Abstract
Aim:
This review study was conducted to evaluate the symptoms of COVID-19 in pregnant women with a focus on gastrointestinal symptoms.
Background:
COVID-19 is a fatal respiratory disease caused by a novel coronavirus that quickly became a pandemic. Although the main symptoms of this disease include respiratory symptoms, gastrointestinal manifestations have also been observed in some patients suffering from COVID-19. Pregnant women are among the most vulnerable groups in the community to infectious diseases.
Methods:
Scientific databases were searched for articles published up to May 8, 2020. Any type of study investigating the manifestations of COVID-19 in pregnant women was included. Symptoms of the disease in pregnant women with an emphasis on gastrointestinal symptoms were assessed.
Results:
The search resulted in 852 titles and abstracts, which were narrowed down to 43 studies involving 374 women. The most common symptoms of patients were fever (59.1%) and cough (48.4%), respectively. Gastrointestinal symptoms included diarrhea (4.5%), abdominal pain (1.6%), nausea (0.8%), and loss of appetite (0.3%), respectively. In studies on pregnant women with gastrointestinal symptoms, 13 fetal abortions occurred, most of which were induced abortions due to the risks posed by COVID-19.In thirty cases, and infected pregnant women reported a history of chronic pregnancy-related diseases.
Conclusion:
COVID-19 in pregnant women, similar to the general population, can present with gastrointestinal manifestations. The gastrointestinal tract can be a potential route for infection with the novel coronavirus.
Key Words: COVID-19, Novel Coronavirus Infection, Pregnancy, Diarrhea, Gastrointestinal Tract
Introduction
Coronaviruses comprise a large family of viruses that, according to evidence, can cause diseases such as the common cold, to more severe diseases such as the Middle East respiratory syndrome (MERS), or even more severe, such as severe acute respiratory syndrome (SARS) (1). In December 2019, a new type of coronavirus that had not previously been seen in humans was identified in Wuhan, China. The novel virus, called SARS-CoV-2, has been linked to a new respiratory syndrome called COVID-19 (2). This disease spread rapidly, resulting in epidemics in China and reports of multiple cases worldwide, and has been declared by the World Health Organization as a pandemic situation and the sixth public health emergency of international concern (3).
The knowledge and understanding of COVID-19 are advancing rapidly, but evidence specifically focused on pregnant women is limited. They appear to be one of the most vulnerable groups to COVID-19. Physiological changes during pregnancy in the pulmonary system, such as increased oxygen consumption, increased minute ventilation, and decreased lung capacity, increase the risk of developing severe respiratory diseases in pregnant women. In addition, suppression of immune responses during pregnancy increases the risk of infections (4, 5).
Although the main symptoms of this disease include respiratory symptoms such as fever, dry cough, fatigue, and shortness of breath(3, 6), according to the evidence, gastrointestinal manifestations have also been observed in some patients suffering from COVID-19. One hypothesis in this regard is the use by the coronavirus of human angiotensin-converting enzyme 2 (ACE-2) receptors located on intestinal cells, hepatocytes, and cholangiocytes (7). Sellevoll et al. presented a woman with suspected cholecystitis who was admitted with acute abdominal pain and had no symptoms of respiratory infection, but eventually, a coronavirus test was positive (8). Findings from some studies on pregnant women infected by SARS-CoV-2 have indicated gastrointestinal symptoms such as abdominal pain, nausea, vomiting, and diarrhea in addition to respiratory symptoms (9, 10).
This review study was conducted to evaluate the symptoms of COVID-19 in pregnant women with a focus on gastrointestinal symptoms.
Methods
Two investigators searched the Cochrane Library, Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE/PubMed, and SCOPUSfor articles published up to May 8, 2020. The search strategy was: (coronavirus OR “coronavirus disease-19” OR “COVID-19” OR “2019-nCoV disease” OR “2019 novel coronavirus infection” OR “2019-nCoV infection” OR “COVID-19 pandemic” OR “2019 novel coronavirus disease”) AND (pregnant* OR Childbearing OR Prenatal).
Any type of study with original data involving pregnant women infected bySARS-CoV-2in any trimester of pregnancy was included in the study. Articles in languages other than English, those that did not have enough data to answer the research question, and those that were only abstract were excluded. Our outcomes were any type of symptoms of COVID-19, mode of delivery, history of chronic basic diseases, vertical transmission, and maternal complications.
In the first step, two researchers independently examined the search output on each database. They reviewed the titles and abstracts of the articles and removed irrelevant studies. In the second step, the full text of the remaining articles was carefully reviewed. Any disagreement was resolved through discussion. The data retrieval tool was a researcher-made form that included data such as the name of the first author; country; sample size; pregnancy characteristics; general, respiratory, and gastrointestinal symptoms at the time of hospitalization or in the days following; mode of delivery; the history of chronic basic diseases; rate of vertical transmission; and maternal complications.
Throughout the preparation of this article, the researchers adhered to the ethical principles in research; they never manipulated data to achieve their advantages and avoided plagiarism.
