Abstract
This review aimed to compare suspensory and aperture quadriceps tendon autograft femoral and tibial fixation in primary anterior cruciate ligament reconstruction (ACL-R) and the clinical outcomes and complication profiles of each fixation method. Greater understanding of the optimal graft fixation technique for quadriceps tendon (QT) autografts may assist surgeons in improving outcomes after ACL-R. PubMed, EMBASE, and MEDLINE were searched from database inception to September 2017, and again to July 2018, and identified 3670 articles, 21 studies of which, satisfied inclusion/exclusion criteria. Across included studies, 1155 QT ACL-R patients [mean age 28.7 years (range, 15–59), mean post-operative follow-up 36.1 months (range, 3.4 −120 months)] were analyzed. Suspensory fixation on both sides demonstrated a higher percentage of patients (81.7%) achieving the highest rating of “A or B” on the International Knee Documentation Committee (IKDC) Knee Ligament Examination form compared to aperture fixation on both sides (67.7%). Moreover, suspensory fixation had a lower side-to-side difference in anterior laxity (1.6 mm) when compared to aperture fixation (2.3 mm). Among studies which reported graft failure, all of which employed aperture fixation, the rate was 3.2%. Across available data, primary ACL-R using QT grafts appears to have successful short-term outcomes with a short-term graft failure rate of 3% independent of fixation method. While there is limited data regarding the comparison of aperture and suspensory SQT fixation in ACL-R, the findings of this systematic review suggest that suspensory fixation and aperture fixation in both the femoral and tibial tunnels are equally efficacious based on clinical outcome data on IKDC grade and measured laxity.
INTRODUCTION
Multiple techniques for utilizing the quadriceps tendon (QT) autograft during anterior cruciate ligament reconstruction (ACL-R) have been described, including harvesting a combined quadriceps tendon, pre-patellar retinaculum, and patellar tendon autograft,[1] the central third of the quadriceps tendon with a patellar bone block (QTB), or an all soft-tissue quadriceps tendon (SQT) autograft.[2,3] Commonly cited reasons for using a QT autograft include prior evidence that QT autografts yield comparable or improved clinical outcomes with reduced graft site morbidity and improved knee extension when compared to bone patellar-tendon bone (BPTB) and hamstring tendon (HS) autografts.[4–11]
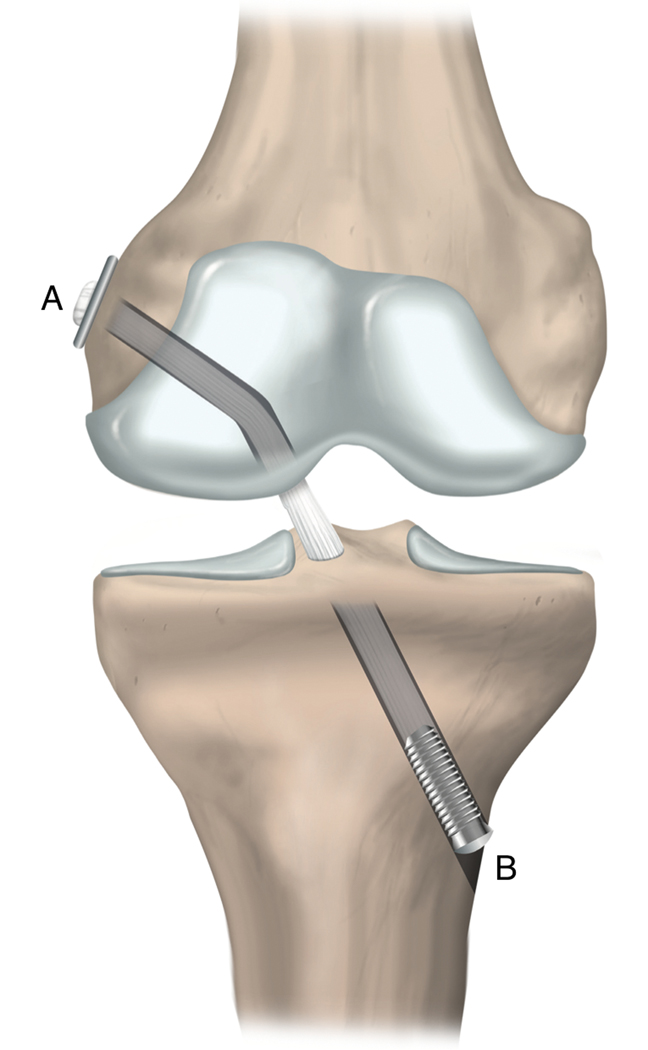
There are several aspects of primary ACL-R using QT autografts that may influence clinical outcomes, one of which is graft fixation. Graft fixation is commonly cited as the weakest link in the immediate post-operative period,[12,13] which has been supported by multiple animal studies.[14–16] Given the emphasis of early mobilization and immediate weight-bearing in current post-operative rehabilitation protocols,[17,18] optimizing graft fixation is paramount to maximizing the stability of the reconstructed ACL in the short- to immediate post-operative period, when graft-to-bone healing has not yet occurred.[19,20] Effective graft fixation is essential for minimizing graft slippage, improving graft strength and stiffness, and limiting longitudinal and sagittal graft motion. Methods of graft fixation are frequently categorized as suspensory (extra-tunnel; Figure 1A) or aperture (intra-tunnel; Figure 1B) fixation. Examples of suspensory fixation methods include suspensory cortical buttons, a screw and washer, and a cortical plate and screw, and examples of aperture fixation methods include interference screws. Several studies have reported methods of augmenting aperture fixation with either sutures or by using an anchor at the end of the graft, such as a bio-degradable poly-lactic acid (PLA) ball or a bone disc obtained during tunnel drilling, to help serve as an “anchor” during press-fit fixation.[3,21,22] The choice of graft fixation (suspensory vs. aperture), is considered the second most important factor, behind tunnel placement, in determining the integrity and success of ACL-R.[23]
Figure 1.
Representation of aperture and suspensory fixation methods. A: Suspensory fixation; B: Aperture fixation.
The choice of graft fixation is influenced by several factors, including surgeon preference and training, cost, ease of use, and clinical experience.[24] The ideal ACL-R fixation method must adhere to the principles of a strong, stiff, and slip-resistant fixation. In addition, it has been reported that the choice of graft fixation can influence risk of revision after ACL-R. [25] Multiple biomechanical studies have found that aperture fixation methods, which provide fixation closer to the tunnel aperture and more anatomically reproduce the native ACL insertion site, may provide greater tensile strength than suspensory fixation methods.[19,26,27] In contrast, other studies have found that suspensory fixation methods have a greater pull-out strength than multiple aperture fixation methods.[28,29] There are theoretical risks to aperture methods of fixation, including concerns that the screw may affect tendon-to-bone healing and the possibility of tunnel blow-out.[19] While some studies have found greater knee stability[26,27,30] and decreased graft-tunnel motion under anterior tibial loading[31] with aperture fixation of soft-tissue grafts when compared to suspensory fixation, there is no clear consensus on the optimal method of graft fixation.[19] Despite multiple randomized control trials comparing graft fixation with HT and BPTB, there have been no prospective studies comparing graft fixation with QT. The literature regarding QT remains exclusively in analyzing retrospective data and small patient cohorts and has not specifically examined the optimal graft fixation method.[24]
Thus, the purpose of this systematic review was to compare the outcomes and complications after primary ACL-R using quadriceps tendon autografts between different methods of graft fixation for both the femoral and tibial tunnels. It was hypothesized that, across all studies, suspensory (i.e. extra-tunnel) fixation on both sides, when compared to aperture (i.e. intra-tunnel) fixation, would be associated with improved clinical outcomes, including improved scores on patient-reported outcome measures, decreased anterior laxity, and decreased incidence of graft failure.
METHODS
Search Strategy
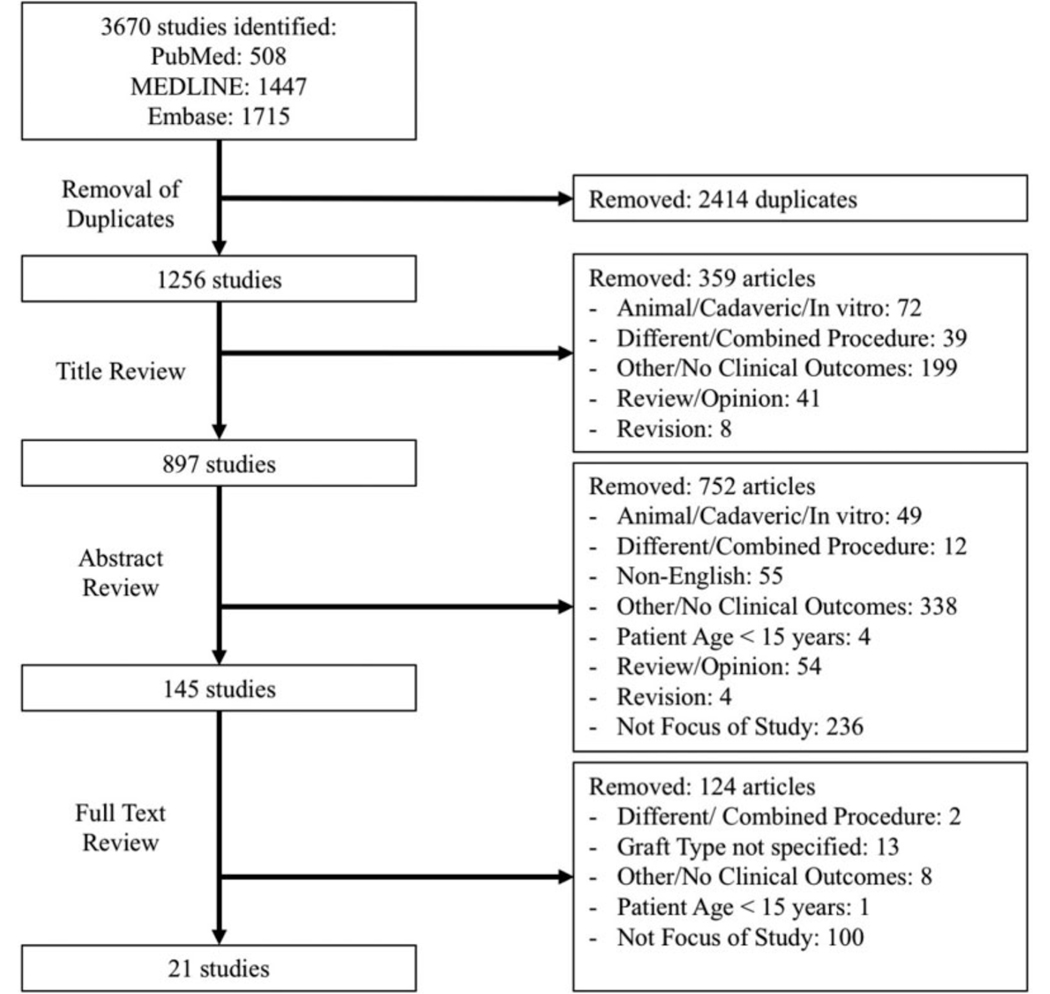
Three databases, specifically PubMed, Ovid (MEDLINE), and EMBASE, were searched from database inception until September 1, 2017 using the terms “quadriceps tendon,” “anterior cruciate ligament reconstruction, and “autograft.” The search was repeated on July 28, 2018 to capture any additional studies given the renewed interest in the quadriceps tendon autograft in primary ACL-R.[32] The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analyses) and R-AMSTAR (Revised Assessment of Multiple Systematic Reviews) statement was used for the reporting of study selection.[33,34] Two reviewers screened the titles, abstracts, and full-text articles independently and in duplicate (Figure 2). During the full-text screening process, the reviewers discussed any discrepancies to arrive at a consensus, and a third author was consulted to make the final decision on inclusion or exclusion.
