Abstract
Objective:
To compare the effects of Global Postural Reeducation (GPR) with Manual Therapy (MT) in participants with chronic nonspecific neck pain (NP).
Methods:
Pre- and post-treatment analysis of cross-over data from an RCT was done. Seventy-eight subjects with chronic nonspecific NP aged 18 to 80 years completed the trial. The group who had received GPR crossed-over to MT and the previous MT group received GPR for 9 sessions once or twice a week. Measures were assessed at pre-treatment and post-treatment. Outcome measures included pain intensity [Visual Analogue Scale (VAS)], disability (Neck Disability Index), cervical Range of Motion (ROM), and kinesiophobia [Tampa Scale of Kinesiophobia (TSK)].
Results:
GPR targeted to crossed-over participants produced greater improvements in pain [Diff=-8.6; 95%CI=(-13.3; -3.8)], disability [Diff=-1.5; 95%CI=-2.8; -0.1], kinesiophobia [Diff=-1.8; 95%CI=(-3.2; -0.3)], and flexion/extension neck ROM [Diff=5.6; 95%CI=(1.8; 9.3)] at post-treatment compared to the MT group. When evaluating clinical improvement, by means of Minimal Clinically Important Differences, we found that GPR relevantly reduced neck disability with respect to MT [OR=2.13; 95% CI=(1.05; 4.35)], whereas the improvement of pain did not differ between groups [OR=1.84; 95%CI=0.85; 3.99)].
Conclusions:
These results within the crossed-over group confirm previous findings from an RCT with the same sample. Sequence of treatment (GPR-to-MT vs MT-to-GPR) does not seem to weaken the greater effects of GPR compared to MT approach for chronic NP. Our findings suggest that GPR can induce hypoalgesic effects, reduce disability and kinesiophobia, and improve flexion/extension in neck ROM.
Key words: Posture, manual therapy, cervical pain, exercise, disability
Abstract
«La Rieducazione Posturale Globale in pazienti con dolore cervicale cronico non specifico: analisi cross-over di uno studio randomizzato controllato».
Obiettivo:
Sono stati confrontati gli effetti della Rieducazione Posturale Globale (RPG) e di un intervento di Terapia Manuale (TM) in partecipanti con dolore cervicale cronico non specifico.
Metodi:
È stata effettuata una analisi pre-trattamento e post-trattamento dei dati cross-over da un RCT. Settantotto soggetti, affetti da dolore cervicale non specifico cronico, con età compresa tra 18 e 80 anni, hanno completato lo studio. Il gruppo che aveva ricevuto RPG è passato alla TM e il precedente gruppo trattato con TM ha ricevuto RPG per 9 sedute, una o due volte alla settimana. Le misure sono state valutate pre-trattamento e post-trattamento. Le misure di esito hanno incluso l ’intensità del dolore [Scala Analogo-Visiva (VAS)], la disabilità (Neck Disability Index), il range di movimento cervicale (ROM) e la chinesiofobia [Tampa Scale of Kinesiophobia (TSK)].
Risultati:
La RPG effettuata sui partecipanti ha prodotto maggiori miglioramenti nel dolore [Difference (Diff)= -8.6; 95% CI= (-13.3; -3.8)], nella disabilità [Diff=-1.5; 95% CI=(-2.8; -0.1)], nella chinesiofobia (Diff=-1,8; 95% CI=(-3,2; -0,3)], e nella flesso/estensione cervicale [Diff=5,6; 95% CI=(1,8; 9,3)] rispetto al gruppo che ha ricevuto TM. Nel valutare il miglioramento clinico mediante le “Minimal Clinically Important Differences”, è risultato che la RPG abbia maggiormente ridotto in modo rilevante la disabilità cervicale rispetto alla MT [OR=2.13; 95% CI=(1.05; 4.35)], mentre il miglioramento del dolore non differiva tra i gruppi [OR=1,84, 95% CI=(0,85, 3,99)].
Conclusioni:
Questi risultati all’interno del gruppo incrociato confermano i precedenti risultati di un RCT con lo stesso campione. La sequenza di trattamento (RPG-poi-TM vs TM-poi-RPG) non sembra indebolire gli effetti maggiori della RPG rispetto all’approccio TM per il dolore cervicale cronico. I nostri risultati suggeriscono che la RPG può indurre effetti ipoalgesici, ridurre la disabilità e la chinesiophobia e migliorare la flesso/estensione nell’ambito del ROM cervicale.
Introduction
Neck pain (NP) is a common cause of pain and disability with serious consequences for employees and high costs for employers and society (13). The prevalence of recurring NP is approximately 15% in the adult population (17). The increasing use of electronic devices with viewing screens, such as smart phones and personal computers, for about 8 hours per day on average, appears to influence neck muscle activity at rest and when lifting (15). Furthermore, the forward head posture associated with thoracic kyphosis indirectly affects cervical flexion and rotational range of motion (ROM) (28). Nevertheless, the exact relationship between posture and NP is unresolved (24).
Ergonomic interventions (26), including adjustments of the workplace station and postural correction, have been demonstrated to be effective in reducing NP on some work conditions (21). Many anatomical structures are involved in NP, but zygapophyseal joints have been suggested as sources of pain in symptomatic neck conditions. NP is commonly treated with manual therapy (MT) (10). Manipulation, mobilization, stretching techniques, massage, and fascial manipulation or release have been recommended by various physical therapy clinical guidelines and reviews for treatment of patients with NP (1, 2, 9, 11, 30, 36).
An alternative conservative treatment for NP is Global Postural Reeducation (GPR), a therapeutic strategy developed by Philippe-Emmanuel Souchard (34). It is based on a central concept that postural muscles are organized to act in concert with each other as “muscle chains” located anterior and posterior to the spine (7). It has been hypothesized that specific clinical presentations are caused by “muscle chain retractions” associated with lower back or cervical pain (37). GPR aims to stretch and elongate these muscles which are in a shortened state by using prolonged active postures and by enhancing contraction of the antagonist muscles to promote improved muscle balance and postural symmetry (2). Some studies support GPR’s clinical effectiveness in treating patients with different musculoskeletal disorders and impairments (2, 5, 22, 35, 38).
