Supplemental Digital Content is available in the text.
Keywords: atherosclerosis, baroreceptor, baroreflex, blood pressure, dipping, carotid sinus, stroke
Abstract
Nighttime blood pressure (BP) generally dips by 10% to 20% of the daytime values, and abnormal BP dipping may affect vascular health independently of BP level. The regulation of BP dipping involves arterial baroreflex, whose receptors mainly reside in carotid sinuses and aortic arch. Atherosclerosis in these baroreceptor-resident arteries (BRAs) is frequent among patients with ischemic stroke (IS) and might impair their BP-regulating capacity. We aimed to examine associations between atherosclerosis of BRA and BP dipping in patients with IS. BP dipping ratio was measured by 24-hour ambulatory blood pressure monitoring on the sixth day after IS. With computed tomography angiography, atherosclerosis conditions in 10 segments of carotid sinuses and aortic arch were scored and summed as total atherosclerosis burden of BRA. Among the 245 patients with IS, 78.0% had atherosclerosis in BRA. The total AS burden of BRA was negatively correlated with systolic BP dipping ratio (r=−0.331; P<0.001) and diastolic BP dipping ratio (r=−0.225; P<0.001). After adjusting for age, sex, vascular risk factors, 24-hour BP means, cervical and intracranial atherosclerosis scores, the negative correlations still existed (adjusted β, −0.259 [95% CI, −0.416 to −0.102] and adjusted β, −0.178 [95% CI, −0.346 to −0.010], respectively). In conclusion, higher total atherosclerosis burden of BRA was independently indicative of more blunted dipping of systolic BP and diastolic BP in IS. The total atherosclerosis burden of BRA might be important for predicting and managing BP dipping in patients with IS.
Blood pressure (BP) physiologically decreases by 10% to 20% at night than that during the day.1 The abnormal BP dipping had been found associated with coronary and cerebral atherosclerosis2,3 and multiple organ damage.4,5 Recent meta-analyses concluded that less marked BP dipping portended higher risk of vascular events and death independently of 24-hour BP level.6,7 And there had been preliminary evidence, which showed that restoring normal BP dipping pattern was related to reduced vascular events.8
BP dipping is under delicate neural and humoral regulations, in which the arterial baroreflex plays a key role.9 Receptors of the arterial baroreflex mainly locate at the carotid sinuses and aortic arch, regulating BP in response to the vessel stretch and deformation induced by the transmural pressure.10 These baroreceptor-resident arteries (BRAs) are high-susceptibility sites for atherosclerosis,11 and the presence of atherosclerosis in BRA would make the arterial wall less deformable, thereby impairing the baroreflex-mediated BP regulation.12 Thus, atherosclerosis of BRA might serve as both a contributor and a target-organ damage of the dysregulated BP dipping. Would the atherosclerosis conditions in BRA be a related factor for BP dipping? Whether the relationship could be stronger than that of other arteries, which are less baroreceptor-rich?
Previously, abnormal BP dipping was linked to the presence of carotid atherosclerotic stenosis,3 but the atherosclerosis conditions in BRA had never been evaluated specifically, and its relationship with BP dipping was unexplored. Patients with ischemic stroke (IS) commonly had atherosclerotic plaques and stenosis in BRA,13 offering potential advantages in revealing the relationship between them. But there had been no validated method to characterize the atherosclerosis of BRA for these patients. It might be appropriate to establish a new atherosclerosis score to reflect the overall atherosclerosis severity and extent in both carotid sinuses and aortic arch, namely the total atherosclerosis burden of BRA.
Ambulatory blood pressure monitoring (ABPM) was primarily appropriate to assess the BP dipping14 and could be applied safely and conveniently in patients with IS.15 In this study, ABPM was used to measure the 24-hour BP characteristics of patients with IS, and computed tomography angiography was performed to evaluate the atherosclerosis conditions in aortic arch and cervicocephalic arteries. We aimed to explore the relationship of BP dipping with the total atherosclerosis burden of BRA in patients with IS.
Methods
This was a single-center cross-sectional study. All the procedures complied with the Declaration of Helsinki. The ethics committee at Xuanwu Hospital approved the study and all participants provided informed consent. The data, analytic methods, and material that supported the findings of this study are available from the corresponding author upon reasonable request.
Study Subjects
Patients admitted to the stroke unit in Xuanwu Hospital from January 1, 2018 to September 30, 2018 were consecutively enrolled. Patients were eligible if they were diagnosed as IS with confirmation of computed tomography or magnetic resonance; within 6 days after onset of symptoms; and consent to participate. Patients with suspected nonatherosclerotic arterial stenosis, such as arterial dissection and vasculitis; cardioembolism or intracranial hemorrhage; intravenous thrombolysis; cervicocephalic revascularization; surgery of aortic arch; malignant hypertension or secondary hypertension; obstructive sleep apnea-hypopnea syndrome; administration of adrenoceptor antagonist or agonist; worsening neurological conditions 3 days before the ABPM was performed; hyperthyroidism; poor organ functions or malignant tumor were excluded.
