Abstract
Introduction:
In light of both current Italian radioprotection law and the new European Directive, radiation dose monitoring was carried out on the interventional staff, of the new Papa Giovanni XXIII Hospital in Bergamo, Italy, potentially exposed to high radiation levels.
Methods:
Interventional activities were mapped and personal dose data were collected for three years using thermo-luminescent dosimeters. Effective dose (ED) to whole body and equivalent dose (HT) to hands and eye lenses were estimated from Hp(10) and Hp(0.07) measurements.
Results:
During the monitoring period, individual annual cumulative ED ranged from 0.2 to 9.3 mSv for radiologists (N=4), from 0.1 to 4.6 mSv for neuroradiologists (N=4), from 0.1 to 2.0 mSv for nurses (N=11), and from less than 0.1 to 1.2 mSv for radiographers (N=14). Individual annual HTs to hands ranged from 1.5 to 282.0 mSv for radiologists, from 0.5 to 99.7 mSv for neuroradiologists, from 1.9 to 12.8 mSv for nurses and from 0.7 to 12 mSv for radiographers. Individual annual HTs to eye lenses ranged from 1.1 to 110.9 mSv, from 0.6 to 58.3 mSv, from 0.1 to 8.6 mSv, from less than 0.1 to 11.7 mSv for radiologists, neuroradiologists, nurses and radiographers respectively.
Conclusions:
The doses received by medical doctors were higher than those for the other two groups. The Italian dose limits have been respected for all operator categories. The eye lens dose limit of the new European Directive (BSS 2013) was exceeded in 2013 by three medical doctors, prompting prescription of protective glasses. Since 2015 also this new limit has been observed.
Key words: Worker radioprotection, interventional radiology, effective dose, eye lens dose
Abstract
«Valutazione della dose radiante per il personale esposto in ambito interventistico».
Introduzione:
Alla luce della normativa locale vigente e della nuova Direttiva Europea sulla radioprotezione, è stato effettuato il monitoraggio delle dosi personali del polo angiografico/interventistico, suscettibile di elevati livelli di esposizione, del nuovo Ospedale Papa Giovanni XXIII di Bergamo.
Metodo:
Sono state mappate le attività angiografiche/interventistiche. I dati dosimetrici personali sono stati raccolti con l’utilizzo di dosimetri termoluminescenti calibrati in Hp(10) e Hp(0,07) e successivamente sono state valutate la dose efficace al corpo intero (ED) e le dosi equivalenti (HT) alle mani e al cristallino.
Risultati:
Le stime di dose efficace annuale pro capite hanno evidenziato valori negli intervalli 0,2-9,3 mSv; 0,1-4,6 mSv; 0,1-2,0 mSv e <0,1-1,2 mSv per radiologi (N=4), neuroradiologi (N=4), infermieri (N=11) e tecnici (N=14) rispettivamente. La dose equivalente alle mani ha assunto valori da 1,5 a 282,0 mSv per radiologi, da 0,5 a 99,7 mSv per neuroradiologi, da 1,9 a 12,8 mSv per infermieri e da 0,7 a 12,0 mSv per tecnici; la dose equivalente al cristallino è variata rispettivamente da 1,1 a 110,9 mSv, da 0,6 a 58,3 mSv, da 0,1 a 8,6 mSv, da meno di 0,1 a 11,7 mSv per i quattro gruppi di operatori.
Conclusioni:
Le dosi ricevute dagli operatori medici sono più elevate rispetto a quelle del personale infermieristico e tecnico. Pur rispettando i limiti di dose dell’attuale normativa italiana, nel 2013, per tre medici interventisti si è verificato il superamento del limite di dose al cristallino stabilito dalla nuova Direttiva Europea (BSS 2013). Grazie all’adozione di occhiali protettivi si è ottenuto un significativo risparmio di dose equivalente al cristallino e il rispetto del nuovo limite.
Introduction
In Italy, practices involving X-Ray exposure of persons are regulated by Legislative Decree 230/95 and following integrations (6-8) that acknowledge the European Directives concerning the protection of individuals against ionizing radiation risk. Radiological activities have to comply with the three basic principles of radioprotection, i.e. justification, optimization and dose limitation (12). The third principle states that the dose to individuals should not exceed the appropriate limits - recommended by ICRP (International Commission on Radiological Protection) - to ensure that no individual is exposed to radiation risks that are judged to be unacceptable. In order to address this principle, dose limits have been established for workers, as reported in table 1.
Table 1.
Dose limits for workers indicated in the Decreto Legislativo 230/95 and following integrations (DL 241/00 and 257/01)
| Effective dose (whole body) mSv | Equivalent dose to eye lens mSv | Equivalent dose to skin mSv | Equivalent dose to extremities mSv | Reference |
| 20 | 150 | 500 | 500 | DL 230/95 |
These values refer to the radioprotection quantities “effective dose” (ED) and “equivalent organ dose” (HT) (12), expressed in Sievert (Sv). The effective dose relates to stochastic risk whereas the equivalent organ dose relates to deterministic effects, characterized by threshold dose values above which the effects become manifest, with increasing degrees of seriousness as the dose increases. Dose limits have the goal of keeping stochastic effects at acceptable levels and preventing deterministic effects.
The ICRP, in publication 118 (13), provides a review of the epidemiological literature concerning early and late effects of radiation in normal tissues and organs in the context of radioprotection. In particular, concerning cataracts, because of evidence of higher than expected incidences of injury after low doses - suggesting a dose threshold lower than previously considered (4) - the Commission recommends an updated dose limit for the eye lens of 20 mSv/year (the value indicated in the current local regulations is 150 mSv/year (6)).
The most recent European Directive (Basic Safety Standard BSS 2013) (5), that must be implemented by Member States by 2018, in agreement with ICRP recommendations, lowers the eye lens limit to 20 mSv/year (value averaged across 5 years) with the constraint of 100 mSv cumulated during 5 years and 50 mSv as a maximum yearly value.
In the context of medical exposures, radiologists who carry out interventional procedures stand in proximity to the patient during irradiation, so they are prone to receiving high radiation doses.
