Abstract
Aim
The objective of the present study was to develop a tool for mothers to assess their children’s skin condition with the ultimate goal of its wider use in general health checkups for infants and toddlers.
Methods
This was a single-institution, cross-sectional study in Japan, targeting parents of 200 infants and toddlers who visited a dermatology clinic between December 2018 and March 2019. The parents completed a self-administered survey of the mother’s perception of her child’s dermatological symptoms, itchiness, and sleep status, and a quality-oflife assessment, using a nine-question version of the Quality of life in Primary Caregivers of children with Atopic Dermatitis questionnaire (QP9). The attending physician was asked to complete a form about the child’s dermatological condition and the treatment prescribed. The severity of the dermatological condition noted by the physician was compared with the combined response to the 3 perception items (dermatological condition, itchiness, and sleep) reported by the parents, in order to identify the optimal cutoff score.
Results
Of 200 parent questionnaires distributed, 198 (99% response rate) were returned and analyzed, along with the responses from 198 physician records (100% response rate). The optimal cutoff score was 2/3 for the total score (range 0-6) for 2 items, itchiness and sleep status (sensitivity 73%, specificity 64%). There was a significant difference in QP9 scores between the 2 groups categorized by the cutoff score
Conclusions
A pediatric dermatological screening tool based on 2 symptoms reported by the parents of children with atopic dermatitis was developed, and its precision and criterion-related validity were confirmed. This simple tool could help parents become better aware of their children’s skin condition and allow healthcare workers to provide adequate skin care advice. This practical tool could be widely applicable in primary child care and public health service settings.
Keywords: Pediatric dermatitis, community health, infant, children, quality of life
Introduction
The prevalence of atopic dermatitis in children in Japan is approximately 10%.1 Reflecting the prevalence, the frequency of consultations for pediatric skin conditions during child health checkups is high in Japan.2,3 Skin diseases are characterized by symptoms in locations visible to others, and many disorders are accompanied by itchiness, impacting the quality of life (QOL) of the patients and their families.4-6 In addition, an analysis of pediatric consultations in general practice showed that skin problems were the second most common complaint, after respiratory problems.7
Among various quality of life (QOL) indicators for dermatology patients,8,9 we previously selected and developed a shortened Japanese version (6 items) of the Dermatology Life Quality Index (DLQI)10,11 and examined its validity and reliability for pediatric atopic dermatitis.12 However, very few epidemiological observations focus on general skin diseases or the parents’ perception of their children’s dermatological symptoms. Furthermore, the accuracy of parental skin assessment has not been verified. The present study compared the diagnosis of the medical practitioner with the parents’ perception of their children’s dermatological symptoms, to develop a skin assessment tool for parents of infants and toddlers. The background factors associated with the score of the newly developed tool were also identified. To further test the association with the quality of life assessed by mothers, we used the shortened (9-item) version QP9 (QPCAD shortened to 9 questions)13 of the Japanese 19-item Quality of Life in Primary Caregivers of Children with Atopic Dermatitis (QPCAD).14
In Japan, child health checkups are often conducted in groups at health centers, generally at 4, 18, and 36 months of age. Public health nurses are the main service providers, and they provide parenting consultations based on collected self-administered forms and examination results. We believe that our newly developed skin assessment tool, which can be easily completed by parents, would increase parental awareness about their children’s skin condition and facilitate their communication with healthcare providers. The tool can thus help nurses identify children in need of skin care and refer a child for medical care when needed.
Methods and Materials
The present study was a single-institution cross-sectional study in Japan targeting parents of infants and toddlers (first-time patients, age <7 years) who underwent a physician’s medical examination at the participating research facility between December 2018 and March 2019. Of the 31 294 patients at the facility in 2019, 1392 (4.4%) were infants and toddlers <7 years of age. Parents of all patients who visited a dermatology clinic in a district of Tokyo, Japan, were recruited. Only the first visit during the study period was recorded in our database. The sample size was based on a previous similar study13 involving 148 patients showing a correlation between QP913 and symptoms.