General Characteristics
Age, sex, hypertension history, diabetes mellitus history, hyperlipidemia history, smoking, and overweight (body mass index, ≥25 kg/m2) were collected by interview. Patient was considered as smoking if they actively smoked within the last 12 months. All patients underwent standard blood tests, brain magnetic resonance scan with diffusion-weighted imaging sequence or computed tomography scan within 7 days after admission. The treatment in hospital and after discharge was in accordance to the acute IS management and secondary prevention guidelines.13 All antihypertensive drugs were taken once daily at 7:00 am in hospital. The antihypertensive regimens were recorded. The National Institute of Health Stroke Scale was scored daily after the admission. The etiology of IS was classified according to The Trial of Org10172 in Acute Stroke Treatment criteria.16
Measurement of 24-Hour BP Characteristics
ABPM was performed on the sixth day after symptoms onset using Meditech ABPM-05 device (Meditech Ltd, Hungary), considering that the acute stress of IS and the edema of cerebral infarct could exert relatively huge influence on sympathetic activity and BP regulation in the first 3 to 5 days after symptoms onset,17 which might mask the relationship of BP dipping with atherosclerosis of BRA. We obtained BP readings at 30-minute intervals during daytime (6:00 am to 10:00 pm) and at 60-minute intervals during nighttime (10:00 pm to 5:00 am), eliminating the transition period (5:00 am to 6 am) when BP changed rapidly. Patients with <70% of the expected measurements were excluded for the final analysis. The weighted means of systolic BP (SBP) and diastolic BP (DBP) in the 24 hours, daytime, and nighttime were recorded in respective. BP dipping ratio was calculated as (daytime BP−nighttime BP)/daytime BP×100%. The BP dipping ratio <10% was defined as abnormal BP dipping.14
Measurement of Atherosclerosis Conditions in Aortic Arch and Cervicocephalic Arteries
Computed tomography angiography was performed with a 64-slice spiral computed tomography (Light Speed, General Electric Company) as previously reported.18 GE AW4.2 workstation (General Electric Company) was used for data reconstruction and image analysis. Images were reviewed by a certified radiologist blinded to the clinical and ABPM data.
At first, atherosclerosis conditions in 10 segments of BRA were, respectively, scored 0 to 4 points according to the percentage of vessel circumference affected by atherosclerosis on orthogonal views (0, none; 1, <25%; 2, 25%–49%; 3, 50%–74%; 4, ≥75%). Then, the carotid sinuses atherosclerosis burden was calculated by summing the atherosclerosis scores of 6 BRA segments including bilateral distal common carotid arteries, carotid bifurcations, and origins of internal carotid arteries. And the aortic arch atherosclerosis burden was the sum of atherosclerosis scores of 4 BRA segments including aortic arch (from the opening of brachiocephalic trunk to the opening of left subclavian artery) and the origins of three supra-aortic arteries (brachiocephalic trunk, left common carotid artery, and left subclavian artery). A length of 1 cm would be observed for the origins or distal parts of interested arteries. Finally, the total atherosclerosis burden of BRA was the combination of carotid sinuses atherosclerosis burden and aortic arch atherosclerosis burden (Figure 1).
Figure 1.
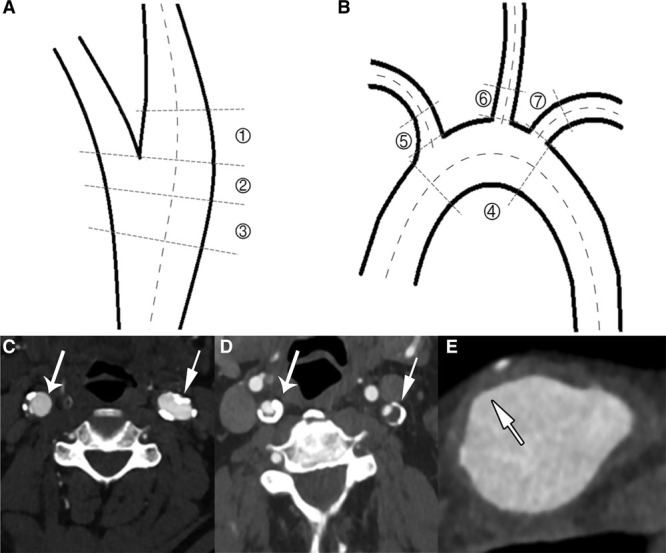
Measurements atherosclerosis (AS) burden of baroreceptor-resident arteries in patients with ischemic stroke. A, The measured segments of bilateral carotid sinuses included ① origin of internal carotid artery, ② carotid bifurcation, and ③ distal common carotid artery. B, The measured segments of aortic arch included ④ aortic arch, ⑤ origin of brachiocephalic trunk, ⑥ origin of left common carotid artery, and ⑦ origin of left subclavian artery. C, The long-tail arrow on the left indicated a distal common carotid artery with 25% to 49% vessel circumference affected by atherosclerosis, scored 2 points; the short-tail arrow on right indicated a carotid bifurcation with 50% to 74% vessel circumference affected by AS, scored 3 points. D, The long-tail arrow on the left and the short-tail arrow on right both indicated origins of internal carotid arteries with 50% to 74% vessel circumference affected by atherosclerosis, scored 3 points. E, The short-tail arrow indicated an aortic arch with 25% to 49% vessel circumference affected by AS, scored 2 points.