Results
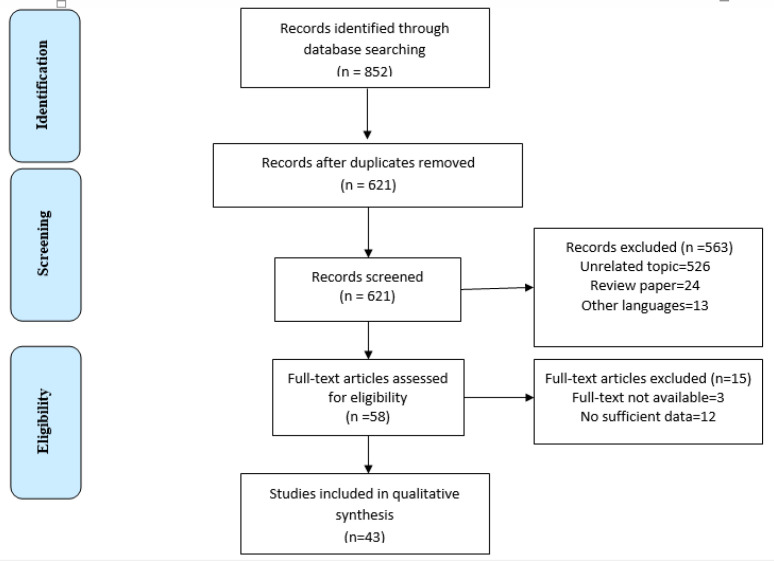
Figure 1 shows the PRISMA flowchart for study inclusion and exclusion. A total of 852 studies corresponding to our search strategy were identified. Throughout data reduction, 563 irrelevant records were excluded based on the title and abstract review. The full-text articles for the remaining 58 articles were retrieved. After review of the full-text articles, 15 articles were excluded and 43met our inclusion criteria for the review. The characteristics of these studies are presented in Table 1.
Figure1.
PRISMA Flow Diagram of the study
Table1.
Characteristics of Studies including COVID-19 in Pregnant Women
| First Author's Name | n | Country | Gestational Age | Symptoms of COVID-19 | |||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| General Symptoms | Respiratory Symptoms | Gastrointestinal Symptoms | |||||||||||||||||||||||||||
| Preterm (<37 weeks) | Term (≥37 weeks) | Fatigue | Myalgia | Headache | F ever | Cough | Dyspnea or shortness of breath. | Nasal congestion | Sputum | Diarrhea | Abdominal pain | Nausea | Loss of appetite | ||||||||||||||||
| Alzamora,MC(46) | 1 | Peru | 1 | - | 1 | 1 | - | 1 | - | 1 | - | - | - | - | - | - | |||||||||||||
| Browne, PC(33) | 1 | USA | 1 | - | - | 1 | - | 1 | 1 | - | - | - | - | - | - | - | |||||||||||||
| Buonsenso, D(40) | 4 | Italy | 3 | 1 | - | - | - | 3 | 4 | 1 | - | - | - | - | - | - | |||||||||||||
| Cao, D(11) | 10 | China | 3 | 7 | 1 | - | - | 7 | 1 | - | - | - | - | - | - | - | |||||||||||||
| Carosso, A(41) | 1 | Italy | - | 1 | - | - | - | 1 | 1 | - | - | - | - | - | - | - | |||||||||||||
| Chen, L(9) | 118 | China | NM | - | 19 | - | - | 84 | 7 | - | - | - | |||||||||||||||||
| Chen, R(12) | 17 | China | 3 | 14 | 1 | - | - | 4 | 4 | 1 | - | - | 1 | - | - | - | |||||||||||||
| Chen, S(13) | 5 | China | - | 5 | - | - | - | 5 | 2 | - | - | 1 | - | - | - | - | |||||||||||||
| Chen, Y(14) | 4 | China | - | 4 | 2 | - | 2 | 3 | 2 | - | - | - | - | - | - | - | |||||||||||||
| De Castro, A(34) | 1 | USA | 1 | - | 1 | - | 1 | 1 | - | - | - | - | - | - | - | - | |||||||||||||
| Fan, C(15) | 2 | China | 1 | 1 | - | - | - | 2 | - | - | 2 | - | - | - | - | - | |||||||||||||
| Ferrazzia, E(42) | 42 | Italy | 12 | 30 | 7 | 20 | 18 | 8 | - | - | 2 | - | - | - | |||||||||||||||
| Gidlöf, S(49) | 1 | Sweden | 1 | - | - | 1 | 1 | 1 | - | - | - | - | - | - | - | - | |||||||||||||
| Hantoushzadeh,S(44) | 9 | Iran | 6 | 3 | - | 4 | - | 9 | 9 | 6 | - | - | - | - | - | - | |||||||||||||
| Hirshberg, A(35) | 5 | USA | 5 | - | 1 | - | 1 | 5 | 3 | 5 | - | - | - | - | - | - | |||||||||||||
| Iqbal, S(36) | 1 | USA | - | 1 | - | 1 | - | 1 | 1 | - | - | - | - | - | - | - | |||||||||||||
| Juusela, A(37) | 2 | USA | 1 | 1 | - | - | - | 1 | - | 1 | - | - | - | - | 1 | - | |||||||||||||
| Kalafat, E(48) | 1 | Turkey | 1 | - | - | - | - | - | 1 | 1 | - | - | - | - | - | ||||||||||||||
| Karami, P(45) | 1 | Iran | 1 | - | - | 1 | - | 1 | 1 | - | - | - | - | - | - | - | |||||||||||||
