Significance
Mutagenic translesion synthesis (TLS) allows cells to increase their survival after DNA damage by bypassing lesions that normally block DNA replication but at the cost of introducing mutations. Interfering with this TLS pathway genetically or with the small molecule inhibitor JH-RE-06 has been shown to improve cisplatin chemotherapy by suppressing tumor growth and enhancing survival in mouse xenograft tumor models. Deleting Rev7, which is a component of both the TLS machinery and a complex that regulates the choice of double-strand break repair pathways, strikingly potentiates cisplatin chemotherapy in a lung cancer model. Moreover, while cisplatin monotherapy resulted in tumor cell apoptosis, Rev7 deletion promoted a cisplatin-induced senescence phenotype, suggesting that targeting Rev7 is an attractive strategy to improve chemotherapy.
Keywords: Rev7, translesion synthesis, chemotherapy, cisplatin, lung cancer
Abstract
Cisplatin is a standard of care for lung cancer, yet platinum therapy rarely results in substantial tumor regression or a dramatic extension in patient survival. Here, we examined whether targeting Rev7 (also referred to as Mad2B, Mad2L2, and FANCV), a component of the translesion synthesis (TLS) machinery, could potentiate the action of cisplatin in non-small cell lung cancer (NSCLC) treatment. Rev7 loss led to an enhanced tumor cell sensitivity to cisplatin and dramatically improved chemotherapeutic response in a highly drug-resistant mouse model of NSCLC. While cisplatin monotherapy resulted in tumor cell apoptosis, Rev7 deletion promoted a cisplatin-induced senescence phenotype. Moreover, Rev7 deficiency promoted greater cisplatin sensitivity than that previously shown following targeting of other Pol ζ-proteins, suggesting that Pol ζ-dependent and -independent roles of Rev7 are relevant to cisplatin response. Thus, targeting Rev7 may represent a unique strategy for altering and enhancing chemotherapeutic response.
Chemotherapeutics that damage DNA, such as cisplatin, have been the mainstay of cancer treatment for decades (1). However, all too often the efficacy of such DNA-damaging chemotherapy is severely limited by intrinsic and acquired drug resistance, as well as by the induction of secondary malignancies. Thus, improvements to existing treatment regimens are critically needed. Agents like cisplatin introduce monoadduct, intrastrand cross-link, and interstrand cross-link DNA lesions that block progression of the replication fork (2). Persistent replication arrest triggers cell cycle arrest and can lead to DNA damage-mediated cell death (2). Cells employ various DNA repair systems to remove lesions from DNA but are also able to tolerate DNA damage by utilizing specialized DNA polymerases, like Pol ζ and Rev1, that bypass the lesion site in a process known as translesion synthesis (TLS) (2, 3). Pol ζ and Rev1 are also required for the repair of interstrand cross-links (4).
A promising strategy for improving chemotherapy is to inhibit Rev1/Pol ζ-dependent mutagenic TLS. For example, knocking down the Pol ζ-catalytic component Rev3 strikingly improved cisplatin efficacy in a mouse model of human non-small cell lung cancer (NSCLC), while knocking down both Rev1 and Rev3 strikingly improved chemotherapy response in a prostate cancer xenograft mouse model (5, 6). Furthermore, a small molecule that blocks Rev1 from recruiting its partner Pol ζ improves cisplatin chemotherapy (7).
In this study, we focused on the HORMA domain protein, Rev7, which uses its seatbelt loop to wrap around partner proteins. By wrapping around Rev3 to form Pol ζ and then interacting with Rev1 (8), Rev7 plays a critical role in mutagenic TLS. By wrapping around SHLD3 and then interacting with SHLD2 in the four-protein Shieldin complex (9), Rev7 plays a critical role in double-strand break (DSB) repair pathway choice. When Shieldin represses DSB resection, nonhomologous end joining (NHEJ) is favored, but when Rev7 is released from the Shieldin complex in a TRIP13-dependent manner, homology-directed repair (HDR) is favored (9, 10).
Although loss of Rev7 sensitizes certain cancer cell lines to DNA-damaging agents, Rev7’s dual involvement in mutagenic TLS and DSB repair pathway choices make it difficult to predict the impact that targeting Rev7 may have on the efficacy of DNA-damaging chemotherapy in vivo. Here, we examined the effect of Rev7 loss on the response to cisplatin in a KrasG12D, p53−/− (KP) preclinical mouse model of NSCLC (11).