The questionnaire survey for parents was an anonymous, self-administered survey. The physician involved in the research explained the study and distributed the questionnaires and consent forms, which were then collected at the clinic reception area. Subsequently, the medical information sheet was completed by the physician about the children whose parents had given consent. The sheets for the parents and the doctor had an identical number, so data could be matched. The gold standard for medical conditions was the physician’s diagnosis, as opposed to the mother’s assessment based on her child’s symptoms. Because the diagnosis was made by a single dermatologist, there was no risk of inter-rater variation.
The mother responded to questions about her age, health status, and occupation, as well as the father’s identical information. In formation on mental health15 was obtained directly only from mothers. We previously developed and validated a self-check list for atopic dermatitis, which was a six-item version of the 10-item DLQI questionnaire.12 This was partially modified and used as the questions for the children’s dermatological symptoms. Specifically, the atopic dermatitis self-check questions were revised into general dermatitis questions addressed to parents. Since this was targeting infants and toddlers, items related to the “effects on work/school and problems of everyday life other than work/school” were excluded. Questions related to the skin condition of the children in the previous 1 week were asked, and responses were given on a four-point scale. The question items were:
What was the condition of the skin?
Did it seem that they were experiencing itchiness or pain (burning, tingling, or throbbing sensations) or were there any scratch marks?
-
Did they wake up or did they have difficulty falling asleep due to itchiness?
The skin condition assessment sub-scale (B with 3 items) of a commonly used indicator for caregivers of children with atopic dermatitis (QP9)13 was used for the criteria-related validation.
As for the physician’s form, the atopic dermatitis questionnaire form from the Clinical Practice Guidelines for the Management of Atopic Dermatitis 2018 was used to assess disease severity (mild, moderate, or severe).1 In addition, items for the diagnosis of the medical condition (infant and toddler eczema, eczema, atopic dermatitis, others), level of understanding of parents, course of treatment, and treatment plans were asked along with the child’s basic information (age at the time of consultation and onset of dermatological symptoms).
When developing a questionnaire, items from commonly used child health checkup forms in Japan were collected. In addition, healthcare providers who actually provide health guidance and parenting support were consulted. We first referred to the content of parenting consultation at the time of child health checkups among infants and toddlers and previous studies. Comments on the draft questionnaire were then obtained from 2 public health nurses involved in the child health checkups at a public health center, 2 nurses with hospital experience in dermatology, and a researcher of health literacy issues. Subsequently, a pre-test for confirming survey acceptability was administered to 2 parents with infants and toddlers to see if the parents could complete the survey easily.
In the data analysis, the severity of the dermatological condition (moderate/severe) noted by the physician was considered the gold standard, and it was compared with the combined response to the 3 perception items (dermatological condition, itchiness, and sleep) reported by the parents of the children with dermatological symptoms. Since each item was scored between 0 and 3 points, the score range for combining 2 items was between 0 and 6 points. When combining 3 items, the score range was between 0 and 9 points. To determine the optimal cutoff score to develop the scale, the sensitivity and specificity at the cutoff scores for the combination of each item were calculated, receiver operating characteristic (ROC) curves were plotted, and the combinations were compared. Using the determined cutoff score of a combination, the chi-squared test, Fisher’s exact probability test, or the t-test was performed to examine background factors and QP9.13 The analysis was conducted using the statistical analysis software IBM Statistical Package for the Social Science (SPSS) version 26. The significance level was set at 5%.
The present study was conducted after receiving approval from the ethics committee of Fukushima Medical University (No. 30189).
Results
A total of 200 questionnaire surveys were handed out to parents, and responses from 198 parents (99% response rate) and 198 physicians (100%) were collected and analyzed. The responses from parents were all from mothers.
As for the patients’ characteristics, 51.0% were female, 6.2% were low-birthweight infants, 5.6% were premature births, and 58.2% were first-born children (Table 1). The median age of the mothers was 36.0 (22, 47) years, 98.5% reported good health status, approximately 20% had depressive tendencies, and 60.5% were employed.
Table 1.
