Abstract
Background:
Emotional demands may be a significant risk factor for wellbeing in healthcare professionals. Nurses have been considered the most exposed to emotional burden known as emotional labour. Scholars define it as the process by which nurses sometimes hide/fake the real emotion or struggle to display the appropriate emotion to meet the emotional work requirements. Emotional labour can result in physical, psychological and behavioural disorders. A specific tool to measure it among nurses is still missing.
Objectives:
This study aims to develop and validate an emotional labour scale for nurses.
Methods:
The design process consisted of three different phases. In the first one, 24 items have been selected from different tools. The second consisted of the assessment of the face and content validity. In the third phase, the Emotional labour scale has been psychometrically evaluated through a cross validation approach, including both exploratory factor analysis performed on a sample of 205 Italian nurses, with the final selection of an 11- items tool, and confirmatory factor analysis.
Results:
Emotional labour is acted through surface acting, compliance and restraint. The Emotional Labour Nursing scale showed good psychometric properties and was found to be valid and reliable for assessing emotional labour among nurses. The association between emotional labour and burnout was investigated.
Conclusions:
The Emotional Labour scale may foster a fuller understanding of the consequences of emotional labour. Since emotional demands and emotional labour are not included in the most common psychosocial risk assessment tools currently available, our results point out to their role in work stress prevention.
Key words: Emotional labour, nurses, burnout, validation scale, emotional burden
Abstract
«Sviluppo e validazione in Italia della Scala dell’Emotional Labour negli infermieri».
Introduzione:
Le richieste emotive possono rappresentare un significativo fattore di rischio per il benessere degli operatori sanitari. Gli infermieri vengono considerarti la categoria professionale più esposta al disagio emotivo conosciuto come emotional labor. I ricercatori definiscono l’emotional labor come il processo attraverso il quale gli infermieri a volte nascondono o falsificano le emozioni realmente sentite o si sforzano di mostrare l’emozione appropriata allo scopo di soddisfare le esigenze emotive dettate dal proprio lavoro. L’emotional labor può dare luogo a disturbi di tipo fisico, psicologico e del comportamento. Uno strumento specifico che misuri l’emotional labor negli infermioeri ancora è mancante.
Obiettivi:
Questo studio ha l’obiettivo di sviluppare e validare una scala per la misurazione dell’emotional labor negli infermieri.
Metodi:
Il processo di ricerca si è sviluppato in 3 diverse fasi. Nella prima, 24 items sono stati selezionati da diversi strumenti. La seconda fase ha comportato la valutazione della validità di facciata e di contenuto. Nella terza fase la scala dell’emotional labor è stata valutata psicometricamente con un approccio di validazione incrociata che ha incluso sia l’analisi fattoriale esplorativa condotta su un campione di 205 infermieri italiani, con la selezione di una scala a 11 items, che l’analisi fattoriale confermativa.
Risultati:
L’emotional labor consta di 3 dimensioni: recitazione, adesione e controllo. La scala dell’emotional labor ha evidenziato buone proprietà psicometriche ed è un valido e affidabile strumento per la misurazione dell’emotional labour negli infermieri. Infine è stata indagata l’ associazione tra l’emotional labour e il burnout.
Conclusioni:
La scala dell’emotional labor può favorire una più completa comprensione delle conseguenze dell’emotional labour negli infermieri. Poiché le richieste emotive e l’emotional labour non sono inclusi tra i più comuni strumenti di valutazione del rischio psicosociale lavorativo attualmente disponibili, i nostri risultati evidenziano il loro ruolo nella prevenzione dello stress lavorativo.
Table S1.
Synopsis of items deleted through CVI and EFA
Tavola S1. Sinopsi degli items rimossi dopo CVI e EFA
Introduction
Although it is widely acknowledged that emotional demands may be a critical stress factor in certain occupations, such as in health care professions, they are often underestimated. Continuous and prolonged exposure to emotional demands is a risk factor for mental distress and international literature has recognized its role together with common psychosocial and personal psychological risk factors in health care organizations (8,29). The health care professionals, such as nurses, are one of the most exposed, and scholars are paying more attention to emotional demands and the role of the emotional labour on the genesis of work related stress. Emotional labour (EL) refers to the management of emotions and emotional displays in interpersonal relationships occurring in the workplace. Hochschild (40), the originator of EL theory, argued that some workers, especially those engaged in interpersonal relationships in the workplace, are sometimes required to suppress authentic emotions and to display emotions deemed more appropriate.
In over 30 years of research, different research perspectives and ways of conceptualizing and investigating EL have been proposed (37). Grandey tried to summarize different conceptualizations defining that what makes “EL is when emotion regulation is performed in response to job based emotional requirements in order to achieve organizational goals” (37, p. 18).
Scholars have developed various scales to fit these theoretical perspectives of EL (12, 21, 22, 24, 32, 35, 53, 54, 55, 59, 61, 74, 77, 82, 85, 96). Although scholars have shown a growing interest in EL among nurses (92), Glomb and Tews (35) note that the literature provides no clear consensus about how to measure emotional labour. A review of the literature reveals many EL tools, but scholars sometimes do not define these tools’ underlying theoretical dimensions, nor do they clearly define the comprehensive bounds of EL among nurses (24, 32, 53, 69, 74). Although there are different tools, no scale has been developed and validated exclusively for nurses. Different measurement scales have been validated on mixed samples, which included health care professionals, doctors, nurses, teachers, call centers, debt collectors and other ones (12, 21, 22, 24, 32, 35, 54, 74, 77, 82, 85, 96). Some scholars have used items from different scales to capture the complexity of EL (69). Other authors have suggested the need for a specific model to investigate the specificity of EL in healthcare professionals (62) but didn’t validate a specific measurement scale to measure EL among nurses. This highlights the fact that the specificity of EL among nurses has been discounted even if the relationships with patients are a central component of nursing work. Nurses engage in deeper interactions with the patient than other health care professionals, thereby they could be at high risk of experiencing EL (49, 63).
Nursing profession lacks a specific operationalization of the EL construct and we do not have a valid and reliable tool to measure the EL among Italian nurses; moreover, most of the research on EL focused on understanding the negative outcomes for employees and organizations and neglected the importance to correctly measure EL in different research contexts (43).
Several studies found significant associations between emotional exhaustion, depersonalization, disengagement and EL (17, 43, 50). The Job Demand Control model clarifies how an organizational context, characterized by high demands, can generate burnout syndrome.
Moreover, interpersonal strain, a construct studied together with burnout, is a new burnout facet because it measures relational overload and explores stress deriving from emotional requirements (19, 20). It is significant for nurses because they are exposed to increasing emotional demands.
The Management Standards Model from Health and Safety Executive (ISPSEL-HSE), a tool validated to measure work related stress, does not widely evaluate the stress generated by the management of emotional demands in working relationships (47). To fill this gap in the research, our study aimed to develop and psychometrically evaluate a scale measuring EL among Italian nurses. We also aimed to test its correlations with burnout dimensions.
Background
Emotional management is a core competence in nursing practice (38). A review of the concept of EL has clarified this phenomenon and identified its most common facets, surface acting (SA) and deep acting (DA) (43). Deep acting “is equivalent to managing the underlying feelings to really and truly feel the emotion required by display rules” (48, p. 319). Surface acting occurs when “the worker falsifies his emotions by changing the external behavior to adapt to the display rules required by the organization, while their innermost feelings remain unaltered “ (51, p. 349). Other concepts have been introduced, but, as highlighted in a recent review, they are related concepts such as emotional dissonance, emotional suppression, etc (6). Emotional dissonance is described as discrepancy between required and felt emotions, or the conflict between experienced emotions and emotions expressed to conform to display rules (1, 45).
