Abstract
Novel corona virus disease 2019 (COVID-19), which first emerged in December 2019, has become a pandemic. This study aimed to investigate the associations between meteorological factors and COVID-19 incidence and mortality worldwide. This study included 1,908,197 confirmed cases of and 119,257 deaths from COVID-19 from 190 countries between 23 January and 13 April, 2020. We used a distributed lag non-linear model with city-/country-level random intercept to investigate the associations between COVID19 incidence and daily temperature, relative humidity, and wind speed. A series of confounders were considered in the analysis including demographics, socioeconomics, geographic locations, and political strategies. Sensitivity analyses were performed to examine the robustness of the associations. The COVID-19 incidence showed a stronger association with temperature than with relative humidity or wind speed. An inverse association was identified between the COVID-19 incidence and temperature. The corresponding 14-day cumulative relative risk was 1.28 [95% confidence interval (CI), 1.20–1.36] at 5 °C, and 0.75 (95% CI, 0.65–0.86) at 22 °C with reference to the risk at 11 °C. An inverse J-shaped association was observed between relative humidity and the COVID-19 incidence, with the highest risk at 72%. A higher wind speed was associated with a generally lower incidence of COVID-19, although the associations were weak. Sensitivity analyses generally yielded similar results. The COVID-19 incidence decreased with the increase of temperature. Our study suggests that the spread of COVID-19 may slow during summer but may increase during winter.
Keywords: COVID-19 incidence, COVID-19 mortality, Meteorology, Temperature, Relative humidity, Wind speed
Graphical abstract
1. Introduction
The coronavirus disease 2019 (COVID-19), caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), emerged in Wuhan, China, in December 2019. Although most countries have implemented a series of large-scale intervention programmes, the number of COVID-19 cases and related deaths continue to increase dramatically. The World Health Organization has declared COVID-19 as a pandemic since 11 March, 2020. As of 15 Oct, 2020, approximate 39 million confirmed cases including an estimate of 1.1 million deaths have been reported in 235 countries/areas/territories (World Health Organization, 2020). The COVID-19 outbreak has aroused unprecedented public health concern worldwide.
It has been demonstrated that meteorological factors, including temperature, relative humidity, and wind speed, may be associated with evolving transmission of known coronavirus diseases, such as severe acute respiratory syndrome (SARS), and Middle East respiratory syndrome coronavirus (MERS-CoV) (Donnelly et al., 2003; Nair et al., 2011). Laboratory experiments have indicated that SARS-CoV-2 is highly stable in cold environments but sensitive to increased temperature (Chin et al., 2020). Evidence regarding the effects of ambient meteorological factors on COVID-19 incidence/mortality are controversial. Some epidemiological/ecological studies have reported a negative association between temperature and the number of confirmed COVID-19 cases in one specific country, including China (J Liu et al. 2020; Qi et al., 2020; Shi et al., 2020a), Brazil (Prata et al., 2020), the United States (Runkle et al., 2020), Turkey (Sahin, 2020) and other countries (Abdollahi and Abdollahi and Rahbaralam, 2020). In contrast, other studies have observed positive associations (Ahmadi et al., 2020; Bashir et al., 2020; Tosepu et al., 2020; Zhu and Zhu and Xie, 2020) or no association (Yao et al., 2020). The inconsistency may be ascribed to the relatively small sample size and short study period, in addition to the fact that most previous studies have considered a narrow range of meteorological factors. Literature on this topic from large-scale studies based on various climate zones and countries were limited and inconsistent (Awasthi et al., 2020; Baker et al., 2020; Chiyomaru and Chiyomaru and Takemoto, 2020; Islam et al., 2020; Le et al., 2020; Pan et al., 2020; Sajadi et al., 2020; Sobral et al., 2020). Furthermore, few studies have examined the potential nonlinear associations between meteorological factors and COVID-19 and the delayed effects of the meteorological factors on the incidence of COVID-19. Such information is important to allow us to understand the activity and viability of SARS-CoV-2 in the natural environment and may thus be useful in the development of appropriate strategies to control the spread of COVID-19.
We therefore conducted a study in 190 countries to investigate the associations between COVID-19 incidence and the meteorological factors including temperature, relative humidity, and wind speed.
2. Methods
2.1. Study design and participants
This time-series study included a total of 415 sites (comprising 235 cities from 10 countries and 180 countries) between 23 January, 2020 and 13 April, 2020. Information on daily number of confirmed cases and deaths from COVID-19 was derived mainly from the data repository sourced from Johns Hopkins University Centre for Systems Science and Engineering (JHU CSSE) and the Wind Financial database (WFD), both of which archive data from official websites of health ministries worldwide (Dong et al., 2020; Wind, 2020). Database of JHU CSSE is the most popular and widely used database for daily updated COVID-19 cases and deaths. This database provides open-accessed data at both country-level and state-level. But the state-level data provided by this database were limited to four countries (i.e. United States of America, Australia, Canada, and China as of 13 April, 2020). Wind is a leading financial information services industry in China, which provides accurate and real-time data through paid membership. Compared to the JHU CSSE database, WFD contains more detailed information on COVID-19 at city-/state-level in ten countries (i.e. Australia, Canada, United States of America, China, Germany, Italy, Japan, Korea, Norway and Spain). We therefore derived the COIVD-19 data from these two databases. Namely, data for the 235 cities from the ten aforementioned countries were derived from WFD, whilst data for the 180 countries were derived from JHU CSSE.
The process of data cleaning is shown in Fig. S1 in Appendix. Initially, a total of 43,197 observations from 419 study sites of 190 countries were collected between 1 Jan and 15 April, 2020. We excluded 208 observations from 4 study sites because there were no confirmed cases reported in these sites. 9130 observations were also excluded because they were before 22 Jan, 2020. We further excluded 28 observations with daily confirmed cases <0, possibly due to the adjustment for misdiagnosis of COVID-19. Finally, this study included a total of 33,831 observations from 415 sites of 190 countries.
