Abstract
Background:
Sick building syndrome (SBS) is defined as a condition occurring in those who live or work in a modern building and who suffer from symptoms such as headache, fatigue, lack of concentration and irritation of the skin and mucous membranes.
Objectives:
The aim of this study was to evaluate the relationship between personal characteristics, environmental factors and the prevalence of SBS among the secretaries working in a hospital.
Method:
In this cross-sectional study, questionnaires were administered to all secretaries who were working in Kütahya hospital in January and March 2018. The questionnaire used in the study included the sociodemographic characteristics of the participants and the question form “MM 040 NA Hospital” to evaluate SBS symptoms. These symptoms were the clinical symptoms reported by the secretaries as a result of exposure to factors within the hospital. Temperature, humidity, carbon dioxide concentration, light intensity and noise level were measured in the indoor environment of the hospital. Chi square test, Spearman’s correlation coefficient and logistic regression models were used in the analysis of data.
Results:
The study was completed with 177 people, 61.6% women, and the mean age was 30.14±5.7. The prevalence of SBS was found to be 20.9%. The risk of SBS was found to be 2.9 times higher for females, 2.8 times higher for individuals who described the working environment as dusty, 2.6 times higher for subjects complaining of stuffy “bad” air, dry air and an unpleasant odour. All measurements were found to be within acceptable limits. The risk of SBS was found to be 1.2 times higher with increases in the measured noise level, and 2.1 times higher with increased carbon dioxide (CO2) concentrations.
Conclusion:
The factors impacting the risk of experiencing SBS were determined. Bearing these factors in mind, we think that hospital administrations should be informed about arrangements and measures that will improve the quality of the internal environment of the hospital.
Key words: Sick building syndrome, hospital, indoor air quality
Abstract
«Relazione tra la sindrome da edificio malato e la qualità dell’aria indoor nel personale ospedaliero».
Introduzione:
La sindrome da edificio malato o Sick building syndrome (SBS) è descritta come una condizione che si manifesta in coloro che vivono o lavorano in un edificio moderno e che soffrono di sintomi quali mal di testa, stanchezza, difficoltà di concentrazione e irritazione della pelle e delle mucose.
Obiettivi:
Valutare la relazione tra caratteristiche personali, fattori ambientali e prevalenza della SBS tra il personale di segreteria di un ospedale.
Metodi:
In questo studio trasversale sono stati somministrati questionari al personale di segreteria dell’ospedale Kütahya (Turchia) tra gennaio e marzo 2018. Il questionario usato nello studio comprendeva le caratteristiche sociodemografiche dei partecipanti e il modulo MM 040 NA Hospital. Questo modulo ha consentito di raccogliere i sintomi clinici associati alla SBS come risultato di esposizione a fattori ambientali. Temperatura, umidità, concentrazione di diossido di carbonio, intensità della luce e livello del rumore sono stati misurati negli ambienti di lavoro. Per la valutazione dei dati sono stati utilizzati il test del chi quadrato, il coefficiente di correlazione di Spearman e i modelli di regressione logistica.
Risultati:
Lo studio ha coinvolto 177 lavoratori, 61.6% donne, età media 30.14±5.7. La prevalenza di SBS è risultata del 20.9%. Il rischio di SBS è risultato essere 2.9 volte più alto nelle donne, 2.8 volte maggiore negli individui che hanno descritto l’ambiente di lavoro come polveroso, 2.6 volte maggiore nei soggetti che lamentavano aria viziata, aria secca e odori spiacevoli. Le misurazioni dei fattori ambientali hanno mostrato valori nella norma. Il rischio di SBS è risultato essere 1.2 volte maggiore in corrispondenza con l’aumento dei livelli di rumore misurati e 2.1 volte maggiore con livelli più alti della concentrazione di diossido di carbonio (CO2).
Conclusioni:
In questo studio sono stati determinati i fattori di rischio personali e ambientali per la SBS. Alla luce di questi risultati, riteniamo che gli amministratori degli ospedali dovrebbero essere informati circa accertamenti e misure in grado di migliorare la qualità dell’ambiente interno degli ospedali.