The expectation that nurses should be emotionally involved in care is present among patients and health care organizations, as well as in the conventional images of nursing care (93). Nurses can experience many emotions in their job: frustration towards a patient with unrealistic expectations, hopelessness when a patient’s prognosis is poor or sadness when a patient is dying and there is nothing more to do. They can also experience happiness, for example when a patient recovers and is discharged home. Moreover, nurses must continuously face both pleasant and unpleasant situations (46). Depending on the situation, nurses may be expected to suppress undesired emotions (i.e. frustration), to express other emotions deemed more appropriate (i.e. happiness) or to show neutrality. This can constitute EL.
Nurses perform EL in many situations. For example, they may need to suppress anger or frustration when facing disrespectful patients. They may also need to express feelings of sympathy or display friendly emotions as appropriate in certain situations (60).
The discrepancy between true feelings and expressed emotions can be deleterious over time, and this can serve to increase nurses’ stress and negatively affect their well-being (23, 40). The need to display appropriate emotions while hiding negative ones can contribute to role overload and burnout. A review indicated significant associations between emotional exhaustion, depersonalization and EL (17, 43, 50). According to Maslach (64), the requirement to care for patients and continuously meet emotional demands is emotionally burdensome for health care professionals. Some authors have argued that emotion management and EL could factor into a nurse’s workload (63). EL can negatively affect a nurse’s job performance, the quality of care provided and patient satisfaction, it can also impact patients’ psychological and physical well-being (25, 34, 52, 73). A valid and reliable tool measuring emotional labour, designed specifically for nurses, would facilitate the investigation of EL and its relationships with burnout and interpersonal strain.
Methods
Design
This study used a cross sectional design to develop and psychometrically evaluate a scale measuring EL among nurses. The design process consisted of three different phases. In the first one, 24 items have been selected from different tools. The second phase consisted of an assessment of the face, content and cultural validity of the Emotional Labour in Nursing scale (ELNS). In the third phase, the ELNS has been evaluated psychometrically through a cross validation approach, including both exploratory factor analysis (EFA), performed on a sample of 205 Italian nurses, with the final selection of an 11- item tool, and confirmatory factor analysis (CFA).
Phase 1: Development of the ELN scale
In the first phase, the authors reviewed the most used and relevant tools (12, 21, 22,24, 32, 35, 53, 54, 55, 60, 61, 74, 77, 82, 85, 96). They have not been developed for nurses, but targeted to various health care professionals and workers. So the authors selected items relevant for nurses and suitable in the Italian health care context. The items selected refer to EL behavioral strategies and refer both to surface and to deeper behavioral strategies. The authors chose to adopt EL conceptualization that consider EL a strategy to display the appropriate emotion “in response to job based emotional requirements in order to achieve organizational goals” (37). According to authors EL for nurses is the act of displaying appropriate emotions in face-to-face interactions with patients in response to job-based emotional requirements. This emotional labour is an intrinsic part of the nurse’s work role. To display appropriate emotions, nurses must sometimes hide or fake felt emotions, if inappropriate in some situations, or they have to try to experience expected emotions. Therefore, EL consists of intentional behaviour and strategies that allow the management of dissonance between real feelings and displayed emotions.
In the next phase, items deriving from different EL scales (12, 21, 22, 24, 32, 35, 53, 54, 55, 60, 61, 74, 77, 82, 85, 96) have been translated into Italian by the first author. The resulting translation was reviewed by a researcher and a psychologist to make the items more fluid and culturally relevant. Each item was then translated into English by a bilingual translator. Then, the original and translated versions of the items were compared to confirm conceptual equivalence. Afterwards, to select the most relevant items, a panel of three experts (an organizational researcher, a nurse researcher, and a psychologist) was asked to rate the relevance of each item according to the given definition of EL among nurses. The experts responded using a scale ranging from 0 (disagree) to 4 (completely agree). The items yielding an average score of <3 were deleted or modified. The experts deleted some items not appropriate for nurses or not suitable for the Italian health care system. The experts selected items 1, 2, 3, 4 and 5 from the surface acting subscale and items 6, 7 and 8 from the deep acting subscale from Brotheridge and Lee’s (22) Emotional Labour Scale. In addition, they included all of the items from Mann’s (63) Emotional Requirements Inventory (MERI) (items 9, 11, 18, 19 and 22 from the emotional suppression subscale; items 10, 12, 13, 14, 16 and 17 from the emotional faking subscale and items 15, 20, 21, 23 and 24 from the expectations about emotional display subscale). Mann’s Emotional Requirements Inventory (MERI), which was originally a scale of agreement/disagreement ranging from 1 to 8, has been converted into a frequency measure on a five-point Likert scale.
The final composition consisted of 24 items selected from different existing scales. The tool is rated on a five-point Likert scale ranging (from 1=never to 5 = very often). Higher scores indicate higher EL.
Phase 2
Face and content validity
In the second phase, the initial draft of the tool with 24 items identified was given to 10 specialists with experience in the EL field (five psychologists and five nursing researchers) in the form of a content validity index (CVI). By tradition, and based on the advice of Lynn (57), as well as Waltz and Bausell (89), the items were rated on a four-point ordinal scale (from 1=not relevant to 4=highly relevant). The experts also answered open-ended questions regarding the clarity of the items and provided suggestions. Based on Lynn (57) and Polit and Beck (71), we computed the content validity index of individual items (I-CVI) and the content validity index of the overall scale (S-CVI) as “the proportion of items of an instrument that achieved a rating of 3 or 4 by the content experts” (11, p. 209). Not every item yielded adequate content validity (>0.78).
Other instruments
To evaluate the concurrent validity of the 11-item ELN scale, the authors decided to use the Emotion Work Requirement Scale.
Emotion Work Requirement Scale. We used all items from Best, Downey and Jones’ Emotion Work Requirement scale (EWRS) (12). EWRS includes seven items on a five-point scale (1=not at all, 5=always required). It assesses job’s emotional requirements and measures the extent to which nurses are required to show or hide an emotion in order to be effective and to reach organizational goals. (i.e. how many times one is required to express friendly emotions, how many times one is required to hide fear and to express calm). They measure similar constructs, emotion requirements at work.
To test the EL correlations to burnout, we used the Maslach Burnout Inventory.
Maslach Burnout Inventory. Burnout was measured through the dimensions of emotional exhaustion, cynicism and interpersonal strain. The last dimension was included to account for the theoretical construct of relational work overload; it assesses the social strain reaction associated with different types of work relationships (19, 28, 79). For the first two dimensions, we used the Maslach Burnout Inventory–General Survey (MBI-GS) (18, 65, 78). For the third dimension, we used the six-item Interpersonal Strain at Work scale (19, 20). Interpersonal strain has recently been proposed as a new facet of burnout corresponding to the disengagement reaction in working relationships (20). The tool investigates the frequency by which worker is exposed to relational distress situations at work (i.e. “At work I find myself to be insensitive to other people’s problems” or “At work, I feel more comfortable keeping my distance from other people”). Interpersonal strain is relevant for nurses since they are exposed to increasing interpersonal and emotional demands. The resulting instrument to measure burnout is an 18-item scale using a seven-point Likert scale ranging from 0 (none) to 6 (every day). Higher scores on the subscales of emotional exhaustion, depersonalization and interpersonal strain denote greater levels of burnout.
Phase 3: Psychometric testing
Participants and setting
Institutional review board approval was obtained for this study from the ethics committee of the hospital. Once ethical approval was obtained, different workplaces were approached.