2.2. Meteorological factors
Hourly meteorological data, including temperature, relative humidity, and wind speed were obtained from the ground-based monitoring network of the World Meteorological Organization global telecommunications system. The hourly data were then aggregated as daily average meteorological data. If a study site had more than one monitoring stations, the average values of the meteorological factors were weighted by population density using the following formula:
In which, T i is the meteorological value at the ith monitoring station and W i is the corresponding weight. W i= 1, 2, 3, 4 and 5 for an area with a population density of <10, ≥10–<100, ≥100–<1000, ≥1000–<10,000, and ≥10,000 persons/km2, respectively.
2.3. Covariates
Information on demographic and socio-economic status, geographic locations and intervention policies for each city/country was also collected, including population size (number of persons) and density (persons per square kilometre), median age (years), Global Health Security Index (GHSI) (Bannister-Tyrrell et al., 2020; Chang and McAleer, 2020; Kandel et al., 2020), and public health interventions (i.e., intervention policy on transportation restriction, large-scale testing, wearing of masks, propaganda, emergency level and social distancing). Information on population size and density and median age was obtained from United Nations, Department of Economic and Social Affairs, Population Division (Elaboration of data by United Nations, 2019), and from the countries' Statistics Bureau. The Henley Index data were collected from the International Air Transport Association ((IATA), 2020). Henley Index is a common indicator for population morbidity between countries. The GHSI data were collected from the GHSI report (Johns Hopkins, 2019). GHSI is mainly used to assess health security capabilities of a country in the following six categories: emergence prevention or pathogens release, early detection and reporting, rapid response and mitigation, patient treatment and health worker's protection, compliance with global norms, as well as risk environment. The Education Index data were obtained from the United Nations Development Programme. It is measured by the average of school years of adults and the expected school years of children. Because the Henley Index, GHSI and Education Index data are only available at the country level, we applied them to all cities within the same country. We also searched the official webpages of the 415 cities/countries and obtained information on the policy of public health interventions.
2.4. Statistical analysis
We used the distributed lag non-linear model (Gasparrini et al., 2015), a standard time-series regression model, to investigate the associations between the meteorological factors and the COVID-19 incidence. This model can present non-linear exposure-response associations between meteorological factors and health outcomes. The lag-response associations can also be examined to show the delayed effects on health. We also included the first date of reported cases to control for the variations in the beginning of COVID-19 epidemic in different countries.
In this study, negative binomial distribution was used to control potential over-dispersion. We applied the natural cubic spline function with one internal knot placed at the 50th percentile of the meteorological factors to investigate the exposure-response associations between the meteorological factors and the COVID-19 incidence. The lag-response associations were investigated using the same function with two equally spaced internal knots from 0 to 14 days (Guan et al., 2020; Lauer et al., 2020). The cumulative associations (7 consecutive days and 10 consecutive days) were presented. Various numbers of knots were also examined in the sensitivity analyses. Akaike Information Criteria was used to assess the goodness of fit and the simplicity of models.
The following covariates were included in the model: logarithm of population to offset population effects across regions, a natural cubic spline of time with 2 degree of freedom (Liu et al., 2019) to control seasonal and long-term trends over the study period, an indicator of the day of the week and public holidays to account for weekly or periodically variations in the number of people who accepted testing, and the number of confirmed cases reported on the previous day to account for temporal autocorrelation. The following city-/country-level confounders were also included: the date of the first reported cases to account for the detection time, the population density to account for the higher transmission rate in regions with a high population density, the national median age to account for the higher incidence among older adults, the GHSI to account for countries' capacity to prevent and mitigate epidemics and pandemics, the latitude and longitude to account for potential spatial autocorrelation, and the intervention policies implemented (i.e., yes vs no for whether implementing the policies of transportation restriction, large-scale nucleic acid examinations, mask wearing, propaganda strategies, declaration of public health emergency and social distancing) to account for the effectiveness of the implemented intervention.
Both cumulative and single-day relative risks (RRs) with a 95% confidence interval (CI) at the 25th and 75th percentiles of the meteorological factors were used to present the strengths of the associations. Because the associations were generally non-linear, we used overall median value of meteorological factors as the reference levels. We also plotted the exposure-response curves to show the overall associations.
A series of sensitivity analyses were performed to examine the robustness of the estimated associations: 1) we applied the same method to investigate the association between COVID-19 mortality and the meteorological factors; 2) we extended the lag period from 14 days to 23 days to examine the possible long incubation period reported in previous literature (Lauer et al., 2020); 3) we compared various numbers of knots of meteorological factors (i.e., from 2 to 4 placed at equally spaced values) to examine whether the number of knots may affect the associations; 4) we analyzed the associations by including only a single meteorological factor in the model to avoid potential correlation between these factors; 5) we investigated the associations by excluding Hubei province in China, which was a significant outlier in the model; 6) we excluded sites with the highest or lowest 5% of the values for temperature, relative humidity and wind speed to avoid potential outlying effects; 7) we excluded the covariates “mask wearing” and “propaganda” separately in the model to avoid collinear effects (the Spearman correlations coefficient for “mask wearing” and “propaganda” was 0.7); 8) we excluded 50 study sites with one or no monitoring station because population weight averages of meteorological factors were unavailable; 9) we excluded the 10 countries with the largest area (including Russian Federation, Brazil, India, Argentina, Kazakhstan, Algeria, Democratic Republic of the Congo, Saudi Arabia, Mexico and Indonesia) but without state-/province-level data to minimize the potential effects of exposure misclassification; and 10) to simplify the model and improve statistical power, linear meteorological variables (i.e., mean temperature, relative humidity and wind speed) and a shorter lag period (i.e., 7 days) were used.
All data analyses were performed using R 3.6.1 (R Core Team, Vienna, Austria) with ‘dlnm’ and ‘lme4’ packages. A two-tailed P value of <0.05 was considered statistically significant.
