Abstract
Background:
Healthcare workers (HCWs) are faced with an elevated risk of exposure to SARS-COV-2 due to the clinical procedures they perform on COVID-19 patients. However, data for frontline HCWs level of exposure and risk of COVID-19 virus infection are limited.
Objective:
We investigated the level of exposure and risk of COVID-19 virus infection among HCWs in COVID-19 treatment centers in Ghana.
Methods:
A cross-sectional study was utilized in this study and HCWs were invited by convenience to participate in the study, 408 HCWs in 4 COVID-19 treatment centers participated in the study. Adherence to infection prevention and control (IPC) measures were used to categorized HCWs as low or high risk of COVID-19 virus infection. The WHO COVID-19 risk assessment tool was used to collect quantitative data from the study participants.
Results:
There was a high (N = 328, 80.4%) level of occupational exposure to the COVID-19 virus. However, only 14.0% of the exposed HCWs were at high risk of COVID-19 virus infection. Healthcare workers who performed or were present during any aerosol-generating procedures (AGP) were 23.8 times more likely to be exposed compared to HCWs who did not perform or were absent during any AGP (AOR 23.83; 95% CI: 18.45, 39.20). High risk of COVID-19 virus infection was less likely among registered nurses (AOR = 0.09; 95% CI: 0.02, 0.60), HCWs who performed or were present during any AGP (AOR = 0.05; 95% CI: 0.01, 0.50) and HCWs with a master’s degree qualification (AOR 0.06; 95% CI: 0.01, 0.63).
Conclusion:
Despite the high level of exposure to the COVID-19 virus among HCWs in the treatment centers, only 14.0% were at high risk of COVID-19 virus infection. To protect this group of HCWs, treatment centers and HCWs should continue to adhere to WHO and national IPC protocols in managing of COVID-19 cases.
Keywords: COVID-19, healthcare workers, exposure risk, infectious diseases, safety, infection prevention and control, Ghana
Background
The novel coronavirus disease 2019 (COVID-19) has ravaged almost every part of the globe.1 It is disrupting global public health systems, economies, societies and personal lives.2-4 Indeed, COVID-19 has caused significant morbidity and mortality across different regions of the globe. WHO as of September 27, 2020 (1:08 pm CEST) reports of over thirty-two million (32 000 000) confirmed cases of COVID-19 worldwide, of which over nine hundred and ninety thousand (990 000) have died giving a case fatality rate of 3.1%.5 In Africa, there are approximately 1 000 000 confirmed cases of COVID-19 with over 25 000 deaths as of September 27, 2020 (1:08 pm CEST).5 On March 12, 2020, Ghana confirmed its first 2 cases of COVID-19; the 2 cases were returnees from Norway and Turkey.6 Since then, Ghana had recorded 46,353 laboratory-confirmed cases of COVID-19 as at September 22, 2020, of which there were 299 deaths and 45 577 recoveries giving a case fatality rate of 0.6%.7
COVID-19 is a viral respiratory disease that was initially discovered in Wuhan, China, in a group of patients with a severe respiratory infection. COVID-19 is caused by a novel coronavirus which was scientifically named severe acute respiratory syndrome coronavirus 2 (SARS-COV-2).8 It has alarming characteristics of spreading rapidly among populations, causing a severe form of the disease in older adults and in patients with underlying medical conditions.9,10 Evidence suggests that the main route of human-to-human transmission is via respiratory droplets generated through coughing and sneezing. Contacts with an infected person or a contaminated surface and subsequent transfer from the hands to the nose, mouth, and eye also promote the transmission of SARS-COV-2.10,11 COVID-19 has an average incubation period of 5 to 6 days, which can extend up to 14 days with an infected individual going symptomless for several days, thereby making the diagnosis and interruption of human-to-human transmission of the disease difficult.12
The clinical manifestation of COVID-19 is not specific but ranges from asymptomatic to severe symptoms such as pneumonia, multiple organ failure, and finally death.12 Data from several studies indicate that COVID-19 manifests clinically with common symptoms such as fever, cough, sore throat, myalgia, fatigue, shortness of breath, and sputum production.12-14
Currently, there is no effective vaccine or antiretroviral drug for the prevention and treatment of COVID-19.15 Therefore, prevention remains the best weapon against COVID-19; preventive strategies focus on minimizing exposure to the COVID-19 virus through the use of PPEs regular handwashing with soap, observing physical distancing and covering coughs and sneezes with flexed elbow or tissue.15,16 Healthcare workers, in particular, are strongly recommended to adhere to appropriate IPC measures in managing COVID-19 cases to minimize the risk of COVID-19 virus infection.17 To further protect frontline HCWs, the WHO urgently issued interim guidance to guide HCWs on IPC protocols during healthcare management of COVID-19 cases.17 Non-adherence to IPC protocols by HCWs in managing infectious diseases such as COVID-19 puts HCWs, patients, and communities at risk.18 In contrast, compliance with IPC practices by HCWs will interrupt the transmission of pathogens such as SARS-COV-2 from patients to HCWs as well as to their friends, relatives, and caregivers.19 Adherence to appropriate IPC practices can, therefore play a critical role by minimizing HCWs exposure to SARS-COV-2. However, the inadequacy of IPC logistics in healthcare facilities poses a serious challenge for HCWs to adhere strictly to IPC protocols.19,20
Healthcare workers are at the forefront of fighting against the COVID-19 pandemic and play a critical role in the clinical management of patients with COVID-19.21 They are therefore faced with an elevated risk of exposure to SARS-COV-2 due to the clinical procedures they perform on COVID-19 patients.4 Indeed, there are reports of COVID-19 infections among HCWs across the globe.22 Similarly, in Ghana, there have been over 2000 COVID-19 infections among doctors, nurses and other healthcare workers.23 However, the level of HCWs exposure to the COVID-19 virus and the extent of risk in the designated treatment centers in Ghana are not known. Understanding HCW levels of exposure to the COVID-19 virus is crucial not only for characterizing HCW levels of exposure to the virus but also for preventing HCW exposure to the COVID-19 virus and informing the IPC policies and protocols in the designated COVID-19 treatment centers.