During the last few decades, the number of interventional procedures has grown enormously (16), thanks to the technological development of high performance X-Ray systems, allowing for several new fluoroscopically guided procedures to be introduced and replace conventional surgery, with the advantage of being less invasive.
Nevertheless, the spread of radiological practices has increased the number of individuals exposed to ionizing radiation. As a consequence, the attention to exposure-related risk for individuals has risen too (12, 23). Several efforts have been made in order to endorse the ALARA (As Low As Reasonably Achievable) principle, in light of guaranteed safety for both patients, who benefit from the procedures, and operators. Such efforts have involved the development of imagers with improved detection efficiency (so that adequate image quality can be obtained with lower radiation dose levels); the introduction of collective and comfortable individual protection devices; the dissemination of educational material (for instance, presentations are available from the IAEA web site) to promote safe protection habits. Different guidelines (14, 16) have been published to address radioprotection optimization and surveys have been carried out (3, 10, 15, 18, 20) to assess occupational radiation doses. The present work reports the results of three years of monitoring the interventional staff, including radiologists, neuroradiologists, nurses and radiographers, of the new Hospital Papa Giovanni XXIII in Bergamo, Italy. In light of both local current regulations and the new European Directive, monitoring aimed at assessing whether exposure limits were respected and at identifying situations that could be optimized.
Methods
Data were collected during the period January 2013 - December 2015.
Staff and activity
The interventional staff consists of 4 neuro-radiologists and 4 radiologists, supported by 14 radiographers and 11 nurses who interchange between the two areas of activity. All staff, during the period considered in this work, were classified “A”, because they were considered susceptible to cross the threshold value of 2 mSv/year for the whole body effective dose (Regional indication (19)).
On average each year about 500 and 1000 neuroradiology and radiology procedures are performed, respectively, using angiographic systems.
The activity is performed in a dedicated area of the Imaging Department, including two operating theaters (S1 and S2), and in a third operating theater (A9) located in the Surgery Block.
Also about 500 Computed Tomography (CT) guided neuro-radiological procedures are carried out in the Imaging Department, Neuroradiology unit.
The X-Ray Systems available in the above mentioned rooms and the fundamental procedures performed are listed in table 2.
Table 2a.
X-Ray Systems available in our Institution, location and main usage in Radiology applications
| Room | X-Ray System (Model – Brand – Detector type) | Main Radiology applications |
| S1 | 1) AlluraXper FD20 – Philips – Digital Detector |
Uro-nefrology interventions:
Emergency:
|
Table 2b.
X-Ray Systems available in our Institution, location and main usage for Neuro-Radiology applications.* procedures performed mostly or exclusively using CT
| Room | X-Ray System (Model – Brand ) |
Main Neuro-Radiology applications |
| S2 |
|
Neurovascular procedures (Head&neck&spine vascular diseases)
|
| A9 | 4) AlluraXper FD 20 biplane – Philips (Digital Detector) 5) O-Arm – Medtronic (Digital Detector &Cone Beam System) 6) OEC 9800 Plus - General Electric (Conventional Image Intensifier) |
Spinal Procedures
|
| TC NRad | 7) TC Brillance 64 -Philips |
The angiographic rooms are equipped with collective protection devices, consisting of ceiling-suspended protective screens and tableside lead shielding drapes (lead-lined wall panels are installed for the protection of adjacent rooms). All personnel wear individual protection devices: 0.25 (rear) and 0.5 (front) mm lead-equivalent skirt and waistcoat, 0.5 mm lead equivalent collar, insuring high protection levels, as shown in table 3. Almost all personnel wear 0.75 mm lead equivalent glasses.
Table 3.
Percentage of radiation transmitted through individual protection devices IPD at different KVs
| Radiation transmitted through IPD (%) | |||
| KV | Glasses | Apron single layer (back side) | Apron double layer (front side) |
| 60 | 0.4 | 24.6 | 1.3 |
| 80 | 0.9 | 32.0 | 3.9 |
| 100 | 2.1 | 38.5 | 7.3 |
| 120 | 2.7 | 44.2 | 10.8 |
Radioprotection indices and physical quantity
The ED is defined as ED=∑TWTHT (unit Sievert) (12),
HT being the equivalent dose in tissue or organ, and WT the appropriate tissue weighting factor, reported by ICRP 103; the equivalent dose in tissue or organ is given by HT=Dm*WR where Dm is the absorbed dose averaged in that tissue or organ (due to radiation R), multiplied by the radiation weighting factor WR (for photons WR is equal to 1 for all energies).
Neither ED nor HT can be measured directly, but they can be estimated from practical quantities, Hp(10) and Hp(0.07) (11) that can be easily measured.
The personal dose equivalent, Hp(d) (11), is the dose equivalent in ICRU tissue, at an appropriate depth (d) in mm below a specified point on the body (unit J/kg).
In our hospital, thermo-luminescent dosimeters were used to record these physical quantities. For radiologists and neuroradiologists, who wear two “whole body” dosimeters, the ED was then evaluated using the following formula (17):
E=0.98*Hp(10)under+0.02*Hp(0.07)above
with “under” and “above” indicating the position of the dosimeter under the apron (in correspondence to the abdomen) and above the apron (at chest level) respectively.
Roughly, Hp(10) can be considered as a conservative estimation of the ED, whereas Hp(0.07) is representative of the skin dose of unprotected parts of the body.
For radiographers and health care assistants, wearing only one “whole body” dosimeter, ED was estimated as E=f*Hp(10) where f is a factor that accounts for the use of the protective clothing. It is estimated as:
f=(3/4* t double + ¼ t single)+0.02~0.15; t is the fraction of the radiation transmitted by the double/single layer of the shielding cloth at the operative KVolt (KV). The double layer (front) is given a higher weight because the operator is exposed frontally. 0.02 is the fraction of the unshielded Hp(10) contributing to the whole body ED.