3. Results
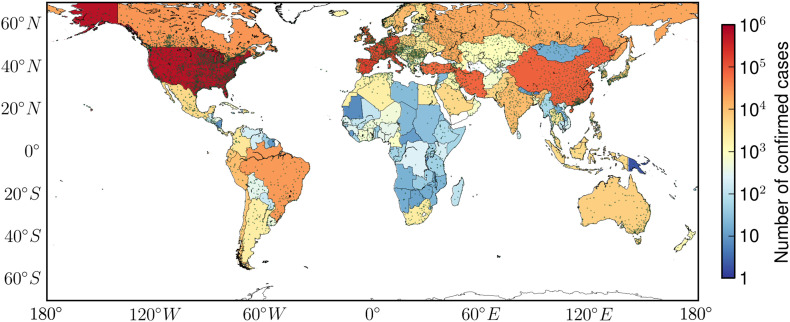
In this study, 415 sites were included in the analysis (Table S2 in Appendix A). As of 13 April, 2020, 1,908,197 confirmed cases of and 119,257 confirmed deaths from COVID-19 had been identified. The ten countries with the largest numbers of confirmed cases were the United States of America, Spain, Italy, France, Germany, The United Kingdom, China, Iran, Turkey, and Belgium. United States of America had 577,165 confirmed cases (accounting for 30.25% of total COVID-19 cases worldwide) and 23,402 deaths (accounting for 19.62% of global deaths from COVID-19). The median (interquartile range, IQR) of the daily average temperature, relative humidity and wind speed were 11 °C (5 °C–22 °C), 71% (59%–79%), and 3 m/s (2 m/s–4 m/s), respectively. Table S2 in the Appendix shows the characteristics of each country included. Fig. 1 shows the spatial distributions of cumulative confirmed cases and the ground-level meteorology monitoring stations. The 415 study sites covered four climate zones, including cold (e.g., Canada), temperate (e.g., the United Kingdom), subtropical (e.g., South Africa) and tropical (e.g., Singapore). Fig. S2 presents the time-series plots of daily confirmed cases, deaths, temperature, relative humidity, and wind speed between 23 Jan, 2020 and 13 Apr, 2020. The spatial distributions of meteorological factors, GHSI, median age and population density are shown in Figs. S3-S4 in Appendix.
Fig. 1.
Spatial distribution of cumulative confirmed cases of COVID-19 and meteorological monitoring stations worldwide as of 13 April, 2020.
Green points represent the locations of meteorological monitoring stations and colours represent the number of cumulative confirmed cases of COVID-19 as of 13 April, 2020. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Table 1 presents the associations of the COVID-19 incidence with the three meteorological factors for 7 consecutive days (Lag 0–7), 14 consecutive days (Lag 0–14), the current day (Lag 0), the seventh day (Lag 7) and the 14th day (Lag 14), respectively. Fig. 2 shows the associations between the 14-day cumulative risk of COVID-19 incidence and the three meteorological factors.
Table 1.
Association of COVID-19 incidence with meteorological factors worldwide.
| Lag 0–14 |
Lag 0–7 |
Lag 0 |
Lag 7 |
Lag 14 |
|
|---|---|---|---|---|---|
| RR (95%CI)a | RR (95%CI)a | RR (95%CI)a | RR (95%CI)a | RR (95%CI)a | |
| Temperature | |||||
| 5 °C | 1.28 (1.20, 1.36) | 1.18 (1.12, 1.25) | 1.04 (1.02, 1.07) | 1.01 (1.00, 1.02) | 0.99 (0.97, 1.01) |
| 22 °C | 0.75 (0.65, 0.86) | 0.99 (0.85, 1.15) | 1.04 (0.99, 1.11) | 0.96 (0.94, 0.99) | 0.97 (0.91, 1.03) |
| Relative humidity | |||||
| 59% | 0.82 (0.79, 0.86) | 0.81 (0.78, 0.84) | 0.95 (0.94, 0.96) | 0.99 (0.98, 1.00) | 1.04 (1.02, 1.05) |
| 79% | 0.99 (0.94, 1.04) | 1.04 (1.01, 1.08) | 1.02 (1.01, 1.04) | 1.00 (0.99, 1.00) | 0.98 (0.96, 0.99) |
| Wind speed | |||||
| 2 m/s | 0.90 (0.83, 0.98) | 0.96 (0.9, 1.02) | 1.00 (0.98, 1.02) | 0.99 (0.98, 1.00) | 0.99 (0.97, 1.01) |
| 4 m/s | 1.08 (1.02, 1.14) | 1.04 (1.00, 1.08) | 1.00 (0.99, 1.02) | 1.00 (1.00, 1.01) | 1.01 (1.00, 1.03) |
5 °C, 11 °C, and 22 °C correspond to the 25th, 50th and 75th percentiles of daily average temperature, respectively; 59%, 71% and 79% correspond to the 25th, 50th and 75th percentiles of daily relative humidity, respectively; 2 m/s, 3 m/s and 4 m/s correspond to the 25th, 50th and 75th percentiles of daily wind speed, respectively.
Associations between COVID-19 incidence and temperature, relative humidity and wind speed are shown as relative risk (RR) with 95% confidence intervals with reference to the 11 °C, 71% and 3 m/s, respectively.
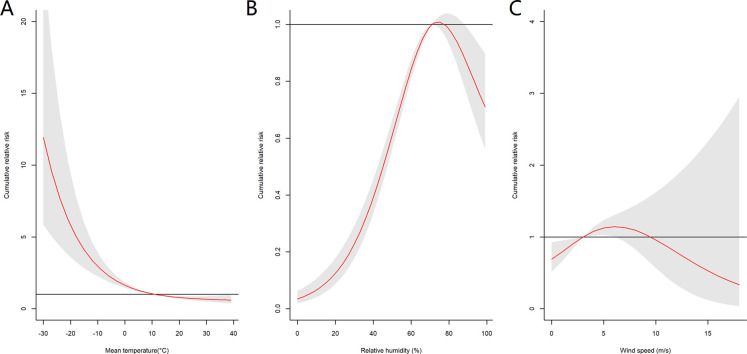
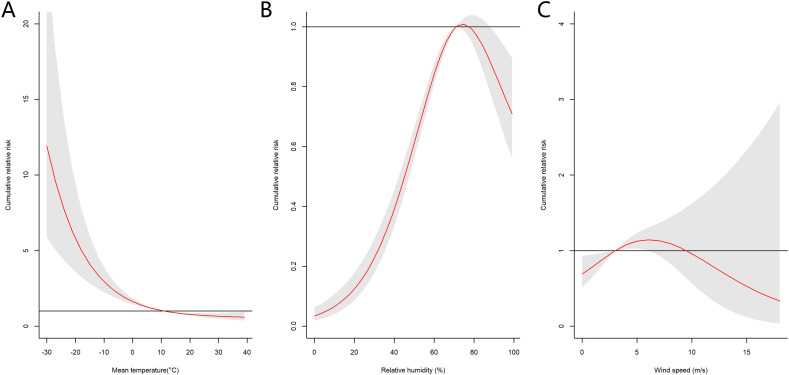
Fig. 2.