| Kelly, JC(38) | 1 | USA | 1 | - | - | - | - | 1 | 1 | 1 | - | - | - | - | 1 | - | |||||||||||||
| Khan, S-1(16) | 3 | China | 1 | 2 | - | - | - | 2 | 3 | - | - | - | - | - | - | - | |||||||||||||
| Khan, S-2(17) | 17 | China | 3 | 14 | - | - | - | 3 | 6 | 2 | 2 | 1 | 3 | - | - | - | |||||||||||||
| Lee, DH(51) | 1 | Korea | - | 1 | - | - | - | 1 | 1 | - | - | 1 | - | - | - | - | |||||||||||||
| Li, J(18) | 1 | China | 1 | - | - | - | - | 1 | 1 | 1 | - | - | - | - | - | - | |||||||||||||
| Li, Y(19) | 1 | China | 1 | - | - | - | - | - | 1 | - | - | - | - | - | - | - | |||||||||||||
| Liao, J(20) | 10 | China | 1 | 9 | - | - | - | 5 | 3 | - | - | - | - | - | - | - | |||||||||||||
| Liu,D(21) | 15 | China | 7 | 8 | 4 | 3 | - | 13 | 9 | 1 | - | - | 1 | - | - | - | |||||||||||||
| Liu, Y(22) | 13 | China | 10 | 3 | 4 | - | - | 10 | 2 | 3 | - | - | - | - | - | - | |||||||||||||
| Lu, D(23) | 1 | China | - | 1 | - | - | - | - | - | - | - | - | - | - | - | - | |||||||||||||
| Lyra, J(47) | 1 | Portugal | - | 1 | - | - | - | - | 1 | - | - | - | - | - | - | - | |||||||||||||
| Martinelli, I(43) | 1 | Italy | 1 | - | - | - | - | - | - | 1 | - | - | - | - | - | - | |||||||||||||
| Peng, Z(24) | 1 | China | 1 | - | 1 | - | - | 1 | - | 1 | - | - | - | - | - | - | |||||||||||||
| Qiancheng, X(25) | 28 | China | 9 | 19 | - | 1 | - | 5 | 7 | 2 | - | - | - | 5 | - | - | |||||||||||||
| Schnettler, WT(39) | 1 | USA | 1 | - | - | 1 | - | 1 | 1 | 1 | - | - | - | - | - | - | |||||||||||||
| Wang, S(26) | 1 | China | - | 1 | - | - | - | 1 | - | - | - | - | - | 1 | - | - | |||||||||||||
| Wang,X(27) | 1 | China | 1 | - | - | - | - | 1 | - | - | - | - | - | - | - | - | |||||||||||||
| Wu, C(28) | 8 | China | 2 | 6 | - | - | - | 4 | - | - | - | - | - | - | - | - | |||||||||||||
| Wu, X(29) | 23 | China | 6 | 17 | - | - | - | 4 | 6 | - | 1 | - | - | - | - | - | |||||||||||||
| Xiong, X(30) | 1 | China | 1 | - | - | - | - | 1 | 1 | - | - | - | - | - | - | - | |||||||||||||
| Yu, N(31) | 7 | China | - | 7 | - | - | - | 6 | 1 | 1 | - | - | 1 | - | - | - | |||||||||||||
| Zamaniyan, M(10) | 1 | Iran | 1 | - | - | 1 | - | 1 | 1 | 1 | - | - | - | - | 1 | 1 | |||||||||||||
| Zambrano, LI(50) | 1 | Central America | 1 | - | 1 | 1 | - | 1 | 1 | - | - | - | - | - | - | - | |||||||||||||
| Zhu, H(32) | 10 | China | 6 | 4 | - | - | - | 9 | 5 | - | - | - | 1 | - | - | - | |||||||||||||
| Total | 374 | - | 95 | 161 | 36 | 23 | 12 | 221 | 181 | 47 | 5 | 3 | 17 | 6 | 3 | 1 | |||||||||||||
NM: Not Mentioned
Participants and settings
A total of 374 samples were involved, ranging from 1 to 118 per study. In general, the gestational age in most women was 37 weeks or more (n=161, 62.9%). Twenty-three studies were undertaken in China(9, 11-32), seven studies were conducted in the USA(33-39), four studies in Italy(40-43), three in Iran(10, 44, 45), and one study each in Peru(46), Portugal(47), Turkey(48), Sweden(49), Central America(50), and Korea(51).
