Abstract
Objective
To characterize the cortical macrostructure and microstructure of behavioral and cognitive changes along the amyotrophic lateral sclerosis (ALS)–frontotemporal dementia (FTD) continuum.
Methods
We prospectively recruited 88 participants with a 3T MRI structural and diffusion-weighted imaging sequences: 31 with ALS, 20 with the behavioral variant of FTD (bvFTD), and 37 cognitively normal controls. Participants with ALS underwent a comprehensive cognitive and behavioral assessment and were dichotomized into ALS without cognitive or behavioral impairment (ALSno-cbi; n = 12) and ALS with cognitive or behavioral impairment (ALScbi; n = 19). We computed cortical thickness and cortical mean diffusivity using a surface-based approach and explored the cortical correlates of cognitive impairment with the Edinburgh Cognitive and Behavioral ALS Screen.
Results
The ALSno-cbi and ALScbi groups showed different patterns of reduced cortical thickness and increased cortical mean diffusivity. In the ALSno-cbi group, cortical thinning was restricted mainly to the dorsal motor cortex. In contrast, in the ALScbi group, cortical thinning was observed primarily on frontoinsular and temporal regions bilaterally. There were progressive cortical mean diffusivity changes along the ALSno-cbi, ALScbi, and bvFTD clinical continuum. Participants with ALS with either cognitive or behavioral impairment showed increased cortical mean diffusivity in the prefrontal cortex in the absence of cortical thickness.
Conclusions
Cortical mean diffusivity might be a useful biomarker for the study of extramotor cortical neurodegeneration in the ALS-FTD clinical spectrum.
Classification of evidence
This study provides Class III evidence that the cortical microstructure correlates with cognitive impairment in the ALS-FTD continuum.
Amyotrophic lateral sclerosis (ALS) is the most common form of motor neuron disease and is clinically characterized by progressive weakness due to upper and lower motor neuron degeneration.1 Although ALS was historically considered a selective motor system disorder, both clinical and postmortem studies suggest that ALS should be considered within a disease spectrum together with frontotemporal dementia (FTD).1,2 From a pathologic perspective, TAR DNA-binding protein 43 (TDP-43) aggregates are often found in the brain of both patients with ALS and those with FTD, and a sequential staging of pathology progression through the CNS has been described.3 From a clinical perspective, the characterization of cognitive and behavioral changes in ALS is crucial due to its impact on prognosis,4,5 decision-making, and engagement in end-of-life and legal decisions.6 In the last decade, it has become clear that cognitive or behavioral impairment is observed in nearly 50% of patients with ALS when patients are evaluated with specifically designed tools such as the Edinburgh Cognitive and Behavioral ALS Screen (ECAS).7,8
However, the relationship between extramotor cerebral changes (i.e., cortical thickness, TDP-43 deposition, or synaptic loss) and cognitive and behavioral impairment in the ALS-FTD continuum is under debate.8–11 Neuroimaging techniques represent valuable tools for the study of extramotor cortical changes in ALS and may provide essential insights into the cortical underpinnings of nonmotor features in the ALS-FTD continuum.12,13 However, previous neuroimaging studies investigating the structural correlates of cognitive and behavioral impairment have failed to define a consistent topography of extramotor involvement.14–16 One limitation of previous studies is the application of neuroimaging techniques that may not capture the earliest cortical changes driving cognitive and behavioral impairment in ALS such as gray matter density or cortical thickness. In addition, previous studies using diffusion tensor imaging have focused on the microstructural properties of white matter due to the technical difficulties of studying the cortical microstructure.17–19 Recently, we have proposed that diffusion tensor imaging can be used to measure cortical microstructural changes using the mean diffusivity metric. Cortical mean diffusivity captures the average amount of diffusion of water molecules at the cerebral cortex. It is a measure of cortical microstructure integrity and has proved to be a sensitive tool for the study of the earliest cortical changes in neurodegenerative diseases, including the behavioral variant of FTD (bvFTD).20–22 We hypothesized that this novel neuroimage metric could also be applied for the objective quantification of extramotor cortical changes in ALS. This information may be of great interest to enrich ALS classification systems.23
In this study, our aim was to investigate the cortical correlates of cognitive and behavioral impairment along the ALS-FTD clinical continuum with a novel surface-based approach, cortical mean diffusivity.
Methods
Standard protocol approvals, registrations, and patient consent
The study was approved by the local ethics committee and was conducted following the Declaration of Helsinki. All participants gave their written informed consent to participate in the study.