Characteristics of children and parents and medical information.
| N (%)† or Median (min, max) |
|||||||
|---|---|---|---|---|---|---|---|
| Total (n = 198) | Itchiness + sleep score (0 to 2 points) (n = 105) | Itchiness + sleep score (3 to 6 points) (n = 93) | P value* | ||||
| Child | |||||||
| Age, months* | 32.5 | (2, 82) | 30.0 | (2, 82) | 34.0 | (2, 80) | .76 |
| Sex | .91 | ||||||
| Girls | 101 | (51.0) | 54 | (51.4) | 47 | (50.5) | |
| Boys | 97 | (49.0) | 51 | (48.6) | 46 | (49.5) | |
| Birth weight | .47 | ||||||
| <2500 g | 12 | (6.2) | 5 | (5.0) | 7 | (7.7) | |
| ≥2500 g | 182 | (93.8) | 97 | (95.0) | 85 | (92.3) | |
| Gestational weeks | .56 | ||||||
| <37 | 10 | (5.6) | 4 | (4.6) | 6 | (7.7) | |
| ≥37 | 167 | (94.4) | 83 | (95.4) | 73 | (92.3) | |
| Birth order | .45 | ||||||
| First child | 114 | (58.2) | 63 | (60.6) | 51 | (55.4) | |
| Second child and beyond | 82 | (41.8) | 41 | (39.4) | 41 | (44.6) | |
| Mother | |||||||
| Age, years* | 36.0 | (22, 47) | 36.0 | (22, 47) | 36.0 | (24, 47) | .33 |
| Health status | .64 | ||||||
| Good | 194 | (98.5) | 103 | (98.1) | 91 | (98.9) | |
| Poor | 3 | (1.5) | 2 | (1.9) | 1 | (1.1) | |
| Depression tendency‡ | .59 | ||||||
| Present | 38 | (19.2) | 22 | (21.0) | 16 | (17.2) | |
| Absent | 160 | (80.8) | 83 | (79.0) | 77 | (82.8) | |
| Occupation | .34 | ||||||
| Employed | 118 | (60.5) | 65 | (63.7) | 53 | (57.0) | |
| Not employed | 77 | (39.5) | 37 | (36.3) | 40 | (43.0) | |
| Father | |||||||
| Age, years* | 38.0 | (24, 60) | 37.5 | (26, 60) | 39.0 | (24, 60) | .24 |
| Health status | .62 | ||||||
| Good | 191 | (98.5) | 100 | (98.0) | 91 | (98.9) | |
| Poor | 3 | (1.5) | 2 | (2.0) | 1 | (1.1) | |
| Occupation | - | ||||||
| Employed | 194 | (100.0) | 101 | (100.0) | 93 | (100.0) | |
| Not employed | 0 | (0.0) | 0 | (0.0) | 0 | (0.0) | |
| Family configuration | .92 | ||||||
| Extended family | 16 | (13.0) | 8 | (7.6) | 8 | (12.7) | |
| Nuclear family | 107 | (87.0) | 52 | (49.5) | 55 | (87.3) | |
| Medical information* | |||||||
| Age in months at disease onset | 12.0 | (1,66) | 12.0 | (1,66) | 12.0 | (1,65) | .86 |
| Duration of the disease (months) | 13.0 | (0,72) | 12.0 | (0,72) | 13.0 | (0,68) | .37 |
| Diagnosis | .74 | ||||||
| Eczema (seborrheic and infant/toddler) | 58 | (29.3) | 32 | (30.5) | 26 | (28.0) | |
| Atopic dermatitis | 135 | (68.2) | 71 | (67.6) | 64 | (68.8) | |
| Undiagnosed | 5 | (2.5) | 2 | (1.9) | 3 | (3.2) | |
| History of treatment | .45 | ||||||
| With no history | 26 | (13.1) | 13 | (12.4) | 13 | (14.0) | |
| With history | 172 | (86.9) | 92 | (87.6) | 80 | (86.0) | |
| Treatment plan§ | |||||||
| Topical steroid ointment | 176 | (88.9) | 86 | (81.9) | 90 | (96.8) | <.01 |
| Topical tacrolimus ointment | 1 | (0.5) | 0 | (0.0) | 1 | (1.1) | .29 |
| Moisturizing agent | 162 | (81.8) | 85 | (81.0) | 77 | (82.8) | .74 |
| Oral antihistamine medication | 27 | (13.6) | 8 | (7.6) | 19 | (20.4) | <.01 |
| Others | 10 | (5.1) | 5 | (4.8) | 5 | (5.4) | .84 |
| Understanding of parents | .33 | ||||||
| Good | 151 | (76.6) | 84 | (80.8) | 67 | (72.0) | |
| Normal | 43 | (21.8) | 19 | (18.3) | 24 | (25.8) | |
| Poor | 3 | (1.5) | 1 | (0.9) | 2 | (2.2) | |
Percentage using valid responses from the questionnaire survey as a parameter. For some items, the percentages do not add up to 100% owing to data unavailability.