Results and Discussion
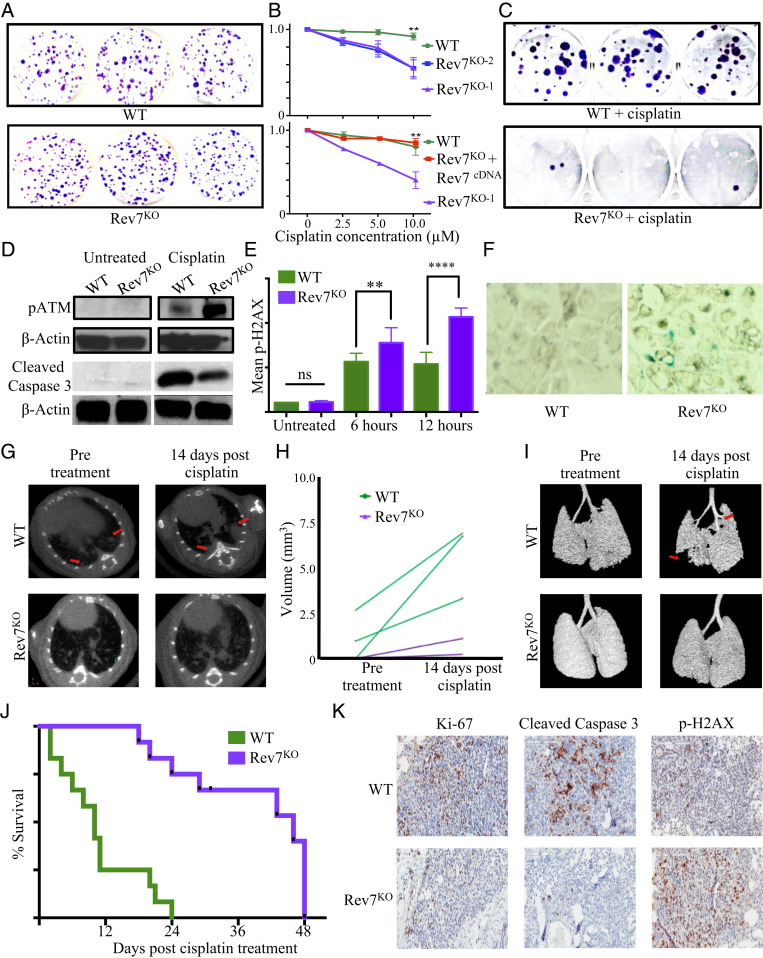
We employed CRISPR-Cas9 mutagenesis to knock out (KO) Rev7 in a KP-derived cell line. While colony formation assays did not reveal any significant differences in cell growth between KP wild type (WT) and KP Rev7KO (hereafter referred to as WT and Rev7KO) cells (Fig. 1A), we found that Rev7KO cells were significantly sensitized to cisplatin (Fig. 1B). Rev7KO also severely inhibited long-term cell recovery following treatment with cisplatin, as seen in a drastic reduction of colony formation ability (Fig. 1C). Importantly, reexpression of wild-type Rev7 in Rev7KO cells restored the level of cisplatin resistance to that observed in WT cells (Fig. 1B).
Fig. 1.
(A) Colony formation assay comparing untreated WT and Rev7KO cells. (B) Graph showing cell survival following cisplatin treatment was for WT versus Rev7KO cells. (C) Colony formation assay comparing WT and Rev7KO treated with 15 μM cisplatin. (D) Western blot loaded showing anti-pATMSER1981 (Above) or anti-cleaved caspase 3 (Below) staining in whole cell lysates from untreated or 10 µM cisplatin-treated WT and Rev7KO cells. (E) Quantification of anti-p-γ-H2AX antibody fluorescence intensity in WT and Rev7KO cells that were treated with 10 μM cisplatin for 12 h. (F) Representative pictures of SA (senescence associated) β-gal-stained WT and Rev7KO cisplatin-treated cells. (G) Representative axial images of mouse lungs harboring transplanted lung adenocarcinoma cells. Red arrowheads demarcate individual tumors in treated control mice that respond poorly to cisplatin treatment. (H) Graph showing individual tumor volume calculations for WT and Rev7KO transplants before and 2 wk after cisplatin treatment. (I) Three-dimensional isosurface projections of selected lung regions. Red arrows indicate lung adenocarcinoma mass. (J) Kaplan–Meier curve comparing survival of mice bearing WT and Rev7KO tumors following treatment with cisplatin (WT, n = 12, Rev7KO n = 12; median survival time = 10 and 46 d, respectively). P values were determined using a log-rank test. (K) Anti-Ki67, anti-cleaved caspase 3, and anti-p-γ-H2AX IHC of WT and Rev7KO tumor sections 48 h following treatment with 10 mg/kg cisplatin. **P ≤ 0.01; ****P ≤ 0.0001; ns, not significant.
