Abstract
Background:
The safety of laparoscopic surgery in SARS-CoV-2 positive patients remains unclear. The presence of the virus within peritoneal fluid and the peritoneal tissues is not known. We report an asymptomatic COVID-19 positive patient who underwent laparoscopic appendectomy with negative peritoneal sampling for SARS-CoV-2.
Materials and Methods:
During a standard 3 port laparoscopic surgery samples peritoneal fluid, peritoneal brushings, and surgical smoke plum were collected. Specific real-time reverse transcriptase-polymerase chain reaction targeting SARS-CoV-2 were used to detect the presence of the virus in the samples.
Results:
SARS-CoV-2 was not detected on multiple samples of the peritoneum in an asymptomatic patient.
Conclusions:
SARS-CoV-2 was not found in the peritoneum of a single patient with asymptomatic infection. Further studies comparing SARS-CoV-2 surgical candidates are needed to address safety concerns.
Key Words: SARS-Cov-2, COVID-19, coronavirus, appendicitis, laparoscopy, appendectomy
BACKGROUND
The coronavirus disease (COVID-19) is caused by the novel coronavirus SARS-CoV-2, an enveloped single strand RNA virus in the Coronarviridae family. This highly infectious respiratory illness causes mild and self-limiting symptoms in the majority of patients. In a subset of patients, however, the syndrome can lead to a number of severe complications, including respiratory failure, severe coagulopathy, multiorgan shock, and cardiac dysfunction. As the number of cases continues to increase, we have seen a focus on the safety of the health care workers who are directly caring for infected individuals.
For surgeons, a specific area of concern is the risk of transmission during aerosolizing procedures, such as laparoscopic surgery. On the basis of extrapolated information from other viral diseases it is believed there is a risk of transmission with the use of laparoscopy and electrosurgery.1 A recent report from Italy described the isolation of SARS-CoV-2 in the peritoneum of a symptomatic patient, which has increased these concerns.2 Yet, even if SARS-CoV-2 is detected in the peritoneal cavity, it’s infective potential is not well known. As the understanding of the virus has grown so has the literature in both the medical and surgical management of infected patients. We sought to evaluate the potential of the virus’ presence in asymptomatic COVID-19 positive patient who underwent laparoscopic appendectomy with negative peritoneal sampling for SARS-CoV-2.
MATERIALS AND METHODS
A healthy 23-year-old male presented with right lower quadrant abdominal pain, nausea, and diarrhea for 2 days. His symptoms were evaluated with basic laboratory studies and computed tomography imaging of the abdomen and were consistent with uncomplicated acute appendicitis. A large appendicolith was noted at the base of the appendix which precluded nonoperative management. He denied fever, chills, shortness of breath, cough, sore throat, or increased sputum production. He did not have a known exposure to COVID-19 before his presentation. In preparation for the operating room a nasopharyngeal swab was taken and noted to positive for SARS-CoV-2; however, a computed tomography of the chest showed no evidence of pneumonia.
The patient was brought to the operating room for a standard laparoscopic appendectomy. Noninvasive representative samples of peritoneal fluid, peritoneal brushings, and surgical smoke were collected during the procedure. The case was performed in a negative pressure room with appropriate measures in place including all staff wearing full personal protective equipment as per institutional protocol. Pneumoperitoneum was established using the Pneumoclear system (Stryker, MI) and the trocars were placed in the standard location. The standard nasopharyngeal swab for SARS-CoV-2 detection was used to obtain brushing samples from the parietal peritoneum (Fig. 1A). A suction irrigator was then used to collect peritoneal fluid, which was swabbed and SARS-CoV-2 detection (Fig. 1B). At this time, a 3-way circuit was created using a stop-valve and a 20 mL syringe filled with 10 mL of normal saline along the Pneumoclear tubing (Fig. 2).
FIGURE 1.
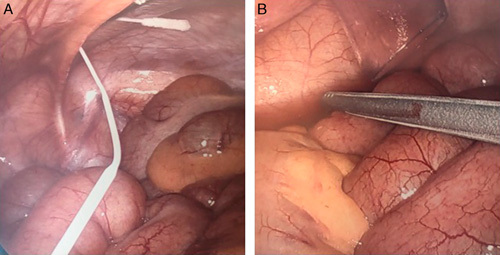
Laparoscopic sampling of the specimen. A, Sampling of the parietal peritoneum. B, Sampling of peritoneal fluid.
FIGURE 2.
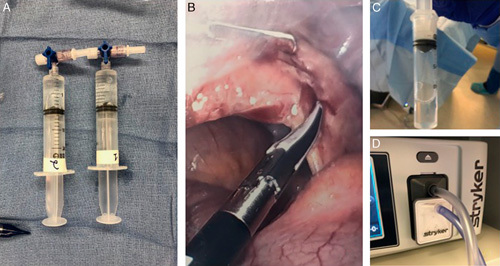
Aerosolized particles sampling. A, Three-way circuit was created using a stop-valve and a 20 mL syringe filled with 10 mL of normal saline along the Pneumoclear tubing. B, Smoke generated during the appendectomy. C and D, Smoke sampled using Pneumoclear.
The appendix was then mobilized and the mesoappendix was taken with an energy device, which created a generous amount of smoke plume for collection. At this time, one of the trocars was opened to evacuate the smoke into the collection syringe. This process was repeated 2 times and representative swabs of the solution were sent for SARS-CoV-2 detection (Fig. 2). Specific real-time reverse transcriptase-polymerase chain reaction targeting SARS-CoV-2 were used to detect the presence of the virus in the samples.
RESULTS
All collected samples of the peritoneal cavity were negative for SARS-CoV-2 (Fig. 3). The patient had an uneventful recovery and was discharged on postoperative day 1. Upon discharge he had no respiratory symptoms and was instructed to self-isolate for 7 days to avoid the spread of the disease.