Study participants and classification
Participants in this study were prospectively recruited at both the memory unit and the motor neuron disease clinic of Hospital de Sant Pau in Barcelona from December 2015 to May 2019. Inclusion criteria were diagnosis of motor neuron disease fulfilling El Escorial revised criteria for probable, probable laboratory-supported, or definite ALS and 3T MRI available for surface-based analysis. We selected a group of age-matched cognitively normal controls from the Sant Pau Initiative on Neurodegeneration cohort24 (santpaumemoryunit.com/our-research/spin-cohort/) with suitable 3T MRI for cortical mean diffusivity analyses. This group of controls has previously been reported in a multicenter study.20 Finally, to evaluate the other end of the ALS-FTD spectrum, we included the subgroup of participants diagnosed with bvFTD at our center in a previous multicenter study.20 In particular, we included participants with bvFTD with any of the following: progressive functional deterioration during follow-up, emergence of a secondary frontotemporal lobar degeneration (FTLD)–related syndrome, or pathologic or genetic confirmation of FTLD. All participants in the bvFTD group met diagnostic criteria for probable or definitive bvFTD at diagnosis, and none had a concurrent diagnosis of ALS-FTD during follow-up.25,26
Participants with ALS underwent a cognitive and behavioral screening that included a separate interview with a reliable informant and the administration of the ECAS.27 A group of patients with ALS and cognitive or behavioral impairment (ALScbi) was defined to include patients with ALS and at least 1 of the following features: (1) at least 1 abnormal score (<1.5 SDs) on the fluency, language, and executive scores of the ECAS, according to normative data in the Spanish population (data available from Dryad, supplementary table, doi.org/10.5061/dryad.51c59zw5g)28; (2) at least 1 behavioral feature from the bvFTD diagnostic criteria at the time of diagnosis; and (3) verified criteria for both ALS and bvFTD (ALS-FTD).29 The remaining participants with ALS were classified as ALS without cognitive or behavioral impairment (ALSno-cbi).
Sample composition
Figure 1 shows a diagram flow of sample composition. We included 88 participants in this study: 31 with ALS, 20 with bvFTD, and 37 cognitively normal controls. Among patients with ALS, 19 were classified in the ALScbi group and 12 in the ALSno-cbi group.
Figure 1. Diagram flow of the sample composition.
Participants in the behavioral variant of frontotemporal dementia (bvFTD) and control groups have been previously reported by Illán-Gala I et al.20 ALS = amyotrophic lateral sclerosis; DTI = diffusion tensor imaging; PLS = primary lateral sclerosis; PMA = progressive muscular atrophy.
Cognitive, behavioral, and disease-staging measures
A behavioral neurologist with expertise in the evaluation of patients with FTD (I.I.-G.) evaluated all the patients after a comprehensive clinical and behavioral assessment that included the administration of the ECAS test to participants with ALS. The ECAS is a brief cognitive test that has been specifically designed and validated for the evaluation of cognitive and behavioral features in patients with ALS (ecas.psy.ed.ac.uk/).7,30 This cognitive test assesses the following domains: executive function (reverse digit span, alternation, inhibitory sentence completion, social cognition), word fluency (free words beginning with 1 letter and restrained words beginning with 1 letter but with only 4 letters), language (naming, comprehension, and spelling), memory (immediate recall of a short story, delayed percentage retention, and delayed recognition), and visuospatial functions (dot counting, cube counting, and number location).7,30 An ALS-specific score is calculated as the sum of executive function, fluency, and language scored. An ALS-nonspecific score is also calculated as the sum of memory and visuospatial functions. The total ECAS score is calculated as the sum of all subtests. For each participant, behavioral abnormalities were noted by integrating the information obtained in both a separate structured interview with a reliable informant and the clinical interview with the patient. We determined the number of behavioral features that each participant met from the bvFTD diagnostic criteria: disinhibition, apathy or inertia, compulsive or repetitive behaviors, changes in eating behavior, and lack of empathy.20
In the ALS group, we also obtained the revised Amyotrophic Lateral Sclerosis Functional Rating Scale–Revised score at the time of MRI acquisition. We defined disease onset as the time when the first symptom was observed (cognitive/behavioral or motor) according to the information provided by the patient or the informants. In addition, we obtained the Mini-Mental State Examination score as a general measure of cognitive impairment in all clinical groups.
Genetic analysis
All patients were screened for the C9orf72 expansion. Patients with familial history of neurodegenerative diseases or psychiatric illness were also screened for other known causal genes of FTLD (C9orf72, MAPT, GRN) and ALS (TBK1, VCP, TARDBP, and SOD1). Mutations were found in C9orf72 (n = 5), GRN (n = 1), VCP (n = 1), and SOD1 (n = 1).
MRI acquisition
Seventy-five participants were scanned on a 3T Philips Achieve (Best, the Netherlands) using a T1-weighted magnetization-prepared rapid gradient echo protocol with a repetition time of 8.1 milliseconds, echo time of 3.7 milliseconds, 160 slices, and a voxel size of 0.94 × 0.94 × 1 mm. Thirteen participants were scanned on a different 3T Philips Achieva using a T1-weighted magnetization-prepared rapid gradient echo protocol with a repetition time of 6.74 milliseconds, echo time of 3.14 milliseconds, 140 slices, and a voxel size of 0.9 × 0.9 × 1.2 mm.