The atherosclerosis of cervicocephalic arteries was also scored semi-quantitatively. The atherosclerosis conditions in each cervical and intracranial segment was scored 0 to 4 points based on the degree of atherosclerotic stenosis (0, no atherosclerotic plaque; 1, atherosclerotic plaque without obvious lumen stenosis or stenosis <50%; 2, stenosis 50%–69%; 3, stenosis 70%–99%; 4, occlusion).18 The cervical atherosclerosis score was the sum of atherosclerosis scores of 8 arterial segments including bilateral common carotid, subclavian, extracranial carotid, and extracranial vertebral arteries. The intracranial atherosclerosis score was computed by summing the atherosclerosis scores of 11 arterial segments included bilateral intracranial carotid, intracranial vertebral, anterior cerebral, middle cerebral, posterior cerebral arteries, and basilar artery.
Statistical Analysis
Statistical analyses were performed using SPSS (v25.0; IBM). Data were presented as mean±SD for normally distributed continuous variables, count (%) for nominal variables, and median (Q1, Q3) for abnormally distributed continuous variables and ordinal variables. The P value <0.05 was considered statistically significant.
Spearman correlation analysis and partial correlation analysis would be used to evaluate the correlations between BP dipping ratio and various atherosclerosis burden of BRA indices. The preset controlling factors for the partial correlation analysis included age, sex, hypertension history, diabetes mellitus history, hyperlipidemia history, smoking, overweight, antihypertensive therapy, and weighted mean of 24-hour BP. Linear regression model would be used to examine the independent relationship of BP dipping ratio with the total atherosclerosis burden of BRA, with adjustments for age, sex, weighted 24-hour mean of BP, and all potentially related general characteristics (P<0.1 in linear regression analysis for BP dipping ratio after adjusting age and sex). Variables would be transformed as appropriate for the linear regression model. The β value was estimated with 95% CI. Indicative value of total atherosclerosis burden of BRA for the abnormal BP dipping (BP dipping ratio <10% as defined above) was also tested with logistic regression analysis. The odd ratio was estimated with 95% CI.
Results
Total Study Population
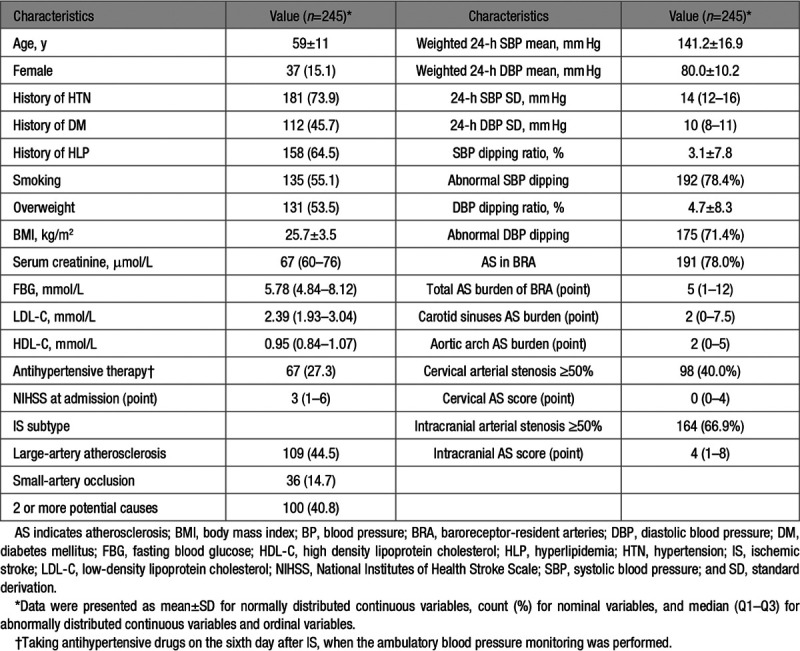
A total of 245 patients with IS were finally included (Figure S1 in the Data Supplement). The average age was 59±11 years, and males were predominant (84.9%). The weighted means of 24-hour SBP and DBP were 141.2±16.9 and 80.0±10.2 mm Hg, respectively, when 27.3% patients were taking antihypertensive drugs. The dipping ratios of SBP and DBP were 3.1±7.8% and 4.7±8.3% on average. The abnormal SBP and DBP dipping was respectively observed in 192 (78.4%) patients and 175 (71.4%) patients. There were 191 (78.0%) patients having atherosclerosis in BRA. The medians of total atherosclerosis burden of BRA, carotid sinuses atherosclerosis burden, and aortic arch atherosclerosis burden were 5 (1–12) points, 2 (0–7.5) points, and 2 (0–5) points. The median cervical and intracranial atherosclerosis scores were 0 (0–4) points and 4 (1–8) points (see Table 1 for more characteristics).
Table 1.