Figure 2.
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram demonstrating the process for systematic review of the literature regarding aperture and suspensory fixation of quadriceps tendon autografts in ACLR.
Assessment of Study Eligibility
The research question as well as the inclusion and exclusion criteria were established a priori. The inclusion criteria were as follows: studies investigating the use of QT autografts during primary ACL-R, English-language studies; studies on humans 15 years or older of age; studies with reported clinical outcomes; and studies with all levels of evidence (Level I to V). Studies including the use of cross pins for aperture fixation were not included. Studies with only biomechanical or neuromuscular testing results, such as peak quadriceps torque, with no reported clinical outcomes or complications, were excluded.
Assessment of Agreement
Inter-reviewer agreements for the title, abstract, and full- text articles were determined with Cohen’s kappa coefficient (κ) statistic for quantifying inter-rater agreement. The values were categorized a priori using previously suggested guidelines as follows: κ of 0.81 to 0.99 was considered almost perfect agreement; κ of 0.61 to 0.80, substantial agreement; κ of 0.41 to 0.60, moderate agreement; κ of 0.21 to 0.40, fair agreement; and κ of 0.20 or less, slight agreement.[35]
Quality Assessment
The levels of evidence of all included studies were determined using the American Academy of Orthopaedic Surgeons classification system.[36] The methodologic quality of all included studies was assessed using the MINORS (Methodological Index for Non-randomized Studies) checklist.[37] Under the MINORS checklist, comparative and non-comparative studies may obtain maximum scores of 24 and 16, respectively. A minimum follow-up time of 12 months was deemed as an acceptable follow-up interval for the purposes of using the MINORS checklist.
Data Extraction and Analysis
Data was extracted from the included studies and recorded the results in a Microsoft Excel spreadsheet (version 2016; Microsoft, Redmond, WA). Study characteristics, including author, year of publication study design, and sample size were recorded. The reviewer also extracted descriptive statistics from each study including the patients’ age and sex, follow-up interval, and details of surgical management. Clinical outcomes at final follow-up were recorded. The primary outcomes assessed were percentage of patients presenting at follow up with International Knee Documentation Committee (IKDC) grades of A and B, Lysholm Score, anterior laxity, and postoperative positive pivot shift. Due to heterogeneous and limited reporting, these data were not amenable to a meta-analysis and were summarized descriptively. Descriptive statistics, including means, standard deviations, ranges, and percentages were calculated as appropriate. When an outcome was not reported across all studies, weighted means were calculated considering only the patients across studies in which that outcome was reported. Means were compared using a student’s t-test with pre-determined alpha of 0.05. All statistics were calculated using SPSS software (v24; IBM Corp).
RESULTS
Search Strategy
The initial search yielded a total of 3670 studies. After 2414 duplicates were removed, 1256 unique studies remained for assessment. A second search performed in July 2018 captured two additional studies since the original September 2017 search with perfect agreement between reviewers (κ=1). Systematic screening of the titles, abstracts, and full-text articles was performed, yielding twenty-one studies that met the inclusion criteria for evaluation in this review (Figure 2).[38–42] There was substantial agreement between reviewers at the title screening stage (κ=0.72) and almost-perfect agreement at the abstract (κ=0.81) and full-text (κ=0.91) screening stages.
Study Quality / Characteristics
Of the twenty-one studies included for assessment, there were two level II studies, fourteen level III studies, and six level IV studies. The studies included represented a diverse and international group of researchers (47.7% South Korea, 14.3% United States of America, 9.2% Switzerland, 4.7% Denmark, 4.7% Turkey, 4.7% Taiwan, 4.7% Brazil, 4.7% Japan, and 4.7% Austria). The median MINORS score for non-comparative studies was 6 ± 1.9, and the MINORS score for the single comparative study was 13.8 ± 2.6, indicating moderate quality studies. A detailed summary of the characteristics of the included studies is shown in Table 1. These studies examined a total of 1155 patients (29.3% female, 70.7% male) with a mean age of 28.7 years (range, 15–59) and mean post-operative follow-up of 36.1 months (range, 3.4 −120 months).
Table 1:
Study Characteristics
| Authors | Year | Country in which Study was Conducted | Study Design (Level of Evidence) | Number of Patients | Number of Knees | % Female | Age (years) | Follow-Up Time (months) |
|---|---|---|---|---|---|---|---|---|
| Aperture Fixation | ||||||||
| Cavaignac et al. | 2017 | Switzerland | Cohort Study (III) | 45 | 45 | 45% | 32.1 +/− 8 | 3.4 +/− 0.6 |
| Geib et al. | 2009 | United States of America | Retrospective Case Series (IV) | 41 | 41 | 46.3 | NR | 40.5 |
| Gorschewsky et al. | 2007 | Switzerland | Prospective Cohort Study (III) | 124 | 124 | NR | NR | 24 |
| Han et al. | 2008 | South Korea | Therapeutic Study (III) | 72 | 72 | 5.56% | 27.8 (15–51) | 39.7 (24–90) |
| Joseph et al. | 2006 | United States of America | Prospective Comparative Study (II) | 18 | 18 | NR | NR | NR |
| Kim et al. | 2009 | South Korea | Therapeutic Study (III) | 29 | 29 | 62.10% | 25.3 (20–39) | 24 |
| Kim et al. | 2009 | South Korea | Retrospective Comparative Study (III) | 21 | 21 | 14.30% | 27.1 (18–48) | 25.8 (24–37) |
| Kim et al. | 2009 | South Korea | Retrospective Cohort Study (III) | 21 | 21 | 14.30% | 27.1 +/− 9.94 (18–48) | 25.8 +/− 4.4 (24–37) |
| Kwak et al. | 2018 | Korea | Retrospective Cohort Study (III) | 45 | 45 | 15.60% | 34.5 +/− 12.8 | 29.8 +/−0 6.5 (24.9–44.3) |
| Lee et al. | 2007 | South Korea | “Diagnostic Study of Nonconsecutive patients without consistently applied reference gold standard” (III) | 137 | 137 | 10.20% | 27 (16–51) | 59 (37–73) |
| Lee et al. | 2007 | South Korea | Prospective Cohort Study (III) | 247 | 247 | 11.30% | 29 (16–58) | 44 (25–87) |
| Lee et al. | 2016 | South Korea | Cohort Study (III) | 48 | 48 | 8.30% | 31.12 (17–57) | 35.6 (24–61) |
| Lee et al. | 2004 | South Korea | Case Series (IV) | 67 | 67 | 13.40% | 28 (18–51) | 41 (27–49) |
| Lund et al. | 2014 | Denmark | Randomized Control Trial (II) | 26 | 26 | 16% | 30 +/− 9 | |
| Sofu et al. | 2013 | Turkey | Retrospective Cohort Study (III) | 23 | 23 | 8.70% | 26.8 | 37.6 (8–70) |
| Theut et al. | 2003 | United States of America | Prospective Case Series (IV) | 68 | 68 | 57.4 | 31 (15–46) | 20 (12–29) |
| Suspensory Fixation | ||||||||
| Chen et al. | 1999 | Taiwan | Prospective Case Series (IV) | 12 | 12 | 33.30% | 26 (20–39) | 18 (15–24) |
| Chen et al. | 2006 | South Korea | Therapeutic Study (III) | 34 | 34 | 35.30% | 26 (20–59) | 62 (48–84) |
| Guimaraes et al. | 2009 | Brazil | Prospective Cohort Study (III) | 17 | 17 | 11.80% | 28.53 | 10 years |
| Iriuchishima et al. | 2017 | Japan | Prospective Case Series (IV) | 20 | 20 | 90 | 49 | 12 |
| Runer et al. | 2018 | Austria | Prospective Cohort Study (III) | 40 | 40 | 42.50% | 34.6 +/− 11.0 | 6, 12, and 24 |
Surgical Technique
A summary of the surgical techniques used in each study is shown in Table 2. Femoral and tibial-sided QT fixations were performed by aperture fixation in 77.3% of patients (seventeen studies; 1032 patients) and suspensory fixation in 22.7 % of patients (five studies; 123 patients). The specific methods of fixation for the aperture fixation group were femoral and tibial fixation with bioabsorbable interference (BAI) screws (eight studies; 367 patients), femoral fixation with a metal interference screw and tibial fixation with a BAI screw (six studies; 457 patients), and both femoral and tibial fixation with metal interference screws (three studies; 208 patients). The specific methods of fixation for the suspensory fixation group were femoral aperture fixation using a metal interference screw and tibial suspensory fixation using a cortical screw and washer (three studies; 63 patients), fixation of the femoral side with a cortical button and the tibial side with a cortical plate and screw (one study; 20 patients), and fixation of the femoral side with a suspensory button and tibial side with a BAI screw (one study; 40 patients). Considering only the studies that reported femoral tunnel drilling techniques, transtibial drilling was used in 47% (eight studies; 375 patients) of aperture studies and in 20% (one study; 12 patients) of suspensory studies. The anteromedial portal drilling technique was used in 11.7% (two studies; 74 patients) of aperture studies and in 40% (two studies; 60 studies) of the suspensory studies. The included suspensory studies used QTB graft in 80% of studies and the SQT graft in the remaining 20%. The included aperture fixation studies used QTB graft in 81.3% of studies and SQT in 18.7% of studies. Across all studies, the thickness of the grafts (partial vs full-thickness) were not consistently reported.