We next examined the effect of Rev7 loss on the DNA damage response (DDR). Western blot analysis revealed that Rev7 loss enhanced a cisplatin-induced increase in pATM (pATM, Ser1981), a key mediator of the DDR (Fig. 1D). Additionally, Rev7KO cells exhibit increased phospho γ-H2AX, a marker of double-strand DNA breaks, as seen via immunofluorescence after cisplatin treatment (Fig. 1E). These data are consistent with recent studies implicating Rev7 in DNA end processing following damage (9, 10).
To investigate whether the enhanced sensitivity of Rev7KO cells to cisplatin was due to apoptosis, we assessed the levels of cleaved caspase 3, a marker of apoptotic cell death, in cells following drug treatment. Strikingly, we observed a decrease in cleaved caspase 3 in Rev7KO cells after cisplatin treatment (Fig. 1D). These data suggest that the loss of cell viability observed in Rev7KO cells might be due to mechanisms other than apoptotic cell death.
Another process that might limit cell outgrowth following cisplatin treatment is cellular senescence, as persistent DNA damage is known to induce long-term or irreversible growth arrest in certain contexts (12). Indeed, Rev7KO cells exhibited characteristics of DNA damage-induced senescence, including the appearance of a flattened, vacuolized cell morphology and the induction of senescence-associated β-galactosidase activity (Fig. 1F).
We next evaluated the potential of targeting Rev7 as an adjuvant therapy to enhance the response to cisplatin in vivo. We transplanted Rev7KO or WT cells into syngeneic recipient mice and examined cisplatin response by microCT imaging 3 to 4 wk after transplantation. Rev7KO tumors exhibited a dramatically enhanced response to cisplatin relative to controls. This response was apparent at the level of individual tumors (Fig. 1 G and H) and the entire lung (Fig. 1I). Additionally, Kaplan–Meier analysis showed that mice harboring Rev7KO tumors survived more than twice as long following cisplatin treatment as mice bearing control tumors (Fig. 1J). This result was specific to the treatment setting, as untreated WT and Rev7KO tumors produced terminal disease after a similar latency.
Rev7 loss reduced tumor cell proliferation as well as apoptosis in WT tumors treated with cisplatin, as evidenced by decreases in the proliferation marker KI-67 and cleaved caspase 3-positive cells, respectively (Fig. 1K). Conversely, treated Rev7KO tumors showed significantly increased numbers of γ-H2AX-positive tumor cells following cisplatin treatment. Similar to our in vitro findings, these data strongly suggest that Rev7 loss shifts the cisplatin response away from apoptosis toward a senescence phenotype.
This study provides cancer target validation for Rev7 in a treatment refractory malignancy in vivo. This enhanced drug efficacy could be attributable to Rev7’s ability to promote cisplatin resistance via the TLS DNA damage tolerance pathway and/or its regulation of DSB repair pathway choice. Indeed, Rev7 inactivation enhances cisplatin efficacy beyond that seen with disruption of other Pol ζ-components (5), suggesting that the effects of Rev7 deficiency extend beyond its role in TLS.
Our data suggest that Rev7 deficiency promotes DNA damage-induced cytostasis and senescence phenotypes. There is increasing evidence that cellular senescence—and senolytic tumor cell engagement—represents a desirable therapeutic outcome (13). Senescent cells are rapidly recognized and cleared by the innate immune system (14, 15). Indeed, in our in vivo treatment setting, Rev7KO tumor cells treated with cisplatin are readily targeted in the absence of significant measurable levels of apoptosis. Notably, a companion study (16) shows that small molecule inhibition of Pol ζ also induces a senescence-like response to cisplatin treatment. Thus, senescence may represent an on-target consequence of Pol ζ-inhibition and combination therapy treatments involving cisplatin and Pol ζ-inhibitors may be an effective strategy for inducing senolytic tumor responses in vivo.