Recently, a randomized controlled trial (RCT) demonstrated that GPR treatment addressed to the cervical area induced hypoalgesic effects and disability reduction (4, 25). This original paper was a superiority trial in which we demonstrated the effectiveness of GPR vs MT. Nevertheless, we know that every RCTs could be influenced by confounding covariates (23). In this case, these covariates could have been the difference found between the two samples at the baseline, or the difference among the physiotherapists involved in the treatment activities. In fact, each physiotherapist approaches a patient in a unique manner with a different expertise and so therapeutic results may be influenced by these factors and not by the method adopted. Moreover, other covariates could have influenced the results, such as the different settings in which patients were treated. Finally, it is possible that specific patient characteristics, including the individual’s expectations for treatment, belief in the therapist’s competence, and other psycho-social factors could influence outcomes. A crossover trial helps to account for these factors and minimize these sources of bias.
The aim of this study is to compare the effectiveness of GPR versus MT interventions in a crossover trial, treating subjects who previously received MT with GPR, and vice-versa.
Methods
We conducted a crossover study, approved by the Independent Ethics Committee of Sant’Orsola-Malpighi hospital, Bologna (Italy) and registered in Clinical Trials database (NCT01947231). This is a follow-up study of the original report previously published in Physical Therapy Journal, in which also the explanation of sample size calculation is comprised (23).
All participants signed an informed consent, including commitment to continue participation in the crossover portion of the study, and all procedures were conducted according to the Declaration of Helsinki. Participants with NP not related to specific conditions and lasting at least for 3 months had been randomly assigned to an experimental or control group using simple randomization with a random number generator. Allocation was concealed by generating each allocation after enrollment.
Data were collected at four points in time: at Time 0 (pre-treatment), at Time 1 (immediately after the first treatment period, i.e., 9 sessions of GPR or MT interventions); at Time 2 (after the washout period of 6-months), and finally, at Time 3 (after the second treatment period, again 9 sessions of crossed-over interventions). Outcome measures were administered at each Time by an assessor blinded to the participants’ allocated group.
Participants
Eligible participants were all consecutive patients addressed to the Occupational Unit of S.Orsola-Malpighi hospital for NP from September 2013 to April 2014. Inclusion criteria for this study were age between 18 and 80 years of both genders, and able to read and speak Italian. Exclusion criteria were acute or subacute neck pain (lasting less than 3 months), specific cause of NP (e.g. systemic, rheumatic, neuromuscular diseases), central or peripheral neurological signs, cognitive impairment, spinal surgery, or physical therapy treatments in the last 6 months prior to baseline assessment. Moreover, during the entire trial period participants were excluded if they suffered for adverse effects or relevant worsening of symptoms or if they took drugs or received other therapies for their NP. The independent assessor during Times 1, 2, and 3 screened these further exclusion criteria.
Interventions
Participants were treated once or twice a week as determined by assignment in this single-blind, randomized, cross-over design study.
Global Postural Reeducation
This intervention included two lying postures from the eight different therapeutic postures of the GPR method (34): the supine posture with leg extension, which progressively stretches the anterior muscle chain (figure 1a and 1b), and the supine posture with hip flexion, which stretches the posterior muscle chain (figure 2a and 2b). The first therapeutic posture is characterized by a progression from the flexion to the extension of both hips and knees, whereas in the second posture the progression includes hip flexion and knee extension.
Figure 1a.
Supine posture with leg extension progression: anterior muscle chain stretching. Starting position
Figure 1b.
Supine posture with leg extension progression: anterior muscle chain stretching. Final position
Figure 2a.
Supine posture with leg flexion progression: posterior muscle chain stretching. Starting position
Figure 2b.
Supine posture with leg flexion progression: posterior muscle chain stretching. Final position
During GPR treatment, manual traction was applied to both lumbar and cervical areas, and isometric contractions of the stiff muscles were elicited to induce post-isometric relaxation (16). Each posture was practiced for about 20 minutes. At the end of each session, subjects were requested to correct their standing posture and to perform simple cervical movements maintaining the corrected posture for a total of ten minutes. The correct posture was related not only to the neck region (e.g. straightening a forward head posture), but also to the entire spine and the pelvis (e.g. correcting lumbar lordosis or pelvic tilt). The final part of each session aimed to facilitate the integration of the postural correction into daily functional activities (2, 25).
Manual Therapy
This intervention included a standardized combination of different therapeutic techniques. Axial cervical general traction and mobilization of muscle fascia (3) were performed for at least 30 minutes. Then, passive mobilization was applied to the cervical spine using Maitland’s technique (14, 40). Therapeutic massage was applied to neck and shoulders areas as the final technique for approximately fifteen minutes (25).
GPR intervention was applied by physical therapists trained in this method; MT was performed by physical therapists expert in myofascial and passive techniques. Both GPR and MT interventions lasted 9 sessions, one hour each, with one-to-one supervision.
Both treatments included home exercises, aiming to improve the therapeutic effects of supervised sessions. Furthermore, all subjects received an educational booklet, containing some practical instruction for subjects to prevent NP and correctly manage their cervical area during the different daily activities.
Interventions crossover started 6 months after the end of first treatment sessions: the group which had received GPR in the previous study was crossed-over to receive an MT program, and vice-versa.
Outcome measures
The primary outcomes of this study were pain and disability. These measures are the most relevant for physical therapy practice in chronic pain, as stated by the International Association for the Study of Pain in its “Curriculum Outline on Pain for Physical Therapy” (33).
Mean rates of perceived pain during the last 24 hours were measured by using a 0-100 Visual Analogue Scale (VAS), while cervical disability was rated using the Italian version of the Neck Disability Index (NDI-I) (19). To evaluate the Minimal Clinically Important Difference (MCID) for these outcome measures, we adopted 28% reduction or 17 points reduction in NP measured with a numerical VAS, and 5 points reduction on a 50-points NDI-I (27).