Table 2:
Surgical Technique
| Authors | Year | Graft Type | Femoral Fixation | Tibial Fixation | Femoral Tunnel Drilling Technique | Graft Thickness |
|---|---|---|---|---|---|---|
| Aperture Fixation | ||||||
| Cavaignac et al. | 2017 | QTB | Intra-tunnel (Bioabsorbable Interference Screw) | Intra-tunnel (Bioabsorbable Interference Screw) | Anteromedial Portal | 9 +/− 0.62 mm |
| Geib et al. | 2009 | SQT | Intra-tunnel (Bioabsorbable interference screw, 2 mm smaller than tunnel) | Intra-tunnel (Bioabsorbable interference screw, 1 mm smaller than tunnel, augmented with sutures tied through periosteum) | Transtibial | 7–8 mm |
| Gorschewsky et al. | 2007 | QTB | Intra-tunnel (Bioabsorbable Interference Screw; 7×23 mm) | Intra-tunnel (Bioabsorbable Interference Screw; 7×23 mm) | Transtibial` | Full |
| Han et al. | 2008 | QTB | Intra-tunnel (Metal interference screw; 7 × 25 mm) | Intra-tunnel (Bioabsorbable interference screw 8/9 × 25 mm) | Not reported | 6–8 mm |
| Joseph et al. | 2006 | SQT | Intra-tunnel (Bioabsorbable interference screw, 23 mm long, same width as tunnel, augmented with bone disk anchor) | Intra-tunnel (Bioabsorbable interference screw, 23 mm long, same width as tunnel) | Not reported | 6–7 mm |
| Kim et al. | 2009 | QTB | Intra-tunnel (Bioabsorbable interference screw) | Intra-tunnel (Bioabsorbable interference screw | Anteromedial Portal | 8 mm |
| Kim et al. | 2009 | QTB | Intra-tunnel (Bioabsorbable Interference screw) | Intra-tunnel (Bioabsorbable Interference Screw) | Not reported | 6–7 mm |
| Kim et al. | 2009 | QTB | Intra-tunnel (Bioabsorbable Interference Screw) | Intra-tunnel (Bioabsorbable Interference Screw) | Not Reported | 6–7 mm |
| Kwak et al. | 2018 | QTB | Intra-tunnel (8×25 mm metal interference screw) | Intra-tunnel (10×25 mm Metal Interference Screw augmented by tying sutures over a cortical screw with knee extended) | Transtibial | 6–8 mm |
| Lee et al. | 2007 | QTB | Intra-tunnel (Metal Interference Screw, 7 × 25 mm) | Intra-tunnel (Bioabsorbable Interference Screw, 9/10 × 25 mm) | Transtibial | 9–10 mm |
| Lee et al. | 2007 | QTB | Intra-tunnel (Metal interference screw; 7×25 mm) | Intra-tunnel (Bioabsorbable interference screw; 9/10 × 25 mm) | Not reported | 7 mm |
| Lee et al. | 2004 | QTB | Intra-tunnel (Metal interference screw; 7×25mm) | Intra-tunnel (Bioabsorbable Interference Screw; 8/9×25 mm) | Not reported | 6–8 mm |
| Lee et al. | 2016 | QTB | Intra-tunnel (Metal interference screw) | Intra-tunnel (Bioabsorbable screw, 9–10 mm/25mm, augmented with sutures tied over a distal bicortical screw) | Transtibial | 6–8 mm |
| Lund et al. | 2014 | QTB | Intra-tunnel (Titanium interferences crew (7× 25 mm) | Intra-tunnel (Titanium interferences crew (7× 25 mm) | Transtibial | 9–10 mm |
| Sofu et al. | 2013 | QTB | Intra-tunnel (Metal interference screw) | Intra-tunnel (bioabsorbable interference screw) | Transtibial | Not reported |
| Theut et al. | 2003 | SQT | Intra-tunnel (Bioabsorbable interference screw, 23 mm long, same width as tunnel, augmented with bone disk anchor) | Intra-tunnel (Bioabsorbable interference screw, 23 mm long, same width as tunnel) | Transtibial | 6–7 mm |
| Suspensory Fixation | ||||||
| Chen et al. | 2005 | QTB | Intra-Tunnel (Interference screw, 20 mm long) | Extra-tunnel (Bicortical screw and washer) | Transtibial | Full |
| Chen et al. | 1999 | QTB | Intra-tunnel (Metal Interference Screw; 7/9 × 20 mm) | Extra-tunnel (Bicortical screw and washer) | Not reported | 6–7 mm |
| Guimaraes et al. | 2009 | QTB | Intra-tunnel (metal interference screw) | Extra-tunnel (Two ethibond #2 sutures and a cancellous screw with a washer) | Not reported | Not reported |
| Iriuchishima et al. | 2017 | SQT | Extra-tunnel (Cortical button) | Extra-tunnel (Cortical plate and screw) | Anteromedial Portal | Full |
| Runer et al. | 2018 | QTB | Extra-tunnel (Suspensory button) | Intra-Tunnel (Bioabsorbable Interference Screw, sutures were tied over an Endotack) | Anteromedial Portal | 5 mm |
Outcomes
A detailed summary of the outcomes reported in all included studies is shown in Table 3, and a comparison of weighted mean outcomes between suspensory and aperture fixation methods is shown in Table 4. There was a higher percentage of patients achieving A and B (A: Return to normal function; B: Return to nearly normal function) scores on the IKDC scale in the aperture fixation group (81.7%) compared to the suspensory fixation group (67.6%). There was no statistically significant difference in Lysholm Scores between the suspensory and aperture fixation groups (92.1 ± 1.4 vs. 91.4 ± 5.4.; p>0.05). Side-to-side difference in anterior laxity, as measured by KT-1000 or KT-2000, was decreased significantly in the suspensory compared to the aperture fixation group (1.64 mm ± 0.18 vs. 2.29 mm ± 0.92 mm; p<0.05). When a side-to-side difference in anterior laxity <3 mm was defined as an optimal outcome, there was one suspensory fixation study (12 patients) that reported 42% of patients meeting a final anterior laxity <3mm.[43] There were four aperture fixation studies (361 patients) that showed a range of 57%−75% of patients meeting a postoperative anterior laxity <3 mm (Ideal postoperative outcome).[44–47] Side-to-side differences at 60 degrees/second and 180 degrees/second using Cybex II were only reported for aperture fixation studies, with a mean across all reported data of 81.7 +/− 16 and 87.7 +/− 12.2 (187 patients), respectively. Only one study (40 patients) using suspensory fixation techniques reported postoperative pivot shift results (0%)[48] and ten studies (480 patients) using aperture fixation techniques reported findings of positive pivot shift (Grade 2 or greater) ranging from 0% to 33%.[9,44,45,47,49–54]
Table 3:
Clinical Outcomes and Complications
| Authors | Year | Femoral / Tibial Fixation | Outcome | Complications |
|---|---|---|---|---|
| Aperture Fixation | ||||
| Cavaignac et al. | 2017 | Intra-tunnel (Bioabsorbable Interference Screws used for both) | Lysholm: 89 +/− 6.9 KOOS: -Pain: 90 +/− 6.8 - Symptoms: 90 +/− 11.2 -ADL: 95 +/− 5.3 -Sport: 82 +/− 11.3 -QOL: 78 +/− 14.7 Tegner: -Last Follow-up: 5.9 +/− 1.4 -Difference in preoperative: 1 +/− 1.05 IKDC subjective: 84 +/− 13 Lachman (0–2): 0 (41 pts; 93.1%), 1 (4 pts; 6.9%) Pivot Shift (0–2): 0 (41 pts; 93.1%), 1 (4 pts; 6.9%) KT-1000: mean= 1.1 +/− 0.9 No. of Pts with >3mm difference: 5; 11.4% Extension Difference: 26.3 +/− 11.3 % Flexion Difference: 8.2 +/− 17.3 % |
1 re-rupture after re-trauma 3 total reoperations: Cyclops lesion (5.7 months); Femoral Screw Removal (13.1 months); Grade 3 cartilaginous injury of the medial condyle (25.2 months) |
| Geib et al. | 2009 | Intra-tunnel (Bioabsorbable interference screw / Bioabsorbable interference screw augmented with suture) | Side-to-side difference in anterior laxity with KT-1000 and manual maximum force: 0.51 mm IKDC Knee Examination Form: A = 18 (66.7%), B = 7 (25.9%), C = 2 (7.4%), D = 0 (0%) 23/41(56.0%) of patients had single-leg hop distances greater than 90% contralateral knee Flexion Deficit: 0.12° Extension Deficit: 0.41° Positive Pivot Shift: 0 (0%) |
Graft Failure: 1 (2%) Post-operative effusion: 0 (0%) |
| Gorschewsky et al. | 2007 | Intra-tunnel (Bioabsorbable interference screws used for both) | IKDC: A (11%), B (72%), C (17%), D (0%) Donor Site Morbidity: Normal (85%), Nearly Normal (15%). Radiographic Findings: Normal Joint Space (19; 20%), Joint Space <4 mm (61; 66%), Joint Space 2–4 mm (13; 14%), Joint Space <2mm (0) One-leg hop test: 82; 89% normal Lysholm Score: 94 +/− 9 Return to Sport: 76 pts (81%) |
2 pts (2.2%): Graft Rupture from re-trauma (18 months post-op) |
