Abstract
Objective
To describe a pediatric stroke syndrome with chronic focal vertebral arteriopathy adjacent to cervical abnormalities.
Methods
At a single pediatric stroke center, we identified consecutive children with stroke and vertebral arteriopathy of the V3 segment with adjacent cervical bony or soft tissue abnormalities. We abstracted clinical presentation, treatment, and follow-up data from medical charts.
Results
From 2005 to 2019, 10 children (all boys, ages 6–16 years) presented with posterior circulation strokes and vertebral arteriopathy with adjacent cervical pathology. Two children had bony abnormalities: one had a congenital arcuate foramen and one had os odontoideum with cervical instability. In children without bony pathology, vertebral artery narrowing during contralateral head rotation was visualized by digital subtraction angiography. Eight boys had recurrent ischemic events despite anti-thrombotic treatment (including 5 with multiple recurrences) and were treated surgically to prevent additional stroke. Procedures included vertebral artery decompression (n = 6), endovascular stent and spinal fusion (n = 1), and vertebral artery endovascular occlusion (n = 1). In boys treated with decompression, cervical soft tissue abnormalities (ruptured atlantoaxial bursa, ruptured joint capsule, or connective tissue scarring) were directly visualized during open surgery. No other etiology for stroke or dissection was found in any of the cases. Two boys without recurrent stroke were treated with activity restriction and antithrombotics. At a median follow-up of 51 months (range 17–84), there have been no additional recurrences.
Conclusions
Children with V3 segmental vertebral arteriopathy frequently have stroke recurrence despite antithrombotics. Cervical bone imaging and angiography with neck rotation can identify underlying pathology.
In studies of healthy volunteers and cadavers, a proportion of subjects narrow or occlude a vertebral artery during head rotation.1,2 In a previously reported series of boys with vertebral artery dissection, digital subtraction angiography (DSA) demonstrated arterial narrowing during passive neck rotation at the level of dissection.3 From these and our observations, we hypothesized that chronic vertebral artery injury from repeated mechanical impingement by adjacent bony or soft tissue abnormalities during head rotation could be a cause of recurrent pediatric posterior circulation strokes. We aimed to describe a series of children with posterior circulation strokes presumed related to mechanical injury of the vertebral artery during head rotation.
Methods
We retrospectively and prospectively identified a consecutive series of patients <18 years of age at the University of California San Francisco (January 2005–July 2019) who had ischemic stroke due to focal V3 segment vertebral arteriopathy. In those with imaging or direct visualization of adjacent bony or soft tissue abnormalities, data were abstracted from medical records in a standardized fashion. Vertebral arteriopathy was defined by luminal irregularity, intimal flap, pseudoaneurysm, or dissection identified on CT angiography or DSA. Ischemic recurrence was a TIA or ischemic stroke after the index stroke. Antithrombotic treatment included antiplatelets or anticoagulation. Follow-up time was calculated from surgical intervention to last follow-up; in boys without surgery, time was calculated from implementation of activity restriction and antithrombotic treatment. Patient characteristics were described with summary statistics.
Standard protocol approvals, registrations, and patient consents
The University of California San Francisco Institutional Review Board approved and waived consent for this minimal risk study.
Data availability
Anonymized data not published within the article are available from the corresponding author upon reasonable request from any qualified investigator.
Results
We identified 14 children with posterior circulation strokes and focal V3 segment vertebral arteriopathy during the study period. Four had an occluded vertebral artery that could not be further evaluated by DSA with head rotation. No cervical bony abnormalities were identified in these 4. Ten children, all boys with adjacent cervical bony or soft-tissue abnormalities, were identified for this series. Eight of 10 had ischemic recurrences despite antithrombotics, including 5 with multiple recurrences and 3 with basilar artery thrombosis. None of the children had ischemic symptoms during head rotation to suggest cerebral hypoperfusion. Age, timing of recurrences, features of arteriopathy, and cervical abnormalities are summarized in the table. Supplemental individual-level data are available from Dryad (datadryad.org/stash/share/zbCMlvTIsN0GCjLm1nMU8fYyD3vW96fKi-dH4ztokqM).
Table.
Summary data of 10 boys with posterior circulation strokes due to vertebral arteriopathy from presumed compression against adjacent cervical abnormalities

All 10 children had cardiac transthoracic echocardiogram (TTE) and hypercoagulable laboratory testing without pertinent findings; no connective tissue disorders or recent major traumas were identified. Three had pertinent family history. One child's mother had a cryptogenic pontine stroke during childbirth. Two boys were brothers. Quartet whole exome sequencing of the brothers and parents did not identify relevant variants.