Secondary outcomes were: kinesiophobia, perceived effect of the intervention, patient satisfaction, and cervical ROM. Kinesiophobia was assessed by the 13-Item Italian version of the Tampa Scale of Kinesiophobia (TSK), which provides a measure of fear of movement or injury (20). The Italian version comprises two subscales: TSK 1 – Activity Avoidance, and TSK 2-Harm (20).
Perceived effect of the intervention was assessed with the Global Perceived Effect Questionnaire (GPE), a 5-point Likert-type scale evaluating the subjective self-reported improvement or deterioration after the intervention. GPE is widely used in the physical therapy literature (29). Patient satisfaction was assessed by the Italian version of the Physical Therapy Patient Satisfaction Questionnaire [PTPSQ-I] (37, 38), which has demonstrated good psychometric properties and a 2-factor structure, related to perceived “Overall Experience” and “Professional Impression”.
Finally, cervical ROM was measured in sitting posture with an inclinometer (CROM – Deluxe model, Performance Attainment, Lindstrom, MN, USA). CROM consists of two gravity-dependent goniometers and one compass dial and a head-mounted frame allowing measurement of ROM in three planes (flexion/extension, lateral flexion, rotation). The CROM has demonstrated good reliability in different orthopedic disorders of the cervical spine (42) and good concurrent validity for active ROM in subacute NP (41).
All outcome measures were captured at baseline (Time 0), immediately after the first intervention (Time 1), at 6-months post-intervention (Time 2) (25) and after cross-over treatment (Time 3) by an assessor blinded to group assignment. The sequence of testing for the outcome measures was randomized among patients. The trial was designed according to the CONSORT publishing guidelines.
Statistical analysis
Across the four time points of measurement, we considered differences from baseline scores (T1 – T0 for the first arm and T3 – T2 for the second arm) as the response variables for each outcome, resulting in two treatments, two sequences, and two periods of cross-over. Our cross-over design was uniform within sequences, as each treatment appeared the same number of times in each sequence, and uniform within periods, as each treatment appeared the same number of times in each period. Therefore, we were able to isolate the period and sequence effects from the treatment effect. To determine the effect of treatment on outcomes, we used repeated measures for linear (i.e. assuming a Gaussian distribution of the outcome) mixed models considering outcome change from baseline as the dependent variable (12). Fixed covariates used in the statistical models were Period, to test equality of period effects (first arm vs second arm of the cross-over); Sequence, to test equality of carry-over effects between the two groups of the study (GPR-MT vs MT-GPR); and Treatment, to test equality of treatment effects (GPR vs MT). A Gaussian-distributed random effect term, specific for each patient, was also introduced in the linear predictor of the model, making use of a compound symmetry measurements covariance structure.
The main hypothesis of interest was the treatment effect (between-groups differences). The between-groups differences were the estimated mean differences in scores (with 95%CI) between the two treatments. All fixed covariates effects were tested for statistical significance by means of F tests.
Additionally, the baseline outcome value was used as a fixed covariate, in order to better explain variability in the outcome and increase precision of the model estimates. For the first arm of the cross-over, the score at T0 was used as baseline value, while for the second arm the score at T2 was used. Both unadjusted between-groups differences and baseline-adjusted between-groups differences were reported. Validity of the linear mixed models fit was assessed: adherence to the Gaussian distribution and absolute magnitude of models’ residuals were checked.
Moreover, in order to assess the clinical significance of the effect of treatment on outcomes, we classified each patient as having (or not) reached the MCID, for each of the two primary outcomes and for each of the two arms of the cross-over (6).
We estimated repeated measures for logistic (i.e. assuming a Bernoulli distribution for the outcome and using a logit link function) mixed models in order to obtain odds ratios (OR) with 95% confidence intervals (CI) for the difference between GPR and MT in the proportion of patients who reached MCID. As in linear mixed models, covariates used were Period effect, Sequence effect and Treatment effect. Again, patient-specific random effects were given a Gaussian distribution and a compound symmetry covariance structure was assumed. Baseline-adjusted ORs with 95%CI were also calculated (12). All analyses were performed with SAS/STAT 9.3 software (SAS Institute, Cary, NC, USA) at 0.05 significance level .
Results
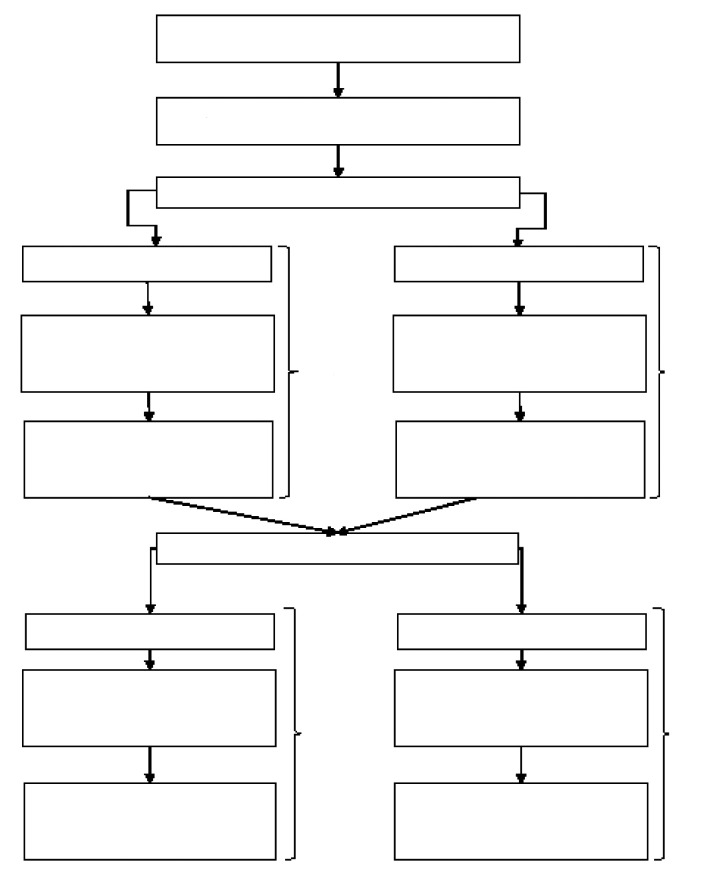
The data reported in this study are a follow-up analysis of 87 participants with chronic nonspecific NP, 78 of whom completed the randomized cross-over to investigate the effects of 9 sessions of GPR or MT, on NP. There were 94 patients enrolled in the initial study and randomized to a treatment group. One patient assigned to the GPR→MT sequence dropped out before the first visit, leaving 93 subjects in our initial sample (46 in the GPR-to-MT sequence and 47 in the MT-to-GPR sequence). Outcome measurements were completed on 89 subjects at Time 1 (44 in the GPR-to-MT group and 45 in the MT-to-GPR group), on 87 subjects at Time 2 (43 in GPR-to-MT and 44 in MT-to-GPR), while 78 subjects were examined at Time 3 (40 in GPR-to-MT and 38 in MT-to-GPR). No relevant differences in baseline characteristics were found between drop out patients and patients that completed the cross-over (data not shown). No important adverse events or side effects happened in each intervention group. Figure 3 provides a flow diagram of subject recruitment and retention through the study.