Materials and Methods
Cell culture, Western blotting, and mouse imaging and treatment studies were performed as described (4, 10). Sequence for the Rev7 gRNA is available upon request. Immunohistochemistry (IHC) and immunofluorescence were performed as described (4). Detection of cleaved caspase 3 was performed with mouse mAb 4526 (Cell Signaling). Rev7, pATM, and cleaved caspase 3 expression were detected by Western blot using anti-Mad2L2 antibody (ab180579, Abcam), anti-phoshoATMSer1981 antibody (mouse mAb 4526), and anti-cleaved caspase 3 antibody (antibody 9661, Cell Signaling), respectively.
Acknowledgments
We thank B. Engelward, J. Lees, Y. Soto-Feliciano, K. Yamanaka, P. Bruno, S. Dalin, V. Govcheva, Y. Liu, and A. Zhang. This project was supported in part by the Massachusetts Institute of Technology (MIT) Center for Precision Cancer Medicine and the Koch Institute Support (core) Grant P30-CA14051 from the National Cancer Institute (NCI). M.T.H. acknowledges funding from the Ludwig Center at MIT. This work was also supported in part by NCI R01-CA233477 and R01-CA226898 to M.T.H., National Institute of Environmental Health Sciences Grants R01-ES015818 and R35-0ES028303 to G.C.W., and the P30-ES002109 grant to the MIT Center for Environmental Health Sciences. F.-M.V. was supported in part by NIH Pre-Doctoral Training Grants T32GM007287 and T32ES007020. G.C.W. is an American Cancer Society Professor.
Footnotes
The authors declare no competing interest.
Data Availability.
All study data are included in the article and supporting information.
References
- 1.Galluzzi L., et al. , Systems biology of cisplatin resistance: Past, present and future. Cell Death Dis. 5, e1257 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jung Y., Lippard S. J., Direct cellular responses to platinum-induced DNA damage. Chem. Rev. 107, 1387–1407 (2007). [DOI] [PubMed] [Google Scholar]
- 3.Yamanaka K., Chatterjee N., Hemann M. T., Walker G. C., Inhibition of mutagenic translesion synthesis: A possible strategy for improving chemotherapy? PLoS Genet. 13, e1006842 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Budzowska M., Graham T. G., Sobeck A., Waga S., Walter J. C., Regulation of the Rev1-pol ζ complex during bypass of a DNA interstrand cross-link. EMBO J. 34, 1971–1985 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Doles J., et al. , Suppression of Rev3, the catalytic subunit of Polzeta, sensitizes drug-resistant lung tumors to chemotherapy. Proc. Natl. Acad. Sci. U.S.A. 107, 20786–20791 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Xu X., et al. , Enhancing tumor cell response to chemotherapy through nanoparticle-mediated codelivery of siRNA and cisplatin prodrug. Proc. Natl. Acad. Sci. U.S.A. 110, 18638–18643 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wojtaszek J. L., et al. , A small molecule targeting mutagenic translesion synthesis improves chemotherapy. Cell 178, 152–159.e11 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wojtaszek J., et al. , Multifaceted recognition of vertebrate Rev1 by translesion polymerases ζ and κ. J. Biol. Chem. 287, 26400–26408 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Setiaputra D., Durocher D., Shieldin–The protector of DNA ends. EMBO Rep. 20, e47560 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Clairmont C. S., et al. , TRIP13 regulates DNA repair pathway choice through REV7 conformational change. Nat. Cell Biol. 22, 87–96 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Oliver T. G., et al. , Chronic cisplatin treatment promotes enhanced damage repair and tumor progression in a mouse model of lung cancer. Genes Dev. 24, 837–852 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hernandez-Segura A., Nehme J., Demaria M., Hallmarks of cellular senescence. Trends Cell Biol. 28, 436–453 (2018). [DOI] [PubMed] [Google Scholar]
- 13.Lee S., Schmitt C. A., The dynamic nature of senescence in cancer. Nat. Cell Biol. 21, 94–101 (2019). [DOI] [PubMed] [Google Scholar]
- 14.Krizhanovsky V., et al. , Senescence of activated stellate cells limits liver fibrosis. Cell 134, 657–667 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pallasch C. P., et al. , Sensitizing protective tumor microenvironments to antibody-mediated therapy. Cell 156, 590–602 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chatterjee N., et al. , REV1 inhibitor JH-RE-06 enhances tumor cell response to chemotherapy by triggering senescence hallmarks. Proc. Natl. Acad. Sci. U.S.A. 117, 28918–28921 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All study data are included in the article and supporting information.