Recent studies have linked coronavirus disease 2019 (COVID-19) infection with an increased risk of ischemic stroke and acute myocardial infarction (AMI).1,2 However, the evidence base is small and current data are limited mainly to case reports and 2 cohort studies.1–4 Therefore, in a nationwide register-based study considering all patients diagnosed with COVID-19 at Danish hospitals, we assessed the association between COVID-19 infection and the risk of ischemic stroke and AMI during the acute phase of infection using the self-controlled case series method.5
We used Danish nationwide registers to identify all patients diagnosed at Danish hospitals with a positive test for COVID-19 infection up to July 16, 2020 (International Classification of Diseases–10 codes: B342, B342A, B972, B972A). From this population, we identified all patients who were admitted to the hospital with either a primary or secondary diagnosis of first-ever ischemic stroke (International Classification of Diseases–10 codes: I63 through I66) or first-ever AMI (International Classification of Diseases–10 code: I21) up to 180 days before COVID-19 diagnosis and until the end of available data (July 16, 2020). If a patient experienced >1 outcome during the observation period, only the first was considered. We based our statistical analysis on the self-controlled case series design.5 This design is ideal for assessing the effect of transient exposures such as infections, because each patient acts as his or her own control. Consequently, all confounders, even if unmeasured, are natively controlled for as long as they do not vary within the observation period.5 We defined the risk interval as the 14 days after the date of laboratory-confirmed COVID-19 diagnosis. The control interval was defined as up to 180 days before COVID-19 diagnosis and until the end of available data (July 16, 2020), excluding the risk interval. The date of COVID-19 diagnosis was used as the index date for defining the exposure. The relative incidence of AMI and ischemic stroke associated with the risk interval was calculated using a conditional Poisson regression model comparing the incidence within the risk interval with the incidence in the control interval.5 We conducted several sensitivity analyses to ascertain the robustness of our results, including controlling for calendar time in 3-month bands, varying the risk interval, varying the control interval, introducing preexposure periods, and restricting the analysis to only consider the time period after the first case of confirmed COVID-19 infection was diagnosed in Denmark (February 27, 2020; Table). According to Danish law, purely register-based studies do not require informed consent or approval by an ethics review board. The data used for this study are governed by The Danish Health Data Authority and Statistics Denmark and cannot be made available on request by the authors. Access to the data may only be provided through direct submission of a formal request to these agencies.
Table 1.
Incidence Ratios for Acute Myocardial Infarction (AMI) and Ischemic Stroke After COVID-19 Diagnosis
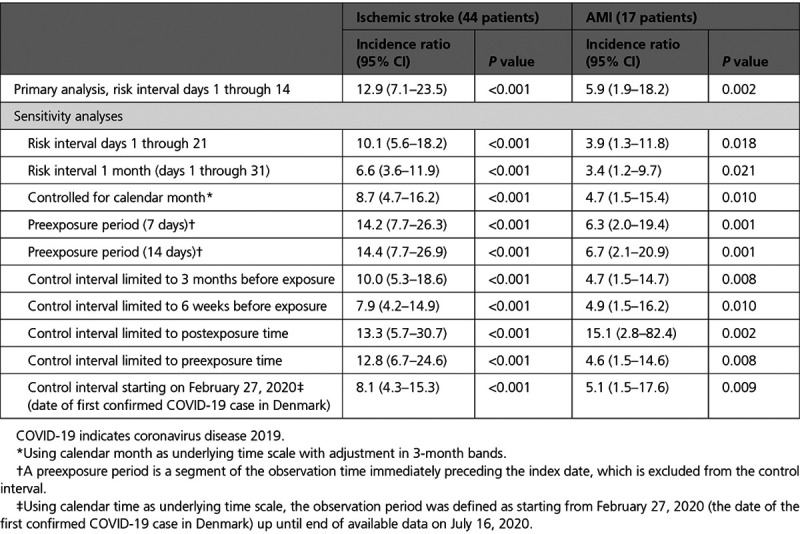
A total of 5119 patients diagnosed with COVID-19 at Danish hospitals were identified. A total of 1945 patients (38%) had received an inpatient diagnosis of COVID-19; 3174 (62%) had received an outpatient diagnosis. Among this population, 44 patients had first-ever ischemic stroke during the observation period. The mean age of the study population was 77 years (SD 9) and 52% were male. A total of 6 patients had diabetes (15%), 20 had hypertension (45%), and 15 had dyslipidemia (34%). Eleven patients had an outpatient diagnosis of COVID-19 (25%); 33 patients received an inpatient diagnosis of COVID-19 (75%). A total of 18 strokes occurred during the 14-day risk interval. The incidence of ischemic stroke was ≈10 times higher during the 14 days after COVID-19 diagnosis (Table) as compared with the control interval. The incidence of ischemic stroke remained statistically significantly elevated when the risk interval was extended to 21 and 31 days after COVID-19 diagnosis (Table). The results remained robust in all sensitivity analyses (Table).
