Abstract
Background:
Biological injuries are the most common and serious among health care workers.
Objectives:
This study aims to estimate the injuries’ incidence, job distribution and temporal trend in a hospital in Southern Italy.
Methods:
Data on accidents, collected from January 2010 to December 2016, were analyzed. Poisson distribution was used to calculate incidence rates and respective 95% confidence intervals. Trends were analyzed using the Joinpoint regression model. A multiple logistic regression model was used to identify factors associated with injuries.
Results:
Three hundred and thirty-five injuries were reported from 2010 to 2016, occurring mainly in the morning (54%) and frequently caused by needlestick (70%). We observed a significant decline in the incidence rates of the total amount of injuries (ACP=-11.3; 95% CI: -16.3 - -5.9), for nurses (ACP=-15.7; 95% CI: -24.3 - -6.2) and for health and social care assistants (ACP=-13.2; 95% CI: -23.1 - -2.0). Among male physicians the risk of biological accident was higher than female physicians (OR=3.67; 95% CI:1.9-7.1), while among male nurses the risk was lower than among female nurses (OR=0.31; 95% CI: 0.17-0.59). For the nursing category, “afternoon” and “night” represented risk factors with OR=2.19 (95% CI: 1.2-3.7) and OR=8.8 (95% CI: 3.4-22.8) respectively. For physicians, surgical intervention was a risk factor (OR=7.71; 95% CI: 3.2-18.4).
Conclusions:
Our findings confirm the need for continuous monitoring and improved control of work-related exposures, both for health and the associated costs.
Key words: Biological risk injuries, trend analysis, injuries prevention
Abstract
«Analisi temporale e fattori associati a infortuni biologici tra gli operatori sanitari del Sud Italia».
Introduzione:
Gli incidenti a rischio biologico sono i più comuni ed i più gravi tra gli operatori sanitari, con un’incidenza in Italia di 100.000 infortuni l’anno.
Obiettivi:
Investigare gli infortuni con rischio biologico in un ospedale del Sud Italia.
Metodi:
I tassi di incidenza e gli intervalli di confidenza al 95%, sono stati da calcolati con distribuzione di Poisson, da gennaio 2010 a dicembre 2016. La regressione Joinpoint è stata utilizzata per l’analisi dei trend, la regressione logistica multipla per identificare i fattori associati agli infortuni.
Risultati:
Nel periodo considerato sono stati segnalati 335 infortuni, verificatisi principalmente durante la degenza, al mattino (54%) e causati da aghi (70%). Abbiamo osservato un calo significativo dei tassi di incidenza totali (ACP=-11,3; IC 95%: -16,3 - -5,9), tra gli infermieri (ACP=-15,7; IC 95%: -24.3 - -6.2) e tra gli assistenti socio-sanitari (ACP=-13,2; IC 95%: -23,1 - -2,0). Tra i medici il rischio di incidente è più alto tra gli uomini (OR=3,67; IC 95%: 1,9-7,1), tra gli infermieri il rischio è più basso di quello delle infermiere (OR=0,31; IC 95%: 0,17-0,59). Per gli infermieri, “pomeriggio” e “notte” rappresentano i fattori di rischio (rispettivamente OR=2,19; IC 95%: 1,2-3,7; e OR=8,8; IC 95%: 3,4-22,8). Per i medici, l’intervento chirurgico rappresenta un fattore di rischio (OR=7,71; IC 95%: 3,2-18,4).
Conclusioni:
Il monitoraggio continuo ed un migliore controllo delle esposizioni appare necessario, sia per la prevenzione della salute sia per i costi degli infortuni.
Introduction
Among occupational accidents of health care workers (HCWs), injuries with biological risk are frequent and they are the most dangerous ones, presenting an incidence of about 1,200,000 injuries/year in Europe and 100,000 injuries/year in Italy (10, 24). Health care workers from clinical units are considered more exposed to biological risk injuries compared to workers from service and administrative units, because of the high exposure to blood and biological liquids (5, 6, 27).
The most important consequence of biological injury is the exposure to illnesses’ etiological agents and blood transmission, in particular to the hepatitis B virus (HBV), the hepatitis C virus HCV), and the human immunodeficiency virus (HIV) (22).