Figure 3.
Flow chart
Table 1 shows the numerical results for all outcomes at different visits (T0, T1, T2, and T3), for each treatment sequence. More specifically, results concerning pain intensity, neck disability, kinesiophobia, and cervical ROM are included.
Table 1.
Mean (SD) for outcomes at all study visits for each sequence of treatments
| Outcome | Groups | |||||||
| Baseline (T0) | T1 | T2 | T3 | |||||
| GPR-MT (n=46) | MT-GPR (n=47) | GPR-MT (n=44) | MT-GPR (n=45) | GPR-MT (n=44) | MT-GPR (n=43) | GPR-MT (n=40) | MT-GPR (n=38) | |
| VAS | 47.0 (24.1)> |
42.0 (21.0) |
13.5 (13.2) |
24.2 (20.6) |
35.2 (23.8) |
41.1 (24.7) |
23.6 (19.8) |
19.2 (19.4) |
| NDI-I |
15.9 (7.0) |
14.6 (5.9) |
7.8 (6.4) |
9.0 (5.7) |
12.9 (7.0) |
15.0 (6.0) |
9.1 (6.7) |
8.5 (5.5) |
| TSK | 30.7 (7.1) |
27.8 (7.9) |
26.5 (7.4) |
26.3 (5.8) |
28.4 (7.6) |
29.3 (6.9) |
26.2 (6.7) |
24.2 (6.8) |
| TSK 1 | 12.1 (3.5) |
12.0 (3.9) |
10.6 (3.6) |
10.9 (3.0) |
12.0 (3.9) |
12.7 (3.6) |
10.6 (3.4) |
10.3 (3.3) |
| TSK 2 | 18.5 (4.4) |
15.8 (4.6) |
15.8 (4.3) |
15.3 (3.3) |
16.4 (4.2) |
16.7 (3.9) |
15.6 (3.9) |
13.9 (4.1) |
| ROM Flexion and Extension | 84.2 (22.5) |
90.7 (25.9) |
105.3 (22.2) |
105.0 (21.1) |
95 (23.1) |
91.6 (24.5) |
103.3 (21.6) |
108.1 (23.7) |
| ROM Lateral Flexion | 57.7 (18.1) |
64.7 (19.9) |
72.0 (20.8) |
74.0 (17.8) |
63.6 (17.1) |
62.4 (17.1) |
71.6 (19.1) |
69.9 (19.0) |
| ROM Rotation | 106.7 (16.9) |
106.0 (17.8) |
123.7 (18.0) |
121.9 (18.1) |
110.5 (18.5) |
111.3 (17.0) |
122.7 (16.2) |
119.7 (22.5) |
GPR=Global Postural Reeducation group, MT=Manual Therapy group, VAS=Visual Analog Scale, NDI-I=Neck Disability Index, TSK=Tampa Scale of Kinesiophobia, TSK 1=TSK activity avoidance subscale, TSK 2=TSK harm subscale, ROM=Range of Motion.
The treatment performed on each group in each period is indicated in bold.
Table 2 shows the absolute and percentage number of patients who reached the MCID at T1 and at T3. It appears that higher number of patients receiving GPR treatment reached MCID for pain (67 vs 59) and disability (56 vs 41), in both treatments periods.
Table 2.
Number (%) of patients who reached MCID in primary outcomes for each sequence of treatments
| Outcome | Groups | |||
| T1 | T3 | |||
| GPR-MT (n=44) | MT-GPR (n=45) | GPR-MT (n=40) | MT-GPR (n=38) | |
| VAS | 38 (86.4%) |
31 (68.9%) |
28 (70.0%) |
29 (76.3%) |
| NDI-I | 32 (72.7%) |
21 (46.7%) |
20 (50.0%) |
24 (63.2%) |
GPR=Global Postural Reeducation group, MT=Manual Therapy group, VAS=Visual Analog Scale, NDI-I=Neck Disability Index.
The treatment performed on each group in each period is indicated in bold.
Our main hypothesis of interest was the treatment effect (between-groups differences).
Table 3 shows the differences between groups for all outcomes, also adjusted for baseline score, to account for the significant difference between groups concerning disability level. Statistically significant baseline-adjusted between-groups differences were found for VAS (Diff=-8.6; 95% CI=[-13.3; -3.8]), NDI-I (Diff=-1.5; 95% CI=[-2.8; -0.1]), TSK (Diff=-1.8; 95% CI=[-3.2 ; -0.3]), TSK2 (Diff=-1.4; 95% CI=[-2.2 ; -0.5]), ROM flexion and extension (Diff=5.6; 95% CI=[1.8 ; 9.3]), while the same did not happen for TSK1(Diff=-0.4; 95% CI=[-1.2; 0.4]), ROM lateral flexion (Diff=2.0; 95% CI=[-1.3; 5.3]) and ROM rotation (Diff=-0.8; 95% CI=[-4.2; 2.5]). Moreover, table 3 shows Odds Ratios for reaching MCID values in primary outcomes. Here, patients in the GPR group were more likely to reach NDI-I MCID (OR=2.13; 95% CI=[1.05; 4.35]), while the same was not true for VAS MCID (OR=1.84; 95% CI=[0.85; 3.99]).