Manifestations of COVID-19
The symptoms of COVID-19 were classified into three categories: general, respiratory, and gastrointestinal. The most common general symptoms of COVID-19 in the studied pregnant women were fatigue (n=36, 9.6%) and myalgia (n=23, 6.1%), respectively. The most common respiratory symptoms in pregnant women included fever (n=221, 59.1%), cough (n=181, 48.4%), and dyspnea or shortness of breath (n=47, 12.5%), respectively. Among the gastrointestinal symptoms associated with novel coronavirus infection, diarrhea (n=17, 4.5%) and abdominal pain (n=6, 1.6%) were more common than others.
Focus on studies of pregnant women with gastrointestinal symptoms of COVID-19:
In 12 studies (n=259), pregnant women reported gastrointestinal symptoms caused by COVID-19 (Table 2). Most of these studies were conducted in China (66.6%). Gastrointestinal symptoms included diarrhea, abdominal pain, nausea, and loss of appetite. In studies of pregnant women with gastrointestinal symptoms, 159 cesarean sections (61.4%) and 40 vaginal deliveries (15.4%) were performed. There were also 13 abortions, most of which were induced abortions due to the risks posed by COVID-19.
Table2.
Characteristics of Studies with Gastrointestinal Symptoms of COVID-19 in Pregnant Women
| First Author's Name | N | Country | GA (weeks) | Gastrointestinal Symptoms of COVID-19 | Method of Birth | History of Chronic Basic Diseases |
Vertical transmission | Maternal Complications | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Preterm | Term | Diarrhea | Abdominal pain | Nausea | Loss of appetite | Vaginal delivery | Cesarean section | Pregnant at End of Study | Abortion | DM | GDM | High blood pressure | Obesity | PCOD | Hypothyroidism | Anemia | Hepatitis B | Not Mentioned | Death | Mechanical ventilation | |||||
| Chen, L (9) | 118 | China | NM | 8 | - | - | 5 | 63 | 41 | 9 | - | - | - | - | - | - | - | - | + | 0/8 | - | - | |||
| Chen, R (12) | 17 | China | 3 | 14 | 1 | - | - | - | - | 17 | - | - | 2 | - | 1 | - | - | - | 5 | - | - | - | - | - | |
| Ferrazzia, E (42) | 42 | Italy | 12 | 30 | 2 | - | - | - | 24 | 18 | - | - | - | 6 | - | - | - | - | - | - | - | 3/42 | - | NM | |
| Juusela, A (37) | 2 | USA | 1 | 1 | - | - | 1 | - | 2 | - | - | - | - | 1 | - | 2 | 1 | - | - | - | - | NM | - | 1 | |
| Kelly, JC (38) | 1 | USA | 1 | - | - | - | 1 | - | - | 1 | - | - | - | - | - | 1 | - | - | - | - | - | - | - | 1 | |
| Khan, S-2 (17) | 17 | China | 3 | 14 | 3 | - | - | - | - | 17 | - | - | - | - | - | - | - | - | - | - | + | 2/17 | - | - | |
| Liu,D (21) | 15 | China | 7 | 8 | 1 | - | - | - | 1 | 10 | 4 | - | - | 1 | - | - | - | - | - | - | - | NM | - | - | |
| Qiancheng, X (25) | 28 | China | 9 | 19 | - | 5 | - | - | 5 | 17 | 2 | 4 | 2 | - | 1 | - | - | 1 | - | 2 | - | 0/23 | - | - | |
| Wang, S (26) | 1 | China | - | 1 | - | 1 | - | - | - | 1 | - | - | - | - | - | - | - | 1 | - | - | - | 1 | - | - | |
| Yu, N (31) | 7 | China | - | 7 | 1 | - | - | - | - | 7 | - | - | - | - | - | - | 1 | 1 | - | - | - | 1/3 | - | - | |
| Zamaniyan, M (10) | 1 | Iran | 1 | - | - | - | 1 | 1 | - | 1 | - | - | - | - | - | - | - | 1 | - | - | - | 1 | - | - | |
| Zhu, H (32) | 10 | China | 6 | 4 | 1 | - | - | 3 | 7 | - | - | - | - | - | - | - | - | - | - | + | 0/9 | - | - | ||
| Total | 259 | - | 17 | 6 | 3 | 1 | 40 | 159 | 47 | 13 | 4 | 8 | 2 | 3 | 2 | 4 | 5 | 2 | - | 8/104 | - | 2 | |||
DM: Diabetes Mellitus; GMM: Gestational Diabetes Mellitus; PCOD: Polycystic Ovarian Disease; NM: Not Mentioned
In thirty cases, infected pregnant women reported a history of chronic or pregnancy-related diseases. In order of frequency, they were gestational diabetes mellitus (26.6%), anemia (16.6%), diabetes mellitus (13.3%), hypothyroidism (13.3%), obesity (10%), high blood pressure (6.6%), polycystic ovarian disease (6.6%), and hepatitis B (6.6%). The vertical transmission rate was 7.6%. No maternal deaths were reported. The need for mechanical ventilation was 0.9%.