Background
“Sick building syndrome” (SBS) is used to describe situations in which building occupants experience negative effects on their health and comfort, which appear to be linked to time spent in a building, although no specific illness or cause can be identified. The complaints may be localized to a particular room or zone, or may be widespread throughout the building (26). Furthermore, most of the complainants report relief soon after leaving the building (26, 28). SBS is defined by the World Health Organization as a condition occurring in those who live or work in a modern building and who suffer from symptoms such as headache, fatigue, lack of concentration and irritation of the skin and mucous membranes (13, 28). Personal factors, such as work-related stress, psychosocial factors and allergic conditions, can contribute to SBS, but building-related factors such as inadequate heating, ventilation and air conditioning systems, noise, poor indoor air quality, air pollutants (nitrogen dioxide, sulfur dioxide, ozone, particulate matter, volatile organic compounds, carbon dioxide) mould and humidity are all possible determinants for the onset of SBS (4, 11, 14, 22, 27). SBS can result from exposure to these factors, and symptoms of SBS may be observed in employees’ low levels of productivity and high absenteeism, while institutional functioning can also be adversely affected (27). Criteria such as good indoor air quality, positive environmental and ergonomic characteristics and the thermal comfort of the building all contribute to the satisfaction and comfort of the employees (3, 11, 22, 27). Determinants for the onset of SBS are likely to exist where people spend long periods in indoor environments, such as office buildings, university buildings, schools and hospitals. In relation to the hospital environment, these positive environmental qualities should be provided for both the patients and the health care workers.
The objective of the study was to evaluate the relationship between personal characteristics, environmental factors and the prevalence of SBS. Hospital staffs belong to heterogeneous group since the working hours and working conditions of staff members will differ greatly, they are affected differently by building-related factors. For this reason, it is important that a study of SBS in a hospital is conducted with a homogeneous group. Thus we have preferred to work with the secretaries. As a group, hospital secretaries have similar experiences in terms of their ergonomic conditions, working hours and task descriptions as listed; 1) to provide a professional, 2) effective medical secretarial and 3) administrative service to the doctors and the technical team within the department, 4) to act as the frontline between clinicians, doctors, patients to work collaboratively to ensure the smooth running of the multi-disciplinary team, 5) to assist in the organisation of the consultants workload, 6) to respond effectively and appropriately to telephone, 7) to accurately and appropriately maintain manual and computerised records. For this reason, the hospital secretaries were selected as the study population and measurements were taken from the area where each secretary was located.
The Kütahya Evliya Çelebi Training and Research Hospital (ECTRH) was constructed in 1954 and 2008 and consists of two separate buildings, of eight and four floors, with closed areas of 19 917 m2 and 33 000 m2, respectively. The hospital has a total of 727 beds and 155 polyclinic rooms. Ventilation for the hospital is provided by a general hygienic air handling unit. This unit consist of 10 sections (three hygienic-hepa filter units and seven general air conditioning units). The intensive care unit is ventilated by the three hygienic-hepa units, and the remaining areas are ventilated by the general air conditioning units. All the locations chosen for the study were polyclinic rooms with common facilities provided by the centralised air conditioning system. All hospitals prohibit smoking inside the premises.
Objectives
The objective of the study was to evaluate the relationship between personal characteristics (gender, age, clinical symptoms, perceived work quality), environmental factors (temperature, humidity, carbon dioxide concentration, light intensity and noise level) and the prevalence of SBS among the secretaries working in Kütahya ECTRH.
Methods
In this cross-sectional study, questionnaires were administered to all secretaries who were working in Kütahya ECTRH in January and March 2018. Approval from the local ethics committee and administrative permits were obtained. Since the target population for the study was all the medical secretaries working in the hospital, there was no sample size calculation. Participation in the study was on a voluntary basis and those who had worked for a period shorter than three months and those with diagnosed COPD, asthma and allergic symptoms were excluded from the study. The study was completed with 177 secretaries from a total number of 200 (participation 89%).
The questionnaire used in the study included the sociodemographic characteristics of the participants and the question form “MM 040 NA Hospital”.
MM 040 NA Hospital form
This form was developed by Andersson et al. in 1985 to assess indoor air quality and its effects on people living in these environments (2). In other words, it is a form that includes questions that investigate the presence of SBS in closed environments. Over the years, different versions of this questionnaire have been used in offices, schools and hospitals, each under a different name. The version used in our study was the “MM 040 NA Hospital” (3). This form was translated from English into Turkish and back from Turkish to English by two experts. The intelligibility, validity and reliability of the questionnaire were tested with a group of 10 participants (Cronbach’s α: 0.938).