Bone imaging in 2 boys identified abnormalities. One had placement of a vertebral artery stent to treat worsening arteriopathy before an occult atlantoaxial fracture was recognized. Later evaluation identified cervical instability related to os odontoideum, subsequently treated with C1-C2 fusion. In the second, a competitive wrestler, bone imaging demonstrated a congenital arcuate foramen of the atlas. In 8 children without bony cervical pathology or vertebral artery occlusion, DSA demonstrated luminal narrowing or occlusion of the V3 segment suggestive of impingement from adjacent tissue during contralateral head rotation (figures 1 and 2). One child with a progressively worsening pseudoaneurysm was treated with endovascular vertebral artery occlusion. Six children with rotational vertebral narrowing were treated with surgical decompression by removing the bony canal surrounding the vertebral artery at C1. In these 6, cervical soft tissue abnormalities (ruptured atlantoaxial bursa, ruptured joint capsule, or C1-C2 connective tissue scarring) were directly visualized during the open surgery and excised. Postoperative DSA demonstrated resolution of rotational narrowing after decompression in all 6 cases. The children without ischemic recurrence were managed with aspirin and strict activity restriction (avoidance of contact sports and activities with forceful neck rotation). Median follow-up was 58 months (range 21–90 months). During follow-up after surgical treatment or implementation of activity restriction, there have been no additional ischemic recurrences.
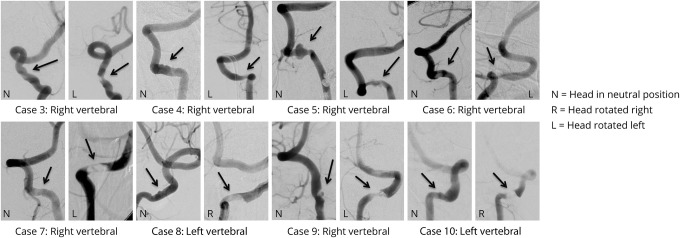
Figure 1. Cervical vertebral arteriopathies demonstrated by digital subtraction angiography (DSA) with segmental narrowing during contralateral head rotation.
DSA in 8 boys with stroke and vertebral arteriopathy, demonstrating the appearance of the V3 segment with head in neutral position (N) and dynamic narrowing during contralateral head rotation (R = head rotated right, L = head rotated left).
Figure 2. CT angiography (CTA) demonstrating vertebral artery narrowing during contralateral head rotation.

CTA of case 6 demonstrating the right vertebral artery with luminal narrowing (arrow) in relationship to adjacent cervical bony and soft tissue structures during head rotation to the left.
Discussion
We describe an underrecognized childhood stroke syndrome related to chronic, focal vertebral arteriopathy. Atlanto-axial instability associated with os odontoideum or atlantoaxial dislocation are causes of vertebral artery dissection treatable with arthrodesis.4,5 Presence of an arcuate foramen, an anatomical variation in which the atlas vertebral artery groove is covered by a bony ridge, is also associated with vertebral arteriopathy and childhood stroke.6,7 During open surgery, adjacent ruptured joint capsule, ruptured bursa, or bands of scar tissue were observed in 6 of our cases. We speculate that adjacent cervical bony or soft tissue pathology can exert mechanical compression or impingement of the V3 segment during head rotation after an initial event, resulting in poor arterial healing and, frequently, stroke recurrence.
This syndrome is important to identify because it is relevant to prognosis and may influence management. Eight of 10 children sustained an ischemic recurrence after the index stroke, including 3 with basilar thrombosis, an event with potentially high morbidity. In comparison, only 2 of 132 adults with vertebral artery dissection in the Cervical Artery Dissection in Stroke Study had an ischemic recurrence during 12 months of follow-up.8
We observed a striking sex disparity. All 10 children were boys, as were the 7 children in the Dallas series.3 Pediatric stroke overall is more common among boys.9 Our series also suggests a possible familial vulnerability. Two boys were brothers, and the mother of a third boy also had a posterior circulation stroke as a young adult.
Standard pediatric stroke evaluation includes cerebrovascular imaging, TTE, and hematologic tests. This series suggests a more extensive evaluation should be considered in children with posterior circulation stroke and V3 arteriopathy, particularly after recurrent ischemic events. We perform cervical flexion-extension X-rays and CT of the cervical spine to evaluate for cervical instability and bone abnormalities, and consider dynamic head-turning DSA to identify narrowing of the diseased vertebral artery segment during head rotation.