Discussion
To the best of our knowledge, this is the first study that focused on the gastrointestinal symptoms of COVID-19 in pregnant women. We did not find any similar study on pregnant women focusing on gastrointestinal symptoms of COVID-19 to compare with our findings. In the present study, the most common gastrointestinal symptoms of COVID-19 in pregnant women were diarrhea (4.5%) and abdominal pain (1.6%), respectively. Evidence suggests that approximately 2% to 33% of patients suffered from diarrhea as one of the symptoms of COVID-19 (53, 54).Chan et al. stated that 10.6% of patients with SARS and 30% of patients with MERS complained of diarrhea(55).It has been shown that MERS coronavirus can survive in simulated gastrointestinal juice and can cause intestinal infections(55).Some studies have shown the presence
of SARS-CoV-2 in the stool of patients suffering from COVID-19 (54, 56). Such evidence suggests that the gastrointestinal tract may be one of the potential routes of SARS-CoV-2 invasion and transmission, and there is also the possibility of oral-fecal transmission, indicating the need for effective revision of diagnostic and diagnostic guidelines.
According to our results, the second most common gastrointestinal symptom in infected pregnant women was abdominal pain (1.6%). Studies on non-pregnant populations have shown that abdominal pain as one of the symptoms of COVID-19 was rated from 2.2% to 5.8% (55, 57). In some studies, liver damage caused by SARS-CoV-2, impaired liver function tests, and increased bilirubin levels have also been reported in infected patients (58). Therefore, the presence of gastrointestinal symptoms with or without respiratory symptoms may be a warning sign of COVID-19.
Although the main mechanism that explains the presence of gastrointestinal manifestations caused by COVID-19is unknown; one possible mechanism is the ability of SARS-CoV-2, like SARS-CoV, to bind to ACE-2 receptors, which are abundantly expressed in the gastrointestinal tract (57). Pan et al. stated that SARS-CoV-2 itself may cause disorders of the intestinal flora, which could result in gastrointestinal manifestations (59). Another possible mechanism is that changes in the composition and function of the gastrointestinal tract and respiratory tract flora can affect each other. This effect is called the “gut-lung axis" and can help explain why patients with COVID-19 often have gastrointestinal symptoms (60).
A significant number of pregnant women in whom gastrointestinal symptoms were among the manifestations of COVID-19 were predisposed to underlying chronic diseases. According to increasing evidence, the risk of developing COVID-19 and worsening of the condition of those with a chronic disease such as high blood pressure, lung disease, kidney problems, diabetes, or heart disease is higher than it is in healthy people(61).Therefore, it is recommended that pregnant women suffering from underlying diseases quarantine at home, because the weakening of their immune system and specific physiological changes related to pregnancy in interaction with the underlying disease increase the risk of infection by SARS-CoV-2and its serious complications.
The current study found that COVID-19 gastrointestinal symptoms were lower in pregnant women than in the non-pregnant populations reported in some studies (59). It seems that because the disease first appeared with respiratory symptoms, these have been the focus of most studies, and gastrointestinal symptoms have been neglected in some lower quality studies. Non-English language studies were also excluded from the current study, which may be a factor in this finding. To achieve more reliable and accurate results, more original, higher quality studies should be conducted.
Covid-19 in pregnant women, similar to the general population, can present with gastrointestinal manifestations. The gastrointestinal tract can be a potential route for infection with the novel coronavirus. According to the evidence, there is also the possibility of oral-fecal transmission. In pregnant women, as in the non-pregnant population, gastrointestinal symptoms in addition to the respiratory symptoms of COVID-19 should be considered.
Acknowledgment
The authors thank the reviewers for their valuable comments that improved the quality of the article.
Conflict of interests
The authors declare that they have no conflict of interest.