The sample was recruited from among Italian RNs (Registered Nurses) employed in two university hospitals located in northern and central Italy, including nurses from an intensive care unit and a trauma centre. Data were collected between September and December 2016. A total of 500 paper questionnaires were distributed to all hospital nurses. The final sample was composed of 409 nurses who had correctly completed the questionnaire (a 90.8% response rate). The participants were approached by nursing students specifically trained in the administration of the questionnaire. An informational letter was attached to the questionnaire to describe the aim of the study. Potential respondents were assured that their participation in the study was voluntary and that the information they provided would be protected. Responses were anonymous and untraceable to individual nurses. Participants were given one week to complete the questionnaires. Surveys were returned and placed in a drop-off box located in the nursing administration office.
Data analysis
Descriptive statistics (mean, standard deviation [SD], frequency and percentage) were used to describe the socio-demographic characteristics of the sample (age, gender, sex, previous profession and education) as well as to analyse item scores. Skewness and kurtosis indices were used to evaluate item distribution. Missing data were ensured to be missing at random.
Construct validity was assessed through exploratory factorial analysis (EFA) and confirmatory factor analysis (CFA). We used a cross validation approach, randomly splitting the sample into two subgroups (by odd and even participant codes). We performed an EFA on the first subgroup (N=205) and CFA on the second subgroup (N=204). Before proceeding with EFA, Bartlett’s sphericity test and the Keiser-Meyer-Olkin indicator were examined to assess the factorability of the correlation matrix. EFA was conducted using promax oblique rotation. We assessed the best EFA solution and the number of factors to extract based on multiple criteria: the simplicity of the solution (primary factor loadings >0.30 and no cross loadings), the interpretability of the factor structure (88), a screen plot of eigenvalues and the theoretical sense of the factors (27) (table 1). CFA was performed using the robust maximum likelihood estimator method (MLR), which produces standard maximum likelihood parameter estimates with corrected standard errors and chi-square test statistics robust to non-normality and non-independence of observations (68).
Table 1.
Factor Loading at EFA and psychometric characteristics of items of Emotional Labor scale among nurses (N=205)
| Mean | SD | Skew | Kurt | F1 | F2 | F3 | ||
| 1) | I resist expressing my true feelings | 2.89 | 0.96 | -0.11 | -0.33 | -0.02 | 0.63 | -0.01 |
| 2) | I pretend to have emotions that I don’t really feel | 2.01 | 1.02 | 0.63 | -0.54 | 0.52 | 0.38 | -0.17 |
| 3) | I hide my true feelings about a situation | 2.53 | 0.97 | 0.04 | -0.56 | 0.10 | 0.76 | -0.10 |
| 4) | I make an effort to actually feel the emotions that I need to display toward others | 2.16 | 1.06 | 0.45 | -0.86 | 0.58 | 0.18 | 0.01 |
| 5) | In some moments, I intentionally convey (or attempt to convey) a positive emotion or feeling that I don’t really feel but that is appropriate at the time (I pretend to be happy, excited, interested) | 2.28 | 1.04 | 0.25 | -0.91 | 0.71 | 0.02 | 0.23 |
| 6) | In some moments, I intentionally convey (or attempt to convey) a negative emotion or feeling that I don’t really feel but that is appropriate at the time (I pretend to be angry, upset, dismayed, etc.) | 1.88 | 0.90 | 0.65 | -0.60 | 0.86 | -0.16 | -0.01 |
| 7) | I feel that I suppress or hide (or try to) positive emotions in some moments (e.g. I feel happy or excited but I try not to show it) | 2.12 | 0.92 | 0.05 | -0.51 | 0.15 | 0.54 | 0.03 |
| 8) | I feel that I suppress or hide (or try to) negative emotions in some moments (e.g. I feel angry, depressed or dismayed but I try not to show it) | 2.65 | 0.93 | 0.05 | -0.51 | -0.22 | 0.63 | 0.33 |
| 9) | I feel in some moments, the other person expect me to have a particular “face” or disposition (e.g. expect me to act friendly, helpful, caregiver, warm, etc.) | 2.67 | 1.06 | -0.01 | -0.66 | 0.15 | 0.02 | 0.63 |
| 10) | I think that there are rules or protocol about how I have to speak or act during interactions with others (e.g. my employers expect people in my position to behave in a certain way or display some feelings) | 2.93 | 1.13 | -0.14 | -0.72 | -0.04 | -0.02 | 0.85 |
| 11) | I “psyche” myself up so that I will genuinely feel any emotion that I am expected to feel (e.g. the other person is very worried so I try to work up concern too and reassure him/her) | 2.87 | 1.15 | -0.20 | -0.93 | 0.01 | -0.01 | 0.66 |
Note: SD=standard deviation; Skew=skewness; Kurt=kurtosis. The primary factor loading for each item is in bold
Based on Hoyle’s (41) recommendations and a multifaceted approach to the assessment of model fit (42, 86), we considered omnibus fit indices such as chi-square (χ2) and incremental fit indices such as the comparative fit index (CFI; values ≥0.90 indicate a good fit), the Tuker and Lewis Index (TLI; values ≥0.90 indicate a good fit), the standardized root mean square residual (SRMR; values ≤0.08 indicate a good fit), and the root mean square error of approximation (RMSEA; values ≤0.06 indicate a good fit) (9).
We evaluated the reliability of the ELN scale using Cronbach’s alpha to assess the internal consistency of each dimension and the overall scale. A coefficient greater than 0.70 was considered to indicate acceptable internal consistency, and coefficients greater than 0.80 were considered to indicate good internal consistency (70).
To establish the concurrent validity of the ELN scale, we examined its associations with scales measuring the same construct (70). This was evaluated using Pearson’s correlation with the three dimensions of burnout as well as with the EWRS. Correlation values from 0.10 to 0.29 were considered weak, those from 0.30 to 0.40 moderate and those greater than 0.50 strong (26).
Statistical analyses were performed using SPSS version 22.0 and Mplus7.1 (68).
Results
Sample characteristics
The study participants (N=409) were employed on a full-time or part-time basis as direct-care providers in all types of clinical settings and a variety of care units. Ages ranged from 22 to 63, with an average age of 37.3 (SD 9.4). The sample consisted mainly of women (n=303; 74%). A percentage of 44% (n=180) had a partner. A percentage of 51.8% (n=212) had achieved a degree in nursing. The average length of time participants had worked as nurses was 13.7 years (SD=9.76).
Construct validity: EFA
The 24 items tool has been administered to a sample of 205 nurses. In accordance with statistical analysis (explorative factor analysis, corrected item-total correlations, internal consistency following an item’s removal), 13 items were removed (see table S1). Items selection was based on results based both on stastistical analysis performed on a sample of 205 nurses and results from CVI.
The final ELN scale consists of 11 items. The S-CVI average of the 11-item scale was 0.80.
The Bartlett test of sphericity was significant (λ2=831.66; d.f.=55; P<0.01) and the Kaiser-Meyer-Olkin test result was 0.84, suitable results for the factorial analysis. EFA was performed using the maximum likelihood method with a promax rotation to examine the dimensionality of the scale.
The factorial analysis with 11 items pointed out a solution with three factors. After rotation, these factors explained 19.20% of the common variance for the first factor, 18.35% for the second factor and 16.48% for the third factor. The total variance explained in the EL scale was 54.04%. Factor loadings were all greater than 0.30 (table 1). These results suggested that we should proceed to cross validation with CFA.