All operators wear a “bracelet” dosimeter, in order to evaluate the dose to hands as follows:
Hhand=Hp(0.07)*1.3. The factor 1.3 accounts for the fact that fingers receive a higher dose compared to the wrist, where the dosimeter is positioned.
Concerning the eye lens, the proper quantity is Hp(0.3) (2, 22). Nevertheless, the feasibility of using Hp(10) or Hp(0.07) values and appropriate correction factors to estimate the eye lens dose was demonstrated (22). In the present work such a quantity was estimated as follows:
Hlens=Hp(10)above*fcorr*(α +(1-α)*fglasses)
where fcorr(1.3) is the correction factor reported in literature (22), and the value adopted for fglasses is 0.1. The fraction of radiation transmitted by the protective lenses at the working KV is about 2-3%, for direct irradiation with primary beam (see table 3). Nevertheless, it has been reported (16) that in clinical settings, where the operator is exposed to scattered photons, the fraction of radiation reaching the eyes is higher by a factor of 2 to 3. 0.1 is a conservative value. The use of protective glasses, prescribed in 2013, has become more systematic starting from 2014. Periodically, a check of the effective use of glasses is performed, so that the fraction of activity carried out without glasses (α) and the complementary fraction with glasses (1-α) can be assessed. A form is used to report who/when has started/stopped using glasses and the reason for not using them (for instance, broken glasses or need for correction lenses). Two people reported nausea when they wear glasses, so they use them only about 50% of the time spent in the operating theaters.
Dosimeters are replaced each 3 months.
Statistical analysis
The impact of the different professions on each dose index was assessed by a one-way ANOVA. Profession was considered as the independent variable (factor) and dose indices as dependent variables.
A post-hoc test (the least significant difference test) was performed to identify the main source of variability. If a significant F value was found for the independent variable, this was reported as a main effect. When a main effect was found, then a post-hoc test was performed to compare the dependent variable upon the levels of the factor 2x2, thus identifying the main sources of variability.
Analysis was performed with Statistica version 6.0 (StatSoft Inc., Tulsa, OK, USA) using a two-sided type I error rate of p=0.05.
Mean individual annual doses were used as input data.
Results
Dose data
Table 4 summarizes range, 25th, 50th and 75th percentile of the annual individual ED, HT to hands and HT to eye lenses for the four groups of operators. Figures 1, 2 and 3 show the data of table 4, without the value range. Figure 4 shows the trend for the HT to eye lens for the 4 groups of operators from 2013 to 2015.
Table 4.
Individual annual effective dose (ED), equivalent dose to hand (Hand HT) and equivalent dose to eye lenses (Eye lens HT) for radiologists, neuroradiologists, nurses and radiographers estimated from Hp(10) and Hp(0.07) recorded between 2013 and 2015. Range (minimum, maximum), 25th percentile, 50th percentile and 75th percentile are reported
| Radiologist (4 subjects) mSv | Neuroradiologist (4 subjects) mSv | Nurse (11 subjects) mSv | Radiographer (14 subjects) mSv | |||||||||
| WB | Hand | Eye lens | WB | Hand | Eye lens | WB | Hand | Eye lens | WB | Hand | Eye lens | |
| ED | HT | HT | ED | HT | HT | ED | HT | HT | ED | HT | HT | |
| min | 0.2 | 1.5 | 1.1 | 0.1 | 0.5 | 0.6 | 0.1 | 1.9 | 0.1 | <0.1 | 0.7 | <0.1 |
| max | 9.3 | 282.0 | 110.9 | 4.6 | 99.7 | 58.3 | 2.0 | 12.8 | 8.6 | 1.2 | 12.0 | 11.7 |
| 25th perc | 2.0 | 32.7 | 5.8 | 0.3 | 3.3 | 2.3 | 0.3 | 4.2 | 0.5 | 0.2 | 2.0 | 0.4 |
| 50th perc | 4.5 | 59.6 | 8.4 | 1.9 | 32.1 | 3.3 | 0.5 | 6.8 | 1.5 | 0.4 | 4.2 | 1.4 |
| 75th perc | 6.5 | 137.5 | 31.4 | 2.8 | 49.5 | 9.5 | 0.9 | 9.8 | 3.6 | 0.5 | 5.8 | 3.3 |
Figure 1.
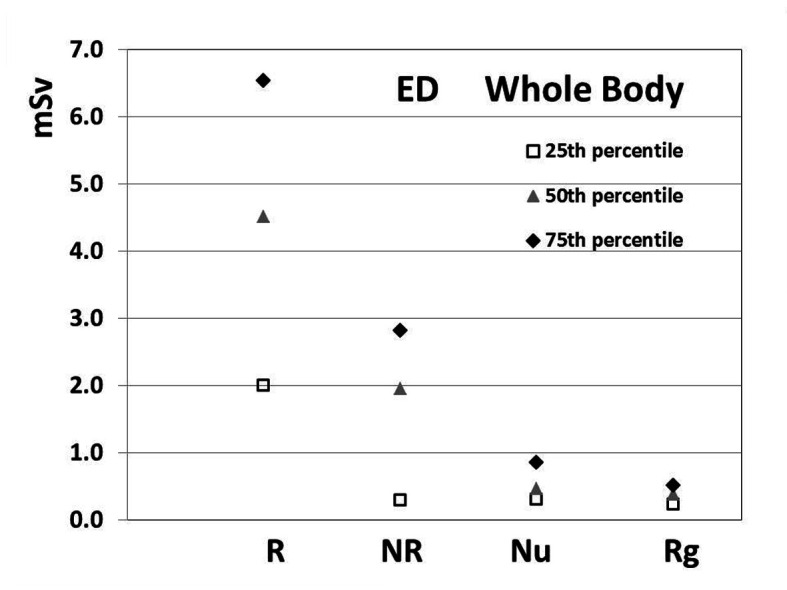
25th 50th and 75th percentile of individual annual effective doses (ED) estimated for the four groups of operators from 2013 to 2015. (R Radiologist, NR Neuroradiologist, Nu Nurse, Rg Radiographer)
Figure 2.