The accidents at risk of emo-transmitted illnesses represent about 40% of all injuries in the hospital setting (13).
Various measures have been implemented in Ita-ly and Europe to minimize the risk of sustaining needlestick and sharps injuries (NSIs) (5, 14, 16). To our knowledge, few Italian studies have been focused on the incidence rate of injuries with biological risk in HCWs. The studies we are familiar with have examined rates in individual Italian hospitals over short time spans or for specific health worker categories (2, 7, 11, 26).
Understanding the rate variation of the injury and the associated factors is useful to interpret results from performed prevention strategy and to compare rates among hospitals. This was a pilot study to contribute to planning a specific hospital surveillance system on occupational accidents with biological risk, among all the hospital workers. The principal aim of this study was to investigate the incidence trend rate of injuries at biological risk among the HCWs; the secondary objective was to investigate the factors associated with injuries among physicians and nurses.
Methods
This observational study used administrative data on injuries with biological risk among 5.671 HCWs employed in “SS. Filippo e Nicola” Hospital in Southern Italy.
The study was authorized by the Hospital Management of SS. Filippo e Nicola Hospital, and the data were treated anonymously.
Measurements
Administrative data on biological accidents, defined as blood or body fluids splash, needlestick injury, or a cut made by a contaminated instrument, collected by the Hospital Management, from January 2010 to December 2016, were analyzed.
The data set include information on:
- characteristics of injured health workers (sex, age, job category, years of practice, vaccination and serological status);
- work injuries (event description, Department, type of exposure, type of used devices, type of involved procedures, use of individual protection devices).
Statistical analysis
We calculated incidence rates with 95% CIs for each year with Poisson distribution. The numerator was the number of injuries in each professional group on focus, while the denominator was the number of person-years in the equivalent group of the workforce. Person-years were calculated separately in all strata, meaning that a person could contribute in different groups for each year.
We further analyzed the data with Joinpoint regression model to investigate the pattern of the incidence rates. Joinpoint regression model analyses rates, proportions, and any other measure that can be considered (e.g., counts) over time, in order to identify the possible time points at which any given trend changes (these are the joinpoints) and to estimate the regression function with the previously identified joinpoints (23).
We used the log transformation of half-yearly data from 2010 to 2016 and we fixed to 1 the maximum number of joinpoints. We selected the final model using the method of Permutation Test (PT) with alpha 0.05.
Among injuries, we performed a categorization of nurses’ injuries (yes/no) and physicians’ injuries (yes/no) and we performed a separate logistic model to investigate the factors associated with injuries. The variables sex, age (20-40; 41-60), years of practice (continuous), area of practice (medicine/surgery), needlestick injuries (yes/no), timing of injury (morning, afternoon, night), type of involved procedures (needle use, surgery, other) were entered as covariates in a multiple logistic regression model to identify factors associated with injuries among physicians and nurses separately, with the backward stepwise procedures (pe=0.15, pr=0.20). The odds ratios (OR) and the 95% confidence intervals (95% CI) were calculated. The Joinpoint Regression Program, Version 4.5.0.1 - June 2017; Statistical Methodology and Applications Branch, Surveillance Research Program, National Cancer Institute was used for the Jointpoint regression analysis (http://www.srab.cancer.gov/joinpoint/), while Stata 14 was used for all other analysis; alpha error was set at 0.05.
Results
Three hundred and thirty-five injuries were collected from 2010 to 2016, related to 5,671 HCWs. The analyses were based on high quality records. The fraction of missing information (FMI) was 0.3% for seven variables (one missing) and 1.8% for one variable (six missing).
The overall incidence rate of work injuries per 100 person-years was 5.9 (95% CI: 5.3 to 6.6).
Table 1 describes the injured HCWs, reporting demographic and professional characteristics during the study period.
Table 1.