Cortical thickness and cortical mean diffusivity processing
Surface-based cortical reconstruction was performed with FreeSurfer version 5.1 software package (surfer.nmr.mgh.harvard.edu). We used a previously described homemade surface-based approach to process cortical diffusion MRI.20,21 As we have shown in previous works, surface-based methods can accurately measure microstructural changes in other neurodegenerative diseases.21,31 A significant advantage of these methods is the mitigation of partial volume effects or kernel-sensitive CSF signal inclusion during the smoothing step.32 Briefly, we first corrected diffusion-weighted imaging data for motion effects by applying a rigid body transformation, and nonbrain tissue was removed with the Brain Extraction Tool. Next, we fitted diffusion tensors and computed mean diffusivity using the FSL dtifit command. Finally, we computed the affine transformation between the skull-stripped b0 and the segmented T1-weighted volume with a boundary-based algorithm using bbregister (as implemented in FreeSurfer). This approach takes advantage of the precise segmentation of the white matter surface and pial surface in FreeSurfer to accurately register the b0 and the T1-weighted image. Visual inspection was done by an expert in neuroimage processing (V.M.) blinded to the patients' diagnoses, and participants with erroneous coregistration were excluded. Then, we sampled the mean diffusivity volume of each participant at the midpoint of the cortical ribbon (half the distance between the white matter surface and the gray matter surface) and projected mean diffusivity volume to each individual surface reconstruction obtained during the FreeSurfer processing with mri_vol2surf command. By doing this, we were able to create a surface map of cortical mean diffusivity for each participant. All individual cortical mean diffusivity maps were normalized to an average standard surface using a spherical registration to enable an accurate interparticipant matching of cortical locations for the statistical analyses. We applied a gaussian kernel of 15 mm, consistent with our previous work with cortical mean diffusivity.33,34
Neuroimage analyses
We first performed group analyses for both cortical thickness and cortical mean diffusivity, with a 2-class general linear model (as implemented in FreeSurfer version 5.1) between healthy controls and participants with ALS with impaired ALS-specific cognitive measures: impaired fluency (n = 10), language (n = 7), executive (n = 8), and ALS-specific score (n = 9). Similarly, participants with ALS with behavioral impairment were compared to healthy controls (n = 11). We introduced age, sex, education, and magnetic resonance equipment as covariates in all group comparisons. To control for false positives, we tested in all analyses a Monte-Carlo simulation with 10,000 repeats, as implemented in FreeSurfer (family-wise error <0.05).
We computed the Cohen d effect size metric for both cortical thickness and cortical mean diffusivity on a vertex-wise basis to obtain a topographic representation of the effect size for the group comparisons. Effect size computation was restricted to cortical regions showing statistically significant differences between participants with ALS and healthy controls.
Other statistical analysis
We assessed the differences between groups using analysis of variance or t test for continuous variables and the χ2 test for dichotomous or categorical data. Statistical significance for all tests was set at 5% (α = 0.05), and all statistical tests were 2 sided. All analyses were performed with SPSS 24 (IBM Corp, Armonk, NY).
Primary research question/classification of the evidence
Our primary research question was to compare the pattern of cortical thickness and cortical mean diffusivity along the ALS-FTD continuum with cognitively normal controls. We also explored the relationship between cortical thickness and cortical mean diffusivity with behavioral changes and cognitive performance (as measured by the ECAS test) in the ALS group. This study provides Class III evidence that cortical microstructure correlates with cognitive impairment in the ALS-FTD continuum.
Data availability
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
Results
Demographics and sample composition
Table 1 shows the demographics and clinical data of the participants. There were no differences in age at symptom onset, disease duration at MRI acquisition, or level of education between the ALS, bvFTD, and healthy control groups. There were more female participants in the control and ALS groups than in the bvFTD group. Both the ALS and the bvFTD groups showed lower Mini-Mental State Examination scores than the control group. Within the ALS group, those with ALSno-cbi were younger at symptom onset and MRI acquisition and showed longer disease duration than those with ALScbi. Conversely, we did not observe differences in sex distribution, education, and Amyotrophic Lateral Sclerosis Functional Rating Scale–Revised score at diagnosis between the ALSno-cbi and ALScbi groups. In the ALScbi group, 11 of 19 (58%) participants showed behavioral changes in at least 1 domain. In particular, disinhibition and apathy were the behavioral changes more frequently found in the ALScbi group (n = 8, 41%, and n = 6, 32%, respectively).
Table 1.
Clinical, demographic, and neuropsychological data
Cortical thickness and cortical mean diffusivity group comparisons
First, we compared the cortical thickness and cortical mean diffusivity for each group with those of healthy controls. Overall, figure 2 illustrates the existence of different patterns of cortical thickness (figure 2A) and mean diffusivity (figure 2B). We observed cortical mean diffusivity increases in the absence of cortical thinning in prefrontal regions and cortical thinning without cortical mean diffusivity increases in the motor cortex in both hemispheres.
Figure 2. Group differences in cortical thickness and cortical mean diffusivity between participants along the ALS-FTD spectrum and controls.
Group comparisons between those with amyotrophic lateral sclerosis (ALS) without cognitive or behavioral impairment (ALSno-cbi; left column), those with ALS with cognitive or behavioral impairment (ALScbi; middle column), and those with behavioral variant of frontotemporal dementia (bvFTD; right column) compared to controls for (A) cortical thickness and (B) cortical mean diffusivity. Regions in blue represent thinner cortex; regions in green represent higher cortical mean diffusivity; and regions in purple represent lower cortical mean diffusivity. All analyses were adjusted for age, sex, education, and MRI equipment. Only clusters that survived family-wise error correction p < 0.05 are shown.
Furthermore, we found a progression of cortical thickness and mean diffusivity changes along the ALS-FTD continuum (figure 2). In the ALSno-cbi group, cortical thinning was observed mainly in the primary motor cortex and in other paracentral frontal cortex and precuneus and, to a lesser extent, other posterior regions (figure 2A). In this group, we observed cortical mean diffusivity increases in the superior frontal cortex of both hemispheres and the precentral cortex (left hemisphere), paracentral frontal cortex, and lingual cortex of the right temporal lobe. Of note, we observed a small cluster with decreased mean diffusivity at the inferior frontal cortex of the right hemisphere (data available from Dryad, supplementary figure, doi.org/10.5061/dryad.51c59zw5g).