Overall association of the cumulative risk of COVID-19 incidence with temperature, relative humidity, and wind speed.
Red lines represent the estimated cumulative relative risks of COVID-19 incidence with shaded bands as 95% confidence intervals. A, B, and C represent the associations of the 14-day cumulative risk of COVID-19 incidence with daily temperature, relative humidity, and wind speed, respectively. The corresponding reference levels were 11 °C, 71% and 3 m/s, respectively. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
An inverse association was observed between temperature and the COVID-19 incidence (Fig. 2A). The cumulative RR decreased sharply with increased temperature as the temperature lower than 11 °C. The curve flattened when the temperature was greater than 11 °C. The corresponding cumulative RRs were 1.28 (95% CI, 1.20–1.36) at 5 °C, and 0.75 (95% CI, 0.65–0.86) at 22 °C, respectively, with reference to 11 °C (Table 1).
An inverse J-shaped association was observed between relative humidity and the COVID-19 incidence, and the cumulative RR peaked at 72% (Fig. 2B). The 14-day cumulative RRs were 0.82 (95% CI, 0.79–0.86) at a relative humidity of 59% and 0.99 (95% CI, 0.94–1.04) at a relative humidity of 79% with reference to 72% (Table 1).
The overall associations between wind speed and COVID-19 incidence were weak. The 14-day cumulative RR of the COVID-19 incidence increased a little as the wind speed increased up to 6 m/s and then started to decrease as the wind speed continue to increase (Fig. 2C). No significant association was observed when wind speeds was above 6 m/s. The 14-day cumulative RRs were 0.9 (95% CI, 0.83–0.98) at a wind speed of 2 m/s, and 1.08 (95% CI, 1.02–1.14) at 4 m/s with reference to 3 m/s (Table 1).
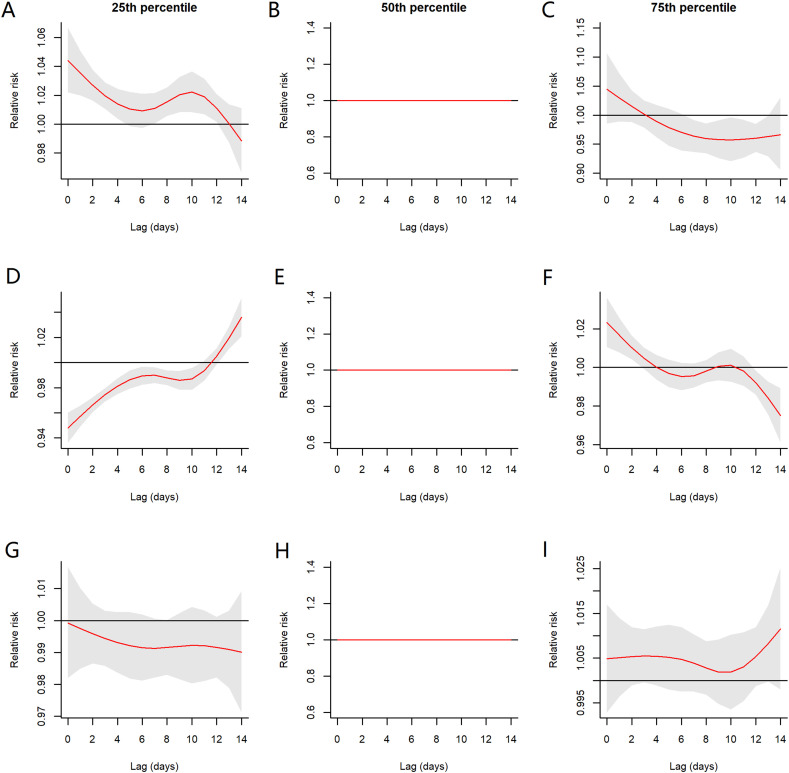
Fig. 3 shows the associations of the daily risk of COVID-19 incidence with the 25th, 50th and 75th percentiles of the meteorological factors over a period of 14 consecutive days. The patterns were generally consistent across percentiles except for the relative humidity at the 75th percentile. The risk of COVID-19 incidence was generally higher between the 6th and 10th days due to the harvest effects and the effects generally disappeared after 12 days. Fig. S5 shows the associations between the COVID-19 incidence and the meteorological factors on the current day (Lag 0), the 7th day (Lag 7) and the 14th day (Lag 14).
Fig. 3.
Associations of the daily risk of COVID-19 incidence with the 25th, 50th and 75th percentiles of meteorological factors over a 14 consecutive days.
Red lines represent the estimated relative risks (RRs) of COVID-19 incidence with shaded bands as 95% confidence intervals. A, B, and C show the relative risk of COVID-19 incidence by comparing the 25th (5.0 °C), 50th (11.0 °C), and 75th (22.0 °C) percentiles of daily average temperature to median value (7 °C), respectively. D, E, and F indicate the RRs of COVID-19 incidence by comparing the 25th (59%), 50th (71%) and 75th (79%) percentiles of daily relative humidity to the median humidity (71%), respectively. G, H, and I represent the RRs of COVID-19 incidence by comparing the 25th (2 m/s), 50th (3 m/s), and 75th (4 m/s) percentiles of daily wind speed to the median wind speed (3 m/s), respectively. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Sensitivity analyses generally yielded similar results. The association of meteorological factors with the COVID-19 mortality was similar to their association with COVID-19 incidence (Table S3). We did not observe substantial changes in the results by extending the lag period from 14 days to 23 days (Table S4), including various numbers of internal knots in the model (Table S5), including only a single meteorological factor in the model (Table S6), excluding outlier province (Hubei, China) and extreme meteorological values (Tables S7-S8), excluding the covariates of “mask wearing” or “propaganda” (Table S9), excluding the countries with one or no monitoring station (Table S10), excluding the 10 countries with the largest area but without state-/province-level data (Table S11), and using linear meteorological variables and shorter lag days (Table S12).