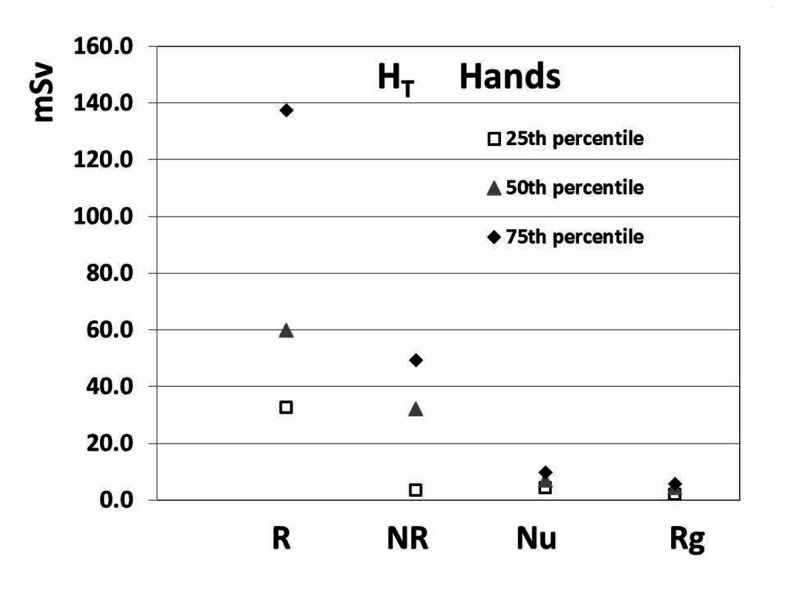
25th 50th and 75th percentile of annual individual equivalent hand doses estimated for the four groups of operators from 2013 to 2015. (R Radiologist, NR Neuroradiologist, Nu Nurse, Rg Radiographer)
Figure 3.
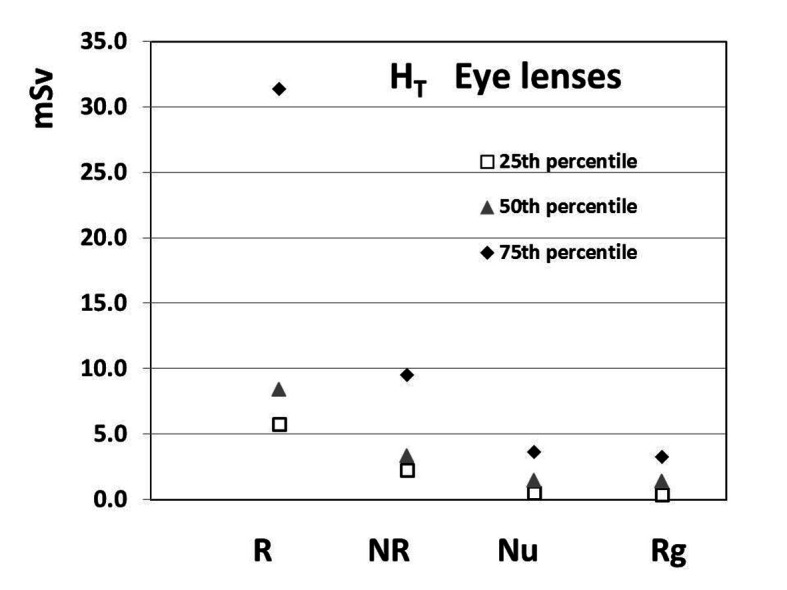
25th 50th and 75thpercentile of annual individual equivalent eye lens dose estimated for the four groups of operators from 2013 to 2015. (R Radiologist, NR Neuroradiologist, Nu Nurse, Rg Radiographer)
Figure 4.
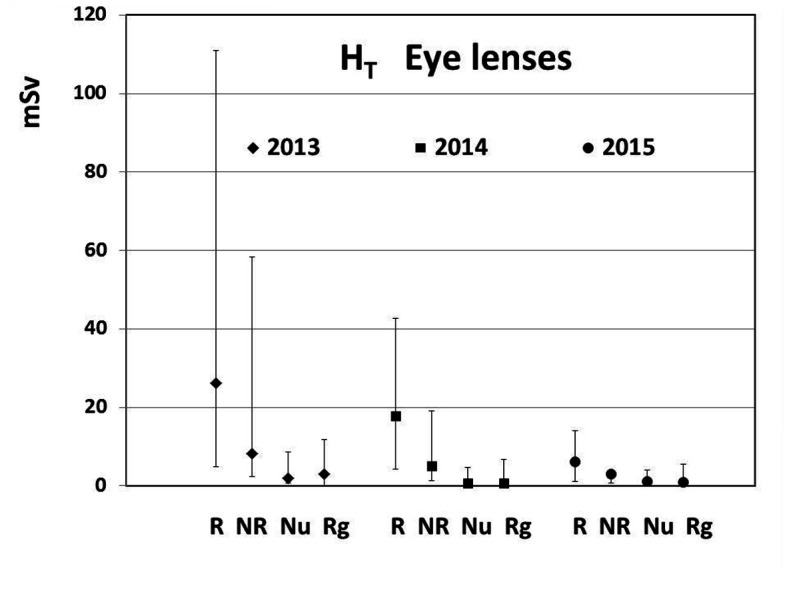
Trend for the eye lens equivalent dose from 2013 to 2015 for the four groups of operators (R Radiologist, NR Neuroradiologist, Nu Nurse, Rg Radiographer). Minimum, maximum and median values are shown
Statistical test results
The profession was a main effect with a statistically significant impact on the ED (F=17.6; p<0.0001), HT to the hands (F=11.1; p<0.0001) and HT to the eye lenses (F=9.2; p=0.0001).
Post-hoc test of the different professions showed a significant decrease in ED values from radiologists to neuroradiologists (4.4±3.1mSv vs 1.9±1.6 mSv; p=0.002), from neuroradiologists to nurses (0.6±0.3 mSv; p=0.03) while no significant differences were found between nurses and radiographers (0.4±0.2 mSv; p=0.71).