Methods and Materials
The study was a cross-sectional study that was conducted among HCWs managing COVID-19 cases in treatment centers located in the Greater Accra and Ashanti regions. The 4 treatment centers has an estimated population of 600 healthcare workers comprising of both clinical and non-clinical staff. Quantitative data were collected to better understand the HCW levels of exposure to the COVID-19 virus. Greater Accra and Ashanti regions were purposively chosen because these 2 regions are the epicenters of COVID-19 cases in Ghana with the Greater Accra region alone, having over 50% of Ghana’s confirmed cases.
The study population included all healthcare workers who are working in the designated COVID-19 treatment centers in the Greater Accra and Ashanti regions. For this study, a frontline healthcare worker was defined as all clinical and non-clinical staff in the COVID 19 treatment centers involved in the provision of care for COVID-19 patients, including those who may not have provided direct care to the COVID-19 patients but may have contact with COVID-19 patients’ body fluids and potentially contaminated items or environmental surfaces. Hence, they included healthcare professionals, allied health professionals, and other health workers, such as cleaning and laundry personnel, respiratory therapists, X-ray physicians, technicians, nutritionists, admission/reception clerks, phlebotomists, laboratory personnel, pharmacists/pharmacy technicians, catering staffs, and cleaners.18
Study Measures
Demographic characteristics of the HCWs: The demographic information of the HCWs included age (<35, ≥35); Gender (Male, Female); Marital status (Single, Married, Separated/divorced/widowed); Type of health professional (Assistant nurses/nurse technician or equivalent, catering staffs, cleaners, laboratory personnel, medical doctors, midwives, registered nurses, Pharmacists, and other health professionals); staff category (non-clinical, clinical); Type of health facility (cleaning services, emergency, laboratory, medical unit, outpatient, pharmacy, others); Highest level of qualification (SSCE/WASSCE, Certificate, Diploma, Bachelors, Masters); Work experience (≤ 10, > 10); Tested for COVID-19 (yes, no); Source of information on COVID-19 (international organization, government sites and media, social media, academic journals, News media); Have family member infected with COVID-19 (yes, no); performed/present during any AGP (yes, no).
Community exposure to the COVID-19 virus: This was measured using the WHO COVID-19 exposure risk assessment tool.24 Healthcare worker was considered community exposure to COVID-19 virus if he/she responded “yes” to having a history of staying in the same household or classroom environment with a confirmed COVID-19 patient or having a history of traveling together in close proximity (within 1 m) with a confirmed COVID-19 patient in any kind of conveyance.
Occupational exposure to COVID-19 virus: This was also measured using the WHO COVID-19 risk assessment tool.24 Exposure to COVID-19 virus was assessed by a “yes” response to performing any of the following activities on a COVID-19 patient: providing direct care to a COVID-19 patient, performed/present when aerosol-generating procedures were performed on COVID-19 patients and had direct contact with the environment where confirmed COVID-19 patient was cared for.
Risk categorization of healthcare workers exposed to the COVID-19 virus. Healthcare workers exposed to the COVID-19 virus were further categorized as “high risk for COVID-19 virus infection” and “low risk of COVID-19 virus infection.” Healthcare worker was considered high risk for COVID-19 virus infection if he/she did not respond “always, as recommended” during healthcare interaction with a confirmed COVID-19 patient to any of the following IPC measures: wearing of single-use gloves, medical masks, face shield or goggles/protective glasses, disposable gown, removing and replacing PPE according to protocol, performing hand hygiene (before and after touching a COVID-19 patient, before and after any clean or aseptic procedure, after exposure to body fluids, after touching patient surroundings) and decontaminating high touch surfaces at least 3 times daily.
It also included if a healthcare worker did not respond “always, as recommended” during aerosol-generating procedures (AGPs) on COVID-19 patient to any of the following IPC measures: wearing of single-use gloves, N95 mask (or equivalent operator), face shield or goggles/protective glasses, disposable gown, waterproof apron, removing and replacing PPE according to protocol, performing hand hygiene (before and after touching a COVID-19 patient, before and after any clean or aseptic procedure, after exposure to body fluids, after touching patient surroundings), decontaminating high touch surfaces at least 3 times daily, whether the healthcare worker had any type of accident with body fluid/respiratory secretions of a COVID-19 patient. Any other response by the HCW was considered low risk to COVID-19 virus infection.
Sample Size and Sampling Procedure
The sample size was determined using the Cochran formula,25 at 95% confidence interval, 5% margin error (d) with assumed exposure level (p) of 50% where N is the sample size, Z2 (statistic) = 1.96, p (Exposure level) = 0.5 and d (margin of error) = 0.05.