Table 3.
Mean (95% CI) difference between groups, mean (95% CI) difference between groups adjusted for baseline score, difference in proportion (95% CI) of patients who reached MCID and difference in proportion (95% CI) of patients who reached MCID adjusted for baseline score
| Outcome | Difference between groups | Difference between groups, adjusted for baseline score | Difference in proportion of patients who reach MCID | Difference in proportion of patients who reach MCID, adjusted for baseline score |
| T1 minus Baseline | T1 minus Baseline | Odds Ratio | Odds Ratio | |
| GPR minus MT | GPR minus MT | GPR vs MT | GPR vs MT | |
| VAS | -12.4 (-19.7; -5.1) |
-8.6 (-13.3; -3.8) |
1.99 (0.94; 4.19) |
1.84 (0.85; 3.99) |
| NDI-I | -2.2 (-3.9; -0.5) |
-1.5 (-2.8; -0.1) |
2.29 (1.20; 4.39) |
2.13 (1.05; 4.35) |
| TSK | -2.5 (-4.3; -0.6) |
1.8 (-3.2; -0.3) |
- | - |
| TSK 1 | -0.5 (-1.5; 0.5) |
-0.4 (-1.2; 0.4) |
- | - |
| TSK 2 | -2.0 (-3.1; -0.9) |
-1.4 (-2.2; -0.5) |
- | - |
| ROM Flexion and Extension | 7.2 (2.8; 11.6) |
5.6 (1.8; 9.3) |
- | - |
| ROM Lateral Flexion | 2.7 (-0.8; 6.3) |
2.0 (-1.3; 5.3) |
- | - |
| ROM Rotation | -0.9 (-4.7; 2.9) |
-0.8 (-4.2; 2.5) |
- | - |
GPR=Global Postural Reeducation group, MT=Manual Therapy group, VAS=Visual Analog Scale, NDI-I=Neck Disability Index, TSK=Tampa Scale of Kinesiophobia, TSK 1=TSK activity avoidance subscale, TSK 2=TSK harm subscale, ROM=Range of Motion
Table 4 shows the results of the F tests on the linear mixed model’s components. Treatment factors in baseline-adjusted mixed models were significant for VAS, NDI-I, TSK, TSK-2 and ROM flexion and extension (p=0.0006, p=0.0358, p=0.0187, p=0.0025, p=0.0039, respectively) according to the associated F tests.
Table 4.
F tests (p-value) on the linear mixed model’s components
| Outcome | Effect | |||
| Treatment | Time | Sequence | Baseline score | |
| VAS | 12.88 (0.0006) |
2.74 (0.1022) |
1.36 (0.2461) |
173.38 (<0.0001) |
| NDI-I | 4.57 (0.0358) |
3.12 (0.0814) |
0.08 (0.7717) |
69.56 (<0.0001) |
| TSK | 5.77 (0.0187) |
0.58 (0.4492) |
0.23 (0.6345) |
71.36 (<0.0001) |
| TSK 1 | 0.91 (0.3420) |
0.74 (0.3930) |
0.01 (0.9132) |
84.67 (<0.0001) |
| TSK 2 | 9.77 (0.0025) |
0.24 (0.6223) |
0.44 (0.5072) |
67.06 (<0.0001) |
| ROM Flexion and Extension | 8.89 (0.0039) |
5.24 (0.0249) |
0.04 (0.8501) |
48.71 (<0.0001) |
| ROM Lateral Flexion | 1.46 (0.2308) |
8.08 (0.0058) |
2.17 (0.1445) |
10.42 (0.0019) |
| ROM Rotation | 0.25 (0.6172) |
10.32 (0.0019) |
0.98 (0.3245) |
20.09 (<0.0001) |
GPR=Global Postural Reeducation group, MT=Manual Therapy group, VAS=Visual Analog Scale, NDI-I=Neck Disability Index, TSK=Tampa Scale of Kinesiophobia, TSK 1=TSK activity avoidance subscale, TSK 2=TSK harm subscale, ROM=Range of Motion
The sequence of the cross-over (GPR-to-MT vs MT-to-GPR) was not statistically significant (all, p>0.05), while all baseline score factors were (all, p<0.0001), according to F tests (table 4). Time or period factors (first administration vs crossed-over second administration of the intervention) were only significant for the three ROM outcomes (p=0.0249, p=0.0058 and p=0.0019, respectively).
Adherence to the Gaussian distribution of the linear mixed model residuals, measured with Shapiro-Wilk p-value (p>0.05), was equal to 0.9255 for VAS, 0.0082 for NDI, 0.8636 for TSK, 0.4466 for TSK1, 0.5150 for TSK2, 0.1365 for ROM flexion and extension, 0.2365 for ROM lateral flexion and 0.0162 for ROM rotation (results not shown in tables).
Table 5 shows the results of the F tests on the logistic mixed model’s components. Treatment factors in baseline-adjusted mixed models were significant for NDI-I (p=0.0375). Sequence factors and Time factors were not significant, while all baseline scores were for both primary outcomes (p<0.0001).
Table 5.