4. Discussion
This study investigated the associations between the COVID-19 incidence and meteorological factors in 415 sites from 190 countries. We observed significant non-linear associations for temperature, relative humidity, and wind speed. The association of COVID-19 incidence with temperature was much stronger than those with relative humidity and wind speed. An increase in temperature from 7 °C to 22 °C was associated with a decrease of 25% in the cumulative risk of COVID-19 incidence over a 14-day period. Sensitivity analyses generally yielded similar results, thus suggesting the robustness of the associations.
4.1. Comparison with previous studies
In line with our study, most previous studies have reported a negative association between temperature and COVID-19 incidence or mortality in China (Gupta, 2020; J Liu et al. 2020; Qi et al., 2020; Shi et al., 2020b), Brazil (Prata et al., 2020), the United States (Runkle et al., 2020), Turkey (Sahin, 2020), other countries (Runkle et al., 2020; Triplett, 2020), and multi-city regions (Baker et al., 2020; Chiyomaru and Chiyomaru and Takemoto, 2020; Islam et al., 2020; Le et al., 2020; Sobral et al., 2020). We observed an overall inverse association between temperature and the COVID-19 incidence at a global scale. The COVID-19 incidence decreased sharply with temperature as the temperature was lower than 11 °C. The temperature-related effects on the COVID-19 incidence flattened when the temperature was higher than 11 °C. We did not find an optimum temperature for the COVID-19 incidence. In contrast to our study, some previous studies have reported no significant association (Awasthi et al., 2020; Pan et al., 2020) or a positive association in some specific countries (Bashir et al., 2020; Bu et al., 2020; Tosepu et al., 2020; Zhu and Zhu and Xie, 2020). This inconsistency is likely due to the limited study sites in previous studies, and the fact that most studies used a linear or log-linear model to examine the association. The non-linear association and the delayed effects of temperature on COVID-19 should be further explored and confirmed in future studies.
We observed a reverse J-shaped association between relative humidity and the COVID-19 incidence. The cumulative risk of COVID-19 incidence peaked at a relative humidity of 72%. There is relatively sparse information on the association between COVID-19 incidence and relative humidity at a global scale. A few studies have reported the associations between COVID-19 and humidity in China (Ma et al., 2020; Wang et al., 2020) and in the world (Baker et al., 2020; Islam et al., 2020; Sajadi et al., 2020), whereas others have found positive association (Sobral et al., 2020), no significant association (Awasthi et al., 2020; Chiyomaru and Takemoto, 2020; Pan et al., 2020), or have reported that the association varies among regions (Guo et al., 2020; Runkle et al., 2020). The linear/nonlinear hypothesis for the associations and different study areas may contribute to these inconsistent findings.
We observed an inverse U-shaped association between wind speed and COVID-19 incidence. The higher wind speed was generally associated with a lower risk of COVID-19 incidence as wind speed was higher than 6 m/s. Two previous studies reported similar findings (Islam et al., 2020; Qiu et al., 2020). The negative associations were also observed in Iran (Ahmadi et al., 2020), Turkey (Sahin, 2020) and China (Zhu and Xie, 2020). In contrast, three multi-city studies (Chiyomaru and Takemoto, 2020; Pan et al., 2020; Sajadi et al., 2020) did not observe significant linear association between wind speed and the cases/basic reproduction number of COVID-19. Further studies on this topic are warranted.
Although the measurements of temperature (°C), relative humidity (%) and wind speed (m/s) differ, the association of COVID-19 incidence with temperature seems more apparent and much stronger than those with relative humidity and wind speed in this study. The 14-day cumulative effect of temperature on COVID-19 incidence was the greatest when the three factors changed by the same percentile (e.g., an increase from the 25th to 50th percentile in temperature, relative humidity and wind speed was associated with decreases of 28%, −18% and −10% in the risk of COVID-19 incidence, respectively).
4.2. Potential mechanism
The potential mechanism underlying the associations between meteorological factors and COVID-19 incidence remains unclear. The negative association of COVID-19 incidence with temperature found in our study is supported by a few laboratory studies, in which SARS-CoV-2 was shown to be highly stable in a cold environment but sensitive to increased temperature (Chin et al., 2020). SARS-CoV-2 is a member of the coronavirus family. A few studies have reported that other coronaviruses such as SARS-CoV-1 or MERS-CoV may lose viability at a high temperature (Chan et al., 2011). A laboratory experiment shows that coronaviruses were inactivated more rapidly at 20 °C than at 4 °C. In addition to SARS-CoV-1's sensitivity to temperature, we speculated that poor indoor ventilation during winter is another possible reason for the strong association between low ambient temperature and a high risk of COVID-19. People generally stay indoors more during winter with the doors and windows closed to keep the indoor environment warm, resulting in poor ventilation. Studies have shown that aerosols from infected persons may pose an inhalation threat even at considerable distances and in enclosed spaces with poor ventilation (Y. Liu et al. 2020; van Doremalen et al., 2020).
Little is known about the relationship between humidity and SARS-CoV-2, but a previous study showed that both titre and genome copies of MERS-CoV decreased more in an environment with a relative humidity of 70% than in an environment with a relative humidity of 40% at the same temperature of 20 °C (Van Doremalen et al., 2013). COVID-19 is transmitted mainly via respiratory droplets generated by coughing and sneezing. Aerosol transmission may also contribute to the spread of COVID-19. Higher wind speeds may blow away the droplets and reduce the concentration of infected aerosol particles.
4.3. Strengthens and limitations:
First, the large sample size enabled us to have more stable results and to conduct a series of sensitivity analyses to confirm the robustness of the associations. Second, our study included 190 countries and covered four major climate zones with a wide temperature range (from −30 °C to 40 °C), which allowed us to investigate the effects of very low or high temperature. Third, we applied a standard and flexible statistical method that can examine nonlinear exposure-response associations. This approach also enabled us to examine non-linear lag-response associations including immediate, delayed, and cumulative effects simultaneously. Fourth, we adjusted for a series of important confounders in the model, including socio-demographics, health security capacities, and interventions for containing the spread of COVID-19. Finally, this study provides urgent and timely evidences for policy makers to develop appropriate strategies for COVID-19 control in the coming seasons.