The form contains a section on sociodemographic information and a work section, in which the physical conditions of the working environment are questioned (air flow, odour, temperature, noise etc.). In addition, business conditions, sickness background, current symptoms and the overall quality of the indoor environment are questioned. Each section is evaluated separately. Hospital indoor quality (general impression, colour scheme, common areas, connection with the outside etc.) and perceived quality of work (adequacy of working conditions, difficulty of work, job satisfaction and business performance) were both evaluated on a five point Likert-type scale. The total score that could be derived from the responses was between four and 20. The average score for hospital indoor quality was 11.72 and the average score for perceived quality of work was 13.85. Areas that fell below these average scores in the evaluations of hospital indoor quality and perceived quality of work were considered inadequate.
Definition of SBS
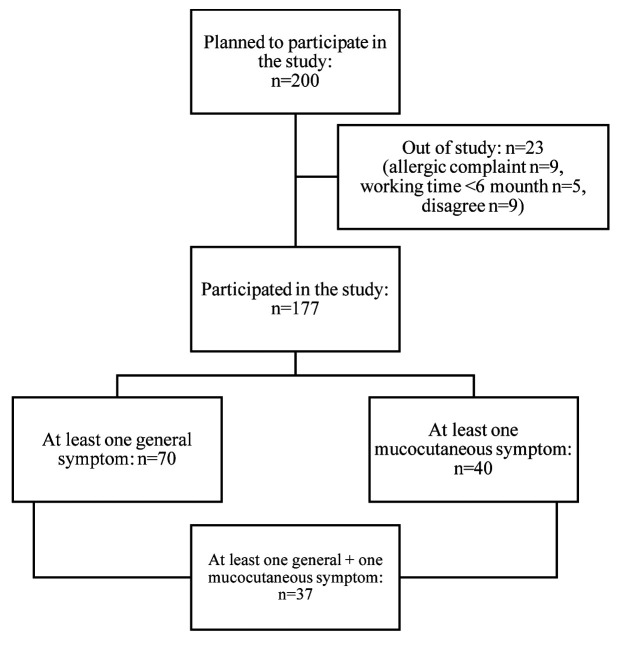
The incidence of general symptoms (fatigue, headache, nausea/dizziness, feeling heavy-headed, difficulties in concentration) and mucocutaneous symptoms (itching/burning/irritation of the eyes, irritated/stuffy/runny nose, hoarse/dry throat, cough, dry/flushed facial skin, scaling/itching scalp or ears, hands dry/itching/red skin) as occurring in the last three months were questioned. Participants were asked whether the symptoms occurred “every week”, “sometimes” or “never”. Those who answered “every week”, were then asked to answer “yes”, “no” or “do not know” to the following question: “Do you think the symptoms are caused by your work environment?” Among those who answered “yes” to this question, SBS was considered positive if there was at least one symptom from the general symptoms group and at least one symptom from the mucocutaneous symptoms group (5, 27) (figure 1).
Figure 1.
Flow diagram of participants showing symptoms of SBS
Measurements
Simultaneously with the questionnaire being answered, temperature, humidity, CO2 concentration, light intensity and noise level were measured in the indoor environment of the hospital. The measurements were made on each floor of the hospital, at two points in the corridors and in all polyclinic rooms. (Measurements were taken in every region where the secretaries work) These measurements were taken in places away from the air conditioning outlets, open doors and windows between 10:00 and12:00 in the morning, and again at the same place between 14:00 and16:00 in the afternoon.
A mobile, manual, sensor-based, “Testo 480 - multifunction measuring instrument” and a “Testo 816 - sound level meter” were used for the measurements.
Statistics
The SPSS package program, chi square, the Spearman correlation test and logistic regression were used in the evaluation of the data. In univariate analysis, two multivariate models were constructed with independent variables giving p<0.10 values, corrected for age and gender, with the dependent variable SBS. Hosmer-Lemeshow test results (p>0.05) showed that the model-data fit was sufficient. For the first model with independent variables, categorical variables were constructed according to the responses to the questions about environmental disturbance factors, such as indoor environment, air flow, odour, temperature, noise, lighting, dust, air quality, and the effects of these factors on working performance. For the second model, variables were created by taking the values measured in the environment (the linear logarithm of some were taken to provide a normal distribution). The statistical significance was set to p<0.05.