Characteristics of the Included Patients With IS
Correlations of BP Dipping Ratio and Various Atherosclerosis Burden of BRA Indices in IS
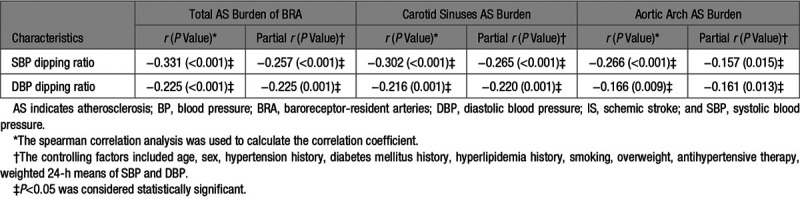
Among the 245 patients with IS, Spearman correlation analyses showed that both dipping ratios of SBP (r=−0.331; P<0.001) and DBP (r=−0.225; P<0.001) were negatively correlated with the total atherosclerosis burden of BRA. The associations of BP dipping ratio with carotid sinuses atherosclerosis burden (r=−0.302, P<0.001 for SBP; r=−0.216, P=0.001 for DBP) and aortic arch atherosclerosis burden (r=−0.266, P<0.001 for SBP; r=−0.166, P=0.009 for DBP) were similar to that with total atherosclerosis burden of BRA, though the correlation coefficients were numerically smaller (Figure 2). These correlations remained statistically significant after controlling age, sex, hypertension history, diabetes mellitus history, hyperlipidemia history, smoking, overweight, antihypertensive therapy, and weighted 24-hour means of SBP and DBP (Table 2).
Figure 2.
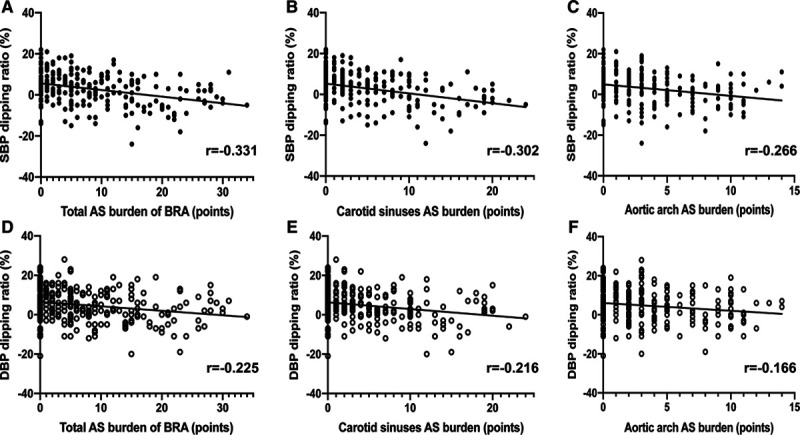
Scatter plots of blood pressure dipping ratio and various atherosclerosis (AS) burden of baroreceptor-resident artery (BRA) indices in patients with ischemic stroke. DBP indicates diastolic blood pressure; and SBP, systolic blood pressure.
Table 2.
Correlations of BP Dipping Ratio and Various AS Burden of BRA Indices in Patients With IS
Independent Relationship of BP Dipping Ratio With the Total Atherosclerosis Burden of BRA in IS
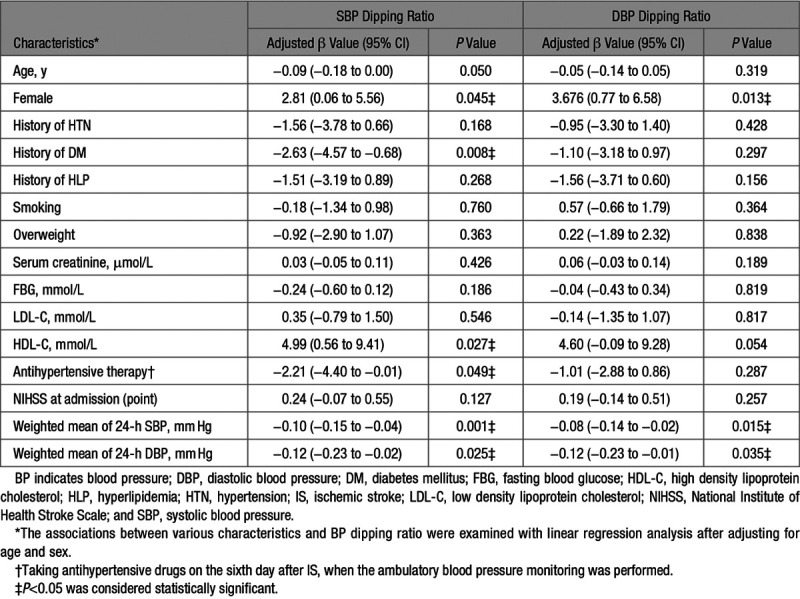
The general characteristics of patients with IS that might be associated with BP dipping ratio were explored at first, using linear regression models with adjustments for age and sex. Both SBP and DBP dipping was more blunted in males than females, while a positive history of diabetes mellitus the antihypertensive therapy and a lower level of high-density lipoprotein cholesterol were associated with more blunted SBP dipping (P<0.05). Besides, patients with higher 24-hour means of SBP and DBP showed more blunted SBP and DBP dipping (P<0.05) (Table 3).
Table 3.
Linear Regression Analysis of Associations Between General Characteristics and BP Dipping Ratio in Patients With IS
Then 2 basic models for predicting SBP and DBP dipping ratios were built with age, sex, 24-hour means of SBP and DBP, and general characteristics with P<0.1 in above linear regression analyses. Entering the total atherosclerosis burden of BRA into the basic models would increase the R2 of models from 0.109 to 0.175 for SBP dipping ratio and from 0.066 to 0.108 for DBP dipping ratio. And the total atherosclerosis burden of BRA showed independent predictive value for both dipping ratios of SBP (adjusted β, −0.297 [95% CI, −0.431 to −0.162) and DBP (adjusted β, −0.242 [95% CI, −0.386 to −0.098]) in patients with IS (Table 4).