Chi-squared, Fisher’s exact test, or Mann-Whitney U test.
Two-question screening for depression.
Multiple choice.
The median age in months at the time of onset was 12.0 (1, 66) months and the median duration of the disease was 13.0 (0, 72) months (Table 1). As for the diagnoses, 68.2% were atopic dermatitis, and 29.3% were eczema (seborrheic eczema and infant and toddler eczema). For the degree of severity, 30% were moderate and severe cases. Whereas 13.1% had no history of treatment, treatment plans consisted of external steroid ointments (88.9%), moisturizing agents (81.8%), and oral antihistamine medication (13.6%).
Regarding parents’ perceptions, 46.5% responded that the dermatological conditions were “not very good/not good,” and 72.7% responded that their children “sometimes/always” had itchiness (Table 2). As for sleep, 26.3% said that their children were not getting good sleep, and that they were waking up “sometimes/always” due to itchiness. The parents’ perception of the dermatological condition was “not very good/not good” in 38.4% of cases whose severity diagnosed by the physician was mild and in 65.0% of moderate/severe cases. As for the perception of having itchiness “sometimes/always,” the proportion was 64.5% in physician-diagnosed mild cases and in 91.7% in moderate/severe cases. Likewise, the perception that they were not getting good sleep and that they were waking up was “sometimes/always” in 19.5% of mild cases and in 41.7% of moderate/severe cases.
Table 2.
Mother’s Perception of her Child’s Dermatological Symptoms and the Physician’s Diagnosis of Severity (Based on Observations of the Previous Week).
| Mother’s perception of her child’s dermatological symptoms | N (%) | |||||||
|---|---|---|---|---|---|---|---|---|
| Severity diagnosed by the physician | ||||||||
| n = 198 | Mild | Moderate | Severe | |||||
| n = 138 (69.7) | n = 57 (28.8) | n = 3 (1.5) | ||||||
| Skin condition | ||||||||
| 0. Good | 12 | (6.1) | 10 | (7.2) | 2 | (3.5) | 0 | (0.0) |
| 1. Fairly good | 94 | (47.5) | 75 | (54.3) | 19 | (33.3) | 0 | (0.0) |
| 2. Not very good | 81 | (40.9) | 50 | (36.2) | 31 | (54.4) | 0 | (0.0) |
| 3. Not good | 11 | (5.6) | 3 | (2.2) | 5 | (8.8) | 3 | (100.0) |
| Itchiness | ||||||||
| 0. None | 29 | (14.6) | 27 | (19.6) | 2 | (3.5) | 0 | (0.0) |
| 1. Not much | 25 | (12.9) | 22 | (15.9) | 3 | (5.3) | 0 | (0.0) |
| 2. Sometimes | 89 | (44.9) | 64 | (46.4) | 25 | (43.9) | 0 | (0.0) |
| 3. Always | 55 | (27.8) | 25 | (18.1) | 27 | (47.4) | 3 | (100.0) |
| Waking up or difficulty falling asleep due to itchiness | ||||||||
| 0. None | 108 | (54.5) | 87 | (63.0) | 21 | (36.8) | 0 | (0.0) |
| 1. Not much | 38 | (19.2) | 24 | (17.4) | 13 | (22.8) | 1 | (33.3) |
| 2. Sometimes | 40 | (20.2) | 22 | (15.9) | 16 | (28.1) | 2 | (66.7) |
| 3. Always | 12 | (6.1) | 5 | (3.6) | 7 | (12.3) | 0 | (0.0) |
The ROC comparing the total score of the various combinations of parents’ perception of their children’s dermatological symptoms (dermatological condition, itchiness, and sleep) showed that the area under the curve (AUC) was highest (0.736) for the total score of all 3 items, followed by the “itchiness + sleep” score at 0.731 (Figures 1 and 2). When the total of the 3 items (dermatological condition, itchiness, and sleep) was dichotomized by the cut-off value of 4/5 (0 to 4 and 5 to 9 points), the sensitivity was 65%, and the specificity was 71%. Although the AUC was slightly lower, when the total score of 2 items (itchiness and sleep) was dichotomized with the cut-off value of 2/3 (0 to 2 and 3 to 6 points), the sensitivity was 73%, and the specificity was 64%. In addition, the positive predictive value for this cut-off value in the survey participants was 47.3%, and the negative predictive value was 84.7%. When it was dichotomized into another 2 categories (0 to 3 and 4 to 6 points), the sensitivity was 55%, and the specificity was 78%. The point closest to the left upper corner of the ROC diagram and with the higher sensitivity was selected as the best cutoff value for this screening tool.