Results
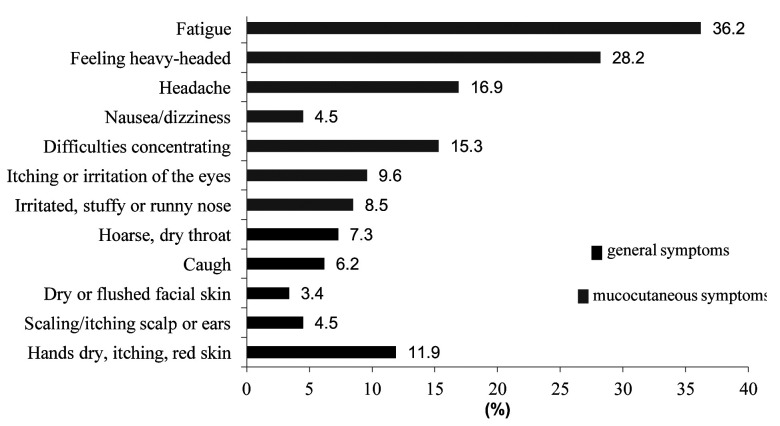
The study was completed with 177 people, 61.6% (n: 109) women, and the mean age was 30.14±5.7 (min: 21, max: 46). The prevalence of SBS was found to be 20.9% (n: 37). When the symptoms that employees reported as originating from work were assessed, the general symptoms, in order of frequency, were 36.2% fatigue, 28.2% feeling heavy-headed and 16.9% headache. The mucocutaneous symptoms were 11.9% hands dry, itching, red skin, 9.6% itching, burning or irritation of the eyes, and 8.5% irritated, stuffy or runny nose (figure 2).
Figure 2.
Percentage of the presence of SBS symptoms (general and mucocutaneous) in participants
Situations in the hospital environment where the secretaries were disturbed were interrogated and model 1 was formed around their answers. The percentages of situations found unfavourable were identified as follows: 50.8% had stuffy “bad” air with an unpleasant odour; 40.1% had an unsuitable temperature, 32.8% were noisy and 26.6% were dusty or dirty, in that order of frequency. Of the participants, 56.5% stated that the indoor quality of the hospital was inadequate, while 55.4% of the participants stated that the perceived quality of the work was inadequate (table 1).
Table 1.
Perceived indoor environmental conditions at the hospital
| n | % | |
| Unsuitable temperature | 71 | 40.1 |
| Noisy | 58 | 32.8 |
| Unsuitable light | 27 | 15.3 |
| Dusty and dirty | 47 | 26.6 |
| Indoor quality of the hospital (inadequate) | 100 | 56.5 |
| Perceived quality of work (inadequate) | 98 | 55.4 |
| Stuffy “bad” air with an unpleasant odour | 90 | 50.8 |
| Smoking | 30 | 16.9 |
As a result of model 1, the risk of SBS was found to be 2.9 times higher (p: 0.041) for females, 2.8 times higher (p: 0.040) for individuals who described the working environment as dusty, 2.6 times higher (p: 0.05) for subjects complaining of stuffy “bad” air, dry air and an unpleasant odour (table 2).
Table 2.