In the ALScbi group, we observed a different pattern of cortical thinning involving the insula, the temporal lobes, and the inferior frontal cortex of both hemispheres. Of note, in the ALScbi group, we observed significant cortical thinning of the motor cortex only in the inferior portion of both hemispheres. Conversely, in the ALScbi group, we observed increased cortical mean diffusivity in the insula, medial, and lateral temporal, precentral cortex, and prefrontal cortex bilaterally (including superior frontal, rostral middle frontal, lateral orbitofrontal, and anterior cingulate cortex).
Finally, in the bvFTD group, we observed cortical thinning in the prefrontal cortex, insula, cingulate gyrus, orbitofrontal cortex, anterior temporal pole, lateral and medial temporal lobe, angular gyrus, and precuneus of both hemispheres. In this group, we found widespread increases in cortical mean diffusivity along the frontal and temporal cortices, extending bilaterally to posterior regions such as the inferior parietal and occipital lobe.
Cortical thickness and cortical mean diffusivity changes in participants with ALS
Participants with ALS with behavioral impairment (n = 11) did not show cortical thinning compared to healthy controls (figure 3A). However, we observed significant cortical mean diffusivity increases in the superior frontal, prefrontal dorsolateral, insula, anterior cingulate, medial temporal lobe, and precuneus of both hemispheres (figure 3A).
Figure 3. Group differences in cortical thickness and cortical mean diffusivity in participants with ALS with behavioral impairment and abnormal ALS-specific cognitive score.
(A) Group comparison between participants with amyotrophic lateral sclerosis (ALS) with behavioral impairment (n = 11) and controls. (B) Group comparison between participants with ALS with abnormal ALS-specific cognitive score (n = 9) and controls. All analyses were adjusted for age, sex, education, and MRI equipment. Only clusters that survived family-wise error correction p < 0.05 are shown.
We then compared the differences in cortical thickness and cortical mean diffusivity between participants with ALS with impaired ALS-specific cognitive score (n = 13). As shown in figure 3B, in participants with ALS with impaired ALS-specific score, we found reduced cortical thickness only in the left insula. However, these participants showed cortical mean diffusivity increases in the superior frontal, premotor cortex, precuneus, and middle temporal lobe (figure 3B).
Cortical thickness and cortical mean diffusivity correlates of ALS-specific cognitive domains
To further investigate the cortical correlates of cognitive impairment in participants with ALS, we compared cortical thickness and cortical mean diffusivity between healthy controls and each subgroup of participants with ALS with abnormal scores in ALS-related cognitive domains (fluency, language, and executive function scores). As figure 4A shows, participants with ALS with decreased fluency scores (n = 10) showed cortical thinning only in the right insula. However, these participants displayed significant increases in mean diffusivity in the superior frontal, middle temporal lobe, and premotor cortex (including caudal middle frontal) in the left hemisphere. As shown in figure 4B, participants with ALS with abnormal language scores (n = 7) showed cortical thinning in the insula, anterior cingulate, and superior temporal lobe of both hemispheres. However, in this group of participants, we observed cortical mean diffusivity increases in the insula, superior frontal, premotor cortex, and medial temporal lobe (both hemispheres), anterior cingulate (left hemisphere), and precuneus (right hemisphere). Finally, participants with ALS with abnormal scores on executive function displayed cortical thinning in the insula, superior temporal, and precuneus of both hemispheres (figure 4C). However, cortical mean diffusivity was also observed in these regions and extended to the superior temporal and premotor cortex of both hemispheres.
Figure 4. Group differences in cortical thickness and cortical mean diffusivity in participants with ALS with abnormal fluency, language, and executive scores.
(A) Group comparison between participants with amyotrophic lateral sclerosis (ALS) with abnormal fluency score (n = 10) and controls; (B) group comparison between participants with ALS with abnormal language score (n = 7) and controls; and (C) group comparison between participants with ALS with an abnormal executive score (n = 8) and controls. All analyses were adjusted for age, sex, education, and center. Only clusters that survived family-wise error correction p < 0.05 are shown.
Discussion
In this study, we compared the pattern of cortical thickness and cortical mean diffusivity changes along the ALS-FTD continuum. The main findings of this study are as follows: (1) the ALSno-cbi, ALScbi, and bvFTD groups displayed different patterns of reduced cortical thickness and a continuum of cortical mean diffusivity changes (minimal in ALSno-cbi and maximal in bvFTD); (2) those with ALSno-cbi and ALScbi displayed cortical mean diffusivity changes in extramotor regions in the absence of cortical thinning, suggesting that cortical mean diffusivity may capture subtle microstructural changes antedating gray matter loss; and (3) the subgroups of participants with ALScbi showed partially overlapping cortical mean diffusivity increases in extramotor regions extending beyond regions with significant cortical thinning.