F tests (p-value) on the logistic mixed model’s components
| Outcome | Effect | |||
| Treatment | Time | Sequence | Baseline score | |
| VAS | 4.49 (0.0375) |
0.00 (0.9793) |
1.05 (0.3088) |
20.74 (<0.0001) |
| NDI-I | 2.50 (0.1180) |
0.22 (0.6385) |
0.98 (0.3254) |
8.24 (0.0053) |
GPR=Global Postural Reeducation group, MT=Manual Therapy group, VAS=Visual Analog Scale, NDI-I=Neck Disability Index, TSK=Tampa Scale of Kinesiophobia, TSK 1=TSK activity avoidance subscale, TSK 2=TSK harm subscale, ROM=Range of Motion
Discussion
The current follow-up analysis found a difference in the effects of the treatment (GPR vs MT) on pain, disability, kinesiophobia, and flexion/extension neck ROM, confirming the findings of a previous RCT (25). Neither the period (first administration vs crossed-over second administration of the intervention), nor the sequence of the cross-over (GPR-to-MT vs MT-to-GPR) significantly affected the results. Treatment effect (GPR vs MT), measured with the between-groups difference adjusted for baseline score appeared as substantial as our previous study (23).
This cross-over design was helpful in accounting for the influence of some confounding covariates and to balance our analyses as each patient served as his or her own control. One of the most important covariates to address was the difference found at baseline in the original study between the two groups in a secondary outcome, kinesiophobia, as measured by the TSK-2. Crossing-overall subjects after the washout time reduced potential bias from this covariate. We similarly accounted for the differences among the physiotherapists providing the treatment, the different settings in which the two groups of patients were treated, as well as participant’s expectations, beliefs and other psychosocial variables which may have been different in each patient and also could have influenced the outcome.
Notably, we observed a significant effect of time (first vs. second cycle of treatment, regardless of the type of treatment delivered) on improving cervical ROM, suggesting that both therapeutic approaches, despite some different elements, may provide similar results with respect to the amount of active ROM. As a consequence, we can expect a significant ROM improvement after a first sequence of 9 physical therapy sessions, and fewer changes after a second sequence delivered 6 months apart in subjects with chronic NP and restricted cervical ROM, irrespective of treatment approach.
From a clinical point-of-view, GPR may be an interesting option to treat chronic spinal pain. This non-invasive procedure is safe, and can be easily integrated with home exercises. Some studies indicate the effectiveness of GPR and static stretching exercises in reducing pain and improving ROM and quality of life in conditions other than chronic NP, such as ankylosing spondylitis and temporomandibular joint disorders (18).
GPR has been shown to produce greater improvements than MT on pain, disability, kinesiophobia, and flexion/extension neck ROM, although it is not clear what might account for this phenomenon. In many aspects, these two different treatments have the potential to produce similar outcomes. Therefore, we would hypothesize that the difference might lie both in what is provided to the patient, and in how the treatment is delivered.
MT as provided in our study did not require the patient’s active engagement in the change to be produced. Thus, it might be less effective in promoting behavioral change such as exhibiting improved postural alignment during the performance of daily activities. In contrast, GPR actively engages a patient in eliciting and maintaining an improved postural alignment, incorporating a practice component at the end of every treatment session. Such active engagement presumably added an element of motor learning that could enhance behavioral change that was not part of MT as it was provided in our two studies. As noted by Sarig Bahat et al, kinematic training such as active and quick head movements and fine head movement control and stability significantly improved neck disability, cervical ROM, and head movement velocity and accuracy in chronic NP (31). Moreover, as observed by Vernon et al. in chronic whiplash sufferers, self-ratings of disability, fear-avoidance beliefs, and nonorganic pain behaviors significantly influence the presentation of impairment with respect to their ranges of neck motion (39). Concerning the clinical relevance of these results, we observed a higher proportion of subjects whose scores reached the adopted MCIDs for pain (from a minimum of 68.9% for MT to a maximum of 86.4% for GPR) than for disability (from a minimum of 46.7% for MT to a maximum of 72.7% for GPR). A larger proportion of subjects had scores reaching the target MCIDs after the first 9 sessions of treatment, regardless of the group.
In general, we observed a higher number of patients whose scores reached the target MCIDs for pain and disability after GPR compared to MT. Nevertheless, the odds ratios for reaching MCID values were significantly different between groups only for disability. This results may be related to a better effect induced by GPR concerning the active involvement in daily living activities, as explained before. Furthermore, the low-moderate level of perceived pain at baseline may have reduced the odds of relevant pain changing during time, as observed in low back pain (32).
Limitations
Some limitations of this study are typical of a crossover design. First of all, the order in which GPR and MT were administrated might influence the outcomes. Nevertheless, statistical analysis demonstrated that this issue was not relevant in our sample. Secondly, we cannot exclude a carryover effect, especially the impact that a therapy might have on a particular outcome after cessation period. Moreover, there might be a learning effect as a consequence of the first therapy received, that could have an impact in the development of the second therapy. To reduce these limits, we chose a long washout period (6 months).
A lack of blinding of the participants and therapists may have been a source of bias in this study. Presence of drop-out patients was also a potential limitation, since we performed a per-protocol analysis. However, we didn’t find relevant differences in baseline characteristics of drop-out patients, compared to patients who completed the study. Moreover, only 1 drop-out patient left the study for reasons related to the treatment and 6 drop-out patients left for their health status. Another limitation is that randomization did not lead to completely homogeneous groups.
Patient and investigator related factors are interrelated (e.g., therapists’ beliefs can influence patients’ expectations of benefit) and have been shown to be influential in clinical trials of interventions for pain. An important limitation of our study was also the fact that we did not measure long-term follow-up or passive cervical ROM. Finally, inclusion criteria included a diagnosis of chronic non-specific NP, regardless of the presence of cognitive or behavioral dysfunctions, which may have affected group characteristics.
Conclusions
The results of this randomized cross-over trial suggest that GPR applied to the cervical area induces hypoalgesic effects and contributed to reduction of disability in participants with chronic nonspecific NP and should be considered as effective approach for treating this condition.