Table 4.
Linear Regression Analysis of Independent Relationship of BP Dipping Ratio With Total AS Burden of BRA in Patients With IS
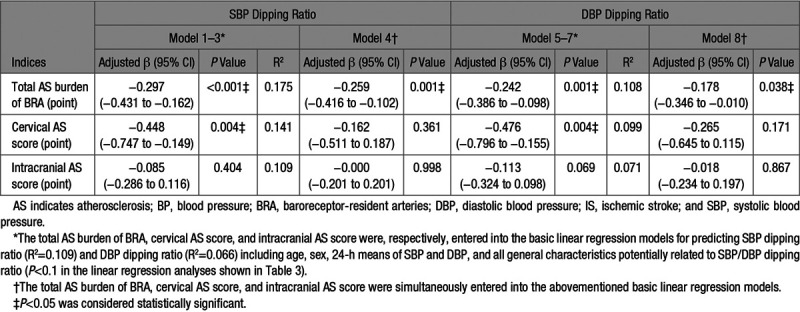
If the cervical atherosclerosis score was entered into the basic models instead of the total atherosclerosis burden of BRA, the R2 of models would reduce to 0.141 for SBP dipping ratio and to 0.099 for DBP dipping ratio. The R2 of models would further decrease if the total atherosclerosis burden of BRA was substituted with the intracranial atherosclerosis score. If the total atherosclerosis burden of BRA, cervical atherosclerosis score, and intracranial atherosclerosis score were simultaneously entered into the basic models, only the total atherosclerosis burden of BRA was independently associated with SBP dipping ratio (adjusted β, −0.259 [95% CI, −0.416 to −0.102]) and DBP dipping ratio (adjusted β, −0.178 [95% CI, −0.346 to −0.010]; Table 4).
Indicative Value of the Total Atherosclerosis Burden of BRA for the Abnormal BP Dipping in IS
Dipping ratios of SBP and DBP were both abnormal (<10%) in 167 (68.2%) patients, while another 33 (13.5%) patients had abnormality in only one of the dipping ratios of SBP and DBP. According to the logistic regression analysis, higher total atherosclerosis burden of BRA was a significant indicator of the abnormal SBP dipping (odds ratio, 1.086 [95% CI, 1.029–1.146]; P=0.003) and the abnormal DBP dipping (odds ratio, 1.056 [95% CI, 1.012–1.102]; P=0.012), independent of age and sex.
Discussion
This study mainly showed that the total atherosclerosis burden of BRA was negatively correlated with the dipping ratios of both SBP and DBP, independently of age, sex, vascular risk factors, 24-hour means of SBP and DBP, cervical and intracranial atherosclerosis scores.
Accumulating evidence indicates that abnormal BP dipping is related to atherosclerosis of coronary and carotid arteries.1–3 Based on the unique BP-regulating capacity of BRA, we further supposed that BP dipping and atherosclerosis of BRA should be tightly associated. However, the overall atherosclerosis conditions in BRA had not been specifically observed before. The total atherosclerosis burden of BRA was measured in this study and might have some advantages. First, it was a semiquantitative score reflecting both severity and extent of atherosclerosis in BRA, which might provide more information than merely paid attention to the presence or absence of a specific atherosclerosis characteristic in a binary fashion. Second, previous research had found that baroreflex sensitivity was obviously impaired in patients with mild (<50%) carotid stenosis, similar to those with more severe stenosis.19 Consequently, we scored the atherosclerosis conditions in each segment of BRA according to the atherosclerotic percentage of vessel circumference, rather than the severity of luminal stenosis. It might be helpful to build a more reliable connection between atherosclerosis degree and baroreflex impairments. Third, atherosclerosis conditions in both carotid sinuses and aortic arch were comprehensively evaluated. Although the baroreceptors of carotid sinus are thought to be more sensitive to abrupt perturbations to BP than those of aortic arch,20 our results demonstrated that atherosclerosis burdens of both carotid sinuses and aortic arch were significantly correlated with the BP dipping ratio (Table 2). It provided further rationale for the use of total atherosclerosis burden of BRA in revealing the associations between BP dipping and atherosclerosis of BRA.
In the study, we also scored the atherosclerosis conditions in cervical and intracranial arteries semiquantitatively and found them less potent in predicting BP dipping ratio compared with the total atherosclerosis burden of BRA (Table 4). It further indicated the necessity to evaluate total atherosclerosis burden of BRA to make a more precise prediction for BP dipping among patients with IS. Moreover, there was no baroreceptor being located in the intracranial arteries, and the baroreceptor-rich carotid sinuses constituted only a small part of the cervical arteries. Thus, the capacity of atherosclerosis conditions in different arteries for predicting BP dipping appeared to be dependent on the abundance of arterial baroreceptors in this study. This finding perhaps implied a direct involvement of baroreceptor in the BP dipping regulation.