Relationship between SBS and perceived indoor environmental conditions at the hospital
| Model 1 | Regression coefficient (ß) | Standard Error (SE) | Wald | p | Odds Ratio (OR) | 95% Confidence Interval (CI) for OR | |
| Lower | Upper | ||||||
| Sex | 1.065 | 0.523 | 4.157 | 0.041 | 2.90 | 1.042 | 8.083 |
| Unsuitable temperature | 0.124 | 0.521 | 0.056 | 0.812 | 1.13 | 0.407 | 3.144 |
| Noisy | 0.349 | 0.546 | 0.408 | 0.523 | 1.42 | 0.486 | 4.136 |
| Unsuitable light | -0.383 | 0.579 | 0.436 | 0.509 | 0.68 | 0.219 | 2.123 |
| Dusty and dirty | 1.056 | 0.513 | 4.237 | 0.040 | 2.87 | 1.052 | 7.851 |
| Indoor quality of the hospital (inadequate) | -0.795 | 0.487 | 2.666 | 0.103 | 0.45 | 0.174 | 1.173 |
| Perceived quality of work (inadequate) | 0.518 | 0.473 | 1.199 | 0.274 | 1.68 | 0.664 | 4.247 |
| Stuffy “bad” air with an unpleasant odour | 0.961 | 0.508 | 3.578 | 0.050 | 2.61 | 1.012 | 7.077 |
| Smoking | 0.901 | 0.498 | 3.278 | 0.070 | 2.46 | 0.928 | 6.529 |
| Age | -0.016 | 0.035 | 0.200 | 0.655 | 0.98 | 0.920 | 1.054 |
All measurements were found to be within normally acceptable limits. Hospital indoor measurement results are presented in table 3. As a result of the variant model 2, which was formed from the indoor measurement results, the risk of SBS was found to be 1.2 times higher (p: 0.014) with increases in the measured noise level, and 2.1 times higher (p: 0.043) with increased CO2 concentrations (table 4).
Table 3.
Hospital indoor measurement results
| Mean (median) | Standard deviation | Min-max | |
| Noise (dB) | 52.92 | 4.36 | 44-66 |
| Light (lux) | 269.43 (271.82) | 106.04 | 105-501 |
| Temperature (°C) | 21.86 | 1.36 | 20-24 |
| Humidity (%) | 28.81 | 6.47 | 22-45 |
| CO2 (ppm) | 129.26 (104.71) | 102.59 | 28-559 |
dB:decibel, ppm:parts per million
Table 4.
Relationship between SBS and hospital indoor measurements
| Model 2 | Regression coefficient (ß) | Standard Error (SE) | Wald | p | Odds Ratio (OR) | 95% Confidence Interval (CI) for OR | |
| Lower | Upper | ||||||
| Noise | 0.142 | 0.058 | 6.042 | 0.014 | 1.20 | 1.029 | 1.291 |
| Light intensity* | 0.001 | 0.003 | 0.123 | 0.726 | 0.99 | 0.994 | 1.004 |
| Temperature | 0.201 | 0.284 | 0.499 | 0.480 | 1.22 | 0.700 | 2.132 |
| Humidity | 0.061 | 0.074 | 0.688 | 0.407 | 1.06 | 0.920 | 1.228 |
| CO2* | 1.940 | 0.959 | 4.096 | 0.043 | 2.14 | 1. 22 | 2.941 |
| Sex | 1.199 | 0.462 | 6.735 | 0.009 | 3.32 | 1.341 | 8.204 |
| Age | -0.010 | 0.034 | 0.089 | 0.765 | 0.99 | 0.927 | 1.058 |
* A linear logarithm was taken to fit the normal distribution
Discussion
Although many studies in the literature examine SBS and indoor air quality in the office environment (4-6, 10, 11, 13, 22, 25), insufficient work has been done among hospital staff, and especially among secretaries. Our study was planned with a cross-sectional design, and the symptoms reported by individuals were evaluated according to the criteria for SBS diagnosis. The prevalence of SBS was found to be 20.9%. At the same time, measurements were taken in the indoor environment of the hospital. Variables that could be related to SBS were evaluated with two models. The first model considered the relationship between the variables and the indoor measurement results, and the second involved the factors reported by individuals who were disturbed by the environmental conditions.
Other studies have evaluated symptoms such as fatigue, headache, feeling heavy-headed, difficulties concentrating, burning itching of the eyes, stuffy or runny nose, dry throat, cough, dry facial skin, dry or itching hands. In these studies, the symptoms were classified as either general or mucocutaneous, and a symptom from each group was considered sufficient for a diagnosis of SBS (4, 5, 12, 18, 19, 24, 27). In some studies, each symptom was evaluated separately (8, 11, 14, 20, 22). In a study by Gómez-Acebo et al., a different scoring and predictive model was developed to describe the SBS that originates from the hospital’s indoor environment (8). When all these studies are evaluated, most of them have a cross-sectional design, but the diagnostic criteria for SBS appear to be different, although the symptoms examined are the same. It should not be forgotten that the indoor environment will vary in these studies, which are carried out in different countries and buildings. This can lead to conclusions that suggest a different prevalence of SBS across the studies. The prevalence of SBS ranges from 31.9% to 86.4% in studies conducted in hospital buildings (8, 24, 27). In a hospital study in Sweden, the most common general symptoms were found to be fatigue, feeling heavy-headed and headache, and the most common mucocutaneous symptoms were hand and face dryness, redness, dry throat and eye complaints (19). When the symptoms reported by secretaries in our study were evaluated, similar results were found as those reported in the literature. In one study, high noise levels were shown to cause symptoms such as high-level headache and dizziness (10). Rostron noted that the disturbing effects of noise level changes were related to physiological and psychological factors in the person concerned (21). In our study, it was seen that the risk of developing SBS was related to increases in the noise level. From examining a large number of patients, we can confidently say that working in a noisy environment causes fatigue and headache.