Exposure of HCWs to the COVID-19 virus is not known in Ghana; hence, the justification for an exposure level of 50%. Ten percent was added to cater to non-response, resulting in a final sample size of 424 study participants.
With proportional allocation of the sample size to the 4 treatment centers and by convenience, the research team approached the HCWs at the treatment centers and invited them to participate in the study. Those who consented to participate in the study signed a consent form before being given the questionnaire. Treatment centers that participated in the study were Ga East Municipal Hospital, Pentecost Convention Center, Barekese and Kumasi South Hospital. Four hundred and eight HCWs agreed to participate in the study (response rate of 96%).
Data Collection
The data collection tool consisted of demographic characteristics (7 items), HCW Community exposure to the COVID-19 virus (2 items), HCW activities performed on COVID-19 patient in the treatment center (7 items), adherence to IPC measures during healthcare interaction (10 items), adherence to IPC measures when performing aerosol-generating procedures (11 items), and an accident with biological material (2 items). The data were collected through self-administration in adherence to national COVID-19 protocols.
Data Analysis
The data were entered into Epidata Entry Client version 4.6.0.2 and later exported to STATA 14.2 for further analysis. The data presentation included sociodemographic characteristics of the HCWs, exposure to COVID-19 virus and risk of COVID-19 infection. Frequency and percentages were used for categorical variables, while means and standard deviation were calculated for numerical variables. Chi-square and multivariate logistic regression analysis was used to determine the association between the outcome variables and the independent variables. Only variables that were significant after the chi-square analysis were included in the multivariate analysis. Variables were significant at P-value less than .05.
Results
Sociodemographic Characteristics of the Study Participants
The sociodemographic characteristics of the study participants, which represents the workforce in the treatment centers are presented in Table 1. A total of 408 HCWs comprising of registered nurses (39.5%), assistant nurses (11.5%), medical doctors (6.9%), laboratory personnel (2.5%), midwives (7.1%), cleaners (12.3%) and other health professionals (14.5%). The median age of the study participants was 32.3 years, with minimum and maximum ages of 19 and 49 years, respectively. More females (57.6%) than males participated in the study, with 49.3% of the HCWs married.
Table 1.
Sociodemographic Characteristics of the Study Participants.
| Independent variables | Frequency N = 408 | Percent (%) |
|---|---|---|
| Mean age (SD), Min–Max | 32.3 (6.2), 19–49 | |
| Age (in years) | ||
| <35 | 277 | 67.9 |
| ≥35 | 131 | 32.1 |
| Gender | ||
| Female | 235 | 57.6 |
| Male | 173 | 42.4 |
| Marital status | ||
| Single | 200 | 49.0 |
| Married | 201 | 49.3 |
| Separated/Divorced/Widowed | 7 | 1.7 |
| Type of health professional | ||
| Assistant nurse | 47 | 11.5 |
| Catering staff | 16 | 3.9 |
| Cleaner | 50 | 12.3 |
| Laboratory personnel | 10 | 2.5 |
| Medical doctor | 28 | 6.9 |
| Midwives | 29 | 7.1 |
| Registered nurse | 161 | 39.5 |
| Pharmacist | 8 | 2.0 |
| Other health professionalsa | 59 | 14.5 |
| Staff category | ||
| Non-clinical | 123 | 30.2 |
| Clinical | 285 | 69.9 |
| Type of health facility | ||
| Cleaning services | 50 | 12.3 |
| Emergency | 117 | 28.7 |
| Laboratory | 10 | 2.5 |
| Medical unit | 91 | 22.3 |
| Outpatient | 40 | 9.8 |
| Pharmacy | 10 | 2.5 |
| Othersb | 90 | 22.1 |
| Highest level of qualification | ||
| SSSCE/WASCE | 55 | 13.5 |
| Certificate | 129 | 31.6 |
| Diploma | 100 | 24.5 |
| Bachelor | 100 | 24.5 |
| Masters | 24 | 5.9 |
| Work experience (in years) | ||
| ≤10 | 339 | 83.1 |
| >10 | 69 | 16.9 |
| Tested for COVID-19 | ||
| No | 331 | 81.1 |
| Yes | 77 | 18.9 |
| Sources of information on COVID-19† | ||
| International organizations (eg, WHO, CDC) | 275 | 67.4 |
| Government sites and media (eg, GHS, MOH-Ghana) | 292 | 71.6 |
| Social media (eg, WhatsApp, Facebook, Twitter) | 248 | 60.8 |
| Academic journal | 107 | 26.2 |
| News media (eg, TV, Radio, Newspaper) | 351 | 86.0 |
| Have family member infected with Covid-19 | ||
| No | 395 | 96.8 |
| Yes | 13 | 3.2 |
| Performed/present during any AGP | ||
| No | 328 | 80.1 |
| Yes | 80 | 19.6 |
Others—Pharmacy technician/dispenser, Physical and respiratory therapist, Admission/reception clerks, accountants, administrative and IT manager, Clinical engineers.
Others—Isolation center, Catering services.
Multiple response variables.