Figure 1.
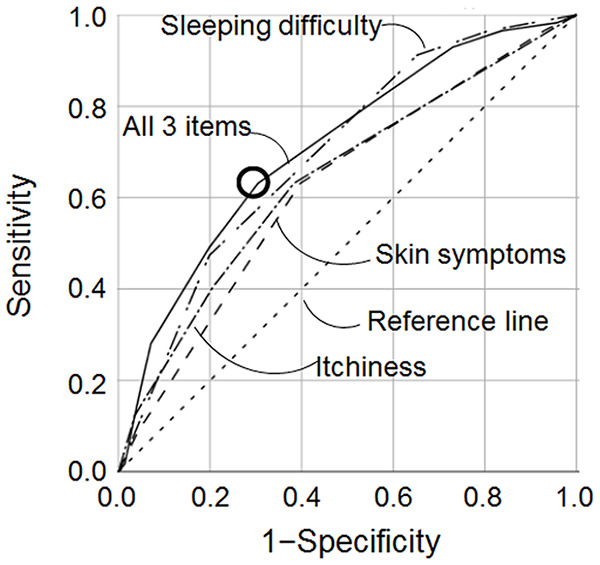
Receiver operating characteristic (ROC) curve of itchiness, skin symptoms, sleeping difficulty, and all 3 for predicting physician diagnosis.
Figure 2.
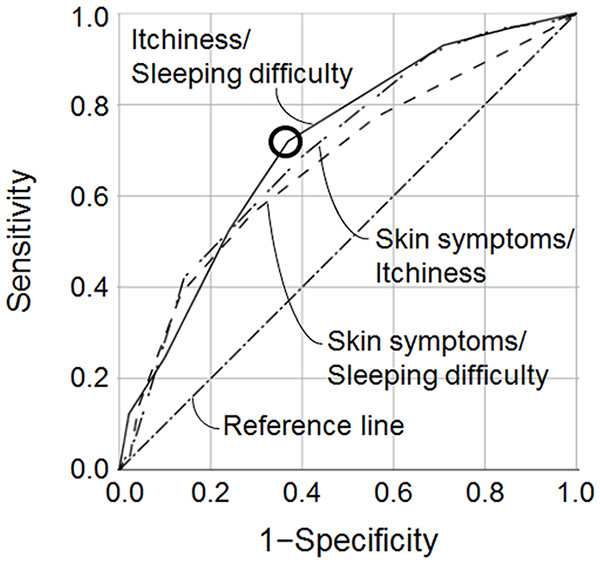
ROC curve of combinations of itchiness/sleeping difficulty, skin symptoms/sleeping difficulty, and skin symptoms/itchiness for predicting physician diagnosis. Sensitivity is 73% and specificity is 64% for the cut-off value of 2/3 of the itchiness/sleeping difficulty score.
The same analysis limited to atopic dermatitis was conducted as a sub-analysis. When the total score for itchiness and sleep was divided using a cutoff score of 0 to 2 and 3 to 6 points, the sensitivity was 70%, and the specificity was 64%.
Proportion of cases with a treatment plan including external steroid ointments was significantly higher for the 3 to 6 points group (96.8%) compared to the 0 to 2 points group (81.9%). That of oral antihistamine medications was also higher for the 3 to 6 points group (20.4%) compared to the 0 to 2 points group (7.6%). For the subscale B scores of the QP9,13 the score of the 3 to 6 points group (5.12, SD = 2.77) was significantly higher than that of the 0 to 2 points group (3.21, SD = 2.92). Of note, a lower QP9 score indicates a better condition.