A few study limitations should be noted. First, the study period was relatively short and two seasons were included. However, the disease transmission has been well controlled in many countries/regions in Asia and Oceania since May 2020 because of the rigorous interventions implemented in these countries/regions. It might not be appropriate to extend the study period because the interventions may substantially affect the associations. Second, some countries had a narrow range of meteorological factors, although the overall range was large for all countries included. This is the exact reason why we could not build models at a country-/city-level. Thus, generalisation of the findings to a specific country/city should be cautious. Third, although we included city-/state-level data in 10 countries, the country-level data were used in the rest 180 countries. Variations in the meteorological factors within countries might lead to exposure misclassification. However, some countries had very small number of COVID-19 cases and we used the population weighted averages of meteorological factors. We also conducted a sensitivity analysis by excluding those countries with single monitoring station or no monitoring station. Our main aim was to explore the associations between meteorological factors and COVID-19 at a global scale rather than in a specific country. Therefore, the variations should not bias our findings. Finally, the proportion of COVID-19 test in each country/city and other potential confounders were not available. However, we included GHSI in the final model. GHSI is a widely used indicator of each country's abilities of early detection and reporting for epidemics.
5. Conclusions
In conclusion, we found nonlinear and delayed associations between COVID-19 incidence and temperature, relative humidity, and wind speed. The association with temperature is strong and inverse. An increase in temperature from 5 °C to 11 °C was associated with a decrease of 28% in the cumulative risk of COVID-19 over a 14-day period. Our findings indicate that summer may slow the COVID-19 outbreak in northern hemisphere, whereas countries in the southern hemisphere should be vigilant in the coming seasons as the temperature decreases. We should utilise the opportunity presented by summer to prepare for better control of the disease in winter.
Funding
This work was in part supported by RGC-General Research Fund (14603019) and Environmental Health Research Fund of the Chinese University of Hong Kong (7104946). Cui Guo is in part supported by the Faculty Postdoctoral Fellowship Scheme of the Faculty of Medicine of the Chinese University of Hong Kong. Yacong Bo and Yiqian Zeng is supported by the PhD Studentship of the Chinese University of Hong Kong.
CRediT authorship contribution statement
CG, AKHL and XQL conceptualized and designed the study. HBL, CG, CL, JWMC, YZ and YB acquired the data. CG, YB and YZ searched literature. CG analyzed data. CG, YB, AKHL and XQL interpreted the data. CG, YB, CL and XQL drafted the manuscript and produced the figures. All authors critically revised the manuscript. XQL and AKHL obtained the funding and supervised this study.
Declaration of competing interest
The authors declared that they have no competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Editor: Jay Gan
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.scitotenv.2020.143783.
Appendix A. Supplementary data
Table S1. Data sources for COVID-19 cases and deaths and covariates.
Table S2. Characteristics of COVID-19 cases and deaths and meteorological factors by country/
Table S3. Association of COVID-19 mortality with meteorological factors worldwide.
Table S4. Association of the cumulative risk of COVID-19 incidence with meteorological factors with extended periods to 23 days.
Table S5. Association of cumulative risk of COVID-19 incidence with meteorological factors with two to four internal knots included in the model.
Table S6. Association of the cumulative risk of COVID-19 incidence with a single meteorological factor included in the model.
Table S7. Association of the cumulative risk of COVID-19 incidence with meteorological factors by excluding data from Hubei province, China.
Table S8. Association of the cumulative risk of COVID-19 incidence with meteorological factors by excluding sites with the highest or lowest 5% of temperature, relative humidity, and wind speed.
Table S9. Association of the cumulative risk of COVID-19 incidence with meteorological factors by excluding mask wearing or propaganda.
Table S10. Association of the cumulative risk of COVID-19 incidence with meteorological factors by excluding the 50 countries with one or no monitoring station.
Table S11. Association of the cumulative risk of COVID-19 incidence with meteorological factors by excluding the 10 largest countries without states-/city-level data.
Table S12. Association of COVID-19 incidence with linear meteorological factors with a maximum lag of 7 days.
Fig. S1. The process of data cleaning.
Fig. S2. Time series plots of daily COVID-19 confirmed cases and deaths, as well as meteorological factors worldwide
Fig. S3. Spatial distribution of mean temperature, relative humidity and wind speed between 22 Jan and 13 April 2020.
A, B, and C represent the spatial distribution of average values of mean temperature, relative humidity and wind speed, respectively.
Fig. S4. Spatial distribution of Global Health Security Index, median age, and population density between 22 Jan and 13 April 2020.
A, B, and C represent the spatial distribution of Global Health Security Index, median age, and population density, respectively.
Fig. S5. Associations of COVID-19 incidence with meteorological factors on the current day (Lag 0), 7th day (Lag 7) and 10th day (Lag 10).
Red lines represent the estimated relative risks of COVID-19 incidence with shaded bands as 95% confidence intervals. A, B, and C show the associations between COVID-19 incidence and daily mean temperature on the current day, lag 7 days, and lag 14 days, respectively with 11°C as reference. D, E, and F indicate the associations between COVID-19 incidence and daily relative humidity at the current day, lag 7 days, and lag 14 days, respectively with 71% as reference. G, H, and I represent the associations between COVID-19 incidence and daily wind speed at the current day, lag 7 days, and lag 14 days, respectively with 3 m/s as reference.
References
- (IATA) IATA . 2020. The Henley Passport Index. [Google Scholar]
- Abdollahi A., Rahbaralam M. Effect of temperature on the transmission of covid-19: a machine learning case study in Spain. medRxiv. 2020 [Google Scholar]
- Ahmadi M., Sharifi A., Dorosti S., Jafarzadeh Ghoushchi S., Ghanbari N. Investigation of effective climatology parameters on covid-19 outbreak in Iran. Sci. Total Environ. 2020;729 doi: 10.1016/j.scitotenv.2020.138705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Awasthi R, Nagori A, Singh P, Pal R, Joshi V, Sethi T. 2020. Temperature and humidity do not influence global covid-19 incidence as inferred from causal models. medRxiv.