It had been recognized that hardened carotid arteries due to atherosclerosis would impair the stretch of baroreceptors, leading to a diminished baroreflex function and excess BP variability.21 Among patients with IS, we further found that the total atherosclerosis burden of BRA had important predictive value for both SBP and DBP dipping ratios. Physiologically, though arterial baroreflex is best known as a buffer against rapid BP changes,10 it is also indispensable to the wake-to-sleep BP regulation.22 Abnormal BP dipping had been postulated to be associated with impaired baroreflex-mediated parasympathetic activity.23 And the imbalance between the sympathetic and parasympathetic activity had been shown in IS patients with internal carotid atherosclerotic stenosis.24 Supposedly, the atherosclerosis of BRA would increase the wall stiffness12 and decrease the transmural pressure, thereby generating less baroreflex afferent impulses, resulting in enhanced sympathetic activity, relatively reduced parasympathetic activity,10 and finally giving rise to the blunted BP dipping ratio. Those patients with higher atherosclerosis burden of BRA might have less physiological baroreflex reserve. So, the atherosclerosis of BRA could be not only a target-organ damage but also a contributor of the abnormal BP dipping, offering a possible explanation for our observation that BP dipping ratio seemed to be more closely associated with the total atherosclerosis burden of BRA than the cervical and intracranial atherosclerosis scores.
Perspectives
This preliminary study discovered an independent association between BP dipping and the total atherosclerosis burden of BRA in patients with IS. Evaluating the overall atherosclerosis burden of carotid sinuses and aortic arch, where the arterial baroreceptors reside, might aid in predicting the BP dipping and selecting patients with IS who should further undergo 24-hour ABPM. Further research would be needed to test and optimize our measuring methods of atherosclerosis conditions in BRA and reveal the precise mechanisms responsible for the relationship of BP dipping with the total atherosclerosis burden of BRA and determine the utility in improving risk assessment and stratification of vascular events. More importantly, our results hinted the possibility that the atherosclerosis of BRA might participate in the genesis of BP dipping abnormality. Then, the total atherosclerosis burden of BRA might become a potential target to modulate BP dipping pattern, laying foundations for developing a pathophysiology-based management of abnormal BP dipping.
Limitations
This cross-sectional study had several limitations. First, as a single-center study in east Asia with relatively small sample size, cautions must be taken in generalization of our findings to other populations. In particular, we only included patients with IS, whose atherosclerosis conditions in BRA were generally serious. It should be noted that 78.0% of our participants had atherosclerosis in BRA. Second, we assessed BP dipping on the sixth day after IS symptoms onset when there could be persisted sympathetic overactivity. But most acute stress from IS diminished after 3 to 5 days,17 and we excluded patients with progressive neurological deficits in 3 days before the ABPM was performed. In addition, the neurological deficit of all patients was relatively minor (mean National Institutes of Health Stroke Scale at admission was 3 points). Third, considering that sleep quality could exert significant influence on the BP dipping pattern,25 a relatively long ABPM recording interval was used in this study to avoid much disturbance to the patients. The frequency of BP measurement was half lower in this study than the guidelines recommended,14 though it had been successfully applied in several previous studies.26,27 At last, we relied on computed tomography angiography to obtain the total atherosclerosis burden of BRA, which had limited tissue resolution. But computed tomography angiography was the preferable noninvasive imaging method to simultaneously assess atherosclerosis conditions in cervicocephalic arteries and aortic arch,18 guaranteeing the evaluation scope of all interested BRA segments.
Conclusions
The atherosclerosis in BRA was frequent among patients with IS. Higher total atherosclerosis burden of BRA was a significant indicator of more blunted SBP and DBP dipping in IS, irrespective of age, sex, vascular risk factors, 24-hour BP means, and atherosclerosis conditions in cervicocephalic arteries. Evaluating the total atherosclerosis burden of BRA might be important for the prediction and clinical management of BP dipping in patients with IS.
Acknowledgments
We acknowledged the support from Guiling Wan, Sufang Xue, and other doctors and nurses in the Department of neurology, Xuanwu Hospital for obtaining the patient consents and performing the 24-hour ABPM with high quality. We also acknowledged the support from the Clinical Center for Cardio-cerebrovascular Disease, Capital Medical University, Beijing, China.
Sources of Funding
This work was supported by grants from the Beijing Municipal Administration of Hospitals Clinical Medicine Development (No. ZYLX201706) and the Beijing Municipal Natural Science Foundation (No. 7172093).
Disclosures
None.
Supplementary Material
Footnotes
The Data Supplement is available with this article at https://www.ahajournals.org/doi/suppl/10.1161/HYPERTENSIONAHA.120.15036.
Novelty and Significance
What Is New?
The regulation of blood pressure (BP) dipping involves arterial baroreflex, whose receptors reside in carotid sinuses and aortic arch. The associations between atherosclerosis of these baroreceptor-resident arteries (BRAs) and BP dipping were first explored.
Atherosclerosis conditions in 10 segments of BRA were specifically scored and summed as the total atherosclerosis burden of BRA.
The total atherosclerosis burden of BRA was negatively correlated with BP dipping ratio among patients with ischemic stroke, independently of age, sex, vascular risk factors, 24-hour BP means, and cervicocephalic atherosclerosis.
What Is Relevant?
The total atherosclerosis burden of BRA was shown as an independent related factor and a potential determinant of BP dipping in ischemic stroke.