| Han et al. | 2008 | Intra-tunnel (Metal interference screw / Bioabsorbable Interference Screw) | Lysholm: Preop (70.7) vs Postop (91.5) Cybex II: At 6m (n=34): 60 degree/second (%) 59 ± 15 (n=19); 180 degree/second (%) 62 ± 17. At 1 year (n=25): 60 degree/second (%) 78 ± 13 (n=19); 180 degree/second (%) 82 ± 11. At 2 years: 60 degree/second (%) 82 ± 15 (n=19); 180 degree/second (%) 89 ± KT-1000: < 3: 48 (66.6%); 3–5: 21 (29.2%), 5–10: 3 (4.2%), >10: ROM: extension deficit < 5 degree: 3 (4.17%); extension deficit of 10 degrees: 1 (1.39%); flexion deficit of 10 degrees: 2 (2.78%); flexion deficit of 40 degree: 1 (1.39%) IKDC: Preoperative: I (strenuous): 38; II (moderate): 57; III (light): 5; IV (sedentary) 0 Postoperative: I (strenuous): 28; II (moderate): 56; III (light): 16; IV (sedentary) 0 IKDC Subjective Satisfaction: Grades: (A) Normal or (B) Nearly Normal: 66 patients (92%) |
Of the two patients with graft failure in the QTPB group, one had a traumatic rupture, which occurred while playing soccer 45 months after surgery, and the other graft failed from an unknown etiology (without a history of distinct injury), and the patient then underwent reoperation 30 months after surgery. |
| Joseph et al. | 2006 | Intra-tunnel (Bioabsorbable interference screw augmented with bone disk anchor / Bioabsorbable interference screw) |
Time to attainment of full extension: 3.9 weeks Time to attainment of straight leg raise without lag: 3.7 weeks Time to attainment of 120° of flexion while prone: 4.7 weeks |
None recorded |
| Kim et al. | 2009 | Intra-tunnel (Bioabsorbable interference screws used for both) | Preoperative Lachman (7, 24% Grade 3; 22, 76% Grade 2) vs Postoperative Lachman (20, 69% Grade 0; 9, 31% Grade 1) Preoperative Pivot-shift test (1, 3% Grade 3, 25, 86% Grade 2; 3, 10% Grade 1) vs Postoperative (29, 100% Grade 0) KT-2000 Postop assessment: (Mean +/− St. Dev (mm)= 2.03+1.11)/Side to side diff: <3 mm= 23, 79%; 3–5 mm=6,21%; >5 mm= 0,0%) Preop HSS Score (65.7 +/− 11.4) vs Postop HSS score (92.1 +/− 6.1) Preop Lysholm (51.7 +/− 10.7) vs Postop Lysholm (91.1 +/− 6.8) |
1 pt.: posterior femoral cortex perforated during fixation of anteromedial bundle 1 pt.: fixed patellar bone plug in tibial tunnel migrated proximally during pre-tensioning of graft |
| Kim et al. | 2009 | Intra-tunnel (Bioabsorbable interference screws used for both) | Postoperative Lachman: (17, 81% Grade 0; 2, 19% Grade 1; 2, 19% Grade 2) Postoperative Pivot Shift: (17, 85.7% Grade 0; 2, 14.3% Grade 1; 2, 14.3% Grade 2) KT-2000: Side to side difference: (<3 mm, 12; 3–5 mm, 6; >5 mm, 3) IKDC Score: Preinjury: (A, 9, 44%; B, 12, 56%) vs Follow-up: (A, 8, 38%; B, 10, 48%, C, 3, 14%) |
No Complications Reported |
| Kim et al. | 2009 | Intra-tunnel (Bioabsorbable interference screws used for both) | Postoperative Lachmann: Grade 0: 17, 81% Grade 1: 2, 19% Grade 2: 2 (19%) Grade 3: 0, 0% Postoperative Pivot Shift: Grade 0: 17, 85.7% Grade 1: 2, 14.3% Grade 2: 2, 14.3% Grade 3: 0, 0% Single-leg hop test: 17 pts (81%) KT-2000: <3 mm (12 pts) 3–5 mm (6 pts) >5 mm *3 pts) Anterior knee pain score: 90.2 IKDC A: Preop (9, 44%) vs Postop (8, 38%) B: Preop (12, 56%) vs Postop (12, 48%) C: preop (0, 0%) vs Postop (3, 14%) D: Preop (0) vs Postop (0) |
2 pts (9%) reported mild discomfort at the quadriceps tendon graft site |
| Kwak et al. | 2018 | Intra-Tunnel (Metal Interference Screw used for both) | Anterior Drawer Test: Preoperative (Grade 0, 4, 8.9%; Grade 1, 15, 33.3%; Grade 2, 21, 46.7%, Grade 3, 5, 11.1%) vs Postoperative (Grade 0, 32, 71.1%; Grade 1, 13, 28.9%; Grade 2, 0, 0.0%; Grade 3, 0, 0.0%) Lachman Test: Preoperative (Grade 0, 3, 6.7%; Grade 1, 14, 31.3%; Grade 2, 19, 42.2%, Grade 3, 9, 20.0%) vs Postoperative (Grade 0, 29, 64.4%; Grade 1, 15, 33.3%; Grade 2, 1, 2.2%; Grade 3, 0, 0.0%) Pivot Shift Test: Preoperative (Grade 0, 4, 8.9%; Grade 1, 22, 48.9%; Grade 2, 14, 31.1%, Grade 3, 5, 11.1%) vs Postoperative (Grade 0, 29, 64.4%; Grade 1, 16, 35.6%; Grade 2, 0, 0.0%; Grade 3, 0, 0.0%) KT-2000 (mm): Preoperative (4.5 +/− 1.8) vs Postoperative (1.4 +/− 1.2) KT-2000: <3 mm: Preop (5, 11.1%) vs Postop (34, 75.6%) 3–5 mm: Preop (30, 66.7%) vs Postop (11, 24.4%) >5 mm: Preop (10, 22.2%) vs Postop (0, 0%) IKDC score: Preop (42.7 +/− 22.6) vs Postop (67.3 +/− 16.8) Lysholm Score: Preop (62.4 +/− 8.4) vs Postop (87.0 +/− 5.3) Tegner Scale: Preop (2.8, 1.8–4) vs Postop (7.2, 6.3–8.2) KOOS: Preop (273.8 +/− 87.5) vs Postop (423.1 +/− 50.9) |
2 pts had paresthesia on lateral side of knee (disappeared after 2 months) 3 pts had clicking sensation in knee during activities (relieved after 3 months) |
| Lee et al. | 2007 | Intra-tunnel (Metal interference screw / bioabsorbable interference screw) | Lachmann Test: Negative (113, 82.48%) Pivot Shift: Grade 0 (100, 73%) Lysholm: Preoperative (73.5) vs Postoperative (93) Cybex: Preop (76.2%) vs Postop (84.70%) KT-1000: Preop (7.1 mm) vs Postop (2.4 mm) ROM: Preop (137.8 degrees) vs Postop (139.5 degrees) Flexion Contracture: Preop (0.8 Degrees) vs Postop (0.6 Degrees) |
Graft Rupture: 3 (2.19%) |
| Lee et al. | 2007 | Intra-tunnel (Metal interference screw, Bioabsorbable Interference Screw) | Lysholm: Preop (71) vs Postop (90) KT-1000: Preop (6.2 ± 2.5 mm (mean + SD); < 3: 43 (18%); 3–5: 92 (38%), 6–10: 103 (43%), >10: 2 (1%) vs Postop ( 2.4 ± 1.7 mm (mean + SD); < 3: 162 (68%); 3–5: 67 (28%), 6–10: 11 (5%), >10: 0) ROM: Preop (137.3) vs Postop ( 137.5° (mean); 234 (97.5%) had extension deficit of <3°; 235 (97.9%) had lack of flexion of <5° at latest follow-up) IKDC: 209 Pts (87.0%) were Grade A or B IKDC levels of activity: Strenuous of moderate (211) IKDC Knee Grade: Grade A or B, 212 pts (88.3%) |
Graft Rupture: 7/247 ruptures (4 traumatic, 3 graft failure) |
| Lee et al. | 2016 | Intra-tunnel (Metal interference screw / Bioabsorbable interference screw) | Anterior Drawer Test: Grade 0: Preop (5) vs Postop (34) Grade 1: Preop (25) vs Postop (13) Grade 2: Preop (15) vs Postop (1) Grade 3: Preop (3) vs Postop (0) Lachman Test: Grade 0: Preop (6) vs Postop (32) Grade 1: Preop (23) vs Postop (15) Grade 2: Preop (17) vs Postop (1) Grade 3: Preop (2) vs Postop (0) Pivot Shift Test: Grade 0: Preop (12) vs Postop (32) Grade 1: Preop (15) vs Postop (16) Grade 2: Preop (19) vs Postop (0) Grade 3: Preop (2) vs Postop (0) KT-2000 side-to-side difference mm: Preop (70.2 +/− 9.6) vs Postop (92.1 +/− 8.7) Tegner Activity Score: Preoperative (4.6 +/− 1.8) vs Postop (4.7+/− 1.2) IKDC Subjective Score: Preop (60.3 +/− 17.8) vs Postop (80.2 +/− 10.0) Extensor Strength (60 deg/s) 1-year (71.9 +/− 24.4) vs 2-year (81.0 +/− 17.7) Extensor Strength (180 deg/s) 1-year (73.5 +/− 25.1) vs 2-year (83.8 +/− 17.8) Flexor Strength (60 deg/s) 1-year (87.0 +/− 15.7) vs 2-year (92.2 +/− 17) Flexor Strength (180 deg/s) 1-year (94.6 +/− 17.1) vs 2-year (99.6 +/− 15.0) |
|
| Lee et al. | 2004 | Intra-tunnel (Metal interference screw / Bioabsorbable Interference Screw) | Lachman Test: Preop (Grade 1: 10; Grade 2: 52; Grade 3: 5) vs Postop (Grade 0: 47; Grade 1: 17; Grade 2: 3) Anterior Drawer Test: Preop (Grade 1: 11; Grade 2: 50; Grade 3: 6) vs Postop (Grade 0: 50; Grade 1: 14; Grade 2: 3) Pivot Shift Test: Preop (Grade 1: 11; Grade 2: 42; Grade 3: 14) vs Postop (Grade 0: 41; Grade 1: 23; Grade 2: 3) KT-2000: <2 mm: Preop (0%) vs Postop (75%) 3–5 mm: Preop (15%) vs Postop (19%) 6–10 mm: Preop (77%) vs Postop (6%) >10 mm: Preop (8%) vs Postop (0%) Final IKDC: I (13%), II (75%), III (12%), IV (0%) Overall Knee Function Subjective Score: -Normal (45%) - Nearly Normal (42%) - Abnormal (12%) - Severe (1%) Quadriceps strength (Cybex II): - 60degrees/sec: Preop (72 +/− 14%) vs 6 Mo (64+/−15%) vs 12 Mo (82+/−13%) vs 24 Mo (82+/−15%) - 180 degrees/sec: Preop (78+/−11%) vs 6 Mo (74+/−20%) vs 12 Mo (82+/−13%) vs 24 Mo (89+/−8%) |
4 pts: Revision ACLR (6%) |