Post-hoc test of the different professions showed a significant decrease in HT to the hands from radiologists to neuroradiologists (94.6±95.9 mSv vs 31.0±29.6 mSv; p=0.004), while no significant differences were found between neuroradiologists and nurses (6.5±3.2 mSv; p=0.15) and between nurses and radiographers (4.5±2.4 mSv; p=0.84).
Post-hoc test of the different professions showed a significant decrease in HT to the eye lens from radiologists to neuroradiologists (23.2±22.8 mSv vs 9.8±11.65 mSv; p=0.02), while no significant differences were found between neuroradiologists and nurses (2.2±1.5mSv; p=0.09) and between nurses and radiographers (2.5±2.1 mSv; p=0.91).
Discussion
Operators involved in interventional procedures make use of pulsed fluoroscopy (and cine angio-radiography) combined with injection of contrast agents and DSA (Digital Subtraction Angiography) technique. Operators are essentially exposed to the radiation field scattered by the patient irradiated with the primary radiation beam. In general, during cine acquisition staff move outside the X-Ray room (or as far as possible from the X-Ray source inside the room), so that their major source of exposure is fluoroscopy. Fluoroscopy times range from a few minutes to above 1 hour, depending on the complexity of the intervention. Figure 5a shows the distribution of the fluoroscopy time from a sample of 470 procedures monitored during 2015 in our hospital in room S1. The mean fluoroscopy time is about 11 minutes and the 75th percentile is about 15 minutes for this set of data. The distribution of KV for the same sample of procedures is shown in figure 5b.
Figure 5.
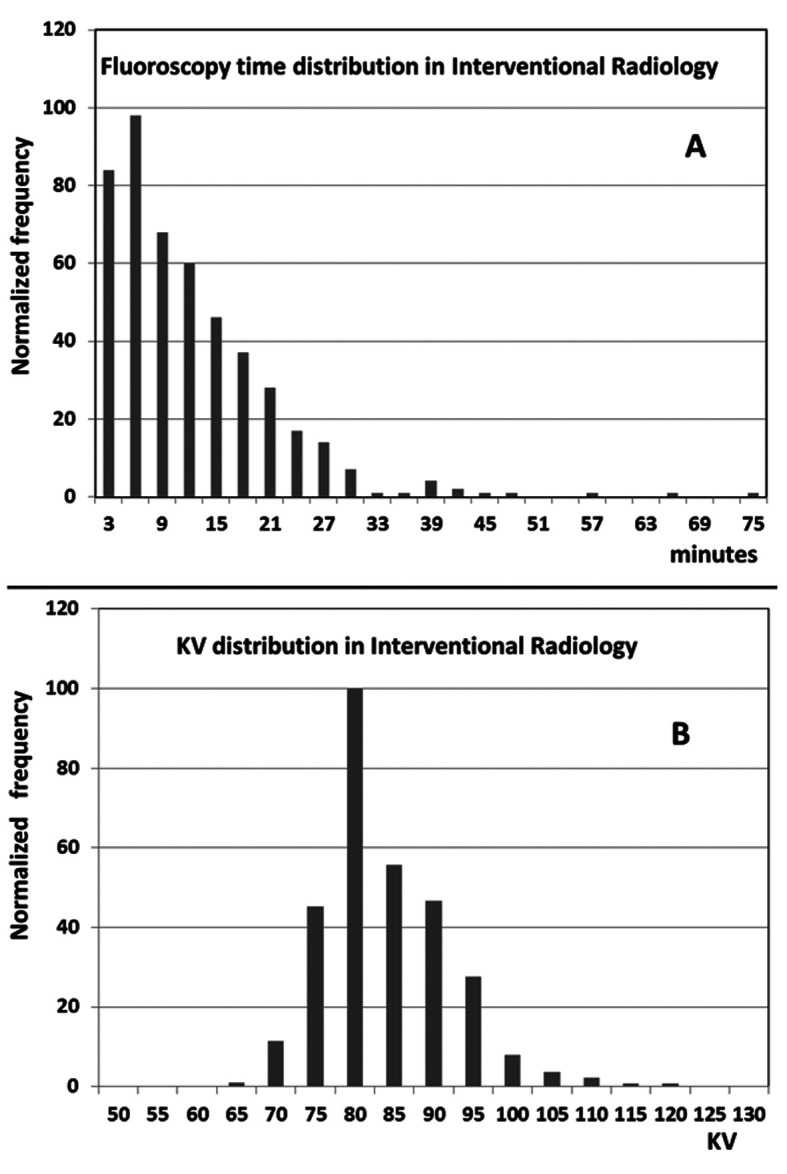
A: fluoroscopy time distribution from a sample of 470 procedures. Mean and 75th percentile are about 11 and 15 minutes respectively; B: KV distribution from the same sample of procedures as figure 5A
The intensity of the scattered field depends on several factors, such as intensity and quality of the primary beam (KV and filtration), extension of the irradiated volume, angle of incidence of the primary beam on the patient, operator-patient distance and position of the operator relative to the tube-detector orientation.
ACE (Automatic Control of Exposure) devices determine the intensity of the primary beam (X-Ray tube output), upon input of the detector. Such intensity is modulated as a function of the patient size, the image quality requested (low, medium and high dose options are available in order to obtain low, medium and high quality image) and image magnification (different “zoom” selections are available); larger irradiated volumes cause a higher quantity of scattered radiation; also the correct positioning of the patient (as far as possible from the X-Ray source and as close as possible to the detector) is important; scattered radiation field intensity decreases as the distance from the patient increases; when the primary beam axis is parallel to the floor, the intensity of the radiation field is lower on the detector side with respect to the tube side; the cumulative absorbed dose increases with irradiation time. Ambient dose measurements taken in our hospital during the irradiation of a phantom confirm these findings (see figure 6). Awareness of the dependence of the dose on such factors helps in selecting the appropriate irradiation protocol for each clinical application and in addressing staff behavior during the procedures. Patient dose saving results directly in operator dose saving, due to the interdependence of patient and operator exposures (14, 16, 24). Williams (24) assessed the dependence of doses to radiologists on DAP (Dose Area Product) for different procedures and demonstrated that this patient dose index is also of great value in evaluating radiologist exposure.