Summary
The independent relationship of BP dipping with total atherosclerosis burden of BRA might be important for BP dipping prediction and management in patients with ischemic stroke.
References
- 1.Parati G, Ochoa JE, Lombardi C, Bilo G. Assessment and management of blood-pressure variability. Nat Rev Cardiol. 2013;10:143–155. doi: 10.1038/nrcardio.2013.1. doi: 10.1038/nrcardio.2013.1. [DOI] [PubMed] [Google Scholar]
- 2.Mousa T, el-Sayed MA, Motawea AK, Salama MA, Elhendy A. Association of blunted nighttime blood pressure dipping with coronary artery stenosis in men. Am J Hypertens. 2004;17:977–980. doi: 10.1016/j.amjhyper.2004.05.020. doi: 10.1016/j.amjhyper.2004.05.020. [DOI] [PubMed] [Google Scholar]
- 3.Yan B, Peng L, Han D, Sun L, Dong Q, Yang P, Zheng F, Ong H, Zeng L, Wang G. Blood pressure reverse-dipping is associated with early formation of carotid plaque in senior hypertensive patients. Medicine (Baltimore) 2015;94:e604. doi: 10.1097/MD.0000000000000604. doi: 10.1097/MD.0000000000000604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Scuteri A, Rovella V, Alunni Fegatelli D, Tesauro M, Gabriele M, Di Daniele N. An operational definition of SHATS (Systemic Hemodynamic Atherosclerotic Syndrome): role of arterial stiffness and blood pressure variability in elderly hypertensive subjects. Int J Cardiol. 2018;263:132–137. doi: 10.1016/j.ijcard.2018.03.117. doi: 10.1016/j.ijcard.2018.03.117. [DOI] [PubMed] [Google Scholar]
- 5.Di Daniele N, Fegatelli DA, Rovella V, Castagnola V, Gabriele M, Scuteri A. Circadian blood pressure patterns and blood pressure control in patients with chronic kidney disease. Atherosclerosis. 2017;267:139–145. doi: 10.1016/j.atherosclerosis.2017.10.031. doi: 10.1016/j.atherosclerosis.2017.10.031. [DOI] [PubMed] [Google Scholar]
- 6.Hansen TW, Li Y, Boggia J, Thijs L, Richart T, Staessen JA. Predictive role of the nighttime blood pressure. Hypertension. 2011;57:3–10. doi: 10.1161/HYPERTENSIONAHA.109.133900. doi: 10.1161/HYPERTENSIONAHA.109.133900. [DOI] [PubMed] [Google Scholar]
- 7.Salles GF, Reboldi G, Fagard RH, Cardoso CR, Pierdomenico SD, Verdecchia P, Eguchi K, Kario K, Hoshide S, Polonia J, et al. Prognostic effect of the nocturnal blood pressure fall in hypertensive patients: the ambulatory blood pressure collaboration in patients with hypertension (ABC-H) meta-analysis. Hypertension. 2016;67:693–700. doi: 10.1161/HYPERTENSIONAHA.115.06981. doi: 10.1161/HYPERTENSIONAHA.115.06981. [DOI] [PubMed] [Google Scholar]
- 8.Hermida RC, Ayala DE, Smolensky MH, Fernández JR, Mojón A, Portaluppi F. Chronotherapy with conventional blood pressure medications improves management of hypertension and reduces cardiovascular and stroke risks. Hypertens Res. 2016;39:277–292. doi: 10.1038/hr.2015.142. doi: 10.1038/hr.2015.142. [DOI] [PubMed] [Google Scholar]
- 9.Chadachan VM, Ye MT, Tay JC, Subramaniam K, Setia S. Understanding short-term blood-pressure-variability phenotypes: from concept to clinical practice. Int J Gen Med. 2018;11:241–254. doi: 10.2147/IJGM.S164903. doi: 10.2147/IJGM.S164903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fadel PJ, Ogoh S, Keller DM, Raven PB. Recent insights into carotid baroreflex function in humans using the variable pressure neck chamber. Exp Physiol. 2003;88:671–680. doi: 10.1113/eph8802650. doi: 10.1113/eph8802650. [DOI] [PubMed] [Google Scholar]
- 11.VanderLaan PA, Reardon CA, Getz GS. Site specificity of atherosclerosis: site-selective responses to atherosclerotic modulators. Arterioscler Thromb Vasc Biol. 2004;24:12–22. doi: 10.1161/01.ATV.0000105054.43931.f0. doi: 10.1161/01.ATV.0000105054.43931.f0. [DOI] [PubMed] [Google Scholar]
- 12.Cox RH, Bagshaw RJ, Detweiler DK. Alterations in carotid sinus reflex control of arterial hemodynamics associated with experimental hyperlipemia in the racing greyhound. Circ Res. 1980;46:237–244. doi: 10.1161/01.res.46.2.237. doi: 10.1161/01.res.46.2.237. [DOI] [PubMed] [Google Scholar]
- 13.Kernan WN, Ovbiagele B, Black HR, Bravata DM, Chimowitz MI, Ezekowitz MD, Fang MC, Fisher M, Furie KL, Heck DV, et al. Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45:2160–2236. doi: 10.1161/STR.0000000000000024. doi: 10.1161/STR.0000000000000024. [DOI] [PubMed] [Google Scholar]