We found different patterns of cortical thinning along the ALS-FTD continuum. In the ALSno-cbi group, we observed cortical thinning of the motor cortex with the preservation of operculum and frontoinsular regions. Conversely, in the ALScbi group, we observed cortical thinning at the left operculum, bilateral insula, and temporal cortex (medial and lateral). At the extreme of the ALS-FTD spectrum, participants with bvFTD showed extensive cortical thinning in the frontal, temporal, and more posterior areas, consistent with previous reports.20 The observed differences in the topography of neurodegeneration between the ALSno-cbi and ALScbi groups support earlier observations of a distinct phenotype in ALS with FTD that is characterized by severe and predominantly affected bulbar and distal upper limb muscles.35 This motor phenotype corresponds well with the observed neurodegeneration in the ALScbi, affecting cortical motor areas of the motor homunculus related to bulbar weakness and extramotor features.35 Conversely, the ALSno-cbi group showed a pattern of neurodegeneration involving dorsal motor areas and minimal extramotor involvement, in agreement with the lower frequency of bulbar presentation in this group.12 Of note, when we compared the cortical thickness of all ALS groups with controls, we found cortical thinning in the primary motor cortex and inferior frontal, in agreement with previous meta-analyses of neuroimaging studies.14
We also report large increases in cortical mean diffusivity in the prefrontal cortex of ALScbi. Higher cortical mean diffusivity reflects microstructural disorganization and disruption of cellular membranes and has been proposed to antedate macroscopic cortical changes.22 In previous studies, we suggested that cortical mean diffusivity may be a sensitive tool for the study of subtle microstructural changes at the cortex of other neurodegenerative diseases.20–22
Of note, in the ALSno-cbi group, we observed a small cluster with decreased mean diffusivity at the inferior frontal cortex of the right hemisphere. This is an interesting finding because decreased cortical mean diffusivity has also been observed in the preclinical stage of Alzheimer disease when amyloidosis and inflammatory changes occur in the absence of tau and neurodegeneration.21,36 We hypothesize that in ALS these changes may reflect early inflammation and astroglial activation, while increased mean diffusivity may reflect early neurodegeneration and synapse and tissue integrity loss.37,38 Further multimodal biomarker studies should explore the specific correlate of cortical mean diffusivity decreases in extramotor regions in ALS.
In this study, we applied a specifically designed and previously validated cognitive test to investigate the cortical correlates of ALS-related cognitive impairment along the ALS-FTD clinical continuum. This test has shown to overcome some of the problems and limitations of cognitive evaluation in patients with ALS.7 Our findings suggest that cortical mean diffusivity may be more sensitive than cortical thickness to capture the pathologic substrate of cognitive impairment. Of note, we found cortical mean diffusivity increases in both medial temporal and posterior regions, in agreement with the observed occipital hypometabolism in patients with ALS39 and similar to the posterior cortical mean diffusivity changes that have previously been observed in bvFTD.20
On the other hand, the relative scarcity of regions showing cortical thinning in our study deserves further comment. In participants with ALS with impaired ALS-specific score, we found significant cortical thinning only in the left insula. This region has been related to phonologic, executive functions, and theory-of-mind measures in patients with bvFTD.40 Although some studies have found significant correlations of cognitive function in patients with ALS, other studies have found significant relationships only with white matter microstructure.17,18 Our results are in agreement with a recent pathology-confirmed study of a cognitively characterized ALS cohort in whom cortical thickness and synapse loss were quantified in the prefrontal cortex of path-confirmed ALS cases.41 In this study, synapse loss at the prefrontal cortex, not cortical thickness, correlated with premortem cognitive performance as assessed by the ECAS test.41 Prefrontal hypometabolism has proved to be an independent predictor of shorter survival in ALS.42 Taking the findings of this study together with our previous report, we hypothesize that the cortical microstructure could be capturing early synapse loss in the prefrontal cortex of patients with ALS, and we speculate that these changes could have prognostic implications. Further studies should explore the relationship between gray and white matter microstructure by combining our approach with conventional measures of white matter microstructure. This would be an important step to unveil the specific contribution of both cortical and subcortical structures to motor, cognitive, and behavioral impairment in ALS. In addition, longitudinal and pathology-confirmed studies are needed to determine the neuropathologic underpinnings of cortical mean diffusivity and its relationship with neuroinflammation and TDP-43 aggregate distribution.
The main strengths of this study are the prospective inclusion of participants from the whole ALS-FTD clinical spectrum; the thorough characterization of the motor, cognitive, and behavioral features of the participants; and the surface-based analysis using a previously validated technique to study the cortical microstructure. This surface-based approach allowed us to explore the cortical microstructure in the ALS-FTD continuum and solves some of the limitations and methodologic concerns that have previously been reported with the use of a voxel-based approach to investigate cortical microstructure.32 Both participants with ALS and those with bvFTD were prospectively recruited in the same center and comprehensively characterized by a clinician with expertise in cognitive and behavioral neurology and experts in motor neuron diseases following a standardized protocol. Nevertheless, this approach resulted in a small sample size, which is the main limitation of this study. We also acknowledge that participants with ALScbi could be overrepresented in our sample for several reasons. Some participants with ALS did not participate in the study because they were unable to perform MRI as a result of intolerance of the supine position due to diaphragm weakness (figure 1). Because the availability of MRI was an inclusion criterion, this could also have affected the composition of the ALS group. In addition, the protocol in our center includes assessment by motor neuron disease specialists of all patients with suspected FTD and the assessment by behavioral neurologists of patients with motor neuron disease. These factors also could have resulted in a higher detection rate of motor neuron disease cases with cognitive and behavioral symptoms and could limit the generalization of our results.