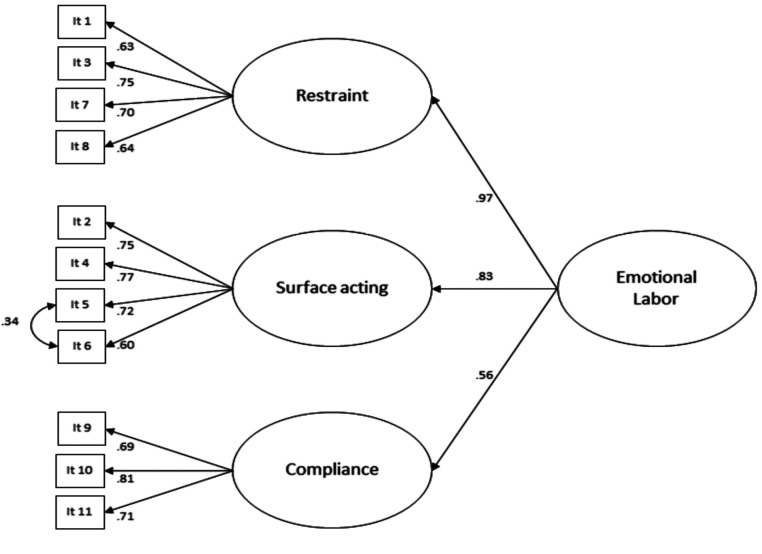
The construct validity: CFA
The results of EFA suggested that the three-dimensional model was the best model to be cross- validated with CFA. CFA (figure 1) was performed in the subgroup of 204 nurses, and the findings confirmed the three-dimensional model with a satisfactory fit of the data λ2 (40; N=204)=106.53; P<0.001; RMSEA=0.090 (90% I.C.=0.070-0.111); P(RMSEA<0.05)<0.01; CFI=0.922; TLI=0.893 and SRMR=0.061. All factor loadings were >0.60.
Figure 1.
ELN scale dimensions
The items that loaded into the first factor corresponded to intended hiding/suppressing/conveying emotions; thus, this dimension was named restraint (items 1, 3, 7 and 8). The items that loaded into the second factor corresponded to explicit acting or expressing an emotion not really felt, faking o struggling to fake, if required, the appropriate emotion; thus, this dimension was named surface acting (items 2, 4, 5 and 6). The items that loaded into the third factor corresponded struggling to feel and display the required emotion; thus, this dimension was named compliance (items 9, 10 and 11).
In addition, a second-order factor was specified to account for the overall EL dimensions, as the three dimensions were positively correlated with each other (table 2). We also specified a covariance among the residuals of items 5 and 6, as both referred to emotions that were intentionally conveyed or feelings that were not really felt; this covariance was significant at 0.34.
Table 2.
Correlations among EL, requirements and burnout (N=409)
| Variable | Mean | SD | α | Surface acting | Restraint | Compliance | Requirements pos | Requirements neg | Exaustion | Cynicism | Interpersonal strain |
| Surface acting | 2.06 | 0.81 | 0.82 | 1.00 | |||||||
| Restraint | 2.54 | 0.73 | 0.74 | 0.61** | 1.00 | ||||||
| Compliance | 2.82 | 0.89 | 0.70 | 0.39** | 0.49** | 1.00 | |||||
| Requirements pos | 3.79 | 0.82 | 0.86 | 0.07 | 0.14** | 0.26** | 1.00 | ||||
| Requirements neg | 3.20 | 1.01 | 0.86 | 0.21** | 0.30** | 0.27** | 0.62** | 1.00 | |||
| Exhaustion | 2.58 | 1.13 | 0.85 | 0.35** | 0.35** | 0.23** | -0.07 | 0.12* | 1.00 | ||
| Cynicism | 1.57 | 1.30 | 0.87 | 0.39** | 0.41** | 0.26** | -0.11* | 0.10* | 0.64** | 1.00 | |
| Interpersonal strain | 1.10 | 1.02 | 0.88 | 0.39** | 0.38** | 0.23** | -0.08 | 0.13* | 0.48** | 0.71** | 1.00 |
Note: α=Cronbach’s alpha; *<0.05; **<0.01; ***<0.001
Internal consistency was 0.85 (Cronbach α) for the overall scale: 0.82 for surface acting, 0.70 for restraint and 0.70 for compliance (table 3).
Table 3.
Correlations between ELNs dimensions (N=409)
| Mean | SD | Skewness | Kurtosis | Restraint | Surface | Compliance | |
| Restraint | 2.54 | 0.73 | 0.04 | -0.33 | (0.70) | ||
| Surface | 2.06 | 0.81 | 0.45 | -0.56 | 0.61** | (0.82) | |
| Compliance | 2.82 | 0.89 | -0.20 | -0.43 | 0.49** | 0.39** | (0.70) |
Note: The comparison between the means is significant with F=287.89 and P=<0.001
On the diagonal is the Cronbach alpha of each dimension
**=p<0.001
Scores and concurrent validity
Participants reported higher levels of compliance than of surface acting (p<0.01), resulting from repeated measures ANOVA.
The ELN scale was also tested for concurrent validity as a final estimation of construct validity. The construct validity, as the ability of the scale to grasp relations with items referring to a similar construct, has been tested by the Emotion Work Requirement Scale (EWRS).
Furthermore, table 2 shows correlations between EL, emotional work requirements and burnout. Compliance dimension (r=0.32) was positively correlated with positive emotional work requirements.
Negative work requirements were significantly correlated with all dimensions of the ELN scale. Positive work requirements were correlated only with the restraint and compliance dimensions. All burnout dimensions were positively correlated with EL dimensions.
We also computed statistical differences among different clinical settings. As can be seen in table 4, there were significant statistical differences between the means of the emotional labour scores among nurses in different clinical settings. The emotional labour average in surgical wards was statistically higher than the averages in other wards (Mean=2.72; SD=0.74).
Table 4.
Differences according clinical wards (N=409) (ANOVA)
| Clinical Area | N (%) | M (SD) Restraint | M (SD) Surface | M (SD) Compliance | M (SD) Emotional Labor |
| Medical Area | 123 (33.3) | 2.47a (0.72) | 1.99ab (0.82) | 2.74a (0.86) | 2.37a (0.65) |
| Surgical Area | 55 (14.9) | 2.77a (0.83) | 2.34b (0.94) | 3.16b (0.79) | 2.72b (0.74) |
| Emergency R./ICU | 110 (29.8) | 2.50a (0.71) | 1.99ab (0.78) | 2.77ab (0.92) | 2.39a (0.62) |
| O.R./D.H.-D.S. | 36 (9.8) | 2.44a (0.71) | 1.78a (0.72) | 2.59a (1.01) | 2.24a (0.64) |
| Oncological Area | 22 (6.0) | 2.74a (0.81) | 2.28ab (0.80) | 2.71ab (0.66) | 2.57ab (0.64) |
| Pediatric Area | 23 (6.2) | 2.47a (0.67) | 2.01ab (0.74) | 2.71ab (1.05) | 2.37ab (0.71) |
| F | 1.87 | 2.80 | 2.39 | 3.35 | |
| P value | 0.10 | <0.05 | <0.05 | <0.01 |
Note: means by column with different superscripts letter are significantly different from each other at pair comparisons with Tukey post hoc test; SD=standard deviation; O.R.=Operating Room; ICU=Intensive Care Unit;
D.H.=Day Hospital; D.S.=Day Surgery
Discussion
Validation of the ELN scale revealed three dimensions that capture emotional labor in nurses. We termed these dimensions surface acting, restraint and compliance. Examples of these dimensions are provided throughout the literature on EL.
