. Baseline characteristics by diet group and sex. Table S3. Food and nutrient intake by diet group and sex. Table S4. Risks of subtypes of main site fractures. Table S5-Sensitivity analyses. Table S6. Risks of hip fractures by age, sex, menopausal status, physical activity and BMI.
Data Availability Statement
The data access policy for the EPIC-Oxford study is available via the study website (www.epic-oxford.org/data-access-sharing-and-collaboration/).