| Lund et al. | 2014 | Intra-tunnel (Titanium interferences crews used for both) | Average KOOS Score: Preoperative (65 +/− 20) vs 1 Year (68 +/− 21) vs 2 years (82 +/− 16) Subjective IKDC Score: Preoperative (68 +/− 14) vs 1 Year (76 +/− 16) vs 2 Years (84 +/− 13) KT-1000 Side to side difference (1.1 +/− 1.4 mm) <2 mm AP laxity (77%) 3–4 mm (19%) >5 mm (4%) Positive Pivot Shift at 1 year: (14%) |
48% of pts experienced crural sensitivity loss of 39 cm2 1 pt.: Early superficial infection treated successfully with IV antibiotics 1 pt.: Medial pain 2 years postop with inflamed medial plica that upon resection resulted in relief of symptoms. |
| Sofu et al. | 2013 | Intra-tunnel (metal interference screw / bioabsorbable interference screw) | Lysholm Score: <64 (poor): Preop (22, 95.6%) vs Postop (1, 4.3%) 65–83 (Fair): Preop (1, 4.4%) vs Postop (2, 8.7%) 84–94 (Good): Preop (0, 0%) vs Postop (14, 60.8%) 95–100 (Excellent): Preop (0, 0%) vs Postop (6, 26.2%) Single Leg Hop Test: 10 pts, 43.5% could achieve 90% performance at follow-up KT-2000: Operated knee joint laxity mm: 5.65 (3.5–8.0); Health knee joint laxity mm: 2.86 (1.5–4.0) |
|
| Theut et al. | 2003 | Intra-tunnel (Bioabsorbable interference screw augmented with bone disk anchor / Bioabsorbable interference screw) |
Side-to-side difference in anterior laxity with KT-1000 and manual maximum force: 2.1 m | Graft Failure: 4 (5.9%) |
| Suspensory Fixation | ||||
| Chen et al. | 1999 | Intra-tunnel (Metal Interference Screw / Bicortical Screw and Washer) | IKDC Categories: Subjective: (5 normal, 5 nearly normal, 2 abnormal) Symptoms (5 normal, 6 nearly normal, 1 abnormal) ROM (9 normal, 2 nearly normal, 1 abnormal) Laxity (5 normal, 6 nearly normal, 1 abnormal) Crepitus (9 normal, 2 nearly normal, 1 abnormal) Donor Site (10 normal, 1 nearly normal, 1 abnormal) X-ray (11 normal, 1 nearly normal) Functional Test (4 normal, 6 nearly normal, 2 abnormal) Overall Final Rating (7 normal, 3 nearly normal, 2 abnormal) KT-1000 Results: (<3mm=5 pts; 4–5 mm=6 pts; >5 mm=1 pt.) 100-point knee scale (Mean w range=86.5, 81–93) 11/12 patients recovered quadriceps strength to 80% of normal knee after 1 year Mean Quadriceps isokinetic percentage = 86% (71–105%) |
1 pt.: Mild harvest site tenderness 1 pt.: Patellofemoral pain |
| Chen et al. | 2006 | Intra-tunnel (Interference screw / Bicortical screw and washer?) | Lysholm knee scores: Preoperative Mean +/− SD (61.4 +/− 8.9) vs Postoperative Mean +/− SD (93.0 +/− 7.9) IKDC Activity Level: Pre-operative Activity level (Strenous:5; Moderate: 4; Light: 6; Sedentary: 19) vs Postoperative Activity (Strenuous: 17; Moderate: 9; Light: 5; Sedentary: 3) Anterior Knee Laxity (KT-1000 test): Preoperative Mean +/− SD (11.88 +/− 1.09) vs Postoperative (1.74+/− 1.80) Lachman Test: Preoperative (24 Grade III; 10 Grade IV) vs Postoperative (30 Grade I; 3 Grade II; 1 Grade III) Thigh Girth: (Preoperative (14.26 +/− 5.69 mm) vs Last Follow-up (9.65 +/− 5.53); p<0.01) Extensor Strength Ratio: Preoperative (79.71 +/− 8.06) vs Postoperative (91.65 +/− 8.09) mm; p<0.01 Flexor Strength Ratio: Preoperative (82.62 +/− 9.25) vs Follow-up (90.18 +/− 8.59) mm; p<0.01) |
Two patients sustained stitch abscesses at incision wound that needed retrieval of stiches. Two complained of numbness at lateral side of original tibial incision. One complained of irritation of tibial screw head that was removed later. |
| Guimaraes et al. | 2009 | Intra-tunnel (Metal interference screw / Cancellous screw with washer) | Lysholm: 1st year (98.71 +/− 2.47) vs 10th year (97.35 +/− 3.12) HSS Score: 1st year (95.07 +/− 5.23) vs 10th year (94.87 +/− 4.16) 16 patients: Thigh diameter 2 cm lower than other leg Lachmann test negative in 13 pts (76.47%) Anterior drawer test negative in 12 pts (70.59%) No decreases in patellofemoral joint space in any patients |
|
| Iriuchishima et al. | 2017 | Extra-tunnel (Cortical button / Cortical plate and screw) |
IKDC Knee Examination Form: A=18 (90%), B = 2 (10%), C = 0 (0%), D = 0 (0%) Mean anterior tibial translation on stress radiograph: 1.0 +/− 0.8 mm Positive Pivot Shift: 0 (0%) Mean quadriceps strength pre-operatively and 3, 6, 9, 12 months post-operatively (compared to contralateral extremity): 90.5 ± 19, 67.8 ± 21.4, 84 ± 17.5, 87.5 ± 15, and 85.1 ± 12.6 % Mean hamstrings strength pre-operatively and 3, 6, 9, 12 months post-operatively (compared to contralateral extremity): 99.5 ± 13.7, 78.7 ± 11.4, 90.5 ± 19, 91 ± 10.3 and 96.7 ± 13.8 % |
Graft Site Pain: 0 (0%) |
| Runer et al. | 2018 | Extra-Tunnel (Endobutton / Hybrid Interference Screw with Endotack) | Lysholm: Pre-injury (94.7 +/− 8.2) vs 6 Mo (87.2 +/− 10.4) vs 12 Mo (88.8 +/− 10.6) vs 24 Mo (93.4 +/− 7.5) VAS Pain: Pre-injury (0.90 +/− 1.1) vs 6 Mo (1.6 +/− 1.8) vs 12 Mo (1.2 +/− 1.4) vs 24 Mo (0.6 +/− 1.0) Tegner Score: Pre-injury (6; 1–9) vs 6 Mo (6; 3–9) vs 12 Mo (6; 3–9) vs 24 Mo (6; 2–9) Return to Activity: 6 months (80%), 12 Months (80%), 24 Months (67%) |
|
Table 4:
Comparison of Intra- and Extra-Tunnel Quadriceps Tendon Graft Fixation
| Outcome Measure | Aperture Fixation | Suspensory Fixation | Significant? |
|---|---|---|---|
| Score of “A and B” on IKDC Knee Ligament Examination Form (%) | 81.7% | 67% | Yes; P<0.05 |
| Lysholm Score | 91.4 +/− 5.4 | 92.1 +/− 1.4 | No; P>0.05 |
| Mean instrumented anterior laxity (mm) | 2.29 mm +/− 0.92 mm | 1.64 mm +/− 0.18 mm | Yes; P<0.05 |
| Graft Failure (%) | 3.2% | NR |
Complications
Incidence of graft failure (rupture) was only reported in eight studies (801 patients), all of which used aperture fixation. Considering only the patients in these eight studies, the mean incidence of graft failure was 3.2%. Of these studies reporting, 80% of those studies used the transtibial technique for tunnel drilling. There was no incidence of graft failure reported in those studies using suspensory fixation techniques. Regardless of graft fixation method, there was no reported data across various permutations of graft fixation as it pertained to graft strength, graft stiffness, and graft slippage. Three suspensory studies reported postoperative graft site pain or irritation including and ranging from 0% graft pain (0/20 patients),[55] 8.8% (3/34 patients),[56] and 16.7% (2/12 patients).[43] One aperture study reported mild graft site discomfort in 9% of patients (2/21 patients).[45] Two studies using aperture fixation reported postoperative paresthesia rates including 48% of patients experiencing a loss crural sensitivity in one study (12/26 patients)[52] and 4.4% of patients experiencing self-resolving lateral knee paresthesia (2/45 patients).[51]
DISCUSSION
With regards to quadriceps autograft fixation in primary ACL reconstruction, aperture fixation techniques resulted in: more “Normal” and “Nearly Normal” IKDC outcomes; less abnormal differences in side-side KT-1000- and KT-2000 anterior laxity; but higher rates of positive pivot shift. The primary finding of this systematic review was that, across the twenty-one studies that met inclusion criteria, neither aperture nor suspensory graft fixation appear to have improved outcomes across the majority of reported data, disproving the hypothesis under study. This finding aligns well with multiple previous studies and meta-analyses that have found no difference in patient-reported outcomes or anterior laxity between aperture and suspensory fixation methods for other graft options.[57,58] However, it is worth noting that no prior studies were able to be found that specifically looked at QT autografts when comparing fixation methods. While the conclusions of this study are limited by comparatively fewer studies of QT autografts compared to other more commonly used graft choices, the results of this review nevertheless support the use of either aperture or suspensory fixation methods during ACL-R with QT autografts.