Antithrombotic treatment is a standard recommendation for children with stroke and arteriopathy. The majority of boys in the Dallas series were surgically treated with C1/C2 fusion.3 We treated with cervical fusion in one case with cervical instability. If rotational narrowing or occlusion is seen at the site of the arteriopathy, we recommend antithrombotics and activity restriction. In some cases, we utilized a cervical collar to limit the degree of head rotation as a temporizing measure until follow-up imaging or while considering treatment options. If stroke recurs despite these interventions, we consider additional surgical options. In children with robust contralateral vertebral artery flow and an intact circle of Willis, we consider endovascular vertebral artery occlusion to remove the embolic source. As an alternative to preserve the vertebral artery, we consider surgical decompression of the cervical artery,6,10 an approach similar to adults with bow-hunter syndrome.6,10
Our series was observational and has limitations. The children were treated after extensive discussions within our multidisciplinary team and counseling of the unknown risk–benefit of these options to families. Treatments were not randomized. We do not have controls for comparison. Our observations may not be widely generalizable, and we do not know the optimal strategies to prevent stroke recurrence.
Bony or soft-tissue cervical anomalies may be an underlying cause of chronic V3 vertebral arteriopathy in boys, conveying high risk for recurrent stroke. Cervical bone imaging and angiography with head rotation aid with diagnosis, although the best strategies for secondary stroke prevention remain unclear.
Glossary
- DSA
digital subtraction angiography
- TTE
transthoracic echocardiogram
Appendix. Authors
Study funding
No targeted funding reported.
Disclosure
C.K. Fox, H.J. Fullerton, S.W. Hetts, V.V. Halbach, K.I. Auguste, and M.T. Lawton report no disclosures relevant to the manuscript. N. Gupta is a consultant for Oscine Therapeutics and Y-mAbs Therapeutics. Go to Neurology.org/N for full disclosures.
References
- 1.Toole JF, Tucker SH. Influence of head position upon cerebral circulation: studies on blood flow in cadavers. Arch Neurol 1960;2:616–623. [DOI] [PubMed] [Google Scholar]
- 2.Brown BSJ, Tatlow WF. Radiographic studies of the vertebral arteries in cadavers: effects of position and traction on the head. Radiology 1963;81:80–88. [DOI] [PubMed] [Google Scholar]
- 3.Rollins N, Braga B, Hogge A, Beavers S, Dowling M. Dynamic arterial compression in pediatric vertebral arterial dissection. Stroke 2017;48:1070–1073. [DOI] [PubMed] [Google Scholar]
- 4.Fukuda M, Aiba T, Akiyama K, Nishiyama K, Ozawa T. Cerebellar infarction secondary to os odontoideum. J Clin Neurosci 2003;10:625–626. [DOI] [PubMed] [Google Scholar]
- 5.Nandish HS, Borkar SA, Kale SS, Sharma BS, Mahapatra AK. Pediatric posterior cerebral artery stroke as a presentation of atlantoaxial dislocation. J Pediatr Neurosci 2015;10:149–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cushing KE, Ramesh V, Gardner-Medwin D, et al. Tethering of the vertebral artery in the congenital arcuate foramen of the atlas vertebra: a possible cause of vertebral artery dissection in children. Dev Med Child Neurol 2001;43:491–496. [DOI] [PubMed] [Google Scholar]
- 7.Greiner HM, Abruzzo TA, Kabbouche M, Leach JL, Zuccarello M. Rotational vertebral artery occlusion in a child with multiple strokes: a case-based update. Childs Nerv Syst 2010;26:1669–1674. [DOI] [PubMed] [Google Scholar]
- 8.Markus HS, Levi C, King A, Madigan J, Norris J; Cervical Artery Dissection in Stroke Study Investigators. Antiplatelet therapy vs anticoagulation therapy in cervical artery dissection: the Cervical Artery Dissection in Stroke Study (CADISS) randomized clinical trial final results. JAMA Neurol 2019;76:657–664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Golomb MR, Fullerton HJ, Nowak-Gottl U, Deveber G; International Pediatric Stroke Study Group. Male predominance in childhood ischemic stroke: findings from the international pediatric stroke study. Stroke 2009;40:52–57. [DOI] [PubMed] [Google Scholar]
- 10.Zaidi HA, Albuquerque FC, Chowdhry SA, Zabramski JM, Ducruet AF, Spetzler RF. Diagnosis and management of bow hunter's syndrome: 15-year experience at Barrow Neurological Institute. World Neurosurg 2014;82:733–738. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Anonymized data not published within the article are available from the corresponding author upon reasonable request from any qualified investigator.