References
- 1.Qiao J. What are the risks of COVID-19 infection in pregnant women? The Lancet. 2020;395:760–2. doi: 10.1016/S0140-6736(20)30365-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Breslin N, Baptiste C, Gyamfi-Bannerman C, Miller R, Martinez R, Bernstein K, et al. COVID-19 infection among asymptomatic and symptomatic pregnant women: Two weeks of confirmed presentations to an affiliated pair of New York City hospitals. Am J Obstet Gynecol MFM. 2020:100118. doi: 10.1016/j.ajogmf.2020.100118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. The lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wong SF, Chow KM, Leung TN, Ng WF, Ng TK, Shek CC, et al. Pregnancy and perinatal outcomes of women with severe acute respiratory syndrome. AJOG2004. 191:292–7. doi: 10.1016/j.ajog.2003.11.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dashraath P, Jeslyn WJL, Karen LMX, Min LL, Sarah L, Biswas A, et al. Coronavirus Disease 2019 (COVID-19) Pandemic and Pregnancy. AJOG. 2020;222:521. doi: 10.1016/j.ajog.2020.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rajkumar RP. COVID-19 and mental health: A review of the existing literature. Asian J Psychiatr. 2020;52:102066. doi: 10.1016/j.ajp.2020.102066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Agarwal A, Chen A, Ravindran N, To C, Thuluvath PJ. Gastrointestinal and Liver Manifestations of COVID-19. J ClinExpHepatol. 2020;10:263–65. doi: 10.1016/j.jceh.2020.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sellevoll HB, Saeed U, Young VS, Sandbæk G, Gundersen K, Mala T. Acute abdomen as an early symptom of COVID-19. Tidsskr Nor Legeforen. 2020;10:4045. doi: 10.4045/tidsskr.20.0262. [DOI] [PubMed] [Google Scholar]
- 9.Chen L, Li Q, Zheng D, Jiang H, Wei Y, Zou L, et al. Clinical Characteristics of Pregnant Women with Covid-19 in Wuhan, China. N Engl J Med. 2020;382:e100. doi: 10.1056/NEJMc2009226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zamaniyan M, Ebadi A, Aghajanpoor Mir S, Rahmani Z, Haghshenas M, Azizi S. Preterm delivery in pregnant woman with critical COVID-19 pneumonia and vertical transmission. Prenat Diagn. 2020;10:1002. doi: 10.1002/pd.5713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cao D, Yin H, Chen J, Tang F, Peng M, Li R, et al. Clinical analysis of ten pregnant women with COVID-19 in Wuhan, China: A retrospective study. Int J Infect Dis. 2020;23:30263–70. doi: 10.1016/j.ijid.2020.04.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen R, Zhang Y, Huang L, Cheng BH, Xia ZY, Meng QT. Safety and efficacy of different anesthetic regimens for parturients with COVID-19 undergoing Cesarean delivery: a case series of 17 patients. Can J Anesth. 2020:67655–63. doi: 10.1007/s12630-020-01630-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen S, Liao E, Cao D, Gao Y, Sun G, Shao Y. Clinical analysis of pregnant women with 2019 novel coronavirus pneumonia. J Med Virol. 2020;92:1556–61. doi: 10.1002/jmv.25789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chen Y, Peng H, Wang L, Zhao Y, Zeng L, Gao H, et al. Infants Born to Mothers With a New Coronavirus (COVID-19) Front Pediatr. 2020;8:1–5. doi: 10.3389/fped.2020.00104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fan C, Lei D, Fang C, Li C, Wang M, Liu Y, et al. Perinatal Transmission of COVID-19 Associated SARS-CoV-2: Should We Worry? Clin Infect Dis. 2020;10:1093. doi: 10.1093/cid/ciaa226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Khan S, Peng L, Siddique R, Nabi G, Nawsherwan , Xue M, et al. Impact of COVID-19 infection on pregnancy outcomes and the risk of maternal-to-neonatal intrapartum transmission of COVID-19 during natural birth. Infect Control Hosp Epidemiol. 2020;41:748–50. doi: 10.1017/ice.2020.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Khan S, Jun L, Nawsherwan , Siddique R, Li Y, Han G, et al. Association of COVID-19 with pregnancy outcomes in health-care workers and general women. Clin Microbiol Infect. 2020;26:788–90. doi: 10.1016/j.cmi.2020.03.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li J, Wang Y, Zeng Y, Song T, Pan X, Jia M, et al. Critically ill pregnant patient with COVID-19 and neonatal death within two hours of birth. Int J Gynaecol Obstet. 2020;5:13189. doi: 10.1002/ijgo.13189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li Y, Zhao R, Zheng S, Chen X, Wang J, Sheng X, et al. Lack of Vertical Transmission of Severe Acute Respiratory Syndrome Coronavirus 2, China. Emerg Inf Dis. 2020:26. doi: 10.3201/eid2606.200287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liao J, He X, Gong Q, Yang L, Zhou C, Li J. Analysis of vaginal delivery outcomes among pregnant women in Wuhan, China during the COVID-19 pandemic. Int J Gynaecol Obstet. 2020;29:13188. doi: 10.1002/ijgo.13188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liu D, Li L, Wu X, Zheng D, Wang J, Yang L, et al. Pregnancy and Perinatal Outcomes of Women With Coronavirus Disease (COVID-19) Pneumonia: A Preliminary Analysis. AJR Am J Roentgenol. 2020:1–6. doi: 10.2214/AJR.20.23072. [DOI] [PubMed] [Google Scholar]