Healthcare Workers’ Occupational and Community Exposure to the COVID-19 Virus
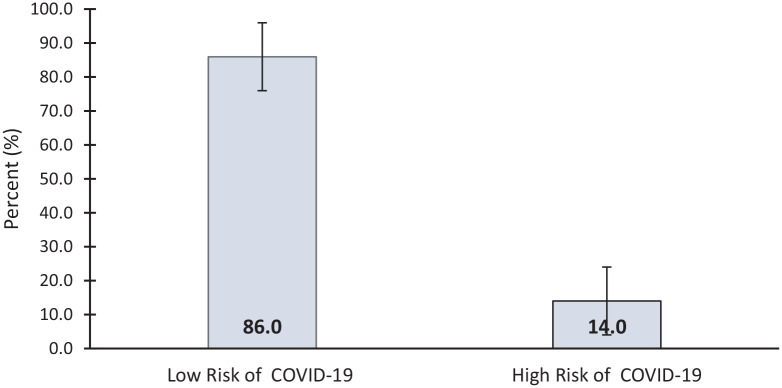
The prevalence of occupation exposure and community exposure of HCWs to the COVID-19 virus was 80.4% (95% CI = 72.2-84.1) and 8.8% (95% CI =6.3-12.1), respectively (Figure 1).
Figure 1.
Healthcare workers’ occupational and community exposure to the COVID-19 virus.
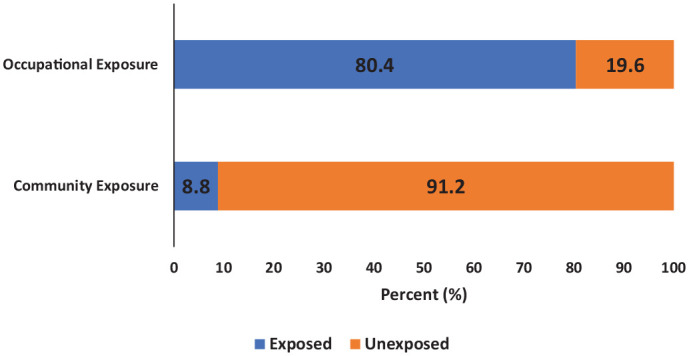
Among HCWs with occupational exposure (N = 328) to the COVID-19 virus, a vast majority (86.0%) were at low risk for COVID-19 virus infection, while 14% were at high risk for COVID-19 virus infection (Figure 2).
Figure 2.
Risk of COVID-19 virus infection among the exposed healthcare workers.
Factors Associated with Increased Occupational Exposure of HCWS to the COVID-19 Virus
A chi-square of independence found a statistically significant association between type of health professional, staff category, type of unit/department, highest level of qualification, performed/present during any AGP and workplace exposure to COVID-19 virus (Table 2).
Table 2.
Distribution of Study Participants Characteristics by Occupational Exposure to COVID-19 Virus and Risk for COVID-19 Virus Infection.
| Occupational exposure to COVID-19 |
Risk of COVID-19 virus infection |
||||||
|---|---|---|---|---|---|---|---|
| No (n = 80) | Yes (n = 328) | P-value | LR (n = 282) | HR (n = 46) | P-value | ||
| Variables | n (%) | n (%) | n (%) | n (%) | |||
| Age (in years) | |||||||
| <35 | 277 (67.9) | 57 (71.3) | 220 (67.1) | .473 | 190 (67.4) | 30 (65.2) | .773 |
| ≥35 | 131 (32.1) | 23 (28.7) | 108 (32.9) | 92 (32.6) | 16 (34.8) | ||
| Gender | |||||||
| Female | 235 (57.6) | 50 (62.5) | 185 (56.4) | .322 | 163 (57.8) | 22 (47.8) | .206 |
| Male | 173 (42.4) | 30 (37.5) | 143 (43.6) | 119 (42.2) | 24 (52.2) | ||
| Marital status | |||||||
| Single | 200 (49) | 44 (55) | 156 (47.6) | .492† | 132 (46.8) | 24 (52.2) | .036† |
| Married | 201 (49.3) | 35 (43.8) | 166 (50.6) | 147 (52.1) | 19 (41.3) | ||
| Separated/Divorced/Widowed | 7 (1.7) | 1 (1.3) | 6 (1.8) | 3 (1.1) | 3 (6.5) | ||
| Type of health professional | |||||||
| Assistant nurse | 47 (11.5) | 2 (2.5) | 45 (13.7) | <.001† | 39 (13.8) | 6 (13) | <.001† |
| Catering staff | 16 (3.9) | 15 (18.8) | 1 (0.3) | 1 (0.4) | 0 (0.0) | ||
| Cleaner | 50 (12.3) | 13 (16.3) | 37 (11.3) | 27 (9.6) | 10 (21.7) | ||
| Laboratory personnel | 10 (2.5) | 0 (0.0) | 10 (3.0) | 10 (3.5) | 0 (0.0) | ||
| Medical doctor | 28 (6.9) | 2 (2.5) | 26 (7.9) | 26 (9.2) | 0 (0.0) | ||
| Midwife | 29 (7.1) | 5 (6.3) | 24 (7.3) | 21 (7.4) | 3 (6.5) | ||
| Registered nurse | 161 (39.5) | 18 (22.5) | 143 (43.6) | 139 (49.3) | 4 (8.7) | ||
| Pharmacist | 8 (2.0) | 2 (2.5) | 6 (1.8) | 3 (1.1) | 3 (6.5) | ||
| Others | 59 (14.5) | 23 (28.7) | 36 (11.0) | 16 (5.7) | 20 (43.5) | ||
| Staff category | |||||||
| Non-Clinical | 123 (30.1) | 51 (63.7) | 72 (22.0) | <.001 | 43 (15.2) | 29 (63) | <.001 |
| Clinical | 285 (69.9) | 29 (36.3) | 256 (78.0) | 239 (84.8) | 17 (37) | ||
| Type of health facility | |||||||
| Cleaning services | 50 (12.3) | 13 (16.3) | 37 (11.3) | <.001† | 26 (9.2) | 11 (23.9) | <.001† |
| Emergency | 117 (28.7) | 11 (13.8) | 106 (32.3) | 101 (35.8) | 5 (10.9) | ||
| Laboratory | 10 (2.5) | 0 (0.0) | 10 (3.0) | 10 (3.5) | 0 (0.0) | ||
| Medical unit | 91 (22.3) | 6 (7.5) | 85 (25.9) | 83 (29.4) | 2 (4.3) | ||
| Out patient | 40 (9.8) | 6 (7.5) | 34 (10.4) | 28 (9.9) | 6 (13) | ||
| Pharmacy | 10 (2.5) | 2 (2.5) | 8 (2.4) | 4 (1.4) | 4 (8.7) | ||
| Others | 90 (22.1) | 42 (52.5) | 48 (14.6) | 30 (10.6) | 18 (39.1) | ||
| Highest level of qualification | |||||||
| Secondary level qualification | 55 (13.5) | 20 (25) | 35 (10.7) | .010† | 19 (6.7) | 16 (34.8) | <.001† |