A greater portion of the patients who underwent aperture fixation on both sides had a higher IKDC knee examination form rating of “A or B” than those who underwent suspensory fixation. Moreover, the mean anterior laxity for patients who underwent suspensory fixation was less than that of aperture fixation on both sides. In addition, when anterior laxity was only reported as <3mm total laxity, the studies using aperture fixation reported a larger percentage of patients attaining anterior laxity <3mm compared to suspensory fixation. This discrepancy in findings is most likely indicative of heterogeneous reporting including different methods of measurement of anterior laxity (KT-1000 vs KT-2000) and reporting of results (mean laxity vs laxity ranges).In addition, quantitative measures of anterior laxity are susceptible to measurement errors as the positioning of the device, experience of the user, and low inter-rater reliability all can contribute to discrepancies in measurement.[59,60] These discrepancies and limitations of quantifying anterior laxity preclude any conclusions from being drawn from this data as well as suggest that the observed difference in anterior laxity reported within is clinically insignificant. While these findings may align with the results of previous studies which have shown that aperture fixation with BAI screws is associated with lower loads-to-failure than suspensory fixation with cortical buttons,[61,62] further studies are needed to draw any definitive conclusions regarding the optimal method of fixation for QT autografts. Moreover, given that only not all included studies reported subjective outcomes, it is unclear whether any of these differences in objective measures are clinically significant.
Previous literature comparing graft fixation methods for other grafts have found varying results. One meta-analysis reported a lower graft failure rate with interference screws (i.e. aperture fixation), than all non-interference screw fixation types for femoral fixation of HS autografts.[63] In contrast to this, one meta-analysis of six randomized-controlled trials found no difference in patient-reported outcomes or post-operative anterior laxity when comparing aperture fixation with cross pins versus suspensory fixation with cortical buttons.[57] Similarly, one meta-analysis of 66 studies found no difference in anterior laxity on instrumented testing between suspensory and aperture fixation.[58] Despite the presence of numerous meta-analyses comparing methods of aperture and suspensory fixation, it remains unclear whether there is any clinically significant difference between aperture and suspensory fixation during ACL-R. Disparities among studies may be explained by the notion that graft fixation is another aspect of ACL-R that needs to be individualized for each patient based on factors such as age and concomitant osteoporosis.[64,65]
Graft failure (as defined as graft rupture) was only reported in studies using aperture fixation. Across the available clinical data, the mean overall failure rate of 3.2% reported for aperture fixation ACL-R is low in comparison to the previously reported rates of failure. Reported rates of graft failure range from 6%−16.8% for BPTB and HS autografts[66–69] and 8.8–34.4% for allografts.[67,70,71] The low rate observed in the present investigation is likely related to the relatively short length of follow-up in this cohort which may not capture cases of ACL failure that take place with higher rates of return to sport 12 months after surgery.[72] In addition, since the cause graft failure was inconsistently reported across included studies, it is possible that the reported rate of specific types of graft failure for QT fixation are even lower than reported. A multicenter epidemiological review of ACL-R reported that graft failure is a product of traumatic injury to the graft, biologic etiology, and technical error regarding graft preparation and fixation.[73] Traumatic injury has been reported to cause 32% of ACL-R failure followed by technical error at 24%.[73] While trauma remains the greatest cause of graft failure, technical error, including fixation technique, accounts for a not insignificant amount of graft failure.[74,75][76,77][77,78]
While QT is currently not the most popular surgical approach for ACL-R, it is important to note that QT is gaining increasing popularity among surgeons. This growing interest in the use of the QT for ACL-R is reflected in the development of the International Quadriceps Tendon Interest (IQTI) initiative. The IQTI was created to garner international interest in developing further understanding and application of QT ACL-R. With the development of international interest in the subject, it is quite possible that this paucity in research and understanding regarding QT ACL-R will be narrowed in the near future. An inherent strength of this review stems from the novelty of comparing graft fixation technique using QT for ACL-R. This is the first systematic review to demonstrate equal efficacy of aperture and suspensory fixation for QT ACL-R in both patient reported outcomes and clinical measure of postoperative success.
This systematic review was limited by both the quantity and quality of available studies reporting on clinical outcomes and complications after primary ACL-R using QT autografts. All the studies included in this review had methodologic flaws including a lack of a control group for comparison and low sample sizes. It should be noted that, although there were differences in reported objective outcomes between certain methods of graft fixation, heterogeneity in reporting precluded any statistical comparisons across studies. Moreover, while a variety of previous studies have examined fixation systems with hamstring tendon grafts using cyclic loading tests,[28,29,79] there are less such studies with QT and, in addition to clinical studies, future biomechanical in vitro testing of QT will also be valuable. The low failure rate for QT grafts reported here may be due to shorter follow-up times in the present studies. Studies of graft fixation are susceptible to numerous confounding factors. While many studies of ACL-R often are assumed to utilize the principles of anatomic reconstruction, it has been noted that details regarding surgical technique in ACL-R studies are often under-reported.[80] The results of studies of graft fixation may be profoundly influenced by tunnel placement, which has been shown to affect the transmission of forces across the graft and graft fixation system.[81,82]
The relative paucity of studies available for inclusion in this systematic review despite the high volume of literature on primary ACL-R reflects the fact that, across all autograft types, the QT has historically not been as commonly used as other graft sources such as the hamstring and patellar tendons. While the literature regarding QT autograft fixation is currently limited, future studies with higher levels of evidence will enhance clinical understanding. Large cohort trials in combination with cadaveric and robotic studies are essential for answering questions of graft strength, stiffness, and slippage with different permutations of graft fixation.
CONCLUSIONS
Across available data, primary ACL-R using QT grafts appears to have successful short-term outcomes with a short-term graft failure rate of 3% independent of fixation method. While there is limited data regarding the comparison of aperture and suspensory SQT fixation in ACL-R, the findings of this systematic review suggest that suspensory fixation and aperture fixation in both the femoral and tibial tunnels are equally efficacious based on clinical outcome data on IKDC grade and measured laxity.
LIST OF ABBREVIATIONS
- ACL-R
Anterior Cruciate Ligament Reconstruction
- QT
Quadriceps Tendon
- QTB
Quadriceps Tendon with a Patellar Bone Block
- SQT
Soft-tissue Quadriceps Tendon
- BPTB
Bone Patellar-tendon Bone
- HS
Hamstring Tendon
- PLA
Poly-lactic Acid
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-analyses
- MINORS
Methodological Index for Non-randomized Studies
- IKDC
International Knee Documentation Committee
- BAI
Bioabsorbable Interference
- IQTI
International Quadriceps Tendon Interest Group
Footnotes
Level of Evidence:
Systematic Review of Level III/IV studies, Level IV
REFERENCES
- 1.MARSHALL JL, WARREN RF, WICKIEWICZ TL et al. The Anterior Cruciate Ligament: A Technique of Repair and Reconstruction. Clin Orthop Relat 1979; 143: 97–106 [PubMed] [Google Scholar]
- 2.Blauth W. RESTORATION OF THE ANTERIOR CRUCIATE LIGAMENT WITH A 2-STRIP QUADRICEPS TENDON GRAFT. Unfallheilkunde-traumatology 1984; 87: 45–51 [PubMed] [Google Scholar]
- 3.Fulkerson JP. Central quadriceps free tendon for anterior cruciate ligament reconstruction. Oper Tech Sports Med 1999; 7: 195–200 [Google Scholar]
- 4.Lee S, Seong SC, Jo H et al. Outcome of anterior cruciate ligament reconstruction using quadriceps tendon autograft. Arthroscopy 2004; 20: 795–802 [DOI] [PubMed] [Google Scholar]
- 5.Antonogiannakis E, Yiannakopoulos CK, Hiotis I et al. Arthroscopic anterior cruciate ligament reconstruction using quadriceps tendon autograft and bioabsorbable cross-pin fixation. Arthroscopy 2005; 21: 894. e891–894. e895 [DOI] [PubMed] [Google Scholar]