Surface acting refers to the display of an emotion that is regarded as appropriate but not actually felt, for example in order “to pretend to have the emotions you need to display for the job” (23, 94). Individuals who engage in surface acting assume a mask and change their facial or bodily expression. This surface-level process was first conceptualized by Hochschild (40) and later supported by others (4, 22, 23, 36). Using the strategy of surface acting, employees can modify and control their emotional expression. For example, in order to meet their job and role requirements, nurses might enhance or fake a smile when in a bad mood or in the presence of a difficult patient. Eyers and Adams (31) provide an example of the complex interplay of emotions occurring in some settings. They reported how nurses working with elderly dementia patients may need to detach themselves from negative emotions, such as revulsion at unpleasant smells and body fluids, in order to resist to negative sensations (31). In another study, a nurse explained further, “Often we keep up the mask all day and then explode when we get home” (14, p. 91). In our sample, participants reported engaging less in surface acting than in restraint and compliance. This may be due to the nature of nursing, as the closeness of relationships between nurses and patients reinforces the need for nurses to provide patients with emotional nurturance and support. So, nurses’ interactions may be facilitated by the capacity to empathize with patients to create a climate of trust, confidence and interrelatedness (38). This is especially true in a profession such as nursing, where empathic concerns and emotional nurturance typify practitioners’ social image (38, 87).
Restraint refers to the suppression or inhibition of the authentic expression of emotions regarded as inappropriate in a specific context. According to literature, suppressing and hiding genuinely felt emotions may constitute EL. Nurses are aware that the emotional component of caring relationships can improve the quality of care. Nurses are also aware that it can be necessary to convey a negative or positive emotion, or to suppress or try to hide a negative or a positive feeling, depending on the situation. As Hochschild (40) has suggested, patients judge the quality of health services by the emotional style with which they are provided. Since nurses consider emotional aspects of care to be important (72, 75, 83), they engage in restraint. For example, a nurse described her feelings when handling a dead foetus after a delivery, in particular how she suppressed a sense of despair and managed to block the sensations deriving from the touch and smell of the dead foetus (15, p. 12).
Compliance refers to the process of controlling feelings to match the rules governing emotional displays in the workplace. It is a strategy that aims to produce required emotions: nurses feel that patients expect to behave and act in a specific way; nurses feel that there are social rules about how to behave in some situations and so struggle to feel the appropriate emotions or to behave in the expected way.
Other authors have suggested that workers feel the behavioral rules and thus sometimes invoke thoughts, images and memories to induce appropriate emotional responses (e.g. empathy or cheerfulness) (54). For example, a nurse described the process of communicating with parents about the death of their baby. She explained her emotional involvement: “When I’m preparing the baby for the parents I go through a grieving process every time” (13, p. 32).
In our sample, the mean of the compliance dimension was very high, supporting the idea that nurses in our sample were very sensitive to emotional work and patients’ requirements.
We also examined the associations between EL and burnout. Past research has investigated the relationships between emotional labour, well-being and burnout. Some studies have used quantitative review and meta-analysis to investigate and clarify these relationships (17, 33, 44, 50). In our sample, all EL dimensions showed a significant positive correlation with the three dimensions of burnout. This is in line with studies, supporting the hypothesis that high levels of EL can be deleterious for nurses by increasing their risk of burnout (30, 36, 44, 94). As expected, cynicism, which occurs when relationships with patients and colleagues become cold, distant and cynical, was significantly associated with all EL dimensions, in particular with restraint. This may be due to the fact that intentionally conveying a positive or negative emotion that is not really felt can introduce a feeling of falsehood within relationships. This increases one’s risk of becoming inauthentic and emotionally detached. Interpersonal strain was associated, as expected, with all dimensions of the ELN scale. In fact, along with feelings of inauthenticity, EL exerts its deleterious effects through emotional estrangement from oneself and from others (40). Faking emotions that are not really felt, along with suppressing and hiding felt emotions that would be inappropriate to display, if prolonged over time can lead to interpersonal strain, a particular aspect of disengagement found in work relationships. The more nurses reported EL, the more they were affected by emotional exhaustion, cynicism and interpersonal strain. Hochschild (40) argued that engaging in emotional labour over a long time may result in feeling detached, not only from one’s true feelings, but also from the feelings of other people, suggesting a relationship with burnout. According to Maslach (62), for health care professionals, the need to attend to and care for patients continuously creates an excessive emotional burden. The risk associated with fully and continuously meeting such emotional demands is that workers will soon become exhausted, which will then make them unable to conceal their true (and inappropriate) emotions.
Our respondents also completed the EWRS scale, which explored emotional working demands. As expected, the requirement to hide negative emotions and to show positive emotions was strongly associated with surface acting, restraint and compliance. The requirement to display positive emotions, as expected, was more strongly associated with compliance (r=0.26). No significant association was found between the requirement to display positive emotions and the dimension of surface acting
We also measured EL within different clinical settings. As expected, there were significant statistical differences in the emotional labour scores among nurses working in these different settings. In our sample, nurses in surgical wards experienced more EL than nurses working in other areas, such as in the emergency ward and the intensive care unit (ICU). In postoperative wards, patients need both highly technical and comforting care, and nursing work is intensive and multidimensional. Nurses working in surgical wards need to have excellent critical care skills and a high level of technical expertise to manage patients’ complex clinical conditions in the immediate postoperative period (56, 66). The caring process demands both technical and affective skills, which is stressful (90). Surgical nurses are faced with demanding situations in which they must provide compassionate care and engage in respectful interactions with patients, assume responsibility for pain assessment and pain management and at the same time provide a high level of technical competence (74). Moreover, work in surgical wards is high-pressure because it involves multitasking competence and interdisciplinary collaboration (91, 76).
The feeling of pressure among nurses in surgical wards may be due to several other factors. Some researchers have identified barriers that concern the organizational aspects of surgical wards, such as workload, lack of staff and lack of inter-professional collaboration, especially with medical staff (5, 67). Others have identified legal or institutional constraints, because caring relationships in surgical wards are necessarily limited by time and together highly specialized. Overall, these organizational constraints reinforce emotional distress and decrease investment in relationships (7, 58). Based on our analysis, we believe that the lower levels of EL found in the ICU and the emergency ward were likely due to the relatively simpler demands placed on nurses in these wards. In wards with less complex demands, higher level technical skills are prioritized over deeper and ongoing interactions with patients.
Limitations
This study had several important limitations. First, the sample size was small, and the data were collected only from two institutions using convenience sampling. We included different clinical practice environments. However, the clinical wards are important co-factors and an a posteriori analysis should be made to verify the estimate, first increasing the sample size.
Second, the ELN scale was tested only in Italian health care settings. Further testing in different cultural settings would enhance our findings. Furthermore, future studies should investigate the relation between emotional requirements and display rules as antecedents of EL behavioral strategies.
Third, since the tool investigates issues related to job experience, participants could have been influenced by social desirability and the difficulty in admitting to the existence of negative emotions. Finally, the complexity and variety of the EL experience could have limited the scale’s development process.
Conclusion
Emotional burden may be a specific and significant stress factor together with common psychosocial and personal psychological risk factors in health care organizations. Emotional labour is a central aspect of nursing, but it is still considered an underestimated facet of care work (39, 84). The advancements of EL research need to recognize the complexity of the EL construct, and researchers need a specific tool to explore EL experiences more widely and to measure EL among nurses. This pilot study aimed to develop and validate an 11-item tool to measure EL among nurses. Our results showed evidence of internal consistency, content validity and construct validity. In agreement with international literature, positive associations with burnout dimensions were found.
We considered a multifaced approach to the emotional labour construct. First, our operationalization focuses on behavioural emotional strategies in accordance with display rules to which nurses may sometimes conform (4). Second, our conceptualization recognizes the roles of both positive and negative emotions, as EL may involve both the expression of positive emotions and the suppression of negative emotions. Third, with our delineation of three dimensions, our conceptualization distinguishes among faked, suppressed and compliant emotions.