| Certificate | 129 (31.6) | 22 (27.5) | 107 (32.6) | 97 (34.4) | 10 (21.7) | ||
| Diploma | 100 (24.5) | 19 (23.8) | 81 (24.7) | 71 (25.2) | 10 (21.7) | ||
| Bachelor | 100 (24.5) | 18 (22.5) | 82 (25.0) | 75 (26.6) | 7 (15.2) | ||
| Masters | 24 (5.9) | 1 (1.3) | 23 (7.0) | 20 (7.1) | 3 (6.5) | ||
| Work experience (in years) | |||||||
| 1-10 | 339 (83.1) | 68 (85) | 271 (82.6) | .611 | 235 (83.3) | 36 (78.3) | .400 |
| >10 | 69 (16.9) | 12 (15) | 57 (17.4) | 47 (16.7) | 10 (21.7) | ||
| Performed/present during any AGP | |||||||
| No | 328 (80.4) | 80 (100.0) | 248 (75.6) | <.001† | 203 (72) | 45 (97.8) | <.001† |
| Yes | 80 (19.6) | 0 (0.0) | 80 (24.4) | 79 (28) | 1 (2.2) | ||
Abbreviations: LR, low risk of COVID-19 virus infection; HR, high risk of COVID-19 virus infection.
Bold entries; Significant P-value <.05.
Fisher’s exact P-value (some cell frequencies <5)
In a multivariate logistic regression model, HCWs who perform or were present during any AGP were 23.8 times more likely to be exposed compared to those respondents who were not present or did not perform any AGP (AOR = 23.83; 95% CI: 18.45-39.20) (Table 3).
Table 3.
Factors Associated with Increased Occupational Exposure to COVID-19 Virus and Risk of COVID-19 Virus Infection Among the Exposed Healthcare Workers.
| Variables | Occupational exposure to COVID-19 |
Risk of COVID-19 virus infection |
||||
|---|---|---|---|---|---|---|
| AOR | 95%CI | P-value | AOR | 95%CI | P-value | |
| Age (in years) | ||||||
| <35 | Ref | |||||
| ≥35 | 1.13 | 0.51-2.50 | .764 | 0.57 | 0.18-1.80 | .338 |
| Gender | ||||||
| Female | Ref | |||||
| Male | 1.56 | 0.84-2.87 | .156 | 1.27 | 0.51-3.20 | .610 |
| Marital status | ||||||
| Single | Ref | |||||
| Married | 1.19 | 0.64-2.21 | .582 | 0.93 | 0.36-2.38 | .880 |
| Separated/Divorced/Widowed | 2.04 | 0.25-16.86 | .507 | 9.74 | 0.58-16.76 | .114 |
| Type of health professional | ||||||
| Assistant nurse | Ref | |||||
| Catering staff | 0.05 | 0.00-2.94 | .150 | – | – | |
| Cleaner | 1.19 | 0.02-6.63 | .930 | 1.58 | 0.01-3.68 | .861 |
| Laboratory personnel | 2.2 | 0.06-8.98 | .674 | – | – | |
| Medical doctor | 0.45 | 0.06-3.11 | .417 | – | – | |
| Midwife | 0.23 | 0.04-1.37 | .107 | 0.61 | 0.07-5.17 | .648 |
| Registered nurse | 0.39 | 0.09-1.68 | .206 | 0.09 | 0.01-0.60 | .013 |
| Pharmacist | 0.14 | 0.00-5.24 | .284 | 16.89 | 0.02-23.91 | .425 |
| Other health professionals | 0.68 | 0.02-2.98 | .836 | 19.26 | 1.13-34.51 | .045 |
| Staff category | ||||||
| Non-Clinical | Ref | |||||
| Clinical | 2.54 | 0.09-7.38 | .584 | 1.76 | 0.02-17.04 | .809 |
| Type of health facility | ||||||
| Cleaning services | Ref | |||||
| Emergency | 2.7 | 0.49-14.79 | .253 | 0.62 | 0.06-6.73 | .694 |
| Laboratory | – | – | – | – | ||
| Medical unit | 5.18 | 2.85-9.79 | .075 | 0.26 | 0.02-3.76 | .324 |
| Out patient | 1.66 | 0.27-3.18 | .581 | 2.71 | 0.23-31.47 | .426 |
| Pharmacy | 2.34 | 0.07-7.82 | .636 | 0.21 | 0.00-2.49 | .658 |
| Others | 0.86 | 0.18-4.25 | .858 | 0.03 | 0.00-0.56 | .018 |
| Highest level of qualification | ||||||
| Secondary level qualification | Ref | |||||
| Certificate | 1.43 | 0.52-3.92 | .489 | 0.32 | 0.08-1.39 | .130 |
| Diploma | 1.08 | 0.37-3.15 | .887 | 0.74 | 0.15-3.62 | .709 |
| Bachelor | 0.83 | 0.28-2.42 | .726 | 0.30 | 0.05-1.64 | .164 |
| Masters | 5.50 | 2.78-7.39 | .088 | 0.06 | 0.01-0.63 | .019 |
| Work experience (in years) | ||||||
| 1–10 | Ref | |||||
| >10 | 1.04 | 0.36-3.02 | .939 | 2.33 | 0.58-9.40 | .236 |
| Performed/present during any AGP | ||||||
| No | Ref | |||||
| Yes | 23.8 | 18.45-39.20 | .026 | 0.05 | 0.01-0.50 | .010 |
Significant P-value <.05, bold entries.