No potential conflict of interest relevant to this article was reported by the authors
References
- 1.Bertozzi L, Gardenghi I, Turoni F, et al. Effect of therapeutic exercise on pain and disability in the management of chronic nonspecific neck pain: systematic review and meta-analysis of randomized trials. Physical therapy. 2013;93:1026–1036. doi: 10.2522/ptj.20120412. [DOI] [PubMed] [Google Scholar]
- 2.Bonetti F, Curti S, Mattioli S, et al. Effectiveness of a ‘Global Postural Reeducation’ program for persistent low back pain: a non-randomized controlled trial. BMC musculoskeletal disorders. 2010;11:285. doi: 10.1186/1471-2474-11-285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chiu TW, Wright A. To compare the effects of different rates of application of a cervical mobilisation technique on sympathetic outflow to the upper limb in normal subjects. Manual therapy. 1996;1:198–203. doi: 10.1054/math.1996.0269. [DOI] [PubMed] [Google Scholar]
- 4.Cunha AC, Burke TN, Franca FJ, et al. Effect of global posture reeducation and of static stretching on pain, range of motion, and quality of life in women with chronic neck pain: a randomized clinical trial. Clinics. 2008;63:763–770. doi: 10.1590/S1807-59322008000600010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.De Lima ESRF, Vanti C, Banchelli F, et al. The effect of Global Postural Reeducation on body weight distribution in sitting posture and on musculoskeletal pain. A pilot study. La Medicina del lavoro. 2017;108:187–196. doi: 10.23749/mdl.v108i3.5458. [DOI] [PubMed] [Google Scholar]
- 6.Dworkin RH, Turk DC, Wyrwich KW, et al. Interpreting the clinical importance of treatment outcomes in chronic pain clinical trials: IMMPACT recommendations. The journal of pain: official journal of the American Pain Society. 2008;9:105–121. doi: 10.1016/j.jpain.2007.09.005. [DOI] [PubMed] [Google Scholar]
- 7.Fortin C, Feldman DE, Tanaka C, et al. Inter-rater reliability of the evaluation of muscular chains associated with posture alterations in scoliosis. BMC musculoskeletal disorders. 2012;13:80. doi: 10.1186/1471-2474-13-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Freburger JK, Carey TS, Holmes GM, et al. Exercise prescription for chronic back or neck pain: who prescribes it? who gets it? What is prescribed? Arthritis and rheumatism. 2009;61:192–200. doi: 10.1002/art.24234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gross AR, Kaplan F, Huang S, et al. Psychological Care, Patient Education, Orthotics, Ergonomics and Prevention Strategies for Neck Pain: A Systematic Overview Update as Part of the ICON Project. The open orthopaedics journal. 2013;7:530–561. doi: 10.2174/1874325001307010530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Guzman J, Haldeman S, Carroll LJ, et al. Clinical practice implications of the Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Associated Disorders: from concepts and findings to recommendations. Spine. 2008;33:S199–213. doi: 10.1097/BRS.0b013e3181644641. [DOI] [PubMed] [Google Scholar]
- 11.Isgro M, Buraschi R, Barbieri C, et al. Conservative management of degenerative disorders of the spine. Journal of neurosurgical sciences. 2014;58:73–76. [PubMed] [Google Scholar]
- 12.Jones B, Kenward MG. Design and Analysis of Cross-Over Trials. Chapman & Hall, Boca Raton (FL) 2015. [Google Scholar]
- 13.Koh MJ, Park SY, Park EJ, et al. The effect of education on decreasing the prevalence and severity of neck and shoulder pain: a longitudinal study in Korean male adolescents. Korean journal of anesthesiology. 2014;67:198–204. doi: 10.4097/kjae.2014.67.3.198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.La Touche R, Fernandez-de-las-Penas C, Fernandez-Carnero J, et al. The effects of manual therapy and exercise directed at the cervical spine on pain and pressure pain sensitivity in patients with myofascial temporomandibular disorders. Journal of oral rehabilitation. 2009;36:644–652. doi: 10.1111/j.1365-2842.2009.01980.x. [DOI] [PubMed] [Google Scholar]
- 15.Lee SM, Lee CH, O’Sullivan D, et al. Clinical effectiveness of a Pilates treatment for forward head posture. Journal of physical therapy science. 2016;28:2009–2013. doi: 10.1589/jpts.28.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lewit K, Simons DG. Myofascial pain: relief by post-isometric relaxation. Archives of physical medicine and rehabilitation. 1984;65:452–456. [PubMed] [Google Scholar]
- 17.Lopez-Lopez A, Alonso Perez JL, Gonzalez Gutierez JL, et al. Mobilization versus manipulations versus sustain apophyseal natural glide techniques and interaction with psychological factors for patients with chronic neck pain: randomized controlled trial. European journal of physical and rehabilitation medicine. 2015;51:121–132. [PubMed] [Google Scholar]
- 18.Maluf SA, Moreno BG, Crivello O, et al. Global postural reeducation and static stretching exercises in the treatment of myogenic temporomandibular disorders: a randomized study. Journal of manipulative and physiological therapeutics. 2010;33:500–507. doi: 10.1016/j.jmpt.2010.08.005. [DOI] [PubMed] [Google Scholar]
- 19.Monticone M, Ferrante S, Vernon H, et al. Development of the Italian Version of the Neck Disability Index: cross-cultural adaptation, factor analysis, reliability, validity, and sensitivity to change. Spine. 2012;37:E1038–1044. doi: 10.1097/BRS.0b013e3182579795. [DOI] [PubMed] [Google Scholar]
- 20.Monticone M, Giorgi I, Baiardi P, et al. Development of the Italian version of the Tampa Scale of Kinesiophobia (TSK-I): cross-cultural adaptation, factor analysis, reliability, and validity. Spine. 2010;35:1241–1246. doi: 10.1097/BRS.0b013e3181bfcbf6. [DOI] [PubMed] [Google Scholar]