Mucocutaneous symptoms, such as skin and throat dryness, are often seen as signs of dry, dusty air (17). Temperature and humidity both affect the emotions and symptoms of employees, with a low humidity causing dryness in the eyes, nose and throat, and a general discomfort. In some studies, temperature and humidity are shown to be significantly associated with SBS symptoms (17, 18). While the recommended indoor humidity level is in the range of 30-65%, in winter the temperature should be within the range 20 to 25.5°C, as this is specified as being suitable for thermal comfort (9). We think that the absence of an association between temperature and humidity and SBS in our study may be due to the fact that the hospital ventilation and heating systems are adequate. In addition, humidity was measured as being at normal levels, showing that the air is not dry. We suggest that the many dry eye complaints of secretaries reflect that fact that they spend long periods in front of computers.
In many studies, the prevalence of SBS and the prevalence of symptoms were significantly higher in females than in males (7, 25, 29). The reasons for this may be differences in workload or gender characteristics (15). Eriksson et al. stated that females carry more responsibilities outside of the workplace, such as housework and childcare, and this increases the likelihood that they will show symptoms of SBS (7). In a study conducted in a hospital in Spain, the risk of SBS was reported to be approximately twice as high in females as in males (8).
In our study, SBS prevalence was significantly higher among those who thought that the environment in which they worked was dusty and dirty, among those who described the environment in which they worked as airless or dry, and among those who were uncomfortable due to the unpleasant odour in the environment. That their attitudes may have made them more susceptible. In one study, more symptoms of SBS were seen in those who complained of inadequate ventilation and bad odour (27). In Magnavita’s study, the most common complaints were sudden changes in indoor temperature, stuffy air, unpleasant odour, tobacco smoke, dust and dirt (12). In a study similar to ours in Finland, SBS was found to be higher in those who had an airless environment, dry air, and where there were complaints of dust and dirt (20).
In some studies that evaluated SBS, indoor environment measurements were reported in addition to the symptoms (6, 10, 16, 18, 23, 29).
According to the standards of the American Society of Heating, Refrigerating and Air Conditioning Engineers (ASHRAE), it is recommended that, when controlling indoor air quality, a threshold of 700 ppm for CO2 concentration should not be exceeded (1). In our study, CO2 levels measured in the indoor environment of the hospital were within acceptable values. However, it has been recognised that the risk of developing SBS increased two times with increase in CO2 concentration. In many studies, a significant correlation has been found between increases in CO2 level and increases in the prevalence of SBS (6, 16). Although there are seldom complaints of SBS in naturally ventilated buildings, there is a study in which CO2 levels were found to be high in these buildings, and an inversely proportional relation was found between CO2 level and SBS complaints (29). It is known that the CO2 level decreases as the indoor air flow rate increases (23). The low CO2 levels in our study can be explained by the adequate ventilation in the environment as well as the low patient concentration on the days when the measurements are taken.
A limitation of the study is that only the secretaries were surveyed, and the measurement times were relatively short. Another limitation is that the diagnosis of SBS was based on the answers of the participants and memory factors can affect the answers of participants. In addition, the study was conducted in winter, and this may have caused seasonal differences that affect results. Because of our limitations in terms of equipment, CO2 was measured as a single chemical indicator for indoor air measurements in this study. Other indoor air pollutants such as nitrogen dioxide, sulfur dioxide, ozone, volatile organic compounds and particulate matters could not be measured due to this technical limitation. More efficient results could be obtained if measurements were made over a longer period and in more than one hospital, with the participation of all hospital employees.