- 6.Cavaignac E, Coulin B, Tscholl P et al. Is Quadriceps Tendon Autograft a Better Choice Than Hamstring Autograft for Anterior Cruciate Ligament Reconstruction? A Comparative Study With a Mean Follow-up of 3.6 Years. Am J Sports Med 2017; 45: 1326–1332 [DOI] [PubMed] [Google Scholar]
- 7.Pigozzi F, Di Salvo V, Parisi A et al. Isokinetic evaluation of anterior cruciate ligament reconstruction: quadriceps tendon versus patellar tendon. J Sports Med Phys Fitness 2004; 44: 288. [PubMed] [Google Scholar]
- 8.Gorschewsky O, Klakow A, Putz A et al. Clinical comparison of the Autologous Quadriceps Tendon (BQT) and the Autologous Patella Tendon (BPTB) for the reconstruction of the Anterior Cruciate Ligament. Knee Surg Sports Traumatol Arthrosc 2007; 15: 1284–1292 [DOI] [PubMed] [Google Scholar]
- 9.Kim S-J, Kumar P, Oh K-S. Anterior cruciate ligament reconstruction: autogenous quadriceps tendon–bone compared with bone–patellar tendon–bone grafts at 2-year follow-up. Arthroscopy: The Journal of Arthroscopic & Related Surgery 2009; 25: 137–144 [DOI] [PubMed] [Google Scholar]
- 10.Han HS, Seong SC, Lee S et al. Anterior cruciate ligament reconstruction. Clin Orthop Relat 2008; 466: 198–204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Adams DJ, Mazzocca AD, Fulkerson JP. Residual strength of the quadriceps versus patellar tendon after harvesting a central free tendon graft. Arthroscopy 2006; 22: 76–79 DOI: 10.1016/j.arthro.2005.10.015 [DOI] [PubMed] [Google Scholar]
- 12.Noyes FR, Butler D, Grood E et al. Biomechanical analysis of human ligament grafts used in knee-ligament repairs and reconstructions. J Bone Joint Surg Am 1984; 66: 344–352 [PubMed] [Google Scholar]
- 13.Kurosaka M, Yoshiya S, Andrish JT. A biomechanical comparison of different surgical techniques of graft fixation in anterior cruciate ligament reconstruction. Am J Sports Med 1987; 15: 225–229 [DOI] [PubMed] [Google Scholar]
- 14.Rodeo SA, Arnoczky SP, Torzilli PA et al. Tendon-healing in a bone tunnel. A biomechanical and histological study in the dog. J Bone Joint Surg Am 1993; 75: 1795–1803 [DOI] [PubMed] [Google Scholar]
- 15.Goradia VK, Rochat MC, Kida M et al. Natural history of a hamstring tendon autograft used for anterior cruciate ligament reconstruction in a sheep model. Am J Sports Med 2000; 28: 40–46 [DOI] [PubMed] [Google Scholar]
- 16.Papageorgiou CD, Ma CB, Abramowitch SD et al. A multidisciplinary study of the healing of an intraarticular anterior cruciate ligament graft in a goat model. Am J Sports Med 2001; 29: 620–626 [DOI] [PubMed] [Google Scholar]
- 17.Wright RW, Haas AK, Anderson J et al. Anterior cruciate ligament reconstruction rehabilitation: MOON guidelines. Sports Health 2015; 7: 239–243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Van Grinsven S, Van Cingel R, Holla C et al. Evidence-based rehabilitation following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 2010; 18: 1128–1144 [DOI] [PubMed] [Google Scholar]
- 19.Brand J, Weiler A, Caborn DN et al. Graft fixation in cruciate ligament reconstruction. Am J Sports Med 2000; 28: 761–774 [DOI] [PubMed] [Google Scholar]
- 20.Singhal MC, Fites BS, Johnson DL. Fixation devices in ACL surgery: what do I need to know? Orthopedics 2005; 28: 920–924 [DOI] [PubMed] [Google Scholar]
- 21.DeAngelis JP, Fulkerson JP. Quadriceps tendon--a reliable alternative for reconstruction of the anterior cruciate ligament. Clin Sports Med 2007; 26: 587–596 DOI: 10.1016/j.csm.2007.06.005 [DOI] [PubMed] [Google Scholar]
- 22.Nagarkatti DG, McKeon BP, Donahue BS et al. Mechanical evaluation of a soft tissue interference screw in free tendon anterior cruciate ligament graft fixation. Am J Sports Med 2001; 29: 67–71 [DOI] [PubMed] [Google Scholar]
- 23.Jagodzinski M, Krettek C. Evolving Techniques in ACL Graft Fixation. Techniques in Orthopaedics 2013; 28: [Google Scholar]
- 24.Macaulay AA, Perfetti DC, Levine WN. Anterior cruciate ligament graft choices. Sports health 2012; 4: 63–68 DOI: 10.1177/1941738111409890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Persson A, Gifstad T, Lind M et al. Graft fixation influences revision risk after ACL reconstruction with hamstring tendon autografts. Acta orthopaedica 2018; 89: 204–210 DOI: 10.1080/17453674.2017.1406243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ishibashi Y, Rudy TW, Livesay GA et al. The effect of anterior cruciate ligament graft fixation site at the tibia on knee stability: evaluation using a robotic testing system. Arthroscopy 1997; 13: 177–182 [DOI] [PubMed] [Google Scholar]
- 27.Morgan CD, Kalmam VR, Grawl DM. Isometry testing for anterior cruciate ligament reconstruction revisited. Arthroscopy 1995; 11: 647–659 [DOI] [PubMed] [Google Scholar]
- 28.Giurea M, Zorilla P, Amis AA et al. Comparative pull-out and cyclic-loading strength tests of anchorage of hamstring tendon grafts in anterior cruciate ligament reconstruction. Am J Sports Med 1999; 27: 621–625 [DOI] [PubMed] [Google Scholar]
- 29.Magen HE, Howell SM, Hull ML. Structural properties of six tibial fixation methods for anterior cruciate ligament soft tissue grafts. Am J Sports Med 1999; 27: 35–43 [DOI] [PubMed] [Google Scholar]
- 30.Johnson D, Houle J, Almazan A. Comparison of intraoperative AP translation of two different modes of fixation of the grafts used in ACL reconstruction. Arthroscopy 1998; 14: 425 [Google Scholar]
- 31.Tsuda E, Fukuda Y, Loh JC et al. The effect of soft-tissue graft fixation in anterior cruciate ligament reconstruction on graft-tunnel motion under anterior tibial loading. Arthroscopy 2002; 18: 960–967 [DOI] [PubMed] [Google Scholar]
- 32.Slone HS, Romine SE, Premkumar A et al. Quadriceps tendon autograft for anterior cruciate ligament reconstruction: a comprehensive review of current literature and systematic review of clinical results. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association 2015; 31: 541–554 DOI: 10.1016/j.arthro.2014.11.010 [DOI] [PubMed] [Google Scholar]
- 33.Moher D, Liberati A, Tetzlaff J et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS medicine 2009; 6: e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kung J, Chiappelli F, Cajulis OO et al. From Systematic Reviews to Clinical Recommendations for Evidence-Based Health Care: Validation of Revised Assessment of Multiple Systematic Reviews (R-AMSTAR) for Grading of Clinical Relevance. The open dentistry journal 2010; 4: 84–91 DOI: 10.2174/1874210601004020084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Landis JR, Koch GG. The measurement of observer agreement for categorical data. biometrics 1977: 159–174 [PubMed] [Google Scholar]
- 36.Wright JG. Levels of Evidence and Grades of Recommendations. AAOS Bulletin 2005: [Google Scholar]
- 37.Slim K, Nini E, Forestier D et al. Methodological index for non‐randomized studies (MINORS): development and validation of a new instrument. ANZ J Surg 2003; 73: 712–716 [DOI] [PubMed] [Google Scholar]
- 38.Geib TM, Shelton WR, Phelps RA et al. Anterior cruciate ligament reconstruction using quadriceps tendon autograft: intermediate-term outcome. Arthroscopy 2009; 25: 1408–1414 [DOI] [PubMed] [Google Scholar]
- 39.Schulz AP, Lange V, Gille J et al. Anterior cruciate ligament reconstruction using bone plug-free quadriceps tendon autograft: intermediate-term clinical outcome after 24–36 months. Open Access J Sports Med 2013; 4: 243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Theut PC, Fulkerson JP, Armour E et al. Anterior cruciate ligament reconstruction utilizing central quadriceps free tendon. Orthop Clin North Am 2003; 34: 31–39 [DOI] [PubMed] [Google Scholar]
- 41.Joseph M, Nissen C, Fulkerson J et al. Short-term recovery after anterior cruciate ligament reconstruction: a prospective comparison of three autografts. Orthopedics 2006; 29: [DOI] [PubMed] [Google Scholar]
- 42.Iriuchishima T, Ryu K, Okano T et al. The evaluation of muscle recovery after anatomical single-bundle ACL reconstruction using a quadriceps autograft. Knee Surg Sports Traumatol Arthrosc 2017; 25: 1449–1453 [DOI] [PubMed] [Google Scholar]
- 43.Chen CH, Chen WJ, Shih CH. Arthroscopic anterior cruciate ligament reconstruction with quadriceps tendon-patellar bone autograft. The Journal of trauma 1999; 46: 678–682 [DOI] [PubMed] [Google Scholar]
- 44.Kim SJ, Chang JH, Kim TW et al. Anterior cruciate ligament reconstruction with use of a single or double-bundle technique in patients with generalized ligamentous laxity. The Journal of bone and joint surgery American volume 2009; 91: 257–262 DOI: 10.2106/jbjs.H.00009 [DOI] [PubMed] [Google Scholar]
- 45.Kim SJ, Kumar P, Oh KS. Anterior cruciate ligament reconstruction: autogenous quadriceps tendon-bone compared with bone-patellar tendon-bone grafts at 2-year follow-up. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association 2009; 25: 137–144 DOI: 10.1016/j.arthro.2008.09.014 [DOI] [PubMed] [Google Scholar]
- 46.Han HS, Seong SC, Lee S et al. Anterior cruciate ligament reconstruction : quadriceps versus patellar autograft. Clinical orthopaedics and related research 2008; 466: 198–204 DOI: 10.1007/s11999-007-0015-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lee S, Seong SC, Jo H et al. Outcome of anterior cruciate ligament reconstruction using quadriceps tendon autograft. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association 2004; 20: 795–802 DOI: 10.1016/j.arthro.2004.06.009 [DOI] [PubMed] [Google Scholar]