This pilot study provides stakeholders and researchers with a practical tool to assess EL among nurses. For researchers, the ELN scale can be a fruitful tool that facilitates the application of some theories (i.e. the stressor-emotion model, JDC model). For stakeholders, a valid ELN tool could be useful to predict clinical performance, quality of care and patient satisfaction. In addition, it could be used to prevent the occurrence of EL by leading to the implementation of strategies and the development of interventions to eliminate unnecessary suffering and negative consequences for nurses and health care facilities. For practitioners, the data provide some evidence to support intervention within clinical settings to prevent work-related stress disorders.
Many scientific studies have shown that in situations of high emotional burden, when nurses are repeatedly stressed by prolonged, emotionally awkward situations, there may be negative effects on the quality of care provided as well as on nurses’ performance, work satisfaction, and physical and psychological health and well-being (2, 3, 10, 73, 80, 81, 96). This study shows that EL is a prominent feature of health care facilities, which underscores the need for a greater investment by researchers and organizational practitioners in this area. Future studies should compare these data with those from other health care facilities. In particular, there is a need to investigate relationships between EL and stress, especially in some high-stress clinical contexts, and to design interventions that consider contextual, organizational and individual factors in the diffusion of EL.
No potential conflict of interest relevant to this article was reported by the authors
References
- 1.Abraham R. The Impact of Emotional Dissonance on Organizational Commitment and Intention to Turnover. J Psycol Interdiscipl Apppl. 1999;133:441–455. doi: 10.1080/00223989909599754. [DOI] [PubMed] [Google Scholar]
- 2.Aiken LH, Clarke SP, Sloane D, et al. Hospital nurse staffing and patient mortality, nurse burnout and job dissatisfaction. J Am Med Assoc. 2002;288:1987–1993. doi: 10.1001/jama.288.16.1987. [DOI] [PubMed] [Google Scholar]
- 3.Aiken LH, Sloane DM, Bruyneel L, et al. Nurses’ reports of working conditions and hospital quality of care in 12 countries in Europe. Int J Nurs Stud. 2013;50:143–153. doi: 10.1016/j.ijnurstu.2012.11.009. [DOI] [PubMed] [Google Scholar]
- 4.Ashforth B, Humphrey RH. Emotional labor in Service Roles-The influence of Identity. Acad Manage Rev. 1993;18:88–115. [Google Scholar]
- 5.Atwal A, Caldwell K. Nurses’ perceptions of multidisciplinary team work in acute health-care. Int J Nurs Pract. 2006;33:359–365. doi: 10.1111/j.1440-172X.2006.00595.x. [DOI] [PubMed] [Google Scholar]
- 6.Badolamenti S, Sili A, Caruso R, Fida R. What do we know about emotional labour in the nursing profession? A literature narrative review. British J Nurs. 2016 doi: 10.12968/bjon.2017.26.1.48. Doi: http://dx.doi.org/10.12968/bjon.2017.26.1.48. [DOI] [PubMed] [Google Scholar]
- 7.Bakker AB, Killmer CH, Siegrist J, et al. Effort-reward imbalance and burnout among nurses. J Adv Nurs. 2000;31:884–891. doi: 10.1046/j.1365-2648.2000.01361.x. [DOI] [PubMed] [Google Scholar]
- 8.Balducci C, Avanzi L, Fraccaroli F. Emotional demands as a risk factor for mental distress among nurses. Med Lav. 2014;105:100–108. [PubMed] [Google Scholar]
- 9.Barbaranelli C, Lee CS, Vellone E, et al. The problem with Cronbach’s Alpha: comment on Sijtsma and van der Ark. Nurs Res. 2015;64:140–145. doi: 10.1097/NNR.0000000000000079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bartram T, Casimir G, Djurkovic N, Stanton P. Do perceived high performance work systems influence the relationship between emotional labour, burnout and intention to leave? A study of Australian nurses. J Adv Nurs. 2012;68:1567–1578. doi: 10.1111/j.1365-2648.2012.05968.x. [DOI] [PubMed] [Google Scholar]
- 11.Beck CT, Gable RK. Ensuring content validity: an illustration of the process. J Nurs Meas. 2001;9:201–215. [PubMed] [Google Scholar]
- 12.Best RG, Downey RG, Jones RG. Incumbent perceptions of emotional work requirements. Paper presented at the12th annual conference of the Society for Industrial and Organizational Psychology. St. Louis, April 1997 [Google Scholar]
- 13.Bolton SC. Who cares? Offering emotion as a “gift” in the nursing labour process. J Adv Nurs. 2000;32:580–586. doi: 10.1046/j.1365-2648.2000.01516.x. [DOI] [PubMed] [Google Scholar]
- 14.Bolton SC. Changing faces: nurses as emotional jugglers. Soc Health Illness. 2001;23:85–100. [Google Scholar]
- 15.Bolton SC. Women’s work, dirty work: the gynaecology nurse as “other”. Gend Work Organ. 2005;12:169–186. [Google Scholar]
- 16.Bone D. Dilemmas of emotion work in nursing under market driven health care. Int J Public Sect Manage. 2014;15:140–150. [Google Scholar]
- 17.Bono EV, Vey MA. Toward understanding emotional management at work: A quantitative review of emotional labor research. Emotions in Organizational Behavior. In: Hartel EJ, Zerbe WJ, Ashkanasy NM, editors. Mahwah (NJ): Lawrence Erlbaum Associates; 2005. pp. 213–233. [Google Scholar]
- 18.Borgogni L, Galati D, Petitta L, Schweitzer CF. Manuale dell’adattamento italiano. Firenze: O.S. Organizzazioni Speciali; 2005. Il questionario Check up organizzativo. [Google Scholar]
- 19.Borgogni L, Armandi F, Amaducci M, Consiglio C. Integrazione alla misura del job burnout: la scala di sovraccarico relazionale. Giornale italiano di psicologia. 2007;34:699–714. [Google Scholar]
- 20.Borgogni L, Consiglio C, Alessandri G, Schaufeli WB. Don’t throw the baby out with the bathwater! Interpersonal strain at work and burnout. Eur J Work Org Psychol. 2012;21:875–898. [Google Scholar]
- 21.Briët M, Näring G, Brouwers A, van Droffelaar A. Emotional labor: Ontwikkelong en validering van de duth questionnaire on emotional labor (d-qel) [The development and validation of the duth questionnaire on emotional labor (d-qel)] Tijdschrift voorr Psychologie en Gezondheid. 2005;33:318–330. [Google Scholar]
- 22.Brotheridge CM, Lee RT. Development and validation of the emotional Labour Scale. J Occup Org Psychol. 2003;76:365–379. [Google Scholar]
- 23.Brotheridge CM, Grandey AA. Emotional labor and burnout: Comparing two perspectives of “people work”. J Voc Behav. 2002;60:17–39. [Google Scholar]
- 24.Chu KH, Murmann SK. Development and validation of the hospitality emotional labor scale. Tourism Manage. 2006;27:1181–1191. [Google Scholar]
- 25.Cigantesco A, Picardi A, Chiaia E, et al. Breif report: job satisfaction among mental health professionals in Rome, Italy. Commun Ment Health J. 2003;39:349–355. doi: 10.1023/a:1024076209376. [DOI] [PubMed] [Google Scholar]