- 22.Liu Y, Chen H, Tang K, Guo Y. Clinical manifestations and outcome of SARS-CoV-2 infection during pregnancy. J Infect . 2020 doi: 10.1016/j.jinf.2020.02.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lu D, Sang L, Du S, Li T, Chang Y, Yang XA. Asymptomatic COVID-19 infection in late pregnancy indicated no vertical transmission. J Med Virol. 2020;24:25927. doi: 10.1002/jmv.25927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Peng Z, Wang J, Mo Y, Duan W, Xiang G, Yi M, et al. Unlikely SARS-CoV-2 vertical transmission from mother to child: A case report. Journal of Infection and Public Health. 2020;13:818–20. doi: 10.1016/j.jiph.2020.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Qiancheng X, Jian S, Lingling P, Lei H, Xiaogan J, Weihua L, et al. Coronavirus disease 2019 in pregnancy. Int J Infect Dis. 2020;95:376–83. doi: 10.1016/j.ijid.2020.04.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang S, Guo L, Chen L, Liu W, Cao Y, Zhang J, et al. A case report of neonatal COVID-19 infection in China. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wang X, Zhou Z, Zhang J, Zhu F, Tang Y, Shen X. A case of 2019 Novel Coronavirus in a pregnant woman with preterm delivery. Clin Infect Dis. 2020;71:844–6. doi: 10.1093/cid/ciaa200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wu C, Yang W, Wu X, Zhang T, Zhao Y, Ren W, et al. Clinical Manifestation and Laboratory Characteristics of SARS-CoV-2 Infection in Pregnant Women. VirolSin. 2020:1–6. doi: 10.1007/s12250-020-00227-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wu X, Sun R, Chen J, Xie Y, Zhang S, Wang X. Radiological findings and clinical characteristics of pregnant women with COVID-19 pneumonia. Int J Gynaecol Obstet. 2020;150:58–63. doi: 10.1002/ijgo.13165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Xiong X, Wei H, Zhang Z, Chang J, Ma X, Gao X, et al. Vaginal Delivery Report of a Healthy Neonate Born to a Convalescent Mother with COVID19. J Med Virol. 2020 doi: 10.1002/jmv.25857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yu N, Li W, Kang Q, Xiong Z, Wang S, Lin X, et al. Clinical features and obstetric and neonatal outcomes of pregnant patients with COVID-19 in Wuhan, China: a retrospective, single-centre, descriptive study. Lancet Infect Dis. 2020;20:559–64. doi: 10.1016/S1473-3099(20)30176-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhu H, Wang L, Fang C, Peng S, Zhang L, Chang G, et al. Clinical analysis of 10 neonates born to mothers with 2019-nCoV pneumonia. Transl Pediatr. 2020;9:51–60. doi: 10.21037/tp.2020.02.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.PC , Linfert JB, Perez-Jorge E. Successful Treatment of Preterm Labor in Association with Acute COVID-19 Infection. Am J Perinatol. 2020;37:866–8. doi: 10.1055/s-0040-1709993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.De Castro A, Abu-Hishmeh M, El Husseini I, Paul L. Haemophilus parainfluenzae endocarditis with multiple cerebral emboli in a pregnant woman with coronavirus. ID Cases. 2019;18:e00593. doi: 10.1016/j.idcr.2019.e00593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hirshberg A, Kern-Goldberger AR, Levine LD, Pierce-Williams R, Short WR, Parry S, et al. Care of critically ill pregnant patients with COVID-19: a case series. Am J Obstet Gynecol. 2020;223:286–90. doi: 10.1016/j.ajog.2020.04.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Iqbal SN, Overcash R, Mokhtari N, Saeed H, Gold S, Auguste T, et al. An Uncomplicated Delivery in a Patient with Covid-19 in the United States. N Engl J Med. 2020;382 doi: 10.1056/NEJMc2007605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Juusela A, Nazir M, Gimovsky M. Two cases of coronavirus 2019-related cardiomyopathy in pregnancy. Am J Obstet Gynecol MFM. 2020;2:100113. doi: 10.1016/j.ajogmf.2020.100113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kelly JC, Dombrowksi M, O'Neil-Callahan M, Kernberg AS, Frolova AI, Stout MJ. False-Negative COVID-19 Testing: False-negative testing for severe acute respiratory syndrome coronavirus 2: consideration in obstetrical care. Am J Obstet Gynecol MFM. 2020;2:100130. doi: 10.1016/j.ajogmf.2020.100130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Schnettler WT, Al Ahwel Y, Suhag A. Severe ARDS in COVID-19-infected pregnancy: obstetric and intensive care considerations. Am J Obstet Gynecol MFM. 2020;2:100120. doi: 10.1016/j.ajogmf.2020.100120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Buonsenso D, Raffaelli F, Tamburrini E, Biasucci DG, Salvi S, Smargiassi A, et al. Clinical role of lung ultrasound for the diagnosis and monitoring of COVID-19 pneumonia in pregnant women. Ultrasound Obstet Gynecol. 2020;56:106–9. doi: 10.1002/uog.22055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Carosso A, Cosma S, Borella F, Marozio L, Coscia A, Ghisetti V, et al. Pre-labor anorectal swab for SARS-CoV-2 in COVID-19 pregnant patients: is it time to think about it? Eur J ObstetGynecolReprodBiol. 