- 14.Parati G, Stergiou G, O’Brien E, Asmar R, Beilin L, Bilo G, Clement D, de la Sierra A, de Leeuw P, Dolan E, et al. European Society of Hypertension Working Group on Blood Pressure Monitoring and Cardiovascular Variability. European Society of Hypertension practice guidelines for ambulatory blood pressure monitoring. J Hypertens. 2014;32:1359–1366. doi: 10.1097/HJH.0000000000000221. doi: 10.1097/HJH.0000000000000221. [DOI] [PubMed] [Google Scholar]
- 15.Jain S, Namboodri KK, Kumari S, Prabhakar S. Loss of circadian rhythm of blood pressure following acute stroke. BMC Neurol. 2004;4:1. doi: 10.1186/1471-2377-4-1. doi: 10.1186/1471-2377-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Adams HP, Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, Marsh EE., III. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in acute stroke treatment. Stroke. 1993;24:35–41. doi: 10.1161/01.str.24.1.35. doi: 10.1161/01.str.24.1.35. [DOI] [PubMed] [Google Scholar]
- 17.Kwarciany M, Gąsecki D, Kowalczyk K, Rojek A, Laurent S, Boutouyrie P, Skrzypek-Czerko M, Nyka WM, Narkiewicz K, Karaszewski B. Acute hypertensive response in ischemic stroke is associated with increased aortic stiffness. Atherosclerosis. 2016;251:1–5. doi: 10.1016/j.atherosclerosis.2016.04.027. doi: 10.1016/j.atherosclerosis.2016.04.027. [DOI] [PubMed] [Google Scholar]
- 18.Kong Q, Ma X, Wang C, Feng W, Ovbiagele B, Zhang Y, Du X, Fang X. Influence of age ranges on relationship of complex aortic plaque with cervicocephalic atherosclerosis in ischemic stroke. J Stroke Cerebrovasc Dis. 2019;28:1586–1596. doi: 10.1016/j.jstrokecerebrovasdis.2019.03.001. doi: 10.1016/j.jstrokecerebrovasdis.2019.03.001. [DOI] [PubMed] [Google Scholar]
- 19.Nasr N, Pavy-Le Traon A, Larrue V. Baroreflex sensitivity is impaired in bilateral carotid atherosclerosis. Stroke. 2005;36:1891–1895. doi: 10.1161/01.STR.0000177890.30065.cb. doi: 10.1161/01.STR.0000177890.30065.cb. [DOI] [PubMed] [Google Scholar]
- 20.Ito CS, Scher AM. Regulation of arterial blood pressure by aortic baroreceptors in the unanesthetized dog. Circ Res. 1978;42:230–236. doi: 10.1161/01.res.42.2.230. doi: 10.1161/01.res.42.2.230. [DOI] [PubMed] [Google Scholar]
- 21.Ziegler MG. Atherosclerosis and blood pressure variability. Hypertension. 2018;71:403–405. doi: 10.1161/HYPERTENSIONAHA.117.10481. doi: 10.1161/HYPERTENSIONAHA.117.10481. [DOI] [PubMed] [Google Scholar]
- 22.Silvani A. Physiological sleep-dependent changes in arterial blood pressure: central autonomic commands and baroreflex control. Clin Exp Pharmacol Physiol. 2008;35:987–994. doi: 10.1111/j.1440-1681.2008.04985.x. doi: 10.1111/j.1440-1681.2008.04985.x. [DOI] [PubMed] [Google Scholar]
- 23.Vaile JC, Stallard TJ, al-Ani M, Jordan PJ, Townend JN, Littler WA. Sleep and blood pressure: spontaneous baroreflex sensitivity in dippers and non-dippers. J Hypertens. 1996;14:1427–1432. doi: 10.1097/00004872-199612000-00007. doi: 10.1097/00004872-199612000-00007. [DOI] [PubMed] [Google Scholar]
- 24.Xiong L, Leung HW, Chen XY, Han JH, Leung WH, Soo OY, Lau YL, Wong KS. Autonomic dysfunction in ischemic stroke with carotid stenosis. Acta Neurol Scand. 2012;126:122–128. doi: 10.1111/j.1600-0404.2011.01617.x. doi: 10.1111/j.1600-0404.2011.01617.x. [DOI] [PubMed] [Google Scholar]
- 25.Cho MC. Clinical significance and therapeutic implication of nocturnal hypertension: relationship between nighttime blood pressure and quality of sleep. Korean Circ J. 2019;49:818–828. doi: 10.4070/kcj.2019.0245. doi: 10.4070/kcj.2019.0245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ingelsson E, Björklund-Bodegård K, Lind L, Arnlöv J, Sundström J. Diurnal blood pressure pattern and risk of congestive heart failure. JAMA. 2006;295:2859–2866. doi: 10.1001/jama.295.24.2859. doi: 10.1001/jama.295.24.2859. [DOI] [PubMed] [Google Scholar]
- 27.Kawai T, Ohishi M, Kamide K, Nakama C, Onishi M, Ito N, Takami Y, Takeya Y, Rakugi H. Differences between daytime and nighttime blood pressure variability regarding systemic atherosclerotic change and renal function. Hypertens Res. 2013;36:232–239. doi: 10.1038/hr.2012.162. doi: 10.1038/hr.2012.162. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