This study provides evidence suggesting the existence of a neurodegeneration continuum between ALS and FTLD and suggests that cortical mean diffusivity may be more sensitive than cortical thickness for the detection of the cortical changes responsible for cognitive and behavioral impairment in the ALS-FTD clinical spectrum. Taken together, our results support the role of cortical mean diffusivity as a potentially valuable neuroimaging biomarker for the study of ALS-related neurodegeneration.
Acknowledgment
The authors thank the patients and their relatives for their support for this study.
Glossary
- ALS
amyotrophic lateral sclerosis
- ALScbi
ALS with cognitive or behavioral impairment
- ALSno-cbi
ALS without cognitive or behavioral impairment
- bvFTD
behavioral variant of FTD
- ECAS
Edinburgh Cognitive and Behavioral ALS Screen
- FTD
frontotemporal dementia
- FTLD
frontotemporal lobar degeneration
- TDP-43
TAR DNA-binding protein 43
Appendix. Authors
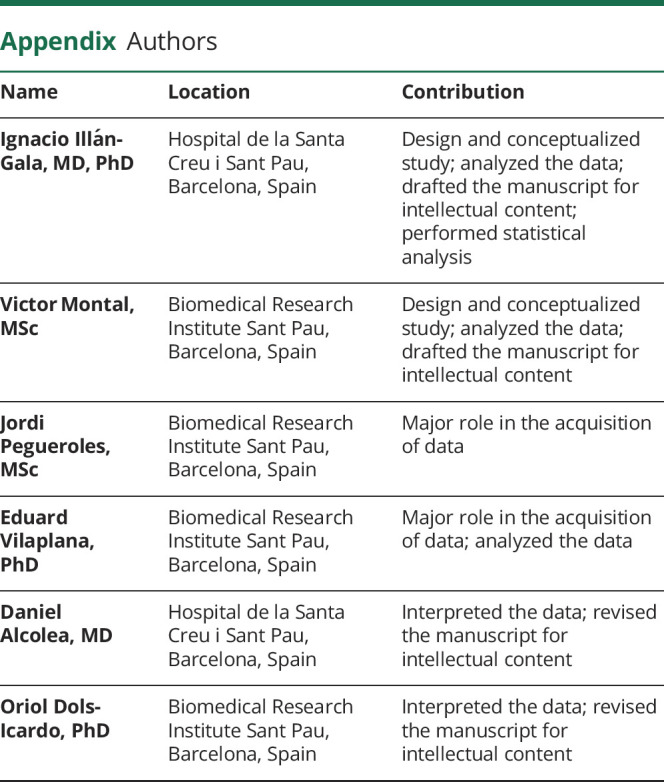

Footnotes
Class of Evidence: NPub.org/coe
Study funding
This study was supported by the Fondo de Investigaciones Sanitario, Instituto de Salud Carlos III (PI14/01126 and PI17/01019 to J.F., PI13/01532 and PI16/01825 to R.B., INT19/00016 and PI18/00435 to D.A., PI15/01618 to R.R.-G., PI14/1561, PI18/00326 to J.C., and PI17/01896 to A.L.) and the CIBERNED program (Program 1, Alzheimer Disease to A.L. and SIGNAL study, signalstudy.es), jointly funded in part by Fondo Europeo de Desarrollo Regional, Unión Europea, “Una manera de hacer Europa.” This work was also supported by the NIH (National Institute on Agiging grants 1R01AG056850-01A1, R21AG056974, and R01AG061566 to J.F.), Departament de Salut de la Generalitat de Catalunya, Pla Estratègic de Recerca i Innovació en Salut (SLT002/16/00408 to A.L.), Fundació La Marató de TV3 (20141210 to J.F., 044412 to R.B., and 201437.10 to R.R.-G.), Fundación Española para el Fomento de la Investigación de la Esclerosis Lateral Amiotrófica FUNDELA, and the Agency for Management of University and Research Grant (2017 SGR 547 to J.C.). I. Illán-Gala is supported by the Rio Hortega grant (CM17/00074) from “Acción Estratégica en Salud 2013–2016” and the European Social Fund and the Global Brain Health Institute (Atlantic Fellow for Equity in Brain Health). O. Dols-Icardo is funded by the Association for Frontotemporal Degeneration (Clinical Research Postdoctoral Fellowship, AFTD 2019–2021). This work was also supported by Generalitat de Catalunya (SLT006/17/00119 to J.F. and SLT006/17/125 to D.A.) and a grant from the Fundació Bancaria La Caixa to R. Blesa.
Disclosure
I. Illán-Gala, V. Montal, J. Pegueroles, and E. Vilaplana report no disclosures. D. Alcolea participated in advisory boards for Fujirebio-Europe and Roche Diagnostics and received speaker honoraria from Fujirebio-Europe, Nutricia, and Krka Farmacéutica S.L. Dr. Alcolea declares a filed patent application (WO2019175379 A1, Markers of Synaptopathy in Neurodegenerative Disease). O. Dols-Icardo, N. de Luna, —J. Turón-Sans, E. Cortés-Vicente, L. Martinez-Roman, M.B. Sánchez-Saudinós, A. Subirana, L. Videla, I. Sala, I. Barroeta, S. Valldeneu, R. Blesa, and J. Clarimón report no disclosures. A. Lleó has served on scientific advisory boards for Fujirebio-Europe, Nutricia, and Biogen and has filed a patent application for synaptic markers in neurodegenerative diseases. J. Fortea has received compensation for consultancies to Novartis and AC Immune. R. Rojas-García reports no disclosures. Go to Neurology.org/N for full disclosures.