Characteristics of the HCWs with injuries (n=335)
| Age (mean±sd) | 41.3±12.0 |
| Gender | |
| Female | 243 (73%) |
| Male | 92 (27%) |
| Job category | |
| Physician | 64 (19%) |
| Nurse | 144 (43%) |
| Nursing student | 65 (20%) |
| Healthcare assistants (HCAs) | 38 (11%) |
| Other professions | 24 (7%) |
| Years of practice (mean±sd) | 11.19±9.7 |
| Department | |
| Surgery | 106 (32%) |
| Medicine | 87 (26%) |
| Emergency | 90 (27%) |
| Operating room | 9 (3%) |
| Others | 41 (12%) |
| Aspartate Aminotransferase (AST)* | 21.9±6.8 |
| Normal § | 323 (96%) |
| Abnormal | 11 (4%) |
| Alanine aminotransferase (ALT)* | 25,2±11,3 |
| Normal §§ | 326 (97%) |
| Abnormal | 8 (3%) |
| Vaccination for HBV | 316 (94%) |
| Protective title use for HBV (yes) | 290 (87%) |
| Anti HBs positive (>10 UI/L) | 288 (86%) |
| Seroconversion | |
| HCV | 0% |
| HIV | 0% |
* Totals differ from 335 due to missing data
§ Normal range: 15-46 U/L ; §§ Normal range: 7-56 U/L
HBV: Hepatitis C Virus; Anti HBs: anti-Hepatitis B surface; HCV: Hepatitis C Virus; HIV: Human Immunodeficiency Virus
Table 2 reports the characteristics of the injuries. The majority of the injuries were registered in the hospital stay, during the needle disposal procedure, in the antemeridian shift and in 70% of cases they were represented by needlestick injuries.
Table 2.
Characteristics of injuries collected in SS. Filippo e Nicola Hospital from 2010 to 2016 (n=335)
| n (%) | |
| Place of injury * | |
| Hospital stay | 141 (42.09%) |
| Operating room | 58 (17.31%) |
| Emergency room | 31 (9.25%) |
| Medical center | 19 (5.67%) |
| Intensive care/Resuscitation | 19 (5.67%) |
| Laboratory | 15 (4.48%) |
| Medical clinic | 11 (3.28%) |
| Sector room/Engraver | 9 (2.69%) |
| Diagnostic Room | 5 (1.49%) |
| Angiographic room | 3 (0.90%) |
| Home care activities | 3 (0.90%) |
| Ambulance | 2 (0.60%) |
| Hemodynamic room | 2 (0.60%) |
| Sterilization center | 1 (0.30%) |
| Timing of injury* | |
| Morning (07:00 – 14:00) | 180 (53.8%) |
| Afternoon (14:00 – 21:00) | 112 (33.4%) |
| Night (21:00 – 07:00) | 39 (11.6%) |
| Type of exposition* | |
| Needlestick injuries | 229 (69.55%) |
| Mucosal exposure | 47 (14.03%) |
| Sharp wound | 35 (10.45%) |
| Damaged skin exposure | 19 (5.67%) |
| Not known | 1 (0.30%) |
| Individual protection devices use | |
| Yes | 300 (89.55%) |
| No | 35 (10.45%) |
| Procedure being performed at the time of exposure | |
| Needle disposal | 50 (14.93%) |
| Withdrawal | 33 (9.85%) |
| Surgery | 33 (9.85%) |
| Waste/linen disposal | 15 (4.48%) |
| Drip removal | 21 (6.27%) |
| Intramuscular injection | 9 (2.69%) |
| Laboratory activity | 8 (2.39%) |
| Surgical instruments washing | 6 (1.79%) |
| Dialysis switch-off | 1 (0.30%) |
| Recapping | 1 (0.30%) |
| Other practices | 158 (47.16%) |
*Totals differ from 335 due to missing data
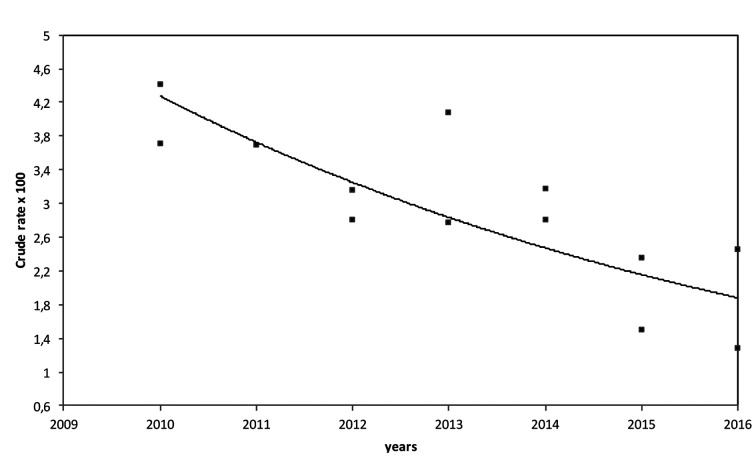
The joint regression analysis didn’t report jointpoint for risk injuries during the 6 years study period (p=0.25), but indicated a significant negative trend (β=-0.12, p<0.001) with a significant annual change percent ACP=-11.3 (CI95%: -16.3 - -5.9, p<0.001) (figure 1).