Discussion
The present study analyzed the difference between the parents’ (mothers’) perception of their children’s dermatological symptoms of non-specific dermatological diseases and the physician’s diagnosis. While only about half of the parents responded that their child’s dermatological condition was “not very good/not good,” approximately 70% said that itchiness in particular was “sometimes/always” present, causing sleep disturbance in about 30% of the cases. Mothers sought medical consultation focusing on symptoms, and the physician’s diagnosis of severity was mild/severe in approximately 70% of the cases.
As for deciding the cutoff value of the mothers’ assessment, having a higher sensitivity is better suited as a screening tool. Therefore, the optimal cutoff score for the present study was when the total score for 2 items, itchiness and sleep, was categorized as 0 to 2 points and as 3 to 6 points, giving a sensitivity of 73% and a specificity of 64% for predicting physician diagnosis of moderate/severe. It was assumed that it was easier for parents (mothers) to respond to symptoms rather than a pathological diagnosis. To confirm the criterion-related validity, there was a significant difference in the QP913 score between the 2 groups divided by the cutoff value. The accuracy of such symptom-based diagnosis is often reported, especially in reproductive tract infection. According to a recent pooled analysis by the World Health Organization (WHO), the sensitivity and specificity for cervical infections were 27% and 85%, respectively, and, similarly for vaginal infections, they were 60% and 64%, respectively.16 The similarities in both the skin diseases of infants and toddlers addressed in the present study and the reproductive tract infections of women are that both diseases are not life-threatening and do not require immediate treatment, their chief complaint is itchiness, and the perceptions of the symptoms come mainly from women. Therefore, the sensitivity and specificity obtained in the present study from only 2 items were deemed to have acceptable accuracy. A practical and easy to fill-in tool for parents to assess children’s skin condition would be widely applicable in primary child care and public health service settings.
When the parents’ perception of their children’s skin condition was investigated among the subjects of the present study, the parents of 21 children said that their child’s skin condition was “good/fairly good,” whereas the severity reported by the physicians was moderate in 21 cases (zero severe cases). This finding indicated that the parents of children with dermatological symptoms had a low perception of skin symptoms compared to their physician. A prolonged disease duration, even under moderate conditions, may give the perception that the symptoms are improving, and that could be the reason why there was a difference with the one-time observation by the physician. In patients that suffer chronic illnesses, it has been reported that a response shift in QOL occurs. The response shift is a better outcome over time not because the patient is doing better, but because the patients have now adapted to new life circumstances.17
The present study had the following 3 main limitations. First, the study was limited to the winter season. Diseases like miliaria and impetigo contagiosa that are frequent in summer were not included. However, their symptoms are similar to those of eczema and dermatitis, and our tool would be applicable for these summer-specific diseases. Second, the parents that responded to the survey were all mothers. Whereas about 60% of the mothers were employed, 100% of the fathers were working, and the reality was that the mothers attended the medical consultations. In Japan, mothers are often the main care givers, so that their perceptions of children’s symptoms become a valuable screening tool.18 However, if another member of the family plays a key role in parenting, then the decisions made by that family member need to be emphasized. Third, the present study was a survey targeting patients who underwent medical consultations at a single institution. Validity was established in a limited range of subjects.
The developed tool can thus help nurses identify children in need of skin care, and we plan to determine the reliability and validity of this tool for use in general health checkups for infants and toddlers.
Footnotes
Authors’ Note: The work was previously presented in part as a digital poster in Japanese at the 119th Annual Meeting of the Japanese Dermatological Association in 2020.
Author Contributions: All authors were involved in the data interpretation, manuscript writing and revision, and approved the final version.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was funded by a 2020 JSPS KAKENHI Grant (C20K02652).