- 26.Cohen J. 2nd ed. Hillsdale (NJ): Lawrence Earlbaum Associates; 1988. Statistical power analysis for the behavioral sciences. [Google Scholar]
- 27.Comrey AL, Lee HB. Broadway (NJ): Lawrence Erlbaum associates Inc; 1992. A first course in Factor Analysis. [Google Scholar]
- 28.Consiglio C. Interpersonal strain at work: a new burnout facet relevant for the health of hospital staff. Burnout Res. 2014;1:69–75. [Google Scholar]
- 29.Cox T, Griffiths A, Rial-Gonzáles E. Research on work related stress. European Agency for Safety and Health at Work. Bilbao. 2002 [Google Scholar]
- 30.Diefendorff JM, Croyle MH, Grosserand RH. The dimensionality and antecedents of emotional labor strategies. J Voc Behav. 2005;66:339–357. [Google Scholar]
- 31.Eyers I, Adams T. Emotional Labour in Dementia Care. The experience of dementia care nurses. In: Adams T, editor. Basingstoke: Palgrave Macmillan; 2008. [Google Scholar]
- 32.Gaan N. Development of Emotional Labour Scale in Indian context. Vision. 2011;15:41–48. [Google Scholar]
- 33.Garrosa E, Moreno-Jimenez B, Liang Y. The relationship between socio-demographic variables, job stressors, burnout, and hardy personality in nurses: an exploratory study. Int J Nurs Stud. 2008;45:418–427. doi: 10.1016/j.ijnurstu.2006.09.003. [DOI] [PubMed] [Google Scholar]
- 34.Gelderen B, Heuven E, Veldhoven M, et al. Psychological strain and emotional labor among police-officers: a diary study. J Voc Behav. 2007;71:446–459. [Google Scholar]
- 35.Glomb TM, Tews MJ. Emotional labor: A conceptualization and scale development. J Voc Behav. 2004;54:1–23. [Google Scholar]
- 36.Grandey AA. When “the show must go on”: surface acting and deep acting as determinants of emotional exhaustion and peer-related service delivery. Acad Manage J. 2003;46:86–96. [Google Scholar]
- 37.Grandey AA, Diefendorff JM, Rupp DE. Diverse perspective on Emotion Regulation at Work. NY: Routledge; 2013. Emotional labor in the 21st century. [Google Scholar]
- 38.Gray B. The emotional labour of nursing-defining and managing emotions in nursing work. Nurs Educ Today. 2009;29:168–175. doi: 10.1016/j.nedt.2008.08.003. [DOI] [PubMed] [Google Scholar]
- 39.Henderson A. Emotional labor and nursing: an under-appreciated aspect of caring work. Nurs Inq. 2001;8:130–138. doi: 10.1046/j.1440-1800.2001.00097.x. [DOI] [PubMed] [Google Scholar]
- 40.Hochshild A. London: University of California Press Ltd, 2003; 1983. The Managed Heart. Commercialization of Human Feeling with a new afterword. [Google Scholar]
- 41.Hoyle RH. Newbury Park (CA): Sage Publications; 1995. Structural Equation Modeling: Concepts, Issues, and Applications. [Google Scholar]
- 42.Hu L, Bentler PM. Fit indices in covariance structure modeling: Sensitivity to underparameterized model misspecification. Psychol Methods. 1998;3:424–453. [Google Scholar]
- 43.Hülsheger R, Schewe AF. On the costs and benefits of emotional labor: A meta-analysis of three decades of research. J Occup Health Psychol. 2011;16:361–389. doi: 10.1037/a0022876. [DOI] [PubMed] [Google Scholar]
- 44.Hülsheger UR, Lang JWB, Maier GW. Emotional labor, strain and performance: Testing reciprocal relationship in a longitudinal panel study. J Occup Health Psychol. 2010;15:505–521. doi: 10.1037/a0021003. [DOI] [PubMed] [Google Scholar]
- 45.Indregard AMR, Ulleberg P, Knardahl S, Nielsen MB. Emotional Dissonance and Sickness Absence Among Employees Working With Customers and Clients: A Moderated Mediation Model via Exhaustion and Human Resource Primacy. Frontiers in Psychology. 2018 doi: 10.3389/fpsyg.2018.00436. https://doi.org/10.3389/fpsyg.2018.00436 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Isfahani SS, Hosseini MA, Khoshknab MF, et al. Nurses’ creativity: Advantage or disadvantage. Iran Red Crescent Med J. 17(2):e20895. doi: 10.5812/ircmj.20895. DOI: 10.5812/ircmj.20895 Published online 2015 February 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.ISPSEL (Istituto Superiore per la Prevenzione e la Sicurezza sul Lavoro). La valutazione e gestione dello stress lavoro–correlato. Approccio integrato secondo il modello Management Standards HSE contestualizzato alla luce del D.Lgs 81/2008. ISPSEL, 2010 [Google Scholar]
- 48.Johnson HA, Spector PE. Service with a smile: Do emotional intelligence, gender, and autonomy moderate the emotional labour process. J Occup Health Psychol. :319–333. doi: 10.1037/1076-8998.12.4.319. [DOI] [PubMed] [Google Scholar]
- 49.Judge TA, Woolf EF, Hurst C. Is emotional labor more difficult for some than for others? A multilevel, experience-sampling study. Personnel Psychol. 2009;62:57–88. [Google Scholar]
- 50.Kammeyer-Mueller JD, Rubenstein AL, Long DM, et al. A meta-analytic structural model of dispositional affectivity and emotional labor. Personnel Psychol. 2013;66:47–90. [Google Scholar]
- 51.Karatepe OM, Aleshinloye KD. Emotional dissonance and emotional exhaustion among hotel employees in Nigeria. Int J Hosp Manag. 2009;28:349–358. [Google Scholar]
- 52.Karim J. Emotional labor and psychological distress: testing the mediatory role of work family conflict. Eur J Soc Sci. 2009;11:584–598. [Google Scholar]
- 53.Katayama Y, Ogasawara C, Tsuji C, et al. Development of Emotional Labor Inventory for Nurses. Jpn J Nurs Sci. 2005;25:20–27. [Google Scholar]
- 54.Kruml SM, Geddes D. Exploring the dimensions of Emotional Labor. The hearth of Hochschild’s work. Manage Commun Quarterly. 2000;14:8–49. [Google Scholar]
- 55.Lin SP. A study of the development of emotional labor loading scale. Sun Yat-Sen Manage Rev. 2000;8:427–447. [Google Scholar]
- 56.Lindsay M. Is the postanesthesia care unit becoming an intensive care unit. Perianesth Nurs. 1999;11:248–258. doi: 10.1016/s1089-9472(99)80020-3. [DOI] [PubMed] [Google Scholar]
- 57.Lynn MR. Determination and quantification of content validity. Nurs Res. 1986;35:382–385. [PubMed] [Google Scholar]
- 58.Mackintosh C. Protecting the self: a descriptive qualitative exploration of how registered nurses cope with working in surgical areas. Int J Nurs Stud. 2007;44:982–990. doi: 10.1016/j.ijnurstu.2006.04.009. [DOI] [PubMed] [Google Scholar]
- 59.Mann S. Achieving frontline communication excellence: the potential cost to health. IEEE Trans Prof Commun. 1998;41:1–12. [Google Scholar]
- 60.Mann S. London: Shaftesbury Element; 1999. Hiding what we feel, faking what we don’t. Understanding the role of your emotions at work. [Google Scholar]
- 61.Mann S. Emotions at work: to what extent are we expressing, suppressing or faking it. Europ J Work Organ Psychol. 2002;8:347–369. [Google Scholar]