- 21.Moustafa IM, Diab AA, Harrison DE. The effect of normalizing the sagittal cervical configuration on dizziness, neck pain , and cervicocephalic kinesthetic sensibility: a 1-year randomized controlled study. European journal of physical and rehabilitation medicine. 2016 doi: 10.23736/S1973-9087.16.04179-4. [DOI] [PubMed] [Google Scholar]
- 22.Oliveri M, Caltagirone C, Loriga R, et al. Fast increase of motor cortical inhibition following postural changes in healthy subjects. Neuroscience letters. 2012;530:7–11. doi: 10.1016/j.neulet.2012.09.031. [DOI] [PubMed] [Google Scholar]
- 23.Ozan MO, Stufken J. Assessing the impact of carryover effects on the variances of estimators of treatment differences in crossover designs. Statistics in medicine. 2010;29:2480–2485. doi: 10.1002/sim.4009. [DOI] [PubMed] [Google Scholar]
- 24.Peolsson A, Marstein E, McNamara T, et al. Does posture of the cervical spine influence dorsal neck muscle activity when lifting? Manual therapy. 2014;19:32–36. doi: 10.1016/j.math.2013.06.003. [DOI] [PubMed] [Google Scholar]
- 25.Pillastrini P, de Lima ESRF, Banchelli F, et al. Effectiveness of Global Postural Re-education in Patients With Chronic Nonspecific Neck Pain: Randomized Controlled Trial. Physical therapy. 2016;96:1408–1416. doi: 10.2522/ptj.20150501. [DOI] [PubMed] [Google Scholar]
- 26.Pillastrini P, Mugnai R, Farneti C, et al. Evaluation of two preventive interventions for reducing musculoskeletal complaints in operators of video display terminals. Physical therapy. 2007;87:536–544. doi: 10.2522/ptj.20060092. [DOI] [PubMed] [Google Scholar]
- 27.Pool JJ, Ostelo RW, Hoving JL, et al. Minimal clinically important change of the Neck Disability Index and the Numerical Rating Scale for patients with neck pain. Spine. 2007;32:3047–3051. doi: 10.1097/BRS.0b013e31815cf75b. [DOI] [PubMed] [Google Scholar]
- 28.Quek J, Pua YH, Clark RA, et al. Effects of thoracic kyphosis and forward head posture on cervical range of motion in older adults. Manual therapy. 2013;18:65–71. doi: 10.1016/j.math.2012.07.005. [DOI] [PubMed] [Google Scholar]
- 29.Reid SA, Rivett DA, Katekar MG, et al. Comparison of mulligan sustained natural apophyseal glides and maitland mobilizations for treatment of cervicogenic dizziness: a randomized controlled trial. Physical therapy. 2014;94:466–476. doi: 10.2522/ptj.20120483. [DOI] [PubMed] [Google Scholar]
- 30.Rolving N, Christiansen DH, Andersen LL, et al. Effect of strength training in addition to general exercise in the rehabilitation of patients with non-specific neck pain. A randomized clinical trial. European journal of physical and rehabilitation medicine. 2014;50:617–626. [PubMed] [Google Scholar]
- 31.Sarig Bahat H, Takasaki H, Chen X, et al. Cervical kinematic training with and without interactive VR training for chronic neck pain - a randomized clinical trial. Manual therapy. 2015;20:68–78. doi: 10.1016/j.math.2014.06.008. [DOI] [PubMed] [Google Scholar]
- 32.Schwind J, Learman K, O’Halloran B, et al. Different minimally important clinical difference (MCID) scores lead to different clinical prediction rules for the Oswestry disability index for the same sample of patients. The Journal of manual & manipulative therapy. 2013;21:71–78. doi: 10.1179/2042618613Y.0000000028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Slater H, Sluka K, Söderlund A, et al. Curriculum Outline on Pain for Physical Therapy, In: Pain, I.A.f.t.S.o. (Ed.) 2009 [Google Scholar]
- 34.Souchard P. Rieducazione Posturale Globale (RPG – Il metodo) Elsevier, Milan. 2012. [Google Scholar]
- 35.Teodori RM, Negri JR, Cruz MC, et al. Global Postural Re-education: a literature review. Revista brasileira de fisioterapia. 2011;15:185–189. [PubMed] [Google Scholar]
- 36.Tozzi P, Bongiorno D, Vitturini C. Fascial release effects on patients with non-specific cervical or lumbar pain. J Bodyw Mov Ther. 2011;15:405–416. doi: 10.1016/j.jbmt.2010.11.003. [DOI] [PubMed] [Google Scholar]
- 37.Vanti C, Generali A, Ferrari S, et al. [General postural rehabilitation in musculoskeletal diseases: scientific evidence and clinical indications] Reumatismo. 2007;59:192–201. [PubMed] [Google Scholar]
- 38.Vanti C, Monticone M, Ceron D, et al. Italian version of the physical therapy patient satisfaction questionnaire: cross-cultural adaptation and psychometric properties. Physical therapy. 2013;93:911–922. doi: 10.2522/ptj.20120170. [DOI] [PubMed] [Google Scholar]
- 39.Vernon H, Guerriero R, Kavanaugh S, et al. Self-rated disability, fear-avoidance beliefs, nonorganic pain behaviors are important mediators of ranges of active motion in chronic whiplash patients. Disability and rehabilitation. 2013;35:1954–1960. doi: 10.3109/09638288.2013.768302. [DOI] [PubMed] [Google Scholar]
- 40.Villafane JH, Fernandez-de-Las-Penas C, Pillastrini P. Botulinum toxin type A combined with cervical spine manual therapy for masseteric hypertrophy in a patient with Alzheimer-type dementia: a case report. Journal of chiropractic medicine. 2012;11:280–285. doi: 10.1016/j.jcm.2012.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Williams MA, Williamson E, Gates S, et al. Reproducibility of the cervical range of motion (CROM) device for individuals with sub-acute whiplash associated disorders. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2012;21:872–878. doi: 10.1007/s00586-011-2096-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Youdas JW, Carey JR, Garrett TR. Reliability of measurements of cervical spine range of motion--comparison of three methods. Physical therapy. 1991;71:98–104. doi: 10.1093/ptj/71.2.98. discussion 105-106. [DOI] [PubMed] [Google Scholar]