References
- 1.Brown RH, Al-Chalabi A. Amyotrophic lateral sclerosis. N Engl J Med 2017;377:162–172. [DOI] [PubMed] [Google Scholar]
- 2.Al-Chalabi A, Jones A, Troakes C, King A, Al-Sarraj S, van den Berg LH. The genetics and neuropathology of amyotrophic lateral sclerosis. Acta Neuropathol 2012;124:339–352. [DOI] [PubMed] [Google Scholar]
- 3.Brettschneider J, Arai K, Del Tredici K, et al. TDP-43 pathology and neuronal loss in amyotrophic lateral sclerosis spinal cord. Acta Neuropathol 2014;128:423–437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Elamin M, Phukan J, Bede P, et al. Executive dysfunction is a negative prognostic indicator in patients with ALS without dementia. Neurology 2011;76:1263–1269. [DOI] [PubMed] [Google Scholar]
- 5.Elamin M, Bede P, Byrne S, et al. Cognitive changes predict functional decline in ALS: a population-based longitudinal study. Neurology 2013;80:1590–1597. [DOI] [PubMed] [Google Scholar]
- 6.Merrilees J, Klapper J, Murphy J, Lomen-Hoerth C, Miller BL. Cognitive and behavioral challenges in caring for patients with frontotemporal dementia and amyotrophic lateral sclerosis. Amyotroph Lateral Scler 2010;11:298–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Niven E, Newton J, Foley J, et al. Validation of the Edinburgh Cognitive and Behavioural Amyotrophic Lateral Sclerosis Screen (ECAS): a cognitive tool for motor disorders. Amyotroph Lateral Scler Frontotemporal Degener 2015;16:172–179. [DOI] [PubMed] [Google Scholar]
- 8.Crockford C, Newton J, Lonergan K, et al. ALS-specific cognitive and behavior changes associated with advancing disease stage in ALS. Neurology 2018;91:e1370–e1380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brettschneider J, Del Tredici K, Toledo JB, et al. Stages of pTDP-43 pathology in amyotrophic lateral sclerosis: ALS stages. Ann Neurol 2013;74:20–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cykowski MD, Powell SZ, Peterson LE, et al. Clinical significance of TDP-43 neuropathology in amyotrophic lateral sclerosis. J Neuropathol Exp Neurol 2017;76:402–413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Prudlo J, König J, Schuster C, et al. TDP-43 pathology and cognition in ALS: a prospective clinicopathologic correlation study. Neurology 2016;87:1019–1023. [DOI] [PubMed] [Google Scholar]
- 12.Geevasinga N, Menon P, Özdinler PH, Kiernan MC, Vucic S. Pathophysiological and diagnostic implications of cortical dysfunction in ALS. Nat Rev Neurol 2016;12:651–661. [DOI] [PubMed] [Google Scholar]
- 13.Christidi F, Karavasilis E, Rentzos M, Kelekis N, Evdokimidis I, Bede P. Clinical and radiological markers of extra-motor deficits in amyotrophic lateral sclerosis. Front Neurol 2018;9:1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shen D, Cui L, Fang J, Cui B, Li D, Tai H. Voxel-wise meta-analysis of gray matter changes in amyotrophic lateral sclerosis. Front Aging Neurosci 2016;8:64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chang JL, Lomen-Hoerth C, Murphy J, et al. A voxel-based morphometry study of patterns of brain atrophy in ALS and ALS/FTLD. Neurology 2005;65:75–80. [DOI] [PubMed] [Google Scholar]
- 16.Consonni M, Contarino VE, Catricalà E, et al. Cortical markers of cognitive syndromes in amyotrophic lateral sclerosis. Neuroimage Clin 2018;19:675–682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Trojsi F, Caiazzo G, Siciliano M, et al. Microstructural correlates of Edinburgh Cognitive and Behavioural ALS Screen (ECAS) changes in amyotrophic lateral sclerosis. Psychiatry Res Neuroimaging 2019;288:67–75. [DOI] [PubMed] [Google Scholar]
- 18.Menke RAL, Körner S, Filippini N, et al. Widespread grey matter pathology dominates the longitudinal cerebral MRI and clinical landscape of amyotrophic lateral sclerosis. Brain 2014;137:2546–2555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Trojsi F, Esposito F, de Stefano M, et al. Functional overlap and divergence between ALS and bvFTD. Neurobiol Aging 2015;36:413–423. [DOI] [PubMed] [Google Scholar]
- 20.Illan-Gala I, Montal V, Borrego-Ecija S, et al. Cortical microstructure in the behavioural variant of frontotemporal dementia: looking beyond atrophy. Brain 2019;142:1121–1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Montal V, Vilaplana E, Alcolea D, et al. Cortical microstructural changes along the Alzheimer's disease continuum. Alzheimers Dement 2018;14:340–351. [DOI] [PubMed] [Google Scholar]
- 22.Weston PSJ, Simpson IJA, Ryan NS, Ourselin S, Fox NC. Diffusion imaging changes in grey matter in Alzheimer's disease: a potential marker of early neurodegeneration. Alzheimers Res Ther 2015;7:47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Al-Chalabi A, Hardiman O, Kiernan MC, Chiò A, Rix-Brooks B, van den Berg LH. Amyotrophic lateral sclerosis: moving towards a new classification system. Lancet Neurol 2016;15:1182–1194. [DOI] [PubMed] [Google Scholar]