Figure 6.
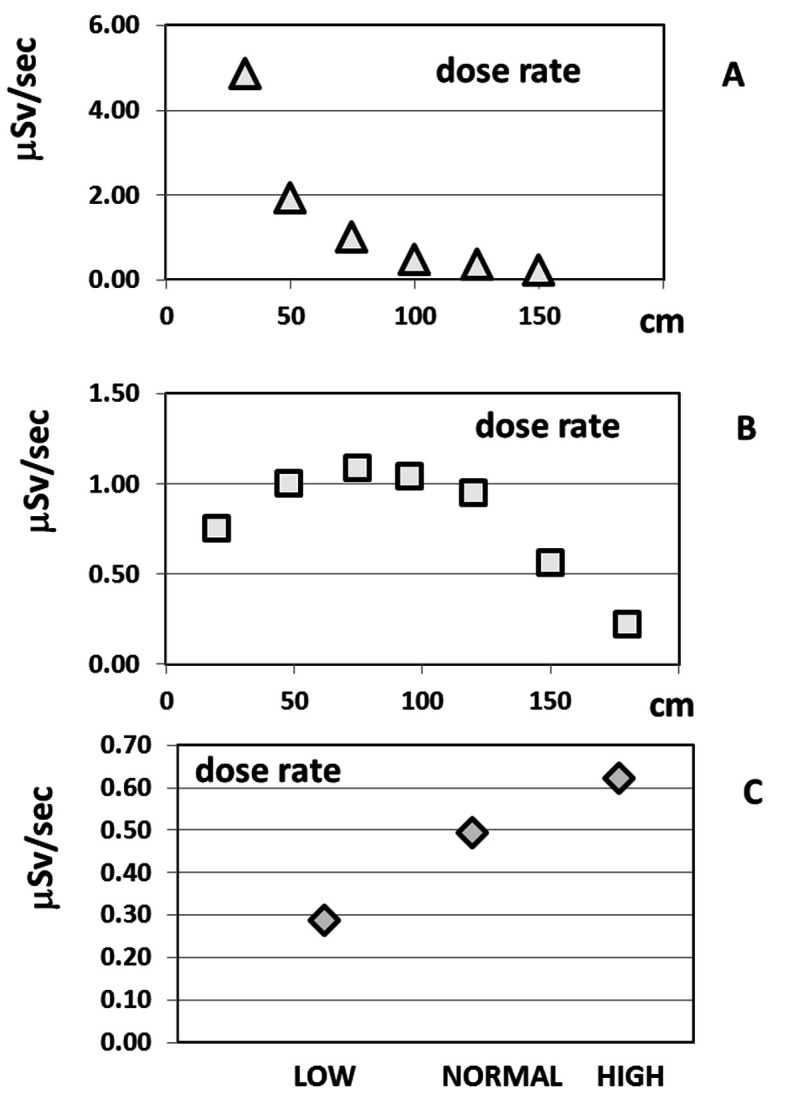
Ambient dose, measured in room S1, while irradiating a water-equivalent solid phantom, simulating a patient. A) dependence of the dose rate (microSievert/sec) on the distance from the irradiated phantom, along an axis parallel to the floor, at 110 cm height, X-Ray tube under the table, field size 37X37 cm2; B) dependence of the dose rate (microSievert/sec) on the distance from the floor, along a vertical line at 70 cm from the irradiated phantom; C) dependence of the dose rate (microSievert/sec) on the “fluo mode” (Low/Normal/High dose, correspondent to different levels of image quality), in a fixed position
In case of CT guided interventions, in general a spiral scan of the region of interest and a stationary acquisition of a thin section located around the interventional point are done preliminarily, while the operators stand in the console room. Then fluoro CT driven operations (drug injection or biopsy) are performed with highly collimated radiation beams (<10 mm) producing a modest scattered radiation field. Hand dose estimations, based on phantom measurements, indicated about 30 μSv per procedure.
Our data shows higher radiation dose for the medical doctors compared to nurses and radiographers. This is consistent with the fact that, as first operators, they stand closer to the patient than the other two categories. Also, it has been assessed that radiologists receive higher doses than neuroradiologists. Although the present work did not aim at investigating the dependence of individual doses on kind and number of procedures, some comments can be made. The workloads are not distributed homogeneously among the operators. Concerning the neuroradiology activity, spinal percutaneous procedures (about 400/year using angiographic systems) are mainly performed by two neuroradiologists (NR1 and NR2), whereas vascular head/neck procedures (about 100/year) are almost exclusively performed by one neuroradiologist (NR3). The fourth neuroradiologist (NR4) intervenes only for a small fraction of cases. NR1 and NR2 also perform CT-guided spinal procedures. Mean annual individual EDs were 2.7, 3.8, 0.8 and 0.4 mSv for NR1, NR2, NR3 and NR4 respectively. Mean annual HTs to hands were 48.4, 63.7, 8.4 and 3.6 mSv respectively. It can be seen that the ED of operator NR3 is lower than those of operators NR1 and NR2 (the number of procedures is lower; also the head/neck region produces less scattered radiation than the abdomen); operator NR4 has the lowest dose because of the smallest workload.
Radiology interventions are mainly performed by three operators (R1, R2, R3). The fourth interventional radiologist (R4) covers a small fraction of the activity. Mean annual individual EDs for these operators were 8.1, 4.7, 4.3, 0.5 mSv for R1, R2, R3 and R4 respectively; mean annual HTs to hands were 228.9, 92.5, 48.8, 8.1 mSv respectively. Operator R4 received much lower doses than the others, because of the limited workload. Radiologists have, on average, higher doses than neuroradiologists.
The three doctors R1, R3 and NR1 started using protective glasses (with corrective lenses) during the second semester of 2014 or later. The cumulative HTs to eye-lenses in 2013, 2014 and 2015 were 110.9, 42.6 and 6.1 mSv for R1, 43.4, 27.7 and 14.1 for R3 and 58.3, 19.1 and 3.3 for NR1. Significant dose saving is evident for these operators.