- 62.Mann S. A health-care model of emotional labour. J Health Organ Manage. 2005;19:304–317. doi: 10.1108/14777260510615369. [DOI] [PubMed] [Google Scholar]
- 63.Mann S, Cowburn J. Emotional labour and stress within mental health nursing. J Psychiatr Ment Health Nurs. 2005;12:154–162. doi: 10.1111/j.1365-2850.2004.00807.x. [DOI] [PubMed] [Google Scholar]
- 64.Maslach C. Englewood Cliffs (NJ): Prentice Hall; 1982. Burnout: the cost of caring. [Google Scholar]
- 65.Maslach C, Jackson SE, Leiter MP. 3rd ed. Palo Alto (CA): Consulting Psychologists; 1996. The Maslach Burnout Inventory. [Google Scholar]
- 66.McGarvey H, Chambers M, Boore J. Development and definition of the role of the operating department nurse: a review. J Adv Nurs. 2000;32:1092–1100. doi: 10.1046/j.1365-2648.2000.01578.x. [DOI] [PubMed] [Google Scholar]
- 67.Miller KL, Reeves S, Zwarenstein M, et al. Nursing emotion work and inter-professional collaboration in general internal medicine wards: a qualitative study. J Adv Nurs. 2008;64:332–343. doi: 10.1111/j.1365-2648.2008.04768.x. [DOI] [PubMed] [Google Scholar]
- 68.Muthén LK, Muthén BO. 6th ed. Los Angeles (CA): Muthén & Muthén; 2012. Mplus User’s Guide. [Google Scholar]
- 69.Näring G, Briët M, Brouwers A. Validation of the Dutch questionnaire on Emotional Labor (D-QEL) in nurses and teachers. In Richter P, Peiro JM, Schaufeli WB (eds): Psychosocial resources in human services work. München: Hampp Publishers. 2007:135–145. [Google Scholar]
- 70.Nunnally JC, Bernstein IH. 3rd ed. New York (NJ): McGraw-Hill; 1994. Psychometric Theory. [Google Scholar]
- 71.Polit DF, Beck CT. The content validity index: Are you sure you know what’s being reported? Critique and recommendations. Res Nurs Health. 2006;29:489–497. doi: 10.1002/nur.20147. [DOI] [PubMed] [Google Scholar]
- 72.Pugh SD, Groth M, Hennig-Thurau T. Willing and able to fake emotions: A closer examination of the link between emotional dissonance and employee well-being. J Appl PsychoL. 2011;96:377–390. doi: 10.1037/a0021395. [DOI] [PubMed] [Google Scholar]
- 73.Pugliesi K. The consequences of emotional labor: effects on work stress, job satisfaction and well-being. Motivation Emotion. 1999;23:125–154. [Google Scholar]
- 74.Quiñones-García C, Rodríguez-Carvajal R, Clarke N, Moreno-Jiménez B. Development and cross-national validation of the Emotional Effort Scale (EEF) Psycothema. 2013;25:363–369. doi: 10.7334/psicothema2012.289. [DOI] [PubMed] [Google Scholar]
- 75.Rafaeli A, Sutton R. Expression of emotion as part of the work role. Acad Manage Rev. 1987;12:23–37. [Google Scholar]
- 76.Schafheutle EI, Cantrill JA, Noyce APR. Why is pain management suboptimal on surgical wards. J Adv Nurs. 2001;33:728–737. doi: 10.1046/j.1365-2648.2001.01714.x. [DOI] [PubMed] [Google Scholar]
- 77.Schaubroeck J, Jones JR. Antecedents of workplace emotional labor dimensions and moderators of their effects on physical symptoms. J Organ Behav. 2000;21:163–183. [Google Scholar]
- 78.Schaufeli WB, Leiter MP, Maslach C, Jackson SS. Maslach burnout inventory-general survey. Maslach Burnout Inventory manual. In: Maslach C, Jackson SE, Leiter MP, editors. Palo Alto (CA): Consulting Psychologists Press; 1996. [Google Scholar]
- 79.Schaufeli WB. The balance of give and take. Toward a social exchange model of burnout. Int Rev Soc Psychol. 2006;19:87–131. [Google Scholar]
- 80.Schmidt K, Diestel S. Are emotional labor strategies by nurses associated with psychological costs? A cross-sectional survey. Int J Nurs Stud. 2014;51:1450–1461. doi: 10.1016/j.ijnurstu.2014.03.003. [DOI] [PubMed] [Google Scholar]
- 81.Scott BA, Barnes CM. A multi-level field investigation of emotional labor, affect, work withdrawal and gender. Acad Manage J. 2011;54:116–136. [Google Scholar]
- 82.Shigemoto T, Okura M, Abe Y. Factor structure of emotional labor and its correlates in Japanese nurses. Bull Tokushima Bunri University. 2005;82:101–104. [Google Scholar]
- 83.Smith P. The nursing process: raising the profile of emotional care in nurse training. J Adv Nurs. 1991;16:74–81. doi: 10.1111/j.1365-2648.1991.tb01500.x. [DOI] [PubMed] [Google Scholar]
- 84.Smith P, Cowie H. Perspectives on emotional labour and bullying: reviewing the role of emotions in nursing and healthcare. Int J Work Organ Emotions. 2010;3:227–236. [Google Scholar]
- 85.Strazdins LM. Integrating emotions: Multiple role measurement of emotional work. Aust J Psychol. 2000;52:41–50. [Google Scholar]
- 86.Tanaka JS. Multifaceted conceptions of fit in structural equation models. Testing structural equation models. In: Bollen KA, Long JS, editors. Newbury Park (CA): Sage; 1993. [Google Scholar]
- 87.Theodosius C. London (UK): Routledge; 2008. Emotional Labour in Health Care: The Unmanaged Heart of Nursing. [Google Scholar]
- 88.Thurstone LL. Chicago (IL): University of Chicago Press; 1947. Multiple Factor Analysis. [Google Scholar]
- 89.Waltz CF, Bausell RB. Philadelphia: F. A. Davis Co; 1981. Nursing research: Design, statistics, and computer analysis. [Google Scholar]
- 90.Wilkin K, Slevin E. The meaning of caring to nurses: an investigation into the nature of caring work in an intensive care unit. J Clin Nurs. 2004;13:50–59. doi: 10.1111/j.1365-2702.2004.00814.x. [DOI] [PubMed] [Google Scholar]
- 91.Willis K, Brown C, Sahling I, et al. Working under pressure: a pilot study of nurse work in a postoperative setting. Clin Nurse Spec. 2005;19:87–91. doi: 10.1097/00002800-200503000-00068. [DOI] [PubMed] [Google Scholar]
- 92.World Health Organization: World Health Statistics. Geneva (Switzerland): WHO Press; 2010. [Google Scholar]
- 93.Ybema J, Smulders P. Emotional demands and the need to hide emotions at work. Gedrag en Organisatie. 2002;15:129–146. [Google Scholar]
- 94.Zamanzadeh V, Rassouli M, Ghahramanian A. Factors influencing communication between the patients with cancer and their nurses in oncology wards. Indian J Palliat Care. 2014;20:12–20. doi: 10.4103/0973-1075.125549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Zammuner VL, Galli C. The relationship with patients: emotional labor and its correlates in hospital employee. Emotions in Organizational Behavior. In: Hartel CEJ, Zerbe WJ, Ashkanasy NM, editors. Mawah (NJ): Routledge; 2005. pp. 251–285. [Google Scholar]
- 96.Zapf D, Vogt C, Seifert C, et al. Emotion work as a source of stress: The concept and development of an instrument. Europ J Work Org Psychol. 1999;8:371–400. [Google Scholar]
- 97.Zapf D. Wellbeing: causes and consequences of emotion regulation in work settings. Int Rev Psychiatry. 2005;17:355–364. doi: 10.1080/09540260500238348. [DOI] [PubMed] [Google Scholar]