Figure 1.
Injuries trend during the study period 2010-2016 (crude rate*100 person-years): ACP 11.27 (p<0.01)
The trend of injuries that occurred in the afternoon was significantly decreased ACP=-17.2; [95% CI: -24.7 - -12.9, p<0.001]. There was a significant negative trend for needlestick injuries with ACP= -5.1 [95% CI: -8.8 - -1.3 p<0.00]. In general, there were negative trends for females and males with ACP (females)=-4.6; [95% CI: -8.1 - -0.9, p<0.001], and ACP (males) -5.8; [95% CI: -10.3 - -1.1, p<0.001].
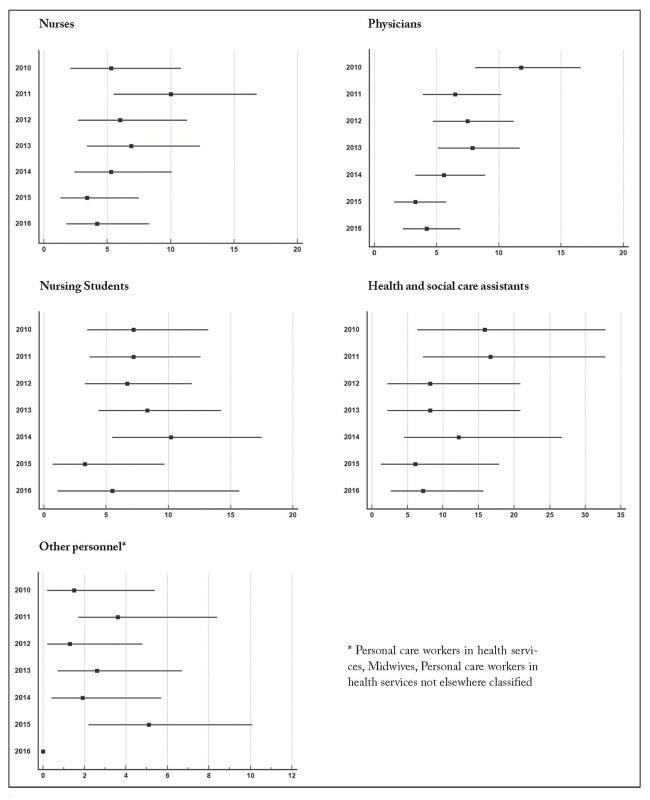
Trend analysis indicated a significant decline for injuries among nurses and health and social care assistants with ACP=-15.7; [95% CI: -24.3 - -6.2, p<0.001] and ACP=-13.2; [95% CI: -23.1 - -2.0, p<0.001], respectively. Negative trends were also estimated for other professional categories but the reduction was not significant.
As reported in figure 2, among nurses, the incidence rate estimated in 2010 (11.8*100 person-years) was significantly higher than the rate calculated in 2015 (3.3*100 person-years) and the rate calculated in 2016 (4.2*100 person-years).
Figure 2.
Incidence rate (x100 person-years) for personnel employed in SS Filippo e Nicola Hospital (2010-2016)
The multivariate logistic model indicated that for physicians, male gender and surgical intervention were risk factors for injuries, while for nurses, male gender and working in the surgical area, rather than the medical area, were protective factors (table 3).
Table 3.