No significant difference exists between nurses and radiographers. Nurses stay in the X-Ray room for almost the whole duration of the procedure, but at a greater distance from the patient than the medical doctors; the radiographers divide their working time between the X-Ray room and the console room. In case of procedures carried out with the mobile system, the radiographer controls the machine from inside the room, standing very close to the first operator.
In this work the power of the statistical design is penalized by the limited sample size for operators and the heterogeneity of the dose data in the four groups investigated. Nevertheless, EDs and equivalent hand doses of the present survey are comparable with those reported by other authors mentioned above. Chida et al (3) evaluated annual EDs of 3.0+1.5 mS, 1.3+0.5 mSv and 0.6+0.5 mSv for doctors, nurses and radiographers respectively. Pinto et al reported mean annual HTs to extremities of 137 mSv, 52 mSv and 40 mSv for doctors, auxiliary doctors and nurses respectively (this team performed 7 procedures/week). Sanchez et al (20) reported, for a group of interventional doctors, monthly readings ranging from 0 to 3.8 mSv for Hp(10)under, from 0.3 to 20.2 mSv for Hp(0.07)above and from 0.3 to 63.1 mSv for extremities. Foti et al (10) reported annual EDs ranging from 0.5 to 6 mSv for a team of cardiac laboratory doctors. Martin (15) reported doses to eye lenses ranging from 5 to 439 μSv/procedure (median 34 μSv/procedure) and doses to hands ranging from 8 to 514 μSv/procedure (median 136 μSv/procedure) from an interventional cardiac review study. The authors argue that differences in both workloads and protection habits are responsible for differences in occupational doses. The use of collective and individual protection devices (1, 9, 14, 16) is an important issue: tableside lead shielding drapes have been proved to be very efficient in reducing doses to unprotected legs and ankles (21); ceiling-suspended screens should be used whenever possible. Aprons and collars shield the most radio-sensitive organs and tissue (for instance gonads, internal organs, breast and thyroid), prone to stochastic risk (ICRP 103), whereas glasses protect eye lenses prone to cataract (4, 13). The availability of lead-equivalent materials, efficient in shielding and relatively light and comfortable, has increased operators’ compliance in wearing them. Also, protective gloves are used by medical doctors in our hospital during procedures where hands are in close proximity to the radiation source, for instance during percutaneous biliary interventions and spinal interventions with angiographic systems. In these cases, the bracelet dosimeter is worn under the protective glove.
Recently, protective drapes have been proposed in order to achieve hand dose saving. This device, positioned on the patient, shields the radiation scattered by the irradiated volume, reducing operator exposure. We evaluated the shielding effectiveness of the device by exposing it to the direct X-Ray beam at different KVs. Our measurements show that the attenuation decreases with increasing KV values and is higher than 80% for tube potential in the clinical range, in agreement with the data presented by other peers (Iacco M, Pasquali C: Drape Armour: a sterile shield to reduce radiation exposure to the operator. Comunicazione orale Congresso AIFM (Associazione Italiana Fisica Medica), Perugia 25-28 feb. 2016).
The drape was also tested during the exposure of an anthropomorphic phantom. For abdominal irradiation, a reduction of 40% in the scattered radiation in proximity to the imaged region was found. We think that drapes are useful tools to reduce hand exposure, provided attention is paid to correct positioning thus avoiding interference with the primary radiation field and optimizing the shielding effect for scattered radiation on the operator side. Repositioning is required in case the incident angle of the primary beam is changed.
Concerning educational aspects, since 2016 the physicist in charge of radioprotection of the interventional team has organized meetings with operators to share the golden rules of radioprotection published in ISTISAN Report 15/41 (14) and make them aware of the results of internal surveys as well as data reported by other sources.
Conclusions
ED to radiologists are higher than those to neuroradiologists that, in turn, are higher than those to nurses and radiographers (figure 1). Also, the equivalent doses to the hands and to the eye lenses assessed for the radiologists are higher than those evaluated for the other three groups (figures 2 and 3).
The results of the present survey are consistent with those reported by other Authors.
Individual effective doses and equivalent doses to hands and eye lenses, estimated for the operators of the interventional staff, complied with the current local regulations limits (published in 1995, based on ICRP 60 - now replaced by ICRP 103). Nevertheless, in 2013, the eye lens dose of three medical doctors exceeded the limit of 20 mSv set in the European directive (BSS 2013, based on ICRP 118 and ICRP 103). The prescription and use of protective glasses allowed for significant eye dose reduction to be achieved, so that the new dose limit has been observed since 2015 (figure 4).
No potential conflict of interest relevant to this article was reported by the authors
Acknowledgments:
The Author wishes to acknowledge the whole interventional staff of the Hospital Papa Giovanni XXIII of Bergamo, Italy, in particular G. Bonaldi, R. Agazzi, M. Cellerini and G. Gallizioli for their collaboration, M.C. Casalini, coordinator of radiographers, for help with monitoring the use of individual protection devices, M. Brambilla for help with statistical tests, and L. Gnani and P. Rizzi for their support in X-Ray equipment quality tests.