Conclusion
The greatest risks of experiencing SBS were determined as being female, thinking that the working environment was dusty and dirty, being uncomfortable with the air, because it was dry or had an unpleasant odour, and where there were increased CO2 and noise levels. Bearing these factors in mind, we think that hospital administrations should be informed about arrangements and measures that will improve the quality of the internal environment of the hospital. Future studies should be planned to determine the relationship between the health of the staff working in hospitals and the quality of the health service provided.
No potential conflict of interest relevant to this article was reported by the authors
References
- 1.American Society of Heating Refrigerating and Air Conditioning Engineer (ASHRAE) Standard. Ventilation for Acceptable Indoor Air Quality. 2013; 38 ASHRAE Standard 62-1989. Ventilation for acceptable indoor air quality. Atlanta: American Society of Heating, Refrigerating and Air-conditioning Engineers Incorporated, 1989 [Google Scholar]
- 2.Andersson K, Fagerlund I, Bodin L, Ydreborg B. Questionnaire as an instrument when evaluating indoor climate. Healthy Buildings ’88, Stockholm. 1988;1:139–146. [Google Scholar]
- 3.Andersson K, Stridh G. Levy F, Maroni., editor. The use of standardized questionnaires in building related illness (BRI) and sick building syndrome (SBS) surveys. NATO/CCMS pilot study on indoor air quality. National Institute of Occupational Health, Oslo. 1992:47–64. Retrieved from http://www.mmquestionnaire.se/mmq/mm040_care.pdf . [Google Scholar]
- 4.Azuma K, Ikeda K, Kagi N, et al. Evaluating prevalence and risk factors of building-related symptoms among office workers: Seasonal characteristics of symptoms and psychosocial and physical environmental factors. Environ Health Prev Med. 2017;22:38. doi: 10.1186/s12199-017-0645-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chirico F, Ferrari G, Taino G, et al. Prevalence and risk factors for Sick Building Syndrome among Italian correctional officers: A pilot study. J Health Soc Sci. 2017;2:31–46. [Google Scholar]
- 6.Erdmann CA, Apte MG. Mucous membrane and lower respiratory building related symptoms in relation to indoor carbon dioxide concentrations in the 100-building BASE dataset. Indoor Air. 2004;14:127–134. doi: 10.1111/j.1600-0668.2004.00298.x. [DOI] [PubMed] [Google Scholar]
- 7.Eriksson NM, Stenberg BG. Baseline prevalence of symptoms related to indoor environment. Scand J Public Health. 2006;34:387–396. doi: 10.1080/14034940500228281. [DOI] [PubMed] [Google Scholar]
- 8.Gómez-Acebo I, Dierssen-Sotos T, Pérez-Belmonte E, Llorca J. Investigating an outbreak of non-specific building-related symptoms in workers of a general hospital. Int J Occup Med Environ Health. 2013;26:563–571. doi: 10.2478/s13382-013-0130-2. [DOI] [PubMed] [Google Scholar]
- 9.Indoor air quality handbook. A practical guide to indoor air quality investigations. 2013. Retrieved 16 August 2018 from http://www.tsi.com/uploadedFiles/_Site_Root/Products/Literature/Handbooks/IAQ_Handbook_2011_US_2980187-web.pdf . [Google Scholar]
- 10.Jafari MJ, Khajevandi AA, Najarkola SAM, et al. Association of sick building syndrome with indoor air parameters. Tanaffos. 2015;14:55–62. [PMC free article] [PubMed] [Google Scholar]
- 11.Lu CY, Tsai MC, Muo CH, et al. Personal, Psychosocial and Environmental Factors Related to Sick Building Syndrome in Official Employees of Taiwan. Int J Environ Res Public Health. 2017;15:7–16. doi: 10.3390/ijerph15010007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Magnavita N. Work-related symptoms in indoor environments: a puzzling problem for the occupational physician. Int Arch Occup Environ Health. 2015;88:185–196. doi: 10.1007/s00420-014-0952-7. [DOI] [PubMed] [Google Scholar]