Associations between factors and injuries among Physicians and Nurses (Multivariate Logistic regression analysis)
| Job category | Variables | OR | p | 95% CI |
| Physicians | ||||
| Gender | ||||
| Female | 1 | |||
| Male | 3.67 | 0.00 | 1.9-7.1 | |
| Timing of injury | ||||
| Morning (7am-2pm) | 1 | |||
| Afternoon (2pm-9pm) | 2.0 | 0.04 | 1.0-3.9 | |
| Type of procedures involved | ||||
| Needle use | 1 | |||
| Surgical intervention | 7.71 | 0.00 | 3.2-18.4 | |
| Nurses | ||||
| Gender | ||||
| Female | 1 | |||
| Male | 0.31 | 0.00 | 0.2-0.6 | |
| Age (range) | ||||
| 20-40 | ||||
| 41-60 | 1.62 | 0.11 | 0.9-2.9 | |
| Years of practice | 1.04 | 0.02 | 1.0-1.1 | |
| Timing of injury | ||||
| Morning (7am-2pm) | 1 | |||
| Afternoon (2pm-9pm) | 2.1 | 0.01 | 1.2-3.7 | |
| Night (9pm-7am) | 8.8 | 0.00 | 3.4-22.8 | |
| Area of practice | ||||
| Medicine | 1 | |||
| Surgery | 0.36 | 0.00 | 0.2-0.6 |
Discussion
Injuries with biological risk among HCWs represent the main professional risk in the hospital setting (40-50% total) with the hazard of significant costs, increasing over time (16, 26).
We evaluated annual injuries with biological risk incidence rates among HCWs in an Italian hospital from 2010 to 2016. The overall incidence rate of work injuries per 100 person-years was 5.9 (95% CI: 5.3 to 6.6), and as expected, because of the introduction of new legislation, the trend was significantly negative with ACP=-11.3; [CI95%: -16.3 - -5.9; p<0.001].
The reduction was expected as a consequence of the introduction of the Law “Testo unico sulla salute e sicurezza sul lavoro (2008)” and the following European directive of 2010. This reduction was probably correlated to the fact that in the examined Hospital, since 2013/2014 specific programs of prevention for HCWs safety at work were promoted.
According to Macias et al., injuries mainly occur during the morning, likely because in this time period there is more personnel at work and the activity in Italian hospital units is more intense, compared to afternoon and evening shifts (15).
Injury time trends based on time slots showed a significant decrease only in the afternoon shift with ACP=-17.2; [CI 95%: -24,7 - -12,9, p<0,001]. Our analysis highlighted that the nursing category is mainly affected, in line with the evidence provided by previous studies (10, 19, 25, 26). The incidents reported by nurses or health and social assistants significantly diminished with time and in particular the incidence rates amongst nurses were reduced from 2015.
For the categories of physicians, nursing students and other operators, the trend was negative but it was not significant. This result appears to be in line with what was reported by the 2012 Italian study, in which it was emphasized that nurses were more cautious in prevention than physicians (8).
The study points out that in the examined hospital, the majority of injuries were linked to needlestick injuries with a total value of 70% in line with what was reported by Di Bari et al. (75%) and Davanzo et al. (76%) but in contrast with the data reported in other studies (4, 19, 21). The differences highlighted should probably be considered in relation to the conclusions drawn by other studies, as well as the different logistical characteristics of the hospitals investigated and the various relevant health authorities.
The study has noted that needlestick injury trends have significantly decreased with ACP=-5.1 [CI 95%: -8.8 - -1.3; p<0.001], underlining a meaningful decrease from 2014, likely correlated to the implementation of security procedures in the hospital over the years.
The risk of needlestick injuries and infection through contaminated blood is usually a consequence of inadequate use of personal protection devices; in this case it is stressed that the primary method to avoid these injuries is represented by the correct and scrupulous application of the standard precautions (12, 18, 28).
From our analysis, thirty-one injuries (9%) occurred to HCWs without the appropriate protection, lower than the 31% reported by a German study (3).
In our study, a statistically significant relationship was found between the occurrence of injuries and gender, in line with the study of Pili et al (20).
Males were at risk less than females among nurses (OR=0.31; 95% CI: 0.17-0.59), but more than females among physicians (OR=3.32; 95% CI:1.8-6.2). This result could be related to the unbalance gender data between physicians and non-physicians health workers.
Our results are consistent with the findings from different studies about the fact that female nurses were at higher risk of injuries than other HCWs, particularly for needlestick injuries, in developed as well as developing countries (1, 29).
Some studies report that work experience is associated with injuries: in our study, years of practice is not a factor associated with injuries neither among doctors nor nurses (3,18).