Of the 5119 patients diagnosed with COVID-19, 17 patients had first-ever AMI during the observation period. The mean age of the population was 73 years (SD 13), and 53% were male. Fewer than 4 patients had diabetes, 11 patients had dyslipidemia (65%), and <4 patients had hypertension. The majority of patients had an inpatient diagnosis of COVID-19, and <4 patients had an outpatient diagnosis. A total of 4 AMIs occurred during the risk interval. The incidence of AMI was ≈5 times higher during the 14 days after COVID-19 diagnosis (Table) as compared with the control interval. When the risk interval was extended to 21 days and 31 days after COVID-19 diagnosis, the incidence of AMI remained statistically significantly elevated as compared with the control interval (Table). The results were robust throughout all sensitivity analyses (Table).
Our findings extend those of previous reports1–4 and provide evidence that COVID-19 may increase the risk of ischemic cardiovascular events. Similar to other acute infections, the underlying mechanisms may include cytokine-mediated plaque destabilization and hypercoagulability. Our study is limited by the low number of cases, which is likely the result of the low burden of infection observed in Denmark during the study period.
Disclosures
None.
Footnotes
Contributor Information
Brian Claggett, Email: BCLAGGETT@BWH.HARVARD.EDU.
Caroline Sindet-Pedersen, Email: carolinesindet@gmail.com.
Mats Christian Højbjerg Lassen, Email: mcha@live.dk.
Kristoffer Grundtvig Skaarup, Email: kristofferskaarup@hotmail.com.
Jens Ulrik Stæhr Jensen, Email: jens.ulrik.jensen@regionh.dk.
Michael Fralick, Email: mike.fralick@mail.utoronto.ca.
Morten Schou, Email: morten.kjoebek.lamberts@regionh.dk.
Morten Lamberts, Email: morten.kjoebek.lamberts@regionh.dk.
Thomas Gerds, Email: tag@biostat.ku.dk.
Matthew Phelps, Email: mPhelps@hjerteforeningen.dk.
Kristian Hay Kragholm, Email: kdks@rn.dk.
Mikkel Porsborg Andersen, Email: mikkel.porsborg.andersen@regionh.dk.
Lars Køber, Email: Lars.koeber.01@regionh.dk.
Christian Torp-Pedersen, Email: ctp@heart.dk.
Scott D. Solomon, Email: ssolomon@rics.bwh.harvard.edu.
Gunnar Gislason, Email: gunnar.gislason@regionh.dk.
Tor Biering-Sørensen, Email: tor.biering@gmail.com.
References
- 1.Oxley TJ, Mocco J, Majidi S, Kellner CP, Shoirah H, Singh IP, De Leacy RA, Shigematsu T, Ladner TR, Yaeger KA, et al. Large-vessel stroke as a presenting feature of Covid-19 in the young. N Engl J Med. 2020; 382:e60 doi: 10.1056/NEJMc2009787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bangalore S, Sharma A, Slotwiner A, Yatskar L, Harari R, Shah B, Ibrahim H, Friedman GH, Thompson C, Alviar CL, et al. ST-segment elevation in patients with Covid-19: a case series. N Engl J Med. 2020; 382:2478–2480. doi: 10.1056/NEJMc2009020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Merkler AE, Parikh NS, Mir S, Gupta A, Kamel H, Lin E, Lantos J, Schenck EJ, Goyal P, Bruce SS, et al. Risk of ischemic stroke in patients with coronavirus disease 2019 (COVID-19) vs patients with influenza. JAMA Neurol. 2020; 77:1366–1372. doi: 10.1001/jamaneurol.2020.2730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bilaloglu S, Aphinyanaphongs Y, Jones S, Iturrate E, Hochman J, Berger JS. Thrombosis in hospitalized patients with COVID-19 in a New York City health system. JAMA. 2020; 324:799–801. doi: 10.1001/jama.2020.13372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Whitaker HJ, Farrington CP, Spiessens B, Musonda P. Tutorial in biostatistics: the self-controlled case series method. Stat Med. 2006; 25:1768–1797. doi: 10.1002/sim.2302 [DOI] [PubMed] [Google Scholar]