- Baker R.E., Yang W., Vecchi G.A., Metcalf C.J.E., Grenfell B.T. Susceptible supply limits the role of climate in the early sars-cov-2 pandemic. Science. 2020 doi: 10.1126/science.abc2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bannister-Tyrrell M, Meyer A, Faverjon C, Cameron A. 2020. Preliminary evidence that higher temperatures are associated with lower incidence of covid-19, for cases reported globally up to 29th february 2020. medRxiv. [DOI] [PMC free article] [PubMed]
- Bashir M.F., Ma B., Komal B., Bashir M.A., Tan D., Bashir M. Correlation between climate indicators and covid-19 pandemic in New York, USA. Sci. Total Environ. 2020 doi: 10.1016/j.scitotenv.2020.138835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bu J., Peng D.-D., Xiao H., Yue Q., Han Y., Lin Y., et al. 2020. Analysis of Meteorological Conditions and Prediction of Epidemic Trend of 2019-nCoV Infection in 2020. [Google Scholar]
- Chan K., Peiris J., Lam S., Poon L., Yuen K., Seto W. The effects of temperature and relative humidity on the viability of the sars coronavirus. Adv Virol. 2011;2011 doi: 10.1155/2011/734690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang C.L., McAleer M. Alternative global health security indexes for risk analysis of covid-19. Int J Environ Res Pub Health. 2020;17:3161. doi: 10.3390/ijerph17093161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chin A.W.H., Chu J.T.S., Perera M.R.A., Hui K.P.Y., Yen H.-L., Chan M.C.W., et al. Stability of sars-cov-2 in different environmental conditions. The Lancet Microbe. 2020;1:e10. doi: 10.1016/S2666-5247(20)30003-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiyomaru K, Takemoto K. 2020. Global covid-19 transmission rate is influenced by precipitation seasonality and the speed of climate temperature warming. medRxiv.
- Dong E., Du H., Gardner L. An interactive web-based dashboard to track covid-19 in real time. Lancet Infect. Dis. 2020;20:533–534. doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donnelly C.A., Ghani A.C., Leung G.M., Hedley A.J., Fraser C., Riley S., et al. Epidemiological determinants of spread of causal agent of severe acute respiratory syndrome in Hong Kong. Lancet. 2003;361:1761–1766. doi: 10.1016/S0140-6736(03)13410-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elaboration of data by United Nations DoEaSA, Population Division . 2019. World Population Prospects: The 2019 Revision. [Google Scholar]
- Gasparrini A., Guo Y., Hashizume M., Lavigne E., Zanobetti A., Schwartz J., et al. Mortality risk attributable to high and low ambient temperature: a multicountry observational study. Lancet. 2015;386:369–375. doi: 10.1016/S0140-6736(14)62114-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guan W.J., Ni Z.Y., Hu Y., Liang W.H., Ou C.Q., He J.X., et al. Clinical characteristics of coronavirus disease 2019 in China. N. Engl. J. Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo X.J., Zhang H., Zeng Y.P. 2020. Transmissibility of Covid-19 and Its Association With Temperature and Humidity. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta D. 2020. Effect of Ambient Temperature on Covid 19 Infection Rate. [Google Scholar]
- Islam N, Shabnam S, Erzurumluoglu AM. 2020. Temperature, humidity, and wind speed are associated with lower covid-19 incidence. medRxiv.
- Johns Hopkins, Bloomberg School of Public Health . 2019. Global Health Security Index. [Google Scholar]
- Kandel N., Chungong S., Omaar A., Xing J. Health security capacities in the context of covid-19 outbreak: an analysis of international health regulations annual report data from 182 countries. Lancet (London, England) 2020;395:1047–1053. doi: 10.1016/S0140-6736(20)30553-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lauer S.A., Grantz K.H., Bi Q., Jones F.K., Zheng Q., Meredith H.R., et al. The incubation period of coronavirus disease 2019 (covid-19) from publicly reported confirmed cases: estimation and application. Ann. Intern. Med. 2020;172:577–582. doi: 10.7326/M7320-0504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le N.K., Le A.V., Parikh J., Brooks J.P., Gardellini T., Izurieta R. Ecological and health infrastructure factors affecting the transmission and mortality of covid-19. BMC Infect. Dis. 2020 [Google Scholar]
- Liu C., Chen R., Sera F., Vicedo-Cabrera A.M., Guo Y., Tong S., et al. Ambient particulate air pollution and daily mortality in 652 cities. N. Engl. J. Med. 2019;381:705–715. doi: 10.1056/NEJMoa1817364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J., Zhou J., Yao J., Zhang X., Li L., Xu X., et al. Impact of meteorological factors on the covid-19 transmission: a multi-city study in China. Sci. Total Environ. 2020;726 doi: 10.1016/j.scitotenv.2020.138513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y., Ning Z., Chen Y., Guo M., Liu Y., Gali N.K., et al. Aerodynamic analysis of sars-cov-2 in two Wuhan hospitals. Nature. 2020:1–6. doi: 10.1038/s41586-020-2271-3. [DOI] [PubMed] [Google Scholar]
- Ma Y., Zhao Y., Liu J., He X., Wang B., Fu S., et al. Effects of temperature variation and humidity on the death of covid-19 in Wuhan, China. Sci. Total Environ. 2020:138226. doi: 10.1016/j.scitotenv.2020.138226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nair H., Brooks W.A., Katz M., Roca A., Berkley J.A., Madhi S.A., et al. Global burden of respiratory infections due to seasonal influenza in young children: a systematic review and meta-analysis. Lancet. 2011;378:1917–1930. doi: 10.1016/S0140-6736(11)61051-9. [DOI] [PubMed] [Google Scholar]