There are some limitations in this study that should be taken into consideration when interpreting the results.
A limit of the study is that the collected data don’t allow us to correlate the injuries with the typology of treated patients, neither with the hours worked by the employees at the moment of the injury, that could represent an important risk factor (9).
However, the study could be useful for a first level analysis - at low cost- to identify the personnel categories or the areas that need to be studied further.
Another limit of the study is the lack of information about the subsequent work absence caused by the injury, that would allow an investigation of the knock-on costs resulting from the injury.
Nevertheless, the study could represent a valuable resource both for the sensitization of the biological risk theme and for the protection of workers’ health. The research confirms the importance of a surveillance system and prevention strategies, in the business and the social perspective to control the costs associated with the work accident. While the costs for their prevention may seem high at the beginning, ultimately they prove to be the opposite because of resulting cost savings (16).
Conclusions
The call to prevention and security management among health care workers has certainly contributed to the better administration of the injury risk and the biological risk amongst the hospital employees in the case study. The hope is to implement a surveillance system that could promptly allow to intervene in a specific and effective manner for the control of injuries, mainly in the categories in which a significant reduction wasn’t registered.
No potential conflict of interest relevant to this article was reported by the authors
References
- 1.Afridi AA, Kumar A, Sayani R. Needle stick injuries-risk and preventive factors: a study among health care workers in tertiary care hospitals in Pakistan. Glob J Health Sci. 2013;5:85–92. doi: 10.5539/gjhs.v5n4p85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bergamini M, Cucchi A, Stefanati A, et al. Knowledge of preventive measures against occupational risks and spread of healthcare-associated infections among nursing students. An epidemiological prevalence study from Ferrara, Italy. J Prev Med Hyg. 2009;50:96–101. [PubMed] [Google Scholar]
- 3.Chalya PL, Seni J, Mushi MF, et al. Needle-stick injuries and splash exposures among health-care workers at a tertiary care hospital in north-western Tanzania. Tanzania Journal of Health Research. 2015:17. [Google Scholar]
- 4.Chambers A, Mustard CA, Etches J. Trends in needle-stick injury incidence following regulatory change in Ontario, Canada (2004-2012): an observational study. Bmc Health Services Research. 2015:15. doi: 10.1186/s12913-015-0798-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Corrao CR, Mazzotta A, La Torre G, et al. Biological risk and occupational health. Ind Health. 2012;50:326–337. doi: 10.2486/indhealth.ms1324. [DOI] [PubMed] [Google Scholar]
- 6.Council Directive 2010/32/EU [Google Scholar]
- 7.Crescenzi F, Scarpati F, Cannavacciuolo L. Injuries with biological risk within Salerno ASL hospitals: descriptive epidemiologic analyses in the period 2006-2008. G Ital Med Lav Ergon. 2011:266–268. [PubMed] [Google Scholar]
- 8.Davanzo E, Frasson C, Morandin M, et al. Occupational blood and body fluid exposure of university health care workers. Am J Infect Control. 2008;36:753–756. doi: 10.1016/j.ajic.2008.04.254. [DOI] [PubMed] [Google Scholar]
- 9.Dembe AE, Erickson JB, Delbos RG, et al. The impact of overtime and long work hours on occupational injuries and illnesses: new evidence from the United States. Occup Environ Med. 2005;62:588–597. doi: 10.1136/oem.2004.016667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Di Bari V, De Carli G, Puro V, et al. Prevention of accidental needle sticks before the Directive 2010/32/EU in a sample of Italian hospitals. Med Lav. 2015;106:186–205. [PubMed] [Google Scholar]
- 11.Ferrario MM, Landone S, De Biasi M, et al. Time trends of incidence rates of work accident with blood contamination in a North Italian teaching hospital. G Ital Med Lav Ergon. 2012;34:275–277. [PubMed] [Google Scholar]