ORCID iD: Hiroko Sato  https://orcid.org/0000-0002-8061-869X
https://orcid.org/0000-0002-8061-869X
References
- 1. Katoh N, Ohya Y, Ikeda M, et al. Clinical practice guidelines for the management of atopic dermatitis 2018. J Dermatol. 2019;46:1053-1101. [DOI] [PubMed] [Google Scholar]
- 2. Murai C, Hayashi C, Yokoyama Y. Consultations with mothers and background factors related to seeking advice about child rearing: analysis of data from health check-ups 3 months after delivery. Jpn J Public Health Nurse. 2014;3:1-10. [Google Scholar]
- 3. Kaminiwa J, Fujiu K. The anxiety on childcare of mothers with infants –Ⅰ. A longitudinal study from 1 month after birth to 3 years of age –. Jpn Soc Child Health. 2003;62:504-510. (In Japanese) [Google Scholar]
- 4. Dodington SR, Basra MK, Finlay AY, Salek MS. The Dermatitis Family Impact questionnaire: a review of its measurement properties and clinical application. Br J Dermatol. 2013;169:31-46. [DOI] [PubMed] [Google Scholar]
- 5. Takahashi N, Suzukamo Y, Nakamura M, et al. Japanese version of the Dermatology Life Quality Index: validity and reliability in patients with acne. Health Qual Life Outcomes. 2006;4:46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Yang EJ, Beck KM, Sekhon S, Bhutani T, Koo J. The impact of pediatric atopic dermatitis on families: a review. Pediatr Dermatol. 2019;36:66-71. [DOI] [PubMed] [Google Scholar]
- 7. O’Doherty J, Hannigan A, Hickey L, et al. An analysis of childhood consultation in general practice: a multi-practice study. Ir J Med Sci. 2019;188:1239-1244. [DOI] [PubMed] [Google Scholar]
- 8. Fukuhara S, Suzukamo Y. DLQI Japanese version and Skindex-29 Japanese version. Allergy Pract. 2007;358:23-27. (In Japanese) [Google Scholar]
- 9. Higaki Y, Kawamoto K, Kamo T, Horikawa N, Kawashima M, Chren MM. The Japanese version of Skindex-16: a brief quality-of life measure for patients with skin diseases. J Dermatol. 2002;29:693-698. [DOI] [PubMed] [Google Scholar]
- 10. Ooya Y, Sasaki R, Matumoto M, et al. Development of the Japanese version of the Quality of Life Index for Childhood Atopic Dermatitis (CDLQI). Jpn J Allergol. 2002;51:265. (In Japanese) [Google Scholar]
- 11. Lewis-Jones MS, Finlay AY. The Children’s Dermatology Life Quality Index (CDLQI): initial validation and practical use. Br J Dermatol. 1995;132:942-949. [DOI] [PubMed] [Google Scholar]
- 12. Nakagawa H, Etou T, Asahina A, Ishizi T, Sato H, Saeki H. Research on self-management of allergic diseases, support system for improvement of living environment, distance education system, and patient registration and long-term observation system using ubiquitous-internet: research on assessment of patients with atopic dermatitis using a mobile phone. Health Labour Sciences Research Grant report 2010. [Google Scholar]
- 13. Katunuma T, Tan A, Ooya Y. Development and clinical evaluation of a short version of the Quality of Life Survey Table (QP9) for caregivers of pediatric atopic dermatitis patients. Jpn J Allergol. 2013;62:33-46. (In Japanese) [Google Scholar]
- 14. Kondo-Endo K, Ohashi Y, Nakagawa H, et al. Development and validation of a questionnaire measuring quality of life in primary caregivers of children with atopic dermatitis (QPCAD). Br J Dermatol. 2009;161:617-625. [DOI] [PubMed] [Google Scholar]
- 15. Mishina H, Hayashino Y, Fukuhara S. Test performance of two-question screening for postpartum depressive symptoms. Pediatr Int. 2009;51:48-53. [DOI] [PubMed] [Google Scholar]
- 16. Zemouri C, Wi TE, Kiarie J, et al. The performance of the vaginal discharge syndromic management in treating vaginal and cervical infection: a systematic review and meta-analysis. PLoS One. 2016;11:e0163365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Rapkin BD, Schwartz CE. Advancing quality-of-life research by deepening our understanding of response shift: a unifying theory of appraisal. Qual Life Res. 2019;28:2623-2630. [DOI] [PubMed] [Google Scholar]
- 18. Honda Y, Fujiwara T, Kawachi I. Higher child-raising costs due to maternal social isolation: large population-based study in Japan. Soc Sci Med. 2019;233:71-77. [DOI] [PubMed] [Google Scholar]