- Pan J., Yao Y., Liu Z., Meng X., Ji J.S., Qiu Y., et al. Warmer weather unlikely to reduce the covid-19 transmission: an ecological study in 202 locations in 8 countries. Sci. Total Environ. 2020 doi: 10.1016/j.scitotenv.2020.142272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prata D.N., Rodrigues W., Bermejo P.H. Temperature significantly changes covid-19 transmission in (sub)tropical cities of Brazil. Sci. Total Environ. 2020;729 doi: 10.1016/j.scitotenv.2020.138862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qi H., Xiao S., Shi R., Ward M.P., Chen Y., Tu W., et al. Covid-19 transmission in Mainland China is associated with temperature and humidity: a time-series analysis. Sci. Total Environ. 2020;728 doi: 10.1016/j.scitotenv.2020.138778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiu Y., Chen X., Shi W. 2020. Impacts of Social and Economic Factors on the Transmission of Coronavirus Disease 2019 (Covid-19) in China. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Runkle J.D., Sugg M.M., Leeper R.D., Rao Y., Mathews J.L., Rennie J.J. Short-term effects of weather parameters on covid-19 morbidity in select us cities. J. Popul. Econ. 2020;33:1127–1172. doi: 10.1016/j.scitotenv.2020.140093. 140093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahin M. Impact of weather on covid-19 pandemic in Turkey. Sci. Total Environ. 2020;728 doi: 10.1016/j.scitotenv.2020.138810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sajadi M.M., Habibzadeh P., Vintzileos A., Shokouhi S., Miralles-Wilhelm F., Amoroso A. Temperature, humidity, and latitude analysis to estimate potential spread and seasonality of coronavirus disease 2019 (covid-19) JAMA Netw. Open. 2020;3:e2011834. doi: 10.1001/jamanetworkopen.2020.11834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi P., Dong Y., Yan H., Li X., Zhao C., Liu W., et al. 2020. The Impact of Temperature and Absolute Humidity on the Coronavirus Disease 2019 (Covid-19) Outbreak - Evidence From China. [Google Scholar]
- Shi P., Dong Y., Yan H., Zhao C., Li X., Liu W., et al. Impact of temperature on the dynamics of the covid-19 outbreak in China. Sci. Total Environ. 2020;728 doi: 10.1016/j.scitotenv.2020.138890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobral M.F.F., Duarte G.B., da Penha Sobral A.I.G., Marinho M.L.M., de Souza Melo A. Association between climate variables and global transmission of sars-cov-2. Sci. Total Environ. 2020;729 doi: 10.1016/j.scitotenv.2020.138997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tosepu R., Gunawan J., Effendy D.S., Ahmad O.A.I., Lestari H., Bahar H., et al. Correlation between weather and covid-19 pandemic in Jakarta, Indonesia. Sci. Total Environ. 2020;725 doi: 10.1016/j.scitotenv.2020.138436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Triplett M. 2020. Evidence That Higher Temperatures Are Associated With Lower Incidence of Covid-19 in Pandemic State, Cumulative Cases Reported up to March 27, 2020. [Google Scholar]
- Van Doremalen N., Bushmaker T., Munster V. Stability of middle east respiratory syndrome coronavirus (mers-cov) under different environmental conditions. Eurosurveillance. 2013;18 doi: 10.2807/1560-7917.es2013.18.38.20590. [DOI] [PubMed] [Google Scholar]
- van Doremalen N., Bushmaker T., Morris D.H., Holbrook M.G., Gamble A., Williamson B.N., et al. Aerosol and surface stability of sars-cov-2 as compared with sars-cov-1. N. Engl. J. Med. 2020;382:1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J., Tang K., Feng K., Lv W. 2020. High Temperature and High Humidity Reduce the Transmission of Covid-19. [Google Scholar]
- Wind . 2020. Wind Financial Database. [Google Scholar]
- World Health Organization . 2020. Coronavirus Disease (Covid-2019) Situation Reports. [Google Scholar]
- Yao Y., Pan J., Liu Z., Meng X., Wang W., Kan H., et al. No association of covid-19 transmission with temperature or uv radiation in chinese cities. Eur. Respir. J. 2020;55 doi: 10.1183/13993003.00517-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Y., Xie J. Association between ambient temperature and covid-19 infection in 122 cities from China. Sci. Total Environ. 2020:138201. doi: 10.1016/j.scitotenv.2020.138201. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Data sources for COVID-19 cases and deaths and covariates.
Table S2. Characteristics of COVID-19 cases and deaths and meteorological factors by country/
Table S3. Association of COVID-19 mortality with meteorological factors worldwide.
Table S4. Association of the cumulative risk of COVID-19 incidence with meteorological factors with extended periods to 23 days.
Table S5. Association of cumulative risk of COVID-19 incidence with meteorological factors with two to four internal knots included in the model.
Table S6. Association of the cumulative risk of COVID-19 incidence with a single meteorological factor included in the model.
Table S7. Association of the cumulative risk of COVID-19 incidence with meteorological factors by excluding data from Hubei province, China.
Table S8. Association of the cumulative risk of COVID-19 incidence with meteorological factors by excluding sites with the highest or lowest 5% of temperature, relative humidity, and wind speed.
Table S9. Association of the cumulative risk of COVID-19 incidence with meteorological factors by excluding mask wearing or propaganda.
Table S10. Association of the cumulative risk of COVID-19 incidence with meteorological factors by excluding the 50 countries with one or no monitoring station.
Table S11. Association of the cumulative risk of COVID-19 incidence with meteorological factors by excluding the 10 largest countries without states-/city-level data.
Table S12. Association of COVID-19 incidence with linear meteorological factors with a maximum lag of 7 days.
Fig. S1. The process of data cleaning.
Fig. S2. Time series plots of daily COVID-19 confirmed cases and deaths, as well as meteorological factors worldwide
Fig. S3. Spatial distribution of mean temperature, relative humidity and wind speed between 22 Jan and 13 April 2020.
A, B, and C represent the spatial distribution of average values of mean temperature, relative humidity and wind speed, respectively.
Fig. S4. Spatial distribution of Global Health Security Index, median age, and population density between 22 Jan and 13 April 2020.
A, B, and C represent the spatial distribution of Global Health Security Index, median age, and population density, respectively.
Fig. S5. Associations of COVID-19 incidence with meteorological factors on the current day (Lag 0), 7th day (Lag 7) and 10th day (Lag 10).
Red lines represent the estimated relative risks of COVID-19 incidence with shaded bands as 95% confidence intervals. A, B, and C show the associations between COVID-19 incidence and daily mean temperature on the current day, lag 7 days, and lag 14 days, respectively with 11°C as reference. D, E, and F indicate the associations between COVID-19 incidence and daily relative humidity at the current day, lag 7 days, and lag 14 days, respectively with 71% as reference. G, H, and I represent the associations between COVID-19 incidence and daily wind speed at the current day, lag 7 days, and lag 14 days, respectively with 3 m/s as reference.