Factors Associated with Increased Risk of COVID-19 Virus Infection among the Exposed Healthcare Workers
Pearson’s chi-square of independence revealed a significant association between HCW marital status, type of health professional, staff category, type of health facility, highest level of qualification, performance or presence during any AGP and risk of COVID-19 virus infection (Table 2).
In a multivariate analysis, the odds of registered nurses were (AOR = 0.09; 95% CI: 0.01-0.60), indicating that the odds of high risk of COVID-19 virus infection were 98% less likely in registered nurses than in assistant nurses. The odds of high risk of COVID-19 virus infection for HCWs working in other units/departments (isolation center, catering services, etc.) was 97% lower than those working at cleaning services (AOR = 0.03; 95% CI: 0.00-0.56). Healthcare workers with a master’s degree had a 94% lower risk of COVID-19 virus infection than HCWs with secondary level education) qualification (AOR = 0.06; 95% CI: 0.01-0.63). Healthcare workers who performed or were present during any AGP were 95% times less likely to be at high risk of COVID-19 virus compared to HCWs who were not present or did not perform any AGP (AOR = 0.05; 95% CI: 0.01-0.50) (Table 3).
Discussion
Frontline HCWs are at increased risk of becoming infected with the COVID-19 virus since they provide direct care to COVID-19 patients.26 Several frontline HCWs in Ghana have been infected with SARS-COV-2. Little is known about how HCW exposure to the COVID-19 virus translates into risk of infection in healthcare settings in Ghana. Our findings revealed a high level of exposure to the COVID-19 virus. This is comparable to a similar study in an Ebola viral disease treatment center in Guinea, where they reported a high incidence of occupational exposure among HCWs.27 The translation of HCW exposure to COVID-19 patients into COVID-19 infection has been reported in previous studies.28,29 The high exposure to the COVID-19 virus in this study was expected since the study sites were designated treatment centers for COVID-19. In this study, healthcare workers reported more occupational exposure than community exposure. In the United States of America, most HCWs were exposed in a healthcare setting compared to the community.30 This further buttresses the point that health workers are at heightened risk for COVID-19 virus infection in healthcare settings. The risk of exposure of HCWs to COVID-19 virus can be mitigated by constant training on IPC protocols coupled with a regular supply of PPEs.
Healthcare workers who performed or were present during any AGP were 23.8 times more likely to be exposed compared to those respondents who did not perform/absent during any AGP. Aerosol-generating procedures are high-risk medical procedures and therefore put HCWs at increased risk of becoming infected with SARS-COV-2.31 The WHO recommends the use of PPEs such as gloves, N95 mask or respirator equivalent, face shield or goggles, disposal gown and waterproof apron during AGPs with laboratory-confirmed or suspected COVID-19 patients.24 Perhaps training HCWs on IPC measures coupled with the supply of appropriate PPEs, followed by compliance with IPC protocols, can protect exposed HCWs from COVID-19 virus infection.