- 48.Runer A, Wierer G, Herbst E et al. There is no difference between quadriceps- and hamstring tendon autografts in primary anterior cruciate ligament reconstruction: a 2-year patient-reported outcome study. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA 2018; 26: 605–614 DOI: 10.1007/s00167-017-4554-2 [DOI] [PubMed] [Google Scholar]
- 49.Lee JK, Lee S, Lee MC. Outcomes of Anatomic Anterior Cruciate Ligament Reconstruction: Bone-Quadriceps Tendon Graft Versus Double-Bundle Hamstring Tendon Graft. The American journal of sports medicine 2016; 44: 2323–2329 DOI: 10.1177/0363546516650666 [DOI] [PubMed] [Google Scholar]
- 50.Lee S, Seong SC, Jo CH et al. Anterior cruciate ligament reconstruction with use of autologous quadriceps tendon graft. The Journal of bone and joint surgery American volume 2007; 89 Suppl 3: 116–126 DOI: 10.2106/jbjs.G.00632 [DOI] [PubMed] [Google Scholar]
- 51.Kwak YH, Lee S, Lee MC et al. Anterior cruciate ligament reconstruction with quadriceps tendon-patellar bone allograft: matched case control study. BMC musculoskeletal disorders 2018; 19: 45 DOI: 10.1186/s12891-018-1959-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lund B, Nielsen T, Fauno P et al. Is quadriceps tendon a better graft choice than patellar tendon? a prospective randomized study. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association 2014; 30: 593–598 DOI: 10.1016/j.arthro.2014.01.012 [DOI] [PubMed] [Google Scholar]
- 53.Cavaignac E, Coulin B, Tscholl P et al. Is Quadriceps Tendon Autograft a Better Choice Than Hamstring Autograft for Anterior Cruciate Ligament Reconstruction? A Comparative Study With a Mean Follow-up of 3.6 Years. The American journal of sports medicine 2017; 45: 1326–1332 DOI: 10.1177/0363546516688665 [DOI] [PubMed] [Google Scholar]
- 54.Geib TM, Shelton WR, Phelps RA et al. Anterior cruciate ligament reconstruction using quadriceps tendon autograft: intermediate-term outcome. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association 2009; 25: 1408–1414 DOI: 10.1016/j.arthro.2009.06.004 [DOI] [PubMed] [Google Scholar]
- 55.Iriuchishima T, Ryu K, Okano T et al. The evaluation of muscle recovery after anatomical single-bundle ACL reconstruction using a quadriceps autograft. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA 2017; 25: 1449–1453 DOI: 10.1007/s00167-016-4124-z [DOI] [PubMed] [Google Scholar]
- 56.Chen CH, Chuang TY, Wang KC et al. Arthroscopic anterior cruciate ligament reconstruction with quadriceps tendon autograft: clinical outcome in 4–7 years. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA 2006; 14: 1077–1085 DOI: 10.1007/s00167-006-0111-0 [DOI] [PubMed] [Google Scholar]
- 57.Jiang H, Ma G, Li Q et al. Cortical Button Versus Cross-pin Femoral Fixation for Hamstring Anterior Cruciate Ligament Reconstruction: A Meta-analysis of Randomized Controlled Trials. Am J Sports Med 2017: 0363546517717672 [DOI] [PubMed] [Google Scholar]
- 58.Prodromos CC, Joyce BT, Shi K et al. A meta-analysis of stability after anterior cruciate ligament reconstruction as a function of hamstring versus patellar tendon graft and fixation type. Arthroscopy 2005; 21: 1202. e1201–1202. e1209 [DOI] [PubMed] [Google Scholar]
- 59.Kowalk DL, Wojtys EM, Disher J et al. Quantitative analysis of the measuring capabilities of the KT-1000 knee ligament arthrometer. The American journal of sports medicine 1993; 21: 744–747 DOI: 10.1177/036354659302100520 [DOI] [PubMed] [Google Scholar]
- 60.Berry J, Kramer K, Binkley J et al. Error estimates in novice and expert raters for the KT-1000 arthrometer. The Journal of orthopaedic and sports physical therapy 1999; 29: 49–55 DOI: 10.2519/jospt.1999.29.1.49 [DOI] [PubMed] [Google Scholar]
- 61.Ahmad CS, Gardner TR, Groh M et al. Mechanical properties of soft tissue femoral fixation devices for anterior cruciate ligament reconstruction. Am J Sports Med 2004; 32: 635–640 [DOI] [PubMed] [Google Scholar]
- 62.Kousa P, Järvinen TL, Vihavainen M et al. The fixation strength of six hamstring tendon graft fixation devices in anterior cruciate ligament reconstruction. Am J Sports Med 2003; 31: 174–181 [DOI] [PubMed] [Google Scholar]
- 63.Colvin A, Sharma C, Parides M et al. What is the best femoral fixation of hamstring autografts in anterior cruciate ligament reconstruction?: a meta-analysis. Clin Orthop Relat 2011; 469: 1075–1081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Pedowitz RA. Editorial Commentary: Fixation of Soft-Tissue Anterior Cruciate Ligament Grafts in Osteoporotic Bone. Arthroscopy 2017; 33: 1701–1702 DOI: 10.1016/j.arthro.2017.03.032 [DOI] [PubMed] [Google Scholar]
- 65.Domnick C, Herbort M, Raschke MJ et al. Anterior Cruciate Ligament Soft Tissue Graft Fixation in the Elderly: Is There a Reason to Use Interference Screws? A Human Cadaver Study. Arthroscopy 2017; 33: 1694–1700 DOI: 10.1016/j.arthro.2017.03.017 [DOI] [PubMed] [Google Scholar]
- 66.Salmon L, Russell V, Musgrove T et al. Incidence and risk factors for graft rupture and contralateral rupture after anterior cruciate ligament reconstruction. Arthroscopy 2005; 21: 948–957 [DOI] [PubMed] [Google Scholar]
- 67.Sun K, Tian S, Zhang J et al. Anterior cruciate ligament reconstruction with BPTB autograft, irradiated versus non-irradiated allograft: a prospective randomized clinical study. Knee Surg Sports Traumatol Arthrosc 2009; 17: 464–474 DOI: 10.1007/s00167-008-0714-8 [DOI] [PubMed] [Google Scholar]
- 68.Sonnery-Cottet B, Saithna A, Cavalier M et al. Anterolateral ligament reconstruction is associated with significantly reduced ACL graft rupture rates at a minimum follow-up of 2 years: a prospective comparative study of 502 patients from the SANTI study group. Am J Sports Med 2017; 45: 1547–1557 [DOI] [PubMed] [Google Scholar]
- 69.Melugin HP, Johnson NR, Wu IT et al. Is Treatment of Segond Fracture Necessary With Combined Anterior Cruciate Ligament Reconstruction? Am J Sports Med 2018; 46: 832–838 DOI: 10.1177/0363546517745280 [DOI] [PubMed] [Google Scholar]
- 70.van Eck CF, Schkrohowsky JG, Working ZM et al. Prospective analysis of failure rate and predictors of failure after anatomic anterior cruciate ligament reconstruction with allograft. Am J Sports Med 2012; 40: 800–807 [DOI] [PubMed] [Google Scholar]
- 71.Chen T, Zhang P, Chen J et al. Long-Term Outcomes of Anterior Cruciate Ligament Reconstruction Using Either Synthetics With Remnant Preservation or Hamstring Autografts: A 10-Year Longitudinal Study. Am J Sports Med 2017; 45: 2739–2750 DOI: 10.1177/0363546517721692 [DOI] [PubMed] [Google Scholar]
- 72.Ardern CL, Taylor NF, Feller JA et al. Sports participation 2 years after anterior cruciate ligament reconstruction in athletes who had not returned to sport at 1 year: a prospective follow-up of physical function and psychological factors in 122 athletes. Am J Sports Med 2015; 43: 848–856 DOI: 10.1177/0363546514563282 [DOI] [PubMed] [Google Scholar]
- 73.Wright RW, Huston LJ, Spindler KP et al. Descriptive epidemiology of the Multicenter ACL Revision Study (MARS) cohort. The American journal of sports medicine 2010; 38: 1979–1986 DOI: 10.1177/0363546510378645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Dargel J, Schmidt-Wiethoff R, Fischer S et al. Femoral bone tunnel placement using the transtibial tunnel or the anteromedial portal in ACL reconstruction: a radiographic evaluation. Knee Surg Sports Traumatol Arthrosc 2009; 17: 220–227 [DOI] [PubMed] [Google Scholar]
- 75.Gadikota HR, Sim JA, Hosseini A et al. The Relationship Between Femoral Tunnels Created by the Transtibial, Anteromedial Portal, and Outside-In Techniques and the Anterior Cruciate Ligament Footprint. Am J Sports Med 2012; 40: 882–888 DOI: 10.1177/0363546511434276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Chalmers PN, Mall NA, Cole BJ et al. Anteromedial versus transtibial tunnel drilling in anterior cruciate ligament reconstructions: a systematic review. Arthroscopy 2013; 29: 1235–1242 [DOI] [PubMed] [Google Scholar]
- 77.Alentorn-Geli E, Lajara F, Samitier G et al. The transtibial versus the anteromedial portal technique in the arthroscopic bone-patellar tendon-bone anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 2010; 18: 1013–1037 [DOI] [PubMed] [Google Scholar]
- 78.Rahr-Wagner L, Thillemann TM, Pedersen AB et al. Increased risk of revision after anteromedial compared with transtibial drilling of the femoral tunnel during primary anterior cruciate ligament reconstruction: results from the Danish Knee Ligament Reconstruction Register. Arthroscopy 2013; 29: 98–105 [DOI] [PubMed] [Google Scholar]
- 79.Coleridge SD, Amis AA. A comparison of five tibial-fixation systems in hamstring-graft anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 2004; 12: 391–397 [DOI] [PubMed] [Google Scholar]
- 80.van Eck CF, Schreiber VM, Mejia HA et al. “Anatomic” anterior cruciate ligament reconstruction: a systematic review of surgical techniques and reporting of surgical data. Arthroscopy 2010; 26: S2–12 DOI: 10.1016/j.arthro.2010.03.005 [DOI] [PubMed] [Google Scholar]
- 81.Yagi M, Wong EK, Kanamori A et al. Biomechanical analysis of an anatomic anterior cruciate ligament reconstruction. Am J Sports Med 2002; 30: 660–666 [DOI] [PubMed] [Google Scholar]
- 82.Markolf KL, Hame S, Monte Hunter D et al. Effects of femoral tunnel placement on knee laxity and forces in an anterior cruciate ligament graft. J Orthop Res 2002; 20: 1016–1024 [DOI] [PubMed] [Google Scholar]