FIGURE 3.

SARS-CoV-2 results. Detected during nasal swab but not detected during the peritoneal sampling.
DISCUSSION
The COVID-19 pandemic has placed a major burden on health care systems across the world. Nonetheless, surgeons have continued to provide emergency surgical care despite a lack of evidence surrounding the safety of this practice. Little is known about the transmission risk of COVID-19 in the operating theater, however, extrapolated data from other infectious diseases suggest a theorical risk of contagion during operations, especially during laparoscopy.1,3 In our patient we were unable to confirm the presence of SARS-CoV-2 in samples obtained during laparoscopy. Our findings are similar to those of Ngaserin et al4 where SARS-CoV-2 was not found in the peritoneal fluid of an asymptomatic patient undergoing laparoscopic appendectomy.
The American College of Surgeons (ACS) and the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) has published recommendations stating that laparoscopy and electrosurgery could be hazardous to health care workers as these produce aerosolizing particles.1,5 Electrocautery is known to create particles smaller than 1 µm that are able to permeate surgical-grade masks.6 Surgical smoke plume contains chemical products which can be harmful to surgeons and the operating team.7 Exposure to these particles is accentuated during laparoscopy as contained smoke increases the concentration of volatile organic compounds, which are then rapidly released as the trocars are opened. Both of these governing bodies have recommended strict use of personal protective equipment and using devices to filter the released aerosolized particles.
During the current epidemic, SARS-CoV-2 has been found in different body fluids including respiratory samples (nasopharyngeal/oropharyngeal swabs, bronchoalveolar lavage)8 but it has also been detected in tears,9 blood,10 stool,10,11 pleural fluid,10 and saliva.12 Most recently, Coccolini et al2 showed that SARS-CoV-2 was present in peritoneal fluid of a symptomatic patient. As we were unable to replicate these findings and the virus has not been persistently found in the blood samples of patients, there is a possibility that not all patients have SARS-CoV-2 in the peritoneum. Our patient and the patient described by Ngaserin and colleagues were both asymptomatic carriers. It is not known if symptomatic patients harbor higher viral loads and possibly have a higher viral burden in the peritoneum and further studies are needed to determine this.
Our study has certain limitations that should be discussed. It is based on a single patient and the false negative rate of the real-time reverse transcriptase-polymerase chain reaction for SARS-CoV-2 is variable.13 Trying to account for this variability, we obtained multiple samples. However, this case adds to the growing literature and with further studies may help elucidate the potential transmission of COVID-19 to the operating staff.
CONCLUSION
SARS-CoV-2 was not found in the peritoneum of a single patient with asymptomatic infection.
Footnotes
Patient authorize the publication of the manuscript. Information was deidentified.
The author declares no conflicts of interest.
REFERENCES
- 1.Pryor A. Sages and eaes recommendations regarding surgical response to covid-19 crisis 2020. Available at: https://www.sages.org/recommendations-surgical-response-covid-19/.
- 2.Coccolini F, Tartaglia D, Puglisi A, et al. SARS-CoV-2 is present in peritoneal fluid in COVID-19 patients.pdf; 2020. Available at: lww.com/annalsofsurgery/Documents/SARS-CoV-2%20is%20present%20in%20peritoneal%20fluid%20in%20COVID-19%20patients.pdf Accessed May 13, 2020. [DOI] [PMC free article] [PubMed]
- 3.Zheng MH, Boni L, Fingerhut A. Minimally invasive surgery and the novel coronavirus outbreak: lessons learned in China and Italy. Ann Surg. 2020. Doi: 10.1097/SLA.0000000000003924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ngaserin SH-N, Koh FH, Ong B-C, et al. COVID-19 not detected in peritoneal fluid: a case of laparoscopic appendicectomy for acute appendicitis in a COVID-19-infected patient. Langenbecks Arch Surg. 2020. Doi: 10.1007/s00423-020-01891-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.COVID-19: Elective Case Triage Guidelines for Surgical Care. American College of Surgeons; 2020. Available at: www.facs.org/covid-19/clinical-guidance/elective-case. Accessed April 11, 2020.
- 6.Alp E, Bijl D, Bleichrodt RP, et al. Surgical smoke and infection control. J Hosp Infect. 2006;62:1–5. [DOI] [PubMed] [Google Scholar]
- 7.Choi SH, Kwon TG, Chung SK, et al. Surgical smoke may be a biohazard to surgeons performing laparoscopic surgery. Surg Endosc. 2014;28:2374–2380. [DOI] [PubMed] [Google Scholar]
- 8.Zou L, Ruan F, Huang M, et al. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N Engl J Med. 2020;382:1177–1179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Xia J, Tong J, Liu M, et al. Evaluation of coronavirus in tears and conjunctival secretions of patients with SARS-CoV-2 infection. J Med Virol. 2020;92:589–594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lescure F-X, Bouadma L, Nguyen D, et al. Clinical and virological data of the first cases of COVID-19 in Europe: a case series. Lancet Infect Dis. 2020;20:697–706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Holshue ML, DeBolt C, Lindquist S, et al. First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020;382:929–936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.To KK-W, Tsang OT-Y, Yip CC-Y, et al. Consistent detection of 2019 novel coronavirus in saliva. Clin Infect Dis. 2020:ciaa149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kucirka LM, Lauer SA, Laeyendecker O, et al. Variation in false-negative rate of reverse transcriptase polymerase chain reaction–based SARS-CoV-2 tests by time since exposure. Ann Intern Med. 2020:M20–M1495. [DOI] [PMC free article] [PubMed] [Google Scholar]