Our analysis showed that 14.0% of the exposed HCWs were at high risk of COVID-19 virus infection. This is supported by a previous study in the US that found few HCPs to be at high risk of COVID-19 virus infection.28 Our findings could be an indication of the availability of PPEs in the COVID-19 treatment centers in Ghana. Healthcare workers with inadequate PPE while caring for COVID-19 patients are at higher risk of COVID-19 virus infection than those with adequate PPEs.32 Healthcare workers at high risk are safe when appropriate PPEs are used while caring for COVID-19 patients; however, a shortage of PPEs could put them at substantial risk of becoming infected with SARS-COV-2.33 The translation of high risk of COVID-19 virus infection into a positive COVID-19 test has been reported in the US.28 For HCWs at high risk of COVID-19 virus infection, WHO recommends suspension of all forms of healthcare interactions with patients, being/getting tested for COVID-19 and quarantined for 14 days. This should also be coupled with psychosocial support and compensation for the period of the quarantine.24
Majority of the HCWs in this study were at low risk of COVID-19 virus infection. This is similar to what has been reported in a previous study where a vast majority of HCWs were at low risk of Ebola viral infection in a treatment center.27 The availability of appropriate PPEs coupled with compliance with IPC measures by HCWs can translate into a low risk of COVID-19 virus infection. For exposed HCWs at low risk of COVID-19 virus infection, WHO recommends continued self-temperature monitoring and monitoring for respiratory symptoms daily for 14 days after the last exposure.24
Multivariate analysis showed registered nurses were less likely to be at high risk of COVID-19 virus infection compared to assistant nurses. Similarly, other healthcare professionals (ie, Pharmacy/dispensary technicians, physical and respiratory therapists, admission/reception clerks, accountants, administrative staff, IT managers and clinical engineers) were 19.3 times more likely to be at high risk for COVID-19 virus infection than assistant nurses. These foregoing findings may be an indication of gaps in the supply of PPEs to the various HCWs groups within the COVID-19 treatment centers. Perhaps, behavior change towards adherence to IPC measures could minimized the risk of COVID-19 infection among these group of HCWs in the treatment centers. There is the need for targeted technical training in addition to the supply of PPEs to these groups of HCWs. Our findings also revealed that HCWs who perform/present during any AGP were better protected from being at high risk of COVID-19 virus infection than those who did not perform/absent during any AGP. This may be an indication of prioritization of PPEs to HCWs who perform AGPs since they are high risk clinical procedures. Healthcare workers who performed AGP that is, tracheotomy are at greater risk of contracting SAR-COV-2.34
The study has 3 limitations. First, exposure to COVID-19 virus was self-reported and could be prone to recall bias. Second, we could not establish how exposure translates into COVID-19 infection, and lastly, the study was limited to treatment centers in the Greater Accra and Ashanti regions of Ghana.
Conclusion and Recommendation
Despite the high level of exposure to the COVID-19 virus among the frontline health workers, only 14.0% were at high risk of COVID-19 virus infection. Exposure to COVID-19 virus was more likely among HCWs who perform/present during any AGP. However, high risk of COVID-19 virus infection was less likely among HCWs who perform/present during any AGP, registered nurses and HCWs with a master’s degree as their highest qualification. Healthcare workers in the designated COVID-19 treatment centers are critical to Ghana’s fight against the COVID-19 pandemic. To protect these group of HCWs, treatment centers and HCWs should continue to adhere to WHO and national IPC protocols. Constant training of the HCWs on IPC protocols coupled with a regular supply of appropriate PPEs to all groups of HCWs in the treatment centers, monitoring and supportive supervision of HCWs exposed to the COVID-19 virus are also recommended. This is crucial in minimizing the risk of COVID-19 virus infection among HCWs in the designated COVID-19 treatment centers.
Acknowledgments
We are most grateful to managers of the COVID-19 treatment centers and the HCWs for their cooperation.
Footnotes
Author Contributions: Authors MEA, SKA, VD and PKA conceived and designed the study. Authors SDD, RR and KEA collected, analyzed and interpreted the data. Authors MEA, SKA, KEA and PKA wrote the draft manuscript. Authors SDD, AA and MEA did the literature review and discussed the findings of the study. All authors reviewed and approved the final manuscript.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: We confirm receipt of funding from Conrard Hilton Foundation through IRC-Ghana.
Ethical consideration: Ethical clearance for the study was granted by Ghana Health Service Ethics Review Committee. Written Informed consent was obtained from all respondents.
ORCID iDs: Mary Eyram Ashinyo  https://orcid.org/0000-0002-8493-9378
https://orcid.org/0000-0002-8493-9378
Stephen Dajaan Dubik  https://orcid.org/0000-0001-9833-2676
https://orcid.org/0000-0001-9833-2676
Kingsley Ebenezer Amegah  https://orcid.org/0000-0002-5251-1166
https://orcid.org/0000-0002-5251-1166
Anthony Ashinyo  https://orcid.org/0000-0002-1105-3795
https://orcid.org/0000-0002-1105-3795
Rita Larsen-Reindorf  https://orcid.org/0000-0003-3481-0266
https://orcid.org/0000-0003-3481-0266
References
- 1. WHO. Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV). 2020. https://www.who.int/news-room/detail/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov)
- 2. Alanagreh LA, Alzoughool F, Atoum M. The human coronavirus disease COVID-19: its origin, characteristics, and insights into potential drugs and its mechanisms. Pathogens. 2020;9:331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Maliszewska M, Mattoo A, Van Der Mensbrugghe D. The potential impact of COVID-19 on GDP and trade: a preliminary assessment. 2020. http://documents1.worldbank.org/curated/en/295991586526445673/pdf/The-Potential-Impact-of-COVID-19-on-GDP-and-Trade-A-Preliminary-Assessment.pdf