References
- 1.AIFM/Gruppo Regionale Lombardia. Problema Dose al Cristallino. Indicazioni Operative, 2012 Available on line at the address http://www.aifm-rp.it/limite-dose-cristallino . [Google Scholar]
- 2.Behrens R, Dietze G. Monitoring the eye lens: which dose quantity is adequate? Phys Med Biol. 2010;55:4047–4062. doi: 10.1088/0031-9155/55/14/007. [DOI] [PubMed] [Google Scholar]
- 3.Chida K, Kaga Y, Haga Y, et al. Occupational Dose in Interventional Radiology Procedures. AJR. 2013;200:138–141. doi: 10.2214/AJR.11.8455. DOI:10.2214/AJR.11.8455. [DOI] [PubMed] [Google Scholar]
- 4.Chodick G, Bekiroglu N, Hauptmann M, et al. Risk of Cataract after Exposure to Low Doses of Ionizing Radiation: A 20-Year Prospective Cohort Study among US Radiologic Technologists. Am J Epidemiol. 2008;168:620–631. doi: 10.1093/aje/kwn171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Council Directive 2013/59/EURATOM of 5 December 2013 laying down basic safety standards for protection against the dangers arising from exposure to ionising radiation, and repealing Directives 89/618/Euratom, 90/641/Euratom, 96/29/Euratom, 97/43/Euratom and 2003/122/Euratom. Official Journal of the European Union. [Google Scholar]
- 6. Decreto Legislativo 230/95: Attuazione delle direttive Euratom 80/836, 84/467, 84/466, 89/618, 90/64, 92/3 in materia di radiazioni ionizzanti. [Google Scholar]
- 7. Decreto Legislativo 241/00: Attuazione della direttiva 96/29/EURATOM in materia di protezione sanitaria della popolazione e dei lavoratori contro i rischi derivanti dalle radiazioni ionizzanti. [Google Scholar]
- 8. Decreto Legislativo 257/2001: Disposizioni integrative e correttive del decreto legislativo 26 maggio 2000, n. 241, recante attuazione della direttiva 96/29/Euratom in materia di protezione sanitaria della popolazione e dei lavoratori contro i rischi derivanti dalle radiazioni ionizzanti. [Google Scholar]
- 9. Decreto Legislativo 81/2008 – G.U. n. 101 del 30 aprile 2008: Attuazione dell’articolo 1 della legge 3 agosto 2007, n. 123, in materia di tutela della salute e della sicurezza nei luoghi di lavoro. [Google Scholar]
- 10.Foti C, Padovani R, Trianni A, et al. Staff Dosimetry in Interventional Cardiology: Survey on Methods and Level of Exposure. Radiation Protection Dosimetry. 2008;129:100–103. doi: 10.1093/rpd/ncn038. [DOI] [PubMed] [Google Scholar]
- 11. IAEA Safety Reports Series No. 16 Calibration of radiation protection monitoring Instruments, 2000. Available on line at www.pub.iaea.org/MTCD/Publications/PDF/P074_scr.pdf . [Google Scholar]
- 12.ICRP, 2007. The 2007 Recommendations of the International Commission on Radiological Protection. ICRP Publication 103. Ann. ICRP. 37(2-4) doi: 10.1016/j.icrp.2007.10.003. [DOI] [PubMed] [Google Scholar]
- 13.ICRP, 2012. ICRP Statement on Tissue Reactions / Early and Late Effects of Radiation in Normal Tissues and Organs – Threshold Doses for Tissue Reactions in a Radiation Protection Context. ICRP Publication 118. Ann. ICRP. 41(1/2) doi: 10.1016/j.icrp.2012.02.001. [DOI] [PubMed] [Google Scholar]
- 14. ISS: Gruppo di studio per l’assicurazione di qualità in radiologia interventistica: Indicazioni operative per l’ottimizzazione della radioprotezione nelle procedure di radiologia interventistica. Rapporti ISTISAN 15/41, 2015. Available on line at www.iss.it/binary/publ/cont/15_41_web.pdf . [Google Scholar]
- 15.Martin CJ. Personal dosimetry for interventional operators: when and how should monitoring be done? Br J Radiol. 2011;84:639–648. doi: 10.1259/bjr/24828606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Miller D L, Vañó E, Bartal G, et al. Occupational Radiation Protection in Interventional Radiology: A Joint Guideline of the Cardiovascular and Interventional Radiology Society of Europe and the Society of Interventional Radiology. J Vasc Interv Radiol. 2010;21:607–615. doi: 10.1016/j.jvir.2010.01.007. [DOI] [PubMed] [Google Scholar]
- 17.Niklason LT, Marx MV, Chan HP. The estimation of occupational effective dose in diagnostic radiology with two dosimeters. Health Phys. 1994;67:611–615. doi: 10.1097/00004032-199412000-00003. [DOI] [PubMed] [Google Scholar]
- 18.Pinto NGV, Braz D, Vallim MA, et al. Radiation exposure in interventional radiology. Nuclear Instruments and Methods in Physics Research. 2007;A 580:586–590. [Google Scholar]
- 19. Regione Lombardia: Circolare del 20 Dicembre 1995. Entrata in vigore del Decreto Legislativo 17 marzo 1995, numero 230 in materia di radiazioni ionizzanti. [Google Scholar]
- 20.Sánchez RM, Vano E, Fernández JM, et al. Staff Doses in Interventional Radiology: A National Survey. J Vasc Interv Radiol. 2012;23:1496–1501. doi: 10.1016/j.jvir.2012.05.056. http://dx.doi.org/10.1016/j.jvir.2012.05.056 . [DOI] [PubMed] [Google Scholar]
- 21.Shortt CP, Al-Hashimi H, Malone L, et al. Staff Radiation Doses to the Lower Extremities in Interventional Radiology. Cardiovasc Intervent Radiol. 2007;30:1206–1209. doi: 10.1007/s00270-007-9071-0. DOI 10.1007/s00270-007-9071-0. [DOI] [PubMed] [Google Scholar]
- 22.SSK. Monitoring the Eye Lens Dose. Statement by the German Commission on Radiological Protection with Scientific Reasoning. Adopted at the 240th meeting of the German Commission on Radiological Protection on 2 February 2010. Avalaible on line at www.ssk.de/SharedDocs/Beratungsergebnisse_PDF/2010/2010_01e.pdf?__blob=publicationFile . [Google Scholar]
- 23.Wall BF, Haylock R, Jansen JTM, et al. Radiation Risks from Medical X-Ray Examinations as a Function of Age and Sex of the Patient. Health Protection Agency CRCE-028, 2011. Available on line at https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/340147/HPA-CRCE-028_for_website.pdf . [Google Scholar]
- 24.Williams JR. The interdependence of staff and patient doses in interventional radiology. Br J Radiol. 1997;70:498–503. doi: 10.1259/bjr.70.833.9227232. [DOI] [PubMed] [Google Scholar]