- 24.Alcolea D, Clarimon J, Carmona-Iragui M, et al. The Sant Pau Initiative on Neurodegeneration (SPIN) cohort: a data set for biomarker discovery and validation in neurodegenerative disorders. Alzheimers Dement 2019;5:597–609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rascovsky K, Hodges JR, Knopman D, et al. Sensitivity of revised diagnostic criteria for the behavioural variant of frontotemporal dementia. Brain 2011;134:2456–2477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Alcolea D, Vilaplana E, Suárez-Calvet M, et al. CSF sAPPβ, YKL-40, and neurofilament light in frontotemporal lobar degeneration. Neurology 2017;89:178–188. [DOI] [PubMed] [Google Scholar]
- 27.Illan-Gala I, Alcolea D, Montal V, et al. CSF sAPPbeta, YKL-40, and NfL along the ALS-FTD spectrum. Neurology 2018;91:e1619–e1628. [DOI] [PubMed] [Google Scholar]
- 28.Mora JS, Salas T, Fernández MC, et al. Spanish adaptation of the Edinburgh Cognitive and Behavioral Amyotrophic Lateral Sclerosis Screen (ECAS). Amyotroph Lateral Scler Frontotemporal Degener 2018;19:74–79. [DOI] [PubMed] [Google Scholar]
- 29.Strong MJ, Abrahams S, Goldstein LH, et al. Amyotrophic lateral sclerosis - frontotemporal spectrum disorder (ALS-FTSD): revised diagnostic criteria. Amyotroph Lateral Scler Frontotemporal Degener 2017;18:153–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Abrahams S, Newton J, Niven E, Foley J, Bak TH. Screening for cognition and behaviour changes in ALS. Amyotroph Lateral Scler Frontotemporal Degener 2014;15:9–14. [DOI] [PubMed] [Google Scholar]
- 31.Parker TD, Slattery CF, Zhang J, et al. Cortical microstructure in young onset Alzheimer's disease using neurite orientation dispersion and density imaging. Hum Brain Mapp 2018;39:3005–3017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Coalson TS, Van Essen DC, Glasser MF. The impact of traditional neuroimaging methods on the spatial localization of cortical areas. Proc Natl Acad Sci USA 2018;115:E6356–E6365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bejanin A, La Joie R, Landeau B, et al. Distinct interplay between atrophy and hypometabolism in Alzheimer's versus semantic dementia. Cereb Cortex 2019;29:1889–1899. [DOI] [PubMed] [Google Scholar]
- 34.La Joie R, Perrotin A, Barré L, et al. Region-specific hierarchy between atrophy, hypometabolism, and β-amyloid (Aβ) load in Alzheimer's disease dementia. J Neurosci 2012;32:16265–16273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cortes-Vicente E, Turon-Sans J, Gelpi E, et al. Distinct clinical features and outcomes in motor neuron disease associated with behavioural variant frontotemporal dementia. Dement Geriatr Cogn Disord 2018;45:220–231. [DOI] [PubMed] [Google Scholar]
- 36.Vilaplana E, Rodriguez-Vieitez E, Ferreira D, et al. Cortical microstructural correlates of astrocytosis in autosomal dominant Alzheimer disease. Neurology 2020;94:e2026–e2036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Alshikho MJ, Zürcher NR, Loggia ML, et al. Glial activation colocalizes with structural abnormalities in amyotrophic lateral sclerosis. Neurology 2016;87:2554–2561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Alshikho MJ, Zürcher NR, Loggia ML, et al. Integrated magnetic resonance imaging and [11 C]-PBR28 positron emission tomographic imaging in amyotrophic lateral sclerosis. Ann Neurol 2018;83:1186–1197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pagani M, Chiò A, Valentini MC, et al. Functional pattern of brain FDG-PET in amyotrophic lateral sclerosis. Neurology 2014;83:1067–1074. [DOI] [PubMed] [Google Scholar]
- 40.Baez S, Pinasco C, Roca M, et al. Brain structural correlates of executive and social cognition profiles in behavioral variant frontotemporal dementia and elderly bipolar disorder. Neuropsychologia 2019;126:159–169. [DOI] [PubMed] [Google Scholar]
- 41.Henstridge CM, Sideris DI, Carroll E, et al. Synapse loss in the prefrontal cortex is associated with cognitive decline in amyotrophic lateral sclerosis. Acta Neuropathol 2018;135:213–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Van Laere K, Vanhee A, Verschueren J, et al. Value of 18fluorodeoxyglucose-positron-emission tomography in amyotrophic lateral sclerosis: a prospective study. JAMA Neurol 2014;71:553–561. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets analyzed during the current study are available from the corresponding author on reasonable request.