- 13.Marmot AF, Eley J, Stafford M, et al. Building health: an epidemiological study of “sick building syndrome” in the Whitehall II study. Occup Environ Med. 2006;63:283–289. doi: 10.1136/oem.2005.022889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mendell MJ, Lei-Gomez Q, Mirer AG, et al. Risk factors in heating, ventilating, and air-conditioning systems for occupant symptoms in US office buildings: the US EPA BASE study. Indoor Air. 2008;18:301–316. doi: 10.1111/j.1600-0668.2008.00531.x. [DOI] [PubMed] [Google Scholar]
- 15.Norbäck D. An update on sick building syndrome. Curr Opin Allergy Clin Immunol. 2009;9:55–59. doi: 10.1097/ACI.0b013e32831f8f08. [DOI] [PubMed] [Google Scholar]
- 16.Norbäck D, Nordström K. Sick building syndrome in relation to air exchange rate, CO(2), room temperature and relative air humidity in university computer classrooms: an experimental study. Int Arch Occup Environ Health. 2008;82:21–30. doi: 10.1007/s00420-008-0301-9. [DOI] [PubMed] [Google Scholar]
- 17.Norbäck D, Torgen M, Edling C. Volatile organic compounds, respirable dust, and personal factors related to prevalence and incidence of sick building syndrome in primary schools. Br J Ind Med. 1990;47:733–741. doi: 10.1136/oem.47.11.733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nordström K, Norbäck D, Akselsson R. Effect of air humidification on the sick building syndrome and perceived indoor air quality in hospitals: a four month longitudinal study. Occup Environ Med. 1994;51:683–688. doi: 10.1136/oem.51.10.683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nordström K, Norbäck D, Akselsson R. Influence of indoor air quality and personal factors on the sick building syndrome (SBS) in Swedish geriatric hospitals. Occup Environ Med. 1995;52:170–176. doi: 10.1136/oem.52.3.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Reijula K, Sundman-Digert C. Assessment of indoor air problems at work with a questionnaire. Occup Environ Med. 2004;61:33–38. [PMC free article] [PubMed] [Google Scholar]
- 21.Rostron J. Sick building syndrome: A review of causes, consequences and remedies. J Retail Leisure Property. 2008;7:291–303. [Google Scholar]
- 22.Runeson-Broberg R, Norbäck D. Sick building syndrome (SBS) and sick house syndrome (SHS) in relation to psychosocial stress at work in the Swedish workforce. Int Arch Occup Environ Health. 2013;86:915–922. doi: 10.1007/s00420-012-0827-8. [DOI] [PubMed] [Google Scholar]
- 23.Santamouris M, Synnefa A, Asssimakopoulos M, et al. Experimental investigation of the air flow and indoor carbon dioxide concentration in classrooms with intermittent natural ventilation. Energy Build. 2008;40:1833–1843. [Google Scholar]
- 24.Sayehmiri K, Kazemy M, Shirmohamadi N, et al. Evaluation of sick building syndrome prevalence among Mustafa Khomeini hospital staff in Ilam, 2015. Scientific Journal of Ilam University of Medical Sciences. 2018;25:1–9. [Google Scholar]
- 25.Skov P, Valbjørn O, Pedersen BV, et al. Influence of personal characteristics, job-related factors and psychosocial factors on the sick building syndrome. Scand J Work Environ Health. 1989;15:286–295. doi: 10.5271/sjweh.1851. [DOI] [PubMed] [Google Scholar]
- 26.United States Environmental Protection Agency. Indoor Air Facts No. 4 (revised). Sick Building Syndrome. Research and Development (MD-56), 1991 Feb [Google Scholar]
- 27.Vafaeenasab MR, Morowatisharifabad MA, Ghaneian MT, et al. Assessment of Sick Building Syndrome and Its Associating Factors Among Nurses in the Educational Hospitals of Shahid Sadoughi University of Medical Sciences, Yazd, Iran. Glob J Health Sci. 2015;7:247–253. doi: 10.5539/gjhs.v7n2p247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.World Health Organization. Copenhagen: WHO Regional Office for Europe; 1983. Indoor air pollutants: exposure and health effects. (EURO Reports and Studies No 78) [Google Scholar]
- 29.Zweers T, Preller L, Brunekreef B, et al. Health and indoor climate complaints of 7043 office workers in 61 buildings in the Netherlands. Indoor Air. 1992;2:127–136. [Google Scholar]