- 12.Garner JS. Guideline for isolation precautions in hospitals. The Hospital Infection Control Practices Advisory Committee. Infect Control Hosp Epidemiol. 1996;17:53–80. doi: 10.1086/647190. [DOI] [PubMed] [Google Scholar]
- 13.Graia S, Daglio M, Colombo R, et al. Rischio di malattie a trasmissione ematica nel personale ostetrico: aggiornamento della casistica pavese. Bollettino della Società Medico Chirurgica di Pavia. 2011:661–668. [Google Scholar]
- 14.Legislative Decree. (2008). Testo unico sulla salute e sicurezza sul lavoro. N. 81 [Google Scholar]
- 15.Macias DJ, Hafner J, Brillman JC, et al. Effect of time of day and duration into shift on hazardous exposures to biological fluids. Acad Emerg Med. 1996;3:605–610. doi: 10.1111/j.1553-2712.1996.tb03471.x. [DOI] [PubMed] [Google Scholar]
- 16.Mannocci A, De Carli G, Di Bari V, et al. How Much do Needlestick Injuries Cost? A Systematic Review of the Economic Evaluations of Needlestick and Sharps Injuries Among Healthcare Personnel. Infect Control Hosp Epidemiol. 2016;37:635–646. doi: 10.1017/ice.2016.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Martins A, Coelho AC, Vieira M, et al. Age and years in practice as factors associated with needlestick and sharps injuries among health care workers in a Portuguese hospital. Accid Anal Prev. 2012;47:11–15. doi: 10.1016/j.aap.2012.01.011. [DOI] [PubMed] [Google Scholar]
- 18.Marziale MH, Nishimura KY, Ferreira MM. Contamination risks caused by occupational accidents with cutting and piercing material among nursing workers. Rev Lat Am Enfermagem. 2004;12:36–42. doi: 10.1590/s0104-11692004000100006. [DOI] [PubMed] [Google Scholar]
- 19.Parco S, Vascotto F, Simeone R, et al. Manual accidents, biological risk control, and quality indicators at a children’s hospital in north-east Italy. Risk Manag Healthc Policy. 2015;8:37–43. doi: 10.2147/RMHP.S77490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Parsa-Pili J, Izadi N, Golbabaei F. Factors associated with needlestick and sharp injuries among health care workers. International Journal of Occupational Hygiene. 2013;5:191–197. [Google Scholar]
- 21.Porta C, Handelman E, McGovern P. Needlestick injuries among health care workers. A literature review. AAOHN J. 1999;47:237–244. [PubMed] [Google Scholar]
- 22.Puro V, De Carli G, Segata A, et al. Update on the subject of epidemiology of blood-transmitted occupational infections. G Ital Med Lav Ergon. 2010;32:235–239. [PubMed] [Google Scholar]
- 23.Rea F, Pagan E, Compagnoni MM, et al. Joinpoint regression analysis with time-on-study as time-scale. Application to three Italian population-based cohort studies. Epidemiology Biostatistics and Public Health. 2017:14. [Google Scholar]
- 24.Rim KT, Lim CH. Biologically hazardous agents at work and efforts to protect workers’ health: a review of recent reports. Saf Health Work. 2014;5:43–52. doi: 10.1016/j.shaw.2014.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sindoni L, Calisto ML, Alfino D, et al. Retrospective survey on epidemiologic monitoring of accidents due to professional exposure to biological agents in A.O.U. “G. Martino” of Messina, Italy) Ann Ig. 2005;17:67–74. [PubMed] [Google Scholar]
- 26.Stefanati A, Boschetto P, Previato S, et al. A survey on injuries among nurses and nursing students: a descriptive epidemiologic analysis between 2002 and 2012 at a University Hospital. Med Lav. 2015;106:216–229. [PubMed] [Google Scholar]
- 27.Valent F, Liva G, Bellomo F, et al. An ecological study on the association between characteristics of hospital units and the risk of occupational injuries and adverse events on the example of an Italian teaching hospital. Int J Occup Med Environ Health. 2016;29:149–159. doi: 10.13075/ijomeh.1896.00580. [DOI] [PubMed] [Google Scholar]
- 28.Wicker S, Jung J, Allwinn R, et al. Prevalence and prevention of needlestick injuries among health care workers in a German university hospital. Int Arch Occup Environ Health. 2008;81:347–354. doi: 10.1007/s00420-007-0219-7. [DOI] [PubMed] [Google Scholar]
- 29.Zurn P, Dal Poz MR, Stilwell B, et al. Imbalance in the health workforce. Hum Resour Health. 2004;2:13. doi: 10.1186/1478-4491-2-13. [DOI] [PMC free article] [PubMed] [Google Scholar]