- 4. Burdorf A, Porru F, Rugulies R. The COVID-19 (Coronavirus) pandemic: consequences for occupational health. Scand J Work Environ Health. 2020;46:229-230. [DOI] [PubMed] [Google Scholar]
- 5. World Health Organization. Coronavirus disease 2019 (COVID-19) dashboard. 2020. https://covid19.who.int/?gclid=CjwKCAjw8MD7BRArEiwAGZsrBWtn_x-RAgmUJvX0azyudWSbILG49RKSwQKQZmRnNuSeqaXYsriOJxoCw9UQAvD_BwE [PubMed]
- 6. Ministry of Health. Ghana Confirm Two Cases of COVID-19 (PDF). Ghana Health Service; 2020. [Google Scholar]
- 7. Ghana health service COVID-19 update. 2020. https://ghanahealthservice.org/covid19/
- 8. Coronaviridae Study Group of the International Committee on Taxonomy of Viruses. The species Severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nat Microbiol. 2020;5:536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382: 1708-1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Guo YR, Cao QD, Hong ZS, et al. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak–an update on the status. Mil Med Res. 2020;7:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. World Health Organisation. Report of the WHO-China joint mission on coronavirus disease 2019 (COVID-19). 2020. https://www.who.int/publications-detail/report-of-the-who-china-joint-mission-on-coronavirus-disease-2019-(covid-19)
- 12. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497-506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Wen Y, Wei L, Li Y, et al. Epidemiological and clinical characteristics of COVID-19 in Shenzhen, the largest migrant city of China. medRxiv. 2020. https://www.medrxiv.org/content/10.1101/2020.03.22.20035246v1.full.pdf
- 14. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323:1239-1242. [DOI] [PubMed] [Google Scholar]
- 15. Cascella M, Rajnik M, Cuomo A, Dulebohn SC, Di Napoli R. Features, Evaluation and Treatment Coronavirus (COVID-19). Statpearls [internet]. StatPearls Publishing; 2020. [PubMed] [Google Scholar]
- 16. Chang D, Xu H, Rebaza A, Sharma L, Cruz CS. Protecting healthcare workers from subclinical coronavirus infection. Lancet Respir Med. 2020;8:e13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. World Health Organization. Infection prevention and control during health care when novel coronavirus (nCoV) infection is suspected: interim guidance. January 25, 2020. https://www.who.int/publications/i/item/10665-331495
- 18. Sahiledengle B, Gebresilassie A, Getahun T, Hiko D. Infection prevention practices and associated factors among healthcare workers in governmental healthcare facilities in Addis Ababa. Ethiop J Health Sci. 2018;28:177-186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Otieno-Ayayo ZN, Gichuhi AW, Kamau SM, Nyangena E. Health care workers adherence to infection prevention practices and control measures: a case of a level four district hospital in Kenya. http://repository.rongovarsity.ac.ke/handle/123456789/2217
- 20. Houghton C, Meskell P, Delaney H, et al. Barriers and facilitators to healthcare workers’ adherence with infection prevention and control (IPC) guidelines for respiratory infectious diseases: a rapid qualitative evidence synthesis. Cochrane Database Syst Rev. 2020;4:CD013582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. World Health Organization. Protocol for Assessment of Potential Risk Factors for Coronavirus Disease 2019 (COVID-19) among Health Workers in a Health Care Setting. March 23, 2020. World Health Organization; 2020. [Google Scholar]
- 22. International Council of Nurses. 90,000 healthcare workers infected with COVID-19. 2020. https://www.aa.com.tr/en/europe/90-000-healthcare-workers-infected-with-covid-19-icn/1831765#
- 23. Ghana Health Service. Over 2,000 Ghanaian health workers contracted Covid-19. 2020. https://en.as.com/en/2020/07/17/latest_news/1595016557_041674.html
- 24. World Health Organization. Risk Assessment and Management of Exposure of Health Care Workers in the Context of COVID-19: Interim Guidance. March 19, 2020. World Health Organization; 2020. [Google Scholar]
- 25. Cochran WG. Sampling Techniques. 2nd ed. John Wiley & Sons; 1963. [Google Scholar]
- 26. Nguyen LH, Drew DA, Graham MS, et al. Risk of COVID-19 among frontline healthcare workers and the general community: a prospective cohort study. Lancet Public Health. 2020;5:e475-e483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Savini H, Janvier F, Karkowski L, et al. Occupational exposures to Ebola virus in Ebola treatment center, Conakry, Guinea. Emerg Infect Dis. 2017;23:1380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Heinzerling A, Stuckey PM, Scheuer T, et al. Transmission of COVID-19 to health care personnel during exposures to a hospitalized patient—Solano County, California, February 2020. Morb Mortal Wkly Rep. 2020;69:472-476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Chen Y, Tong X, Wang J, et al. High SARS-CoV-2 antibody prevalence among healthcare workers exposed to COVID-19 patients. J Infect. 2020;81. doi: 10.1016/j.jinf.2020.05.067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. COVID TC. Characteristics of health care personnel with COVID-19-United States, February 12-April 9, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:477-481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Tran K, Cimon K, Severn M, Pessoa-Silva CL, Conly J. Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: a systematic review. PLoS One. 2012;7:e35797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. CIDRAP. Health workers, especially minorities, at high risk for COVID, even with PPE. https://www.cidrap.umn.edu/news-perspective/2020/08/health-workers-especially-minorities-high-risk-covid-even-ppe
- 33. Jain U. Risk of COVID-19 due to shortage of personal protective equipment. Cureus. 2020;12: e8837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Mick P, Murphy R. Aerosol-generating otolaryngology procedures and the need for enhanced PPE during the COVID-19 pandemic: a literature review. J Otolaryngol Head Neck Surg. 2020;49:1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]