2020;249:98–9. doi: 10.1016/j.ejogrb.2020.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ferrazzi E, Frigerio L, Savasi V, Vergani P, Prefumo F, Barresi S, et al. Vaginal delivery in SARS-CoV-2 infected pregnant women in Northern Italy: a retrospective analysis. Bjog. 2020;127:1116–21. doi: 10.1111/1471-0528.16278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Martinelli I, Ferrazzi E, Ciavarella A, Erra R, Iurlaro E, Ossola M, et al. Pulmonary embolism in a young pregnant woman with COVID-19. Thromb Res. 2020;191:36–7. doi: 10.1016/j.thromres.2020.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hantoushzadeh S, Shamshirsaz AA, Aleyasin A, Seferovic MD, Aski SK, Arian SE, et al. Maternal Death Due to COVID-19 Disease. Am J Obstet Gynecol. 2020;223:109.e1–16. doi: 10.1016/j.ajog.2020.04.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Karami P, Naghavi M, Feyzi A, Aghamohammadi M, Novin MS, Mobaien A, et al. Mortality of a pregnant patient diagnosed with COVID-19: A case report with clinical, radiological, and histopathological findings. Travel Med Infect Dis. 2020:101665. doi: 10.1016/j.tmaid.2020.101665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Alzamora MC, Paredes T, Caceres D, Webb CM, Valdez LM, La Rosa M. Severe COVID-19 during Pregnancy and Possible Vertical Transmission. Am J Perinatol. 2020;37:861–5. doi: 10.1055/s-0040-1710050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lyra J, Valente R, Rosario M, Guimaraes M. Cesarean Section in a Pregnant Woman with COVID-19: First Case in Portugal. Acta Med Port. 2020;33:429–31. doi: 10.20344/amp.13883. [DOI] [PubMed] [Google Scholar]
- 48.Kalafat E, Yaprak E, Cinar G, Varli B, Ozisik S, Uzun C, et al. Lung ultrasound and computed tomographic findings in pregnant woman with COVID-19. Ultrasound ObstetGynecol. 2020;55:835–7. doi: 10.1002/uog.22034. [DOI] [PubMed] [Google Scholar]
- 49.Gidlöf S, Savchenko J, Brune T, Josefsson H. COVID-19 in pregnancy with comorbidities: More liberal testing strategy is needed. Acta Obstetricia et Gynecologica Scandinavica. 2020;99:948–9. doi: 10.1111/aogs.13862. [DOI] [PubMed] [Google Scholar]
- 50.Zambrano LI, Fuentes-Barahona IC, Bejarano-Torres DA, Bustillo C, Gonzales G, Vallecillo-Chinchilla G, et al. A pregnant woman with COVID-19 in Central America. Travel Med Infect Dis. 2020:101639. doi: 10.1016/j.tmaid.2020.101639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lee DH, Lee J, Kim E, Woo K, Park HY, An J. Emergency cesarean section on severe acute respiratory syndrome coronavirus 2 (SARS- CoV-2) confirmed patient. Korean J Anesthesiol. 2020;73:347–351. doi: 10.4097/kja.20116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Novel Coronavirus Pneumonia Emergency Response Epidemiology Team. Vital surveillances: the epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19)-China. China CDC Wkly. 2020;2:113–22. [PMC free article] [PubMed] [Google Scholar]
- 53.Liang W, Feng Z, Rao S, Xiao C, Xue X, Lin Z, et al. Diarrhoea may be underestimated: a missing link in 2019 novel coronavirus. BMJ. 2020;69:1141–3. doi: 10.1136/gutjnl-2020-320832. [DOI] [PubMed] [Google Scholar]
- 54.Holshue ML, DeBolt C, Lindquist S, Lofy KH, Wiesman J, Bruce H, et al. First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020;382:929–36. doi: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA. 2020;323:1061–9. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Gu J, Han B, Wang J. COVID-19: gastrointestinal manifestations and potential fecal–oral transmission. Gastroenterology. 2020;158:1518–9. doi: 10.1053/j.gastro.2020.02.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Guan G, Gao L, Wang J, Wen X, Mao T, Peng S, et al. Exploring the mechanism of liver enzyme abnormalities in patients with novel coronavirus-infected pneumonia. Zhonghua Gan Zang Bing Za Zhi. 2020;28:E002. doi: 10.3760/cma.j.issn.1007-3418.2020.02.002. [DOI] [PubMed] [Google Scholar]
- 58.Chen H, Guo J, Wang C, Luo F, Yu X, Zhang W, et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet. 2020;395:809–15. doi: 10.1016/S0140-6736(20)30360-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Pan L, Mu M, Yang P, Sun Y, Wang R, Yan J, et al. Clinical characteristics of COVID-19 patients with digestive symptoms in Hubei, China: a descriptive, cross-sectional, multicenter study. Am J Gastroenterol. 2020;115:766–73. doi: 10.14309/ajg.0000000000000620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Budden KF, Gellatly SL, Wood DL, Cooper MA, Morrison M, Hugenholtz P, et al. Emerging pathogenic links between microbiota and the gut–lung axis. Nat Rev Microbiol. 2017;15:55–63. doi: 10.1038/nrmicro.2016.142. [DOI] [PubMed] [Google Scholar]
- 61.Guo W, Li M, Dong Y, Zhou H, Zhang Z, Tian C, et al. Diabetes is a risk factor for the progression and prognosis of COVID‐19. Diabetes Metab Res Rev. 2020:e3319. doi: 10.1002/dmrr.3319. [DOI] [PMC free article] [PubMed] [Google Scholar]